Abstract
Objective: To compare the effect of glucose-lowering drugs on peripheral nerve and kidney function in prediabetes. Methods: Multicenter, randomized, placebo-controlled trial in 658 adults with prediabetes treated for 1 year with metformin, linagliptin, their combination or placebo. Endpoints are small fiber peripheral neuropathy (SFPN) risk estimated by foot electrochemical skin conductance (FESC < 70 μSiemens) and estimated glomerular filtration rate (eGFR). Results: Compared to the placebo, the proportion of SFPN was reduced by 25.1% (95% CI:16.3–33.9) with metformin alone, by 17.3% (95% CI 7.4–27.2) with linagliptin alone, and by 19.5% (95% CI 10.1–29.0) with the combination linagliptin/metformin (p < 0.0001 for all comparisons). eGFR remained +3.3 mL/min (95% CI: 0.38–6.22) higher with the combination linagliptin/metformin than with the placebo (p = 0.03). Fasting plasma glucose (FPG) decreased more with metformin monotherapy −0.3 mmol/L (95%CI: −0.48; 0.12, p = 0.0009) and with the combination metformin/linagliptin −0.2 mmol/L (95% CI: −0.37; −0.03) than with the placebo (p = 0.0219). Body weight (BW) decreased by −2.0 kg (95% CI: −5.65; −1.65, p = 0.0006) with metformin monotherapy, and by −1.9 kg (95% CI: −3.02; −0.97) with the combination metformin/linagliptin as compared to the placebo (p = 0.0002). Conclusions: in people with prediabetes, a 1 year treatment with metformin and linagliptin, combined or in monotherapy, was associated with a lower risk of SFPN, and with a lower decrease in eGFR, than treatment with placebo.
Keywords: prediabetes, peripheral neuropathy risk, glomerular filtration, antidiabetic drugs, lifestyle intervention
1. Introduction
Type 2 diabetes (T2D) is a slowly progressive disease characterized by advancing hyperglycemia. Prediabetes, the intermediate stage between normoglycemia and T2D, is a heterogeneous condition with several pathophysiological phenotypes [1]. Progression from prediabetes to T2D ranges between 5–10% per year [2,3,4] and this rate depends on the sub-phenotype of prediabetes and the risk factor profile; for instance, the level of diabetes risk score [2,3,4].
People with prediabetes have an increased risk for macro- and microvascular (namely nephropathy, neuropathy and retinopathy), complications [5,6,7,8,9,10,11]. The Rotterdam study reported that people with prediabetes have generalized microvascular dysfunction and sequelae representing end-organ damage typical of diabetes [12]. Based on such evidence it has been proposed that the definition of prediabetes should not only be centered on glucose abnormalities but should also incorporate microvascular involvement among its criteria [13,14,15].
Lifestyle intervention studies have shown a reduction in the relative risk of diabetes by 40–70% in individuals with prediabetes [13]. The Finnish Diabetes Prevention Study (DPS) and the US Diabetes Prevention Program (DPP) showed how lifestyle intervention, as compared to the control group, was associated with a 58% reduction in the risk of diabetes after approximately three years. The benefits of lifestyle modification in delaying the onset of T2D in people with prediabetes have been confirmed in meta-analyses of clinical trials [16]. However, approximately half of the people with hyperglycemia in the DPP failed to achieve normal glycaemia with lifestyle interventions alone, and about 1/3 of them progressed to clinical T2D in an average of 10 years [3]. Several glucose-lowering drugs such as acarbose, metformin, rosiglitazone, pioglitazone, insulin glargine and liraglutide have also shown some benefits for the prevention of diabetes in people with prediabetes, but this benefit disappeared when the drug therapy was stopped [17,18,19,20,21]. The dipeptidyl peptidase-4 inhibitor (DPP4i) linagliptin has demonstrated its cardiovascular safety in placebo-controlled trials. It also demonstrated non-inferiority using a composite marker for cardiovascular outcome compared to glimepiride. Both cases happened when the drugs were administered as monotherapy in relatively early T2D [22]. Recently, the VERIFY study [23] has reported on the efficacy and safety of combining metformin with the DPP4i vildagliptin, compared with metformin monotherapy, in early–untreated T2D. Evidence of higher efficacy and safety of dual therapy versus monotherapy and/or lifestyle changes in people with prediabetes does not exist. Evidence for the prevention of microvascular complications is also limited in prediabetes. Few prevention trials have evaluated the potential benefits of lifestyle modification or drug treatment for preventing such complications. The Da Qing study in China was the first published trial reporting a significant long-term reduction in the incidence of diabetic retinopathy with lifestyle modification [24]. The evidence regarding the benefit of lifestyle changes or the use of metformin for the prevention of microvascular complications was also inconclusive in the US-DPP [17]. The DPS has reported that lifestyle intervention improved retinopathy status [25]. Experimental studies have reported that linagliptin has a protective effect on the microvasculature of the diabetic retina, most likely due to a combination of neuroprotective and antioxidative beneficial effects [26]. Several clinical trials have also shown that linagliptin may slow down the progression of albuminuria in patients with T2D and renal dysfunction [27,28].
So far, no trial has reported if microvascular function can be better preserved by combining lifestyle interventions with early glucose-lowering drug treatment (multiple or monotherapy) in people with either early diagnosed T2D [29] or with prediabetes [30]. Therefore, the primary objective of the Early Prevention of Diabetes Complications in People with Hyperglycaemia (ePREDICE) trial is to assess the effects of early intensive management of prediabetes on several microvascular parameters in comparison with placebo and lifestyle modification. The primary endpoint was a combination of three microvascular endpoints: retinal and peripheral nerve and kidney functions in adults with prediabetes. In this paper we report 1 year results on the intermediate independent effect of each glucose-lowering drug regimen and placebo (i.e., lifestyle intervention alone) only on the peripheral nerve (sudomotor function) and eGFR.
2. Material and Methods
The ePREDICE study design and protocol (including details on the definition and measurement of different variables and outcomes, description of inclusion/exclusion criteria and the recruitment strategy) have been published elsewhere [31]. In sum, the ePREDICE trial is an international, multicenter, randomized, double-blind, parallel-group, placebo-controlled, primary prevention trial initiated by investigators to examine the impact of metformin (Glucophage®, Merck KGaA, Darmstadt, Germany), linagliptin (Trajenta® Boehringer Ingelheim, Ingelheim am Rhein, Germany) and a fixed-dose combination of linagliptin/metformin (Jentadueto® Boehringer Ingelheim, Ingelheim am Rhein, Germany) on microvascular parameters compared with matched-placebo. Participants were randomized with equal probability (1:1:1:1) to metformin 850 mg twice a day; linagliptin 5 mg/once a day plus matched-placebo once a day; fixed-dose combination of linagliptin 2.5 mg/metformin 850 mg twice a day; or matched placebo twice a day. Drug treatment was scheduled for 12 months. All randomized participants were also enrolled in a lifestyle intervention program which included 2 individual sessions followed by 12 group sessions of 1.5 hours duration each. Group sessions were repeated every month. The lifestyle intervention program followed the model developed by the European IMAGE Project [32]. All participants attended in the baseline and 12-month follow-up visits for clinical evaluation of microvascular peripheral and kidney function measurements and OGTT assessment. Primary endpoints for this analysis are the 1 year change in foot electrochemical skin conductance (FESC)—measured in μSiemens by SUDOSCAN®; participants were classified according to FESC as low risk of small fiber neuropathy (SFN: FESC > 70 µS) and high risk of SFN (FESC < 70 µS; includes moderate risk of SFN, FESC 50–70 µS, and severe risk of SFN: FESC < 50 µS)—as well as 1 year change in kidney function with estimated glomerular filtration rate (eGFR). Secondary endpoints are 1 year changes in fasting plasma glucose (FPG), 2 hour post-challenge plasma glucose (2 h-PG) and body weight (BW). The study protocol did not change since the previous publication [32]. Here we are only reporting baseline characteristics of the study participants and effects of the study intervention on two single independent components of the primary study composite outcome, i.e., the estimated glomerular filtration rate (eGFR) and small fiber peripheral neuropathy (SFPN) risk at 12 months. In addition, we report the effect of the intervention on body weight (BW) and fasting plasma glucose (FPG).
2.1. Statistical Analysis
The present analysis is based on the full analysis set (FAS) available for the baseline and 12 month follow-up in the central database by September 26, 2019. In this report we analyze the 1 year changes in the variables of interest in those participants randomized at baseline, who also completed the treatment assigned and attended the 1-year appointment for clinical re-assessment (n = 658). For continuous variables, descriptive statistics (mean, SD, percentages and 95% CI) were used. For the comparison of treatment arms at baseline we used a two-sided Mann–Whitney U-test with significance level (p < 0.05) for independent samples. We assessed whether each of the 3 active drugs independently (metformin alone, linagliptin alone or the fixed-dose combination of linagliptin/metformin) had a superior effect on the selected variables compared to the placebo. The 1 year changes for paired samples were analyzed using the Wilcoxon test for continuous variables and the McNemar test for categorical variables. In addition, the mean change obtained from the ANCOVA—adjusted for its baseline value—was calculated for the primary outcome variables. The incidence of serious adverse events (SAE) and adverse effects (AE) of special interest to each study drug compared to the placebo are also presented.
2.2. Ethical Issues
The study was approved by all local ethic committees of the participating centers and all the National Medicine agencies of the participating countries. All participants received detailed information about the study, including the explanation of their right to withdraw their participation at any time. All participants signed written informed consent forms. All centers followed the European Good Clinical Practice Guidelines and the Declaration of Helsinki as revised in 2008.
3. Results
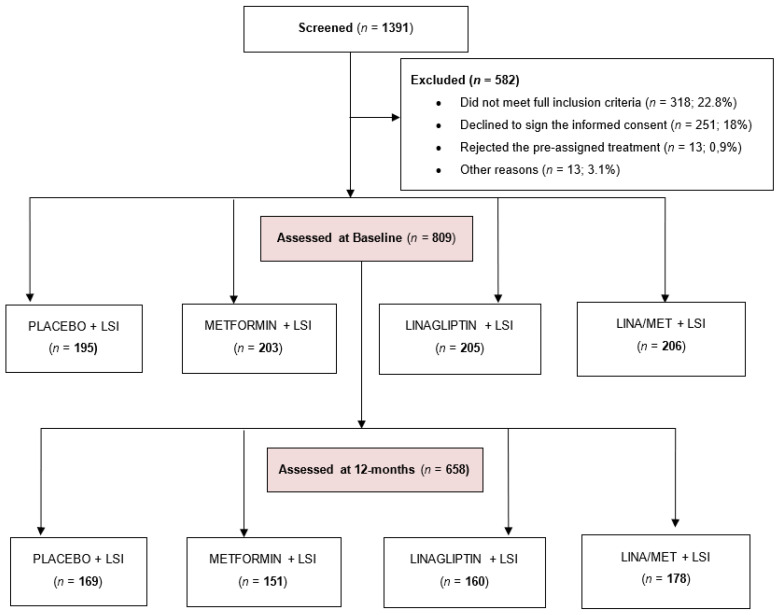
Figure 1 shows the flow-chart of the study population. A total of 1391 potential eligible individuals were screened using a standard 2 h oral glucose tolerance test (OGTT), and 582 (41.8%) of them were excluded: 318 people (22.8%) because they did not meet all the inclusion criteria; 251 (18.0%) declined to sign the informed consent; and 13 people (0.9%) rejected the pre-assigned treatment. In total, 809 participants were fully assessed at baseline and started the assigned drug treatment. After randomization, no demographic differences between the four resulting study groups were observed.
Figure 1.
Flow-chart of ePREDICE study population.
During the first year of the trial, 151 participants (18.6%) withdrew from the study. The discontinuation rates of assigned study drugs were 13.3% (26 participants) in the placebo group; 25.6% (52 participants) in the metformin group; 21.9% (45 participants) in the linagliptin group; and 13.6% (28 participants) in the combined linagliptin/metformin group. After 12 months, 658 participants (81.3%) attended the 1 year follow-up appointment for clinical reassessment. In people who discontinued treatment we did not unmask the assigned drug unless the participant had a medical reason for it. Despite drug withdrawal, we encouraged these participants to continue in the lifestyle intervention program and to attend scheduled clinical appointments. People who discontinued the medication have been excluded from this analysis.
No differences in the variables of interest were observed at baseline between the four study groups, nor among all randomized groups, nor those who completed the 1 year treatment (Table 1).
Table 1.
Characteristics of participants at baseline examination by study arm (n = 809).
| Variables | Placebo (n = 195) |
Metformin (n = 203) |
Linagliptin (n = 205) |
Metformin + Linagliptin (n = 206) |
p-Value |
|---|---|---|---|---|---|
| Percent of females | 57.7 | 58.0 | 58.9 | 56.8 | 0.975 |
| Percent of smokers | 14.4 | 15.6 | 13.2 | 13.5 | 0.793 |
| Percent with family history of diabetes | 36.5 | 41.0 | 37.8 | 46.4 | 0.121 |
| Mean age in years (SD) | 58.5 (7.5) | 58.1 (7.5) | 58.1 (7.4) | 58.1 (8.0) | 0.936 |
| Mean weight in kg (SD) | 84.7 (16.9) | 83.1 (15.8 | 84.0 (16.9) | 84.4 (16.1) | 0.757 |
| Mean BMI in kg/m2 (SD) | 30.9 (5.1) | 30.2 (4.8) | 30.8 (5.5) | 30.6 (4.6) | 0.500 |
| Waist circumference in cm in men (SD) | 104.5 (15.7) | 105.2 (13.6) | 105.1 (12.4)] | 107.6 (10.6) | 0.791 |
| Waist circumference in women in cm (SD) | 101.2 (12.2) | 98.9 (11.4) | 99.2 (11.9) | 98.4 (11.2) | 0.791 |
| Systolic blood pressure (SBP) in mmHg (SD) | 131 (16.0) | 132 (17.1)] | 132 (18.0) | 132 (17.1) | 0.967 |
| Diastolic blood pressure (DBP) in mmHg (SD) | 81 (10.9) | 82 (10.5) | 82 (11.5) | 81 (10.2) | 0.786 |
| Fasting plasma glucose in mmol/L (SD) | 6.3 (0.5) | 6.3 (0.5) | 6.3 (0.5) | 6.4 (0.5) | 0.119 |
| Two-hour plasma glucose in mmol/L (SD) | 8.1 (1.7) | 8.2 (1.7) | 8.2 (1.7) | 8.1 (1.8) | 0.687 |
| Serum total cholesterol (in mmol/L (SD) | 5.3 (1.2) | 5.3 (1.2) | 5.3 (1.1) | 5.2 (1.1) | 0.652 |
| Serum HDL cholesterol in mmol/L (SD) | 1.3 (0.3) | 1.3 (0.4) | 1.4 (0.4) | 1.3 (0.5) | 0.885 |
| Serum LDL cholesterol in mmol/L (SD) | 3.4 (0.9) | 3.3 (1.1) | 3.3 (0.9) | 3.3 (0.8) | 0.755 |
| Serum triglycerides in mmol/L (SD) | 1.5 (0.7) | 1.5 (1.1) | 1.5 (0.7) | 1.6 (0.9) | 0.474 |
| Percentage of HbA1c (SD) | 5.9 (2.6) | 5.8 (0.4) | 5.8 (0.4) | 5.8 (0.4) | 0.683 |
| eGFR CKD-EPI in mL/min per 1.73 m2 (SD) | 94.0 (9.0) | 94.3 (9.4) | 94.0 (10.0) | 94.9 (9.9) | 0.729 |
| Mean ESC of feet in µSiemens (SD) | 79.2 (10.6) | 78.5 (9.8) | 79.6 (22.5) | 78.0 (9.8) | 0.652 |
| Glycemic categories (%) | 0.200 | ||||
| Isolated IGT | 35.1 | 33.5 | 28.3 | 24.3 | |
| Isolated IFG | 37.4 | 35.8 | 38.4 | 39.6 | |
| IGT + IFG combined | 27.5 | 30.7 | 33.3 | 36.0 | |
| Percent with hypertension (SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg or antihypertensive drug use) | 58.1 | 59.0 | 58.4 | 60.8 | 0.940 |
| Percent with hypercholesterolemia (Serum total cholesterol ≥ 200 mg or lipid lowering drug use) | 65.3 | 64.2 | 66.7 | 65.8 | 0.958 |
| Percent with overweight (BMI 25–29 kg/m2) | 25.2 | 25.0 | 31.5 | 29.7 | 0.326 |
| Percent with obesity (BMI ≥ 30 kg/m2) | 52.3 | 50.0 | 47.0 | 53.6 | 0.535 |
| Percent with abdominal obesity (Men: WC ≥ 94 cm) | 41.0 | 42.9 | 41.4 | 46.0 | 0.856 |
| Percent with abdominal obesity (Women: WC ≥ 88 cm) | 59.0 | 57.1 | 58.6 | 54.0 | 0.856 |
| Percent with diabetic retinopathy (ETDRS > 14) | 3.4 | 4.6 | 4.9 | 3.9 | 1.000 |
| Percent with peripheral neuropathy (feet ESC [µS] <50 or hands ESC [µS] <40) | 3.6 | 6.6 | 6.8 | 7.2 | 0.359 |
| Percent with nephropathy (Albumin: creatinine ratio > 30 mg/dL) | 4.5 | 4.7 | 8.2 | 5.0 | 0.280 |
BMI: body mass index; HDL: high-density lipoproteins; LDL: low-density lipoproteins; HbA1c: glycated hemoglobin; eGFR CKD-EPI: estimated glomerular filtration rate–chronic kidney disease epidemiology; ESC: electrochemical conductance; IGT: impaired glucose tolerance; IFG: impaired fasting glucose; ETDRS: early treatment diabetes retinopathy study.
Table 2 shows the baseline-adjusted mean and proportion differences, and their corresponding 95% confidence intervals (95% CI), between baseline and 1 year follow-up within each study group and compared to the placebo. After 1 year of treatment, the proportion of participants with high risk of SFPN increased by 29.6% in the placebo group, while the increase was significantly lower in the three active-drug groups: 4.6% in the metformin group; 12.4% in the linagliptin group; 10.1% with the combination linagliptin/metformin; and 9.6% when considering the three active-drug groups together (p < 0.001 for all comparisons). Compared to the placebo, the proportion of SFPN high-risk estimation by FESC was reduced by 25.1% (95% CI:16.3; 33.9) with metformin alone; by 17.3% (95% CI 7.4; 27.2) with linagliptin alone; by 19.5% (95% CI 10.1; 29.0) with the combination linagliptin/metformin; and by 20.0% (11.5; 28.5) taking together the three active drugs (p value <0.0001 for all comparisons). The 1 year kidney function, measured by eGFR-CKD-EPI per 1.73 m2, remained significantly higher with the fixed-dose combination linagliptin/metformin (3.3 mL/min/year, 95% CI: 0.37; 6.22), p = 0.0270, than with placebo, but not significantly with metformin monotherapy (3.0 mL/min/year: 95% CI; −0.01; 6.01), p = 0.0511, nor with linagliptin monotherapy (1.3 mL/min/year; 95% CI: −2.13; 4.73), p = 0.4577. After 1 year of treatment, FPG was significantly lower with metformin monotherapy (−0.3 mmol/L, 95%CI: −0.48; −0.12), p = 0.0009, with the combination metformin/linagliptin (−0.2 mmol/L, 95% CI: −0.37; −0.03), p = 0.0219, and with the three active drugs taken together (−0.2 mmol/L, 95%CI: −0.349; −0.050), p = 0.008, than with placebo. However, no difference between linagliptin monotherapy and placebo was observed. No significant reductions were observed between any of the three active drugs and placebo for 2 h-PG. The 1 year reduction in body weight was significantly greater (−2.0 kg/year, 95% CI: −5.65; −1.65), p = 0.0006, with metformin monotherapy and with the combination metformin/linagliptin (−1.9 kg/year, 95% CI: −3.02; −0.97), p = 0.0002, than with placebo. However, no significant reductions in body weight were observed with linagliptin monotherapy (−0.1 kg/year; 95% CI: 0.15; 0.95; p = 0.5822) nor with the three active drugs taken together (−1.5 kg/year; 95% CI: −4.4; 1.4; p = 0.316) compared to placebo.
Table 2.
Changes after 1-year treatment by study group and comparisons with placebo in participants who completed the 1-year follow-up examination (n = 658).
| Variable | Placebo (n = 169) |
Metformin Monotherapy (n = 151) |
Linagliptin Monotherapy (n = 160) |
Metformin/Linagliptin Combination (n = 178) |
|---|---|---|---|---|
| Body weight (kg) | ||||
| Mean (SD) baseline | 84.9 (17.0) | 84.0 (16.8) | 84.5 (16.9) | 84.0 (17.0) |
| Mean (SD) year1 | 83.8 (17.0) | 80.9 (16.1) | 83.3 (17.3) | 80.9 (16.0) |
| Mean diff. year1-baseline (95% CI) | −1.1 (−1.8; −0.5) | −3.1 (−4.1; −2.2) | −1.2 (−2.0; −0.4) | −3.1 (−3.7; −2.4) |
| Baseline-adjusted year1 mean (SD) | 83.2 (17.0) | 81.2 (16.1) | 83.1 (17.1) | 81.3 (16.6) |
| Mean difference with placebo (95% CI); p value | 2.0 (−5.6532; −1.6532); p = 0.0006 |
0.1 (.1521; 0.9523); p= 0.5822 |
1.9 (−3.0291; −0.9709) p = 0.0002 |
|
| Waist circumference in males (cm) | ||||
| Mean (SD) baseline | 104.8 (11.4) | 104.8 (11.5) | 105.6 (11.7) | 107.7 (12.4) |
| Mean (SD) year1 | 105.0 (11.1) | 103.3 (11.4) | 104.8 (11.8) | 104.6 (12.6) |
| Mean diff. year1-baseline (95% CI) | 0.2 (−3.4; 3.9) | −1.5 (−3.9; 0.8) | −0.8 (−2.3; 0.8) | −3.1 (−4.5; −1.7) |
| Baseline-adjusted year1 mean (SD) | 105.6 (11.2) | 103.8 (11.3) | 104.9 (11.8) | 103.5 (12.7) |
| Mean difference with placebo (95% CI); p value | 1.8 (−4.2780; 0.6780) p = 0.1539 |
0.7 (−3.1945; 1.7945) p = 0.5813 |
−2.1 (−4.6335; 0.4335) p = 0.1039 |
|
| Waist circumference in females (cm) | ||||
| Mean (SD) baseline | 101.4 (12.3) | 99.8 (11.8) | 100.0 (11.9) | 98.4 (12.4) |
| Mean (SD) year1 | 99.4 (12.7) | 96.4 (11.9) | 98.5 (12.1) | 96.2 (12.8) |
| Mean diff. year1-baseline (95% CI) | −2.0 (−3.6; −0.4) | −3.4 (−5.0; −1.7) | −1.5 (−3.0; −0.1) | −2.2 (−3.7; −0.8) |
| Baseline-adjusted year1 mean (SD) | 98.1 (12.6) | 96.5 (12.2) | 98.4 (12.0) | 97.4 (12.7) |
| Mean difference with placebo (95% CI); p value | −1.6 (−4.3348; 1.1348) p = 0.2506 |
0.3 (−2.3716 to 2.9716) p = 0.8253 |
−0.7 (−3.3725; 1.9725) p = 0.6068 |
|
| Systolic blood pressure (mmHg) |
||||
| Mean (SD) baseline | 132 (13.7) | 132 (14.0) | 132 (14.7) | 131 (14.8) |
| Mean (SD) year1 | 128 (13.6) | 127 (15) | 129 (16.1) | 128 (14.1) |
| Mean diff. year1-baseline (95% CI) | −4.2 (−6.5; −1.8) | −4.9 (−7.5; −2.2) | −2.6 (−5.3; −0.0) | −2.9 (−5.2; −0.6) |
| Baseline-adjusted year1 mean (SD) | 128 (13.6) | 127 (14.9) | 129 (16.2) | 128 (13.9) |
| Mean difference with placebo (95% CI); p value | −1.0 (−4.1347; 2.1347) p = 0.5307 |
1.0 (−2.2378; 4.2378) p = 0.5439 |
0.0 (2.9056; 2.9056) p = 1.0 |
|
| Diastolic blood pressure (mmHg) | ||||
| Mean (SD) baseline | 81 (10.1) | 82 (9.8) | 81 (10.5) | 81 (9,4) |
| Mean (SD) year1 | 79 (9.6) | 78 (9.0) | 79 (9.4) | 78 (9.4) |
| Mean diff. year1-baseline (95% CI) | −1.5 (−3.2; 0.1) | −4.5 (−6.3; −2.7) | −1.3 (−3.1; 0.5) | −2.9 (−4.5; −1.3) |
| Baseline-adjusted year1 mean (SD) | 79 (9.6) | 77 (9.3) | 79 (9.4) | 78 (9.4) |
| Mean difference with placebo (95% CI); p value | −2.0 (−4.0841; 0.0841) p = 0.0599 |
0.0 (−2.0622; 2.0622) p = 1.0 |
1.0 (−3.0064 to 1.0064) p = 0.3276 |
|
| Fasting plasma glucose (mmol/L) | ||||
| Mean (SD) baseline | 6.3 (0.8) | 6.3 (0.8) | 6.37 (0.6) | 6.4 (0.8) |
| Mean (SD) year1 | 6.4 (0.7) | 6.1 (0.9) | 6.4 (0.8) | 6.2 (0.9) |
| Mean diff. year1-baseline (95% CI) | 0.1 (−0.03; 0.2) | −0.2 (−0.3; –0.04) | 0.03 (−0.1; 0.1) | −0.2 (−0.3; −0.1) |
| Baseline-adjusted year1 mean (SD) | 6.4 (0.7) | 6.1 (0.9) | 6.4 (0.8) | 6.2 (0.8) |
| Mean difference with placebo (95% CI); p value | 0.3 (−0.4764; −0.1236) p = 0.0009 | 0,0 (−0.1628; 0.1628) p = 1.0 |
−0,2 (−0.3709; −0.0291) p = 0.0219 |
|
| 2-hour plasma glucose (mmol/L) | ||||
| Mean (SD) baseline | 8.2 (1.9) | 8.3 (2.1) | 8.3 (2.2) | 8.1 (2.3) |
| Mean (SD) year1 | 7.9 (2.2) | 8.0 (2.4) | 7.6 (2.0) | 7.6 (2.3) |
| Mean diff. year1-baseline (95% CI) | −0.3 (−0.6; 0.03) | −0.3 (−0.7; 0.02) | −0.7 (−1.0; −0.4) | −0.5 (−0.8; −0.2) |
| Baseline-adjusted year1 mean (SD) | 7.9 (2.2) | 7.9 (2.4) | 7.6 (2.0) | 7.7 (2.3) |
| Mean difference with placebo (95% CI); p value | 0.0 (−0.5060; 0.5060) p = 1.0 |
−0.3 (−0.7568; 0.1568) p = 0.1973 |
−0.2 (−0.6757 to 0.2757 p = 0.4088 |
|
| Serum triglycerides (mmol/L) | ||||
| Mean (SD) baseline | 1.49 (0.7) | 1.63 (1.1) | 1.43 (0.9) | 1.53 (0.9) |
| Mean (SD) year1 | 1.50 (0.9) | 1.60 (1.1) | 1.40 (0.6) | 1.50 (0.8) |
| Mean diff. year1-baseline (95% CI) | 0.01 (−0.1; 0.1) | 0.03 (−0.1; 0.2) | −0.03 (−0.1; 0.1) | −0.03 (−0.2; 0.1) |
| Baseline-adjusted year1 mean (SD) | 1.5 (0.9) | 1.6 (1.1) | 1.5 (0.6) | 1.5 (0.8) |
| Mean difference with placebo (95% CI); p value | 0.1 (0.1202; 0.3202) p = 0.3722 |
0.0 (−0.1668; 0.1668) p = 1.0 |
0.0 (−0.1851; 0.1851) p = 1.0 |
|
| HbA1c (%) | ||||
| Mean (SD) baseline | 6.0 (0.6) | 5.9 (0.4) | 5.7 (0.4) | 5.9 (0.4) |
| Mean (SD) year1 | 5.8 (0.4) | 5.7 (0.4) | 5.6 (0.4) | 5.6 (0.4) |
| Mean diff. year1-baseline (95% CI) | −0.2 (−0.7; 0.3) | −0.2 (−0.3; −0.1) | −0.1 (−0.2; −0.1) | −0.3 (−0.3; −0.2) |
| Baseline-adjusted year1 mean (SD) | 5.70 (0.42) | 5.68(0.40) | 5.64 (0.43) | 5.60 (0.38) |
| Mean difference with placebo (95% CI); p value | 0.02 (−0.5001; 0.5001) p = 0.9853 |
0.06 (−0.6001 to 0.5001) p = 0.8710 |
−0.1 (−0.5610; 0.3610) p = 0.2318 |
|
| eGFR CKD-EPI (mL/min per 1.73 m2 | ||||
| Mean (SD) baseline | 93.4 (10.6) | 94.3 (14.0) | 93.6 (13.6) | 94.7 (13.7) |
| Mean (SD) year1 | 90.2 (8.9) | 93.7 (10.5) | 91.8 (15.8) | 94.4 (11.4) |
| Mean diff. year1-baseline (95% CI) | −3.2 (−5.6; −0.8) | −0.6 (−2.0; 0.8) | −1.8 (−4.5; 0.9) | −0.3 (−1.7; 1.1) |
| Baseline-adjusted year1 mean (SD) | 90.6 (15.9) | 93.6 (10.3) | 91.9 (15.8) | 93.9 (11.4) |
| Mean difference with placebo (95% CI); p value | 3.0 (−0.0148; 6.0148) p = 0.0511 |
1.3 (−2.1397; 4.7397) p = 0.4577 |
3.3 (0.3780; 6.2220) p = 0.0270 |
|
| Proportion of SFPN high-risk at baseline | 26.3 | 39.4 | 34.8 | 38.6 |
| Proportion of SFPN high-risk at 1-year | 34.1 | 41.2 | 39.1 | 42.5 |
| Difference (1-year change) in high-risk proportion adjusted by baseline | 29.6 | 4.5 | 12.3 | 10.1 |
| Difference 1-year (change) in high-risk proportion compared to placebo (95%CI), p value |
- | −25.1 (−16.3; −33.9) <0.0001 |
−17.3 (−7.4; −27.2) <0.0001 |
−19.5 (−10.1; −29.0) <0.0001 |
In comparison with the placebo, no significant changes after 1 year of treatment were observed in other cardiometabolic risk factors such as blood pressure, waist circumference, serum triglycerides and HbA1c.
3.1. Drug Adherence
In a random subsample of 200 participants (50 patients per study arm), we monitored the participants’ drug adherence during the whole treatment period with the electronic Medication Event Monitoring Systems (MEMS®). The compliance with the assigned study medication was considered optimal (95% or more of the days analyzed) by 75 of the patients. No differences in drug compliance were observed between the four study groups during one year of treatment.
3.2. Safety Analysis
Only four SAEs, each in four different patients, were reported, none of them related to the study medication as determined by the responsible clinical investigator. The drug treatment was immediately unmasked in these four people. Additionally, the drug treatment was unmasked by local investigators in seven more people for different medical reasons, such as scheduled surgery or acute illness. Nevertheless, participants were asked to resume the assigned study treatment in an open-label fashion after the resolution of the event that required the unmasking.
A total of 52 participants (6.0%) reported a drug-related AE (24 in the metformin group, 18 in the linagliptin/metformin group, 6 in the placebo group and 4 in the linagliptin group). The most frequent AEs were diarrhea (46.2%) and unspecific digestive intolerance (36.5%). These symptoms were more frequent with metformin (22.2%) and with the combination linagliptin/metformin (15.3%). Symptomatic hypoglycemia, clinically relevant hyperamylasemia or acute pancreatitis were not reported during the period analyzed.
4. Discussion
Generally speaking, there is a paucity in the scientific literature of interventional studies on the relationship between prediabetes and microvascular complications, specifically to nephropathy and neuropathy, which are the two main focuses of this manuscript. This makes our study a novel one [30]. The ePREDICE trial is an international, investigator-initiated, randomized, placebo-controlled trial aiming at comparing the effects of different glucose-lowering drugs added to lifestyle management with intervention based on lifestyle management alone on the preservation of microvascular function in individuals with prediabetes. In this report, we focus on the effects of three different therapeutic strategies on kidney and sudomotor functions as well as glycemic parameters.
Participants were predominantly middle-aged, Caucasian, female and overweight/obese. The majority were ex-smokers or current smokers and were taking antihypertensive and lipid-lowering drugs. The randomization procedure efficiently generated well-balanced groups in terms of risk stratification.
The number of participants who completed the assigned drug treatment (81.3%; 658/809) can be considered high in comparison with other primary prevention trials combining anti-diabetic drugs and lifestyle modification, where a high proportion of withdrawals usually occur [17]. In our study, the proportion of participants who discontinued the assigned study treatment during the 1 year follow-up did not differ between the four study groups. Regarding kidney function preservation, linagliptin did not produce significant changes in eGFR compared to the placebo at weeks 6, 12, 18 and 24 in the MARLINA-T2D study, a randomized, placebo-controlled, multicenter, Phase IIIb clinical trial. This study suggested that linagliptin may not influence kidney function in patients with T2D within 24 weeks of treatment [27]. SGLT2 inhibitors are known to be effective in preventing kidney function decline with an effect of approximately 0.9 ml per minute per 1.73 m2 (95% CI, 0.61 to 1.25) per year in saved renal function compared to placebo in adults with or without T2D who had an estimated glomerular filtration rate (GFR) of 25 to 75 ml per minute per 1.73 m2 of body surface area [33]. In the DECLARE-TIMI-58 randomized trial [34], patients generally had good eGFR at baseline, which is the case in our study. The authors analyzed the extent to which dapagliflozin and placebo were associated with a decrease in eGFR in people with T2D and eGFR > 90 ml/min at baseline. The difference between groups was 2 ml/min during a 4-year treatment, i.e., 0.5 ml/min per year of preventive effect in favor of dapagliflozin. From this perspective the effect observed in our study seems relatively good. In 1 year of treatment, the eGFR only decreased by 0.3 mL/min in the metformin-alone group, 0.6 mL/min with the combination metformin/linagliptin and 1.8 mL/min in the linagliptin-alone group compared with a greater decrease of 3.2 mL/min per year in the placebo group. Therefore, it is essential to confirm if the preventive effect will persist over a longer time.
A study conducted in active Finnish workers [35] assessed sudomotor function with FESC. Participants with the lowest fitness level were involved in a 12 month training program with recording of their weekly physical activity and a final fitness level evaluation. Significant differences in BMI as well as waist and body fat were seen according to SUDOSCAN risk score classification. Correlation between the SUDOSCAN risk score and estimated VO2max was r = −0.57, p < 0.0001 for women and −0.48, p < 0.0001 for men. A significant increase in estimated VO2max in hand and foot ESC and in SUDOSCAN risk score was observed after lifestyle intervention; it was more important in people with the highest weekly activity during the intervention. This was the first study showing that SUDOSCAN could be used to assess cardio-metabolic disease risk status in a working population and to evaluate individual lifestyle interventions. To our knowledge, the ePREDICE trial is the first randomized, controlled trial in prediabetes assessing the effect of lifestyle intervention in combination with glucose-lowering drugs compared with lifestyle modification intervention on peripheral nerve function.
More recently the GRADE study has also reported no differences among the interventions with respect to the development of microvascular outcomes; the mean overall rate (i.e., events per 100 participant-years) of renal impairment was 2.9, and of diabetic peripheral neuropathy, 16.7 [29].
A possible explanation for the small changes in blood glucose observed in our study could be the mix of people with IFG, IGT and IFG + IGT in the study sample. Future analyses should explore whether a stratification by IFG and IGT separately would produce similar results.
Another interesting finding of our study is a greater reduction in body weight observed with metformin monotherapy and with the fixed-dose combination metformin/linagliptin, but not with linagliptin monotherapy, compared to the placebo. The weight loss in the groups containing metformin in our study, approximately 2%, was somewhat higher than what has been reported in other randomized controlled trials. A systematic review and meta-analysis reported an average weight loss of 1.1 kg with metformin used for varying periods [36]. The randomized design of the trial makes it unlikely that the difference favoring intervention groups containing metformin can be explained by a better adherence to lifestyle intervention. However, in the US Diabetes Prevention Program, the metformin group also achieved a similar weight loss of 2.1% after 2 years; remarkably, this lasted for the next 10 years [37].
One-year differences in other cardiovascular risk factors such as blood lipids and blood pressure were non-significant between the active drug groups and placebo. This finding is consistent with other drug trials in prediabetes using similar therapeutic regimens [38,39]. Although the study protocol encouraged the use of antihypertensive and lipid-lowering drugs when necessary, according to the current guideline recommendations [40], we do not have information on the proportion of participants taking these drugs during the course of the study.
Recently the VERIFY study reported that early combination of metformin and DPPIVi drugs in patients with untreated T2D was associated with higher reductions of HbA1c and FPG, both short-term and long-term, than with metformin in monotherapy [23]. Evidence on drug therapy and lifestyle modification combined, compared with lifestyle intervention alone, for the prevention of T2D is scarce [41,42,43,44,45,46,47]. The results of available studies should be interpreted with caution because in general they were small, short intervention time, non-randomized or open-label trials where systematic bias cannot be excluded. In general, these trials do not support the use of pharmacotherapy in combination with lifestyle intervention to lower the risk in individuals with prediabetes.
5. Limitations
The e-PREDICE study was challenging to implement because of its complex multinational, non-commercial design using pharmacologic intervention, carried out by independent academic investigators with 2-pill/day requirements of four different combined pharmacologic regimens in asymptomatic people without medical complaints. Despite these challenges, the mean percentage of days with optimal drug compliance (higher than 80% of the prescribed dose) was 75% in the monitored participants. However, in 25% of participants the compliance with the evening dose was lower than 80%. This suboptimal compliance of daily doses may have contributed to the small differences observed between the placebo and active drug groups. Missing data due to participant withdrawal is also an important limitation when interpreting the results of primary prevention trials. However, participants who discontinued drug treatment were asked to maintain the lifestyle recommendations and to remain in the study for future observational follow-up. In the DPP, a similar proportion of participants discontinued metformin during the first six months of treatment, and this proportion remained stable for the next two and five years [17]. In the DPP, the adherence to placebo was consistently higher than adherence to metformin, which contrasts with our study. Using the same definitions than other pharmacological trials conducted in people with prediabetes, we identified a similar number of SEAs and AEs during the treatment period [48]. The number of self-reported gastrointestinal AEs associated with the study medication was slightly higher in the metformin group than in the other study arms, but this was not statistically significant. Similar figures have been reported by other trials in prediabetes [48].
The effects of both lifestyle modification and pharmacologic treatment on diabetes prevention are usually observed after several years of intervention. However, the potential benefits of pharmacological treatment in contrast to lifestyle intervention disappear when glucose-lowering drug therapy is stopped [49,50,51,52].
One year is a short period of time, where fluctuations of blood glucose are common. A longer follow-up is needed before drawing any conclusions on the reduction in diabetes incidence or the regression to normoglycemia. The encouraging results of ePREDICE on risk factors such as body weight and microvascular kidney and peripheral nerve functions can be considered to be of relevance, since the objective was to prevent early microvascular impairment in prediabetes.
6. Conclusions
In people with prediabetes, one-year treatment with metformin and linagliptin, either in monotherapy or combination, was associated with a lower risk of small fiber peripheral neuropathy, and with a lower decrease in estimated glomerular filtration rate, than with placebo. In addition, a greater reduction in FPG and body weight was observed with the metformin monotherapy and the fixed-dose combination metformin/linagliptin than with the linagliptin monotherapy or the placebo.
Acknowledgments
Members of the e-PREDICE Consortium: Steering Committee: Jaakko Tuomilehto, Rafael Gabriel, Jaana Lindström, Jesús Egido, Andrea Natali, José Carlos Pastor, Michael Brainin, Marcus Lind, Luis Silva, Peter Schwartz, Aleksandra Gilis-Januszewska. Safety Committee: Carmen Suárez Fernández: Hospital University La Princesa. Madrid, Spain. Beverly Balkau, INSERM Veifville. France. Matti Uusitupa, Institute of Public Health and Clinical Nutrition. University of Eastern Finland, Kuopio, Finland. Internal Ethic Committee: Julio Romero. Hospital University La Princesa, Madrid, Spain. Lars Ryden. Karolinska Institute, Stockholm, Sweden. External Scientific Advisory Board: Ralph DeFronzo, University of Texas. San Antonio, Texas, USA. Manuel Serrano Ríos. Universidad Complutense, Madrid, Spain. Michael Roden, German Center for Diabetes Research (DZD) Heinrich Heine University Düsseldorf, Düsseldorf, Germany. John Nolan, European Diabetes Forum, European Association for the Study of Diabetes, Trinity College Dublin, Ireland. Work package (WP). WP1: coordinador. EVIDEM CONSULTORES Rafael Gabriel, Jaakko Tuomilehto, Nisa Boukichou, Tania Acosta, Ruy López-Ridaura, Luis Silva, Eliana del Águila, Ana Rosón. WP2. CLINICAL CENTRES: Spain. Primary Care centres of SERMAS (Servicio Madrileño de Salud), Madrid. Tomás Gómez-Gascón, Juan Carlos Abánades Herranz, María Esther Sánchez Carranza, Alicia Rodríguez Blanco, Fernando Villasante Claudios,Consuelo Ugarte Pérez, Belén Peláez Raposo, Beatriz Cáceres Sánchez, Sergio González Gasca; Margarita Herrero Delgado, Isabel García Del Río, Mª Lorena Rodríguez Pérez, Mª Carmen Reyes Madridejos, Mª Carmen Castillo López, Mª Jesús Paloma Huerga González, Ana Alayeto Sánchez, Carmen Pascual Díez, Esperanza Villar Coloma, Tirso Galiano Arroyo, Mª Olga Peña Peña, Mª Elena Pejenaute Labari, Mª Mercedes Rojo Tardón, Mª Teresa Recio García, María Campos López-Carrión, Sara Criado Jorge, Virginia García Campo, Almudena Pazos González, Aranzazu Pérez Medina, Ricardo Benito Fernández, Mercedes Ricote Belinchón, Mª Teresa Sánchez-Villares Rodríguez, Noelia Polo Fernández, Antonio Cabrera Majada, Eva María Revuelta Marinez , Itziar Vázquez Carrión, Mª Nuria Fernández De Cano Martín, Manuel Gutiérrez Cabanas, Soledad Fernández Saavedra, Yolanda Jiménez Aguilar, Mª Ángeles Rodríguez Loarce, Emilia Pedroche Morales, Teresa Nieto Monreal, María Begoña Hernández Olivares, Carmen Domínguez Encinas, Ana Martínez-Cabrera Peláez, Mª Inés Casas Jiménez, Pilar Pérez Egea, Concepción Espariz Campano, Ángeles Brieva García, Mª Azucena Saez Berlana, Carlos Casanova García, Mª Carmen Belinchón Moya, Mª Dolores Parejo Pablos, Elisa Varona Lahuerta, Esther Labrador Arranz, Mª Ángeles Conde Llorente, Mª Teresa Gómez Martínez, Milagros Velázquez García, Mª Patrocinio Verde González, Mª Rosario Campo Martínez, Mª Rosario Del Álamo Gutiérrez, Mª Victoria Cantera Urcía, Alejandra González Esteban, Laura Rodríguez Cortizo, Sabrina Sosa Alés, Eva Torres Cantero, Idoia Baíllo Peña, Tamara García López, Cristina Calle Domínguez, Inmaculada Peña Sainz, Mª Antonia Minguito Lobos, Consuelo Viamonte Andrés, Francisco Manuel García García, José María Lobos Bejarano, Raquel Juez Pimienta, Emiliana Villares Motino, Elvira Pérez Peñas, Silvia Jiménez, Laura Manuyama Pacaya, Carmen Morales Guevara, Carmen Melero González, Blanca Novella Arribas, Marta Cuevas, Belén Sierra García, Marta Ruiz, Amelia González Gamarra, Rosa Mª Sánchez Alcalde, Belén Peláez Raposo, Ángela Gallego Arenas, Mª Soledad Mayayo Vicente, Javier López González, Manuel Jovino Arango Victoria, Ana María Santos Caballero, Isabel Jimeno, Juana Iribertegui, Ramón María Salgado, María Olga Ortega de Santos, María Gema García, María José LLoréns Balducel, Juan Carlos de la Fuente, Claudia Fernández Illen, Beatriz Manrique Olmedo, Tati Arévalo Gallego, Juan Machuca Gómez, Esther San José Blázquez, Teresa Castellanos Ruiz, Macarena Espejo Saucedo, María Esther Fernández Yedra, Carmen Torres Martínez, Ángel Lindo Torres, Víctor Raúl Montes Pina , khosrow Dadbin Dadbin, Rosa Ardá Maillo, Inmaculada Parra Álvarez, Justino Flores Ramos, Mª Dolores Vicente de Forondo, Antonio Calvo Cebrian, Yolanda Gines Díaz, Paloma Henares García, Luís La Puente Montoso, Aurora López Gil, Mª Concepción Marcello,Silvia Membrado Gómez, Nieves Puente García, Nuria Rodríguez Pata, Antonio Sánchez Calso, Mª Sánchez Casado, Mª Pilar Saladana Calzo, Carmen Velayos Rodríguez, Consuelo Velaz López, Miguel Ángel Venga Mendía, C. Susana Abad Guijarro, Gema Calderero Castellanos, Esperanza Corral Agüero, Ángeles Fernández Ortega, Carmen García Regidor, Edurne Hernández Sanzano, Pablo Martín Cano, Mª Del Carmen Martínez Coello, Sandrine Miguel Miguel, Mª Jesús Ramos Martín de Argenta, Beatriz Ruescas Aurrecoechea, Esteban González López, Elena Ramos Quirós, David Pérez Manchón, Leticia Pontón, Jon Koldo Sagardui Villamor, Mireia Rey Pérez de Pipaon, Mª Luisa Idarreta Zubiria, Juan Carlos Sánchez Ruiz, Ángela Rodríguez de Cossio, Milagros Merino Pella, Nuria Ruiz Hombrebueno, Rafael Llanes, Yolanda Vicente Prior, Mercedes Picó, Francisco Pérez Durán, Isabel Pérez Botella, Ángeles Cuevas, Francisco Martínez García, Raquel Cobeñas Mateo, María Teresa Rodríguez De Fonseca, Naldi Luz Cerdeña Ocola, Irene Alma Polanco García, María Esther Amez De Castro, Susana Barrios Espinoza, Antonio Guijarro Jiménez, Ana María De La Uz Pardos, Francisco Javier Cabrera Pérez, José Ignacio Torres Jiménez, Francisco Martínez García, María Isabel Vidal De La Riva, María Teresa Rodríguez De Fonseca, Gabriel Barderas Cuevas, Gonzalo Carrillo De Albornoz Martínez Pantoja, Mª Isabel García Romero. Castilla y León. Primary care centers of Ávila. Primary Care centre of Arévalo: Saturio Vega Quiroga; Roberto Aldrich García, Carlos Cañas Ruesgas, Carmen Vian Baron, Josefina Fernández Fernández, Mª Antonia Jiménez Carabias, Laureano López Gay, Mª Pilar Marqués Macías, Almudena Cantalejo Martín, Ana Benito Pérez, Modesta Mulero San José, Vanesa Martín Hernández, Laura Sánchez Domínguez, Rosa Mª García Martín, Victor Manuel Álvarez Zurdo. Primary Care centre of Sotillo de la Adrada: David Álvarez Suárez, Carmen Lázaro del Nogal, Lourdes González López, Mª del Mar Varas Reviejo, Juan Luis Martín Clavo, Mª Isabel Blázquez Blanco,Mª Luisa Ramos González, Guadalupe Rinaldi Català, Montserrat López Ramírez, Vanesa Hernández Blázquez, Vanessa Gutiérrez León, Raquel Pérez Cruz, Josefina Fernández Fernández, Almudena Fernández García, Raquel Alonso Moralejo. Primary care centers of Segovia. Primary Care centre of Carbonero El Mayor: María Soledad Fragua Gil, Virginia Silva Guisasola, Concepción Manrique de la Fuente, Ángeles Lazcoz Fontán, Héctor Aceves Gamarra, Alba Marina Hernández López, Mª Jesús Blanco Ledesma, Alfonso Santos López, Cristina de la Cruz Maeso, Mª del Espíritu Santo Otero Herrero, Cristina Olmos Marinero, Patricia Redondo Arranz, Mónica Álvaro García. Primary Care centre of Segovia III: Luis Gonzálvez López, María Ángeles Raquejo Grado, José Rodríguez Sanz, Juan Manuel de Andrés Rubio, Nuria González Acebes, Joaquina Galán Sánchez, Teresa López Fernández-Quesada, Almudena Sanz Prieto, Carmen Montero Morales, María Dolores Alba Jiménez, Beatriz Ayala Miranda. Castilla-La Mancha. Primary Care centres of CUENCA. Hospital General: Jaime Santiago Aranda Regules, Alba Caterina del Hoyo Herráiz, María Victoria Cantero Ayllón, María José Guillén Izquierdo, María Sandra Ruiz Mora, Ana Peña Cabia, Rosa Sánchez Amo, Mº Josefa Moya López. Cuenca I: Fructuoso Muelas Herráiz, Mº Ángeles Molina Morate, Fernando Salcedo Aguilar. Cuenca II: Nieves Valero Caracena, Beatriz Ortega Noheda, Mº Carmen García González. Cuenca III: Cristina Martínez Martín, Miryam Pardo Villalvilla, Mª Eugenia García Castellanos, María Elena de las Heras Martínez. Primary Care centre of Tarancón: Filomena del Saz Castellanos, Encarnación Palomares Cañada, María Concepción Fraile Jiménez, Pilar Palomar Moreno, Bárbara Martínez Garrido, María Pilar Orgaz Gallego, María José Tricio Armero, Cristina García del Pino Cañadas, Isabel Tierno Aparicio. Málaga. Fundación FIMABIS. Servicio Andaluz de Salud (SAS). Regional University Hospital of Málaga, Biomedical Research Institute of Málaga (IBIMA), University of Málaga (UMA), Málaga, Spain. Medicina Interna: Ricardo Gómez-Huelgas, María Dolores López-Carmona, Luis M Pérez-Belmonte, María Rosa Bernal-López, María Teresa Moyano Paris, Paula Moya Rodríguez, Antonio Vargas Candela, Alberto Vilches Pérez, María Isabel Ruiz Moreno, Maite Muñoz Melero, Pilar Gómez Martin. Oftalmología: Jacinto Villalvilla, Álvaro Santos, Antonio Archilla, Carlos Rocha, Silvia Lozano Ruiz. Primary care centers of Málaga. Alameda- Perchel: Francisco Javier Orellana Lozano, Manuel Guarino Nuño, Alhaurín de la Torre: Daniel Martin Castillo, María José Guerra Maldonado, José Rogelio Sánchez Ortiz. Alozaina-Yunquera: David Fernández Bonilla, J A Cortes, Juan Antonio Cordero Cabrera. Antequera: José Antonio Godínez, José Jesús Moreno Jiménez, David Paniagua Urbano. Archidona: Antonio Cansino Osuna, María Del Carmen Rojo Camacho, Celinda Lara Moreno, Ignacio Hinojosa Núñez, Almudena Puga González, Capuchinos: Yolanda Rey, Yolanda Rodríguez Gallego. Carranque: Carmen Aylón Moliner. Cartama Estacion-Cartama pueblo-Pizarra: Francisco Jose Guirado Hidalgo, María Eva Ruiz Coronado, Susana Barea Diañez, Beatriz Navarro Aranda. Casarabonela: M Carmen Arroyo Martínez. Ciudad Jardin: Antonio Baca Osorio, José Mancera, Salvador Ruiz Vera, Idelfonso Martos Cerezuela. Delicias:Fernando López Verde, Mª Carmen Barba Cañete, Cristóbal Gómez Acevedo, Margarita Sánchez Pavón. La Luz: Antonio Oropez Mesa, Antonio Rojas Barrilado. La Roca: Esther Martin Aurioles, Rocío Ramos, Francisco Javier Camino, María Eugenia Valdes, Dolores Bravo Fernández. Limonar: Silvia Hazañas, Amparo Vargas Machuca Benítez, Eva María Taboada Ríos. Puerta Blanca: Antonio Hormigo Pozo, Idelfonsa Martínez Zaragoza. Rincón de la Victoria: Milagrosa Espinar Toledo, María Del Rosario Rosillo Rein, Gloria Inmaculada Mestre Reoyo, María Auxiliadora Naranjo Sánchez, José Ángel Sánchez Ortiz, Mª José González Vega, José Carlos Pérez Sánchez, Antonia Cabra Navarro, Antonio Vivas Molina. San Andrés-El torcal: Antonio Ramírez Ceballos, Francisco Ruiz Solares. Tiro Pichón: Juan José Bedoya Belmonte, Germán Ortega Núñez, María Encarnación Bueno Caro. Trinidad-Jesús cautivo: Santos Agreda. Victoria: María José Bujalance Zafra, Montse Román Cereto, Rafael Ángel Maqueda. Poland. Uniwersytet Jagiellonski, Collegium Medicum, Poland: Aleksandra Gilis-Januszewska, Alicja Hubalewska-Dydejczyk, Beata Piwońska- Solska, Justyna Biegańska, Katarzyna Cybulska, Bernadeta Marcykiewicz, Magdalena Duraczyńska, Anna Cybulska, Joanna Stankiewicz- Góra, Alina Mruk, Grzegorz Młyński, Lucyna Rozpondek, Michał Sroka, Maciej Gilis-Januszewski, Edyta Sacha, Adela Justyńska, Magdalena Szopa, Bartłomiej Matejko. Greece. National and Kapodistrian University of Athens. Greece: Konstantinos Makrilakis, Stavros Liatis, Evangelia Siami, Chryssoula Stathi, Katerina Barmpagianni, Maria Nikoloudi, Meropi Kontogianni, Ioanna Kechrimpari, Aphroditi Tsiakou, Melina Karaolia. Alexandra Hospital. University of Athens. Greece: Asimina Mitrakou, Georgios Panagopoulos, Paraskevi Kontou, Petros Thomakos, Georgios Giagkou, Evangelia Avgeraki, Eirini Mamalaki. Bulgaria. University Multi-Profile Hospital for Active Treatment Alexandrovska EAD. Sofia, Bulgaria: Zdravko Asenov Kamenov, Antoaneta Trifonova Gateva, Yavor Sashov Assyov, Tsvetan Vladimirov Gatev, Vera Nacheva Karamfilova, Iveta Slavyanova Nedeva. Austria. Gemeinnutzige Salzburger Landeskliniken Betriebsgesellschaft. Salzburg, Austria: Bernhard Paulweber, Ludmilla Kedenko, Andrea Undeutsch. Turkey. Istanbul University Istanbul. Turkey: Ilhan Satman, B. Fulya Turker, Ayse K. Uzum, Sakin Tekin, Ramazan Çakmak, Elif T. Bagdemir, Selda G. Celik, Cemile C. Idiz, Halime C. Sackoparan, Zafer Cebeci, Nur Kir, Dilara Karsidag, Yildiz Tutuncu, Aslihan Demirbas, Busra Yildiz. Serbia. Medical System Beograd-MSB. Belgrade, Serbia. Predrag Djordjevic, Margarita Dodevska, Nevenka Raketic, Aleksandar Stamenkovic, Marko Jovic, Fadil Canovic, Ljiljana Milivojevic, Kristina Savic, Ljiljana Savic, Mirjana Sarkic. Faculty of Medicine, University of Belgrade. Serbia. Nebojsa Lalic, Katerina Lalic, Aleksandra Jotic, Jelena Stanarcic, Ljiljana Lukic, Tanja Milicic, Natasa Rajkovic, Marija Macesic, Dijana Risimic, Mladen Bila. Australia. The Univerity of Sydney. Australia: Stephen Colagiuri, Anthony Keech, Kristine Maddock, Andrzej S. Januszewski, Liping Lee, Tegan Picone, Emma Sainsbury, Alison Coenen, Chelsea Hendy, Namson Lau, Tania Markovic, Erica Bessell, Nick Fuller. Kuwait. Dasman Diabetes Research Institute: Jaakko Tuomilehto, Abdullah Alkandari, Abdullah Bennakhi, Monira Alarouj, Mohammad Jalali, Medinella Fernandez, Makka Ali Osman, Jincy Raj, Ala’a Al-Obaid, Hyatt Alsayegh, Najeeba Almatrouk. WP3. Lifestyle Intervention. Terveyden ja Hyvinvoinnin Laitos. Finland: Jaana Lindström, Päivi Valve, Katri Hemiö, Katja Wikström, Esko Levälahti, Pirjo Saastamoinen. WP4. Central laboratories and Biobank. Instituto de Investigación Sanitaria de la Fundación Jiménez Díaz. Madrid, Spain (Central Laboratory, Biobank and Inflammatory biomarkers): Jesús Egido, Sebastián Mas, Sandra Zazo, Esther Civantos, Rosario de Nicolás, Federico Rojo. Consiglio Nazionale delle Ricerche. Pisa, Italy. (NAFLD laboratory): Amalia Gastaldelli, Fabrizia Carli, Emma Buzzigoli, Melania Gaggini. Fundació Hospital Universitari Vall d' Hebron, Institut de Recerca. Barcelona, Spain (Retinal biomarkers): Rafael Simó, Cristina Hernández, Marta García-Ramirez. Queen Mary University of London. UK (Genetic laboratory): Graham A Hitman. WP5. Microvascular assessment coordination. Universita di Pisa, Italy. (Endotelial assessment): Andrea Natali, Lucrecia Motta. WP6. Retinal Assessment. Instituto de Oftalmobiología Aplicada (IOBA) Universidad de Valladolid, Spain. (Central Retinal Reading Centre): Maribel López, José Carlos Pastor, Lucía Manzanas, Ignacio Alonso, Verónica Velasco, Laura Mena. e-DIAGNOSTIC Oftalmología. Madrid, Spain. (Retinal e-platform): Diana Bravo, Víctor González Rumayor, Marica D´Angelo, Álex Manau. WP7. Neuropsychological assessment. Department for Clinical Neurosciences and Preventive Medicine, Danube University Krems. Krems, Austria: Michael Brainin, Yvonne Teuschl, Alexandra Dachenhausen, Karl Matz. Instituto de Investigación y Asistencia Psiquiátrica (IAP). Madrid, Spain: Laura Ferrando Bundío. Oivauni Oy. Kuopio,Finland: Henri Tuomilehto, Seppo Silvennoinen. WP8. Statistical analysis. Vastra Gotalands Lans Landsting. Gotenburg, Sweden (Statistical Analysis coordinator): Marcus Lind, Aldina Pivodic, Hans Wedel. Institute of Neuroscience, National Research Council (Consiglio Nazionale delle Ricerche). Pavoda, Italy. (Insulin and C-Peptide modeling): Andrea Mari, Andrea Tura. University of Helsinki. Department of Public Health: Pekka Jousilahti. WP9. Technology Assessment. IMPETO Medical. Paris, France (Sudoscan assessment): Jean-Henri Calvet, GaelleLerise, Alice Vilier. Mezen Bouzaien. AARDEX Group SA. Geneva. Switzerland (MEMs drug´s adherence monitoring): Bernard Vrijens, Rodrigo Paiva, Eric Tousset. WP10. Dissemination and communication: Federation Internationale du Diabete Region Europe Lala Rabemananjara. We thank Javier Silva Calvo and María Silva Calvo for the grammatical and stylistic revision of the manuscript.
Author Contributions
All authors listed made substantial contributions to conception and design, acquisition of data or analysis and interpretation. All authors listed participated in drafting the article or revising it critically for important intellectual content. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by all local ethic committees of the participating centers: Comite Etico de Investigacion Clınica del Hospital Universitario La Paz, Madrid, Spain, approval No. 3850 (1 February 2013); Hellenic Republic Ministry of Health National Ethics Committee, Greece, approval No. 74/ 00-01/14 (15 December 2014); The Dean office, Istanbul Medical Faculty Ethical Board for Clinical Trials, Turkey, approval No. 2014/495 (10 April 2014); Etickog Odbora, Beograd, Serbia, approval No. 61/1 (6 April 2013); Ethics Committee of the Faculty of Medicine, University of Belgrade, Serbia, approval No. 29/III-10 (7 March 2013); Komisja Bioetyczna UJ (Uniwersytetu Jagiellonskiego), Poland, approval No. BET/185/L/ 2014 (26 June 2014); Executive Officer of Ethics Review Committee (RPAH) & Human Research Ethics Committee (HREC), Australia, approval No. X13-0046 & HREC/13/RPAH/65 (12 March 2014); кoмисия пo етика "Александрoвска" ЕАД Сoфия, България, Bulgaria, approval No. KИ-213/18.03.15 (18 March 2015); Die Ethikkommission fur das Bundesland Salzburg. "Landeskrankenhaus Salzburg—Universitatsklinikum der PMU, Universitatsklinik fur Innere Medizin I", Austria; approval No. 415-E/1649/10-2014 (8 July 2014).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The clinical trial is still ongoing, patients and data are being managed in a masked fashion. Data cannot be made publicly available since it would compromise confidentiality and might reveal the identity or location of participants. Additionally, public availability of data would be in violation of the Spanish Organic Law 15/1999 of protection of personal data (consolidated text 5/3/2011) and the European Law (EU) 2016/679 from European Parliament and European Council of 27 of April 2016 about Data Protection (RGPD). The data Access Committee of Consejería de Sanidad de la Comunidad de Madrid address: c/Plaza Carlos Trías Bertrán n˚7 (Edif. Sollube) Madrid 28020; (protecciondedatos.sanidad@madrid.org) could consider those requests that do not involve any conflict with these legal regulations. Any acceptable request will be processed and evaluated by the ePREDICE Steering Committee.
Conflicts of Interest
The authors declare no conflict of interest.
Clinical Trial Registration
Clinical Trials Gov Registry Number: NCT03222765. EUDRACT Registry Number: 2013-000418-39.
Funding Statement
This research was funded by European Commission, FP7 EC-GA No. 279074; Boehringher Ingelheim, Ingelheim am Rhein, Germany (IIS Program. Grant number 1218.166); Merck Healthcare KGaA, Darmstadt, Germany (IIS number: EMR200084_621), Instituto de Salud Carlos III, Spain PI11/01653. The study funders were not involved in the design of the study, the collection, analysis and interpretation of data or writing the report and did not impose any restrictions regarding the publication of the report.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Wagner R., Heni M., Tabák A.G., Machann J., Schick F., Randrianarisoa E., de Angelis M.H., Birkenfeld A.L., Stefan N., Peter A., et al. Pathophysiology-based subphenotyping of individuals at elevated risk for type 2 diabetes. Nat. Med. 2021;27:49–57. doi: 10.1038/s41591-020-1116-9. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycemia: Report of a WHO/IDF Consultation. World Health Organization; Geneva, Switzerland: 2006. [Google Scholar]
- 3.Gernstein H.C., Santaguida P., Raina P., Morrison K.M., Balion C., Hunt D., Yazdi H., Booker L. Annual incidence and relative risk of diabetes in people with various categories of dysglycaemia: A systematic overview and meta-analysis of prospective studies. Diabetes Res. Clin. Pract. 2007;78:305–312. doi: 10.1016/j.diabres.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 4.Diabetes Prevention Program Research Group. Knowler W.C., Fowler S.E., Hamman R.F., Christophi C.A., Hoffman H.J., Brenneman A.T., Brown-Friday J.O., Goldberg R., Venditti E., et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374:1677–1686. doi: 10.1016/S0140-6736(09)61457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yeboah J., Bertoni A.G., Herrington D.M., Post W.S., Burke G.L. Impaired Fasting Glucose and the Risk of Incident Diabetes Mellitus and Cardiovascular Events in an Adult Population: MESA (Multi-Ethnic Study of Atherosclerosis) J. Am. Coll. Cardiol. 2011;58:140–146. doi: 10.1016/j.jacc.2011.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heianza Y., Hara S., Arase Y., Saito K., Fujiwara K., Tsuji H., Kodama S., Hsieh S.D., Mori Y., Shimano H., et al. HbA1c 5·7–6·4% and impaired fasting plasma glucose for diagnosis of pre-diabetes and risk of progression to diabetes in Japan (TOPICS 3): A longitudinal cohort study. Lancet. 2011;378:147–155. doi: 10.1016/S0140-6736(11)60472-8. [DOI] [PubMed] [Google Scholar]
- 7.Kanat M., Mari A., Norton L., Winnier D., DeFronzo R.A., Jenkinson C., Abdul-Ghani M.A. Distinct β-Cell Defects in Impaired Fasting Glucose and Impaired Glucose Tolerance. Diabetes. 2012;61:447–453. doi: 10.2337/db11-0995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Plantinga L.C., Crews D.C., Coresh J., Miller E.R., 3rd, Saran R., Yee J., Hedgeman E., Pavkov M., Eberhardt M.S., Williams D.E., et al. Prevalence of chronic kidney disease in US adults with undiagnosed diabetes or pre-diabetes. Clin. J. Am. Soc. Nephrol. 2010;5:673–682. doi: 10.2215/CJN.07891109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singh J.P., Larson M., O’Donnell C.J., Wilson P.F., Tsuji H., Lloyd-Jones D., Levy D. Association of hyperglycemia with reduced heart rate variability (The Framingham Heart Study) Am. J. Cardiol. 2000;86:309–312. doi: 10.1016/S0002-9149(00)00920-6. [DOI] [PubMed] [Google Scholar]
- 10.Tapp R.J., Tikellis G., Wong T.Y., Harper C.A., Zimmet P.Z., Shaw J.E., Australian Diabetes Obesity and Lifestyle Study Group Longitudinal association of glucose metabolism with retinopathy: Results from the Australian Diabetes Obesity and Lifestyle (AusDiab) study. Diabetes Care. 2008;31:1349–1354. doi: 10.2337/dc07-1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Balkau B., Hu G., Qiao Q., Tuomilehto J., Borch-Johnsen K., Pyorala K., DECODE Study Group. European Diabetes Epidemiology Group Prediction of the risk of cardiovascular mortality using a score that includes glucose as a risk factor. The DECODE Study. Diabetologia. 2004;47:2118–2128. doi: 10.1007/s00125-004-1574-5. [DOI] [PubMed] [Google Scholar]
- 12.Barr E.L., Zimmet P.Z., Welborn T.A., Jolley D., Magliano D.J., Dunstan D.W., Cameron A.J., Dwyer T., Taylor H.R., Tonkin A.M., et al. Risk of Cardiovascular and All-Cause Mortality in Individuals With Diabetes Mellitus, Impaired Fasting Glucose, and Impaired Glucose Tolerance: The Australian Diabetes, Obesity, and Lifestyle Study (AusDiab) Circulation. 2007;116:151–157. doi: 10.1161/CIRCULATIONAHA.106.685628. [DOI] [PubMed] [Google Scholar]
- 13.Sorensen B.M., Houben A.J., Berendschot T.T., Schouten J.S., Kroon A.A., van der Kallen C.J., Henry R.M.A., Koster A., Sep S.J.S., Dagnelie P.C., et al. Pre-diabetes and type 2 diabetes are associated with generalized microvascular dysfunction: The Maastricht study. Circulation. 2016;134:1339–1352. doi: 10.1161/CIRCULATIONAHA.116.023446. [DOI] [PubMed] [Google Scholar]
- 14.Tabák A.G., Herder C., Rathmann W., Brunner E.J., Kivimäki M. Pre-diabetes: A high-risk state for diabetes development. Lancet. 2012;379:2279–2290. doi: 10.1016/S0140-6736(12)60283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vas P.R.J., Alberti K.G., Edmonds M.E. Pre-diabetes: Moving away from a glucocentric definition. Lancet Diabetes Endocrinol. 2017;5:848–849. doi: 10.1016/S2213-8587(17)30234-6. [DOI] [PubMed] [Google Scholar]
- 16.Galaviz K.I., Weber M.B., Straus A., Haw J.S., Narayan K.V., Ali M.K. Global Diabetes Prevention Interventions: A Systematic Review and Network Meta-analysis of the Real-World Impact on Incidence, Weight, and Glucose. Diabetes Care. 2018;41:1526–1534. doi: 10.2337/dc17-2222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holman R.R., Coleman R.L., Chan J.C.N., Chiasson J.L., Feng H., Ge J., Gerstein H.C., Gray R., Huo Y., Lang Z., et al. Effects of acarbose on cardiovascular and diabetes outcomes in patients with coronary heart disease and impaired glucose tolerance (ACE): A randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 2017;5:877–886. doi: 10.1016/S2213-8587(17)30309-1. [DOI] [PubMed] [Google Scholar]
- 18.The Diabetes Prevention Program Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DREAM Trial Investigators Effect of rosiglitazone on the frequency of diabetes in patients with glucose impaired tolerance or impaired fasting glucose: A randomized controlled trial. Lancet. 2006;368:1096–1105. doi: 10.1016/S0140-6736(06)69420-8. [DOI] [PubMed] [Google Scholar]
- 20.DeFronzo R.A., Tripathy D., Schwenke D.C., Banerji M.A., Bray G.A., Buchanan T.A., Clement S.C., Henry R.R., Hodis H.N., Kitabchi A.E., et al. ACT NOW Study. N. Engl. J. Med. 2011;364:1104–1115. doi: 10.1056/NEJMoa1010949. [DOI] [PubMed] [Google Scholar]
- 21.Pi-Sunyer X., Astrup A., Fujioka K., Greenway F., Halpern A., Krempf M., Lau D.C., le Roux C.W., Violante Ortiz R., Jensen C.B., et al. A Randomized, Controlled Trial of 3.0 mg of Liraglutide in Weight Management. N. Engl. J. Med. 2015;373:11–22. doi: 10.1056/NEJMoa1411892. [DOI] [PubMed] [Google Scholar]
- 22.Diabetes Prevention Program Research Group The prevalence of retinopathy in impaired glucose tolerance and recent-onset diabetes in the Diabetes Prevention Program. Diabet. Med. 2007;24:137–144. doi: 10.1111/j.1464-5491.2007.02043.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosenstock J., Kahn S.E., Johansen O.E., Zinman B., Espeland M.A., Woerle H.J., Pfarr E., Keller A., Mattheus M., Baanstra D., et al. Effect of Linagliptin vs Glimepiride on Major Adverse Cardiovascular Outcomes in Patients With Type 2 Diabetes: The CAROLINA Randomized Clinical Trial. JAMA. 2019;322:1155–1166. doi: 10.1001/jama.2019.13772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Matthews D.R., Paldánius P.M., Proot P., Chiang Y., Stumvoll M., Del Prato S., VERIFY Study Group Glycaemic durability of an early combination therapy with vildagliptin and metformin versus sequential metformin monotherapy in newly diagnosed type 2 diabetes (VERIFY): A 5-year, multicentre, randomised, double-blind trial. Lancet. 2019;394:1519–1529. doi: 10.1016/S0140-6736(19)32131-2. [DOI] [PubMed] [Google Scholar]
- 25.Gong Q., Gregg E.W., Wang J., An Y., Zhang P., Yang W., Li H., Li H., Jiang Y., Shuai Y., et al. Long-term effects of a randomised trial of a 6-year lifestyle intervention in impaired glucose tolerance on diabetes-related microvascular complications: The China DaQing Diabetes Prevention Outcome Study. Diabetologia. 2011;54:300–307. doi: 10.1007/s00125-010-1948-9. [DOI] [PubMed] [Google Scholar]
- 26.Aro A., Kauppinen A., Kivinen N., Selander T., Kinnunen K., Tuomilehto J., Keinänen-Kiukaanniemi S., Lindström J., Uusitupa M., Kaarniranta K. Life Style Intervention Improves Retinopathy Status—The Finnish Diabetes Prevention Study. Nutrients. 2019;11:1691. doi: 10.3390/nu11071691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dietrich N., Kolibabka M., Busch S., Bugert P., Kaiser U., Lin J., Fleming T., Morcos M., Klein T., Schlotterer A., et al. The DPP4 Inhibitor Linagliptin Protects from Experimental Diabetic Retinopathy. PLoS ONE. 2016;11:e0167853. doi: 10.1371/journal.pone.0167853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Groop P.H., Cooper M.E., Perkovic V., Hocher B., Kanasaki K., Haneda M. Linagliptin and its effects on hyperglycaemia and albuminuria in patients with type 2 diabetes and renal dysfunction: The randomized MARLINA-T2D trial. Diabetes Obes. Metab. 2017;19:1610–1619. doi: 10.1111/dom.13041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rosenstock J., Perkovic V., Johansen O.E., Cooper M.E., Kahn S.E., Marx N., Alexander J.H., Pencina M., Toto R.D., Wanner C., et al. Effect of Linagliptin vs Placebo on Major Cardiovascular Events in Adults with Type 2 Diabetes and High Cardiovascular and Renal Risk: The CARMELINA Randomized Clinical Trial. JAMA. 2019;321:69–79. doi: 10.1001/jama.2018.18269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.GRADE Study Research Group. Nathan D.M., Lachin J.M., Bebu I., Burch H.B., Buse J.B., Cherrington A.L., Fortmann S.P., Green J.B., Kahn S.E., et al. Glycemia Reduction in Type 2 Diabetes—Microvascular and Cardiovascular Outcomes. N. Engl. J. Med. 2022;387:1075–1088. doi: 10.1056/NEJMoa2200436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baranowska-Jurkun A., Matuszewski W., Bandurska-Stankiewicz E. Chronic Microvascular Complications in Prediabetic States—An Overview. J. Clin. Med. 2020;9:3289. doi: 10.3390/jcm9103289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gabriel R., Boukichou Abdelkader N., Acosta T., Gilis-Januszewska A., Gómez-Huelgas R., Makrilakis K., Kamenov Z., Paulweber B., Satman I., Djordjevic P., et al. Early prevention of diabetes microvascular complications in people with hyperglycaemia in Europe. ePREDICE randomized trial. Study protocol, recruitment and selected baseline data. PLoS ONE. 2020;15:e0231196. doi: 10.1371/journal.pone.0231196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lindström J., Neumann A., Sheppard K.E., Gilis-Januszewska A., Greaves C.J., Handke U., Pajunen P., Puhl S., Pölönen A., Rissanen A., et al. Take action to prevent diabetes--the IMAGE toolkit for the prevention of type 2 diabetes in Europe. Horm. Metab. Res. 2010;42((Suppl. 1)):S37–S55. doi: 10.1055/s-0029-1240975. [DOI] [PubMed] [Google Scholar]
- 34.Heerspink H.J.L., Stefánsson B.V., Correa-Rotter R., Chertow G.M., Greene T., Hou F.F., Mann J.F.E., McMurray J.J.V., Lindberg M., Rossing P., et al. Dapagliflozin in Patients with Chronic Kidney Disease. N. Engl. J. Med. 2020;383:1436–1446. doi: 10.1056/NEJMoa2024816. [DOI] [PubMed] [Google Scholar]
- 35.Mosenzon O., Wiviott S.D., Cahn A., Rozenberg A., Yanuv I., Goodrich E.L., Murphy S.A., Heerspink H.J.L., Zelniker T.A., Dwyer J.P., et al. Effects of dapagliflozin on development and progression of kidney disease in patients with type 2 diabetes: An analysis from the DECLARE–TIMI 58 randomised trial. Lancet Diabetes Endocrinol. 2019;7:606–617. doi: 10.1016/S2213-8587(19)30180-9. [DOI] [PubMed] [Google Scholar]
- 36.Räisänen A.M., Eklund J., Calvet J.-H., Tuomilehto J. Sudomotor Function as a Tool for Cardiorespiratory Fitness Level Evaluation: Comparison with Maximal Exercise Capacity. Int. J. Environ. Res. Public Health. 2014;11:5839–5848. doi: 10.3390/ijerph110605839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Domecq J.P., Prutsky G., Leppin A., Sonbol M., Altayar O., Undavalli C., Wang Z., Elraiyah T., Brito J.P., Mauck K.F., et al. Drugs Commonly Associated With Weight Change: A Systematic Review and Meta-analysis. J. Clin. Endocrinol. Metab. 2015;100:363–370. doi: 10.1210/jc.2014-3421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Diabetes Prevention Program Research Group Long-term safety, tolerability, and weight loss associated with metformin in the Diabetes Prevention Program Outcomes Study. Diabetes Care. 2012;35:731–737. doi: 10.2337/dc11-1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barua M., Pathan F., Nabi M.U., Kabir M. Assessment of clinical and biochemical profile of prediabetic subject in Bangladesh, attending in BIRDEM and results of intervention by lifestyle modification, metformin, and DPP4 inhibitor. Diabetes Metab. Syndr. Clin. Res. Rev. 2019;13:1603–1608. doi: 10.1016/j.dsx.2019.03.019. [DOI] [PubMed] [Google Scholar]
- 40.Alvarez-Canales M.F.D.L.L., Salazar-López S.S., Farfán-Vázquez D., Martínez-López Y.E., González-Mena J.N., Jiménez-Ceja L.M., Vargas-Ortiz K., Evia-Viscarra M.L., de Oca-Loyola M.L.M., Folli F., et al. Effect of linagliptin on glucose metabolism and pancreatic beta cell function in patients with persistent prediabetes after metformin and lifestyle. Sci. Rep. 2021;11:8750. doi: 10.1038/s41598-021-88108-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cosentino F., Grant P., Aboyans V., Bailey C.J., Ceriello A., Delgado V. The Task Force for diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and the European Association for the Study of Diabetes (EASD) Eur. Heart J. 2020;41:255–323. doi: 10.1093/eurheartj/ehz486. [DOI] [PubMed] [Google Scholar]
- 42.Stevens J.W., Khunti K., Harvey R., Johnson M., Preston L., Woods H.B., Davies M., Goyder E. Peventing the progression to type 2 diabetes mellitus in adults at high risk: A systematic review and network meta-analysis of lifestyle, pharmacological and surgical interventions. Diabetes Res. Clin. Pract. 2015;107:320–331. doi: 10.1016/j.diabres.2015.01.027. [DOI] [PubMed] [Google Scholar]
- 43.Guardado-Mendoza R., Salazar-López S.S., Álvarez-Canales M., Farfán-Vázquez D., Martínez-López Y.E., Jiménez-Ceja L.M., Suárez-Pérez E.L., Angulo-Romero F., Evia-Viscarra M.L., de Oca-Loyola M.L.M., et al. The combination of linagliptin, metformin and lifestyle modification to prevent type 2 diabetes (PRELLIM). A randomized clinical trial. Metabolism. 2020;104:154054. doi: 10.1016/j.metabol.2019.154054. [DOI] [PubMed] [Google Scholar]
- 44.for the Diabetes Prevention Program Research Group. Aroda V.R., Knowler W.C., Crandall J.P., Perreault L., Edelstein S.L., Jeffries S.L., Molitch M.E., Pi-Sunyer X., Darwin C., et al. Metformin for diabetes prevention: Insights gained from the Diabetes Prevention Program/Diabetes Prevention Program Outcomes Study. Diabetologia. 2017;60:1601–1611. doi: 10.1007/s00125-017-4361-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ramachandran A., Snehalatha C., Mary S., Mukesh B., Bhaskar A.D., Vijay V., Indian Diabetes Prevention Programme (IDPP) The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1) Diabetologia. 2006;49:289–297. doi: 10.1007/s00125-005-0097-z. [DOI] [PubMed] [Google Scholar]
- 46.Chiasson J.-L. Acarbose for the Prevention of Diabetes, Hypertension, and Cardiovascular Disease in Subjects with Impaired Glucose Tolerance: The Study to Prevent Non-Insulin-Dependent Diabetes Mellitus (Stop-Niddm) Trial. Endocr. Pract. 2006;12((Suppl. 1)):25–30. doi: 10.4158/EP.12.S1.25. [DOI] [PubMed] [Google Scholar]
- 47.Le Roux C.W., Astrup A., Fujioka K., Greenway F., Lau D.C.W., Van Gaal L., Ortiz R.V., Wilding J.P.H., Skjøth T.V., Manning L.S., et al. 3 years of liraglutide versus placebo for type2 diabetes risk reduction and weight management in individuals with prediabetes: A randomised, double-blind trial. Lancet. 2017;389:1399–1409. doi: 10.1016/S0140-6736(17)30069-7. [DOI] [PubMed] [Google Scholar]
- 48.Knowler W.C., Crandall J.P. Pharmacologic Randomized Clinical Trials in Prevention of Type 2 Diabetes. Curr. Diabetes Rep. 2019;19:154. doi: 10.1007/s11892-019-1268-5. [DOI] [PubMed] [Google Scholar]
- 49.Griffin S.J., Bethel M.A., Holman R.R., Khunti K., Wareham N., Brierley G., Davies M., Dymond A., Eichenberger R., Evans P., et al. Metformin in non-diabetic hyperglycaemia: The GLINT feasibility RCT. Health Technol. Assess. 2018;22:18. doi: 10.3310/hta22180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Haw J.S., Galaviz K.I., Straus A.N., Kowalski A.J., Magee M.J., Weber M.B., Wei J., Narayan K.M.V., Ali M.K. Long-term Sustainability of Diabetes Prevention Approaches: A Systematic Review and Meta-analysis of Randomized Clinical Trials. JAMA Intern. Med. 2017;177:1808–1817. doi: 10.1001/jamainternmed.2017.6040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.NAVIGATOR Study Group. Holman R.R., Haffner S.M., McMurray J.J., Bethel M.A., Holzhauer B., Hua T.A., Belenkov Y., Boolell M., Buse J.B., et al. Effect of nateglinide on the incidence of diabetes and cardiovascular events. N. Engl. J. Med. 2010;362:1463–1476. doi: 10.1056/NEJMoa1001122. [DOI] [PubMed] [Google Scholar]
- 52.Phung O.J., Sobieraj D., Engel S.S., Rajpathak S.N. Early combination therapy for the treatment of type 2 diabetes mellitus: Systematic review and meta-analysis. Diabetes Obes. Metab. 2014;16:410–417. doi: 10.1111/dom.12233. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The clinical trial is still ongoing, patients and data are being managed in a masked fashion. Data cannot be made publicly available since it would compromise confidentiality and might reveal the identity or location of participants. Additionally, public availability of data would be in violation of the Spanish Organic Law 15/1999 of protection of personal data (consolidated text 5/3/2011) and the European Law (EU) 2016/679 from European Parliament and European Council of 27 of April 2016 about Data Protection (RGPD). The data Access Committee of Consejería de Sanidad de la Comunidad de Madrid address: c/Plaza Carlos Trías Bertrán n˚7 (Edif. Sollube) Madrid 28020; (protecciondedatos.sanidad@madrid.org) could consider those requests that do not involve any conflict with these legal regulations. Any acceptable request will be processed and evaluated by the ePREDICE Steering Committee.