Abstract
Purpose
This paper describes a prospective cohort, Impact of Maternal and Paternal Mental Health: Assessing Concurrent Depression, Anxiety and Comorbidity in The Canadian Family (IMPACT) study, which followed maternal–paternal dyads and their children across the first 2 years post partum.
Participants
A total of 3217 cohabitating maternal–paternal dyads were recruited into the study from 2014 to 2018. Each dyad member separately completed online questionnaires at baseline (<3 weeks post partum) and again at 3, 6, 9, 12, 18 and 24 months on a variety of measures, including mental health, parenting environment, family functioning and child health and development.
Findings to date
At baseline, the mean maternal age was 31.9±4.2 years and 33.8±5.0 years for fathers. Overall, 12.8% of families had a household income below the poverty line of $C50 000, and 1 in 5 mothers and 1 in 4 fathers were not born in Canada. One in 10 women experienced depressive symptoms during pregnancy (9.7%) and 1 in 6 had markedly anxious symptoms (15.4%) while 1 in 20 men reported feeling depression during their partner’s pregnancy and 1 in 10 had marked anxiety (10.1%). Approximately 91% of mothers and 82% of fathers completed the 12-month questionnaire as did 88% of mothers and 78% of fathers at 24 months postpartum.
Future plans
The IMPACT study will examine the influence of parental mental illness in the first 2 years of a child’s life with a focus on understanding the mechanisms by which single (maternal or paternal) versus dual (maternal and paternal) parental depression, anxiety and comorbidity symptoms affect family and infant outcomes. Future analyses planned to address the research objectives of IMPACT will consider the longitudinal design and dyadic interparental relationship.
Keywords: MENTAL HEALTH, Depression & mood disorders, Anxiety disorders, Maternal medicine
Strengths and limitations of this study.
The Impact of Maternal and Paternal Mental Health: Assessing Concurrent Depression, Anxiety and Comorbidity in The Canadian Family (IMPACT) study is the first, large-scale Canada-wide longitudinal study including cohabiting parental dyads to explore parental mental health.
Participants are followed-up online every 3 months during the first year of post partum, and every 6 months during the second year of post partum using self-report standardised assessment tools.
This study will begin to fill the knowledge gap on paternal postpartum depression and anxiety, as well as parental comorbid depression and/or anxiety and the role of paternal mental disorders in child development.
While the overall IMPACT sample is very representative of the Canadian population, it does slightly over-represent higher-educated and higher-income individuals.
This study focused on two-parent families where one identified as female and the other as male, limiting generalisability to non-normative families.
Introduction
Depression is a widespread condition that has become a major public health priority. Although it affects individuals throughout the lifespan, there is an increased risk for both women and men during the postpartum period, with estimates suggesting up to 20% of families are negatively impacted.1 Anxiety commonly co-occurs with depression affecting over 15% of families in the first year post partum.2 Today, it is estimated that over 8 million parents in North America will experience a mental health disorder each year, putting at least 16 million children at risk for adverse outcomes.3 Poor parental mental health can interfere with parenting quality and increase the risk of children developing mental, behavioural and social problems—and evidence is clear that these negative effects begin in the early infant environment.3
To date, the majority of perinatal mental health research has been maternal focused. Research that concentrates on both parents, rather than just mothers, to examine the onset, course and consequences of parental postpartum depression, anxiety and comorbidity is needed to improve family outcomes. The parenting environment is multifaceted and the perceptions and behaviours of parents are inter-related. Some researchers have examined the processes by which the quality of the father’s functioning may buffer the association between maternal mental illness and infant development. Hops et al4 found higher rates of involvement and caring behaviour directed at children by non-depressed fathers when the mother was depressed than by non-depressed fathers when the mother was not depressed. However, Mezulis et al5 reported that an infant’s exposure to a non-depressed father did not buffer the effects of maternal depression even if the father spent large amounts of time with the infant. While support for the paternal moderating effect has been found in a few studies, the results of other investigations suggest that the relationship may be complex. To our knowledge, few studies have examined maternal involvement in moderating the effect of paternal mental health on infant development. Further, the impact of parental involvement when both parents are mentally unwell has not been examined.
To optimise parental and child health, the family environment should be studied more completely. Children of depressed and anxious parents are exposed to compounded negative parental cognitions and behaviours as well as a variety of stressors associated with the mental health concerns.6 These exposures are hypothesised as mechanisms mediating the relationship between parental mental illness and child development,6 that is, that negative parenting cognitions and behaviours can leave parents unable to meet their child’s social and emotional needs. Additional research is warranted to examine the mediating role that maternal and paternal parenting cognitions and behaviours play in relation to parental mental illness and infant development.
Little is known about the determinants of paternal postpartum depression and anxiety and the influence of paternal mental health and parenting behaviours and perceptions on child health and development. Given that both parents are often caring for children in our society, research which focuses on parents together is needed to develop interventions targeting the whole family, not just mothers. In order to address these knowledge gaps, we designed the Impact of Maternal and Paternal mental health: Assessing Concurrent depression, anxiety, and comorbidity in The Canadian family (IMPACT) study, a prospective cohort following cohabiting maternal and paternal dyads and their children across the first 2 years post partum. The primary objectives were to: (1) estimate the prevalence and determinants of parental mental illness including paternal, maternal and dual parental postpartum depression, anxiety, comorbid depression/anxiety and attention deficit-hyperactivity disorder (ADHD); (2) characterise the parenting environment and family functioning and their relationship with parental mental illness; (3) determine the influence of parental mental illness, the parenting environment and family functioning on child development; and (4) determine the roles of mediator/moderator variables that influence differences related to (i) depression/anxiety, (ii) substance use problems, (iii) interpersonal violence, (iv) interparental relationship dissatisfaction, (v) low social support, (vi) decreased parental satisfaction, (vii) problematic parenting behaviours, (viii) low parental involvement, (ix) increased parental stress, (x) perceptions of difficult infant temperament and (xi) health service use.
The IMPACT cohort, design and data collection is described in this paper. We also report the follow-up rates and provide the sociodemographic profile of mothers and fathers at baseline, compared with each other and to the general population using Canadian census data. A summary of obstetrical and pregnancy-related factors is also provided and a description of lifestyle habits and mental health history are provided for both parents. Together, with the sociodemographic profile, these data describe the background context for each parent to better understand the study outcomes.
Cohort description
Study design and setting
A community-based longitudinal prospective study was conducted with recruitment occurring from 2014 to 2018 across Canada (population ~36 million, where ~375 000 births occur annually) where self-report questionnaires were administered at baseline (<3 weeks post partum), 3, 6, 9, 12, 18 and 24 months post partum using the Research Electronic Data Capture (REDCap) online survey platform.7 Each member of the couple dyad was linked to each other. Table 1 outlines the study outcome measures based on timing of data collection.
Table 1.
IMPACT study outcome measures
| Conceptual model | Study variables | Outcome measures | Baseline <3 weeks post partum |
Months post partum | |||||
| 3 | 6 | 9 | 12 | 18 | 24 | ||||
| Demographics | Demographic form | X | |||||||
| Risk | Postpartum depression | SCID | X | X | X | X | X | X | |
| EPDS | X | X | X | X | X | X | X | ||
| GMDS | X | X | X | X | X | X | X | ||
| Moderators | Course of parental PPD | SCID | See above | ||||||
| Anxiety | STAI | X | X | X | X | X | X | X | |
| Parental ADHD | ASRS | X | |||||||
| Relationship style | X | ||||||||
| Adverse childhood experiences | ACE‐IQ | X | |||||||
| Substance abuse Alcohol Use Disorders Identification Test |
CAGE‐AID AUDIT |
X X |
X X |
X X |
|||||
| Parental involvement | PCRI‐I | X | X | X | X | X | |||
| Infant temperament | IBQ‐R ECBQ‐VSF |
X | X | ||||||
| Infant gender | Demographic form | See above | |||||||
| Family functioning | Social support | SPS | X | X | X | X | |||
| Health service utilisation | HSUCCQ | X | X | X | X | X | X | ||
| Mediators | Parental satisfaction | PCRI‐SP | X | X | X | X | X | X | |
| Parental role orientation | PCRI-RO | X | X | ||||||
| Parenting behaviours | PS | X | X | X | |||||
| Infant health promotion | IHPQ | X | X | X | X | ||||
| Marital dissatisfaction | DAS | X | X | X | X | X | X | ||
| Intimate partner violence | WAST | X | X | X | |||||
| Parenting stress | PSI‐SF | X | X | X | X | X | X | ||
| Brief Co‐parenting Relationship Scale |
BCRS | X | |||||||
| Vulnerability for infant development | Infant development | ASQ | X | X | X | X | X | X | |
| Infant mental health | ASQ‐SE | X | |||||||
| Language development | ITC | X | |||||||
| Autism | M‐CHAT | X | |||||||
| Infant Characteristics Questionnaire |
ICQ | X | X | ||||||
| Brief Infant Toddler Social Emotional Assessment |
BITSEA | X | X | X | |||||
ACE-IQ, ACE International Questionnaire; ADHD, attention deficit-hyperactivity disorder; ASQ, Ages and Stages Questionnaire; ASQ-SE, ASQ-Social Emotional; ASRS, Adult ADHD Self-Report Scale; CAGE-AID, CAGE-Adapted to Include Drugs; DAS, Dyadic Adjustment Scale; ECBQ-VSF, Early Childhood Behaviour Questionnaire - Very Short Form; EPDS, Edinburgh Postnatal Depression Scale; GMDS, Gotland Male Depression Scale; HSUCCQ, Health Service Utilisation and Cost of Care Questionnaire; IBQ‐R, Infant Behaviour Questionnaire-revised; IHPQ, Infant Health Promotion Questionnaire; ITC, Infant–Toddler Checklist; M-CHAT, Modified Checklist for Autism in Toddlers; PCRI, Parent–Child Relationship Index; PCRI-I, PCRI-Involvement; PCRI-RO, PCRI-Role Orientation; PCRI-SP, PCRI-Satisfaction with Parenting; PPD, postpartum depression; PS, Parenting Scale; PSI-SF, Parenting Stress Index-Short Form; SCID, Structured Clinical Interview for DSM-5; SPS, Social Provisions Scale; STAI, State-Trait Anxiety Inventory; WAST, Woman Abuse Screening Tool.
Study population
Women living in Canada who recently gave birth, and their cohabitating male partners, were recruited in the immediate postpartum period via postings on social media and perinatal health services and community programmes. Women were considered for inclusion if they were <3 weeks post partum, had a singleton live birth at >33 weeks’ gestation and had a male partner (defined as a male residing with the mother and who was classified as the father) willing to participate. Both parents had to read and understand English and have access to a telephone or the internet. Women with a documented diagnosis of schizophrenia or a bipolar disorder and those with active psychosis or thoughts of suicide were excluded.
Sample size
Determination of sample size was based on the rarest expected mental health outcome group which was postpartum depression among fathers only (ie, father had postpartum depression but their partner did not). We estimated the prevalence for this group to be 9% based on best evidence indicating 11% of fathers may experience postpartum depression in the first 12 months post partum,8 acknowledging that some of the fathers captured in this estimate would have partners who also had postpartum depression, thereby requiring a downward adjustment to the estimated prevalence for fathers only. Based on the 9% prevalence for the rarest risk group, 2144 parenting couples (both mother and father recruited) would be needed to achieve 80% power. This sample size would ensure sufficient power for analyses of the same outcome in mothers, but also analyses of all other less rare outcomes.
Recruitment and enrolment
Recruitment occurred in hospital, through community outreach and self-referral via social media advertisements. In-hospital recruitment occurred at three hospitals in the Greater Toronto Area by trained research assistants who assessed parents for eligibility and obtained informed consent. Women and their partners completed the baseline questionnaire before hospital discharge. Those identified through postpartum outreach and self-referral were telephoned by a trained research assistant who obtained informed consent and administered the baseline questionnaire.
Patient and public involvement
Patients or the public were not involved in the design, conduct, reporting or dissemination plans of our research. Public health and child development experts were consulted in addition to the study team.
Data collection and measures
Background variables
Data from each parent on demographic and socioeconomic factors, obstetrical and pregnancy-related factors, lifestyle habits, history of psychiatric problems, perceived general health and health service use were collected at baseline. Demographic and socioeconomic factors included age, education level, occupation, employment status, immigrant status, extended family in Canada, length of stay in Canada, ethnic background, age at marriage and annual household income. Obstetrical and pregnancy-related factors included use of fertility treatments, mode of birth, preterm birth, birth weight and length of the infant and admission of the infant into the neonatal intensive care unit. Lifestyle habits were assessed by weight and height, alcohol use, number of cigarettes smoked per day and alcohol and recreational drug use during pregnancy. To assess history of psychiatric problems, information on depressive symptoms in a previous pregnancy, before and during the current pregnancy, anxiety symptoms during the current pregnancy, prior diagnosis of mental illness (not depression and anxiety) and family history of mental illness was collected by self-report using a yes/no checklist. General perceived health was assessed using a single-item question where 1=poor health and 5=excellent health. Finally, healthcare use was assessed using the Health Service Utilisation and Cost of Care Questionnaire.9
Exposures, mediators and outcomes
Many of the measures collected in the IMPACT cohort study will be tested as exposures and outcomes. For example, we will assess the determinants of postpartum depression or anxiety (PPD/A) among fathers, but also investigate how PPD/A among fathers influences the parenting environment and, in turn, child health and development. Both mothers and fathers completed separately all measures including child health and development.
Mental health
Postpartum depressive symptoms were assessed using the 10-item Edinburgh Postnatal Depression Scale (EPDS)10 and the depression module of the Structured Clinical Interview for DSM-5 (SCID)11 completed via telephone by trained research staff among those who screened positive during the online version. Among fathers, the Gotland Male Depression Scale (GMDS)12 was also administered. Postpartum anxious symptoms were assessed using the 20-item State-Trait Anxiety Inventory (STAI).13 All measures of depression and anxiety were administered at baseline, 3, 6, 9, 12, 18 and 24 months. The published recommended EPDS cut-off scores of >12 and >9 was used to identify depressive symptoms in a community sample of mothers10 and >9 for fathers.14 We used a score >38 on the STAI to include clinically meaningful moderate or severe anxiety symptoms for both mothers and fathers.13 An indicator for comorbidity was created by identifying those classified as depressed and anxious at the same time point. The Adult ADHD (attention deficit hyperactivity disorder) Self-Report Scale was used to screen for symptoms of inattentiveness and hyperactivity-impulsivity.15
Parenting environment
The Parent–Child Relationship Index (PCRI) was used to assess parenting behaviours and aspects of the parent–child relationship (ie, parental involvement, satisfaction, role orientation) at each time point from 3 to 24 months.16 The Parenting Stress Index-Short Form (PSI-SF), which captures stresses related to parenting, was administered at 3, 6, 9 and 12 months.17 The Parenting Scale (PS), which was assessed at 12, 18 and 24 months, was used to measure parental discipline practices.18 The Brief Coparenting Relationship Scale (BCRS) was used to measure coparenting behaviours at 9 months only.19
Family functioning
First, social support was assessed using the Social Provisions Scale (SPS), a 24-item instrument developed to assess perceived social support.20 Questions about actual support received by family and friends was assessed by questions about the presence of family living in Canada, their availability for assistance and satisfaction with support from family and friends. The marital relationship was assessed using the Dyadic Adjustment Scale (DAS), a 32-item instrument developed to assess marital quality and satisfaction.21 The CAGE-Adapted to Include Drugs (CAGE-AID) questionnaire22 was used to assess substance dependence, a 6-question instrument recommended by Health Canada as a Level I screening measure for alcohol and drugs, and the WHO 10-item Alcohol Use Disorders Identification Test (AUDIT) was used to screen for alcohol use disorders.23 Adverse childhood experiences (ACEs) were evaluated using the WHO’s ACE International Questionnaire (ACE-IQ), where ≥4 adverse childhood experiences over 8 measured categories was considered serious.24 Intimate partner violence was measured using the Woman Abuse Screening Tool (WAST), an 8-item instrument developed to screen for the presence of abuse.25 Finally, material living conditions were assessed by household size and the extent to which the family manages on current income.
Child health and development
The Ages and Stages Questionnaire, third edition (ASQ-3) was used to assess child development and behaviour between 3 and 24 months of age.26 The ASQ-Social Emotional (ASQ-SE) was used to assess socio-emotional development at 6 months of age.26 The Brief Infant–Toddler Social and Emotional Assessment (BITSEA) was used to screen for social-emotional problems and delays in social-emotional competence at 12, 18 and 24 months of age.27 The Infant–Toddler Checklist (ITC) was used to assess child language use at 18 months of age.28 The Modified Checklist for Autism in Toddlers (M-CHAT) screened for symptoms of autism spectrum disorders at 24 months of age.29 The Infant Characteristic Questionnaire (ICQ-R)30 was used to assess infant temperament at 6 and 24 months of age. The Infant Behaviour Questionnaire-revised Very Short Form (IBQ-VSF)30 was used to assess infant temperament at 12 and 24 months of age. Early Childhood Behaviour Questionnaire (ECBQ),31 which measures the three higher-order temperament domains of surgency, negative affect and effortful control, was administered at 24 months of age. Finally, infant health promotion was assessed using a variety of measures, including feeding (eg, breastfeeding duration and exclusivity), sleep behaviours (eg, sleep position and location), immunisation, stimulating environment (eg, reading, play outdoors), screen use and safety behaviours (eg, smoke-free home).
Statistical analysis
The data reported in the current paper was analysed using descriptive statistics, including measures of central tendency and variation, and frequency counts and percentages. To provide context to the sociodemographic composition of the IMPACT sample, comparisons were made with publicly available 2016 Canadian census data. When data were compared between mothers and fathers, χ2 tests were used for frequency counts and t-tests for continuous variables. Future analyses planned to address the research objectives of IMPACT will take into account the longitudinal design and dyadic relationship between mothers and fathers. Multiple statistical methods will be employed including: (1) growth curve modelling to determine trajectories of change in outcomes over time, predictors of trajectories and inter-relationships among trajectories; (2) structural equation modelling and path analysis to evaluate mediating mechanisms of change over time; (3) moderation (interaction) models to examine factors that potentiate or attenuate the relation between constructs; (4) mixture modelling to identify unique subpopulations (ie, profiles) of mothers and fathers with specific clusters of traits and behaviours; and (5) dyadic data analysis to evaluate the influence of each dyad member on the other and of the dyad itself on study outcomes (eg, child development).
Findings to date
A total of 3217 women and their cohabitating male partners were recruited into the study at baseline (figure 1). The follow-up response rates were high for both mothers and fathers: at the second wave (3 months) 94% of mothers and 89% of fathers completed at a minimum >50% of the follow-up questionnaire. By 12 months, 91% of mothers and 82% of fathers and at 24 months, the end of the observation period, 88% of mothers and 78% of fathers completed at a minimum >50% of the follow-up questionnaire with the majority completing all of the measures and receiving a token of appreciation gift card. REDCap was developed so that participants could not move forward in the follow-up questionnaire without answering all questions on the current webpage. This minimised skipped items and missing data. Participants who did not complete the follow-up questionnaire were contacted by highly trained research assistants who provided support to finish the questionnaire and receive their token of appreciation gift card.
Figure 1.
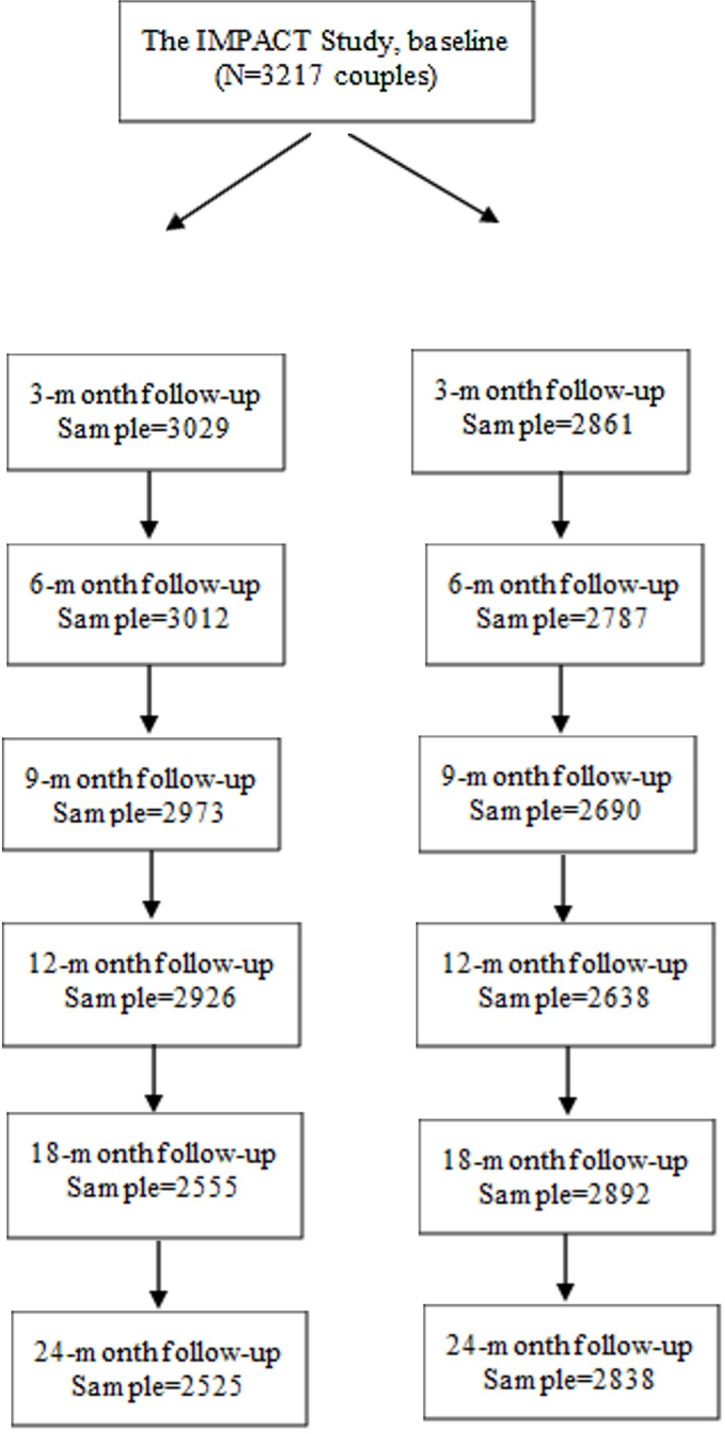
Flow chart for the IMPACT study. Left side of flow chart represents follow-up rates for mothers and the right side represents follow-up rates for fathers.
Baseline characteristics of the IMPACT sample compared with the Canadian population
At baseline, the mean age of mothers was 31.9±4.2 years, which is slightly older than the mean age of first-time mothers in Canada of 29.2 (table 2).32 Fathers were significantly older than mothers (p<0.001) with a mean age of 33.8±5.0 years, which is highly consistent with Canadian census data showing that fathers are generally older than mothers, having their first child at an average age of 33.7.32 Less than one out of five couples were unmarried (16.4%), which is consistent with the number of couples living together without being married (ie, common-law relationship)33 in the Canadian population. Couples had been together for an average of 7.6 years (SD=3.9). The most common household composition was two adults living with one child (57%).
Table 2.
Baseline sociodemographic characteristics of study participants
| Mothers (n=3217) | Fathers (n=3217) | P value | |
| n (%) | n (%) | ||
| Age—mean (SD) | 31.9 (4.2) | 33.8 (5.0) | <0.001 |
| Education level | <0.001 | ||
| Elementary | 19 (0.6) | 41 (1.3) | |
| High school | 247 (7.7) | 513 (16.0) | |
| College/trade school | 607 (18.9) | 891 (27.8) | |
| University undergraduate degree | 1372 (42.7) | 1143 (35.6) | |
| University graduate degree | 969 (30.2) | 622 (19.4) | |
| Employment status | <0.001 | ||
| Part-time | 411 (12.8) | 120 (3.7) | |
| Full-time | 2220 (69.1) | 2797 (87.0) | |
| Not employed | 326 (10.2) | 71 (2.2) | |
| Other | 256 (8.0) | 227 (7.7) | |
| Occupation | <0.001 | ||
| Management, business, finance and administration | 795 (24.8) | 757 (23.6) | |
| Sciences, health, education, law, social/community/government services | 1535 (47.8) | 1154 (35.9) | |
| Sales, service, trades, transport, equipment operators, manufacturing | 263 (8.2) | 854 (26.6) | |
| Other | 618 (19.3) | 447 (13.9) | |
| Immigrant | 680 (21.2) | 789 (24.6) | 0.001 |
| No family in Canada | 227 (7.1) | 302 (9.4) | <0.001 |
| Ethnic background | 0.042 | ||
| European | 1993 (62.0) | 1990 (61.9) | |
| East Asian | 250 (7.8) | 192 (6.0) | |
| South Asian | 206 (6.4) | 199 (6.2) | |
| Latin American/Caribbean | 142 (4.4) | 181 (5.6) | |
| South East Asian | 82 (2.6) | 77 (2.4) | |
| North African/West | 64 (2.0) | 77 (2.4) | |
| Sub-Saharan African | 42 (1.3) | 58 (2.4) | |
| Indigenous | 89 (2.8) | 100 (3.1) | |
| Other/unknown | 345 (10.7) | 337 (10.5) |
Socioeconomic status
The largest share of couples had a family income between $C100 000 and $C149 999 (32.4%). The average Canadian income of couples with children was $C126 200 in 2015.34 Just over 1 in 5 couples had an annual family income of at least $C150 000 (20.9%). More than 1 in 10 families (12.8%) would be considered low-income earning less than $C50 000 annually, which is consistent with the proportion of low-income couple families in Canadian census data.34 Approximately one-quarter of mothers reported that the annual family income was difficult to manage all or some of the time (23.4%).
Fewer fathers than mothers had higher levels of education (p<0.001), which reflects the general Canadian population;35 however, with over half (55%) of fathers and nearly three-quarters (73%) of mothers had completed a university degree. Thus, the educational achievement of the IMPACT sample is higher than the Canadian population of working-aged men and women.35 Consistent with Canadian census data, 81% of mothers were employed prior to giving birth36 and had a lower rate of labour market participation than father (p<0.001). Occupational statuses varied between mothers and fathers (p<0.001). Notably, more fathers (26.6%) than mothers (8.2%) worked in occupational groups associated with precarious or potentially hazardous work conditions (ie, sales, service, manufacturing, trades), while more mothers (47.8%) than fathers (35.9%) worked in areas like education, healthcare, law and government.
Immigrant status and ethnic background
Just over 1 in 5 mothers (21.2%) and fathers (24.6%) were born outside of Canada, which is consistent with the 21.6% of Canadians who are immigrants.37 Mothers and fathers born outside Canada had been living in the country for a median of 12 years. Significantly more fathers than mothers were born outside of Canada (p=0.001). Less than 1 in 10 mothers (7.1%) and fathers (9.4%) reported not having any family in Canada, with fathers reporting this more often (p<0.001). Approximately 38% of mothers and fathers reported an ancestry other than European, which is higher than the 22.3% of Canadians who are visible minorities but comparable to the percentage of visible minorities living in Toronto of 39%.37 The most frequently reported region of origin was East Asia (fathers: 6.0%; mothers: 7.8%) and South Asia (fathers: 6.2%; mothers: 6.4%), which is similar to the makeup of the Canadian population.37 Exactly 3.1% of fathers and 2.8% mothers reported being Indigenous, which is slightly less than the 4.9% of the Canadian population who identify as Indigenous.38 See table 2 for a full description of the socio-demographic characteristics of the IMPACT sample.
Obstetrical and pregnancy-related factors
Two-thirds of mothers had a vaginal delivery (65.8%) and a quarter had a Caesarean section (24.9%) with the balance (9.3%) reporting a vaginal birth with some type of assistance (eg, forceps). The mean gestational age of the infant born was 39.5 weeks±1.4; 2.8% were born before 37 weeks. Most infants (95.1%) were born at a normal weight between 2500 and 4500 g; 2.3% had a low birth weight and 2.5% had a high birth weight. Less than 1 in 10 mothers had their infant taken to the neonatal intensive care unit (8.8%). The majority of women practiced skin-to-skin contact with their infant in the immediate hour after birth (94.6%). Exactly 91.2% of women planned to exclusively breast feed prior to giving birth, and while 96.5% reported they were breast feeding at baseline within the first 3 weeks postpartum, just under 78% were doing so exclusively.
More fathers were overweight (44.3%) and obese (19.8%) based on body mass index than mothers (22.4% and 15.8%, respectively) prior to pregnancy (p<0.001). During their partner’s pregnancy, just over 1 in 10 fathers reported any smoking (11.9%), three-quarters said they drank any amount of alcohol (75.9%) and more than 1 in 20 reported substance use (7.4%). As expected, fathers reported these behaviours at a greater frequency than their partner (all p<0.001). Still, just under 1 in 6 mothers reported drinking any amount during pregnancy (15.1%). Approximately 1% and 3% reported any substance use or any smoking, respectively, while pregnant. Based on self-report data, depression prior to the pregnancy was reported in a quarter of mothers (26.3%) and 1 in 5 fathers (20.0%, p<0.001). One in 10 women felt depressive symptoms during pregnancy (9.7%) and just less than 1 in 6 had high anxiety symptoms (15.4%). While significantly fewer (p<0.001), 1 in 20 men felt depressive symptoms during their partner’s pregnancy and 1 in 10 reported high anxiety (10.1%). More mothers (9.7%) than fathers (6.1%) reported a prior mental health diagnosis other than depression or anxiety (p<0.001). More mothers also reported a family history of mental illness (43.6%) than fathers (35.0%, p<0.001). See table 3 for a description of lifestyle habits and mental health history among mothers and fathers.
Table 3.
Baseline lifestyle habits and mental health history
| Mothers (n=3217) | Fathers (n=3217) | P value | |
| n (%) | n (%) | ||
| BMI prior to pregnancy | <0.001 | ||
| Underweight (BMI <18.5) | 125 (3.9) | 32 (1.0) | |
| Normal weight (BMI ≥18.5 and <25) | 1837 (57.8) | 1106 (34.9) | |
| Overweight (BMI ≥25 and <30) | 712 (22.4) | 1404 (44.3) | |
| Obese (BMI ≥30) | 503 (15.8) | 626 (19.8) | |
| Any smoking during pregnancy | 109 (3.4) | 381 (11.9) | <0.001 |
| Any drinking during pregnancy | 484 (15.1) | 2438 (75.9) | <0.001 |
| Any substance use during pregnancy | 40 (1.2) | 237 (7.4) | <0.001 |
| Depression prior to this pregnancy | 845 (26.3) | 643 (20.0) | <0.001 |
| Felt depressed during pregnancy | 312 (9.7) | 160 (5.0) | <0.001 |
| Felt highly anxious during pregnancy | 494 (15.4) | 324 (10.1) | <0.001 |
| Prior diagnosis of mental illness (not depression and anxiety) | 314 (9.8) | 197 (6.1) | <0.001 |
| Family history of depression or other mental illness | 1402 (43.6) | 1124 (35.0) | <0.001 |
BMI, body mass index.
Strengths and limitations
The current prospective cohort study has many strengths, with the strongest being the recruitment of cohabiting parental dyads—both mothers and fathers. To date, paternal postpartum depression and anxiety, as well as parental comorbid depression and/or anxiety, have not been well studied. This Canadian-wide study significantly adds to this paucity of literature. Furthermore, as little is known on the role of paternal mental disorders in child development, this study can provide important insight into this relationship, including how paternal mental health difficulties compare to maternal difficulties. Another strength is the longitudinal design, with the participants followed-up every 3 months during the first year of post partum, and every 6 months during the second year of post partum. Moreover, this study had low attrition, with follow-ups rated being very high, ranging between 88% and 94% for mothers and between 78% and 89% for fathers. The sample size is large and therefore adequately powered to detect small differences and rare outcomes. The final strength was the use of well-validated tools. In addition to using the EPDS21 and STAI22 to screen parents for depression and anxiety, the SCID23 was used to screen parents for mental disorders and GMDS24 was used to screen fathers for depression. Multiple validated tools including ASQ,25 ASQ-SE,26 BITSEA, ITC for language development27 and M-CHAT28 were used to assess child development by both parents independently, thus providing a high-level summary of children’s development across a number of critical domains.
While this study has strengths, there are some limitations that must be acknowledged. While the overall IMPACT sample is very representative of the Canadian population, it does slightly over-represent higher-educated and higher-income individuals. This is not uncommon for survey research.39 40 Importantly, our sample was heterogeneous in that 21.2% of mothers and 24.6% of fathers were not born in Canada and had immigrant status. The sample included participant self-selection (by responding to advertisements), which may have resulted in bias towards a healthier population overall. The measures were primarily self-report, so future work could consider the use of objective measures of parent and child outcomes in a subgroup of participants. Finally, this study focused on two-parent families where one identified as female and the other as male. This limits generalisability to non-normative families and future work is needed to explore these relations in single and same-sex/non-binary families or those with more diverse family structures.
Supplementary Material
Footnotes
Twitter: @justinedol
Contributors: C-LD is the guarantor and takes responsibility for the work and conduct of the study. She has access to the data and controlled the decision to publish, the integrity of the data and the accuracy of the data analysis. Concept and design: C-LD, SV, SG, HB, SB and FM. Acquisition, analysis or interpretation of data: FM, KF-H, RS, SB and C-LD. Drafting of the manuscript: C-LD, JD, SB and FM. Critical revision of the manuscript for important intellectual content was conducted by C-LD, SV, SG, HB, SB, JD, MW, KF-H, RS and FM; who each author meet the full authorship criteria.
Funding: This study was funded by the Canadian Institutes of Health Research (Grant # #MOP-130383). The sponsor had no role in the design, analysis, interpretation or publication of this study.
Competing interests: SG reports personal fees from AbbVie outside the submitted work. No other authors have competing interests.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request. Data are available for collaboration with permission from C-LD.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by University of Toronto Research Ethics Board (#29655). Participants gave informed consent to participate in the study before taking part.
References
- 1.Davé S, Petersen I, Sherr L, et al. Incidence of maternal and paternal depression in primary care: a cohort study using a primary care database. Arch Pediatr Adolesc Med 2010;164:1038–44. 10.1001/archpediatrics.2010.184 [DOI] [PubMed] [Google Scholar]
- 2.Dennis CL, Falah-Hassani K, Shiri R. Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br J Psychiatry 2017;210:315–23. 10.1192/bjp.bp.116.187179 [DOI] [PubMed] [Google Scholar]
- 3.Committee on Depression and the Healthy Development of Children PP . Depression in parents, parenting, and children: opportunities to improve identification, treatment, and prevention. Washington, D.C: National Research Council; Institute of Medicine, 2009. [Google Scholar]
- 4.Hops H, Biglan A, Sherman L, et al. Home observations of family interactions of depressed women. J Consult Clin Psychol 1987;55:341–6. 10.1037//0022-006x.55.3.341 [DOI] [PubMed] [Google Scholar]
- 5.Mezulis AH, Hyde JS, Clark R. Father involvement moderates the effect of maternal depression during a child’s infancy on child behavior problems in kindergarten. J Fam Psychol 2004;18:575–88. 10.1037/0893-3200.18.4.575 [DOI] [PubMed] [Google Scholar]
- 6.Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev 1999;106:458–90. 10.1037/0033-295x.106.3.458 [DOI] [PubMed] [Google Scholar]
- 7.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (redcap) -- a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paulson JF, Bazemore SD. Prenatal and postpartum depression in fathers and its association with maternal depression: a meta-analysis. JAMA 2010;303:1961–9. 10.1001/jama.2010.605 [DOI] [PubMed] [Google Scholar]
- 9.Brown G. Health service utilization and cost of care questionnaire. Hamilton, ON: Health and Social Service Utilization Research Unit, McMaster University, 2001. [Google Scholar]
- 10.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry 1987;150:782–6. 10.1192/bjp.150.6.782 [DOI] [PubMed] [Google Scholar]
- 11.Spitzer RL, Williams JB, Gibbon M, et al. The structured clinical interview for DSM-III-R (SCID). I: history, rationale, and description. Arch Gen Psychiatry 1992;49:624–9. 10.1001/archpsyc.1992.01820080032005 [DOI] [PubMed] [Google Scholar]
- 12.Sigurdsson B, Palsson SP, Aevarsson O, et al. Validity of gotland male depression scale for male depression in a community study: the sudurnesjamenn study. J Affect Disord 2015;173:81–9. 10.1016/j.jad.2014.10.065 [DOI] [PubMed] [Google Scholar]
- 13.Spielberger CD. STAI manual for the state-trait anxiety inventory. Palo Alto, CA: Consulting Psychologists Press, 1970. [Google Scholar]
- 14.Matthey S, Barnett B, Kavanagh DJ, et al. Validation of the edinburgh postnatal depression scale for men, and comparison of item endorsement with their partners. J Affect Disord 2001;64:175–84. 10.1016/s0165-0327(00)00236-6 [DOI] [PubMed] [Google Scholar]
- 15.Kessler RC, Adler L, Ames M, et al. The World Health Organization adult ADHD self-report scale (ASRS). Psychol Med 2005;35:245–56. 10.1017/s0033291704002892 [DOI] [PubMed] [Google Scholar]
- 16.Gerard AB. Parent-child relationship inventory (PCRI) manual. Los Angeles: WPS, 1994. [Google Scholar]
- 17.Abidin RR. Parenting stress index: professional manual. 3rd ed. Lutz, FL: Psychological Assessment Resources, Inc, 1995. [Google Scholar]
- 18.Arnold DS, O’Leary SG, Wolff LS, et al. The parenting scale: a measure of dysfunctional parenting in discipline situations. Psychol Assess 1993;5:137–44. 10.1037/1040-3590.5.2.137 [DOI] [Google Scholar]
- 19.Feinberg ME, Brown LD, Kan ML. A multi-domain self-report measure of coparenting. Parent Sci Pract 2012;12:1–21. 10.1080/15295192.2012.638870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cutrona C, Russell D. The provisions of social relationships and adaptation to stress. In: Jones W, Perlman D, eds. Advances in personal relationships. Greenwich, CT: JAI Press, 1987: 37–67. [Google Scholar]
- 21.Spanier GB. Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. J Marriage Fam 1976;38:15. 10.2307/350547 [DOI] [Google Scholar]
- 22.Brown RL, Leonard T, Saunders LA, et al. The prevalence and detection of substance use disorders among inpatients ages 18 to 49: an opportunity for prevention. Prev Med 1998;27:101–10. 10.1006/pmed.1997.0250 [DOI] [PubMed] [Google Scholar]
- 23.Babor T, de la Fuente J, Saunders J, et al. AUDIT. The alcohol use disorders identification test. Guidelines for use in primary health care. Geneva; 1992. [Google Scholar]
- 24.World Health Organization . Adverse childhood experiences international questionnaire (ACE-IQ). 2020. Available: https://www.who.int/publications/m/item/adverse-childhood-experiences-international-questionnaire-(ace-iq) [Accessed 15 Jun 2021].
- 25.Brown JB, Lent B, Brett PJ, et al. Development of the woman abuse screening tool for use in family practice. Fam Med 1996;28:422–8. [PubMed] [Google Scholar]
- 26.Bricker D, Squires J. Ages and stages questionnaire. Third edition. Baltimore, MD: Brookes Publishing, 2010. [Google Scholar]
- 27.Briggs-Gowan MJ, Carter AS. Brief infant-toddler social and emotional assessment (BITSEA) mannual, version 2.0. New Haven, CT: Yale University, 2002. [Google Scholar]
- 28.Wetherby AM, Brosnan-Maddox S, Peace V, et al. Validation of the infant-toddler checklist as a broadband screener for autism spectrum disorders from 9 to 24 months of age. Autism 2008;12:487–511. 10.1177/1362361308094501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Robins DL, Casagrande K, Barton M, et al. Validation of the modified checklist for autism in toddlers, revised with follow-up (M-CHAT-R/F). Pediatrics 2014;133:37–45. 10.1542/peds.2013-1813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bates JE, Freeland CA, Lounsbury ML. Measurement of infant difficultness. Child Dev 1979;50:794–803. 10.2307/1128946 [DOI] [PubMed] [Google Scholar]
- 31.Putnam SP, Gartstein MA, Rothbart MK. Measurement of fine-grained aspects of toddler temperament: the early childhood behavior questionnaire. Infant Behav Dev 2006;29:386–401. 10.1016/j.infbeh.2006.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Statistics Canada . Fertility: overview, 2012 to 2016. 2018. Available: https://www150.statcan.gc.ca/n1/pub/91-209-x/2018001/article/54956-eng.htm [Accessed 13 Jul 2021].
- 33.Statistics Canada . Portrait of families and living arrangements in canada. 2018. Available: https://www12.statcan.gc.ca/census-recensement/2011/as-sa/98-312-x/98-312-x2011001-eng.cfm [Accessed 13 Jul 2021].
- 34.Statistics Canada . The economic well-being of women in canada. 2018. Available: https://www150.statcan.gc.ca/n1/pub/89-503-x/2015001/article/54930-eng.htm [Accessed 13 Jul 2021].
- 35.Statistics Canada . Women and education: qualifications, skills and technology. 2016. Available: https://www150.statcan.gc.ca/n1/pub/89-503-x/2015001/article/14640-eng.htm [Accessed 13 Jul 2021].
- 36.Moyser M. Women and paid work. 2017. Available: https://www150.statcan.gc.ca/n1/pub/89-503-x/2015001/article/14694-eng.htm [Accessed 13 Jul 2021].
- 37.Statistics Canada . Focus on geography series, 2016 census - canada. 2016. Available: https://www12.statcan.gc.ca/census-recensement/2016/as-sa/fogs-spg/Facts-can-eng.cfm?Lang=Eng&GK=CAN&GC=01&TOPIC=7 [Accessed 13 Jul 2021].
- 38.Statistics Canada . Aboriginal peoples in canada: key results from the 2016 census. 2017. Available: https://www150.statcan.gc.ca/n1/daily-quotidien/171025/dq171025a-eng.htm?indid=14430-1&indgeo=0 [Accessed 13 Jul 2021].
- 39.Grewenig E, Lergetporer P, Simon L, et al. Can online surveys represent the entire population?; 2018.
- 40.Bethlehem J. Can we make official statistics with self-selection web surveys? Proc Stat Canada Symp 2008; 2009. Available: https://www150.statcan.gc.ca/n1/pub/11-522-x/2008000/article/10989-eng.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request. Data are available for collaboration with permission from C-LD.


