Abstract
There are a number of inconsistencies in the description of the bends of the colon down to the anus. This is historically based on the fact that anatomists saw the colon in its position in the abdominal cavity down to the pelvis and thus from the “outside” and also described it in this way. This view is still useful in clinical practice today (e.g. for the abdominal surgeons). For the greater part of clinicians, however, the view has shifted due to modern endoscopy. This allows examiners to see the terminal section of the intestine and the colon from the “inside”. To accommodate both “ways of looking” in terms of modern medicine, we have been guided by today's clinical needs, and here we attempt to reconcile these with the historically evolved anatomical terms to create a nomenclature that meets all the needs of students, anatomists and clinicians looking at the large intestine from the inside and outside. With this in mind, we propose to speak of colic flexures (right colic flexure = RCF = hepatic flexure, flexura coli sinistra; left colic flexure = LCF = splenic flexure, flexura coli dextra; descending‐sigmoid flexure = DSF; sigmoid‐rectum flexure = SRF) for the colon (colon). For the rectum (rectum), we suggest the term bend (superior, intermediate and inferior) when viewed in the frontal plane, the term curvature (sacral curvature; anorectal curvature = perineal curvature) when viewed in the sagittal plane.
Keywords: colon flexions, colon flexures, large intestine, large intestine anatomy
The large intestine flexures, bends and curvatures. Are we ready for changes….? Bends and curvatures introduced to colon terminology.
1. INTRODUCTION
The large intestine (English) (Latin intestinum crassum) consists of the caecum (caecum) with the appendix (appendix vermiformis), colon (colon) and rectum (rectum). It is suspended on the mesentery (mesenterium) in the abdominal cavity. There are flexures (flexurae) between its parts, the most important are the right (hepatic, RCF) (flexura coli dextra, hepatica) and left (splenic, LCF) (flexura coli sinistra, splenica) colic flexures (Agur & Dalley, 2005; Alazmani et al., 2016; Bourgouin et al., 2012; Coffey et al., 2014, Coffey & O'Leary, 2016; Culligan et al., 2013; Eickhof et al., 2010; FIPAT, 2019; Malas et al., 2004; Moore & Dalley 1999; Paulsen & Waschke, 2011; Standring, 2020; Wozniak et al., 2019). The LCF usually lies more cranial and dorsal than the RCL and forms a more acute angle. The term flexure is used for any bend, flexion or even curvature, regardless of the angle (smaller, 90° or more) at which the adjacent parts unite. The flexure is composed of mesocolic and intestinal components. At each mesenteric flexure, the intestinal segments change from being adjacent to retroperitoneum into being mobile. Peritoneal folds arising from the abdominal (or pelvic) peritoneum merge with the lateral aspects of the right and left colon as well as both sides of the rectum, and are important anatomical features (Coffey et al., 2014; Tirkes et al., 2012). The bend range is a key factor in some medical procedures, among them—colonoscopy, the most commonly performed, important endoscopic examination. The next, less frequently performed examinations in the large intestine, are sigmoidoscopy and rectoscopy. Bends, especially those that are firmly attached to the abdominal wall and bend at a sharp angle, can be problematic when performing these procedures. They play as well a key role in capsule endoscopy and virtual colonography.
Anatomists use the designations according to the Terminologia Anatomica 1998. (FCAT, 1998) and some specialists use the version published online in 2019 by the Federative International Programme for Anatomical Terminology (FIPAT, 2019). Moreover, some specialists often have their own specific designations. The latest internet version has not been accepted by all anatomists yet, and some national anatomical societies decided not to recognise the latest version—among others Dutch, Spanish and German Anatomical Societies. In some countries, like Poland or United Kingdom and Ireland, the decision about acceptance of the FIPAT (FIPAT, 2019) terminology, has not been made yet.
FIPAT updated the anatomical designations used in anatomy. There is a need to use a uniform terminology acceptable for both anatomists and clinicians, for example, this is particularly important for a univocal and exact localization of polyps in the medical records. Thus, the names used to describe the colon need to be accurate for gastroenterologists, surgeons, radiologists, proctologists and medical students. Anatomy teaching should prepare medical students for future challenges in clinical work (Chmielewski, 2020). For this reason, terminology must be simple, logical and descriptive. One of the basic anatomical problems is the use of the term flexure, which deserves further clarification. We pointed at the large intestine flexures problem to be widely discussed by specialists.
The aim of this present work is to present a suggestion for terminology improvement of the large intestine bends and simplify the terminology in the light of its clinical applications.
2. TERMINOLOGY CURRENTLY IN USE
2.1. Colon, colon
According to the FIPAT terminology (Table 1), there are two flexures in the colon—RCF and LCF. A similar description is found in widely used anatomical textbooks and atlases. However, no attention so far has been paid to the transition of the descending colon (colon descendens) into the sigmoid colon (colon sigmoideum) and the sigmoid colon into the rectum.
TABLE 1.
The anatomical names for colon flexures. New Terminologica Anatomica (FIPAT, 2019)
| No. | Latin term | Latin synonym | UK English | US English | English synonym |
|---|---|---|---|---|---|
| 2983 | Flexura dextra coli | Flexura hepatica coli | Right colic flexure | Right colic flexure | Hepatic flexure |
| 2985 | Flexura sinistra coli | Flexura splenica coli | Left colic flexure | Left colic flexure | Splenic flexure; lienalis flexure |
Note: FIPAT.library.dal.ca
2.2. Rectum, rectum
According to the FIPAT terminology (Table 2), there are five flexures in the rectum, three can be seen in the frontal plane—lateral superior (flexura superodextra lateralis recti), intermediate (flexura intermediosinistra lateralis recti) and inferior (flexura inferodextra lateralis recti) and two in the sagittal plane (flexura sacralis) and anorectal (flexura perinealis).
TABLE 2.
The anatomical names for rectum and anal canal flexures. New Terminologica Anatomica (FIPAT, 2019)
| No. | Latin term | Latin synonym | UK English | US English | English synonym |
|---|---|---|---|---|---|
| 2999 | Flexura sacralis recti | N/A | Sacral flexure of rectum | Sacral flexure of rectum | N/A |
| 3000 | Flexurae laterales recti | N/A | Lateral flexures of rectum | Lateral flexures of rectum | N/A |
| 3001 | Flexura lateralis superior recti | Flexura superodextra lateralis recti | Superior lateral flexure of rectum | Superior lateral flexure of rectum | Superodextral lateral flexure of rectum |
| 3002 | Flexura lateralis intermedia recti | Flexura intermediosinistra lateralis recti | Intermediate lateral flexure of rectum | Intermediate lateral flexure of rectum | Intermediosinistral lateral flexure of rectum |
| 3003 | Flexura lateralis inferior recti | Flexura inferodextra lateralis recti | Inferior lateral flexure of rectum | Inferior lateral flexure of rectum | Inferodextral lateral flexure of rectum |
| 3010 | Flexura anorectalis | Flexura perinealis; Flexura perinealis recti | Anorectal flexure | Anorectal flexure | Perineal flexure |
Note: FIPAT.library.dal.ca
Abbreviation: N/A, not applicable.
3. DISCUSSION AND PROPOSAL FOR SIMPLIFICATION
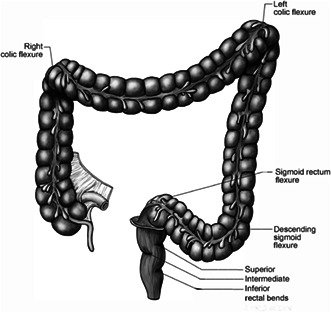
Intestinal morphology is important for both endoscopic and radiological diagnostic procedures and conservative and surgical treatment (Bunni 2022; Kapadia 2017; Utano et al., 2021). There are at least three modern and very popular diagnostic tools – colonoscopy, capsule endoscopy and computed tomography colonography (so‐called virtual colonoscopy). The colon tortuosity plays the main role in conducting these procedures (Figure 1a,b).
FIGURE 1.
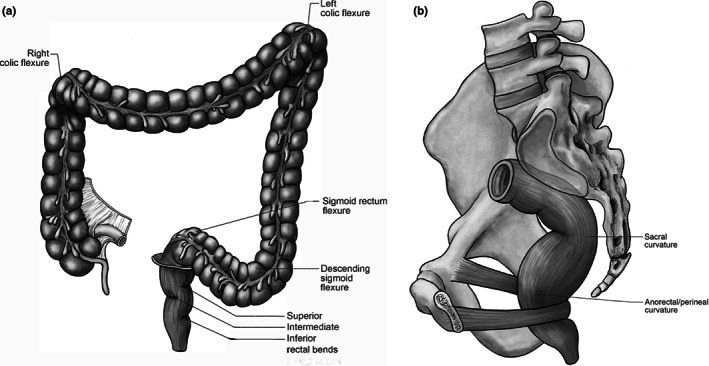
The large intestine – the caecum, colon and rectum with flexures, bends and curvatures. According to FIPAT and our suggestions. (a) Frontal view of the large intestine. (b) Sagittal view of the rectum in pelvis
There are serious terminological inconsistencies between different specialists when describing the colon. The main discrepancies involve the flexures, the term rectosigmoid (some clinicians use the name; Koppen et al., 2017), and the rectum range (differences between surgeons and anatomists).
Precision in using colon terminology to describe pathological findings can be disclosed when performing examinations and is important for several reasons. The lack of precision can lead to misunderstandings. One of the most important sources of misunderstanding could be the description of findings during colonoscopy (Hanson et al., 2007). The specific location of polyps detected during the examination needs to be documented very accurately. Some of the changes are flat (without mucosal elevation) and may be difficult to be located again during a follow‐up colonoscopy, when for example the recheck is conducted after 3–10 years. The time of recheck is established according to histopathological evaluation of mucosa specimens. Moreover, in case of surgical treatment following the endoscopy (e.g. if the specimens taken during endoscopy revealed advanced dysplasia), the flat polyps cannot be palpated from the outer walls, and the intestinal segment which must be removed is difficult to find. In such a case, accurate polyp localisation (stated by a metric scale during endoscopic examination) is a key factor in successful treatment.
The same applies to tumours or diverticula detected during this examination. For instance, the exact description is necessary for planning radiotherapy for tumours. Finally, in planning surgical treatment of a patient, the extent of lymph node resection and neighbouring peri‐intestinal tissue removal is of great importance. Therefore, it is necessary to have a simple, understandable and easy terminology, which is codified and universally accepted.
Unlike for the colic flexures, there is no anatomical term similar to RCF and LCF for the transition of the descending colon into the sigmoid colon. Anatomically, the sigmoid colon with its sigmoid mesocolon (mesocolon sigmoideum) crosses the left gonadal vessels, the left obturator nerve, the left ureter and the left external and internal iliac blood vessels. All these structures are not visible to the examiner during colonoscopy, and, therefore, cannot be used as landmarks for example to define exact location of polyps. For this reason, a description corresponding to RCF/LCR is desirable. In our previous work, we proposed the name descending‐sigmoid colon flexure (DSF). We proposed this name, but eminent specialists prefer the name colosigmoid flexure (flexura colosigmoidea) as sufficiently enough for our purposes.
The flexure was described as acute bend (angle not greater than 90°) in about one‐third of the subjects, and not greater than 120° in two‐thirds (Wozniak et al., 2022). Other authors used the name colosigmoid junction (Shafik et al., 2009). Thus, we found the necessity to emphasise this anatomical landmark DSF, because of its importance in colonoscopy. A great number of incomplete colonoscopies are stopped here (Hanson et al., 2007), mostly due to the tortuosity of the sigmoid colon (Khashab et al., 2009). One of the reason for incompleteness is the fixed, acute bending between the sigmoid colon and rectum.
There is no clear anatomical definition for the transition between the sigmoid colon and the rectum. Some authors use the term rectosigmoid to describe this region. D'Souza et al. suggested that this problem needs to be sorted out (D'Souza et al., 2019).
D'Souza et al. (2019) found that 11 different definitions were used for the transition between the rectum and the sigmoid colon. By most authors, the rectum was identified as the intestinal segment extending 15 cm from the anus (anus) (D'Souza et al., 2019, 2020), so the large intestine segment starting 15 cm from the anus can be named as the sigmoid colon. Some authors prefer to use 19 cm as the measure of the rectum because they stated that the distance from the anal verge to the anterior peritoneal reflection is approximately this length in both sexes (Memon et al., 2009).
Others question the variability for this line (Wasserman et al., 2016). We propose to use the term sigmoid‐rectum flexure (SRF) (flexura sigmoideorectalis) instead of rectosigmoid crossing (Massalou et al., 2018). The introduction of this name is logical and understandable for specialists and medical students. The fact that sigmoid‐rectum goes in a proximo‐distal direction rather than rectosigmoid (which is the opposite) is more logical and easier to remember other than be consistent with other intestinal junctions such as duodeno‐jejunal (flexura duodenojejunalis) and ileocecal (ostium ileale). This is a clear and simple term for this junction, and we would prefer to use the term sigmoid‐rectum and not to support the use of the term rectosigmoid (Koppen et al., 2017). The transition of the rectum into the sigmoid colon is visible to the examiner with the naked eye during rectoscopy/colonoscopy and helps in localization of the colonoscope tip in the large intestine. The border between the rectum and sigmoid colon based on its length can be precisely measured only by endoscopy or imaging methods and is not applicable to surgery. Thus, the borderline based on the anatomical definition (crossing of linea terminalis) or clinical definition on the anterior peritoneum reflexion or sacral vertebra is still very useful and remains its value.
The last section to be discussed, improved and sorted out is the rectum and its curves. Rectum is composed of the ampulla and anal canal. Whereas the beginning of the rectum is at the linea terminalis, the clinical landmark used to locate the beginning of the rectum is at the level of the second or third sacral vertebra. It lies in the pelvic cavity and has a length of approximately 12–15 cm. After passing through the pelvic floor along the sacrum, the rectum becomes the anal canal (canalis analis), which form its length of 3–4 cm and ends at the anus. The anal canal is shorter in women than in men (Regadas et al., 2007). The anorectal junction (junctio anorectalis) projects to the tip of the coccyx, and gets past it. We suggest to rename the anorectal junction and call it recto‐anal junction to keep it consistent with the proximal‐distal order. In the sagittal plane, the rectum has two bends: (1) the dorsally convex sacral flexure (flexura sacralis) and the ventrally convex perineal flexure (flexura perinealis). The latter is the result of the traction by the puborectalis muscle as a part of the levator ani muscle. Below the perineal flexure the anal canal begins. According to the classical terminology, there are three lateral flexures in the rectum: superior (flexura superodextra lateralis or flexura lateralis superior recti), intermediate (flexura lateralis intermedia recti) and inferior (flexura lateralis inferior recti) (Figure 1), which are visible on imaging methods and palpable during digital rectal examination (per rectum). These parts are very easy to pass when performing the large intestine endoscopy. The name flexure suggests some problems when performing colonoscopy, thus we propose the change due to its endoscopic unimportance. In this region, no colonoscopy incompleteness is observed.
However, from an anatomical point of view these flexures are usually difficult for the anatomist to recognise during dissection. Only the intermediate fold is usually palpable 6–7 cm above the anocutaneal line (plica transversa recti media = Kohlrausch Fold). Below this fold, the rectum is dilated to form the rectal ampulla (ampulla recti). The anorectal junction forms the transition area to the anal canal, which can be recognised by the change of the transverse folds of the rectum to the longitudinal anal columns of the anal canal. These features are seen from internal aspects only. Anal canal anatomically and clinically is different, so in our manuscript, we follow the clinical description according to our priority for this work. However, we find no reason to use the term flexures for these rectal wall protrusions. The terms flexures are not very useful in rectal clinical matters—they are in fact not used in colonoscopy or rectoscopy or surgery. The terms lateral rectal flexures are used only in anatomy books. For this reason and from an endoscopic point of view we propose to use the terms bends (flexus) (superior, intermediate and inferior bends, respectively) instead of flexures. We hope this change will sort that problem out. We have a similar terminological problem when matching the rectal course in the sagittal plane to the sacrum and coccyx. Textbooks and atlases of anatomy use the terms sacral flexure and perineal flexure (flexura anorectalis) (Agur & Dalley, 2005; Moore & Dalley 1999; Paulsen & Waschke, 2011; Standring 2020). The sacral flexure is longer and more blunt than perineal. Therefore, we propose the term curvatures (sacral curvature and perineal curvature) to describe the large intestine shape readjusting on the surface of these bones. The anorectal flexure is more acute than sacral, so the introducing and changing this name should be considered with the greatest attention. These large intestine segments are very easy to pass during endoscopic examinations, and, with this in mind we do propose this change.
We hope these simplifications will bring an improvement and resolve these terminology issues. The large intestine morphology is variable in clinical work, not as easy as in anatomical books. For example, when performing the colon examinations in patients, additional loops are found routinely.
The supernumerary intestinal segments are usually found in the sigmoid and/or transverse colon (Eickhof et al., 2010; Khashab et al., 2009; Wozniak et al., 2019). The adjacent colon segments in the loops are joined with bends which could be described as acute or sharp (the angle between the two colic segments does not exceed 90°). Experts also use the term flexures for these bends (Eickhof et al., 2010). We support using these terms. The flexure acuity (sharpness less or more than 90°) is clinically important, for example when performing colonoscopy. We suggest that the term intracolic flexures for these important landmarks are the best.
Here, we would like to recommend that the newly introduced or simplified terms should be used in anatomical books describing large intestine to newly admitted medical students. Becoming acquainted with the terminology should help them to enter the clinical field, because understanding the issues around the bends in the large intestine is important for them. For example, the knowledge can be used during mobilizations of the flexures during surgery, both on the left and right sides (Kennedy et al., 2008; Petropoulou & Amin 2019). The flexures between the descending colon and sigmoid colon (Wozniak et al., 2022) and sigmoid colon and rectum (Massalou et al., 2018) are also of clinical importance, when understanding the reasons described above.
When the Basel Nomina Anatomica were published in 1895, one of the most important rules was to “use only one name for one structure” (Chmielewski 2020). On the other hand, anatomical terminology should be consistent with the clinical view of described structures. We should follow the progress in the clinical procedures.
We hope that these clarifications and suggestions will be a useful complement to the current nomenclature in anatomical textbooks and atlases, as well as for publications in the field of the colon.
The above discussion should represent a first step for starting a discussion on the use of a more simplified terminology aimed at matching anatomical and clinical needs. However, before officially introducing the terminology, this has to be codified in Terminologia Anatomica, discussed and agreed by relevant clinical societies, such as endoscopic and radiological societies, incorporated into their Guidelines and published in clinical journals to avoid confusion when teaching students.
For the purpose of introducing the corresponding Latin names, we suggest that this will be done by the FIPAT committee with the advice of a specialist in Latin language. The terms for which we would suggest this, have been marked by an asterisk.
4. CONCLUSIONS
In summary, we suggest to refer to large intestine flexures and bends as follows:
1. Colon—use the term flexures:
right colic flexure (RCF) = hepatic flexure
left colic flexure (LCF) = splenic flexure
descending‐sigmoid flexure (DSF)*
sigmoid‐rectum flexure (SRF)*
Use the term intracolic flexures—to describe acute (the angle between two consecutive colonic segments does not exceed 90°) flexures.
2. Rectum—frontal plane; use the term bends*:
superior rectal bend*
intermediate rectal bend*
inferior rectal bend*
(instead of superior lateral, intermediate lateral and inferior lateral rectal flexures).
3. Rectum—sagittal plane; use the term curvatures*:
sacral curvature*
anorectal curvature = perineal curvature*
(instead of sacral and anorectal or perineal flexures)
AUTHOR CONTRIBUTIONS
All authors contributed equally to this work.
CONFLICT OF INTEREST
No conflict of interest declared.
ACKNOWLEDGEMENTS
A special thank goes to Jörg Pekarsky from the Institute of Anatomy in Erlangen, for the excellent anatomical drawings.
Wozniak, S. , Quondamatteo, F. & Paulsen, F. (2023) “Flexures and bends of the large intestine: Current terminology and a suggestion to simplify it”. Journal of Anatomy, 242, 695–700. Available from: 10.1111/joa.13800
DATA AVAILABILITY STATEMENT
Data available on request from the authors.
REFERENCES
- Agur, A.M. & Dalley, A.F. (2005) Grant's atlas of anatomy, 11th edition. Baltimore, MD: Lippincott Williams & Wilkins. [Google Scholar]
- Alazmani, A. , Hood, A. , Jayne, D. , Neville, A. & Culmer, P. (2016) Quantitative assessment of colorectal morphology: implications for robotic colonoscopy. Medical Engineering & Physics, 38, 148–154. [DOI] [PubMed] [Google Scholar]
- Bourgouin, S. , Bège, T. , Lalonde, N. , Mancini, J. , Masson, C. , Chaumoitre, K. et al. (2012) Three‐dimensional determination of variability in colon anatomy: applications for numerical modeling of the intestine. Journal of Surgical Research, 178, 172–180. [DOI] [PubMed] [Google Scholar]
- Bunni, J. (2022) Anatomy of the mesentery. Clinics in Colon and Rectal Surgery, 35, 277–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chmielewski, P.P. (2020) New terminologia anatomica highlights the importance of clinical anatomy. Folia Morphologica (Warszawa), 79, 15–20. [DOI] [PubMed] [Google Scholar]
- Coffey, J.C. & O'Leary, D.P. (2016) The mesentery: structure, function, and role in disease. Lancet Gastroenterology and Hepatology, 1, 238–247. [DOI] [PubMed] [Google Scholar]
- Coffey, J.C. , Sehgal, R. , Culligan, K. , Dunne, C. , McGrath, D. , Lawes, N. et al. (2014) Terminology and nomenclature in colonic surgery: universal application of a rule‐based approach derived from updates on mesenteric anatomy. Techniques in Coloproctology, 18, 789–794. [DOI] [PubMed] [Google Scholar]
- Culligan, K. , Remzi, F.H. , Soop, M. & Coffey, J.C. (2013) Review of nomenclature in colonic surgery—proposal of a standardised nomenclature based on mesocolic anatomy. The Surgeon, 11, 1–5. [DOI] [PubMed] [Google Scholar]
- D'Souza, N. , Babberich, M.P.M. , d'Hoore, A. , Tiret, E. , Xynos, E. , Beets‐Tan, R.G.H. et al. (2019) Definition of the rectum: an international, expert‐based Delphi consensus. Annals of Surgery, 270, 955–959. [DOI] [PubMed] [Google Scholar]
- D'Souza, N. , Lord, A.C. , Shaw, A. , Patel, A. , Balyasnikova, S. , Tudyka, V. et al. (2020) Ex vivo specimen MRI and pathology confirm a rectosigmoid mesenteric waist at the junction of the mesorectum and mesocolon. Colorectal Disease, 22, 212–218. [DOI] [PubMed] [Google Scholar]
- Eickhoff, A. , Pickhardt, P.J. , Hartmann, D. & Riemann, J.F. (2010) Colon anatomy based on CT colonography and fluoroscopy: impact on looping, straightening and ancillary manoeuvres in colonoscopy. Digestive and Liver Disease, 42, 291–296. [DOI] [PubMed] [Google Scholar]
- FCAT . (1998) Terminologia anatomica. Stuttgart: Georg Thieme Verlag. [Google Scholar]
- FIPAT . (2019) library.dal.ca.
- Hanson, M.E. , Pickhardt, P.J. , Kim, D.H. & Pfau, P.R. (2007) Anatomic factors predictive of incomplete colonoscopy based on findings at CT colonography. American Journal of Roentgenology, 189, 774–779. [DOI] [PubMed] [Google Scholar]
- Kapadia, M.R. (2017) Volvulus of the small bowel and colon. Clinics in Colon and Rectal Surgery, 30, 40–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy, R. , Jenkins, I. & Finan, P.J. (2008) Controversial topics in surgery: splenic flexure mobilisation for anterior resection performed for sigmoid and rectal cancer. Annals of the Royal College of Surgeons of England, 90, 638–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khashab, M.A. , Pickhardt, P.J. , Kim, D.H. & Rex, D.K. (2009) Colorectal anatomy in adults at computed tomography colonography: normal distribution and the effect of age, sex, and body mass index. Endoscopy, 41, 674–678. [DOI] [PubMed] [Google Scholar]
- Koppen, I.J. , Yacob, D. , Di Lorenzo, C. , Saps, M. , Benninga, M.A. , Cooper, J.N. et al. (2017) Assessing colonic anatomy normal values based on air contrast enemas in children younger than 6 years. Pediatric Radiology, 47, 306–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malas, M.A. , Aslankoç, R. , Ungör, B. , Sulak, O. & Candir, O. (2004) The development of large intestine during the fetal period. Early Human Development, 78, 1–13. [DOI] [PubMed] [Google Scholar]
- Massalou, D. , Moszkowicz, D. , Mariage, D. , Baqué, P. , Camuzard, O. & Bronsard, N. (2018) Is it possible to give a single definition of the rectosigmoid junction? Surgical and Radiologic Anatomy, 40, 431–438. [DOI] [PubMed] [Google Scholar]
- Memon, S. , Keating, J.P. , Cooke, H.S. & Dennett, E.R. (2009) A study into external rectal anatomy: improving patient selection for radiotherapy for rectal cancer. Diseases of the Colon & Rectum, 52, 87–90. [DOI] [PubMed] [Google Scholar]
- Moore, K.L. & Dalley, A.F. (1999) Clinically oriented anatomy, 4th edition. Baltimore, MD: Lippincott Williams & Wilkins. [Google Scholar]
- Paulsen, F. & Waschke, J. (2011) Sobotta atlas of human anatomy. Internal organs, 15th edition. Munich: Elseviere Urban & Fischer. [Google Scholar]
- Petropoulou, T. & Amin, S. (2019) Novel approach for hepatic flexure mobilization with infracolic, suprapancreatic, medial‐to‐lateral approach. Techniques in Coloproctology, 23, 801. [DOI] [PubMed] [Google Scholar]
- Regadas, F.S. , Murad‐Regadas, S.M. , Lima, D.M. , Silva, F.R. , Barreto, R.G. , Souza, M.H. et al. (2007) Anal canal anatomy showed by three‐dimensional anorectal ultrasonography. Surgical Endoscopy and Other Interventional Techniques, 21, 2207–2211. [DOI] [PubMed] [Google Scholar]
- Shafik, A.A. , Asaad, S. , Loka, M.M. , Wahdan, M. & Shafik, A. (2009) Colosigmoid junction: morphohistologic, morphometric, and endoscopic study with identification of colosigmoid canal with sphincter. Clinical Anatomy, 22, 243–249. [DOI] [PubMed] [Google Scholar]
- Standring, S. (2020) Gray's anatomy, 42nd edition. The Anatomical Basis of Clinical Practice. Amsterdam: Elsevier. [Google Scholar]
- Tirkes, T. , Sandrasegaran, K. , Patel, A.A. , Hollar, M.A. , Tejada, J.G. , Tann, M. et al. (2012) Peritoneal and retroperitoneal anatomy and its relevance for cross‐sectional imaging. Radiographics, 32, 437–451. [DOI] [PubMed] [Google Scholar]
- Utano, K. , Nagata, K. , Honda, T. , Kato, T. , Lefor, A.K. & Togashi, K. (2021) Bowel habits and gender correlate with colon length measured by CT colonography. Japanese Journal of Radiology, 40, 298–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman, M.A. , McGee, M.F. , Helenowski, I.B. , Halverson, A.L. , Boller, A.M. & Stryker, S.J. (2016) The anthropometric definition of the rectum is highly variable. International Journal of Colorectal Disease, 31, 189–195. [DOI] [PubMed] [Google Scholar]
- Wozniak, S. , Pytrus, T. , Kobierzycki, C. , Grabowski, K. & Paulsen, F. (2019) The large intestine from fetal period to adulthood and its impact on the course of colonoscopy. Annals of Anatomy, 224, 17–22. [DOI] [PubMed] [Google Scholar]
- Wozniak, S. , Pawlus, A. , Grzelak, J. , Chobotow, S. , Paulsen, F. , Olchowy, C. et al. (2022) Descending‐sigmoid colon flexure – an important but surprisingly ignored landmark. Annals of Anatomy, 239, 151821. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request from the authors.


