Abstract
Shaping network members into sources of support for healthy eating and exercise behaviors may be an effective strategy to enhance obesity treatment outcomes. This pilot study examined the feasibility and preliminary efficacy of a behavioral weight loss intervention adapted for Latinas with a social network component. Twenty-seven Latinas (43.0 ± 10.2 years and BMI 36.9 ± 5.7 kg/m2) participated in a 24 week randomized controlled intervention study. Participants attended group-based treatment either individually (Individual Lifestyle Group; ILG) or with a weight loss partner selected from their existing network (Partner Lifestyle Group; PLG). Repeated measures analysis of variance was conducted to compare ILG and PLG participants on changes in weight or psychosocial variables. Participants in both intervention groups attended 70% of treatment sessions; 96% and 100% completed assessment at post-treatment (12 weeks) and follow-up (24 weeks), respectively. Significant weight loss (p<0.01) was achieved at post-treatment (ILG −4.7 ± 4.2 kg and PLG −4.3 ± 4.4 kg) and follow-up (ILG −5.0 ± 6.4 kg and PLG −4.7 ± 5.0 kg), with nearly 50% of participants losing at least 5% of initial body weight. Both groups also experienced increased self-efficacy for weight loss (p<0.01), self-efficacy for exercise (p=0.02), and family social support for exercise habits (p=0.01). There were no significant differences between groups. Results from this study suggest a behavioral weight loss intervention for Latinas is feasible but there is less support for the efficacy of weight loss partners.
Keywords: obesity, weight loss, social support network, randomized clinical trial, Latina
INTRODUCTION
Latinos are the largest ethnic minority group in the United States and have high rates of obesity, especially among women.1 According to the Behavioral Risk Factor Surveillance System, Latinas were found to be more likely to attempt weight loss than non-Hispanic White women.2, 3 However, they were least likely to follow the recommendations of consuming less calories and exercising at least 150 minutes per week. Furthermore, participating in organized weight loss programs was less common among Latinas than non-Hispanic Whites.3 Therefore, an intervention aimed at helping Latinas develop lifestyle skills shown to promote weight loss is warranted.
Latinas in weight loss studies using more individual treatment approaches tend not to fare as well as non-Hispanic Whites in study outcomes such as attendance, dietary adherence, and weight loss.4, 5 Evidence suggest that implementing social network strategies for weight management may be more culturally salient for Latinas, and therefore potentially improve intervention outcomes over the individually focused methods traditionally used. First, having at least one network member who encourages fruit and vegetable consumption or physical activity is associated with motivation to engage in such behaviors among Latinos.6 Second, family support specific to diet and exercise is associated with greater medical adherence among Mexican Americans.7 Third, Latinas who report knowing people who exercise are more likely to be active.8 Finally, Latinos participating in team-based weight loss interventions lose significantly more weight compared to non-Latinos.9 Hence, identifying potential sources of support or shaping networks to include sources of support for initiation and maintenance of health behaviors may represent an effective strategy to enhance obesity treatment outcomes for this high risk population.
Given that weight-related behaviors are influenced by social relationships10 and obesity clusters in social networks,11 weight loss studies with a social network component have reported positive outcomes. Previous work by Wing and Jeffery12 found that participants attending a behavioral weight control program with friends had better treatment completion and greater weight loss maintenance compared to participants who attended treatment alone. Other studies found that participating with friends or family members was associated with greater weight loss only when the partners or team-mates themselves were successful at adopting dietary changes13, 14 or losing weight,13,15 indicating that the influence that network members have on one another’s behaviors can be harnessed to support adherence to recommended practices important for weight control.
The purpose of this pilot study was to examine the feasibility and preliminary efficacy of a behavioral weight loss intervention for Latinas that included a weight loss partner selected from their existing social network. We hypothesized weight loss partners would improve treatment adherence, study retention, and weight loss in a lifestyle program adapted for Latinas.
METHODS
Recruitment & Eligibility
Figure 1 shows the flow of participants through the study. Participants were recruited through local media outlets, employer intranet, and community organizations. Participants deemed eligible by initial phone screen, were invited to attend an orientation and screening visit where informed consent was obtained and baseline data were collected. To be eligible for the study, participants were required to be female, 18 to 65 years of age, have BMI of 27–50 kg/m2, self-identify as Hispanic or Latino, and report speaking and reading English well. Individuals were excluded for pregnancy, > 5% weight loss in the last 6 months, history of bariatric surgery, and serious medical condition or psychological disorder. The Institutional Review Board at the Miriam Hospital approved the research protocol for this study.
Figure 1:
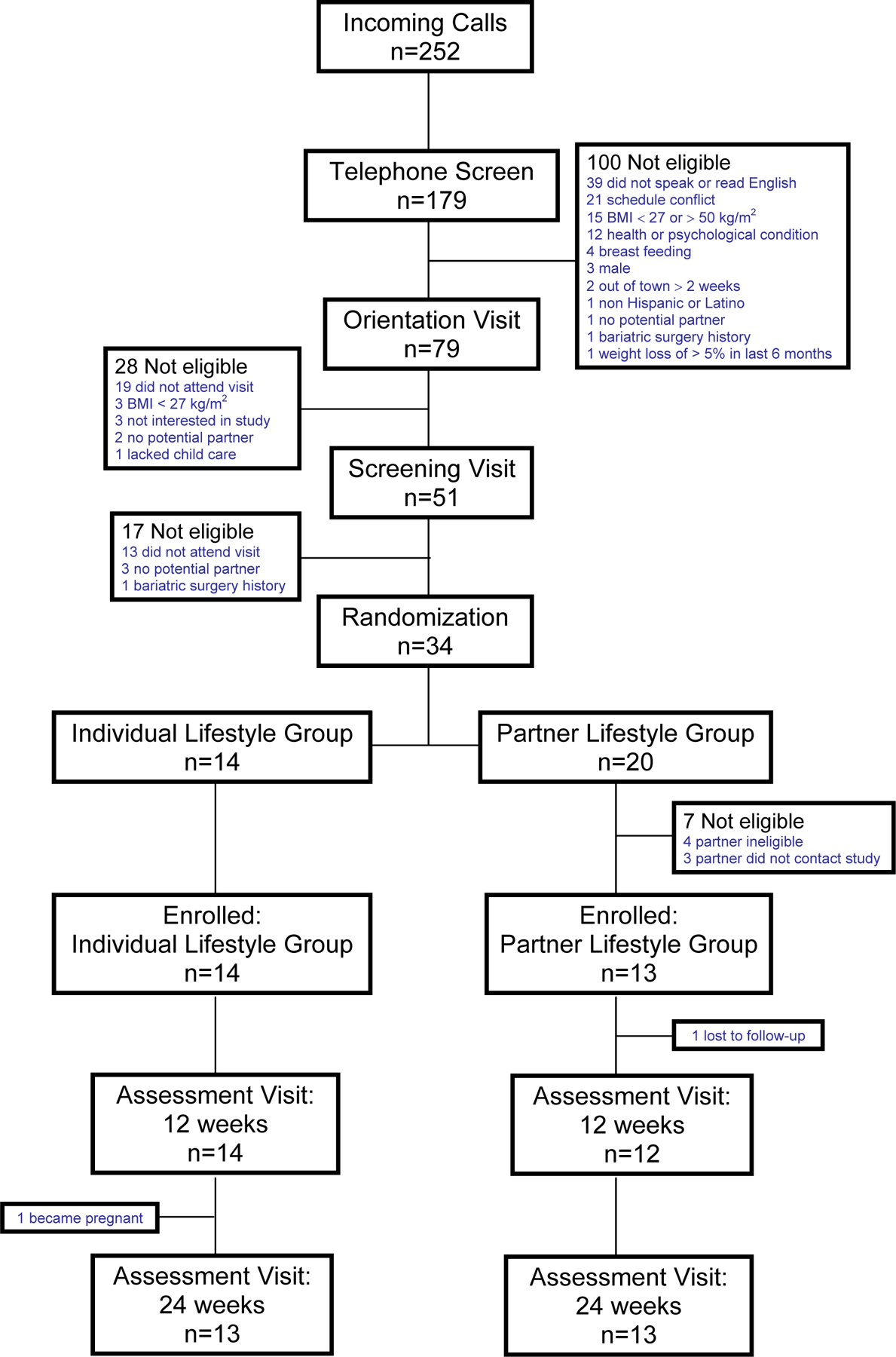
Participant flow in Comadres.
Randomization
Participants were randomly assigned to the Individual Lifestyle Group (ILG) or Partner Lifestyle Group (PLG). Once randomized, PLG assigned participants were required to identify a member of their social network to join them in the program as a weight loss partner. The partner had to contact the study, meet eligibility criteria described previously, and attend an orientation to sign informed consent. If an eligible partner was not identified, the PLG assigned participant could not enroll in the program. Anticipating that some PLG assigned participants would not meet the partner eligibility criteria, we performed 2:3 randomization to achieve equal group sizes at enrollment.
Intervention
Both ILG and PLG participated in a group-based behavioral weight loss program modeled after the Diabetes Prevention Program (DPP) curriculum promoting lifestyle change in diet and exercise. Groups met for 12 weekly sessions at the Weight Control & Diabetes Research Center, in Providence, Rhode Island. All sessions included a private weigh-in and one hour group meeting. Sessions were cofacilitated by a dietitian and doctoral level interventionist.
Participants were prescribed a calorie and fat gram goal designed to produce weight loss of 0.5–1 kg/week. Participants with baseline weight of ≤ 91 kg or ≥ 91 kg were assigned 1200 kcal/day or 1500 kcal/day, respectively, and ≤ 30% of daily calories from fat. A calorie and fat reference book, food scale, measuring cups/spoons, and sample meal plans were given to participants. Participants were instructed to gradually increase physical activity to ≥ 30 minutes/day of moderate intensity activity 5 days/week. Participants were given pedometers and encouraged to work up towards 10,000 steps/day.
Participants were taught standard behavioral weight loss techniques including goal setting, planning ahead, problem solving, stimulus control, cognitive restructuring, and relapse prevention.15 Self-monitoring was strongly emphasized throughout the intervention as participants were asked to record their food (calorie and fat) intake, type and duration of exercise, pedometer steps, and body weight in their daily diaries. Participants submitted their self-monitoring records at each session. Self-monitoring records were returned the following session with written feedback from the interventionists.
Adapted Program Components
The name “Comadres” weight loss program was chosen to promote group identity based on a cultural theme signifying a close bond between women. Based on formative research, we implemented a weight loss program that was exclusively for females, had an all female staff, was cofacilitated by a bilingual/bicultural Latina interventionist, emphasized the health benefits associated with healthy eating and exercise, and promoted walking and dancing for physical activity.
We incorporated information collected from participant food records, recipes, and homework assignments into the nutrition component of the intervention. A booklet called the “Cocina Latina Calorie Guide” with fat and calorie content of ethnic foods was distributed to participants. Culturally adapted nutrition education focused on encouraging continued consumption of traditional meals and modified cooking methods. Participants also received a booklet with their own modified recipes of traditional Latino dishes called “Low Calorie Meals for Any Occasion”.
Difference between ILG and PLG
Both study conditions received the same culturally adapted version of DPP described above but PLG participants also had a female weight loss partner. Session activities focused on improving partner communication and collaboration. We also encouraged dyads to check-in with each other and engage in activity together (i.e., grocery shop, prepare a healthy meal, take a walk) during the week.
Assessments
Assessments took place at baseline, post-treatment (12 weeks), and follow-up (24 weeks). At baseline, participants reported demographic and health information and had their height measured with a stadiometer using standard procedure. At each assessment point, participants were weighed and completed questionnaires. BMI was calculated with the formula weight in kilograms/height in meters2. Questionnaires included the Weight Efficacy Lifestyle Questionnaire,16 self-efficacy for exercise,17 Social Support for Diet and Exercise Behaviors Questionnaire,18 and Paffenbarger Activity Questionnaire.19 Participants were paid $20 for completing the post-treatment and follow-up assessments.
Adherence & Acceptability
Adherence was assessed by number of intervention sessions attended and number of self-monitoring records submitted. To assess acceptability, at post-treatment participants were asked to rate program components on a 7-point Likert scale (1=not at all helpful; 7=extremely helpful) and answer open-ended questions.
Statistical Analyses
Group differences in baseline characteristics were examined using two-sample t-test for continuous variables or chi-square test for categorical variables. Primary outcomes were treatment adherence, study retention, and weight change. Secondary outcomes were changes in psychosocial variables and physical activity. Repeated measures analysis of variance was conducted to compare ILG and PLG participants on changes in weight or psychosocial variables. Differences between PLG participants and their weight loss partners were assessed via paired t-test. An intent-to-treat analysis was performed in which baseline values were substituted for unavailable data. All analyses were performed using SPSS software, version 14 (©SPSS, Inc., Chicago, IL).
RESULTS
Study Population
Thirty-four individuals were randomized to ILG (n=14) or PLG (n=20) (Fig. 1). However, 7 PLG assigned participants could not enroll in the program because their partners were ineligible or did not contact the study. As a result, a final sample of 27 participants was obtained (ILG=14; PLG=13).
There were no differences between ILG and PLG in baseline characteristics (Table 1). Most participants were Caribbean Latinas and born outside the mainland United States (66%). Participants were generally well-educated, married or living with a significant other, and parents of children under the age of 18 years (61%). The average BMI was 36 kg/m2.
Table 1.
Baseline characteristics of participants in Comadres.
| ILG | PLG | Partner | |
|---|---|---|---|
| n | 14 | 13 | 13 |
| Age (mean ± S.D.) | 41.7 ± 10.5 | 44.3 ± 10.0 | 37.0 ± 10.5 |
| Ethnicity (%) | |||
| Dominican | 35.7 | 30.8 | 38.5 |
| Puerto Rican | 14.3 | 30.8 | 23.1 |
| Columbian | 7.1 | 23.1 | 7.7 |
| Other | 42.9 | 15.3 | 30.7 |
| Generation in U.S. (%) | |||
| 1st generation | 64.3 | 69.2 | 65.0 |
| Years residing in U.S. (mean ± S.D.) | 25.2 ± 15.3 | 32.5 ± 6.9 | 21.1 ± 10.2 |
| 2nd generation | 28.6 | 30.8 | 32.5 |
| 3rd generation | 7.1 | 0.0 | 2.5 |
| Language Speak and Read (%) | |||
| More Spanish than English | 21.4 | 15.4 | 7.7 |
| Spanish and English equally | 42.9 | 38.5 | 46.2 |
| More English than Spanish | 28.6 | 46.2 | 38.5 |
| Only English | 7.1 | 0.0 | 7.7 |
| Education (%) | |||
| High School Graduate | 42.9 | 69.2 | 61.5 |
| College Degree | 57.1 | 30.8 | 38.5 |
| Income (%) | |||
| ≥ $10,000–19,999 | 14.3 | 15.4 | 7.7 |
| ≥ $20,000–39,999 | 21.4 | 23.1 | 38.5 |
| ≥ $40,000–59,999 | 35.7 | 38.5 | 38.5 |
| ≥ $60,000 | 28.6 | 23.0 | 15.3 |
| BMI (mean kg/m2 ± S.D.) | 36.6 ± 5.5 | 37.1 ± 6.2 | 34.2 ± 4.1 |
| Weight (mean kg ± S.D.) | 92.5 ± 16.6 | 95.2 ± 19.0 | 88.3 ± 11.0 |
Attendance & Retention
Participants attended an average of 70% of 12 sessions with no significant difference in number of sessions attended for ILG (8.3 ± 3.1) and PLG (8.5 ± 3.4) (p=0.88). More than 60% of absences were because of family responsibilities (childcare, family functions, or tending to an ill family member). Participants submitted an average of 68% self-monitoring diaries, with no significant difference between ILG (8.2 ± 3.7) and PLG (8.0 ± 3.7) (p=0.88). Retention of enrolled participants was high; 96% and 100% of study participants completed assessments at post-treatment and follow-up, respectively.
Changes in Weight, Psychosocial Parameters, & Physical Activity
Both groups achieved significant weight loss at post-treatment (ILG −4.7 ± 4.2 kg and PLG −4.3 ± 4.4 kg) and follow-up (ILG −5.0 ± 6.4 kg and PLG −4.7 ± 5.0 kg), with almost 50% achieving at least 5% weight loss (Table 2). There were no significant differences between groups (p=0.92).
Table 2.
Weight changes* for participants in Comadres.
| Post-treatment | Follow-up | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| ILG | PLG | Partner | ILG | PLG | Partner | |
| Weight change (mean kg ± S.D.) | −4.7 ± 4.2 | −4.3 ± 4.4 | −2.4 ± 3.2 | −5.0 ± 6.4 | −4.7 ± 5.0 | −2.8 ± 3.7 |
| % Weight change (mean ± S.D.) | 5.2 ± 4.2 | 4.4 ± 4.4 | 2.8 ± 3.6 | 5.5 ± 6.0 | 4.7 ± 4.9 | 3.2 ± 4.2 |
| ≥ 5% weight loss (%) | 50.0 | 46.2 | 23.1 | 38.5 | 53.8 | 23.1 |
Different from baseline (p≤0.01). Changes over time are significant for ILG, PLG, and partners but there were no significant differences between ILG and PLG or PLG and partners.
The groups also experienced similar changes in psychosocial parameters, with increases in weight loss self-efficacy (p<0.01), exercise self-efficacy (p=0.02), and family social support for exercise habits (participation and involvement; p=0.01) over time; each of these parameters increased between baseline and post-treatment, but only improvement in weight loss self-efficacy was maintained at follow-up. Changes in physical activity were not significant (p=0.59).
Correlations with Weight Loss
Across groups, there was a positive relationship between weight loss at post-treatment and the number of sessions attended (r=.58, p<0.01), number of diaries submitted (r=.73, p<0.01), total kilocalories per week expended (r=.51, p<0.01), weight loss self-efficacy (r=.44, p=0.03), and friend social support for eating habits (positive comments; r=.59, p<0.01).
Weight Loss Partners
Weight loss partners selected by PLG participants were friends (69%) and family members (31%) including mother, daughters, and sister. The majority of PLG participants (69%) characterized the relationship with their partners as close or very close. PLG participants reported having weekly contact with their partners through phone calls (92%), in-person visits (77%), and e-mails (31%). All PLG participants and partners lived in separate households. There were no significant differences between PLG participants and partners in baseline characteristics (Table 1) except that among the first generation, partners resided less years in the U.S. than PLG participants (p=0.01).
Weight loss partners attended an average of 8.0 ± 3.5 sessions and submitted 7.6 ± 4.0 diaries, which did not differ from PLG participants. There was a strong positive relationship between PLG participants and partners in attendance (r=.91, p<0.01) and diary submission (r=.85, p<0.01). Partners lost an average of −2.4 ± 3.2 kg at post-treatment (p=0.01) and −2.8 ± 3.7 kg at follow-up (p=0.01) (Table 2). Only 25% of partners lost at least 5% of body weight at post-treatment and follow-up. The difference between PLG participants and partners in weight loss did not reach significance at post-treatment (p=0.17) or follow-up (p=0.27). In addition, there was no significant association between the weight loss of PLG participants and their partners at post-treatment (r=.30, p=0.30) or follow-up (r=.24, p=0.43).
Program Acceptability
Overall, the program was well received, with adapted features generally rated among the more helpful components. Written feedback was likewise positive, with comments such as “I never felt that I was on a diet, I love the fact that I learn how to eat healthy but continue to eat my rice and beans.” PLG participants tended to rate the weight loss partner component relatively less helpful. Comments about partners ranged from “She was great, tried to keep me on track and very informative” to “She is very busy between work and family commitments. I don’t think she has the time to check on me.”
DISCUSSION
This culturally adapted intervention was associated with weight losses of over 4 kg and nearly half of participants achieving at least 5% weight loss at post-treatment, with no significant weight regain at follow-up. Weight losses of this magnitude have been shown to provide important health benefits and are clinically relevant.20, 21 Participants who attended more sessions and submitted more self-monitoring diaries, achieved greater weight loss. The intervention also produced other benefits including improved self-efficacy for weight loss or exercise, and increased family support for exercise habits. Such positive outcomes may speak in part to the strength of the behavioral component of the curriculum, which was likewise effective in large randomized clinical trials including DPP20 and Look Ahead.22
The current study was modeled after DPP but attempted to influence the socio-environmental context of women by building on an already existing potential support source. In doing so, we expected to promote health behaviors important for weight management long after the intervention. It has been shown that enhancing social support can be an effective strategy for weight loss. Wing and Jeffery12 found that participants attending a behavioral weight control program with friends had better treatment completion and greater weight loss maintenance compared to participants who attended treatment alone. Given that women were found to respond positively to behavioral treatment with a partner,14 we saw great promise in enlisting social network members as a strategy to treat Latinas in a weight control intervention. However, participating with a weight loss partner did not result in additional improvement in session attendance, diary submissions, or weight loss.
Despite participating as dyads, weight loss partners tended to lose less weight than PLG participants suggesting they may have been less motivated for weight loss. Partners were recruited by PLG participants and may have varied in readiness for lifestyle change. Interestingly, whereas the number of sessions attended and diaries submitted by PLG participants were highly related to those of the partner, weight change was not. In contrast, a previous study reported that participants who brought partners to treatment lost significantly more weight when the partners themselves were successful at losing weight.13 Given that foreign-born partners resided less years in the U.S. than PLG participants even after controlling for age, differences in acculturation may partly explain the lack of weight loss relationship in the current study. Low acculturated overweight Latinas are reportedly less likely to want to lose weight compared to high acculturated Latinas23 because of a cultural preference for a curvier shape or belief that extra weight is a sign of health and prosperity.24–26 Alternatively, because this intervention included a mix of generations in the U.S. and participants often switched from communicating in English to Spanish and vice versa during sessions, partners may have benefited more from an intervention specifically adapted for low acculturated Latinas.
Although enlisting family or friends did not enhance weight loss outcomes for ethnically diverse Latinas, our results are consistent with other weight loss trials of Mexican-American and African-American samples. In Cuidando El Corazon, a 1-year intervention of 168 Mexican-Americans, women attending a lifestyle program with their male partners did not achieve greater weight loss compared to women that attended individually.27 Moreover, in the 2-year SHARE (Supporting Healthy Activity and eating Right Everyday) trial, which consisted of 344 African-Americans, women participating with family members or friends did not experience further weight loss.28
From formative research we learned that for Latinas in the United States traditional culture was still salient. By integrating input from the target population, we were able to offer an adapted weight loss program that was positively received by participants. Participants rated staff features among the more helpful program components. This underscores the importance of having culturally competent staff to establish good rapport with participants from the start and is consistent with the value Latinos place on interpersonal relationships.29, 30
The current study provides valuable information but there are limitations that should be considered. First, as a pilot study our sample size was small and intervention outcomes were not observed beyond 24 weeks. Second, given that our sample was English speaking and generally higher educated, our findings may not be applicable to Spanish speaking and lesser educated Latinas. Third, 7 out of 20 participants randomized to the partner lifestyle group could not enroll in the program because of partner ineligibility, suggesting different recruitment and randomization strategies should be considered. For example, dyads instead of individuals could be recruited and randomized. We did not pursue this approach because we were sensitive to the possibility of disappointing dyads if randomized to the individual lifestyle group which meant only one member would be allowed to participate in the program.
There are several strengths to this study that should be highlighted. A randomized control design was used in this study. We recruited an ethnically diverse sample of Latinas, which increases the generalizability of our findings. We integrated intervention features identified by the target population itself resulting in a culturally relevant program that was well received by participants. The study also had excellent retention and significant weight loss was achieved and maintained. These results are especially relevant given that previous weight loss studies targeting Latinas have reported poor retention and/or weight loss outcomes.27, 31–33
CONCLUSION
Given that the prevalence of obesity continues to rise among Latinas, efforts to develop weight loss programs that address the cultural and socio-environmental needs of this high-risk population are imperative. Results from this pilot study suggest a behavioral weight loss intervention for Latinas is feasible but there is less support for the efficacy of female weight loss partners. Hence, although enlisting members of participants’ social networks did not enhance study outcomes, we found excellent retention, significant weight loss, and positive psychosocial changes could be achieved in an adapted lifestyle program for ethnically diverse Latinas.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA 2012;307(5):491–497. [DOI] [PubMed] [Google Scholar]
- 2.Mack KA, Anderson L, Galuska D, Zablotsky D, Holtzman D, Ahluwalia I. Health and sociodemographic factors associated with body weight and weight objectives for women: 2000 behavioral risk factor surveillance system. J Womens Health (Larchmt) 2004;13(9):1019–1032. [DOI] [PubMed] [Google Scholar]
- 3.Serdula MK, Mokdad AH, Williamson DF, Galuska DA, Mendlein JM, Heath GW. Prevalence of attempting weight loss and strategies for controlling weight. JAMA 1999;282(14):1353–1358. [DOI] [PubMed] [Google Scholar]
- 4.Wadden TA, West DS, Neiberg RH, et al. One-year weight losses in the Look AHEAD study: factors associated with success. Obesity (Silver Spring) 2009;17(4):713–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.West DS, Elaine Prewitt T, Bursac Z, Felix HC. Weight loss of black, white, and Hispanic men and women in the Diabetes Prevention Program. Obesity (Silver Spring) 2008;16(6):1413–1420. [DOI] [PubMed] [Google Scholar]
- 6.Ashida S, Wilkinson AV, Koehly LM. Social influence and motivation to change health behaviors among Mexican-origin adults: implications for diet and physical activity. Am J Health Promot 2012;26(3):176–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wen LK, Shepherd MD, Parchman ML. Family support, diet, and exercise among older Mexican Americans with type 2 diabetes. Diabetes Educ 2004;30(6):980–993. [DOI] [PubMed] [Google Scholar]
- 8.Evenson KR, Sarmiento OL, Ayala GX. Acculturation and physical activity among North Carolina Latina immigrants. Soc Sci Med 2004;59(12):2509–2522. [DOI] [PubMed] [Google Scholar]
- 9.Leahey TM, Crane MM, Pinto AM, Weinberg B, Kumar R, Wing RR. Effect of teammates on changes in physical activity in a statewide campaign. Prev Med 2010;51(1):45–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berkman LF, Glass T. Social integration, social networks, social support, and health. In: Berkman LF, Kawachi I, eds. Social Epidemiology New York: Oxford University Press; 2000:137–173. [Google Scholar]
- 11.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med 2007;357(4):370–379. [DOI] [PubMed] [Google Scholar]
- 12.Wing RR, Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. J Consult Clin Psychol 1999;67(1):132–138. [DOI] [PubMed] [Google Scholar]
- 13.Gorin A, Phelan S, Tate D, Sherwood N, Jeffery R, Wing R. Involving support partners in obesity treatment. J Consult Clin Psychol 2005;73(2):341–343. [DOI] [PubMed] [Google Scholar]
- 14.Wing RR, Marcus MD, Epstein LH, Jawad A. A “family-based” approach to the treatment of obese type II diabetic patients. J Consult Clin Psychol 1991;59(1):156–162. [DOI] [PubMed] [Google Scholar]
- 15.Wing RR. Behavioral approaches to the treatment of obesity. In: Bray GA, Bouchou C, eds. Handbook of obesity 2nd ed. New York: Marcel Dekker, Inc; 2004:147–167. [Google Scholar]
- 16.Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self-efficacy in weight management. J Consult Clin Psychol 1991;59(5):739–744. [DOI] [PubMed] [Google Scholar]
- 17.Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport 1992;63(1):60–66. [DOI] [PubMed] [Google Scholar]
- 18.Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med 1987;16(6):825–836. [DOI] [PubMed] [Google Scholar]
- 19.Paffenbarger RS Jr, Wing AL, Hyde RT. Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol 1978;108(3):161–175. [DOI] [PubMed] [Google Scholar]
- 20.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346(6):393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tuomilehto J, Lindstrom J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001;344(18):1343–1350. [DOI] [PubMed] [Google Scholar]
- 22.Pi-Sunyer X, Blackburn G, Brancati FL, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Diabetes Care 2007;30(6):1374–1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahluwalia IB, Ford ES, Link M, Bolen JC. Acculturation, weight, and weight-related behaviors among Mexican Americans in the United States. Ethn Dis 2007;17(4):643–649. [PubMed] [Google Scholar]
- 24.Lindberg NM, Stevens VJ. Immigration and Weight Gain: Mexican-American Women’s Perspectives. J Immigr Minor Health 2011;13(1):155–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ramirez AG, Chalela P, Gallion K, Velez LF. Energy balance feasibility study for Latinas in Texas: a qualitative assessment. Prev Chronic Dis 2007;4(4):A98. [PMC free article] [PubMed] [Google Scholar]
- 26.Sussner KM, Lindsay AC, Greaney ML, Peterson KE. The influence of immigrant status and acculturation on the development of overweight in Latino families: a qualitative study. J Immigr Minor Health 2008;10(6):497–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cousins JH, Rubovits DS, Dunn JK, Reeves RS, Ramirez AG, Foreyt JP. Family versus individually oriented intervention for weight loss in Mexican American women. Public Health Rep 1992;107(5):549–555. [PMC free article] [PubMed] [Google Scholar]
- 28.Kumanyika SK, Wadden TA, Shults J, et al. Trial of family and friend support for weight loss in African American adults. Arch Intern Med. 2009;169(19):1795–1804. [DOI] [PubMed] [Google Scholar]
- 29.Garcia-Preto N Puerto Rican families. In: McGoldrick M, Giordano J, Garcia-Preto N, eds. Ethnicity & family therapy New York: The Guilford Press; 2005:242–255. [Google Scholar]
- 30.Santiago-Rivera AL, Arredondo P, Gallardo-Cooper M. Counseling Latinos and la familia: A practical guide Thousands Oaks: Sage Publications; 2002. [Google Scholar]
- 31.Poston WS, Reeves RS, Haddock CK, et al. Weight loss in obese Mexican Americans treated for 1-year with orlistat and lifestyle modification. Int J Obes Relat Metab Disord 2003;27(12):1486–1493. [DOI] [PubMed] [Google Scholar]
- 32.Domel SB, Alford BB, Cattlett HN, Rodriguez ML, Gench BE. A pilot weight control program for Hispanic women. J Am Diet Assoc 1992;92(10):1270–1271. [PubMed] [Google Scholar]
- 33.Avila P, Hovell MF. Physical activity training for weight loss in Latinas: a controlled trial. Int J Obes Relat Metab Disord 1994;18(7):476–482. [PubMed] [Google Scholar]


