Abstract
Background:
Proximal femoral fractures (PrFF) are one of the most common causes of emergency admission in the elderly population. The majority of patients have pre-existing conditions that get worsened by unplanned surgery.
Objective:
Purpose of this article was to evaluate if a is single shot of dexamethasone with levobupivacaine administered intrathecally reduces postoperative pain and cognitive complications in patients with proximal femoral fractures.
Methods:
The study was performed at a level II trauma center which is a part of a teaching hospital with a catchment population of around 300,000 patients, the first author’s affiliation. Around 500 PrFF are performed yearly in the center. All participants gave oral and written informed consent before randomization.
Results:
In total, 60 patients with a PrFF, ASA status 2 or 3 were randomized into two groups for spinal anaesthesia as DLSA study group (received 8 mg of dexamethasone and 12.5 mg of 0.5 % levobupivacaine) or LSA control group (received 12.5 mg of 0,5 % levobupivacaine). Postoperative cognitive disturbance was evaluated using simplified Confusion Assessment Method (CAM) scale, pain intensity was measured using Visual Analogue Scale (VAS) and blood samples for defining cortisol concentrations were taken before and after the surgical procedure. The primary outcomes were effects of intrathecal dexamethasone on plasma cortisol affecting cognitive disturbances. Secondary outcomes included pain scores and length of hospital stay. The DLSA group demonstrated a reduced incidence of postoperative cognitive dysfunction (POCD), p=0.043, longer analgesia duration, p<0.001, decreased cortisol levels and shorter hospitalization p=0.045. Intrathecal dexamethasone was the only significant predictor of postoperative delirium, OR 7.76, p=0.019.
Conclusion:
Single shot intrathecal administration of dexamethasone with levobupivacaine used in anaesthesia for proximal femoral fractures reduces the stress response by decreasing plasma cortisol concentrations prolonging analgesia. Complications such as delirium and POCD occurred with significantly lower frequency allowing better postoperative rehabilitation and shortening the hospitalization.
Keywords: proximal femoral fracture, spinal anesthesia, dexamethasone, delirium
1. BACKGROUND
Proximal femoral fractures (PrFFs) are known for most painful stress injuries and in the elderly (1). This pain syndrome can change the cognitive functions, which can be reduced with prompt surgical treatment and punctual quality rehabilitation (2, 3). Postoperative cognitive dysfunction (POCD) is common after hip fracture and, unless systematic screening occurs, is likely to be underrecognized and have a difficult postoperative course (4). Achieving effective analgesia is particularly difficult because it is necessary to personalize the treatments and, at the same time, the ineffective analgesia may lead to serious complications such as patient’s fear and anxiety, lead to aggressive behavior and disturbance of cognition, and has an unfavorable effect on physiological parameters. Significantly higher cortisol levels can last up to eight weeks after injury in elderly patients (5). Hyperactivity of the hypothalamic-pituitary-adrenal (HPA) axis with higher cortisol levels is involved in the pathophysiology of delirium (6) similarly, association between higher plasma cortisol levels and POCD in aged patients following hip fracture surgery occurs (6, 7). Delirium refers to observable changes in consciousness and attention, whereas POCD may refer to a patient exhibiting significant declines from patient’s own baseline level of performance in one or more neuropsychological domains (8). Dexamethasone can inhibit cortisol secretion by inhibiting the hypothalamo-pituitary-adrenal axis primarily at the pituitary level by transcription mechanism in the cells, but not obligatory for adrenocorticotrophic hormone (ACTH) gene synthesis (9). It is comprehended that a harmful stimulus can suppress the HPA axis feedback information which is a possible function of nature and intensity of the stimulus (10). Spinal anesthesia avoids the risks of general anesthesia, and various additives such as epinephrine, phenylephrine, clonidine, opioids, etc. added to local anesthetics were associated with adverse effects (11-13). In a variety of clinical settings dexamethasone administered preoperatively improved postoperative analgesia and decreased opioid consumption and their associated adverse effects (14).
Our hypothesis was that administration of a single dose of intrathecal dexamethasone 0.1 mg/kg preoperatively enhances perioperative analgesia in elderly patients with a PrFF.
2. OBJECTIVE
The purpose of this article was to evaluate if a is single shot of dexamethasone with levobupivacaine administered intrathecally reduces postoperative pain and cognitive complications in patients with proximal femoral fractures.
3. PATIENTS AND METHODS
Patients
This study was approved by the local Ethics committee and registered at clinicaltrials.gov (NCT03856502). The study was performed at a level II trauma center which is a part of a teaching hospital with a catchment population of around 300,000 patients, the first author’s affiliation. Around 500 PrFF are performed yearly in the center. All participants gave oral and written informed consent before randomization. Emergency patients with PrFF receiving spinal anaesthesia for surgical treatment were screened for inclusion. Inclusion criteria were all cooperative patients with a proximal femoral fracture of one leg, aged 50>, with an American Society of Anesthesia (ASA) class<3. Patients were excluded if they had pre-existing cognitive impairment, diabetes mellitus, neurological conditions or tumors, neuroendocrine disorders or tumors, ASA≥4 and unwillingness to participate in the study. Patients were excluded if spinal anaesthesia failed, patients were unsuitable for spinal anaesthesia or if they received an additional peripheral block.
The study design was a randomized controlled trial with two parallel groups. The group assignment was determined by a computer generated algorithm (Randlist®, Datainf, Thübringen, Germany) A researcher who participated in data collection performed randomization in two groups (sizes1:1). Participants were randomized to receive spinal anaesthesia before surgery by either one shot levobupivacaine solution (LSA) or one shot levobupivacaine solution with additional low dose Dexamethasone (DLSA).
Patients read and signed the informed consent after the study has been clearly explained to them.
Proximal femoral fractures were treated either by a partial hip arthroplasty or by intramedullary nailing, depending on the localisation of the fracture. Subtrochanteric fractures were treated with additional cerclage wiring and using an extended length intramedullary nail.
Anesthetic procedure
All spinal anaesthesia were performed by the principal investigator (LŠ). Spinal anesthesia was performed in the sitting position medially or paramedially in the middle lumbar segments (L2-3 or L3-4) via an BD Spinal Needle Quincke Type Point 22-27 G. The skin was anesthetized using lidocaine 10 mg/ml with adrenaline.
One study group (DLSA) received 8 mg of dexamethasone (Dexamethasone Sodium Phosphate, KRKA) and 12,5 mg of 0,5 % levobupivacaine (Chirochaine, Abbott). The control group of thirty patients received 12,5 mg of 0,5 % levobupivacaine intrathecally, the LSA group. Block onset, duration of analgesia as well as duration of surgical procedure was calculated in minutes (min), and was measured from the application, throughout the surgical procedure and in the postoperative recovery.
Motor block was assessed using a modified Bromage scale (0 = able to lift whole extended leg or standing up, 1 = flexion of the knee, 2 = flexion of the ankle, 3 = no flexion of the knee or ankle). If there was a difference in motor block between the legs, the leg with the most intense block was reported.
Plasma cortisol was measured at five time-points: T1- before anesthesia and infusion administration, T2- one hour after surgery, T3- third postoperative day at 6 am, T4- fifth postoperative day at 6 am and T5- on tenth postoperative day at 6 am. Plasma cortisol was assayed by Roche Elecsys Immunoassay System in laboratory reference points (185-624) nmol/L using 0.5 mL of patients’ blood.
Postoperative cognitive impairment was evaluated using simplified Confusion Assessment Method (CAM)score scale (15) in four measure points: T1- one hour after surgery, T2- third postoperative day at 9 am, T3- fifth postoperative day at 9 am and T4- on tenth postoperative day at 9 am to follow cortisol measurements as well. It is a clinical instrument for delirium assessment used by non- psychiatric medical staff. Delirium is described in terms of 4 diagnostic criteria; 1) acute onset or fluctuating course, 2) inattention, 3) disorganized thinking, and 4) altered level of consciousness (alert, lethargic, stupor or coma) and is defined as present when 1 plus 2 or either 3 or 4 is positive. CAM scale criteria was used to exclude delirium. Preoperative cognitive evaluation was based on anesthesiologist guided conversations with the patient and information given by the patient’s closest relative or guardian. Memory and speech were assessed by object naming and verbal fluency by having patients recall the items in any order and name in 60 seconds as many words as possible that began with a specific letter. Higher scores represented greater verbal fluency and better memory. Attention was measured by response time on a dual task having patients naming presented items while using distractors at the same time (16).
Participants were assessed for postoperative pain using a Visual Analogue Scale (VAS) ranging from 0 to 10, including worst pain experienced during rehabilitation. If the participant was asleep at the time of pain query, the pain score was assigned “0”.
Visual Analogue Scale (VAS), was used for evaluating overage pain intensity every three hours when patients were awake in five measure points: T1- before anesthesia and infusion administration, T2- one hour after surgery, T3- third postoperative day, T4- fifth postoperative day and T5- on tenth postoperative day to follow cortisol measurements. Hospitalization was calculated by the number of days preoperatively from the day of admission to the day of surgical treatment and postoperatively from the day of surgical reconstruction to the day of hospital discharge in the time period of up to 30 days.
Weight bearing was allowed as tolerated from postoperative day one. Heparin was administered for thromboprophylaxis.
Outcome measures
The predefined, primary end point of the study were plasma cortisol concentration and incidence of cognitive disturbances. Secondary outcomes included duration of analgesia, postoperative pain intensity at first hour postop, as well as the third, fifth and tenth days after surgery and length of hospital stay. Data was interpreted by investigators blinded to the treatment received (DT,AK).
Ethical statement
The research approved by Ethical Committee of the University hospital “Sveti Duh”, Zagreb, Croatia, reference number 3612, October 30th 2012 and the Croatian School of Medicine University of Zagreb, number: 380-591-0106-13-244212.
Statistical analysis
Normality distribution was tested using the Kolmogorov-Smirnov test. Categorical variables were shown by using absolute frequencies and ratios, quantitative variables were expressed as median [interquartile range] for non-normally distributed variables and mean (±standard deviation) for normally distributed variables. The data for descriptive variables were analyzed by chi-square test, whereas differences in quantitative variables were tested by Mann-Whitney U test. Particular clinical parameters were evaluated by Spearman’s correlation analysis. Multivariate relationship of particular clinical variables related to the group with cognitive impairment was performed using binary logistic regression analysis. With an α = 0.05 and a power = 0.8 we estimated that a total of 60 participants were required and that 30 patients per study group were needed to detect the difference between two groups for the predefined plasma cortisol levels. P<0.05 was considered to be statistically significant. Statistical analysis was performed by the IBM SPSS Statistics v23 (IBM, Armonk, NY, US).
Data availability
Please provide a Data Availability statement under this subsection. Certain data types must be deposited in an appropriate public structured data, and the accession number(s) provided in the manuscript. At publication, full access is required. If full data access is required for peer review, authors must make it available.
4. RESULTS
Sixty patients with PrFF were included in this randomized, prospective, clinical trial. All screened patients could be included (Figure 1).
Figure 1. Flow of patients during study(Color figure can be viewed at Willeyonlinelibrary.com.
Average age was 80.65 (±8.5) years. Preoperatively, there were no significant differences in age, ASA classification, fracture type and preoperative hospital stay duration between the groups (Table 1).
Table 1. Demographic data and outcome measures.
| Variable | Group | P | ||||
|---|---|---|---|---|---|---|
| DLSA | LSA | |||||
| Age, years (mean±SD) | 81.63 (±6.94) | 79.69 (±10.17) | 0.370 | |||
| Gender n, % | Female | 19 | 63,30% | 26 | 86,70% | 0.037 |
| Male | 11 | 36,70% | 4 | 13,30% | ||
| ASA status n, % | 2 | 22 | 73,30% | 19 | 63,30% | 0.405 |
| 3 | 8 | 26,70% | 11 | 36,70% | ||
| Fracture type | Extracapsular | 23 | 76,70% | 16 | 53,30% | 0.058 |
| Intracapsular | 7 | 23,30% | 14 | 46,70% | ||
| Cognitive alterations | None | 21 | 70,00% | 12 | 40,00% | 0.0195 |
| POCD | 8 | 26,67% | 13 | 43,33% | ||
| Delirium | 1 | 3,33% | 5 | 16,67% | ||
| Preoperative hospital stay (hours) | <=48 h | 11 | 36,70% | 5 | 16,70% | 0.08 |
| >48 h | 19 | 63,30% | 25 | 83,30% | ||
| Hospitalisation days (mean±SD) | 15.9 (6.0) | 17.4 (4.0) | 0.045 | |||
Primary outcome measureablehe overall incidence of cognitive alterations, POCD and delirium, was significantly lower in the DLSA group (p=0.0195) (Table 1). Majority of patients were operated on after the 48h mark, without a significant difference between the groups (Table 1). There were no differences in cortisol levels between the two groups at any timepoint (Table 2 and Figure 2). Intrathecal dexamethasone was the only significant predictor of postoperative delirium, OR 7.76 (p=0.019) (Table 3).
Table 2. Plasma cortison values.
| Timeline | Mean (±SD) nMol/L |
p | |
|---|---|---|---|
| Preoperative | DLSA | 731.23 (±170.33) | 0,511 |
| LSA | 757.00 (±216.06) | ||
| 1h postop | DLSA | 410.13 (±190.25) | 0,088 |
| LSA | 479.37 (±166.30) | ||
| 3 days postop | DLSA | 522.63 (±140.29) | 0,865 |
| LSA | 524.80 (±138.28) | ||
| 5 days postop | DLSA | 493.87 (±122.42) | 0,796 |
| LSA | 526.10 (±281.01) | ||
| 10 days postop | DLSA | 433.03 (±115.13) | 0,745 |
| LSA | 433.10 (±159.11) | ||
Figure 2. Graphical analysis of the differences between the groups in plasma cortisol fluctuations. DLSA the study group that received dexamethasone and levobupivacaine in spinal anaesthesia, LSA the control group that received levobupivacaine in spinal anaesthesia.
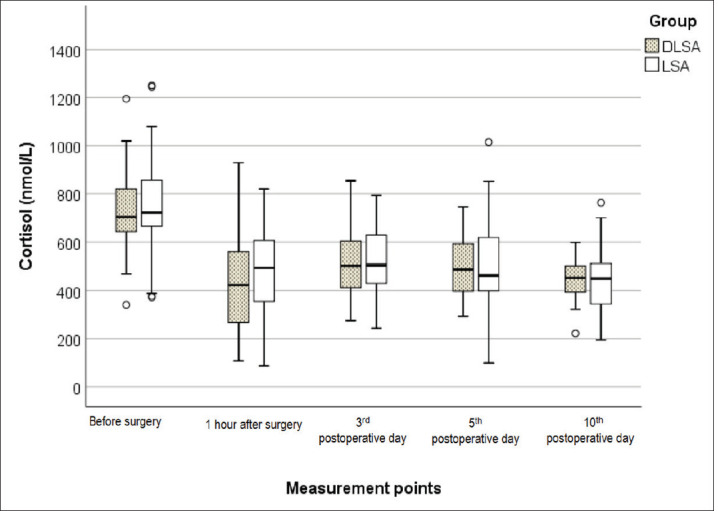
Table 3. Intrathecal dexamethasone as a predictor of postoperative cognitive function.
| Prediction of cognitive disorder | OR | 95% CI | P | |
|---|---|---|---|---|
| lower | upper | |||
| Extracapsular proximal femoral fracture/ Intracapsular proximal femoral fracture | 2,84 | 0,42 | 19,13 | 0,283 |
| LSA / DLSA | 7,67 | 1,39 | 42,36 | 0,019 |
| VAS preoperatively | 2,04 | 0,86 | 4,83 | 0,104 |
| Cortisol preoperatively | 1,00 | 0,99 | 1,00 | 0,365 |
| Age (years) | 1,12 | 1,00 | 1,25 | 0,051 |
| Female / male | 1,20 | 0,16 | 8,77 | 0,860 |
Secondary outcome measure
Analgesia lasted longer in the DLSA group, 540 mins [264] than in the LSA group 330 [122] (p<0.001). From the third postoperative day onwards, pain levels were significantly lower in the DLSA group (Table 4). DLSA patients had a lower mean number of hospitalization days (Table 1).
Table 4. Comparison of pain levels using the Visual-Analog-Scale (VAS) between the groups.
| Timeline | Median[IQR] | p | |
|---|---|---|---|
| Preoperative | DLSA | 8.5 [1.0] | 0.374 |
| LSA | 8.0 [2.0] | ||
| 1h postop | DLSA | 0.0 [0.0] | 0.061 |
| LSA | 0.0 [0.0] | ||
| 3 days postop | DLSA | 1.5 [1.0] | <0.001 |
| LSA | 3.0 [2.0] | ||
| 5 days postop | DLSA | 1.0 [2.0] | <0.001 |
| LSA | 3.0 [1.0] | ||
| 10 days postop | DLSA | 0.0 [1.0] | 0.002 |
| LSA | 1.0 [1.0] | ||
5. DISCUSSION
This study demonstrates that single low dose of dexamethasone with levobupivacaine administered intrathecally received for surgical reconstruction of proximal femoral fractures reduces decreases plasma cortisol levels, provides longer lasting analgesic effect, lowers the incidence of cognitive complications and shortens hospitalization.
Pain sensation varies in this type of fractures and time of surgical reconstructions depending on intensity, quality and duration of pain stimuli involving nociception, inflammation and nerve cells remodeling (11, 16). According to the demographic study findings, proximal femoral fractures are more usual in older female population with significant neuroendocrine stress response to tissue damage, perioperative pain and psychological stress. Although dexamethasone has been used intrathecally for many years, it has not been evaluated when it was given in conjunction with levobupivacaine intrathecally. Single shot effect of intrathecally administered dexamethasone with levobupivacaine affecting postoperative pain, consciousness and outcome in emergency patients with femoral fractures have not yet been evaluated in recent literature. Intrathecal addition of dexamethasone to bupivacaine for elective orthopedic surgery on lower limbs has been shown to significantly prolong duration of sensory block and to decrease opioid requirements in postoperative management (17).
Glucocorticoids are part of induction to anesthesia in different clinical protocols achieving much improved analgesia and minimized inflammation with reduced opioid requirements and less adverse events after surgery (11, 14, 18, 19). Why dexamethasone prolongs regional analgesia is a subject of debate. Dexamethasone relieves pain by reducing inflammation and blocking transmission of nociceptive C-fibers and by suppressing ectopic neural discharge (20) and also that dexamethasone increases the activity of inhibitory potassium channels on nociceptive C fibres, decreasing their activity (21).
Our study findings suggest higher pain intensity and increased cortisol concentrations, occuring on the third postoperative day were directly in correlation with more complex degrees of cognitive impairment in the LSA group, not in the DLSA group. The difference in VAS scores and different in-hospital stay might signify reduced perioperative stress effect when dexamethasone was added intrathecally with enhancement of treatment outcome. Szucs et al. (22) demonstrated significant improvement in postoperative pain with intravenously administered dexamethasone.
Nikkel et al. (23) demonstrated average time to surgery was 1.8 days for PrFF and a longer time to surgery was associated with longer hospital stay. The percentage of patients with most comorbid conditions increased with increasing length of stay. A shorter hospital stay (<5 days and <10 days) was also associated with decreased 30 day mortality.
Although guidelines recommend the surgery to be performed within 24hrs of admission (24), and studies demonstrate a clear benefit of early surgery (25), and no downside of after-hours surgery (26) in the present study hospitalization lasted shorter in the group that received dexamethasone, but was overall long with 73,33% of patients waiting for surgical treatment more than 48h from admission because of preoperative preparation.
Limitation of the study
This study has some limitations. No long-term follow-up has been performed, however, outcome measures were short-term outcomes during in-hospital stay. The in-hospital time to surgery is long compared to the literature and the guidelines. The same study in a setting where these times are shorter might affect the results, especially due to the role of cortisone in a stress reaction such as a hip fracture. Both intramedullary nailing and arthroplasty have been included in the study. Given the complications are similar (27), we do not expect there would be a difference in results if controlled for this particular variable.
6. CONCLUSION
Single shot intrathecal administration of dexamethasone with levobupivacaine used in anesthesia for proximal femoral fractures reduces the stress response by decreasing plasma cortisol concentrations prolonging analgesia. Complications such as delirium and POCD occurred with significantly lower frequency allowing better postoperative rehabilitation and shortening the hospitalization.
Author’s contribution:
All authors were involved in all steps of preparation this article. Final proofreading was made by the first author.
Conflict of interest:
None declared.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Aubrun F. Management of postoperative analgesia in elderly patients. Reg Anesth Pain Med. 2005;30:363–379. doi: 10.1016/j.rapm.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 2.Association of Anaesthetists of Great Britain and Ireland. Griffiths R, Alper J, et al. Management of proximal femoral fractures 2011: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia. 2012;67:85–98. doi: 10.1111/j.1365-2044.2011.06957.x. [DOI] [PubMed] [Google Scholar]
- 3.Simunovic N, Devereaux PJ, Sprague S, et al. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ. 2010;182(1609):1616. doi: 10.1503/cmaj.092220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gottschalk A, Hubbs J, Vikani AR, et al. The Impact of Incident Postoperative Delirium on Survival of Elderly Patients After Surgery for Hip Fracture Repair. Anesth Analg. 2015;121:1336–1343. doi: 10.1213/ANE.0000000000000576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frayn KN, Stoner HB, Barton RN, et al. Persistence of high plasma glucose, insulin and cortisol concentrations in elderly patients with proximal femoral fractures. Age Ageing. 1983;12:70–76. doi: 10.1093/ageing/12.1.70. [DOI] [PubMed] [Google Scholar]
- 6.Roberts NA, Barton RN, Horan MA, White A. Adrenal function after upper femoral fracture in elderly people: persistence of stimulation and the roles of adrenocorticotrophic hormone and immobility. Age Ageing. 1990;19:304–310. doi: 10.1093/ageing/19.5.304. [DOI] [PubMed] [Google Scholar]
- 7.Bisschop PH, de Rooij SE, Zwinderman AH, et al. Cortisol, insulin, and glucose and the risk of delirium in older adults with hip fracture. J Am Geriatr Soc. 2011;59:1692–1696. doi: 10.1111/j.1532-5415.2011.03575.x. [DOI] [PubMed] [Google Scholar]
- 8.Ji M-H, Yuan H-M, Zhang G-F, et al. Changes in plasma and cerebrospinal fluid biomarkers in aged patients with early postoperative cognitive dysfunction following total hip-replacement surgery. J Anesth. 2013;27:236–242. doi: 10.1007/s00540-012-1506-3. [DOI] [PubMed] [Google Scholar]
- 9.Berger M, Nadler J, Browndyke J, et al. Postoperative Cognitive Dysfunction: Minding the Gaps in our Knowledge of A Common Postoperative Complication in the Elderly. Anesthesiol Clin. 2015;33:517–550. doi: 10.1016/j.anclin.2015.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Rijen EA, Harvey RA, Barton RN, et al. Sensitivity of mononuclear leucocytes to glucocorticoids in elderly hip-fracture patients resistant to suppression of plasma cortisol by dexamethasone. Eur J Endocrinol. 1998;138:659–666. doi: 10.1530/eje.0.1380659. [DOI] [PubMed] [Google Scholar]
- 11.Žura M, Kozmar A, Šakić K, et al. Effect of spinal and general anesthesia on serum concentration of pro-inflammatory and anti-inflammatory cytokines. Immunobiology. 2012;217:622–627. doi: 10.1016/j.imbio.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 12.Khaled GM, Sabry AI. Outcomes of intrathecal analgesia in multiparous women undergoing normal vaginal delivery: A randomised controlled trial. Indian J Anaesth. 2020;64:109–117. doi: 10.4103/ija.IJA_572_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moeen SM, Moeen AM. Intrathecal dexamethasone vs. meperidine for prevention of shivering during transurethral prostatectomy: a randomized controlled trial. Acta Anaesthesiol Scand. 2017;61:749–757. doi: 10.1111/aas.12920. [DOI] [PubMed] [Google Scholar]
- 14.Kardash KJ, Sarrazin F, Tessler MJ, Velly AM. Single-dose dexamethasone reduces dynamic pain after total hip arthroplasty. Anesth Analg. 2008;106:1253–1257. doi: 10.1213/ANE.0b013e318164f319. table of contents. [DOI] [PubMed] [Google Scholar]
- 15.Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 16.Rundshagen I. Postoperative cognitive dysfunction. Dtsch Arztebl Int. 2014;111:119–125. doi: 10.3238/arztebl.2014.0119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bani-hashem N, Hassan-nasab B, Pour EA, et al. Addition of intrathecal Dexamethasone to Bupivacaine for spinal anesthesia in orthopedic surgery. Saudi J Anaesth. 2011;5:382–386. doi: 10.4103/1658-354X.87267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beloosesky Y, Hendel D, Weiss A, et al. Cytokines and C-reactive protein production in hip-fracture-operated elderly patients. J Gerontol A Biol Sci Med Sci. 2007;62:420–426. doi: 10.1093/gerona/62.4.420. [DOI] [PubMed] [Google Scholar]
- 19.Movafegh A, Razazian M, Hajimaohamadi F, Meysamie A . Dexamethasone added to lidocaine prolongs axillary brachial plexus blockade. Anesth Analg. 2006;102:263–267. doi: 10.1213/01.ane.0000189055.06729.0a. [DOI] [PubMed] [Google Scholar]
- 20.Golwala MP, Swadia VN, Dhimar A, Sridhar NV. Pain relief by dexamethasone as an adjuvant to local anesthetics in supraclavicular brachial plexus block. Journal of Anaesthesiology Clinical Pharmacology. 2009;25:285–288. [Google Scholar]
- 21.Cummings KC, Napierkowski DE, Parra-Sanchez I, et al. Effect of dexamethasone on the duration of interscalene nerve blocks with ropivacaine or bupivacaine. Br J Anaesth. 2011;107:446–453. doi: 10.1093/bja/aer159. [DOI] [PubMed] [Google Scholar]
- 22.Szucs S, Jessop D, Iohom G, Shorten GD. Postoperative analgesic effect, of preoperatively administered dexamethasone, after operative fixation of fractured neck of femur: randomised, double blinded controlled study. BMC Anesthesiol . 2016;16:79. doi: 10.1186/s12871-016-0247-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nikkel LE, Kates SL, Schreck M, et al. Length of hospital stay after hip fracture and risk of early mortality after discharge in New York state: retrospective cohort study. BMJ. 2015;351:h6246. doi: 10.1136/bmj.h6246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Recommendations | Hip fracture: management | Guidance | NICE.
- 25.Farrow L, Ablett AD, Sargeant HW, et al. Does early surgery improve outcomes for periprosthetic fractures of the hip and knee? A systematic review and meta-analysis. Arch Orthop Trauma Surg. 2021;141:1393–1400. doi: 10.1007/s00402-020-03739-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yeo QY, Kwek EBK. After hours surgery for elderly hip fracture patients: How safe is it? Arch Orthop Trauma Surg. 2021;141:1183–1187. doi: 10.1007/s00402-020-03585-2. [DOI] [PubMed] [Google Scholar]
- 27.Arshi A, Su L, Lee C, et al. Comparison of complication profiles for femoral neck, intertrochanteric, and subtrochanteric geriatric hip fractures. Arch Orthop Trauma Surg. 2021 doi: 10.1007/s00402-021-03978-x. [DOI] [PubMed] [Google Scholar]