Abstract
We aimed to compare the characteristics and outcomes of adult patients hospitalized with myocarditis and either concomitant corona virus disease 2019 (COVID-19) or influenza, and elucidate clinical predictors associated with adverse outcomes in both groups. The study used the national inpatient sample (NIS) from 2019 to 2020 to identify 27,725 adult myocarditis hospitalizations, of which 5840 had concomitant COVID-19 and 1045 had concomitant influenza. After propensity score matching, the in-hospital mortality from myocarditis was significantly higher in COVID-19 compared to influenza. Patients with myocarditis and COVID-19 were more likely to have cardiovascular comorbidities and be older than those with influenza-associated myocarditis. Predictors of mortality were also different in both groups.
Viral infections are the most common cause of myocarditis with a heterogeneous clinical presentation.1 Coronavirus disease 2019 (COVID-19) and influenza virus share a variety of common features, including route of transmission and similar clinical presentations. Both COVID-19 as well as influenza related myocarditis and associated poor outcomes has been described.2 , 3 Previous studies have compared clinical outcomes of influenza and COVID-19 infection, however, a direct comparison of outcomes and characteristics of associated myocarditis has not been reported.4 Analyzing a large, national data set, we aimed to compare the characteristics and outcomes of adult patients hospitalized with myocarditis and either concomitant COVID-19 or influenza, and elucidate clinical predictors associated with adverse outcomes in both groups.
We queried the national inpatient sample (NIS) from 2019 to 2020 for all hospitalizations for myocarditis with concomitant COVID-19 or influenza. The primary outcome of interest was in-hospital mortality. A 1:1 propensity score-matched analysis was performed to adjust for possible confounders. STATA 16.0 was used for analysis.
A total of 27,725 adult myocarditis hospitalizations (11,065 in 2019 and 16,660 in 2020) were identified of which 1045 (3.7%) had concomitant influenza and 5840 (21.1%) had concomitant COVID-19. There was a significantly increasing trend of myocarditis hospitalizations from 2019 to 2020 with ∼1.5 times increase in hospitalization in 2020.
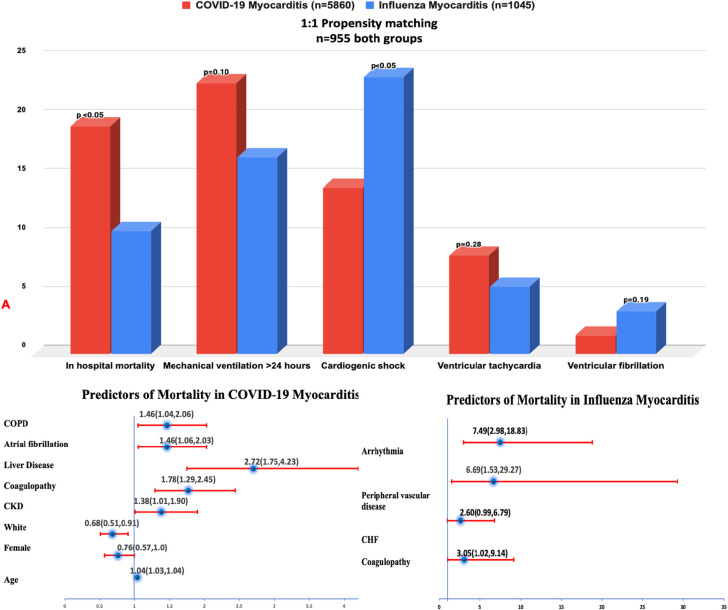
Patients with myocarditis with concomitant COVID-19 vs influenza were more likely to be older (64 vs 48 years, P < 0.001), male (61.6 vs 47.8%, P = 0.0003) and more likely to be African American (21.8% vs 15.3%, P = 0.05). Myocarditis patients with COVID-19 were also more likely to have cardiovascular comorbidities such as hypertension (61.9% vs 50.0%, P < 0.001), diabetes (37.9% vs 21.1%, P < 0.001), chronic kidney disease (24.7% vs 13.9%, P < 0.001), atrial fibrillation (18.3% vs 8.6%, P < 0.001), coronary artery disease (24.7% vs 17.7%, P < 0.05), and obesity (24.1% vs 14.8%, P < 0.001). After propensity score matching, the in-hospital mortality from myocarditis was significantly higher in COVID-19 compared to influenza (19.4% vs 10.5%, P < 0.05). Using logistic regression analysis, age, liver disease, atrial fibrillation, chronic obstructive pulmonary disease, and coagulopathy were identified as independent predictors of mortality in COVID-19 patients. In influenza patients with myocarditis, previous history of arrhythmias and peripheral vascular disease were associated independently with increased odds of mortality (Fig 1 ). Myocarditis with influenza had more cardiogenic shock (23.6% vs 14.4%, P < 0.05). Both groups had similar rates of respiratory failure, respiratory failure requiring ventilation, acute kidney injury requiring dialysis, and utilization of extracorporeal membrane oxygenation.
FIG 1.
A Comparison of outcomes and predictors of mortality in COVID-19 and influenza myocarditis. (Color version of figure is available online.)
In this large real-world population-based study, we report that COVID-19 myocarditis was associated with higher prevalence of cardiovascular and in-hospital mortality compared to influenza associated influenza myocarditis despite cardiogenic shock being more common in patients with myocarditis and influenza.
Although the exact pathophysiology of COVID-19 leading to myocarditis is unknown, the pathophysiology is likely similar to that of other viruses such as influenza. There are many similarities between COVID-19 and influenza infections such as viral transmission, risk factors for infection, and the range of symptoms.4 However, there are also clear differences. The intense cytokine storm that occurs during COVID-19 can result in myocardial inflammation without the presence of viral particle in myocardial biopsy while influenza myocarditis appears to be related mainly to direct viral invasion of myocytes.
In our study, the age and prevalence of cardiovascular comorbidities was higher in patients with myocarditis and COVID-19 compared to influenza. Prior reports have also confirmed a higher prevalence of cardiovascular diseases in patients with COVID-19 infection.5 Predictors of mortality were also different in both groups which can enable us to risk stratify patients who are at high risk.
Previous studies comparing influenza and COVID-19 have demonstrated higher mortality in patients with COVID-19.4 In our study, we also demonstrated that myocarditis associated with COVID-19 was also associated with significantly higher mortality compared to influenza. However, cardiogenic shock as a result of fulminant myocarditis which is the most severe form of myocarditis was more common in myocarditis patients with influenza. The higher rates of mortality in myocarditis with COVID-19 group despite lower risk of severe myocarditis could possibly be due to deaths from noncardiac etiologies such as bacterial coinfection and septic shock.
The NIS is an administrative database that utilizes ICD-10-CM codes and thus could be prone to misclassification errors. Further, laboratory and imaging data to confirm diagnosis was not available however our study draws strength from utilization of a national database with a large sample size overcoming the biases seen with single center studies. In summary, among hospitalizations with myocarditis, concomitant COVID-19 was associated with an increased risk of mortality but lower risk of cardiogenic shock when compared to influenza.
Footnotes
Dr Fonarow reports consulting for Abbott, Amgen, AstraZeneca, Bayer, Eli Lilly, Janssen, Medtronic, Merck, Novartis, and Pfizer. Remaining authors have nothing to disclose.
References
- 1.Pollack A, Kontorovich AR, Fuster V, Dec GW. Viral myocarditis: diagnosis, treatment options, and current controversies. Nat Rev Cardiol. 2015;12(11):670–680. doi: 10.1038/nrcardio.2015.108. [DOI] [PubMed] [Google Scholar]
- 2.Garot J, Amour J, Pezel T, et al. SARS-CoV-2 fulminant myocarditis. Case Rep. 2020;2(9):1342–1346. doi: 10.1016/j.jaccas.2020.05.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baral N, Adhikari P, Adhikari G, Karki S. Influenza myocarditis: a literature review. Cureus. 2020;12(12):e12007. doi: 10.7759/cureus.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khan MS, Shahid I, Anker SD, et al. Cardiovascular implications of COVID-19 versus influenza infection: a review. BMC Med. 2020;18(1):403. doi: 10.1186/s12916-020-01816-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Isath A, Malik AH, Goel A, Gupta R, Shrivastav R, Bandyopadhyay D. Nationwide analysis of the outcomes and mortality of hospitalized COVID-19 patients. Curr Probl Cardiol. 2022;48(2) doi: 10.1016/j.cpcardiol.2022.101440. [DOI] [PMC free article] [PubMed] [Google Scholar]