Background:
Although breast implants of the current generation can, in principle, remain in the body for life, follow-up operations of the augmented or reconstructed breasts are regularly necessary. Capsular contracture is the leading cause for revisional surgery. The aim of this study was to evaluate indications and changes in time intervals between consecutive implant replacements with a focus on capsular contracture.
Methods:
In the period from 2012 to 2017, all patients with breast implant replacements or removals at our institution were identified. From the medical file, the time of the first implantation and earlier replacements were analyzed for indication and timing of surgery.
Results:
A total of 498 operations for implant replacement or removal were analyzed in 323 patients. Including prior operations, 717 procedures could be evaluated. If capsular contracture was the indication, revision surgery was performed on average 14.3 years or 8.4 years in aesthetic or reconstructive cases, respectively. In patients with more than one implant removal or replacement, we saw a reduction in the time interval between the first, second, and third follow-up operation.
Conclusions:
The main indication to perform implant replacements or removals was capsular contracture recurring at increasingly shorter intervals. Patients must be informed about this possible progression when changing implants, but also before the first operation. If capsular contracture occurs after a rather short time period in reconstructive cases, the opportunity of an alternative approach (eg, autologous reconstruction) instead of a renewed implant change should be discussed with the patient.
Takeaways
Question: Do intervals in between subsequent operations change when the breast implant is changed repeatedly due to capsular contracture?
Findings: A retrospective cohort study including 323 patients showed that capsular contracture was the main indication for revision surgery. In patients with more than one implant removal or replacement, a reduction in the time interval between the first, second, and third follow-up operation was seen, both in the overall collective and for capsular contracture.
Meaning: As the number of implant revision surgery increases, capsular contracture occurs at increasingly shorter intervals.
INTRODUCTION
Although breast implants do not actually expire, it is likely that they will have to be replaced at some point. There are many reasons for a possible replacement, but capsular contracture is the leading cause.1–9 In individual cases, it is usually not possible to foresee when a follow-up operation will be necessary. However, there are factors that, for example, favor the occurrence of capsular contracture. These include the indication for implant placement, the implant approach, the implant site, and the surface structure of the implant.2,3,10,11
Reliable data on when the first replacement is required on average are not available due to the large number of influencing factors, surgical variables, and different implant types. In any case, there is no fixed changeover time, so that implants can usually remain as long as the patient is free of complaints and is satisfied with the aesthetic result. Especially when replacing implants, a prognosis of the expected time without recurrence of complaints would be helpful to suggest alternative procedures when indicated, for example, explantation and mastopexy (aesthetic cases) or autologous reconstructions (reconstructive cases). Thus, the aim of this study was to assess changes in time intervals between consecutive implant replacements for the most frequent indication, capsular contracture.
METHODS
After obtaining approval from the local ethical board (Ärztekammer Hamburg, WF-065/19), a retrospective chart review was performed. The observation period was January 1, 2012 to December 31, 2017. To identify breast implant replacements and removals, we performed a systematic search using the documented procedure codes for replacement and removal of a mammary prostheses or skin expanders.
Exclusion criteria were planned expander to implant replacements, removal of temporary implants in autologous tissue reconstructions, and missing or incomplete patient data. For all remaining patients, the time and indication for the first implantation and all previous implant replacements were recorded from the medical history to be able to make a statement about the respective periods of implant placement.
Implant site, implant volume, and implant brand were not recorded. We decided to exclude the mentioned data from evaluation because they were recorded inconsistently in the medical history in the majority of patients. Because almost all the breast implants that we removed were textured, an evaluation of the implant texture was not performed and would have been inconclusive. In addition, the insertion of an ADM (acellular dermal matrix) was also not recorded, as it is rarely used in Germany due to its high cost. For capsular contracture to be listed as an indication for revision surgery, a Baker grade III or IV had to be present. In the event of capsular contracture, complete capsulectomy was always the targeted approach in our hands; with procedures performed outside our hospital, the retention of a capsule could not be evaluated.
The timing of the first and subsequent implant replacement was compared between aesthetic and reconstructive indications for primary placement. If capsular contracture was the cause for implant replacement, we also examined the change in the time periods until the first and subsequent implant replacement. If implant rupture was the cause for implant replacement, we examined the time until the first implant replacement. In addition, we evaluated the influence of prior radiotherapy on the time intervals between replacements.
Statistical analysis of patient data was performed using SPSS version 25 statistical software from IBM (Armon, N.Y.: IBM Corp). Categorical variables were presented using frequency analysis, and numeric variables were presented using the mean, minimum, maximum, 25th, 50th, or 75th percentiles. A confidence interval of 95% was determined for all calculations. Significance testing was performed for categorical variables using a chi-square test, and for independent numeric variables using an independent t test or a Mann-Whitney U test. For dependent numeric variables, a dependent t test or a Wilcoxon test served as significance testing. Before applying the t test, a parametric distribution of the variables was assumed using a histogram. Kaplan-Meier curves were compared using a log-rank test. A P value of less than 0.05 was considered statistically significant.
RESULTS
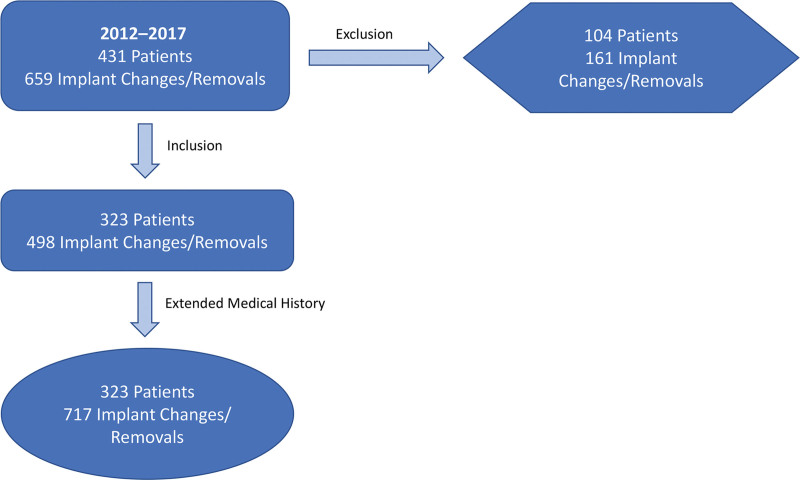
In total, 498 implant replacement or removals in 323 patients could be included in the evaluation. Another 168 operations in 108 patients were excluded. All patients were women. In the further course of the study, a detailed patient history was compiled for the 323 patients included, to evaluate the patients’ former implant replacement or removal. This resulted in a total number of 717 operations for breast implant replacement or removal (Fig. 1).
Fig. 1.
Establishment of the patient collective.
Of the 323 patients included in the evaluation, primary indication for implant placement was aesthetic in 167 patients (51.7%) and reconstructive in 156 patients (48.3%). In a total of 717 performed implant replacement or removals, 451 implants (62.9%) were primarily placed for aesthetic indications, and 266 implants (37.1%) for breast reconstruction (Table 1).
Table 1.
Case Numbers for Breast Implant Replacement/Removals according to Indication of Primary Implant Placement
| Implant Replacement or Removal | Primary Aesthetic Cases (n) | Primary Reconstructive Cases (n) | Total (n) |
|---|---|---|---|
| 1 | 311 | 187 | 498 |
| 2 | 103 | 54 | 157 |
| 3 | 28 | 16 | 44 |
| 4 | 7 | 6 | 13 |
| 5 | 2 | 3 | 5 |
| Total | 451 | 266 | 717 |
The total number of cases for the first breast implant replacement/removal was n = 498, for the second breast implant replacement/removal n = 157, for the third breast implant replacement/removal n = 44, for the fourth breast implant replacement/removal n = 13, and for the fifth breast implant replacement/removal n = 5 (Table 1). Mean age at primary augmentation was 31.8 (18.2-58.7) years, and 48.6 (22.3-76.9) years in reconstructive cases.
The main indication for the first breast implant replacement/removal was capsular contracture in primary aesthetic (70.4%) and reconstructive cases (65.4%), followed by implant rupture in primary aesthetic cases (11.2%) and reconstructive cases (7.8%). All reasons for the first to third implant replacements or removals are summarized in Table 2. Due to the low number of cases for a fourth (n = 13) and fifth (n = 5) breast implant replacement or removal, statistical evaluation was not feasible. The corresponding time intervals up to the following replacements are summarized in Table 3.
Table 2.
Indications for Implant Replacement or Removal
| Indication | First Implant Replacement or Removal | Second Implant Replacement or Removal | Third Implant Replacement or Removal | |||
|---|---|---|---|---|---|---|
| Aesthetic | Reconstructive | Aesthetic | Reconstructive | Aesthetic | Reconstructive | |
| Capsular contracture | 195 (70.4%) | 100 (65.4%) | 72 (75.8%) | 30 (68.2%) | 24 (85.7%) | 7 (63.6%) |
| Implant rupture | 31 (11.2%) | 12 (7.8%) | 2 (2.1%) | 4 (9.1%) | — | 1 (9.1%) |
| Implant dislocation | 12 (4.3%) | 11 (7.2%) | 6 (6.3%) | 3 (6.8%) | 1 (3.6%) | 1 (9.1%) |
| Breast asymmetry | 10 (3.6%) | 9 (5.9%) | — | 2 (4.5%) | — | — |
| Apparent peri-prosthetic infection | 10 (3.6%) | 3 (2.0%) | 6 (6.3%) | 3 (6.8%) | 2 (7.1%) | 1 (9.1%) |
| PIP implant | 8 (2.9%) | 3 (2.0%) | 2 (2.1%) | — | — | — |
| Skin necrosis | 2 (0.7%) | 5 (3.3%) | — | 1 (2.3%) | — | — |
| Recurrence of primary tumor | 1 (0.4%) | 7 (4.6%) | — | — | 1 (3.6%) | 1 (9.1%) |
| Hematoma | 4 (1.4%) | — | 3 (3.2%) | — | — | — |
| Ptosis mammae | 4 (1.4%) | — | 4 (4.2%) | — | — | — |
| Prophylactic risk reducing mastectomy | — | 3 (2.0%) | — | — | — | |
| Seroma | — | — | — | 1 (2.3%) | — | — |
| Total | 277 | 153 | 95 | 44 | 28 | 11 |
| Unknown reasons | 34 | 34 | 8 | 10 | 0 | 5 |
| Total | 311 | 187 | 103 | 54 | 28 | 16 |
Table 3.
Time Intervals Until the First to Third Breast Implant Replacement/Removal
| Time Interval | Aesthetic p1–2 = 0,371 p2–3 = 0,632 | Reconstructive p1–2 = 0,949 p2–3= 0,234 | Total p1–2 = 0,489 p2–3 = 0,243 |
|---|---|---|---|
| First replacement/removal Mean 25th percentile Median 75th percentile CI N P < 0.001 |
12.3 y 5.2 y 11.0 y 18.1 y 11.4–13.4 y 311 |
6.8 y 1.0 y 2.7 y 11.7 y 5.7–7.9 y 187 |
10.2 y 2.1 y 9.6 y 15.6 y 9.5–11.1 y 498 |
| Second replacement/removal Mean 25th percentile Median 75th percentile CI N P = 0.004 |
9.1 y 2.3 y 9.0 y 14.0 y 7.5–10.4 y 103 |
5.8 y 1.0 y 2.9 y 11.4 y 4.2–7.3 y 54 |
8.0 y 1.3 y 6.4 y 13.0 y 6.7–9.0 y 157 |
| Third replacement/ removal Mean 25th percentile Median 75th percentile CI N P = 0.341 |
7.2 y 2.0 y 5.5 y 12.8 y 5.0–9.4 y 28 |
5.5 y 1.0 y 2.7 y 9.4 y 2.3–8.7 y 16 |
6.6 y 1.2 y 5.1 y 11.1 y 4.8–8.4 y 44 |
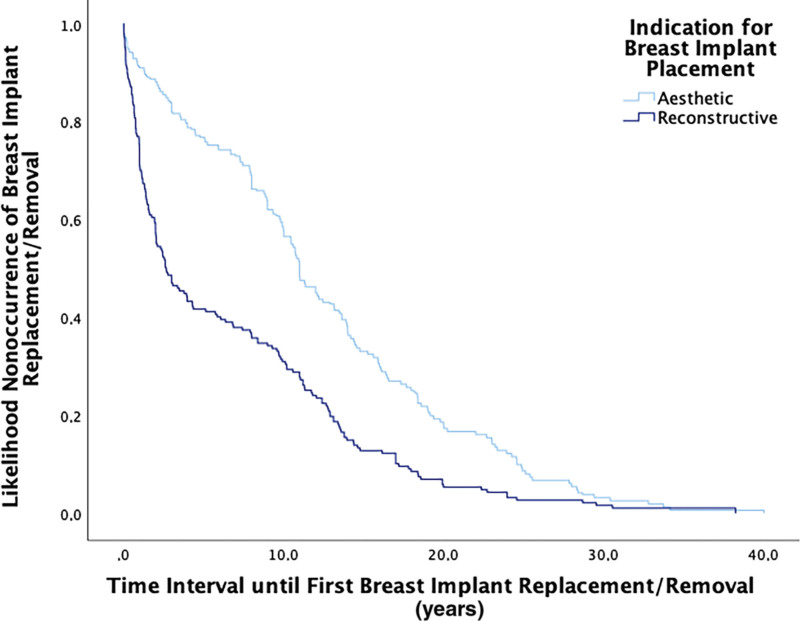
Looking at the time interval until the first breast implant replacement/removal considering the Kaplan-Meier curve, the difference between the aesthetic and reconstructive group becomes clearly visible. Half of all reconstructive implants were replaced or removed after only 2.7 years, whereas in primary aesthetic cases replacement or removal took place after 11.0 years. In one quarter of all reconstructive implants, the breast implant replacement/removal even took place within 1 year, compared with 5.2 years for the aesthetic implants (Fig. 2).
Fig. 2.
Kaplan-Meier curve of time interval until first breast implant replacement/removal, P < 0.001 (log-rank-test).
CAPSULAR CONTRACTURE
If the indication for breast implant replacement/removal was capsular contracture, the mean time interval to surgery was 14.3 years in the group of primary aesthetic augmentation and 8.4 years for the reconstructive. For the second breast implant replacement/removal this time interval was reduced to 9.7 years in the aesthetic group and to 4.1 years in the reconstructive group. In case of a third breast implant replacement/removal, it took place after a mean of 7.0 years in primary aesthetic cases. In the reconstructive patient population, this time interval was not assessable due to the low number of cases (n = 1). In both groups (aesthetic and reconstructive) and in the total collective, we observed a shortening of the time intervals between the procedures with increasing number of breast implant replacement/removals. This difference was significant for the time interval from the first to the second breast implant replacement/removal (p1–2 = 0.042) (Table 4). Further breast implant replacements or removals due to capsular contracture were only included for comparison if capsular contracture was also the reason for the prior revisions. Consequently, the cohort is smaller than the total of all capsular contractures at second and third revision (Table 2).
Table 4.
Time Intervals Until the First to Third Breast Implant Replacement/Removal due to Recurrent Capsular Contracture
| Time Interval | Aesthetic p1–2 = 0,039 p2 –3 = 0,279 | Reconstructive p1–2 = 0,130 | Total p1–2 = 0,042 p2–3 = 0,292 |
|---|---|---|---|
| First replacement/ removal Mean 25th percentile Median 75th percentile CI N P < 0.001 |
14.3 y 8.9 y 12.1 y 19.2 y 13.3–15.5 y 195 |
8.4 y 1.6 y 6.0 y 12.9 y 6.7–10.1 y 100 |
12.3 y 6.1 y 10.8 y 18.0 y 11.4–13.4 y 295 |
| Second replacement/removal Mean 25th percentile Median 75th percentile CI N P = 0.029 |
9.7 y 2.0 y 10.1 y 14.1 y 7.6–11.8 y 62 |
4.1 y 1.0 y 1.8 y 7.3 y 1.4–6.7 y 11 |
8.9 y 1.8 y 9.4 y 14.0 y 7.0–10.7 y 73 |
| Third replacement/removal Mean 25th percentile Median 75th percentile CI N P = 0.277 |
7.0 y 3.2 y 5.2 y 8,4 y 4.3–9.6 y 20 |
0.5 y 0.5 y 0.5 y 0.5 y – 1 |
6.7 y 2.4 y 4.8 y 8.4 y 4.1–9.2 y 21 |
CAPSULAR CONTRACTURE AND RADIATION
In the reconstructive cases, we evaluated the influence of prior radiation therapy on the timing of surgery due to capsular contracture. Thirty-one patients received prior radiotherapy of the breast, whereas 65 did not. The mean time interval until first implant replacement due to capsular contracture was 8.9 versus 6.4 years for nonirradiated or irradiated patients, respectively (P = 0.232). For the second (n = 11) and third implant change or removal (n = 1), the number of cases was too small to obtain a conclusive result.
IMPLANT RUPTURE
The mean time interval until implant rupture related implant replacement or removal was 16.8 years (1.5–39.9 years) in the cohort of primary aesthetic augmentations (n = 31) and 14.3 years (4.1 months–28.6 years) in reconstructive cases (n = 12; P = 0.379).
DISCUSSION
Capsular contracture is the most common cause of revisional surgery after augmentation or implant-based breast reconstruction.1–9 Coroneos et al observed in a cohort of 99,993 patients a 7-year incidence of capsular contracture after primary breast augmentation of 5% to 7% and in revisional augmentation 12% to 18%. In primary breast reconstruction, capsular contracture occurred in 9% to 13%, in revisional breast reconstruction in 10% to 18%.1 After radiotherapy, the risk of developing capsular contracture is reported to be as high as 18% to 42% within a follow-up interval of 8 to 13 years.11–16
To adequately educate patients about possible treatment alternatives before a planned revision, it is crucial to know if and when a relevant recurrence of the capsular contracture can be expected. The question then arises as to whether a new implant should be placed, or a change of procedure is advisable instead. In the case of initial aesthetic breast augmentation, this could be, for example, implant removal with mastopexy or lipofilling. In reconstructive cases, autologous breast reconstruction could be the favorable choice of procedure.
Clinically, we had the impression that capsular contracture occurred at increasingly shorter intervals after each implant replacement. Therefore, the aim of this study was to record changes in the time intervals between capsular contracture recurrences in our patient population. This information could help us provide more specific advice on the advantages and disadvantages of a renewed implant replacement versus change of procedure.
Capsular contracture was by far the most frequent indication for primary implant replacement or removal in our patient population. This applied to both primarily aesthetic (70.4%) and reconstructive cases (65.4%) and is consistent with information from the current literature. Kuehlmann et al found that 61.1% of their reconstructive and 70.8% of their aesthetic patients had developed capsular contracture, which was the main indication for revisional surgery in their study of 319 patients within 16 years.8 Forster et al also observed that 52.6% of their patients required revisional surgery due to capsular contracture; however, their study of 230 patients within 10 years only included aesthetic patients.7
In general, capsular contracture is a complication that usually only becomes clinically symptomatic after several years.7,8,13 In our population, the first implant replacement or removal due to capsular contracture had to be performed after an average of 12.3 years. However, revisional surgery occurred markedly earlier in reconstructive than in aesthetic patients if capsular contracture was the indication. Within the group of primary aesthetic augmentation, the time interval until the first replacement or removal was 14.3 years, whereas in the group of primary reconstructive it was only 8.4 years (P < 0.001). For the second revision, this time interval was 9.7 years and 4.1 years, respectively (P = 0.029). Kuehlmann et al also saw that implant replacement or removal became necessary earlier in their reconstructive patient population when surgery was performed due to capsular contracture. In their study, reconstructive patients required revision after 6.1 years, whereas in aesthetic patients this time interval was 11.9 years.8 The shortened time interval in breast reconstruction cases could be explained by the fact of more intense dissection, prolonged operation time and poor skin and soft tissue cover compared with aesthetic cases.4
Moreover, we found that in cases of recurrence of capsular contracture, time intervals shortened in both aesthetic and reconstructive patients. In the overall population of our patients, the time interval up to the second revision surgery decreased significantly compared with the time interval until the first revision surgery (8.9 years versus 12.3 years, P = 0.012). The time interval decreases again when an implant had to be replaced a third time (6.7 years, P = 0.192). Forster et al were also able to show a shortening of time intervals with increasing number of revisional procedures; however, they only considered a strictly aesthetic patient collective and did not differentiate time intervals for specific indications such as capsular contracture. In their study, the first revision surgery was performed after an average of 8.8 years and the second revision surgery after 11.4 months,7 whereas in our aesthetic patient population, this was only the case after 10.2 years and 8.0 years, respectively. In addition, several studies indicate that revisional surgery is associated with higher rates of capsular contracture than primary surgery.4,10,17–19 Either way, patients should be made aware that as the number of revisional procedures increases, the time interval in between may become significantly shorter. Furthermore, the markedly accelerated occurrence of capsular contracture recurrences suggests that alternative approaches to a renewed implant placement should be discussed with the patient. Autologous breast reconstruction could be considered in reconstructive cases, especially if capsular contracture occurred early after primary implant placement. In aesthetic cases, explantation and mastopexy could be the treatment of choice.
Radiotherapy is a recognized risk factor for complications in breast reconstruction with implants.20–25 Because it can cause fibrosis of the connective tissue,15,20,26 it particularly increases the occurrence of capsular contracture and thus the risk of reoperation.11–16,27,28 We also observed a tendency that radiotherapy is associated with earlier revisional surgery due to capsular contracture. After radiotherapy, the time interval until the first implant replacement or removal due to capsular contracture was 6.4 years, whereas in patients who had not received radiotherapy this was only the case after 8.9 years (P = 0.232). The missing statistical significance might be explained by our small sample size. However, a distinct trend could be identified regarding a shortening of the time interval between subsequent revisional procedures. The current literature reporting on the time interval until revisional procedures due to capsular contracture is very limited. Kuehlmann et al showed a time interval of 6.2 years for their patients who underwent radiotherapy and 5.1 years for their patients who did not, thus stating that capsular contracture does not occur earlier in irradiated patients.8 Eriksson et al also found no difference in time intervals with regard to radiotherapy. In their study, the time interval until revisional surgery was almost identical for nonirradiated and irradiated patients, amounting to approximately 17 months. However, they did not specifically look at patients presenting with capsular contracture, and their median follow-up of 43 months was relatively short.20 In comparison, Whitfield et al found 19.5% of their patients developed capsular contracture requiring revisional surgery within a 6-year interval after radiotherapy, whereas there was no case of capsular contracture in the group without radiotherapy (P > 0.001). Revisional surgery was performed after 21 to 50 months.15 Hvilsom et al also demonstrated that radiotherapy was related to an increased 10-year risk of both capsular contracture and revisional surgery.16 Although they assessed the need for revisional surgery independently of the occurrence of capsular contracture, the studies of Anker et al and Kearney et al indicate similar findings.27,28 For patients in whom radiotherapy is an indispensable part of the treatment, autologous breast reconstruction represents an alternative associated with a lower rate of revisional surgery.23,29,30 We already have concluded that in reconstructive cases, an alternative approach should be considered at an early stage to prevent and treat capsular contracture. Because after previous irradiation of the breast a higher incidence of capsular contracture with earlier onset is to be expected, this likely applies even more to this subgroup.
Implant dislocations or periprosthetic infections were more frequent indications for a second breast implant replacement or removal than for a first revision surgery, possibly due to a capsule left behind during the previous implant replacement. However, this observation was purely descriptive and showed no statistical significance. Nevertheless, Forster et al also found that the rate of both malposition of an implant (9.5 versus 12.6%) and periprosthetic infection (7.8 versus 16.1%) was higher in a second revision surgery.7 Thus, in the presence of a pronounced capsule, a complete capsulectomy might play a beneficial role.
This study is affected by several limiting factors. Firstly, the data have been obtained retrospectively and the sample size is comparatively small. Due to its retrospective nature, only correlations can be observed, but no causalities concluded. As a center for secondary referral, it could be that more patients with difficult courses have visited our clinic. Given that we have not evaluated the time at which the patient presented with clinical symptoms but the time-to-explant, it is possible that patients may decide to undergo surgery earlier for recurrent complaints, based on their previous experience, despite the same symptom course. In the current literature, capsular contracture rates are usually presented at a specific follow-up period, but the actual temporal occurrence is not investigated. Thus, the late course is usually neglected. Furthermore, follow-up is often short, so only a limited proportion of the total number of capsular contractures occurring are recorded at all.
Another limitation of this study is the missing evaluation of the implant site, which can also influence the development of capsular contracture.3,10,17,31,32 Therefore, a change of implant site is often recommended in the literature to reduce the recurrence of capsular contracture.4,31 Consequently, the missing data would certainly have been valuable with regard to an enhanced recommendation toward the prevention and therapy of capsular contracture. There is rather limited evidence on the surgical management of capsular contracture4 and further research might provide cost-effective solutions. Finally, the need for market approval has been the main reason why some survival studies have been conducted by the industry.33 Consequently, to provide an unbiased evaluation on the longevity of breast implants, an independent national or perhaps even international breast implant register may seem reasonable.34
The use of breast implants has become indispensable in modern breast surgery. They are used for both aesthetic and reconstructive indications to modulate and reconstruct the breast. However, the implantation of a foreign body into an organism is always associated with certain risks. The most frequent complication of breast implant surgery is capsular contracture, which necessitates revisional surgery at shorter intervals in recurrent cases. Based on our data, we feel obliged to offer patients with significant early onset capsular contracture the opportunity of an autologous reconstruction to save them the burden of repeated implant failure due to a recurring capsular contracture. However, given the retrospective study design, no definite conclusion can be drawn with any certainty. We recommend a prospective cohort study to provide a higher level of evidence on this important issue.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Coroneos CJ, Selber JC, Offodile AC, et al. US FDA breast implant postapproval studies: long-term outcomes in 99,993 patients. Ann Surg. 2019;269:30–36. [DOI] [PubMed] [Google Scholar]
- 2.Schaub TA, Ahmad J, Rohrich RJ. Capsular contracture with breast implants in the cosmetic patient: saline versus silicone—a systematic review of the literature. Plast Reconstr Surg. 2010;126:2140–2149. [DOI] [PubMed] [Google Scholar]
- 3.Stevens WG, Nahabedian MY, Calobrace MB, et al. Risk factor analysis for capsular contracture: a 5-year Sientra study analysis using round, smooth, and textured implants for breast augmentation. Plast Reconstr Surg. 2013;132:1115–1123. [DOI] [PubMed] [Google Scholar]
- 4.Wan D, Rohrich RJ. Revisiting the management of capsular contracture in breast augmentation: a systematic review. Plast Reconstr Surg. 2016;137:826–841. [DOI] [PubMed] [Google Scholar]
- 5.Blount AL, Martin MD, Lineberry KD, et al. Capsular contracture rate in a low-risk population after primary augmentation mammaplasty. Aesthetic Surg J. 2013;33:516–521. [DOI] [PubMed] [Google Scholar]
- 6.Gabriel SE, Woods JE, O’Fallon WM, et al. Complications leading to surgery after breast implantation. N Engl J Med. 1997;336:677–682. [DOI] [PubMed] [Google Scholar]
- 7.Forster NA, Künzi W, Giovanoli P. The reoperation cascade after breast augmentation with implants: what the patient needs to know. J Plast Reconstr Aesthet Surg. 2013;66:313–322. [DOI] [PubMed] [Google Scholar]
- 8.Kuehlmann B, Burkhardt R, Kosaric N, et al. Capsular fibrosis in aesthetic and reconstructive-cancer patients: a retrospective analysis of 319 cases. Clin Hemorheol Microcirc. 2018;70:191–200. [DOI] [PubMed] [Google Scholar]
- 9.Handel N, Cordray T, Gutierrez J, et al. A long-term study of outcomes, complications, and patient satisfaction with breast implants. Plast Reconstr Surg. 2006;117:757–67; discussion 768. [DOI] [PubMed] [Google Scholar]
- 10.Bachour Y, Bargon CA, de Blok CJM, et al. Risk factors for developing capsular contracture in women after breast implant surgery: a systematic review of the literature. J Plast Reconstr Aesthet Surg. 2018;71:e29–e48. [DOI] [PubMed] [Google Scholar]
- 11.Behranwala KA, Dua RS, Ross GM, et al. The influence of radiotherapy on capsule formation and aesthetic outcome after immediate breast reconstruction using biodimensional anatomical expander implants. J Plast Reconstr Aesthet Surg. 2006;59:1043–1051. [DOI] [PubMed] [Google Scholar]
- 12.Hammond JB, Kosiorek HE, Cronin PA, et al. Capsular contracture in the modern era: A multidisciplinary look at the incidence and risk factors after mastectomy and implant-based breast reconstruction. Am J Surg. 2021;221:1005–1010. [DOI] [PubMed] [Google Scholar]
- 13.Krueger EA, Wilkins EG, Strawderman M, et al. Complications and patient satisfaction following expander/implant breast reconstruction with and without radiotherapy. Int J Radiat Oncol Biol Phys. 2001;49:713–721. [DOI] [PubMed] [Google Scholar]
- 14.Benediktsson K, Perbeck L. Capsular contracture around saline-filled and textured subcutaneously-placed implants in irradiated and non-irradiated breast cancer patients: five years of monitoring of a prospective trial. J Plast Reconstr Aesthet Surg. 2006;59:27–34. [DOI] [PubMed] [Google Scholar]
- 15.Whitfield GA, Horan G, Irwin MS, et al. Incidence of severe capsular contracture following implant-based immediate breast reconstruction with or without postoperative chest wall radiotherapy using 40 Gray in 15 fractions. Radiother Oncol. 2009;90:141–147. [DOI] [PubMed] [Google Scholar]
- 16.Hvilsom GB, Holmich LR, Steding-Jessen M, et al. Delayed breast implant reconstruction: is radiation therapy associated with capsular contracture or reoperations? Ann Plast Surg. 2012;68:246–252. [DOI] [PubMed] [Google Scholar]
- 17.Spear SL, Murphy DK. Natrelle round silicone breast implants: core study results at 10 years. Plast Reconstr Surg. 2014;133:1354–1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lista F, Ahmad J. Evidence-based medicine: augmentation mammaplasty. Plast Reconstr Surg. 2013;132:1684–1696. [DOI] [PubMed] [Google Scholar]
- 19.Maxwell GP, Van Natta BW, Bengtson BP, et al. Ten-year results from the Natrelle 410 anatomical form-stable silicone breast implant core study. Aesthet Surg J. 2015;35:145–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eriksson M, Anveden L, Celebioglu F, et al. Radiotherapy in implant-based immediate breast reconstruction: risk factors, surgical outcomes, and patient-reported outcome measures in a large Swedish multicenter cohort. Breast Cancer Res Treat. 2013;142:591–601. [DOI] [PubMed] [Google Scholar]
- 21.Kronowitz SJ, Robb GL. Radiation therapy and breast reconstruction: a critical review of the literature. Plast Reconstr Surg. 2009;124:395–408. [DOI] [PubMed] [Google Scholar]
- 22.Berry T, Brooks S, Sydow N, et al. Complication rates of radiation on tissue expander and autologous tissue breast reconstruction. Ann Surg Oncol. 2010;17:202–210. [DOI] [PubMed] [Google Scholar]
- 23.Barry M, Kell MR. Radiotherapy and breast reconstruction: a meta-analysis. Breast Cancer Res Treat. 2011;127:15–22. [DOI] [PubMed] [Google Scholar]
- 24.Cordeiro PG, McCarthy CM. A single surgeon’s 12-year experience with tissue expander/implant breast reconstruction: part I. A prospective analysis of early complications. Plast Reconstr Surg. 2006;118:825–831. [DOI] [PubMed] [Google Scholar]
- 25.Ascherman JA, Hanasono MM, Newman MI, et al. Implant reconstruction in breast cancer patients treated with radiation therapy. Plast Reconstr Surg. 2006;117:359–365. [DOI] [PubMed] [Google Scholar]
- 26.Ricci JA, Epstein S, Momoh AO, et al. A meta-analysis of implant-based breast reconstruction and timing of adjuvant radiation therapy. J Surg Res. 2017;218:108–116. [DOI] [PubMed] [Google Scholar]
- 27.Anker CJ, Hymas RV, Ahluwalia R, et al. The effect of radiation on complication rates and patient satisfaction in breast reconstruction using temporary tissue expanders and permanent implants. Breast J. 2015;21:233–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kearney AM, Brown MS, Soltanian HT. Timing of radiation and outcomes in implant-based breast reconstruction. J Plast Reconstruct Aesthet Surg. 2015;68:1719–1726. [DOI] [PubMed] [Google Scholar]
- 29.Wong JS, Ho AY, Kaelin CM, et al. Incidence of major corrective surgery after post-mastectomy breast reconstruction and radiation therapy. Breast J. 2008;14:49–54. [DOI] [PubMed] [Google Scholar]
- 30.Jhaveri JD, Rush SC, Kostroff K, et al. Clinical outcomes of postmastectomy radiation therapy after immediate breast reconstruction. Int J Radiat Oncol Biol Phys. 2008;72:859–865. [DOI] [PubMed] [Google Scholar]
- 31.Stevens WG, Calobrace MB, Harrington J, et al. Nine-year core study data for Sientra’s FDA-approved round and shaped implants with high-strength cohesive silicone gel. Aesthet Surg J. 2016;36:404–416. [DOI] [PubMed] [Google Scholar]
- 32.Namnoum JD, Largent J, Kaplan HM, et al. Primary breast augmentation clinical trial outcomes stratified by surgical incision, anatomical placement and implant device type. J Plast Reconstruct Aesthet Surg. 2013;66:1165–1172. [DOI] [PubMed] [Google Scholar]
- 33.Seigle-Murandi F, Lefebvre F, Bruant-Rodier C, et al. Incidence of breast implant rupture in a 12-year retrospective cohort: evidence of quality discrepancy depending on the range. J Plast Reconstruct Aesthet Surg. 2017;70:42–46. [DOI] [PubMed] [Google Scholar]
- 34.Kuehlmann B, Prantl L. Need for a German Breast Implant Registry – pilot project breast implant template. Handchir Mikrochir Plast Chir. 2016;48:199–204. [DOI] [PubMed] [Google Scholar]