Abstract
Introduction
Our objective was to identify factors associated with episiotomy practice in France, in particular, characteristics of the maternity units and regions of delivery.
Material and methods
We performed a national cross‐sectional population‐based study in all French maternity units in 2016 including 9284 women with vaginal delivery. Our outcome was the performance of an episiotomy. After stratification for parity, associations of episiotomy practice with individual and organizational characteristics and the region of delivery were estimated with multilevel logistic regression models. The variability in maternity unit episiotomy rates explained by the characteristics studied was estimated by the proportional change in variance.
Results
A total of 19.9% of the women had an episiotomy. The principal factors associated with episiotomy practice were maternal and obstetric and delivery in a maternity unit with <2000 annual deliveries. After adjusting for individual, obstetric and organizational characteristics, the practice of episiotomy was strongly associated with women's region of delivery. Additionally, women's individual characteristics did not explain the significant variability in episiotomy rates between maternity units (P < 0.001) but maternity unit characteristics partly did (proportion of variance explained: 7.2% for primiparas and 13.6% for multiparas) and regional differences still more (18% and 30.7%, respectively).
Conclusions
Episiotomy practices in France in 2016 varied strongly between maternity units, largely due to regional differences. Targeted actions by the regional perinatal care networks may reduce the national episiotomy rate and standardize practices.
Keywords: associated factors, episiotomy, maternity units, organizational characteristics, regions, variability
In the French National Perinatal Survey, maternity unit characteristics in part and regional differences especially explained episiotomy rate variability.
Abbreviations
- CI
confidence interval
- CNGOF
French National College of Gynecologists and Obstetricians
- NPS
National Perinatal Survey
- OR
odds ratio
- PCV
proportional change of variance
Key message.
In the French National Perinatal Survey, maternity unit characteristics partly and regional differences especially explained episiotomy rate variability.
1. INTRODUCTION
The routine practice of episiotomies has not shown benefits for either maternal or neonatal morbidity. 1 Its value in reducing the risk of obstetric anal sphincter injuries remains controversial today, but the risks of postpartum hemorrhage, 2 , 3 urinary retention, 4 infection, 5 perineal pain and dyspareunia are well known. 6
Guidelines in the past few years have aimed to limit the practice of episiotomy in most Western countries; its routine use has not been recommended for many years in the USA, 7 Belgium, 8 the UK 9 or France. 10 In 2005, the French National College of Gynecologists and Obstetricians (CNGOF) proposed a maximum episiotomy rate of 30%, which corresponds to the rate in the group with restrictive practices in the last meta‐analysis published before these guidelines 11 ; it concluded that neither maternal nor fetal morbidity differed between routine and restrictive episiotomy practices. The UK National Institute for Health and Care Excellence 11 (NICE) and the World Health Organization (WHO) have issued more recent guidelines about episiotomies in spontaneous vaginal deliveries, but without setting any maximum rates. The guidelines issued by the Society of Obstetricians and Gynecologists of Canada 12 (SOGC) focus on episiotomies in operative vaginal deliveries.
Internationally, episiotomy rates vary strongly but they have nonetheless fallen very substantially in recent years. In the USA, the rate fell from 33% to 12% between 2000 and 2012, in Canada from 24% to 17% between 2000 and 2007, in the UK from 36% to 15% between 1989 and 2010, and in Finland from 42% to 24% between 1997 and 2010. 13
A systematic review recently identified or confirmed some risk factors for episiotomy, mostly obstetric: the absence of a prior vaginal delivery, breech presentation, operative vaginal delivery, oxytocin use during labor, epidural analgesia and birthweight. 14 A French study based on the National Perinatal Survey (NPS) conducted in 2010 found the same factors as well as substantial variability of episiotomy rates between maternity units and between regions. 15
Despite a substantial reduction in recent years, the episiotomy rate remained high in France in 2016. Our objective was to assess the factors related to this practice and in particular the role of the characteristics of maternity units and regions in order to help target actions aimed at improving our practices.
2. MATERIAL AND METHODS
Our data come from the 2016 NPS, a cross‐sectional population‐based survey comprising all stillbirths and live‐born children (after at least 22 weeks of gestation and weighing at least 500 g) in France, during the equivalent of 1 week in March 2016. The data were collected from different sources: a face‐to‐face interview with the women before their discharge from the maternity unit, the women's medical files, and a questionnaire related to the organization of care and the environment of the maternity unit of delivery. Our sample included 13 132 women who gave birth in metropolitan France. We excluded the 548 women who refused to participate and the 834 who did not have a face‐to‐face interview: minors, women with a medically indicated termination of pregnancy or intrauterine death, difficulties expressing themselves in French or health problems (of mother or child and preventing the interview). We also excluded 2282 women with cesarean deliveries and 90 with multiple pregnancies. Finally, data about the performance of an episiotomy were missing for 94 women (1%) (Figure 1).
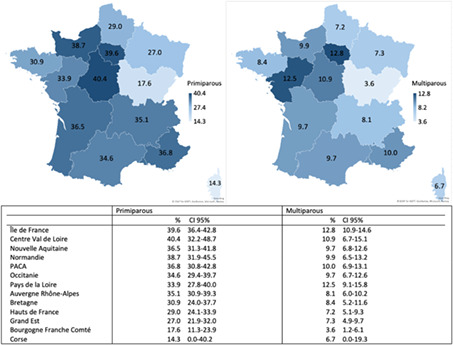
FIGURE 1.
Flow chart of the survey and episiotomy frequency (with 95% confidence interval) in the overall population and according to parity, cesarean history and number of previous vaginal deliveries.
Our outcome was the performance (yes/no) of an episiotomy, a data item collected in the women's medical files. In France, we mainly perform right mediolateral episiotomies.
We studied the following individual characteristics: parity, maternal age (years), country of birth, preconception body mass index, educational level, markers from a deprivation index 16 (if woman were concerned by at least one of the following four variables: (1) receiving an RSA [Revenu de Solidarité Active] allowance, (2) benefitting from the CMU [Couverture Maladie Universelle for households with extremely low incomes] or having no health insurance, (3) not having personal housing or (4) not living with a partner); participation in childbirth education classes, presence of suspected macrosomia (if the medical file included a specific mention of a fetal weight abnormality: fetal weight estimation >4000 g or >90th percentile), gestational age (weeks of gestation), fetal presentation, neuraxial analgesia, oxytocin administration during labor, birth during the daytime (8:00 to 20:00 h) or night‐time (20:00 to 8:00 h), mode of delivery (spontaneous or operative vaginal delivery), as well as the attending practitioner (midwife or obstetrician) and, for instrumental deliveries, the instrument used (forceps, spatula or vacuum). In the analysis of parity, we distinguished multiparous women with a history of cesarean delivery and the number of previous vaginal deliveries.
We also studied the following maternity unit characteristics: hospital status (university or regional center, community hospital center, private non‐profit or other private), the annual number of deliveries, and the presence of at least one delivery room dedicated to normal, ie physiological birth (yes/no). Finally, we studied these data for each of the 13 administrative and health regions in France. We choose the region “Ile de France” as reference because it is the region with the highest number of deliveries (2120/9284 deliveries).
2.1. Statistical analyses
We calculated the episiotomy rates and their 95% confidence intervals (95% CI) in the overall population and then according to parity, cesarean history and number of previous vaginal deliveries. All the statistical analyses were stratified for parity (primi‐ or multiparity) because of its strong influence on the practice of episiotomies. In a univariable analysis, we compared the frequency of episiotomy according to the characteristics of the individuals and the maternity units, as well as the region of delivery.
We used a two‐level hierarchical logistic regression model with women (level 1) nested within regions (level 2). Multilevel analysis was chosen to take into account the hierarchical structure of our data – women at the first and individual level, nested in the second level of maternity units – and the lack of independence between women who delivered in the same maternity unit. First, we estimated a random intercept model, without any predictor variables (M0, “empty model”) to obtain the baseline regional‐level variance (). In a second model (M1), we included the individual characteristics of the mother, her pregnancy, labor and delivery. This model allowed us to estimate the residual regional variation after adjustment for individual‐level variables. We used the proportional change of variance (PCV, defined as PCV = ([n − 1] − [n])/ [n − 1] × 100) to assess the extent to which regional differences may be explained by the compositional factors (ie possible differences in the distribution of individual‐level characteristics) of the regions.
Next, we investigated whether the maternity unit characteristics (M2) and the region of delivery (M3) were associated with episiotomy.
We selected the variables for the multivariable analyses based on the literature and clinical relevance.
The results of the multilevel multivariable models are expressed as adjusted odds ratios (aOR) and their 95% CI.
For each model we tested whether the interhospital variability differed from zero with a Wald test and significance set at 0.05.
With a missing data rate <3% for each variable, we performed complete‐case analyses.
The statistical analyses were performed with SAS software (9.4). 17
2.2. Ethics statement
The 2016 NPS was approved by the French Data Protection Authority on January 14, 2016 (CNIL, approval number: 915197), the National Council on Statistical Information on July 3, 2015 (Comité du Label, approval number: 2016X703SA) and the INSERM Ethics Committee on December 16, 2014 (approval number: IRB00003888 no. 14–191).
3. RESULTS
Our study population comprised 9284 women, among whom 1947 (19.9%) had an episiotomy – 34.6% of the primiparous women and 9.7% of those who were multiparous (Figure 1). Among the latter, depending on their cesarean history and number of previous vaginal deliveries, the frequency of episiotomy varied from 3.4% to 34.7% (Figure 1).
In primiparas, the frequency of episiotomy rose with maternal age and for women with non‐European origins, suspected macrosomia, breech presentation, neuraxial analgesia use, oxytocin use, and as gestational age rose and fell with body mass index (Table 1). Among women with spontaneous vaginal delivery, the frequency of episiotomy was higher for obstetricians than for midwives. Regarding the organizational characteristics, episiotomies were more frequent among primiparous women giving birth in university hospital centers, in private non‐profit hospitals and in maternity units with fewer than 1000 annual deliveries (Table 1).
TABLE 1.
Episiotomy rates by individual and organizational characteristics – analysis stratified by parity.
| Primiparous | Multiparous | |||||
|---|---|---|---|---|---|---|
| n | Episiotomy | n | Episiotomy | |||
| n | % | n | % | |||
| Mothers' characteristics | ||||||
| Maternal age | ||||||
| <25 | 849 | 254 | 29.9 | 394 | 39 | 9.9 |
| ≥25 to <30 | 1548 | 545 | 35.2 | 1462 | 111 | 7.6 |
| ≥30 to <35 | 1019 | 370 | 36.3 | 2183 | 221 | 10.1 |
| ≥35 to <40 | 330 | 121 | 36.7 | 1196 | 129 | 10.8 |
| ≥40 | 57 | 27 | 47.4 | 246 | 30 | 12.2 |
| Country of birth | ||||||
| France | 3247 | 1084 | 33.4 | 4404 | 415 | 9.4 |
| Other European countries | 134 | 40 | 29.9 | 236 | 21 | 8.9 |
| North Africa | 201 | 95 | 47.3 | 419 | 46 | 11.0 |
| Other African countries | 112 | 50 | 44.6 | 270 | 27 | 10.0 |
| China and Southeast Asia | 26 | 14 | 53.9 | 46 | 11 | 23.9 |
| Other | 82 | 33 | 40.2 | 105 | 10 | 9.5 |
| Preconception BMI | ||||||
| <25 | 2849 | 1028 | 36.1 | 3631 | 361 | 9.9 |
| 25–29 | 628 | 202 | 32.2 | 1123 | 104 | 9.3 |
| ≥30 | 279 | 71 | 25.5 | 644 | 55 | 8.5 |
| Educational level | ||||||
| Did not attend middle school | 147 | 54 | 36.7 | 561 | 36 | 6.4 |
| High school | 1327 | 434 | 32.7 | 2023 | 171 | 8.5 |
| 1–2 years post‐secondary education | 731 | 238 | 32.6 | 1040 | 108 | 10.4 |
| 3–4 years post‐secondary education | 786 | 288 | 36.6 | 911 | 102 | 11.2 |
| ≥5 years post‐secondary education | 780 | 290 | 37.2 | 900 | 108 | 12.0 |
| At least one marker from deprivation index | ||||||
| No | 3038 | 1051 | 34.6 | 4287 | 457 | 10.7 |
| Yes | 764 | 265 | 34.7 | 1194 | 73 | 6.1 |
| Pregnancy characteristics | ||||||
| Any previous cesarean and number of previous vaginal deliveries (VD) | ||||||
| No cesarean history and 1 VD | 3130 | 330 | 10.5 | |||
| No cesarean history and ≥2 VD | 1808 | 61 | 3.4 | |||
| Previous cesarean and 1 VD | 141 | 21 | 14.9 | |||
| Previous cesarean and ≥2 VD | 72 | 4 | 5.6 | |||
| Previous cesarean without previous VD | 329 | 114 | 34.7 | |||
| Suspected macrosomia | ||||||
| No | 3664 | 1252 | 34.2 | 5200 | 492 | 9.5 |
| Yes | 121 | 59 | 48.8 | 246 | 35 | 14.2 |
| Childbirth education classes | ||||||
| No | 780 | 249 | 31.9 | 3515 | 299 | 8.5 |
| Yes | 3008 | 1063 | 35.3 | 1941 | 228 | 11.8 |
| Characteristics of labor and delivery | ||||||
| Gestational age | ||||||
| ≤36 | 186 | 41 | 22.0 | 208 | 16 | 7.7 |
| 37–38 | 757 | 251 | 33.2 | 1201 | 92 | 7.7 |
| 39–40 | 2103 | 717 | 34.1 | 3152 | 315 | 10.0 |
| ≥41 | 753 | 307 | 40.8 | 915 | 106 | 11.6 |
| Presentation | ||||||
| Cephalic | 3760 | 1299 | 34.6 | 5436 | 522 | 9.6 |
| Breech | 36 | 16 | 44.4 | 39 | 6 | 15.4 |
| Neuraxial analgesia | ||||||
| No | 375 | 75 | 20.0 | 1359 | 67 | 4.9 |
| Yes | 3424 | 1240 | 36.2 | 4106 | 462 | 11.3 |
| Oxytocin during labor | ||||||
| No | 1379 | 388 | 28.1 | 3239 | 256 | 7.9 |
| Yes | 2408 | 925 | 38.4 | 2222 | 271 | 12.2 |
| Time of birth | ||||||
| 08:00–20:00 h | 2055 | 731 | 35.6 | 2806 | 275 | 9.8 |
| 20:00–08:00 h | 1740 | 586 | 33.7 | 2664 | 255 | 9.6 |
| Mode of delivery | ||||||
| Spontaneous vaginal delivery | 271 | 669 | 24.6 | 5148 | 399 | 7.8 |
| Instrumental vaginal delivery | 1085 | 647 | 59.6 | 332 | 130 | 39.2 |
| Details of delivery | ||||||
| Spontaneous vaginal delivery, attended by midwife | 2371 | 565 | 23.8 | 4499 | 328 | 7.3 |
| Spontaneous vaginal delivery, attended by obstetrician | 329 | 102 | 31.0 | 564 | 67 | 11.9 |
| Forceps | 310 | 247 | 79.7 | 87 | 45 | 51.7 |
| Spatula | 242 | 163 | 67.4 | 67 | 31 | 46.3 |
| Vacuum | 530 | 234 | 44.2 | 177 | 53 | 29.9 |
| Maternity unit characteristics | ||||||
| Status | ||||||
| University or regional hospital center | 719 | 271 | 37.7 | 1002 | 83 | 8.3 |
| Community hospital center | 1854 | 603 | 32.5 | 2837 | 253 | 8.9 |
| Private non‐profit | 345 | 101 | 29.3 | 393 | 44 | 11.2 |
| Other private | 885 | 342 | 38.6 | 1249 | 150 | 12.0 |
| Annual number of deliveries | ||||||
| <1000 | 659 | 257 | 39.0 | 1039 | 114 | 11.0 |
| 1000–1999 | 1183 | 392 | 33.1 | 1700 | 148 | 8.7 |
| 2000–2999 | 842 | 288 | 34.2 | 1209 | 139 | 11.5 |
| ≥3000 | 1119 | 380 | 34.0 | 1553 | 129 | 8.4 |
| Room dedicated to normal birth | ||||||
| No | 2121 | 756 | 35.6 | 3065 | 309 | 10.1 |
| Yes | 1677 | 559 | 33.3 | 2408 | 220 | 9.1 |
Among multiparas, the frequency of episiotomy rose with maternal age and gestational age; it was also higher for women born in China and Southeast Asia compared with all other geographic zones, or with suspected macrosomia, breech presentation or receiving neuraxial analgesia or oxytocin or both. An episiotomy was more frequent for forceps deliveries than for those with spatulas or vacuum deliveries (Table 1).
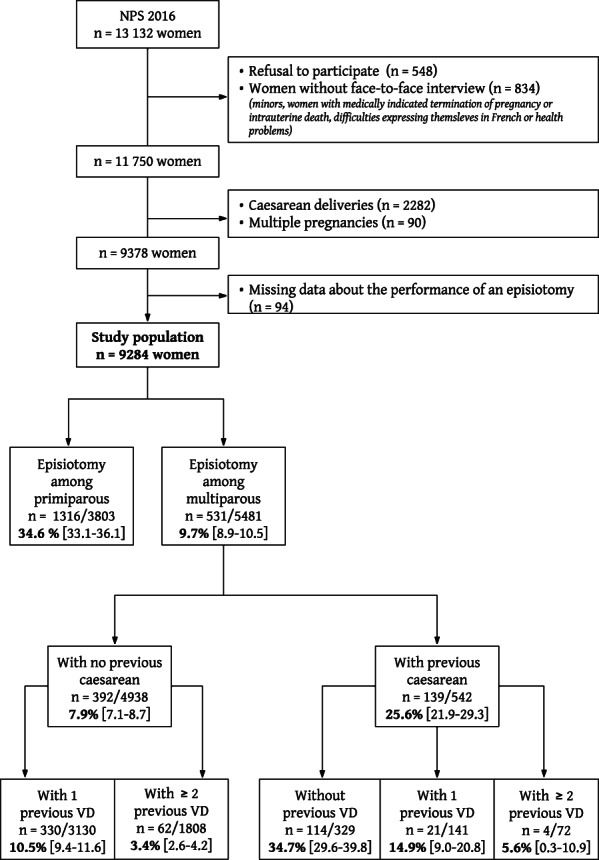
Figure 2 presents the frequency of episiotomy and its 95% CI in each French region by parity. Among primiparas, it varied from 14.3% in Corsica to 40.4% in the Centre‐Val de Loire and in multiparas from 3.6% in Bourgogne Franche Comté to 12.8% in Ile de France (Figure 2).
FIGURE 2.
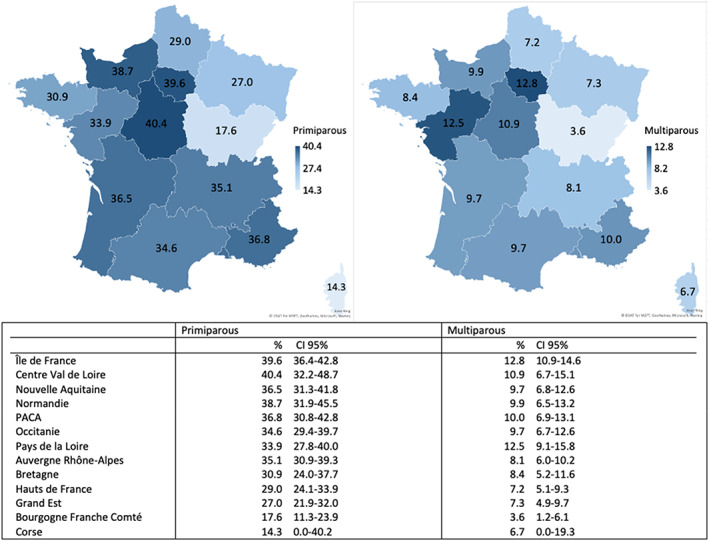
Episiotomy rate (with 95% confidence interval) by region of delivery.
In the multivariable analysis, the following individual characteristics were associated with an episiotomy in both primiparous and multiparous women: maternal birth in Africa, suspected macrosomia and operative vaginal delivery (primiparas: aOR forceps 14.38, 95% CI 10.29–20.10; aOR spatulas 8.28, 95% CI 5.83–11.75; and aOR vacuum delivery 2.79, 95% CI, 2.22–3.52; for multiparas: aOR forceps 7.76, 95% CI 4.61–13.07; aOR spatulas 6.70, 95% CI 3.71–12.10; and aOR vacuum delivery 3.54, 95% CI, 2.35–5.32) (Table 2). In both parity groups, women without neuraxial analgesia were less likely to have an episiotomy than were those with such analgesia.
TABLE 2.
Performance of an episiotomy according to the characteristics of women, their pregnancies, labors, deliveries, maternity units and regions: multilevel multivariate analysis.
| Primiparous | Multiparous | |||
|---|---|---|---|---|
| aOR a | 95% CI% b | aOR a | 95% CI% b | |
| Individual characteristics | ||||
| Maternal age | ||||
| <25 | 0.90 | 0.71–1.14 | 1.36 | 0.87–2.15 |
| ≥25 to < 30 | 1 | 1 | ||
| ≥30 to < 35 | 0.99 | 0.81–1.22 | 1.31 | 0.99–1.73 |
| ≥35 to < 40 | 0.82 | 0.60–1.10 | 1.49 | 1.08–2.04 |
| ≥40 | 1.14 | 0.60–2.15 | 2.07 | 1.25–3.41 |
| Country of birth | ||||
| France | 1 | 1 | ||
| Other European countries | 0.62 | 0.39–0.99 | 0.81 | 0.47–1.42 |
| North Africa | 1.55 | 1.08–2.23 | 1.77 | 1.19–2.63 |
| Other African countries | 1.81 | 1.09–3.00 | 1.70 | 1.00–2.90 |
| China and Southeast Asia | 2.01 | 0.77–5.24 | 2.30 | 0.98–5.37 |
| Other | 1.09 | 0.63–1.89 | 1.05 | 0.46–2.42 |
| Preconception BMI | ||||
| <25 | 1 | 1 | ||
| ≥25 to <30 | 0.81 | 0.65–1.01 | 0.89 | 0.68–1.16 |
| ≥30 | 0.55 | 0.39–0.77 | 0.82 | 0.58–1.16 |
| Educational level | ||||
| Did not attend middle school | 1.28 | 0.82–1.99 | 0.90 | 0.57–1.43 |
| High school | 1 | 1 | ||
| 1–2 years post‐secondary education | 0.90 | 0.71–1.14 | 0.99 | 0.73–1.33 |
| 3–4 years post‐secondary education | 0.95 | 0.75–1.21 | 1.04 | 0.76–1.43 |
| ≥5 years post‐secondary education | 1.05 | 0.82–1.36 | 0.99 | 0.71–1.37 |
| At least one marker of deprivation index | ||||
| No | 1 | 1 | ||
| Yes | 1.05 | 0.83–1.32 | 0.64 | 0.46–0.89 |
| Any previous cesarean and number of previous vaginal deliveries (VD) | ||||
| No previous cesarean with 1 previous VD | 1 | |||
| No previous cesarean with ≥2 VD | 0.29 | 0.21–0.40 | ||
| Previous cesarean with 1 previous VD | 1.47 | 0.87–2.49 | ||
| Previous cesarean with ≥2 previous VD | 0.48 | 0.16–1.42 | ||
| Previous cesarean without previous VD | 2.93 | 2.14–4.00 | ||
| Suspected macrosomia | ||||
| No | 1 | 1 | ||
| Yes | 1.63 | 1.06–2.51 | 1.79 | 1.17–2.74 |
| Childbirth education classes | ||||
| No | 1 | 1 | ||
| Yes | 1.28 | 1.01–1.62 | 0.96 | 0.75–1.21 |
| Gestational age | ||||
| ≤36 | 0.56 | 0.37–0.87 | 0.73 | 0.40–1.33 |
| 37–38 | 1.04 | 0.84–1.28 | 0.72 | 0.54–0.95 |
| 39–40 | 1 | 1 | ||
| ≥41 | 1.30 | 1.05–1.59 | 1.21 | 0.92–1.58 |
| Presentation | ||||
| Cephalic | 1 | 1 | ||
| Breech | 1.99 | 0.90–4.39 | 1.80 | 0.63–5.15 |
| Neuraxial analgesia | ||||
| No | 0.67 | 0.49–0.93 | 0.59 | 0.43–0.82 |
| Yes | 1 | 1 | ||
| Oxytocin during labor | ||||
| No | 1 | 1 | ||
| Yes | 1.21 | 1.01–1.45 | 1.16 | 0.93–1.45 |
| Details of delivery | ||||
| Spontaneous vaginal delivery, managed by midwife | 1 | 1 | ||
| Spontaneous vaginal delivery, managed by obstetrician | 1.59 | 1.14–2.23 | 1.40 | 0.96–2.03 |
| Forceps | 14.38 | 10.29–20.10 | 7.76 | 4.61–13.07 |
| Spatula | 8.28 | 5.83–11.76 | 6.70 | 3.71–12.10 |
| Vacuum extractor | 2.79 | 2.22–3.52 | 3.54 | 2.35–5.32 |
| Maternity unit characteristics | ||||
| Status | ||||
| University or regional hospital center | 1.31 | 0.92–1.87 | 1.08 | 0.74–1.59 |
| Community hospital center | 1 | 1 | ||
| Private non‐profit | 0.86 | 0.56–1.31 | 1.06 | 0.67–1.67 |
| Other private | 0.93 | 0.71–1.22 | 1.10 | 0.81–1.49 |
| Annual number of deliveries | ||||
| <1000 | 1.98 | 1.37–2.85 | 2.22 | 1.49–3.31 |
| 1000–1999 | 1.42 | 1.01–1.99 | 1.52 | 1.04–2.22 |
| 2000–2999 | 1.31 | 0.93–1.83 | 1.84 | 1.29–2.62 |
| ≥3000 | 1 | 1 | ||
| Room dedicated to normal birth | ||||
| No | 1 | 1 | ||
| Yes | 0.89 | 0.72–1.12 | 0.97 | 0.75–1.24 |
| French regions | ||||
| Regions | ||||
| Ile de France | 1 | 1 | ||
| Centre Val de Loire | 1.23 | 0.69–2.18 | 1.02 | 0.55–1.90 |
| Bourgogne Franche Comté | 0.26 | 0.14–0.49 | 0.28 | 0.12–0.63 |
| Normandie | 1.21 | 0.72–2.02 | 1.04 | 0.60–1.83 |
| Hauts de France | 0.59 | 0.39–0.91 | 0.58 | 0.37–0.93 |
| Grand Est | 0.66 | 0.43–1.03 | 0.58 | 0.35–0.96 |
| Pays de la Loire | 1.00 | 0.61–1.64 | 1.24 | 0.75–2.03 |
| Bretagne | 0.73 | 0.43–1.26 | 0.71 | 0.39–1.27 |
| Nouvelle Aquitaine | 0.78 | 0.51–1.19 | 0.74 | 0.45–1.21 |
| Occitanie | 0.72 | 0.50–1.11 | 0.77 | 0.47–1.26 |
| Auvergne Rhône‐Alpes | 0.84 | 0.58–1.23 | 0.69 | 0.45–1.06 |
| Provence Alpes Côte d'Azur | 1.03 | 0.65–1.62 | 0.91 | 0.55–1.50 |
| Corse | 0.37 | 0.04–3.73 | 0.65 | 0.07–5.75 |
aOR = odds ratio adjusted for all of the variables in the model: maternal age, country of birth, preconception BMI, educational level, precarity/social insecurity, previous cesarean delivery, and number of vaginal deliveries, suspected macrosomia, childbirth and parenting preparation course, gestational age, fetal presentation, local‐regional analgesia, oxytocin during labor, details of delivery, status, number of deliveries per year, facilities for physiological births, and regions.
95% confidence interval.
Among primiparas, women who were obese were less likely to have an episiotomy, whereas these procedures were more likely among women who attended childbirth education classes, gave birth late term or post term, received oxytocin during labor or were attended by an obstetrician rather than a midwife for spontaneous vaginal delivery. Among multiparas, the likelihood of episiotomy was higher among women who were older or had a previous cesarean without any previous vaginal delivery; this likelihood was lower for those with at least one marker of deprivation, or with an obstetric history of no previous cesareans and at least two previous vaginal births.
In terms of organization of care, an episiotomy was associated with primiparas giving birth in a maternity unit with fewer than 2000 deliveries per year and with multiparas giving birth in units with fewer than 3000 deliveries annually.
Finally, some regions were significantly associated with episiotomy practice; compared with Ile de France, the aORs for Bourgogne Franche Comté were 0.26 (95% CI 0.14–0.49) among primiparas and 0.28 (95% CI 0.12–0.63) among multiparas, and for Hauts de France, respectively, 0.59 (95% CI 0.39–0.91) and 0.58 (95% CI 0.37–0.93). The aOR for the Grand Est was also 0.58 (95% CI 0.35–0.96) among multiparas.
Episiotomy rates varied significantly between maternity units among both primiparous and multiparous women (P < 0.001) (Table 3). The individual characteristics studied do not explain this variability. On the other hand, 7.2% of the variability of the episiotomy rate between maternity units for primiparas and 15.5% of that for multiparas was explained by adding the organizational characteristics of the maternity units, after adjustment for individual characteristics (model 2 vs model 1). Finally, adding the region to the model while adjusting for both the individual and organizational characteristics made it possible to explain 18% of the variability among primiparas and 30% among multiparas (model 3).
TABLE 3.
Variability of episiotomy rates between maternity units for each successive model and the percentage of variance it explains.
| Primiparous | Multiparous | |||
|---|---|---|---|---|
| Variance | PCV (%) | Variance | PCV (%) | |
| Model 0 | 0.422 | 0.335 | ||
| Model 1 | 0.518 | NC a | 0.376 | NC a |
| Model 2 | 0.481 | 7.2 | 0.317 | 15.5 |
| Model 3 | 0.394 | 18.0 | 0.222 | 30.0 |
Note: PCV calculated in relation to Model n − 1: ( [Mn − 1] − .
Model 0 = model empty.
Model 1 = M0+ individual characteristics (maternal, pregnancy, labor and delivery).
Model 2 = M1+ maternity unit characteristics.
Model 3 = M2+ French regions.
Abbreviation: PCV, proportional change of variance.
A negative PVE was a non‐contributory result and signified that the characteristics included in the model did not explain the variance in episiotomy use between maternity units.
4. DISCUSSION
The episiotomy rate in France in 2016 was 19.9%: 34.6% in primiparas and 9.7% in multiparas. Regardless of parity, the performance of an episiotomy was associated with the following individual factors: maternal birth in Africa, suspected macrosomia, operative vaginal delivery, neuraxial analgesia, previous cesarean delivery, previous cesarean without a history of vaginal delivery, and with one characteristic of the maternity units: smaller size. The variability of the episiotomy rate found between the maternity units was not explained by the women's individual characteristics and was only slightly explained by the organizational characteristics of the maternity units, but was especially explained by the region, for both groups of women.
Our data come from the NPS, which is a large, population‐based nationwide survey. The data, which cover all births during 1 week, are representative of all annual births in metropolitan France. 18 , 19 The NPS furnishes numerous items of information needed to assess the factors related to episiotomy and its variability between maternity units. We took the hierarchical nature of our data into account by using a multilevel model to obtain more exact estimators of variance. The use of several models to introduce the different categories of variables successively enabled us to better determine the percentage of the variance explained by each of these categories. Nonetheless, the NPS is intended to cover numerous topics relevant to the surveillance of perinatal health and the evaluation of perinatal practices. Accordingly, we cannot rule out some residual confounding linked to data not collected in the NPS that could be related to the performance of an episiotomy, such as previous episiotomy practice, fetal presentation at delivery, specific indication for the episiotomy, the details of the delivery or information about the practitioners' years of experience or the department's audit practices. The low variability explained by individual characteristics might be due to the absence of data concerning these characteristics. Due to debate on obstetric violence since 2018 in France and the 2018 recommendations from the CNGOF, 20 we cannot exclude a change in explanatory factors. Although the episiotomy rate has probably decreased, the variability between maternity units persists; however, it is likely that a significant decrease occurs in the population of delivery performed by obstetricians in small maternity units because of the societal context and the consideration of medicolegal implications associated with episiotomy performances.
Among the individual characteristics examined in our study, the risk of episiotomy was particularly high for operative vaginal deliveries, despite its marked decline between the last two national perinatal surveys in 2010 and 2016. In 2010, 15 70.0% of operative vaginal deliveries of primiparas were performed with an episiotomy and 50.4% in multiparas, compared, respectively, with 59.6% and 39.2% in 2016. Moreover, episiotomy practice differed greatly according to the instrument used: primiparas are at higher risk of an episiotomy during a delivery with a forceps or spatula than by vacuum delivery, and these differences are well known in the literature. 21 , 22 A portion of this difference may be explained by the fact that forceps are used more often in the most unfavorable situations, which are also those at highest risk of episiotomy.
On the other hand, characteristics associated with the practitioner may explain some differences in episiotomy practices. We found that women with spontaneous vaginal deliveries were more likely to have an episiotomy when they were attended by an obstetrician than by a midwife. This confirms the findings of several other publications. 23 It is possible that obstetricians have a more interventionist attitude at delivery because they are more accustomed to non‐physiological deliveries. Nonetheless it is also possible that the spontaneous vaginal deliveries by obstetricians were more complex obstetric situations (for example, fetal heart rate abnormalities) that could well justify a higher episiotomy rate. Nonetheless, the individual characteristics of the practitioners who attend child births, other than their occupation (midwife or physician), may also be associated with the performance of an episiotomy. That is, some authors find that the risk of episiotomy is highest in older practitioners, 24 those with the most years of experience. This is probably explained by the more effective diffusion of and adherence to guidelines among younger perinatal professionals. These recommendations are integrated in their initial training, and it is their professors, those practicing in these university hospital centers, who participate in the development of these guidelines. Gachon et al. advanced these hypotheses in 2019 in a publication assessing inter‐practitioner variability in episiotomy use among 389 members of the CNGOF. 25 A qualitative study published in 2020 concluded that care providers' underlying vision on episiotomy and childbirth was an important contributor to the large variations in episiotomy usage. 26 Their clinical expertise was a more important component in decision‐making in episiotomy compared with the literature. Women were minimally involved in the decision to perform episiotomy.
In our study, as in that of Gachon et al., 25 the smallest maternity units were associated with higher episiotomy use. Other studies have shown worse guideline adherence on other topics in the smallest maternity units, such as for oxytocin use 27 and management of postpartum hemorrhage. 28 The literature also indicates that university hospital maternity units 25 , 29 and public obstetrics departments in general 25 , 30 perform fewer episiotomies.
In France, in 2016, as in 2010, the impact of region on the risk of episiotomy, after adjustment for maternal and obstetric characteristics, was substantial, particularly among multiparas. This variability between regions has also been observed in Ireland 31 and Canada, 32 and involves other obstetric practices as well, such as cesarean delivery. 33 To our knowledge, however, few studies have examined the causes of these regional differences. The disparities in episiotomy use between practitioners are linked to the region they practice in, but also to the region where they were trained, 25 through the activities of local leaders active in student instruction and training and in practice audits. In France, for example, there are perinatal networks that often correspond to a region, except in the most populous regions, which contain several such networks. These are groups of medical and paramedical professionals practicing in different facilities, caring for parents and newborns, sharing their skills to optimize and harmonize perinatal management. We know that some perinatal networks have an important influence on practices, eg in Bourgogne Franche‐Comté, where regional perinatal policy, organized within a structured network, has enabled substantial diffusion and adherence to the national guidelines. 34 In 2012, Lutomski et al. published the results of a retrospective Irish cohort study on the regional variations of several obstetric interventions between 2005 and 2009. 31 Those authors argued that the episiotomy rate, which ranged from 18.5% to 27.4%, was strongly influenced by the clinicians' subjective views, experience and habits. Certainly, practitioners' adherence to guidelines can be influenced by the regional perinatal networks, some of which provide training about instrumental delivery and perineal protection.
There is an element of subjectivity in the obstetric practice of every obstetrician and midwife, which is why programs aimed at improving the quality of care are so important. Application of guidelines through the use of a multifaceted strategy based on audit and feedback and facilitated by opinion leaders makes it possible to improve the quality of care, professionals' practices and women's health. This strategy has demonstrated its effectiveness in reducing episiotomy rates in South America 35 and obstetric anal sphincter injuries rates in Iceland. 36 The implementation of a national program (OASI Care Bundle: antenatal information to women, manual perineal protection and mediolateral episiotomy when indicated) in England, Scotland and Wales has reduced OASI rates. 37
Practices analysis with the use of a classification (such as Robson for cesarean section) could help to support some strategies to control the episiotomy rate in some regions or maternity. 38
5. CONCLUSION
In France, in 2016, episiotomies were still being performed for 20% of women. The strong variability in episiotomy practice between maternity units is not explained by the maternal individual characteristics. This rate is higher in small maternity units, those with fewer than 2000 deliveries a year.
Substantial regional differences explain in part the variability between maternity units in the practice of episiotomies. In the absence of scientific evidence of the effectiveness of episiotomy, especially for spontaneous vaginal deliveries, these regional differences raise important questions.
Targeted actions by the regional perinatal care networks may reduce the national episiotomy rate and standardize practices.
AUTHOR CONTRIBUTIONS
JC performed the analyses and led the writing of the article. JM helped with statistical methods and interpretation of the results. BB conceived and planned the survey. CLR contributed to the study design, helped with statistical methods and helped to interpret the results as well as supervised the study. All authors assisted in critical revision of the manuscript and read and approved the final version of the article.
FUNDING INFORMATION
The National Perinatal Survey was funded by the French Ministry of Health (Direction de la Recherche, des Etudes, de l'Evaluation et des Statistiques [DREES], Direction Générale de la Santé (DGS) and Direction Générale de l'Organization des Soins [DGOS]) and by Santé Publique France.
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
ACKNOWLEDGMENTS
We thank the Maternal and Child Health Services in each district, regional perinatal networks, and regional heath agencies without which these surveys could not have been conducted. We also acknowledge all the local investigators who rigorously collected the data in each maternity unit, as well as all the mothers who agreed to be interviewed. We thank the supervisors of all the maternity units (department heads and midwive coordinators) who agreed to have the survey performed in their department.
Cormier J, Merrer J, Blondel B, Le Ray C. Influence of the maternity unit and region of delivery on episiotomy practice in France: a nationwide population‐based study. Acta Obstet Gynecol Scand. 2023;102:438‐449. doi: 10.1111/aogs.14522
REFERENCES
- 1. Jiang H, Qian X, Carroli G, Garner P. Selective versus routine use of episiotomy for vaginal birth. Cochrane Database Syst Rev. 2017;2:CD000081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bonnet MP, Basso O, Bouvier‐Colle MH, et al. Postpartum haemorrhage in Canada and France: a population‐based comparison. PLoS One. 2013;8:e66882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Girault A, Deneux‐Tharaux C, Sentilhes L, Maillard F, Goffinet F. Undiagnosed abnormal postpartum blood loss: incidence and risk factors. PLoS One. 2018;13:e0190845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tiberon A, Carbonnel M, Vidart A, Ben Halima M, Deffieux X, Ayoubi JM. Risk factors and management of persistent postpartum urinary retention. J Gynecol Obstet Hum Reprod. 2018;47:437‐441. [DOI] [PubMed] [Google Scholar]
- 5. Axelsson D, Brynhildsen J, Blomberg M. Postpartum infection in relation to maternal characteristics, obstetric interventions and complications. J Perinat Med. 2018;46:271‐278. [DOI] [PubMed] [Google Scholar]
- 6. Manresa M, Pereda A, Bataller E, Terre‐Rull C, Ismail KM, Webb SS. Incidence of perineal pain and dyspareunia following spontaneous vaginal birth: a systematic review and meta‐analysis. Int Urogynecology J. 2019;30:853‐868. [DOI] [PubMed] [Google Scholar]
- 7. Arnold KC, Flint CJ. Prevention and management of obstetric lacerations at vaginal delivery. Obstetrics Essentials. Springer International Publishing; 2017:253‐259. [Google Scholar]
- 8. Mambourg F, Gaily J, Zhang W. Guideline relative to low risk birth. Brussels, Federaal Kenniscentrum voor de Gezondheidszorg (KCE) Centre Fédéral d'Expertise des Soins de Santé (Belgian Health Care Knowledge Centre); 2010.
- 9. Intrapartum Care for Healthy Women and Babies. National Institute for Health and Care Excellence (NICE); 2017. PMID: 32212591. [PubMed] [Google Scholar]
- 10. CNGOF . Episiotomie: recommadations du CNGOF pour la pratique clinique (2005) [Episiotomy: recommendations of the CNGOF for clinical practice (December 2005)]. In French. Gynecol Obstet Fertil. 2006;34:275‐279. [DOI] [PubMed] [Google Scholar]
- 11. Hartmann K, Viswanathan M, Palmieri R, Gartlehner G, Thorp J, Lohr KN. Outcomes of routine episiotomy: a systematic review. JAMA. 2005;293:2141‐2148. [DOI] [PubMed] [Google Scholar]
- 12. Cargill YM, MacKinnon CJ, Arsenault MY, et al. Guidelines for operative vaginal birth. J Obstet Gynaecol Can. 2004;26:747‐761. [DOI] [PubMed] [Google Scholar]
- 13. Clesse C, Lighezzolo‐Alnot J, De Lavergne S, Hamlin S, Scheffler M. Statistical trends of episiotomy around the world: comparative systematic review of changing practices. Health Care Women Int. 2018;39:644‐662. [DOI] [PubMed] [Google Scholar]
- 14. Clesse C, Lighezzolo‐Alnot J, Lavergne SD, Hamlin S, Scheffler M. Factors related to episiotomy practice: an evidence‐based medicine systematic review. J Obstet Gynaecol. 2019;39:737‐747. [DOI] [PubMed] [Google Scholar]
- 15. Chuilon AL, Le Ray C, Prunet C, Blondel B. L'épisiotomie en France en 2010: variations des pratiques selon le contexte obstétrical et le lieu d'accouchement. J Gynécologie Obstétrique Biol Reprod. 2016;45:691‐700. [DOI] [PubMed] [Google Scholar]
- 16. Opatowski M, Blondel B, Khoshnood B, Saurel‐Cubizolles MJ. New index of social deprivation during pregnancy: results from a national study in France. BMJ Open. 2016;6:e009511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Witte JS, Greenland S, Kim LL, Arab L. Multilevel modeling in epidemiology with GLIMMIX. Epidemiol Camb Mass. 2000;11:684‐688. [DOI] [PubMed] [Google Scholar]
- 18. Quantin C, Cottenet J, Vuagnat A, et al. Qualité des données périnatales issues du PMSI: comparaison avec l'état civil et l'enquête nationale périnatale 2010. J Gynécologie Obstétrique Biol Reprod. 2014;43:680‐690. [DOI] [PubMed] [Google Scholar]
- 19. Blondel B, Coulm B, Bonnet C, Goffinet F, Le Ray C. Trends in perinatal health in metropolitan France from 1995 to 2016: results from the French National Perinatal Surveys. J Gynecol Obstet Hum Reprod. 2017;46:701‐713. [DOI] [PubMed] [Google Scholar]
- 20. Ducarme G, Pizzoferrato AC, de Tayrac R, et al. Perineal prevention and protection in obstetrics: CNGOF clinical practice guidelines (short version). Gynecol Obstet Fertil Senol. 2018;46:893‐899. [DOI] [PubMed] [Google Scholar]
- 21. Macleod M, Strachan B, Bahl R, et al. A prospective cohort study of maternal and neonatal morbidity in relation to use of episiotomy at operative vaginal delivery. BJOG. 2008;115:1688‐1694. [DOI] [PubMed] [Google Scholar]
- 22. Gachon B, Fritel X, Rivière O, Pereira B, Vendittelli F. French guidelines for restrictive episiotomy during instrumental delivery were not followed by an increase in obstetric anal sphincter injury. Sci Rep. 2022;12:6330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Johantgen M, Fountain L, Zangaro G, Newhouse R, Stanik‐Hutt J, White K. Comparison of labor and delivery care provided by certified nurse‐midwives and physicians: a systematic review, 1990 to 2008. Womens Health Issues. 2012;22:e73‐e81. [DOI] [PubMed] [Google Scholar]
- 24. Howard DH, Hockenberry J. Physician age and the abandonment of episiotomy. Health Serv Res. 2019;54:650‐657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gachon B, Charveriat A, Pierre F, Fritel X. Pratiques de l'épisiotomie: enquête auprès des membres du Collège National des Gynécologues Obstétriciens Français. Gynécologie Obstétrique Fertil Sénologie. 2019;47:627‐636. [DOI] [PubMed] [Google Scholar]
- 26. Seijmonsbergen‐Schermers A, Thompson S, Feijen‐de Jong E, et al. Understanding the perspectives and values of midwives, obstetricians and obstetric registrars regarding episiotomy: qualitative interview study. BMJ Open. 2021;11:e037536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Belghiti J, Coulm B, Kayem G, Blondel B, Deneux‐Tharaux C. Administration d'ocytocine au cours du travail en France. Résultats de l'enquête nationale périnatale 2010 [Oxytocin administration during labor. Results from the 2010 French National Perinatal Survey]. In French. J Gynecol Obstet Biol Reprod (Paris). 2013;42:662‐670. [DOI] [PubMed] [Google Scholar]
- 28. Dupont C, Deneux‐Tharaux C, Cortet M, et al. Prise en charge des hémorragies graves du post‐partum après un accouchement par voie basse: étude en population dans 106 maternités françaises. [Practices for management of grave postpartum haemorrhage after vaginal delivery: a population‐based study in 106 French maternity units]. In Franch. J Gynecol Obstet Biol Reprod (Paris). 2012;41:279‐289. [DOI] [PubMed] [Google Scholar]
- 29. Friedman AM, Ananth CV, Prendergast E, D'Alton ME, Wright JD. Variation in and factors associated with use of episiotomy. JAMA. 2015;313:197‐199. [DOI] [PubMed] [Google Scholar]
- 30. Goode KT, Weiss PM, Koller C, Kimmel S, Hess LW. Episiotomy rates in private vs. resident service deliveries: a comparison. J Reprod Med. 2006;51:190‐192. [PubMed] [Google Scholar]
- 31. Lutomski JE, Morrison JJ, Lydon‐Rochelle MT. Regional variation in obstetrical intervention for hospital birth in the Republic of Ireland, 2005–2009. BMC Pregnancy Childbirth. 2012;12:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chalmers B, Kaczorowski J, O'Brien B, Royle C. Rates of interventions in labor and birth across Canada: findings of the Canadian maternity experiences survey. Birth Berkeley Calif. 2012;39:203‐210. [DOI] [PubMed] [Google Scholar]
- 33. Seijmonsbergen‐Schermers AE, Zondag DC, Nieuwenhuijze M, et al. Regional variations in childbirth interventions in The Netherlands: a nationwide explorative study. BMC Pregnancy Childbirth. 2018;18:1‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ginod P, Khallouk B, Benzenine E, et al. Évaluation de la pratique restrictive de l'épisiotomie et de l'impact sur les déchirures périnéales au sein du Réseau périnatal de Bourgogne. J Gynécologie Obstétrique Biol Reprod. 2016;45:1165‐1171. [DOI] [PubMed] [Google Scholar]
- 35. Althabe F, Buekens P, Bergel E, et al. A behavioral intervention to improve obstetrical care. N Engl J Med. 2008;358:1929‐1940. [DOI] [PubMed] [Google Scholar]
- 36. Sveinsdottir E, Gottfredsdottir H, Vernhardsdottir AS, Tryggvadottir GB, Geirsson RT. Effects of an intervention program for reducing severe perineal trauma during the second stage of labor. Birth. 2019;46:371‐378. [DOI] [PubMed] [Google Scholar]
- 37. Gurol‐Urganci I, Bidwell P, Sevdalis N, et al. Impact of a quality improvement project to reduce the rate of obstetric anal sphincter injury: a multicentre study with a stepped‐wedge design. BJOG. 2021;128:584‐592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Desplanches T, Szczepanski E, Cottenet J, Semama D, Quantin C, Sagot P. A novel classification for evaluating episiotomy practices: application to the Burgundy perinatal network. BMC Pregnancy Childbirth. 2019;19:300. [DOI] [PMC free article] [PubMed] [Google Scholar]


