Abstract
Introduction
Fear of childbirth (FOC) is a common obstetrical challenge that affects the health of women. The epidemiology of FOC has not been studied in Finland for the last decade. The aim of this study was to analyze the epidemiology and risk factors for FOC and to evaluate the association between FOC and the rate of elective cesarean section (CS) as an intended mode of delivery.
Material and methods
Data from the National Medical Birth Register were used to evaluate the epidemiology of FOC and to determine the main risk factors for FOC in Finland between 2004 and 2018. Nulliparous and multiparous women were analyzed separately. Logistic regression model was used to determine the main risk factors for FOC. Multivariable logistic regression model was used to assess the intended mode of delivery in those pregnancies with diagnosed maternal FOC. Adjusted odds ratios (aOR) with 95% confidence intervals (CIs) were calculated.
Results
A total of 1 million pregnancies were included. The annual rate of pregnancies with maternal FOC increased from 1.5% (CI: 1.4–1.6) in 2004 to 9.1% (CI: 8.7–9.3) in 2018 for all women. For nulliparous women, the rate increased from 1.1% (CI: 1.0–1.3) in 2004 to 7.1% (CI: 6.7–7.5) in 2018, and from 1.8% (CI: 1.7–2.0) in 2004 to 10.3% (10.0–10.7) in 2018 for multiparous women. The strongest risk factors for maternal FOC were higher maternal age and gestational diabetes. For multiparous women, the strongest risk factors were gestational diabetes and previous CS. The total odds for elective CS were notably higher among women with FOC (aOR 8.63, CI: 8.39–8.88).
Conclusions
The incidence of maternal FOC rose six‐fold during our study period. However, the numbers of elective CS among women with this diagnosis, which had earlier risen in parallel, leveled off in 2014.
Keywords: cesarean section, delivery, fear of childbirth
The rates of diagnosed maternal fear of birth increased radically during year 2004–2018. Moreover, even though the numbers and rates of women with fear of birth diagnoses increased, the rates for elective cesarean section among women with fear of birth diagnosis decreased strongly during the study period.
Abbreviations
- CS
cesarean section
- FOC
fear of childbirth
- MBR
Medical Birth Register
Key message.
The rates of diagnosed maternal fear of childbirth increased radically during year 2004–2018 but the rates for elective cesarean section among women with fear of childbirth diagnosis decreased.
1. INTRODUCTION
Fear of childbirth (FOC) is a common obstetrical challenge affecting the health of women. 1 Higher socioeconomic status, advanced maternal age, and depression as well as previous operative deliveries (vacuum or emergency cesarean delivery) are all predictive factors for FOC. 2 , 3 The most recent study of the incidence of FOC in Finland was published in 2014. According to the findings of that study, the prevalence of FOC increased between 1997 and 2010 from 1.1% to 3.6% in nulliparous women, and from 1.5% to 7.8% in multiparous women. 3 High rates of FOC have also been reported in other Nordic countries. According to the results of a study in Sweden, the prevalence of intense FOC and very intense FOC was 15.8% and 5.7%, respectively. 4 In a study made in Norway, 12% of women reported FOC. 5 Truly high prevalence has also been reported in other countries. For example, according to a cross‐sectional study conducted in Ireland in 2019, the prevalence of severe FOC was 5.3% and the prevalence of high FOC was 36.7%. 6
Cesarean section (CS) can be a lifesaving operation for both women and children and in such situations is medically justified. However, CS is also associated with certain negative outcomes, such as altered immune development of the child or increased risk of uterine rupture. 7 Therefore, the choice of performing CS instead of vaginal delivery should be carefully evaluated. FOC is a common reason for CS and is associated with increased requests for CS 4 , 8 , 9 Interestingly, in recent decades, fear of childbirth has been associated with a major increase in CS rates, mainly elective CS, but also emergency CS. 10 , 11
Based on the hypothesis that the rate of pregnancies with FOC diagnosis has increased and FOC has increased the odds for elective CS, the aim of this study was to calculate the prevalence rates of pregnancies with diagnosed maternal FOC and to evaluate the effects of FOC on the intended mode of delivery. In addition, we aimed to assess the epidemiological trends in the rates of elective CS among women with FOC over the last decades.
2. MATERIAL AND METHODS
In this nationwide retrospective register‐based cohort study, data from the National Medical Birth Register (MBR) were used to evaluate the trends in the epidemiology of FOC and to evaluate the odds for elective CS among women with diagnosed FOC compared to a non‐FOC group. The MBR is maintained by the Finnish Institute for Health and Welfare (THL). The study period was from January 1, 2004, to December 31, 2018.
The MBR contains data on pregnancies, delivery statistics, and the perinatal outcomes of all births with a birthweight of ≥500 g or a gestational age of ≥22+0 weeks. The MBR has high coverage and quality (the current coverage is nearly 100%). 12 , 13 In Finland, all woman are asked about any fears they may have about giving birth during their visits to the antenatal clinic. Those women who experience a significant FOC and who cannot be helped during the antenatal visits to the women and child welfare clinics and/or have requested CS due to FOC are referred to a secondar/tertiary maternity clinic. If FOC is diagnosed, it is dealt with by a physician or specialized midwife during a maternity care visit. In the present study, FOC was defined according to the International Classification of Diseases 10th revision code (ICD‐10) code O99.80 established in 1997. At the beginning of our study period, some diagnoses were registered using the ICD‐10 code O99.8, which are also possible (incorrectly coded) diagnoses for FOC because the registering of FOC in the MBR only started in 2004. These diagnoses are included, and the numbers are shown separately in this study. The diagnoses for FOC were collected from the MBR.
All singleton pregnancies with delivery mode identified in the MBR were included in this study. Pregnancies with unknown mode of delivery (n = 5, none of which with diagnosed maternal FOC) and non‐singleton pregnancies (n = 12 132) were excluded from the analysis. A total of 833 122 pregnancies met the inclusion criteria. The process used to form the study groups is shown as a flowchart in Figure 1.
FIGURE 1.
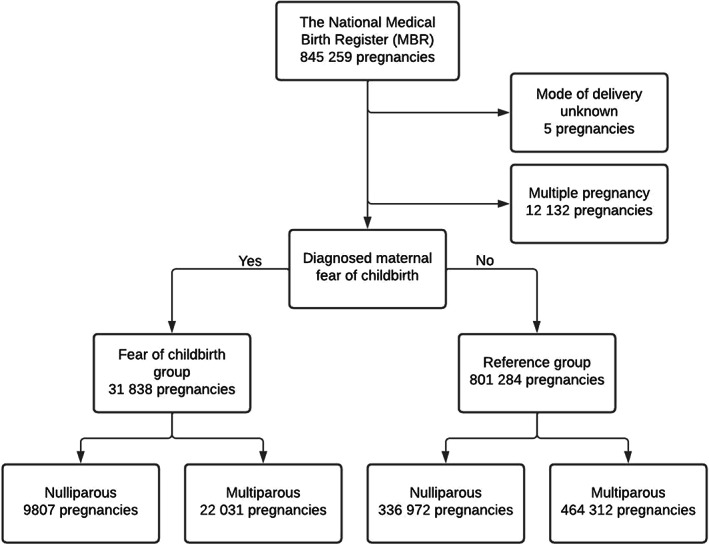
Flowchart depicting the process used to divide the study population into groups.
2.1. Statistical analyses
Continuous variables were interpreted as means with standard deviations or as a median with an interquartile range (IQR) based on the distribution of the data. The categorical variables are presented as absolute numbers and percentages with 95% confidence intervals (CIs). The CIs for rates and percentages were calculated using Poisson regression. The annual absolute numbers and rates for the diagnosed maternal FOC were calculated. The annual rate is presented as percentages with 95% CIs and calculated for both nulliparous and multiparous women. Among women with diagnosed FOC, the annual absolute numbers and percentages of intended mode of delivery (elective CS/trial of labor) were calculated separately for nulliparous and multiparous women. The univariable logistic regression model was used to determine the main risk factors for FOC. Exposure variable was the potential risk factor, and the outcome was the diagnosed maternal FOC. Odds ratios (ORs) with 95% CIs between the groups were compared. The multivariable logistic regression model was used to assess the intended mode of delivery. Women with diagnosed FOC were compared to a control group consisting of all singleton pregnancies without FOC diagnosis. The exposure variable was FOC. The outcome was the intended mode of delivery (elective CS/trial of labor). Adjusted odds ratios (aORs) with 95% CIs between the groups were compared. Adjusted odds ratios were also calculated separately for nulliparous and multiparous women. The model was adjusted by previously recognized potential confounders: maternal age, previous cesarean section, weight of the neonate, 14 , 15 , 16 and year of the pregnancy. The results of this study are reported according to the STROBE guidelines. 17 Statistical analyses were performed using R version 4.0.3 for Windows (R Foundation for Statistical Computing).
2.2. Ethics statement
Both the National Medical Birth Register (MBR) and the Care Register for Healthcare had the same unique pseudonymized identification number for each patient. The pseudonymization was made by the Finnish data authority Findata, and the authors did not have access to the pseudonymization key, as it is maintained by Findata. In accordance with Finnish legislation, no informed written consent was required because of the retrospective register‐based study design and because the patients were not contacted. Permission for the use of this data was granted by FINDATA after evaluation of the study protocol (no. THL/1756/14.02.00/2020) August 1, 2020.
3. RESULTS
A total of 31 838 (3.8%) pregnancies were diagnosed with maternal FOC. Of these, a total of 9807 (30.8%) women were nulliparous and 22 031 (69.2%) women were multiparous. The non‐FOC group comprised 801 284 women. Of these, 336 972 (42.1%) women were nulliparous, and 464 312 (57.9%) women were multiparous. The annual absolute number of pregnancies with diagnosed FOC increased strongly during the years 2004–2018, increasing from 855 (with 167 coded as O99.8) in 2004 to 4184 (with 1 coded as O99.8) in 2018. (Figure S1) The annual rate of pregnancies with diagnosed maternal FOC increased from 1.5% (CI: 1.4–1.6) in 2004 to 9.1% (CI: 8.7–9.3) in 2018 for all women. For nulliparous women, the rate increased from 1.1% (CI: 1.0–1.3) in 2004 to 7.1% (CI: 6.7–7.5) in 2018, and for multiparous women from 1.8% (CI: 1.7–2.0) in 2004 to 10.3% (10.0–10.7) in 2018. (Figure 2).
FIGURE 2.
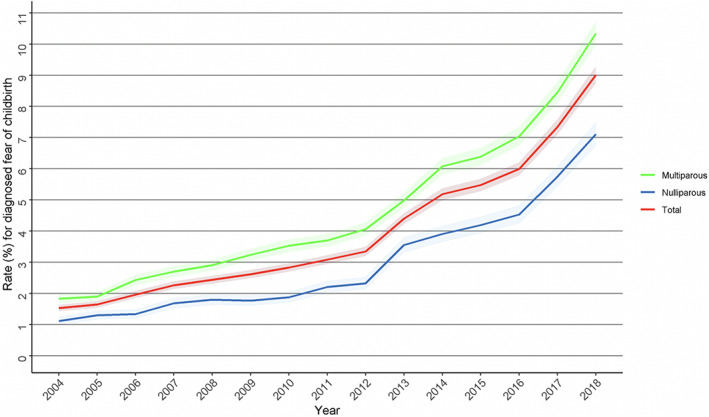
The annual rate (%) with 95% confidence interval (CI) for pregnancies with fear of childbirth in Finland during the years 2004–2018. The total rate and the rate for nulliparous and multiparous women were calculated.
Women with FOC were older at the time of pregnancy when compared to the non‐FOC group (mean 31.1 years vs 29.7 years). A higher rate of women with gestational diabetes was observed in the FOC group (16.7%, CI: 16.2–17.1 vs 12.7%, CI: 12.6–12.8) (Table 1).
TABLE 1.
Background information on the study groups.
| FOC group | Non‐FOC group | |||
|---|---|---|---|---|
| Total number of pregnancies | 31 838 | 801 824 | ||
| n | % (CI) | n | % (CI) | |
| Age (mean; SD) | 31.1 (5.4) | 29.7 (5.4) | ||
| Smoking status smoker | 4763 | 15.0 (15.0–14.5) | 116 725 | 14.6 (14.5–14.6) |
| Maternal BMI (mean; SD) | 24.8 (5.1) | 24.4 (4.8) | ||
| Maternal gestational diabetes | 5303 | 16.7 (16.2–17.1) | 101 626 | 12.7 (12.6–12.8) |
| Neonatal weight, grams (mean; SD) | 3553 (473) | 3522 (546) | ||
| Induction of labor | 6915 | 22.0 (21.2–22.2) | 163 513 | 20.4 (20.3–20.5) |
| Length of pregnancy (weeks + days) (mean; sd) | 39 + 4 (9) | 39 + 6 (13) | ||
| Preterm (<37 gestational weeks) | 802 | 2.5 (2.3–2.7) | 36 920 | 4.6 (4.6–4.7) |
Note: Pregnancies with diagnosed maternal fear of childbirth (FOC) were compared to the ones without FOC diagnosis.
Abbreviations: FOC, fear of childbirth; SD, standard deviation.
For nulliparous women, the strongest associated factors for maternal FOC were higher maternal age (OR 1.05 per year upwards, CI: 1.05–1.06) and gestational diabetes (OR 1.38, CI: 1.30–1.46). For multiparous women, the strongest risk factors were higher maternal age (OR 1.03 per year upwards, CI: 1.03–1.03), gestational diabetes (OR 1.34, CI: 1.29–1.39), and previous CS (OR 3.96, CI: 3.85–4.07). (Table 2).
TABLE 2.
Crude odds ratios (ORs) with 95% confidence intervals (CIs) for the event of diagnosed maternal fear of childbirth.
| OR (CI) | |
|---|---|
| Nulliparous women | |
| Higher maternal age (per year) | 1.05 (1.05–1.06) |
| Overweight (BMI >25.0 kg/m2) | 1.07 (1.03–1.12) |
| Obesity (BMI >30.0 kg/m2) | 1.14 (1.07–1.21) |
| Maternal smoking | 1.20 (1.14–1.26) |
| Gestational diabetes | 1.38 (1.30–1.46) |
| Multiparous women | |
| Higher maternal age (per year) | 1.03 (1.03–1.03) |
| Overweight (BMI >25.0 kg/m2) | 1.11 (1.09–1.15) |
| Obesity (BMI >30.0 kg/m2) | 1.18 (1.14–1.23) |
| Maternal smoking | 1.01 (0.97–1.05) |
| Gestational diabetes | 1.34 (1.29–1.39) |
| Previous cesarean section | 3.96 (3.85–4.07) |
Note: Women with different potential risk factors were compared to those without.
Abbreviation: BMI, body mass index.
A notably higher rate for elective CS was observed among women diagnosed with FOC when compared to the non‐FOC group (36.2%, CI: 35.5–36.8 vs 5.2%, CI: 5.2–5.2). Furthermore, there was also a lower rate of spontaneous vaginal deliveries in the FOC group (70.4%, CI: 69.3–71.6 vs 80.2%, CI: 80.0–80.4) and a higher rate of unplanned CS (18.6%, CI: 18.1–19.2 vs 8.8%, CI: 8.8–8.9). When only nulliparous pregnancies are considered, women had a higher rate of elective CS when compared to the non‐FOC group (35.0%, CI: 33.9–36.2 vs 4.6%, CI: 4.5–4.7). Multiparous women also had a higher rate of elective CS when compared to the non‐FOC group (36.7%, CI: 35.9–37.5 vs 5.6%, CI: 5.5–5.7). (Table 3).
TABLE 3.
Intended mode of delivery and mode of delivery.
| FOC group | Non‐FOC group | |||
|---|---|---|---|---|
| Total number of pregnancies | 31 838 | 801 824 | ||
| n | % (CI) | n | % (CI) | |
| Intended mode of delivery | ||||
| Elective CS | 11 512 | 36.2 (35.5–36.8) | 41 486 | 5.2 (5.1–5.2) |
| Trial of labor | 20 326 | 63.8 (63.0–64.7) | 760 338 | 94.8 (94.6–95.0) |
| Mode of delivery a | ||||
| Spontaneous vaginal | 14 310 | 70.4 (69.3–71.6) | 609 885 | 80.2 (80.0–80.4) |
| Vacuum | 1966 | 9.7 (9.2–10.1) | 69 239 | 9.1 (9.0–9.2) |
| Breech | 52 | 0.3 (0.3–0.3) | 5124 | 0.7 (0.7–0.7) |
| Forceps | 5 | <0.1 (<0.1 to <0.1) | 264 | <0.1 (<0.1 to <0.1) |
| Unplanned CS | 3788 | 18.6 (18.1–19.2) | 67 265 | 8.8 (8.8–8.9) |
| Emergency CS | 205 | 1.0 (0.9–1.2) | 8561 | 1.1 (1.1–1.1) |
| Nulliparous pregnancies | 9807 | 336 972 | ||
| Intended mode of delivery | ||||
| Elective CS | 3434 | 35.0 (33.9–36.2) | 15 507 | 4.6 (4.5–4.7) |
| Trial of labor | 6373 | 65.0 (63.4–66.6) | 321 465 | 95.4 (95.1–95.7) |
| Multiparous pregnancies | 22 031 | 464 312 | ||
| Previous CS | 9975 | 45.3 (44.4–46.2) | 80 613 | 17.4 (17.2–17.5) |
| Intended mode of delivery | ||||
| Elective CS | 8078 | 36.7 (35.6–37.5) | 25 955 | 5.6 (5.5–5.7) |
| Trial of labor | 13 953 | 63.3 (62.3–64.4) | 438 357 | 94.4 (94.1–94.7) |
Note: Pregnancies with diagnosed maternal fear of childbirth (FOC) were compared to the ones without FOC diagnosis.
Abbreviations: CS, cesarean section; FOC, fear of childbirth.
Rates from attempted vaginal deliveries (elective CSs are excluded).
Among women with diagnosed FOC, the rate of elective CS as an intended mode of delivery decreased strongly during our study period from 42% in 2004 to 27% in 2018. (Figure 3) In addition, the rate of unplanned CS (including urgent and emergency CS) among women with diagnosed FOC also decreased during the study period from 18.1% in 2004 to 14.6% in 2018. (Figure S2) The total odds for elective CS were notably higher among women with FOC when compared to the non‐FOC group (aOR 8.63, CI: 8.39–8.88). The odds for elective CS were also higher among nulliparous women (aOR 11.55, CI: 11.03–12.10) and multiparous women (aOR 7.49, CI: 7.22–7.77) (Table 4).
FIGURE 3.
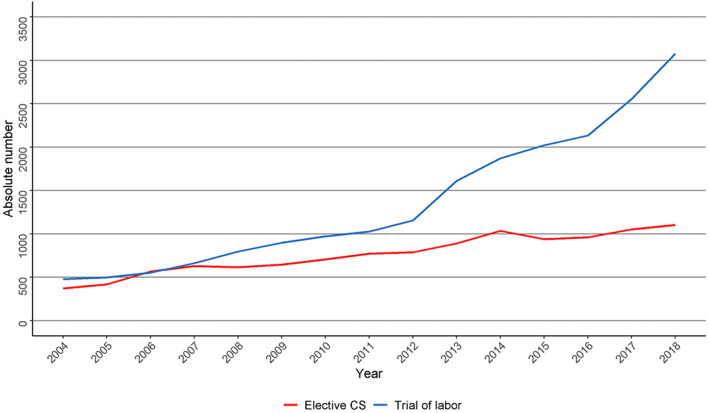
The annual absolute numbers of intended mode of delivery (trial of labor/elective cesarean section [CS]) among women with diagnosed fear of childbirth during the years 2004–2018.
TABLE 4.
Adjusted odds ratios (aOR) with 95% confidence intervals (CIs) for the event of turning mode of delivery into elective cesarean section (CS).
| Risk of CS | ||
|---|---|---|
| aOR a | CI | |
| Total women with FOC | 8.63 | (8.39–8.88) |
| Nulliparous women with FOC | 11.55 | (11.03–12.10) |
| Multiparous women with FOC | 7.49 | (7.22–7.77) |
Note: Pregnancies with diagnosed maternal fear of childbirth were compared to the ones without FOC diagnosis.
Abbreviation: FOC, fear of childbirth.
Adjusted by year of the pregnancy, maternal age, previous cesarean section, and weight of the neonate.
4. DISCUSSION
The main finding of this study was that the rates of diagnosed maternal FOC increased radically during the 14‐year study period. Moreover, even though the numbers and rates of women with FOC diagnoses increased, the rates for elective CS among women with FOC diagnosis decreased strongly during the study period.
The most recent study to examine the epidemiology of FOC diagnoses in Finland covered the years 1997–2010. 3 In that study, the epidemiology of FOC showed an increasing trend, rising from 1.1% to 3.6% in nulliparous women and from 1.5% to 7.8% in multiparous women, which is in line with our results. 3 However, the results of the present study add to the existing literature by revealing a radically increasing trend during the first decades of the present century, with the rate increasing to 7.1% for nulliparous women and 10.3% for multiparous women. However, according to the previous literature, despite the increasing trend in the epidemiology of FOC in Finland, the rate is still low when compared to other countries. According to a cross‐sectional study in Ireland in 2019, the prevalence of severe FOC was 5.3% and high FOC was 36.7%. 6 According to a systematic review of 12 countries in 2018, the prevalence of FOC varied between 6.3% and 14.8% in different countries, with the highest being in Estonia (14%). According to the latest Finnish study, the strongest risk factors for FOC in nulliparous women were advanced maternal age and high or unspecified socioeconomic status. In multiparous women, the strongest risk factors for FOC were depression, previous CS, and high or unspecified socioeconomic status. 3 However, based on our data, the reasons behind FOC remain unknown. The overall health of women giving birth has changed during the last decade. For example, women are older and the incidence of gestational diabetes and obesity has increased. 18 , 19 , 20 These changes can also be associated with the increased rate of FOC. According to the previous literature, other risk factors such challenging or complicated previous deliveries and maternal depression are not available in our data. 2 , 3 According to previous studies, maternal depression has lately had an increasing incidence. 21 The temporal changes in the rates of FOC may be partly explained by the increased incidence of mild FOC, and by the increased amount of registering the FOC diagnosis in the MBR due to an increasing awareness of FOC among physicians. Furthermore, other possible factors, such as a decrease in the quality of antenatal parent training and support or changes in societal attitudes towards vaginal birth, may have increased the fear of childbirth. However, due to the crude nature of our data, these factors are just speculations and further research should be performed to investigate the incidence of the different reasons behind FOC.
The odds for elective CS were notably higher among women with diagnosed FOC. The CS rate for multiparous women with FOC may be associated with a higher rate of previous CS than in the control group. As the indication of CS is not recorded in the MBR, it remains unknown how many of the previous CSs were performed due to FOC. However, despite the increasing number of FOC diagnoses, the rate for elective CS decreased strongly during our study period among women with FOC diagnosis. Although the reason for this decrease remains unclear, there is a variety of possible explanations. One explanation is most likely the rapidly increasing absolute number of FOC diagnoses. Also, deliveries that are supposed to be elective CS may have been registered as unplanned CS if the labor started precipitately. However, as the rate for unplanned CS also showed a decreasing trend, the higher rate of mild FOC might be the main explanation because a higher rate of women with FOC ended up choosing trial of labor. In addition, vaginal delivery may have become an option for more women due to improvements in the treatment of FOC. As the awareness of this progressive obstetrical challenge has increased, resources for the treatment of FOC have also increased. Although a Finnish study of 371 women with fear of childbirth reported no significant effect of psychoeducation on the overall frequency of CS, it did report a 33% increase in spontaneous vaginal births. 22 The increasing incidence of mild FOC could also explain this as these patients might be more easily encouraged to try vaginal delivery.
The strengths of our study are the large nationwide register data used and the long study period which allowed us to analyze the rates of FOC using a large study population. The register data used in our study are routinely collected in structured forms using national instructions, which ensures good coverage (over 99%) and reduces possible reporting and selection biases.
The main limitation of this study is that the indications behind elective CS delivery are not registered in the MBR, which means that indications for these delivery methods remain unknown. Moreover, as there is no uniform criteria or definitions for FOC, the severity of FOC is also unknown. Generally, FOC is defined as anxiety and fear of pregnancy, childbirth, or the parenting of a child that impairs daily wellbeing. FOC takes different forms in different women and may manifest as physical complaints, nightmares, and difficulties to concentrate. 23
5. CONCLUSION
The incidence of maternal FOC has shown a strongly increasing trend during our 14‐year study period. The incidence rose six‐fold during the study period. However the numbers of elective CS among women with this diagnosis, which had earlier risen in parallel, leveled off in 2014.
AUTHOR CONTRIBUTIONS
MV and RL wrote the initial manuscript. IK and MV undertook the study design. Ville MM and MK supervised the study. VP, IK, and VM. MM helped planning appropriate statistical analysis. MK provided clinical expertise. Each author commented on the manuscript during the process and confirmed the final version to be submitted.
CONFLICT OF INTEREST
None.
Supporting information
Figure S1
Figure S2
Vaajala M, Liukkonen R, Kuitunen I, Ponkilainen V, Mattila VM, Kekki M. Trends in the epidemiology of fear of childbirth and association with intended mode of delivery: A nationwide register‐based cohort study in Finland. Acta Obstet Gynecol Scand. 2023;102:430‐437. doi: 10.1111/aogs.14521
REFERENCES
- 1. Nilsson C, Hessman E, Sjöblom H, et al. Definitions, measurements and prevalence of fear of childbirth: a systematic review. BMC Pregnancy Childbirth. 2018;18:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kemppainen V, Niinimäki M, Bloigu A, et al. Fear of childbirth after medical vs surgical abortion. Population‐based register study from Finland. Acta Obstet Gynecol Scand. 2021;100:743‐750. [DOI] [PubMed] [Google Scholar]
- 3. Räisänen S, Lehto SM, Nielsen HS, Gissler M, Kramer MR, Heinonen S. Fear of childbirth in nulliparous and multiparous women: a population‐based analysis of all singleton births in Finland in 1997‐2010. BJOG. 2014;121:965‐970. [DOI] [PubMed] [Google Scholar]
- 4. Nieminen K, Stephansson O, Ryding EL. Women's fear of childbirth and preference for cesarean section—a cross‐sectional study at various stages of pregnancy in Sweden. Acta Obstet Gynecol Scand. 2009;88:807‐813. [DOI] [PubMed] [Google Scholar]
- 5. Henriksen L, Borgen A, Risløkken J, Lukasse M. Fear of birth: prevalence, counselling and method of birth at five obstetrical units in Norway. Women Birth J Aust Coll Midwives. 2020;33:97‐104. [DOI] [PubMed] [Google Scholar]
- 6. O'Connell MA, Leahy‐Warren P, Kenny LC, O'Neill SM, Khashan AS. The prevalence and risk factors of fear of childbirth among pregnant women: a cross‐sectional study in Ireland. Acta Obstet Gynecol Scand. 2019;98:1014‐1023. [DOI] [PubMed] [Google Scholar]
- 7. Sandall J, Tribe RM, Avery L, et al. Short‐term and long‐term effects of caesarean section on the health of women and children. Lancet. 2018;392:1349‐1357. [DOI] [PubMed] [Google Scholar]
- 8. Ryding EL, Lukasse M, Parys ASV, et al. Fear of childbirth and risk of cesarean delivery: a cohort study in six European countries. Birth. 2015;42:48‐55. [DOI] [PubMed] [Google Scholar]
- 9. Waldenström U, Hildingsson I, Ryding E. Antenatal fear of childbirth and its association with subsequent caesarean section and experience of childbirth. BJOG. 2006;113:638‐646. [DOI] [PubMed] [Google Scholar]
- 10. Ryding EL, Wijma B, Wijma K, Rydhström H. Fear of childbirth during pregnancy may increase the risk of emergency cesarean section. Acta Obstet Gynecol Scand. 1998;77:542‐547. [PubMed] [Google Scholar]
- 11. Saisto T, Salmela‐Aro K, Nurmi JE, Könönen T, Halmesmäki E. A randomized controlled trial of intervention in fear of childbirth. Obstet Gynecol. 2001;98:820‐826. [DOI] [PubMed] [Google Scholar]
- 12. Gissler M, Shelley J. Quality of data on subsequent events in a routine medical birth register. Med Inform Internet Med. 2002;27:33‐38. [DOI] [PubMed] [Google Scholar]
- 13. Gissler M, Teperi J, Hemminki E, Meriläinen J. Data quality after restructuring a national medical registry. Scand J Soc Med. 1995;23:75‐80. [DOI] [PubMed] [Google Scholar]
- 14. Lydon‐Rochelle MT, Gardella C, Cárdenas V, Easterling TR. Repeat cesarean delivery: what indications are recorded in the medical chart? Birth Berkeley Calif. 2006;33:4‐11. [DOI] [PubMed] [Google Scholar]
- 15. Jenabi E, Khazaei S, Bashirian S, Aghababaei S, Matinnia N. Reasons for elective cesarean section on maternal request: a systematic review. J Matern‐Fetal Neonatal Med. 2020;33:3867‐3872. [DOI] [PubMed] [Google Scholar]
- 16. Herstad L, Klungsøyr K, Skjærven R, et al. Maternal age and elective cesarean section in a low‐risk population. Acta Obstet Gynecol Scand. 2012;91:816‐823. [DOI] [PubMed] [Google Scholar]
- 17. Von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344‐349. [DOI] [PubMed] [Google Scholar]
- 18. THL . Perinatal statistics ‐ parturients, delivers and newborns ‐ THL. 2018. https://thl.fi/en/web/thlfi‐en/statistics‐and‐data/data‐and‐services/register‐descriptions/newborns
- 19. Kuitunen I, Vähä‐Tuisku S, Huttunen T. Gestational diabetes mellitus and labor analgesia: nationwide register‐based analysis in Finland. Acta Diabetol. 2022;59:1515‐1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kuitunen I, Huttunen TT, Ponkilainen VT, Kekki M. Incidence of obese parturients and the outcomes of their pregnancies: a nationwide register study in Finland. Eur J Obstet Gynecol Reprod Biol. 2022;274:62‐67. [DOI] [PubMed] [Google Scholar]
- 21. Gelaye B, Rondon MB, Araya R, Williams MA. Epidemiology of maternal depression, risk factors, and child outcomes in low‐income and middle‐income countries. Lancet Psychiatry. 2016;3:973‐982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rouhe H, Salmela‐Aro K, Toivanen R, Tokola M, Halmesmäki E, Saisto T. Obstetric outcome after intervention for severe fear of childbirth in nulliparous women—randomised trial. BJOG. 2013;120:75‐84. [DOI] [PubMed] [Google Scholar]
- 23. Saisto T, Halmesmäki E. Fear of childbirth: a neglected dilemma. Acta Obstet Gynecol Scand. 2003;82:201‐208. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1
Figure S2


