Abstract
Social and economic inequality are chronic stressors that continually erode the mental and physical health of marginalized groups, undermining overall societal resilience. In this comprehensive review, we synthesize evidence of greater increases in mental health symptoms during the COVID-19 pandemic among socially or economically marginalized groups in the United States, including (a) people who are low-income or experiencing homelessness, (b) racial and ethnic minorities, (c) women and LGBTQ+ communities, (d) immigrants and migrants, (e) children and people with a history of childhood adversity, and (f) the socially isolated and lonely. Based on this evidence, we propose that reducing social and economic inequality would promote population mental health and societal resilience to future crises. Specifically, we propose concrete, actionable recommendations for policy, intervention, and practice that would bolster five “pillars” of societal resilience: (1) economic safety and equity, (2) accessible healthcare, including mental health services, (3) combating racial injustice and promoting respect for diversity, equity, and inclusion, (4) child and family protection services, and (5) social cohesion. Although the recent pandemic exposed and accentuated steep inequalities within our society, efforts to rebuild offer the opportunity to re-envision societal resilience and policy to reduce multiple forms of inequality for our collective benefit.
Keywords: mental health, COVID-19, resilience, social determinants, intersectionality
The SARS-CoV-2 (COVID-19) pandemic is an unprecedented global public health crisis, entailing the loss of 6,231,018 lives and infection of more than 506 million patients worldwide as of April 20, 2022 (World Health Organization, 2022). Social interactions changed profoundly due to stay-at-home orders and curfews, travel restrictions, social distancing norms, school closures, and shifts to remote work. The pandemic also triggered a deep global economic recession (World Bank, 2020), which reverberated across the world and was also reflected in the United States economy. The National Bureau of Economic Research reported that the U.S. witnessed its largest economic contraction during the pandemic since 1947, when record-keeping began (NBER, 2020). During this pandemic, unemployment rates spiked dramatically and deepened existing inequalities. Those most affected by unemployment were women, racial/ethnic minorities, low-wage workers, and workers with lower educational attainment (Stevenson, 2020). Of concern, families with children experienced greater income losses and food shortages than those without children (Monte et al, 2020). For instance, the rate of food insecurity doubled in the U.S. during the pandemic, but tripled among families with children (Schanzenbach & Pitts, 2020). These health, social, and economic vicissitudes exacted a major toll on population mental health, with a disproportionate burden of these effects falling on the most vulnerable groups in society (Condon et al., 2020; Czeisler et al., 2020; Ettman et al., 2020; Purtle, 2020). We aim to highlight these vulnerable groups, and this review has three major goals.
Our first goal is to summarize evidence and statistics characterizing the social determinants of mental health disparities during COVID-19 in the United States. Specifically, we summarize evidence of greater increases in mental health problems during the pandemic among socially or economically marginalized groups in the U.S., including (a) people with low income or experiencing homelessness, (b) racial and ethnic minorities, (c) women and lesbian, gay, bisexual, transgender, queer, and questioning (LGBTQ+) communities, (d) immigrants and migrants, (e) children and people with a history of childhood adversity, and (f) the socially isolated and lonely. We also highlight how those who belong to multiple vulnerable groups experienced more detrimental impacts.
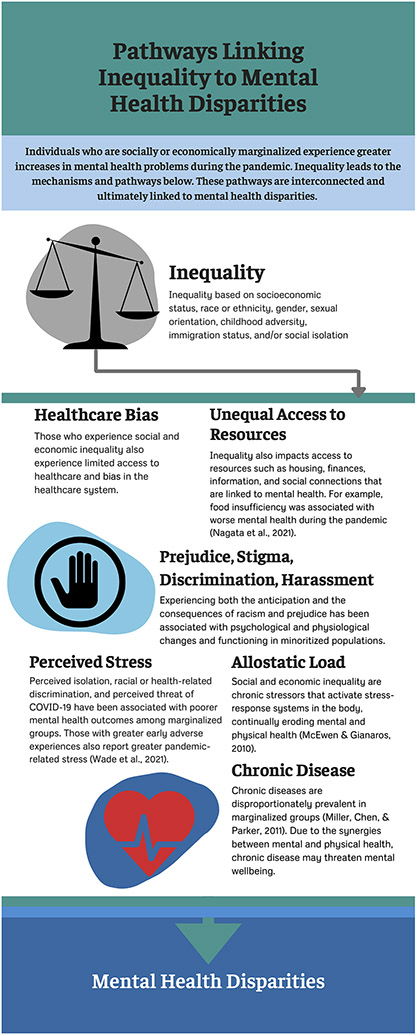
The second goal of this review is to discuss possible mechanisms explaining these disparities by linking current data from COVID-19 to existing theories (e.g., theory of fundamental causes, allostatic load theory, early-life stress sensitization theory) and prior evidence on health disparities, stress, or resilience. For each marginalized group, we first describe the evidence on mental health disparities during COVID-19, followed by a discussion of possible mechanisms contributing to these disparities. Figure 1 depicts a summary of mechanisms and pathways that may have contributed to the compounding of stress and mental health inequities for these groups during this pandemic.
Figure 1.
Infographic on mechanisms and pathways linking social and economic inequality to mental health disparities surveyed in this review.
Lastly, our third goal is to propose concrete, actionable recommendations for policy, intervention, and practice that would reduce existing mental health disparities and prepare us for future calamities. We propose a new framework for promoting societal resilience that is centered on five “pillars” considered essential to societal resilience to future disasters: (1) economic safety and equity; (2) accessible healthcare (including mental health services); (3) combating racial injustice and promoting respect for diversity, equity, and inclusion; (4) child and family protection services; and (5) social cohesion. Because prior studies on mental health disparities tend to document their existence but stop short of suggesting concrete solutions, we aimed to advance this literature by connecting each section on risk to a corresponding set of solutions for promoting societal resilience. These constructive recommendations can be used by policymakers and practitioners to begin addressing mental health disparities through policy changes and intervention programs that can have tangible benefits for marginalized groups.
The scope of the review included peer-reviewed empirical studies from the United States published up to July, 2021 focused on mental health, COVID-19, and the marginalized populations of interest we specified a priori based on the broader health disparities literature (Krieger, 2020; Phelan et al., 2010; Williams et al., 2019). We focused primarily on national and nationally-representative studies as the main source of pandemic evidence to prioritize generalizability, but also drew on smaller studies or pre-pandemic research when discussing possible mechanisms and solutions, or when national studies were not available. We also restricted our review to studies from the United States as a case study, given international differences in responses to the pandemic and the need to tailor policy recommendations, but draw parallels with other countries where possible.
Low Income and Homelessness
Evidence on Disparities during COVID-19
The COVID-19 pandemic threatened the physical, social, and emotional wellbeing of populations worldwide, and can be considered a traumatic event given its life-threatening, disruptive, and unpredictable nature (Goldmann & Galea, 2014).
Consistent with this pattern, there was an overall increase in the prevalence of mental health problems during the pandemic compared to previous periods, but these mental health consequences were stratified based on socioeconomic status (SES). For instance, pronounced spikes in depression symptom prevalence were noted during the pandemic, with some estimates suggesting a 3-fold increase compared to pre-pandemic levels (Ettman et al., 2020). However, these impacts were unequally distributed by SES, with higher levels of depression symptoms affecting those who had lower income, less than $5,000 in savings, and who experienced more stressors (Ettman et al., 2020). Converging evidence supporting low income as a risk factor comes from the nationally representative Understanding America Study of 6,901 adults. In this panel study, participants whose income fell below the federal poverty level had 4.58 times higher odds of developing significant distress during the pandemic compared to those above the poverty level (Riehm et al., 2021). Furthermore, analyses from 63,674 participants of the U.S. Census Household Pulse Survey conducted in 2020 revealed that food insufficiency was associated with worse mental health during the pandemic, particularly symptoms of anxiety and depression (Nagata et al., 2021). However, the receipt of food aid was associated with an attenuated effect of the pandemic on these symptoms (Nagata et al., 2021), suggesting policy solutions that could partially alleviate stress exposure through food aid programs.
People experiencing homelessness or unstable housing were particularly vulnerable during COVID-19, suffering higher rates of infection and illness than the general population, and exhibiting high rates of comorbidity with psychiatric illness and substance use (Fuchs et al., 2021). Adolescent and young adult substance users who were homeless were particularly affected, with one study estimating that 16%-28% reported increased use of alcohol, tobacco, and marijuana after the onset of the pandemic (Tucker et al., 2020). With shelter in place mandates and economic instability limiting residential mobility during the first year of the COVID-19 pandemic, incidences of intimate partner violence increased, and victims were placed at a greater risk for experiencing homelessness (Goodsmith et al., 2021). Future disaster-preparedness programs should address the needs of groups vulnerable to housing instability. Hotel-based isolation and quarantine intervention programs such as Project Roomkey implemented across California (Goodsmith et al., 2021) and the isolation/quarantine program implemented in San Francisco, California, provided housing and services to these groups, reducing rates of infection and leading to behavioral stabilization and improvement on average (Fuchs et al., 2021). The State of California utilized CARES Act funding and followed up these efforts with Project HomeKey, a program that provided funding to local agencies to purchase and repurpose housing (e.g., hotels, motels) to provide housing to Californians experiencing homelessness. These interventions suggest viable strategies for managing and reducing mental health problems among those experiencing homelessness, and could serve as a starting point for providing stable housing, service delivery, and social reintegration support.
Possible Mechanisms
Although the COVID-19 pandemic is unique in the severity of its health, social, and economic disruptions, we propose that its disproportionate impact on lower-SES groups was largely predictable based on existing sociological and psychobiological theories. The sociological theory of fundamental causes, originally formulated by Link and Phelan (1995), proposes that socioeconomic status (SES) “embodies an array of resources, such as money, knowledge, prestige, power, and beneficial social connections that protect health no matter what mechanisms are relevant at any given time” (Phelan et al., 2010, p. S28). This theory and accumulating evidence in support of this theory explains the emergence of socioeconomic disparities in health for numerous health outcomes, over different time periods, and across countries. Because the “flexible resources” (Phelan et al., 2010) provided by SES can circumvent health risks in any given context, they constitute fundamental causes of health disparities and thus apply equally well to patterns observed during the pandemic. In the context of the pandemic, high SES provided greater protection against wage losses and more opportunities for remote work, as well as greater flexibility to avoid public transportation and crowding (Brough et al., 2021), to name just a few protections. In turn, this flexibility protected higher SES people against escalating mental health problems.
Psychobiological theories of stress such as the allostatic load model (McEwen & Gianaros, 2010) also provide plausible biological mechanisms for explaining socioeconomic disparities in the effects of the pandemic. Because social and economic inequality function as chronic stressors that activate stress-response systems such as the hypothalamic-pituitary-adrenal (HPA) axis, autonomic nervous system, and immune system, they can continually erode the mental and physical health of socially and economically marginalized groups (Blair & Raver, 2016; McEwen & Gianaros, 2010). Thus, these groups can be expected to experience exacerbated neurobiological stress responses during new crises like the pandemic.
For low-income groups, mental health deterioration and higher rates of COVID-19 morbidity and mortality were inextricably linked to pre-existing chronic diseases that are known to be more prevalent among socially and economically marginalized groups, such as cardiovascular, metabolic, and immune conditions (Miller, Chen, & Parker, 2011). Thus, social inequality can create a worsening spiral of mutually reinforcing mental and physical health problems (Hostinar, Nusslock, & Miller, 2018). Due to these synergies between mental and physical health, chronic disease morbidity represents an ongoing barrier to the resilience of low-income people, as it threatens both physical and mental wellbeing and it constrains one’s ability to cope with new crises. This may also undermine societal resilience, a point we develop further in our concluding section on societal resilience.
Racial and Ethnic Inequality
Previous work has shown that socioeconomic factors alone do not fully account for health disparities, and racism is another major contributing factor (Williams, 1997). Both structural and cultural racism negatively exacerbate racial/ethnic disparities in mental and physical health outcomes (Williams et al., 2019). These disparities exist in a broader context of structural racism. Structural racism consists of differential treatment and access to resources among racial/ethnic minorities across multiple levels and systems in society – housing, education, employment, criminal justice, and healthcare (Reskin, 2012; Williams et al., 2019). These systems are interconnected and upheld by society, reinforcing inequality. Police brutality, an example of structural racism, set the stage for a year of racial reckoning in 2020, following the murder of George Floyd (New York Times, 2021). The increased awareness of systemic inequities that African Americans have long been confronting led to international protests and calls to action to promote antiracist policies to reduce health disparities from many organizations, including the American Heart Association (Churchwell et al., 2020). These events exposed the ongoing systemic racism and police brutality faced by minoritized populations, which are compounded by the effects of a global pandemic that disproportionately affected disenfranchised groups.
Racially minoritized groups also face cultural racism, which consists of an internalized community-level ideology that reinforces structural racism and generates prejudice, bias, and stereotypes (Williams et al., 2019). Overall, these forms of racism have been linked to heightened stress among racialized groups, both before and during the pandemic (McKnight-Eily et al., 2021; Williams et al., 2019). Thus, it has been proposed that racism is also a fundamental cause of health inequalities (Williams, 1997), akin to SES (Link & Phelan, 1995).
Evidence on Disparities during COVID-19
Evidence supports an increase in racial disparities in mental and physical health during the COVID-19 pandemic (Cooper & Williams, 2020; Selden & Berdahl, 2020). Some of these disparities can be traced back to pre-pandemic structural factors such as residential segregation, which can reduce access to healthcare and expose racial/ethnic minority groups to more acute and chronic stressors (Kramer & Hogue, 2009; White & Borrell, 2011).
During the COVID-19 pandemic, the effects of racism and discrimination on mental health were exacerbated by the disproportionate impact of the pandemic and related crises on racial/ethnic minority groups. Specifically, people of color had a higher risk of infection and death, due to the greater likelihood of being employed as essential workers, with Black workers most represented in high-risk occupations (Hawkins, 2020; Purtle, 2020). Further, Black individuals at risk for severe illness are more likely to live in households with healthcare workers (Selden & Berdahl, 2020). During COVID-19, frontline healthcare workers experience heightened physiological distress and mental health challenges (Kinman et al., 2020; Lai et al., 2020). In addition, the devastating job losses and financial insecurity during the pandemic disproportionately affected racial and ethnic minorities (Purtle, 2020), specifically Black and Latina women (Gould and Wilson, 2020). The pandemic has also had a damaging effect on racial/ethnic minorities' mental health. In a CDC report from June 2020, the percentage of respondents who had seriously considered suicide was significantly higher in Hispanic and Black individuals compared to other groups (Czeisler et al., 2020). During the height of the pandemic in 2020 in Maryland, Black individuals’ suicide rates doubled compared to previous years (Bray et al., 2020). Because COVID-19 mortality rates were higher for minoritized groups, this resulted in elevated rates of grief and related mental health symptoms for family members of individuals who lost their lives due to COVID (Purtle, 2020).
In addition to experiencing greater economic stress during the pandemic, racial/ethnic minorities are at a greater risk of developing severe cases or dying of COVID-19, which adds to pandemic-related stress (Simon et al., 2020). Racial/ethnic minority groups are more likely to experience psychosocial stress during the pandemic, particularly in Hispanic/Latino individuals (McKnight-Eily et al., 2021). Social vulnerability and exclusion, more likely to be experienced by African Americans, have also been found to be associated with an increased COVID-19 death rate (Kim & Bostwick, 2020). Racial disparities in vulnerability for severe COVID-19 illness emerge by middle age, and disparities in hospitalizations are greater than expected by pre-existing conditions alone (Wiemers et al., 2020). Structural racism leads to these disparities in COVID-19 illness. A recent study found that increases in COVID-19 cases and deaths were greater in areas with residential segregation, and this relation was amplified by income inequality (Yu et al., 2021). Furthermore, life expectancy for Black and Latino populations is expected to be reduced nearly 3 to 4 times more than the reduction in life expectancy for White individuals after the pandemic. The COVID-19 pandemic has eliminated the gains made in recent years to close the Black-White life expectancy gap (Andrasfay & Goldman, 2021). While communities grieve in the wake of these COVID-19 deaths, research shows another “wave” of the pandemic: a crisis in mental health, which is disproportionately impacting Black and Hispanic individuals (Simon et al., 2020; McKnight-Eily et al., 2021). The sudden loss of a family member and pandemic-related social disruptions can increase a risk of developing a mental health issue such as prolonged grief disorder or major depressive disorder (Simon et al., 2020; Verdery et al., 2020). Further, in a sample of Black Americans, those who perceived COVID-19 as a threat to one’s health reported higher levels of psychological distress (Cobb et al., 2021). Indeed, being at a greater risk of developing COVID-19 or having a relative who has passed away from the coronavirus is likely a major contributor to mental health problems in these communities, particularly among those with pre-existing mental health conditions (Cooper & Williams, 2020; SAMHSA, 2020).
Since the onset of the pandemic, instances of racism have increased (Bhaskar et al., 2020; Serhan & McLaughlin, 2020). Asian communities in particular have been the targets of racism as a direct result of COVID-19 (Bhaskar et al., 2020; Serhan & McLaughlin, 2020). There are increased reports of racism, discrimination, and violent attacks on Asian individuals across the world, and some have devastatingly turned lethal (Shear & Wright, 2021). Some political leaders have incited negative racial stereotypes through language and phrases that attach a location or ethnicity to COVID-19, such as “Wuhan Virus” (Levenson, 2020). Statements like these, coupled with daily instances of discrimination, are associated with an array of negative mental health outcomes, including anxiety and depression (Hwang & Soto, 2008). Social media may also play a role in recent racism against Asian communities, as a stronger acceptance of social media content is associated with higher reported prejudice toward Chinese individuals (Croucher et al., 2020). Moreover, the proportion of tweets with negative sentiments toward Asians increased over 68% from November 2019 to June 2020 (Nguyen et al., 2020). Results from the “Asian Implicit Association Test” indicate anti-Asian bias declined prior to 2020, but began to increase starting in March 2020, perhaps following stigmatizing rhetoric in the media (Darling-Hammond et al., 2020). Among Chinese American families surveyed in 2020, over 76% of parents and children reported vicarious racism, and nearly half reported perceived health-related anti-Chinese sentiment (Sinophobia). Exposure to racism was related to higher anxiety and depressive symptoms in both adults and children, and health-related Sinophobia was related to poor psychological wellbeing in adults (Cheah et al., 2020).
Ethnic and racial minorities have historically been disproportionately affected by other natural disasters and economic crises, now compounded by the pandemic. Following Hurricane Ike, African Americans were more likely to report post-traumatic stress disorder (PTSD) and depression compared to White and Latino respondents, and African American and Latino participants reported a greater loss of essential services due to the disaster (Davidson et al., 2013). In some cases, these historically marginalized communities who may be rebuilding after previous disasters or acts of racism are now differentially impacted by the COVID-19 pandemic, with a potential new “wave” of mental health issues to ensue.
Possible Mechanisms
Experiencing the consequences of racism has been linked to heightened stress and the development of mental health symptoms (Williams et al., 2019). Over time, these experiences accelerate physical health decline, as has been shown by evidence supporting the weathering hypothesis (Geronimus, 1992) for a variety of health outcomes (Forde et al., 2019).
For example, anticipating prejudice has been associated with a heightened physiological stress response and increased vigilance among Latina participants (Sawyer et al., 2012). Stereotype threat, the threat of being judged or treated unfairly due to culturally-held negative stereotypes, can also affect various aspects of psychological functioning in minoritized populations. Stereotype threat has also been linked to long-term mental health outcomes such as depression and anxiety, particularly when the threat of stereotype spills over into other domains (Inzlicht et al., 2012; Spencer et al., 2016). Internalized racism, involving an individual’s acceptance of negative race-related stereotypes, is associated with poorer mental health and increased discrimination-related distress (Millan & Alvarez, 2014). Discrimination, internalized racism, and stereotype threat further compound disparities in mental health. In Asian Americans, stereotypes such as the “model minority stereotype”, which overlooks current racism and discrimination, can reduce access to healthcare and asking for help, as this group exhibits low usage of mental health services (Chen et al., 2020; Park et al., 2019).
From a developmental perspective, racism may exert its effects most profoundly during particular windows of development, such as adolescence, a time of ethnic identity development and active socialization of racial/ethnic values (French et al., 2006; Umaña-Taylor et al., 2014). Pre-pandemic research suggested that racial/ethnic minoritized adolescents report lower levels of positive affect compared to white youth (Deer et al., 2018), which constitutes a risk factor for depression and suicidal ideation (Rubio et al., 2020). During the pandemic, a study analyzing support-seeking data from a national text-based crisis service reported an increase in suicidal ideation among children and adolescents compared to pre-pandemic levels, with racial/ethnic minorities, LGBTQ and gender-nonconforming youth at greatest risk (Runkle et al., 2022). Previous studies have also shown that perceived racial discrimination in young Black men (ages 20 to 23) predicted an increase in future anxiety and depression symptoms nearly 10 years later (Assari et al., 2017). In Mexican-origin adolescents, reported ethnic discrimination was related to daily stress levels and sleep quality (Zeiders, 2017). Similarly, in another racially diverse sample, adolescents who experienced higher discrimination coupled with poor sleep quality also experienced greater depressive symptoms over time; with higher discrimination related to concurrent depressive symptoms (Yip, 2015). School-aged youth who reported greater experiences of direct racism also had higher loneliness and depressive symptoms (Priest et al., 2014). In addition, White adults who work with children have been shown to hold negative stereotypes of minority children and adolescents, perhaps impacting the functioning of youth in other psychological domains (Priest et al., 2018). In addition to adolescent identity development, there are other mechanisms by which racism likely impacts individuals throughout their development. For example, chronic stress experienced by pregnant women due to racism, prejudice, and discrimination may become biologically embedded during the perinatal period, impacting the developing fetus (Conradt et al., 2020). Thus, experiences of racism and their impact on human development likely start early in development and have implications for future generations of racial/ethnic minorities.
The Impact of COVID-19 on Women and LGBTQ+ Communities
Evidence on Disparities during COVID-19
Sexism, heterosexism, and gender binarism represent societal systems that privilege men, heterosexual, and cisgender people, leading to unequal health outcomes (Krieger, 2020). These are patterns of health disparities that have been noted before the pandemic, but emerging evidence suggests that pandemic-related mental health symptoms followed the same patterns, disproportionately affecting women and LGBTQ+ people.
Nationally-representative surveys examining gender differences between those identifying as women and those identifying as men reported higher rates of distress among women during the pandemic. For example, one nationally-representative survey of adults ages 18 and older in the U.S. showed that the prevalence of elevated depression symptoms was 33.3% in women and 21.9% in men during April 2020 (Ettman et al., 2020). The higher prevalence of distress and depressive symptoms among women compared to men during the pandemic has been documented across specific subpopulations, including seniors (Barcellos et al., 2021), healthcare workers (Prasad et al., 2021), and parents (Zamarro & Prados, 2021). Nuanced results emerged in college students, among whom women exhibited greater increases in alcohol use disorder than men during the pandemic, but similar increases in symptoms of depression (Kim et al., 2021). Pregnant women emerged as a particularly vulnerable during the pandemic, experiencing high rates of depression (36%), thoughts of self-harm (20%), and anxiety (22%) (Liu et al., 2021). Thoughts of self-harm were four times higher among pregnant women who reported death of a family member due to COVID-19 (Liu et al., 2021), suggesting a direct role of the pandemic in the development of these symptoms. Another study revealed that fear of contagion and lack of control doubled the rates of obsessive-compulsive disorder among pregnant women in the U.S., reaching 7.13% (Mahaffey et al., 2021). Future research will need to examine the potential long-term consequences of these mental health problems on both mothers and the offspring who were in utero during the pandemic.
Studies have also begun revealing significant increases in mental health symptoms such as depression and anxiety compared to pre-pandemic levels in the LGBTQ+ population in the U.S. (Flentje et al., 2020; Gonzales et al., 2020) and in multiple other countries (Gato et al., 2021; Kneale & Bécares, 2021). Evidence suggested greater levels of symptoms among sexual and gender minority (SGM) participants than non-SGM participants, even after controlling for pre-existing mental health symptoms and lifetime discrimination (Kamal et al., 2021). Specifically, some data reported greater increases in mental health symptoms among those experiencing discrimination during the pandemic (Kneale & Bécares, 2021). Substance use prevalence may have also increased in this population during the pandemic. Among SGM college students in the U.S., 32% reported greater alcohol use since the start of the pandemic, with effects being particularly pronounced among those whose sex at birth was female (Salerno et al., 2021). Closures of universities and colleges also increased distress for LGBTQ+ students returning home to families who were unsupportive of their identity (Gonzales et al., 2020).
Overall, this evidence indicates that mental health inequities affecting women and LGBTQ+ groups may have exacerbated during the pandemic, but also that more research is needed that specifically collects fine-grained data regarding gender and sexual orientation in order to begin implementing strategies for promoting health equity (Gorczynski & Fasoli, 2020).
Possible Mechanisms
Prevailing theory suggests three general pathways that lead to health disparities for women and LGBTQ+ people (Krieger, 2020). These include structural forces (e.g., laws, policies, and rules) that place these groups at a disadvantage and limit their economic opportunities; interpersonal exposures such as discriminatory behaviors and beliefs of privileged groups against these groups; and internalized beliefs by women and LGBTQ+ people that may harm mental health (Krieger, 2020). Internalized beliefs represent an individual’s acceptance of others’ biased views of them as accurate, leading to shame and mental health difficulties (Krieger et al., 2020). This is exemplified by women experiencing self-blame in the aftermath of experiencing gender-based violence. In addition to these factors suggested by Krieger and colleagues (2020), there are also additional sociocultural and psychobiological factors that disproportionately impacted women during the pandemic.
One specific social and cultural factor with widespread impact on mental health during the pandemic has been increased demand for unpaid care work (e.g., care for dependent children, family caregiving for adults with chronic illness). At the beginning of the pandemic, many schools and daycare centers were closed, and many care services and supports for adults with chronic or acute health needs became inaccessible or curtailed, leaving gaps in childcare and eldercare that were, and continue to be, disproportionately filled by women (Connor et al., 2020; Power, 2020). Caregiving during COVID-19 has been associated with poorer mental health regardless of gender. Family caregivers of adults with chronic illness reported increases in caregiving intensity, complexity, and caregiver burden as a result of the pandemic, in addition to reporting higher anxiety, depression, and substance use to manage COVID-19 stressors than non-caregiving adults (Beach et al., 2021; Cohen et al., 2021; Czeisler et al., 2020; Park, 2021). Similarly, parents caring for minor children reported significantly higher anxiety, depression, suicidal ideation, and alcohol use than adults without childcare responsibilities (Czeisler et al., 2020; Gadermann et al., 2021). For both parents and family caregivers, the burden of care and associated adverse mental health outcomes were more likely to be borne by women. During the pandemic, women have spent significantly more time than men caring for children or for adults with chronic illness, even while maintaining employment (Cohen et al., 2021; Gadermann et al., 2021). In terms of mental health, mothers of young children have reported significantly greater psychological distress during COVID-19 than fathers or women without young children in the home (Zamarro & Prados, 2021). Similarly, for chronic illness caregivers, poor mental health outcomes in response to caregiving stress have been significantly worse for female caregivers (Beach et al., 2021). The widening of gender disparities in mental health during the pandemic has been driven in part by inequitable increases in unpaid care work, and will likely have long-term impacts on women’s health (Almeida et al., 2020; Connor et al., 2020; Power, 2020).
To further specify the psychobiological pathways by which inequality translates into unequal mental and physical health outcomes, the minority stress model has been proposed (Lick et al., 2013; Meyer, 2003). Experiencing or fearing possible harassment, discrimination, and stigma can increase distress and undermine wellbeing (Lick et al., 2013), as these experiences constitute forms of social stress (Meyer, 2003). Studies of stressful experiences among SGM groups have implicated some of the same stress-physiological pathways previously studied in connection with other chronic stressors, such as activation and possible dysregulation of the autonomic nervous system, HPA axis, and immune system, which increase allostatic load and risk of mental and physical health problems (Lick et al., 2013). More research with these populations is needed to fully specify these mechanisms and to test their effects during COVID-19, but initial evidence suggests the need to allocate increased mental health resources to women and LGBTQ+ groups.
Immigrants, Migrants, and Mental Health
Evidence on Disparities during COVID-19
How cultural risk factors and mechanisms have impacted mental health outcomes for immigrants and migrants during the COVID-19 pandemic is relatively understudied. Further examination of COVID-19’s impacts on mental health outcomes for immigrant and migrant communities is necessary and could inform strategies and interventions for improving mental health outcomes for this group.
Because evidence suggests that, before the pandemic, immigrants and migrants were at increased risk of experiencing mental health problems (Garcini et al., 2016), research examining how COVID-19 has potentially exacerbated this risk requires further investigation. Currently, we are aware of two studies that have. One study measured immigrant outpatient mental health outcomes pre-pandemic compared to mental health outcomes during the pandemic and found significant increases in levels of depression, anxiety, and psychological stress (Serafini et al., 2021). Another study examining the effects of social distancing measures (i.e., shelter-in-place orders) found similar results when measuring immigrant workers’ mental health (i.e., depression, anxiety, and stress levels) following a dormitory outbreak of COVID-19 (Saw et al., 2021). The authors found that social distancing measures were positively associated with stress and depression symptomatology, and increased worry about being diagnosed with COVID-19 was positively associated with anxiety symptomatology (Saw et al., 2021). Furthermore, the authors found that immigrant workers who had greater uncertainties about job security, perceived their health as poor, or who had greater exposure to COVID-19 reported higher rates of stress, depression, and anxiety (Saw et al., 2021). Together, these findings suggest that the mental health of immigrant and migrant communities was affected by the pandemic. Yet, more work is needed to better understand mental health outcomes in these communities.
In addition to these mental health concerns, variations in immigration status and socioeconomic position have also contributed to immigrants’ and migrants’ access to mental healthcare resources and treatment. During the pandemic, undocumented immigrants suffered from fear of deportation, lack of access to social services such as healthcare, did not qualify for national unemployment benefits, were initially excluded from government relief packages, and some remain ineligible for federally funded health insurance programs (Page et al., 2020; Wilson & Stimpson, 2020). Some immigrant and migrant communities are also at higher risk of living under poor conditions that exacerbate COVID-19 transmission (e.g., facilities with poor sanitation, confined living conditions), tend to come from lower socioeconomic backgrounds, and have limited access to healthcare and mental health resources (Bhaskar et al., 2020).
Despite efforts by local state governments to support immigrant and migrant groups through policies such as extending stimulus checks to undocumented immigrants in California (Botts, 2021), the further marginalization of immigrant and migrant groups during the pandemic created additional barriers to accessing mental healthcare treatment (Page et al., 2020). Due to the disproportionate impact COVID-19 has had upon the immigrant and migrant community, more action is needed to provide a more effective economic “safety net” to protect this vulnerable group within the United States.
Possible Mechanisms
Examining cultural factors may help elucidate the mechanisms by which the pandemic differentially affected immigrant and migrant communities. Because immigrants are not a monolithic entity, we see significant cultural variability in how immigrants have adapted to U.S. culture and the pandemic (Barry, 1997; Liem et al., 2021). In the U.S., differences between collectivistic versus individualistic cultures can broadly provide valuable insight into possible mechanisms shaping mental health outcomes during and after the COVID-19 pandemic. In collectivistic cultures, for example, cultural values such as familism and filial piety are associated with mental health outcomes (Schwartz et al., 2010). During the pandemic, researchers found that Latino families’ increased worry was connected to concern for one’s local family and community as well as for family members living abroad (Moyce et al., 2021). In a separate study, communities that endorsed more family-oriented beliefs also had increased worries about spreading the coronavirus to relatives (Germani et al., 2020). Another study found that Latino mothers who were essential workers reported economic cutbacks and higher rates of stress and depressive and anxiety symptoms (Hibel et al., 2021). Foreign-born respondents, Latinos, Asians, women, and families with children under 18 also reported higher levels of subjective fear and worry during the pandemic (Fitzpatrick et al., 2020). Overall, these studies provide an understanding of cultural mechanisms that contribute to increased stress, fear, or worry during the pandemic and can help identify pathways by which negative psychological outcomes develop as a result of COVID-19.
Some research has also highlighted the benefits of cultural resources and coping mechanisms in promoting mental health and resilience throughout the COVID-19 pandemic. Despite strict social distancing measures and stay-at-home orders, researchers found that increased reliance on the community and increased communication with family members promoted positive feelings of unity and support (Moyce et al., 2021). In addition, telecommunication created space for immigrant and migrant communities to reconnect with family in their native countries, promoting social support and social connectedness (Moyce et al., 2021). However, decreases in social support have had the opposite effect. In Chinese adolescents, lower social support increased depression and anxiety symptomatology (Qi et al., 2020). Thus, across cultures it appears that maintaining close relationships and utilizing alternative forms of social support is important for alleviating some of the negative mental health consequences resulting from the pandemic. For immigrant communities specifically, increasing collective efficacy can provide additional protective effects against negative mental health outcomes among immigrant-dense neighborhoods (Feldmeyer et al., 2019).
In sum, developing a deeper understanding of the cultural mechanisms impacting mental health during the COVID-19 pandemic is an important area of research. Recognizing how cultural mechanisms can exacerbate risk or promote resilience will provide valuable information for future policy and serve as a blueprint for navigating future disasters. More specifically, for immigrant and migrant communities who are among the most vulnerable populations affected by the pandemic, we can alleviate some of the negative mental health outcomes by providing equitable access to mental healthcare resources and treatment. To achieve this goal, it will be important to develop greater access to affordable health and mental healthcare options and provide culturally sensitive resources to immigrant and migrant communities (e.g., news and resources tailored to each community’s native language, culturally appropriate resources and treatment). As we discuss in more depth in our later section on promoting societal resilience, we also recommend training clinicians and mental health professionals in adopting a cultural humility framework (Tervalon & Murray-García, 1998; Murray-García et al., 2014) to dismantle mental health inequities affecting immigrants and migrants.
Childhood Adversity and the Pandemic
Evidence on Disparities during COVID-19
Adverse childhood experiences (ACEs) are “potentially traumatic events that occur in childhood (0-17 years)” (Centers for Disease Control and Prevention, 2020) and encompass a wide range of experiences, from child maltreatment to parental incarceration. Experiencing more ACEs is associated with altered stress physiology (Deer et al., 2019) and poorer mental and physical health outcomes across the lifespan (Felitti et al., 1998). These outcomes, in turn, are associated with decreased productivity and earlier mortality, which have been shown to have negative economic consequences at the societal level (Bellis et al., 2019; Metzler et al., 2017).
Researchers and practitioners believe the COVID-19 pandemic has increased and exacerbated the prevalence of child maltreatment and domestic violence, especially in low SES communities. Pre-pandemic research had already established links between low SES, income inequality, and child maltreatment (Bryant et al., 2020; Campbell, 2020). Georgetown University’s Center on Education and the Workforce (2021) estimated that 23 million Americans lost their jobs in April 2020, in addition to a vast number of Americans who had their hours and wages reduced during the pandemic. Therefore, the economic impact of COVID-19 on families is an important variable to include when considering what factors led to increases in ACEs during the pandemic.
Lawson et al. (2020), who found that job loss during the pandemic increased the likelihood of child maltreatment, provides further support for the link between the pandemic’s impact on family income and child maltreatment. Similarly, Lee et al. (2021) found that job loss due to the pandemic was associated with increased use of physical punishment as a form of discipline. Additionally, Brown et al. (2020) reported that precarious financial circumstance and symptoms of anxiety or depression were associated with greater child abuse potential in a survey study of 183 families in the U.S. with children under the age of 18. Increases in stress and strain among parents and caregivers are worrying, because they may impair parents’ and caregivers’ abilities to serve as stress buffers for children, thus having spillover negative impacts on child mental health (Condon et al., 2020).
Parental social isolation is another common predictor of child maltreatment in the pre-pandemic literature (Berlin et al., 2011; Rodriguez et al., 2018). This is concerning, as the COVID-19 pandemic has necessitated the loss of physical contact to control the spread of the disease. As such, many schools, businesses, and religious institutions suspended operations or transferred to remote work (Bartik et al., 2020; Olneck-Brown, 2021). Shelter-in-place and social distancing orders therefore led children and adolescents to spend more time at home, potentially with their abusers (Campbell, 2020). Indeed, parental social isolation during the pandemic has been linked to increased verbal aggression as well as harsh discipline and greater conflict between parents and their children (Lee et al., 2021). This higher risk of exposure to maltreatment is compounded by the fact that children and adolescents had reduced contact with mandated reporters and more limited opportunities to disclose their maltreatment to someone they trust outside the home (Donagh, 2020; Welch & Haskins, 2020). Both parents and their children had reduced interactions with friends, teachers, extended family members, larger peer groups, and other community members, limiting their access to social support networks (Rogers, Ha, & Ockey, 2021).
As a result of the pandemic, maltreatment rates are suspected to have increased, but seem to be under-reported. For instance, Swedo et al. (2020) found that the proportion of emergency room visits due to child abuse/neglect increased in 2020 compared to 2019, and a greater number of these visits ended in hospitalization, although reports of child maltreatment to government agencies decreased by an estimated 40-60% (Weiner, et al., 2020). Similar patterns can be seen when examining natural disasters and other large-scale emergencies. For example, one study revealed that child abuse rates increased from one year before to after Hurricane Hugo in South Carolina and after the Loma Prieta earthquake in the Bay Area of California (Curtis et al., 2000). Overall, the literature tends to show that rates of child maltreatment and domestic violence often increase following these types of events, but this is not always reflected in formal reports (Campbell, 2020; Curtis et al., 2000; Parkinson, 2019; Seddighi et al., 2019; but see also Cerna-Turoff et al., 2019).
In summary, there is strong evidence that childhood adversity can have serious negative long-term consequences for mental and physical health, which are costly for society and individuals alike (Edwards et al., 2003; Gilbert et al., 2015; Herzog & Schmahl, 2018; Hughes et al., 2017; Thompson et al., 2019). The COVID-19 pandemic has increased the number of ACEs children and adolescents have experienced, and could be, itself, considered an ACE event for many people. However, while some ACEs are likely detrimental for all children, there is variation in their impact and individual interpretation, as trauma is a subjective experience. For example, the pandemic may be experienced differentially among children from varying levels of SES (Barnett, 2008; Lawson et al., 2020). Therefore, more research is needed to understand the development of individual differences in response to ACEs. Doing so will help elucidate how an event like the COVID-19 pandemic can be a traumatic experience as well as help determine protective factors that combat the negative consequences of the pandemic. Serious efforts need to be made to prevent ACEs, rather than simply trying to mitigate their consequences.
Possible Mechanisms
Childhood adversities may increase risk of mental health problems during the pandemic through the mechanism of early-life stress sensitization, which involves amplification or dysregulation of neurobiological stress responses among those with childhood trauma (Hostinar et al., 2021; Post & Weiss, 1998; Tsur & Abu-Raiya, 2020). Another mechanism is stress accumulation, whereby those who experience early-life adversity often continue to live in environments that expose them to higher rates of adversity and trauma in adulthood, thus compounding the effects of early-life stress throughout the lifespan (Hostinar et al., 2015; Widom et al., 2008). As an example of stress sensitization, John-Henderson (2020) examined the effects of childhood trauma on sleep quality in a population of American Indian adults. Childhood trauma was a significant predictor of greater stress and decreased sleep quality during the COVID-19 pandemic, even after controlling for current socioeconomic circumstances statistically. Similarly, Wade et al. (2021) found that having more pre-pandemic ACEs predicted greater pandemic-related stress and mental health symptoms among adult caregivers, independently of COVID-19-related stress. Parental mental illness is, in itself, considered an ACE (Felitti et al., 1998) and may be another mechanism by which children may be experiencing an increased exposure to ACEs during the COVID-19 pandemic.
Preliminary evidence supports the early-life stress sensitization pathway. For instance, Guo et al. (2020) examined pre-pandemic ACEs and mental health ratings taken during the COVID-19 pandemic in a sample of Chinese adolescents. They found that exposure to more pre-pandemic ACEs predicted more anxiety in their sample, and PTSD symptoms were increased among adolescents who experienced more pre-pandemic ACEs and more COVID-19-related stressors, such being infected with the coronavirus or having a family member, friend, or acquaintance suffer from COVID-19. In another study, Tsur and Abu-Raiya (2020) focused specifically on ACEs related to child maltreatment and examined whether histories of child abuse (sexual abuse, physical abuse, and emotional abuse) predicted COVID-19-related fear and stress. Data were collected in Israel during the early months of the pandemic (March through May 2020). Child abuse survivors experienced more symptoms of complex PTSD, which were in turn related to increased fear and anxiety about COVID-19 (Tsur & Abu-Raiya, 2020).
Another likely pathway is suggested by the biological embedding model (Miller et al., 2011), which describes pathways from experiences of childhood adversity like maltreatment or poverty to later chronic disease via alterations in cardiovascular, metabolic, and immune system functioning. Thus, childhood adversities can worsen physical health, and these pre-existing health conditions can compromise immune competence during pandemics. In turn, these physical health problems can undermine mental health and limit the ability to cope with new crises.
Social Isolation and Loneliness during COVID-19
Evidence of Disparities during COVID-19
When initial stay-at-home orders were implemented to curb the spread of COVID-19, a natural experiment began that exposed people to prolonged periods of reduced social interaction. Although evidence suggests mixed results regarding population-level increases in loneliness as a result of these social restrictions (Luchetti et al., 2020), certain subsets of the population appeared to be at greater risk of experiencing loneliness during quarantine than others.
Given the vast literature that social isolation and loneliness are associated with negative health outcomes (Cacioppo et al., 2015), it is important to identify those who may be at increased risk of being socially isolated and lonely during the pandemic. In the United States, mean-level increases in loneliness were not observed from pre- to 1 month post-pandemic onset in a nationally-representative study of adults ages 18 and up (Luchetti et al., 2020). In fact, participants reported increases in perceived support on average, though this result needs to be interpreted with caution because participants high in loneliness were less likely to participate in the follow-up waves during the pandemic. In addition, certain subgroups such as older adults (65 years or older) reported a small acute increase in loneliness immediately after the stay-at-home orders in March 2020, which levelled off by follow-up in April 2020. Across waves, participants with chronic disease and those who lived alone reported higher levels of loneliness compared to those without chronic disease and those living with others (Luchetti et al., 2020), suggesting similar risk factors for loneliness before and after the pandemic. Consistent with this result, cross-cohort analyses of data from adults in the United Kingdom captured before and during the pandemic also found that risk factors for loneliness were nearly identical before and during the pandemic, suggesting that people who were already at risk of being lonely pre-pandemic were at heightened risk during the COVID-19 pandemic (Bu et al., 2020). Those at risk, specifically, were young adults, people living alone, people with lower education or income, women, and racial/ethnic minority groups (Bu et al, 2020). This is especially alarming, considering that groups who already face health disparities due to their age, sex, race, and SES (Phelan et al., 2010; Williams et al., 2019; Victor & Bowling, 2012) seem to share more of the burden of the impact of social distancing efforts implemented to halt the spread of COVID-19.
In a cross-sectional study, Liu et al. (2020) assessed the potential risk and protective factors for mental health problems in young adults aged 18-30 years old after the onset of the pandemic. Researchers found that a key predictor associated with depression, anxiety, and PTSD during the pandemic was loneliness. Specifically, those participants with high levels of loneliness and worries about the COVID-19 pandemic were more likely to score above clinical cutoffs for depression, anxiety, and PTSD during the pandemic. Although the majority of respondents reported feeling lonely during the first two months of the pandemic (61.5% of this young adult sample), as well as having low resilience (72%) and low distress tolerance (74.1%), this sample also reported having access to both social support and instrumental support (Liu et al., 2020). Concerningly, however, 37% of respondents reported low family support.
Because adults 65 years and older had the highest risk of suffering negative outcomes due to contracting COVID-19 (CDC, 2021), strategies to avoid the spread of coronavirus were especially important for this age group. However, it was feared that these strict measures would have the unintended consequence of increasing social isolation and loneliness. To better understand the experiences of older adults during the COVID-19 pandemic, Kotwal et al. (2021) interviewed 460 community-dwelling older adults in the San Francisco Bay Area during the shelter-in-place orders. While some participants successfully used technology to maintain social connections, others mentioned either discomfort with it or not having adequate access to the Internet (Kotwal et al., 2021). Additionally, over half of participants reported worsened feelings of loneliness and were more likely to self-report worsened depression and anxiety during the study period. In follow-up interviews, several of these participants experienced increased loneliness scores or had loneliness scores that remained high over time. In open-ended responses from participants who reported worsened loneliness, participants described the COVID-19 restrictions as amplifying prior social losses and reported difficulty using technology, overwhelming feelings of being trapped, and loneliness affecting their physical and mental health (Kotwal et al., 2021).
While emerging new evidence is shedding light on the associations between preventative measures enacted to curb the spread of the coronavirus and feelings of loneliness, much more research is needed to identify individual differences in susceptibility to loneliness. The data described here were collected during the first few months of the stay-at-home orders; however, the COVID-19 pandemic is a worldwide stressor without a foreseeable endpoint. Because of this, there is a need for longitudinal studies to focus on long-term trends beyond the first few months of the pandemic. Interventions aimed at decreasing social isolation and feelings of loneliness should target specifically those who need it most and those who experience barriers to using technology to connect with others.
Possible Mechanisms
Social isolation and loneliness have long been recognized as risk factors for depression and anxiety, as well as for premature mortality from varying causes (Banerjee & Rai, 2020; Cacioppo et al., 2015; House et al., 1988). Mechanistic studies have suggested that social isolation and loneliness can elicit neural, neuroendocrine, and behavioral responses that can lead to changes in brain function across multiple brain regions (Cacioppo et al., 2015). In adults, perceived isolation and loneliness can lead to heightened attention to social threats and negative social stimuli, along with increased anxiety, hostility, and social withdrawal (Cacioppo et al., 2015). Social isolation can also activate stress-response systems, continually affecting neural architecture and behavior via changes in gene expression (McEwen, 2018). Specifically, growing evidence suggests that in humans, loneliness and social threat are associated with chronic activation of neuroendocrine stress-response systems like the HPA axis. This is a cause for concern, given that chronically elevated stress hormone production can lead to “wear and tear” (allostatic load) on the body, increasing the risk of numerous deleterious psychological and physical health outcomes (Cacioppo et al., 2015). This research suggests the importance of promoting social cohesion and access to social support at a societal level, particularly during periods when global stressors such as quarantines and other crises diminish social interactions.
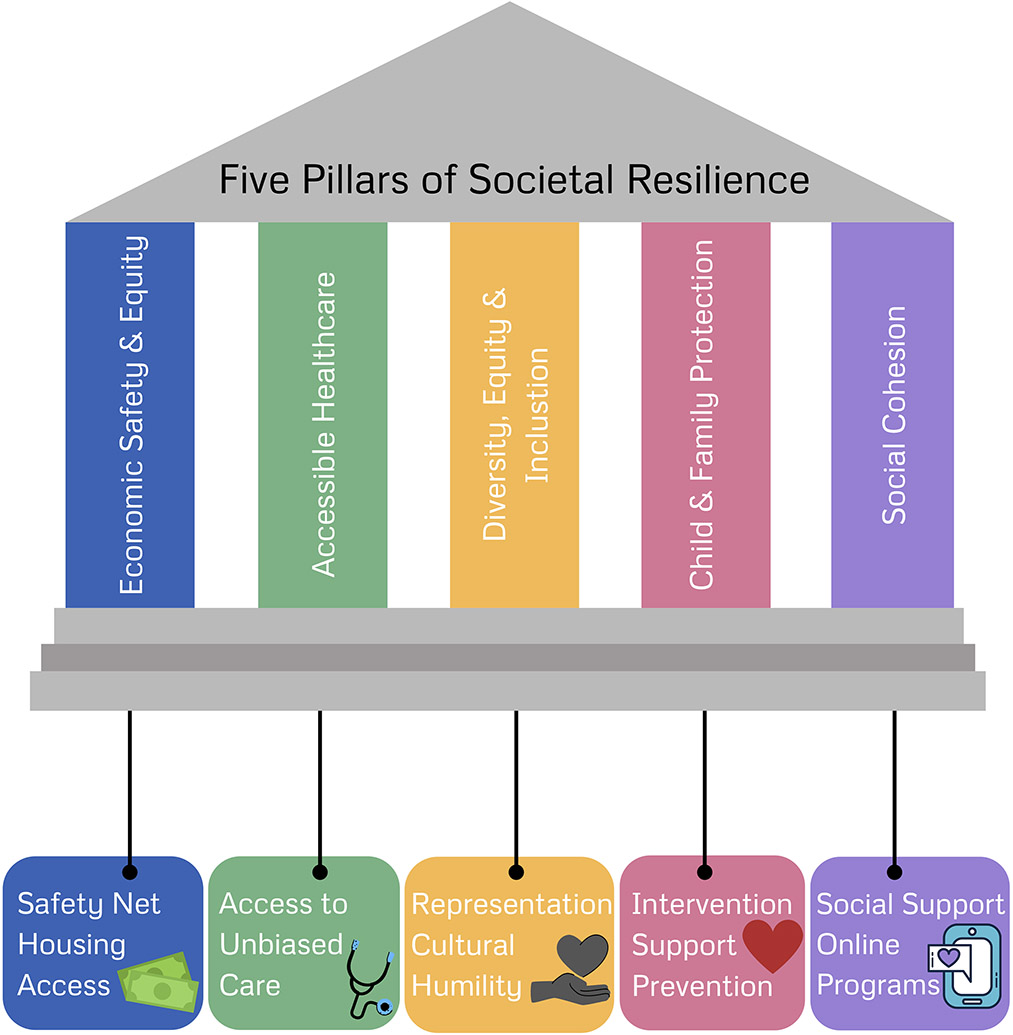
Conclusions and Lessons from COVID-19: Promoting Societal Resilience to Future Disasters
Resilience has been defined as the capacity to adapt to challenges and threats and can characterize individuals as well as broader systems such as countries (Masten, 2020). The resilience of individuals depends on the proper functioning of higher-order social systems that individuals are embedded in, such as local communities and national governments (Masten, 2020). When higher-order systems break down, more stress is placed upon individuals and family systems to compensate. Because of these continuous dynamic transactions between the resilience of individuals and that of society as a whole, we propose strategies to promote five “pillars” of societal resilience (Figure 2). In this model, we consider how (1) economic safety and equity, (2) accessible healthcare, (3) combating racial injustice and promoting respect for diversity, equity, and inclusion, (4) child and family protection services, and (5) social cohesion are beneficial for ensuring the resilience of both individuals and society as a whole. We suggest policies, interventions, and individual or community-level changes that will promote these foundational aspects of societal resilience in response to future disasters.
Figure 2.
Five proposed “pillars” of societal resilience.
During the COVID-19 pandemic, countries with greater income inequality, as reflected by the Gini coefficient, witnessed higher COVID-19 cases and deaths, even after accounting for these countries’ gross domestic product, average life expectancy, proportion of population aged over 65, and stringency of lockdown measures (Wildman, 2021). This pattern suggests that social and economic inequality undermines societal resilience, and that removing these sources of inequality may provide greater societal resilience during times of crisis.
Economic Safety and Equity
Beyond the deleterious impacts of poverty on mental health (Blair & Raver, 2016; Yoshikawa et al., 2012), economic inequality also has a salient impact on life expectancy and mental health in countries like the United States (Hill & Jorgensen, 2018; Ribeiro et al., 2017). Much like the impact of previous disasters, the brunt of the COVID-19 pandemic has been experienced by lower-resourced communities (Fothergill & Peek, 2004; Hawkins, 2020), thus economic safety and equity should be prime targets for promoting population mental health and societal resilience.
To promote resilience to future calamities, existing economic “safety net” policies require expansion, and new policies need consideration and examination. These include cash transfer and income supplement programs, broader food assistance programs, and more support for housing and residential mobility. In late March 2020, the United States passed the Coronavirus Aid, Relief, and Economic Security (CARES) Act, the largest stimulus bill passed until March 2021. The CARES act provided a one-time cash transfer to individuals and families that maintained poverty at pre-crisis levels (Parolin et al., 2020), but did not fully alleviate the economic stress in lower-resourced communities (Bitler et al., 2020). Two later stimulus payments in December 2020/January 2021 and March 2021 were provided. Yet the evidence suggests that sustained cash transfer programs piloted in other nations have been shown to reduce stress, prevent family violence, and increase long-term living standards (Handa et al., 2018; Haushofer et al., 2019). A monthly child allowance has been projected to completely eliminate severe child poverty in the United States, potentially disrupting intergenerational cycles of poverty (Shaefer et al., 2018). The Child Tax Credit is an example of a policy that has been effective at reducing the rate of child and family poverty to historic lows (Wise & Chamberlain, 2022). Cash transfers and child allowances have also shown more efficacy in reducing food insecurity in Canada than the Supplemental Nutrition Assistance Program (SNAP) in the United States, a program tied to income and limited in eligibility terms (Loopstra, 2018).
Additionally, housing unaffordability remains a structural barrier to disaster resilience. Providing permanent housing to the unhoused has become urgent during the COVID-19 pandemic and has increased popularity for innovative policies that aggressively address housing insecurity (Batko et al., 2021). For people living in high-poverty neighborhoods, residential mobility programs such as Moving to Opportunity have shown reductions in personal distress and improved wellbeing 15 years later (Leventhal & Brooks-Gunn, 2003; Ludwig et al., 2012). Among individuals from high-poverty neighborhoods, one standard deviation reduction in neighborhood poverty reduced stress to levels equivalent to those of individuals above the poverty line. Community investments and residential mobility opportunities can be offered in tandem to improve communities for those who wish to remain and provide flexibility for individuals and families seeking new communities. These poverty reduction measures may promote resiliency among higher-level systems, allowing lower-level systems to adapt to stress.
Accessible and Equitable Healthcare
Accumulating research has documented the impact of biases and discriminatory behaviors by healthcare providers on patients’ physical and mental health. Patients who have low socioeconomic status (Arpey et al., 2017; Woo et al., 2004), belong to a racial/ethnic minority group (Hoffman et al., 2016; Miconi et al., 2020), are LGBTQ+ (Cahill & South, 2002; Willging et al., 2006), immigrants (Hacker et al., 2015), are experiencing serious mental illness (Kaufman et al., 2012), or are obese (Phelan et al., 2015) experience barriers to care, as well as biased treatment from providers. The expectation of insufficient care may cause distress or mistrust in healthcare settings, and overall poorer mental health (Phelan et al., 2015). Bias exhibited by providers has been shown to elicit identity and stereotype threat, which can cause distress and, in the long term, have been linked to depression and anxiety (Burgess et al., 2010; Eliacin et al., 2020; Phelan et al., 2015). For these reasons, we propose that equitable and accessible healthcare, including mental health services, would reduce significant sources of inequality and promote societal resilience.
These biases and barriers are not only present in medical settings focused on physical health, they also exist within mental healthcare settings. Biases from mental health providers, and the structure of the mental health system itself, contribute to worse mental health outcomes for patients (Eliacin et al., 2020; Merino et al., 2018). Misinterpretation of patients’ symptoms due to differences in culture and lived experience, a lack of education on specific issues facing different groups, as well as microaggressions committed by providers, may impact diagnosis as well as adherence to and efficacy of treatment (Merino et al., 2018). Additionally, accessing treatment can be difficult for marginalized groups. Previous work found that patients’ socioeconomic status and race predict providers’ decisions to take on new patients, with middle-class and White patients being the primary receivers of care (Kugelmass, 2016). Additionally, even when patients find treatment, there can still be barriers to successful patient-therapist interactions. Individuals who identify as LGBTQ+, especially those living in rural or underserved areas, may encounter providers who may not have specific training in issues related to their identity, leading to worse therapy outcomes (e.g., Willging et al., 2006).
Research examining the effects of the COVID-19 pandemic largely documents that the effects of biases in the healthcare system on mental health have persisted and, in some cases, been amplified. In the United States, as already mentioned, Black and Latino populations have been hit especially hard, with mortality rates much higher than those of White Americans, leading to three-four times larger reduction in life expectancy for Black and Latino populations (Andrasfay & Goldman, 2021). This disparity in health outcomes has led to heightened mental health concerns. Black Americans have reported experiencing increased distress due to the heightened impact of COVID-19 on Black communities (Sneed et al., 2020), especially among those who already held the belief that Black Americans face racial discrimination in health settings (Cobb et al., 2021). Similarly, previously discussed research found that Chinese Americans have experienced an increase in perceived health discrimination, which was associated with poorer mental health (Cheah et al., 2020). Many LGBTQ+ youth, who are already at a higher risk of mental health disorders, lost access to mental health services provided in schools when distance learning was instituted (Salerno et al., 2020). In an attempt to address the amplification of these preexisting disparities, there has been an increase in the use of strategies thought to decrease access disparities, such as the increased availability of telehealth, and increased Medicare reimbursement for Federally Qualified Health Centers (FQHCs) through the CARES act to serve marginalized populations (Demeke et al., 2020). However, preexisting divides in access to care have widened. Current research demonstrates that the digital divide between rural and urban access to internet, as well as lower use of telehealth services among Black, Latino, and LGBTQ+ individuals, despite increased funding for FQHCs, may contribute to the widening disparities (Jaffe et al., 2020; Ruprecht et al., 2021). With the augmentation of these pre-existing effects of bias experienced on mental health, it is important to examine ways to address these biases.
To address the aforementioned disparities, it is imperative to first document their existence. Medical providers and government agencies could collect more uniform and comprehensive data on patient demographics, such as race/ethnicity, sexual orientation, gender identity, disability status, and socioeconomic status (Daugherty Douglas et al., 2015; Maragh-Bass et al., 2017). Lack of information in this area can prevent institutions from fully understanding the extent of inequalities and disparities. While race/ethnicity is documented in the United States, information on LGBTQ+ identity, disability status, and socioeconomic status, among other identities, is not as uniformly recorded, if at all (Daugherty Douglas et al., 2015). Better understanding of these biases can provide a foundation for more targeted interventions.
Anti-bias interventions for healthcare providers aim to increase cultural awareness among providers through increasing knowledge, changing attitudes, and increasing comfort level, in order to improve patients’ experiences. Interventions aimed at promoting positive attitudes may involve patient panels discussing barriers to care, whereas interventions aimed at increasing provider comfort may involve strategies like role play and group discussion (Morris et al., 2019). Interventions aimed at increasing knowledge about and comfort working with patients have been successful for providers working with LGBTQ+ and obese populations (Gendron et al., 2013; Morris et al., 2019; Phelan et al., 2015). These interventions have also been successful in increasing racial/ethnic sensitivity among psychiatric mental health nursing students, particularly those whose training occurred in underserved settings and those who were more advanced in their training (Boyer et al., 2019). However, interventions aimed at promoting positive attitudes towards LGBTQ+ and obese populations have been less successful, with recent reviews documenting mixed results (Morris et al., 2019; Phelan et al., 2015). Overall, how we teach providers principles of cultural awareness and humility, particularly in the context of racial/ethnic disparities, cannot be a one-time training. Single or infrequent sessions, unintegrated with practice and without facilitated learning, may be counterproductive for both the clinician and the patients they serve (Murray-Garcia et al., 2014). We discuss principles of effective cultural humility interventions in more depth in the next section.
In conclusion, a robust healthcare system with equitable access, expanded telehealth infrastructure, and greater emphasis on reducing bias among providers may provide a foundation for more psychological resilience to disasters. Rampant inequality around access to healthcare among medically underserved groups has perpetuated greater disparities in the impact of COVID-19 on physical and mental health (Mackey et al., 2020). Expanded telehealth can provide greater overall access to healthcare and may reduce access disparities among underserved communities (Ortega et al., 2020; Menon & Belcher, 2020). Expansion of telehealth should include infrastructure for increased broadband internet among underserved and rural communities (Bauerly et al., 2019). Although an emphasis on equity throughout healthcare can promote resilience to future disasters, this cannot occur without an effort to combat systemic racism and promote diversity, equity, and inclusion.
Combating Racial Injustice and Promoting Diversity, Equity, and Inclusion
As highlighted previously in this review, racial/ethnic minority and immigrant populations were disproportionately impacted by the COVID-19 pandemic and previous disasters (Abedi et al., 2021; Finch et al., 2010). Solutions to the legacy of racism in the United States are needed because the evidence is clear that racial injustice remains a public health issue that weakens these communities’ ability to adapt to disasters (Wrigley-Field, 2020). At a structural level, these communities can be bolstered against disaster through a policy emphasis on environmental and economic justice, as well as infrastructure investment (Bolin, 2007). In addition, more resources should be allocated to factors that promote community resilience (Xu et al., 2020).
Recognizing that interventions which target racism and discrimination are crucial, an important next question is whether to enact change at the individual or community level. Interventions to change social norms may be more effective when they target group-level processes, such as collective action, which broaden the potential mechanisms to change behavior (Prentice & Paluck, 2020). Specifically, experimental evidence shows that participatory processes can shift attitudes toward social authority and justice (Wu & Paluck, 2020). Beyond community-level interventions, promoting “identity-safe” environments can be accomplished by promoting diverse racial representation and increasing inter-racial contact across sectors of society. Representation of racial and ethnic minorities provides a cue to members of minority groups that diversity is valued in a given environment, such as a healthcare setting (Burgess et al., 2010). Inter-racial contact through structured diversity programs has been shown to increase comfort and understanding among different racial groups. In a study of physicians, Onyeador et al. (2020) found that those who had greater and more positive contact with Black individuals before medical school showed less anti-Black bias in residency. Even accounting for previous contact, positive inter-racial contact during medical school predicted less bias during residency in non-Black physicians.
Education also plays a key role in mitigating the impacts of racism on mental health disparities. Educating children and adults about racism and its effects, changing racist policies, and dispelling racist stereotypes will shift us closer toward more equitable environments (Burgess et al., 2010; Spencer et al., 2016). Additionally, universal economic policies, such as the Child Tax Credit, could also contribute to alleviating racial disparities in child and family wealth and health, particularly among Black and Hispanic families (Marr, 2021).
To reduce racial injustice in healthcare settings, the lens of cultural humility may be one way to mitigate health disparities. Cultural humility is a concept from medical education that has been applied broadly across healthcare disciplines and settings, including mental health services provision (Tervalon & Murray-Garcia, 1998). In contrast to the concept of cultural competence, which suggests that an endpoint of cultural mastery may be suitably achieved (Botelho et al., 2020), cultural humility is framed as an ongoing process of continual engagement with three key principles (Tervalong & Murray-Garcia, 1998): (1) lifelong learning and critical self-reflection, (2) recognizing and challenging power imbalances, and (3) institutional accountability. The first principle, lifelong learning and critical self-reflection, involves an ongoing commitment to listen and learn from individuals and communities that we serve, to recognize and acknowledge what we do not know or understand about their experiences, and seek out knowledge and resources that will improve our ability to provide high-quality care that meets their unique needs and experiences. This process also involves engaging in candid reflection and self-critique to identify biases or actions that perpetuate disparities in care delivery. Lifelong learning and critical self-reflection bring to focus the power differentials that exist in relationships between individual clinicians and patients/families, and between health systems and underserved communities. Recognizing these imbalances, and acting to remedy them in an effort to deliver equitable care, are essential components of the second principle of cultural humility. The third principle, institutional accountability, suggests that the same processes of ongoing learning and self-critique, and remedying power imbalances, must occur on the institutional level, and that institutions must be held publicly accountable for commitments they have made to mitigate health disparities.
Implementing cultural humility principles in the context of COVID-19 has important implications for reducing mental health disparities. One of the immediate repercussions of COVID-19 on mental health service provision was a rapid expansion of telemedicine. Cultural humility is one effective approach that mental health providers used during COVID-19 to successfully build therapeutic alliances with diverse patients (Glass et al., 2021). Mental healthcare delivered using cultural humility principles may also be important for underrepresented individuals and communities who have experienced trauma during the pandemic. There are long-standing disparities by racial, ethnic, and socioeconomic status in terms of both exposure to traumatic experiences, and access to mental health services to mitigate long-term sequelae of trauma exposure.
Who participates in cultural humility interventions may be important for their success. Previous work has found that cultural awareness training is more successful if it works with the entire workforce, including physicians and nurses as well as less front-facing employees such as administrators and security guards (Bonvicini, 2017; Gendron et al., 2013). In order for real progress to be felt, these changes need to be systemic. Another potential way to increase the efficacy of these cultural awareness programs is if, in addition to working with the general workforce, special attention is paid to providers who are most likely to come into contact with underserved populations. Previous work in this area has shown that the barriers to care and biases held by providers cause patients to delay care until it is an emergency (Bonvicini, 2017). This means that their first point of contact with a healthcare provider may be in an emergency setting like an emergency room or a phone hotline (Bonvicini, 2017; Merino et al., 2018; Phelan et al., 2015). In addition to this being the first point of contact, this may be a high-stakes situation, with the patient experiencing a life-threatening mental or physical health emergency, so it is especially important that providers have the tools to successfully care for the patient. The larger context of the cultural climate is another aspect that should be incorporated into the training. In contexts like those of the current global COVID-19 pandemic, there are specific stressors that communities are facing, so education about these stressors needs to be incorporated into treatment plans. Recent literature has drawn attention to the importance of providers understanding these specific stressors and the need for compassion (Li & Galea, 2020).
An important and highly cited call to action to remedy different forms of bias is to increase the diversity within the medical field (e.g., Bonvicini, 2017; Burgess et al., 2010). The presence of providers of similar identities to patients can signal safety to patients and may alleviate stereotype threat and associated stress. However, simply increasing diversity is not enough. Supports need to be in place for underrepresented minority (URM) providers entering and working in the healthcare field, as they are just as likely to experience the same discrimination and biased treatment as patients (Burgess et al., 2010). Prior research has identified strategies for retaining URM providers, such as the use of social networks, visible institutional support through tangible resources, and having administrators who are committed to workplace diversity (Peek et al., 2013). Additionally, there is a need for more research regarding the effects of interventions to decrease healthcare providers’ biases on the mental health of the patients served by these providers. While the presence of these biases has been documented, we still need to examine whether these interventions impact patient mental health. There is a risk that, while these interventions may improve provider knowledge and comfort, these effects are not actually being felt by the patients interacting with these providers. Additionally, the literature in this area emphasizes the need to examine intersectional identities, as the influence of these biases on mental health is likely influenced by all of patients’ identities, such as their gender, race, sexual orientation, and socioeconomic status (e.g., Anastas et al., 2020; Willging et al., 2006). While some studies have explicitly examined intersectional identities, this is still a growing area in the literature that needs further exploration.
In conclusion, the COVID-19 pandemic has clearly widened existing racial and ethnic disparities in mental health, highlighting the need for culturally-responsive services for affected individuals and communities. Delivering these services with cultural humility principles in mind will likely be beneficial for promoting equity in mental health services access and quality for diverse patients, families, and communities (Melendez Guevara et al., 2021).
Child and Family Protection
Children are one of the most vulnerable populations to the effects of disasters, as they are highly dependent on their caregivers for survival. According to the family stress model, the effects of disasters on children are often mediated through breakdowns in family processes due to economic hardship (Conger et al., 2000; Scaramella et al., 2008). Thus, poverty alleviation measures (cash allowance for children, increasing the minimum wage, food and nutrition assistance, job training programs) may alleviate parental stress and reduce rates of child maltreatment.
While poverty reduction measures can reduce the impacts of financial strain on families, current events have shown that sufficient economic relief is not always feasible (Prime et al., 2020; Yoshikawa et al., 2020). Additional support through intervention programs for parents are needed. One potential strategy for delivering parenting interventions during dynamic disaster conditions, such as those experienced during the COVID-19 pandemic, is to adapt existing interventions for online delivery. Prior research suggests that some programs, such as Triple P – a brief intervention aimed at reducing child problem behavior and dysfunctional parenting – maintained efficacy when administered online during a randomized controlled trial (Baker et al., 2017). Another parenting intervention aimed at improving parent-child relationships, The Family Check-Up, has also maintained efficacy when administered online and has been shown to increase use of community resources for high-risk families (Danaher et al., 2018; Leijten et al., 2015). Briefer interventions, such as educational campaigns, could also be promising. A number of organizations dedicated to child protection have disseminated online resources to promote child wellbeing. For example, UNICEF created a series of guides that provide information on positive parenting practices, coping strategies, non-violent discipline techniques, and budgeting money during financially stressful times (see https://www.unicef.org/coronavirus/covid-19-parenting-tips). These guides can be accessed online and shared with community members who need additional assistance but may not have the time to participate in more extensive programs.
To prevent families from becoming socially isolated, community support groups could be created to provide social support and resources to vulnerable populations. In addition, these community support groups could receive training on identifying and reporting potential signs of domestic violence or child maltreatment in the home.
Prevention programs for prenatal and early life care are also an important investment to promote resilience before disasters occur. The COVID-19 pandemic was a significant stressor for new and expecting mothers (Preis et al., 2020). A recent investigation of a prenatal intervention for expecting mothers experiencing depression has shown that treating maternal depression has the potential to reduce psychopathology across the offspring’s lifespan (Davis et al., 2018). Home visiting programs that have served as effective interventions for at-risk and low-resourced recent and expecting mothers have quickly adapted to online formats, yet their efficacy is still to be determined (Williams et al., 2020). Crisis nurseries can also serve as a resource and support for families needing temporary assistance with childcare during a crisis (DePasquale et al., 2020). Finally, to reduce the impact of the pandemic on child and parental mental health, high-quality and easily accessible mental healthcare must be made available to everyone, including those in underserved, rural communities. This includes investing in telehealth options (Mead, 2020). Mental health services may be more effective if they are provided within a unified infrastructure that addresses mental and physical health simultaneously (Bartlett & Stratford, 2021). In sum, high-quality mental healthcare, prevention of childhood adversity and multiple modality interventions will allow a more resilient response to future disasters.
Social Cohesion
Social cohesion has been shown to play an important role in a community’s capacity to adapt to and recover from disasters such as wildfires and floods (Townshend et al., 2015). Social cohesion has been defined as encompassing mutual trust, support, and assistance among community members, and a shared sense of belonging to the same group (Chan et al., 2006). Cohesion can manifest in multiple ways, ranging from social support provided between individuals to volunteering and other forms of civic participation that strengthen communities and the social ties within them.
In the psychobiological literature, social support has been identified as a buffer against stress and a key promoter of resilience (Gunnar & Hostinar, 2015; Hostinar, 2015; Parenteau et al., 2020; Perry et al., 2021). Decades of correlational studies and laboratory experiments with children and adults alike have shown that social and emotional support can reduce the reactivity of the HPA axis and other stress-response systems, resulting in healthier biological profiles (Alen et al., 2020; Hostinar, 2015). Social support can not only reduce measures of allostatic load (McEwen & Gianaros, 2011), but can protect against the development of mental health problems. For example, Liu et al. (2020) found that emotional support from family was associated with low levels of depression and PTSD in young adults during COVID-19, a finding consistent with prior research (Lee et al., 2018). Furthermore, social support attenuates the impact of chronic stressors such as poverty and inequality on mental and physical health (Chen et al., 2017; Hostinar & Miller, 2019). Given this robust evidence, promoting social cohesion and supportive social ties within communities would promote societal resilience during crises.
A potential barrier to promoting social cohesion during the COVID-19 pandemic is the need to use virus-containing measures such as social distancing, masking, and limits on large gatherings. Thus, programs that promote access to social support and overall social cohesion need to be re-envisioned during pandemics. Digital resources, such as internet applications and video chat, could potentially help reduce negative mental health outcomes (Banskota et al., 2020). Online support groups based on specific shared characteristics such as LGBTQ+ identity or being a parent may provide individual community members with coping strategies that are tailored for their specific circumstances. For example, some initial evidence indicates that short-term virtual support groups for parents are highly feasible, low-cost, scalable, and may provide an effective strategy to promote the resilience of parents and their children (Luthar et al., 2019). As already mentioned, expanding access to broadband internet and providing increased assistance to groups who experience difficulties with technology will be necessary for widespread use of virtual social support groups.
A recent review of interventions that were shown to be effective at reducing loneliness before the pandemic and are compatible with social distancing measures identified a few promising candidates (Williams et al., 2021). Educational programs about friendship and social integration, social facilitation software, psychological interventions such as mindfulness meditation, and robotic pets, were the most effective anti-loneliness interventions among those compatible with social distancing measures, although the quality of the trials testing some of these interventions was deemed to be somewhat low (e.g., researchers not blinded to intervention, insufficient details on participant loss to follow-up; Williams et al., 2021). Furthermore, all of this research was conducted before the pandemic, thus the ability of these interventions to reduce loneliness during pandemics and other disasters that prevent social contacts remains to be empirically tested.
In sum, there is robust evidence linking individual perceptions of social support and community-level social cohesion to greater individual and community resilience. However, understanding how to improve access to social support and social cohesion through interventions and during times of crisis necessitates further evidence from high-quality randomized controlled trials, and may also require the development of new interventions.
Considering Intersectionality to Promote Societal Resilience
In summary, we have reviewed evidence that multiple forms of social and economic inequality undermine the ability of individuals and families to respond to disasters with resilience. An important conclusion is that individuals who are marginalized along multiple dimensions of their identity (e.g., being a low-income woman, or an LGBTQ adolescent with a prior history of multiple childhood adversities) have experienced a more negative impact of the pandemic on their mental health. This is because multiple forms of inequality interact and intersect to shape an individual’s experience and health in unique ways according to their social identity (Bauer, 2014; Lewis & Van Dyke, 2018), as has been proposed by intersectionality theory (Cole, 2009; Crenshaw, 1989). Intersectionality describes and considers the combined effects of belonging to multiple social identities (Cole, 2009; Crenshaw, 1989). Originally used to examine the multidimensional experience of discrimination among Black women, intersectional frameworks have been extended to examine and characterize the experience of groups with multiple marginalized social identities (Cole, 2009; Lewis & Van Dyke, 2018). Intersectionality theory posits the impacts of these identities are not necessarily additive and may combine in unique, complex, and “intercategorical” ways (Bauer, 2014; Cole, 2009; McCall, 2005). For example, the experience of what it means to be a woman is different across cultures and racial groups, shaped through cultural processes, positionality, social policies, and historical trauma (Bauer, 2014; Cole, 2009; Hurtado, 1989).
Following an intersectional framework, individuals who hold multiple marginalized identities would be predicted to experience greater impacts on mental health during the COVID-19 pandemic. As emphasized, the effects of the pandemic and resulting containment measures did not affect individuals equally (Maestripieri, 2021; Purtle, 2020). A clear example is the disproportionate impact of the pandemic on women. Women, particularly mothers of young children, have faced a disproportionate impact of caregiving responsibility (lack of childcare, facilitating remote schooling, and providing care for elders) and were also disproportionately impacted by unemployment (Connor et al., 2020; Gould & Wilson, 2020; Laster Pirtle & Wright, 2021). Women with lower socioeconomic status and marginalized racial or ethnic identities experienced greater disadvantage and were overburdened in ways that impacted their well-being and mental health (Connor et al., 2020; Laster Pirtle & Wright, 2021). The compounding effects of these multiple identities suggest the need to allocate additional resources and interventions for those who experience multiple forms of social or economic disadvantage.
The policies we proposed to build the foundational “pillars” of resilience would address these multiple intersecting types of inequality (Figure 2). As discussed, an expansion of economic “safety net” policies that promote economic safety and equity will create greater resilience among communities and families before a disaster occurs, allowing a more robust and adaptive response. Second, accessible and equitable healthcare will create healthier communities and build infrastructure for mental health treatment during and after crises. Third, addressing racial injustice, along with promoting respect for diversity and cultural humility in healthcare settings, may reduce the disparities in how marginalized communities are impacted by disasters. Fourth, strengthening child and family wellbeing through flexible interventions will allow greater access to support during times of crisis and create a healthy foundation for children’s development. Finally, interventions that promote social cohesion will improve access to social support, a key protective factor against stress. Because resilience is an ecological process that requires healthy systems across all levels of society (Masten, 2020), addressing systemic inequalities will enhance both the resilience of individuals and that of society as a whole.
Acknowledgements.
We thank Sarah Hudson for her comments on an early draft of this manuscript.
Funding Statement:
Angelica Carranza was funded by a Eugene Cota Robles Fellowship. Dr. Bidwell is supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant number UL1 TR001860 and linked award KL2 TR001859. Dr. Hostinar is supported by NICHD grant R01 HD104185. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflicts of Interest: None.
References
- Abedi V, Olulana O, Avula V, Chaudhary D, Khan A, Shahjouei S, Li J, & Zand R (2021). Racial, economic, and health inequality and COVID-19 infection in the United States. Journal of Racial and Ethnic Health Disparities, 8(3), 732–742. 10.1007/s40615-020-00833-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alen NV, Sloan RP, Seeman TE, & Hostinar CE (2020). Childhood parental warmth and heart rate variability in midlife: Implications for health. Personal Relationships, 27(3), 506–525. 10.1111/pere.12329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida M, Shrestha AD, Stojanac D, & Miller LJ (2020). The impact of the COVID-19 pandemic on women's mental health. Archives in Women’s Mental Health, 23(6), 741–748. doi: 10.1007/s00737-020-01092-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anastas TM, Miller MM, Hollingshead NA, Stewart JC, Rand KL, & Hirsh AT (2020). The unique and interactive effects of patient race, patient socioeconomic status, and provider attitudes on chronic pain care decisions. Annals of Behavioral Medicine, 54(10), 771–782. 10.1093/abm/kaaa016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrasfay T, & Goldman N (2021). Reductions in 2020 US life expectancy due to COVID-19 and the disproportionate impact on the Black and Latino populations. Proceedings of the National Academy of Sciences, 118(5), e2014746118. 10.1073/pnas.2014746118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arpey NC, Gaglioti AH, & Rosenbaum ME (2017). How socioeconomic status affects patient perceptions of health care: A qualitative study. Journal of Primary Care & Community Health, 8(3), 169–175. 10.1177/2150131917697439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assari S, Moazen-Zadeh E, Caldwell CH, & Zimmerman MA (2017). Racial discrimination during adolescence predicts mental health deterioration in adulthood: Gender differences among Blacks. Frontiers in Public Health, 5, 104. 10.3389/fpubh.2017.00104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker S, Sanders MR, Turner K, & Morawska A (2017). A randomized controlled trial evaluating a low-intensity interactive online parenting intervention, Triple P Online Brief, with parents of children with early onset conduct problems. Behaviour research and therapy, 91, 78–90. 10.1016/j.brat.2017.01.016 [DOI] [PubMed] [Google Scholar]
- Banerjee D, & Rai M (2020). Social isolation in Covid-19: The impact of loneliness. International Journal of Social Psychiatry, 66(6), 525–527. 10.1177/0020764020922269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banskota S, Healy M, & Goldberg E (2020). 15 smartphone apps for older adults to use while in isolation during the COVID-19 pandemic. Western Journal of Emergency Medicine, 21(3). 10.5811/westjem.2020.4.47372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barcellos S, Jacobson M, & Stone AA (2021). Varied and unexpected changes in the well-being of seniors in the United States amid the COVID-19 pandemic. PloS one, 16(6), e0252962. 10.1371/journal.pone.0252962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett MA (2008). Economic disadvantage in complex family systems: Expansion of family stress models. Clinical Child and Family Psychology Review, 11, 145–161. 10.1007/s10567-008-0034-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry JW (1997). Immigration, acculturation, and adaptation. Applied Psychology: An International Review, 46(1), 5–68. [Google Scholar]
- Bartik AW, Bertrand M, Cullen Z, Glaeser EL, Luca M, & Stanton C (2020). The impact of COVID-19 on small business outcomes and expectations. PNAS, 117(30). 10.1073/pnas.2006991117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartlett JD & Stratford B (2021, January 28). A national agenda for children’s mental health. Child Trends. Retrieved from: https://www.childtrends.org/publications/a-national-agenda-for-childrens-mental-health [Google Scholar]
- Batko S, Solari CD, & DuBois N (2021). The Value of Ending Veteran and Chronic Homelessness in Four Communities. [Google Scholar]
- Bauer GR (2014). Incorporating intersectionality theory into population health research methodology: Challenges and the potential to advance health equity. Social Science & Medicine, 110, 10–17. 10.1016/j.socscimed.2014.03.022 [DOI] [PubMed] [Google Scholar]
- Bauerly BC, McCord RF, Hulkower R, & Pepin D (2019). Broadband access as a public health issue: The role of law in expanding broadband access and connecting underserved communities for better health outcomes. The Journal of Law, Medicine & Ethics, 47(2_suppl), 39–42. 10.1177/1073110519857314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach SR, Schulz R, Donovan H, & Rosland AM (2021). Family caregiving during the COVID-19 pandemic. Gerontologist, 61(5), 650–660. doi: 10.1093/geront/gnab049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellis MA, Hughes K, Ford K, Ramos Rodriguez G, Sethi D, & Passmore J (2019). Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: A systematic review and meta-analysis. The Lancet. Public Health, 4(10), e517–e528. 10.1016/S2468-2667(19)30145-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger LM (2005). Income, family characteristics, and physical violence toward children. Child Abuse & Neglect, 29(2), 107–133. 10.1016/j.chiabu.2004.02.006 [DOI] [PubMed] [Google Scholar]
- Berlin LJ, Appleyard K, & Dodge KA (2011). Intergenerational continuity in child maltreatment: Mediating mechanisms and implications for prevention. Child Development, 82(1), 162–176. 10.1111/j.1467-8624.2010.01547.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhaskar S, Rastogi A, Menon KV, Kunheri B, Balakrishnan S, & Howick J (2020). Call for action to address equity and justice divide during COVID-19. Frontiers in Psychiatry, 11, 559905. 10.3389/fpsyt.2020.559905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitler M, Hoynes HW, & Schanzanbach DW (2020). The social safety net in the wake of COVID-19. NBER Working Paper. Retrieved from https://www.nber.org/papers/w27796. doi: 10.3386/w27796 [DOI] [Google Scholar]
- Blair C, & Raver CC (2016). Poverty, stress, and brain development: New directions for prevention and intervention. Academic Pediatrics, 16, S30–S36. doi: 10.1016/j.acap.2016.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolin B (2007) Race, class, ethnicity, and disaster vulnerability. In: Handbook of Disaster Research. Handbooks of Sociology and Social Research. Springer, New York, NY. 10.1007/978-0-387-32353-4_7 [DOI] [Google Scholar]
- Bonvicini KA. LGBT healthcare disparities: What progress have we made? Patient Educ Couns. 2017. Dec;100(12):2357–2361. doi: 10.1016/j.pec.2017.06.003. Epub 2017 Jun 10. [DOI] [PubMed] [Google Scholar]
- Botelho MJ, Lima CA (2020). From cultural competence to cultural respect: A critical review of six models. Journal of Nursing Education, 59(6), 311–318. [DOI] [PubMed] [Google Scholar]
- Botts J (2021, February 17). Lawmakers pass $600 stimulus checks plus boost for undocumented workers. Cal Matters. https://calmatters.org/california-divide/2021/02/california-600-stimulus-checks-undocumented-workers/ [Google Scholar]
- Boyer CJ, Rice MJ, Sorrell TR, & Spurling AM (2019). Advancing racial/ethnic and cultural sensitivity among PMHNP students through education, practice, and experience. Journal of the American Psychiatric Nurses Association, 25(6), 487–495. 10.1177/1078390318824651 [DOI] [PubMed] [Google Scholar]
- Bray MJC, Daneshvari NO, Radhakrishnan I, Cubbage J, Eagle M, Southall P, & Nestadt PS (2020). Racial differences in statewide suicide mortality trends in Maryland during the Coronavirus Disease 2019 (COVID-19) pandemic. JAMA Psychiatry. 10.1001/jamapsychiatry.2020.3938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SM, Doom JR, Lechuga-Peña S, Watamura SE, & Koppels T (2020). Stress and parenting during the global COVID-19 pandemic. Child Abuse & Neglect, 110(2), 104699. 10.1016/j.chiabu.2020.104699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brough R, Freedman M, & Phillips DC (2021). Understanding socioeconomic disparities in travel behavior during the COVID-19 pandemic. Journal of Regional Science, 10.1111/jors.12527. Advance online publication. 10.1111/jors.12527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant DJ, Oo M, & Damian AJ (2020). The rise of adverse childhood experiences during the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S193–S194. 10.1037/tra0000711 [DOI] [PubMed] [Google Scholar]
- Bu F, Steptoe A, & Fancourt D (2020). Who is lonely in lockdown? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health, 186, 31–34. 10.1016/j.puhe.2020.06.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess DJ, Warren J, Phelan S, Dovidio J, & van Ryn M (2010). Stereotype threat and health disparities: What medical educators and future physicians need to know. Journal of General Internal Medicine, 25(S2), 169–177. 10.1007/s11606-009-1221-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Cacioppo S, Capitanio JP, & Cole SW (2015). The neuroendocrinology of social isolation. Annual Review of Psychology, 66(1), 733–767. 10.1146/annurev-psych-010814-015240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cahill S, & South K (2002). Policy issues affecting lesbian, gay, bisexual, and transgender people in retirement. Generations: Journal of the American Society on Aging, 26(2), 49–54. https://www.jstor.org/stable/26555142 [Google Scholar]
- Campbell AM (2020). An increasing risk of family violence during the COVID-19 pandemic: Strengthening community collaborations to save lives. Forensic Science International: Reports, 2, 10.1016/j.fsir.2020.100089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention. (2021, April 2). Older Adults and COVID-19. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html
- Centers for Disease Control and Prevention. (2020, April 3). Preventing Adverse Childhood Experiences. https://www.cdc.gov/violenceprevention/aces/fastfact.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fviolenceprevention%2Facestudy%2Ffastfact.html
- Cerna-Turoff I, Fischer HT, Mayhew S, & Devries K (2019). Violence against children and natural disasters: A systematic review and meta-analysis of quantitative evidence. PloS one, 14(5), e0217719. 10.1371/journal.pone.0217719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan J, To H-P, & Chan E (2006). Reconsidering social cohesion: Developing a definition and analytical framework for empirical research. Social Indicators Research, 75, 273–302. [Google Scholar]
- Cheah CSL, Wang C, Ren H, Zong X, Cho HS, & Xue X (2020). COVID-19 racism and mental health in Chinese American families. Pediatrics, 146(5), e2020021816. 10.1542/peds.2020-021816 [DOI] [PubMed] [Google Scholar]
- Chen E, Brody GH, & Miller GE (2017). Childhood close family relationships and health. The American Psychologist, 72(6), 555–566. 10.1037/amp0000067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen JA, Zhang E, & Liu CH (2020). Potential impact of COVID-19–related racial discrimination on the health of Asian Americans. American Journal of Public Health, 110(11), 1624–1627. 10.2105/AJPH.2020.305858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Churchwell K, Elkind M, Benjamin RM, Carson AP, Chang EK, Lawrence W, … & American Heart Association (2020). Call to Action: Structural racism as a fundamental driver of health disparities: A presidential advisory from the American Heart Association. Circulation, 142(24), e454–e468. 10.1161/CIR.0000000000000936 [DOI] [PubMed] [Google Scholar]
- Cobb RJ, Erving CL, & Byrd WC (2021). Perceived COVID-19 health threat increases psychological distress among Black Americans. Ethnic and Racial Studies, 44, 806–818. 10.1080/01419870.2021.1867216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen SA, Kunicki ZJ, Drohan MM, & Greaney ML (2021). Exploring changes in caregiver burden and caregiving intensity due to COVID-19. Gerontology and Geriatric Medicine, 26(7), 2333721421999279. doi: 10.1177/2333721421999279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole ER (2009). Intersectionality and research in psychology. American Psychologist, 64(3), 170–180. 10.1037/a0014564 [DOI] [PubMed] [Google Scholar]
- Condon EM, Dettmer AM, Gee DG, Hagan C, Lee KS, Mayes LC, ... & Tseng WL (2020). Commentary: COVID-19 and mental health equity in the United States. Frontiers in Sociology, 99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger KJ, Rueter MA, & Conger RD (2000). The role of economic pressure in the lives of parents and their adolescents: The family stress model. In Crockett LJ & Silbereisen RK (Eds.), Negotiating adolescence in times of social change (p. 201–223). Cambridge University Press. [Google Scholar]
- Connor J, Madhavan S, Mokashi M, Amanuel H, Johnson NR, Pace LE, & Bartz D (2020). Health risks and outcomes that disproportionately affect women during the Covid-19 pandemic: A review. Social Science and Medicine, 266, 113364. doi: 10.1016/j.socscimed.2020.113364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conradt E, Carter SE, & Crowell SE (2020). Biological embedding of chronic stress across two generations within marginalized communities. Child Development Perspectives, 14(4), 208–214. 10.1111/cdep.12382 [DOI] [Google Scholar]
- Cooper LA, & Williams DR (2020). Excess deaths from COVID-19, community bereavement, and restorative justice for communities of color. JAMA, 324(15), 1491. 10.1001/jama.2020.19567 [DOI] [PubMed] [Google Scholar]
- Crenshaw K (1989). Demarginalizing the Intersection of Race and Sex: A Black Feminist Critique of Antidiscrimination Doctrine, Feminist Theory and Antiracist Politics, University of Chicago Legal Forum: Vol. 1989: Iss. 1, Article 8. [Google Scholar]
- Croucher SM, Nguyen T, & Rahmani D (2020). Prejudice toward Asian Americans in the Covid-19 pandemic: The effects of social media use in the United States. Frontiers in Communication, 5, 39. 10.3389/fcomm.2020.00039 [DOI] [Google Scholar]
- Curtis T, Miller BC, & Berry EH (2000). Changes in reports and incidence of child abuse following natural disasters. Child abuse & neglect, 24(9), 1151–1162. doi: 10.1016/s0145-2134(00)00176-9. [DOI] [PubMed] [Google Scholar]
- Czeisler MÉ, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, … & Rajaratnam SMW (2020). Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. Morbidity and Mortality Weekly Report, 69(32), 1049–1057. 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danaher BG, Seeley JR, Stormshak EA, Tyler MS, Caruthers AS, Moore KJ, & Cardenas L (2018). The Family Check-Up Online Program for Parents of Middle School Students: Protocol for a Randomized Controlled Trial. JMIR research protocols, 7(7), e11106. 10.2196/11106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darling-Hammond S, Michaels EK, Allen AM, Chae DH, Thomas MD, Nguyen TT, & Johnson RC (2020). After “The China Virus” Went Viral: Racially Charged Coronavirus Coverage and Trends in Bias Against Asian Americans. Health Education & Behavior, 47(6), 870–879. 10.1177/1090198120957949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daugherty Douglas M, Dawes DE, Holden KB, & Mack D (2015). Missed policy opportunities to advance health equity by recording demographic data in electronic health records. American Journal of Public Health, 3, 380–388. 10.2105/AJPH.2014.302384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson TM, Price M, McCauley JL, & Ruggiero KJ (2013). Disaster impact across cultural groups: Comparison of Whites, African Americans, and Latinos. American Journal of Community Psychology, 52(1–2), 97–105. 10.1007/s10464-013-9579-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis EP, Hankin BL, Swales DA, & Hoffman MC (2018). An experimental test of the fetal programming hypothesis: Can we reduce child ontogenetic vulnerability to psychopathology by decreasing maternal depression? Development and psychopathology, 30(3), 787–806. 10.1017/S0954579418000470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deer LK, Bernard K, & Hostinar CE (2019). The influence of maternal stress and child maltreatment on offspring. In Welling L & Shackelford T (Eds.), Oxford Handbook on Evolutionary Psychology and Behavioral Endocrinology (pp. 161–177). New York: Oxford University Press. [Google Scholar]
- Deer LK, Shields GS, Ivory SL, Hostinar CE, & Telzer EH (2018). Racial/ethnic disparities in cortisol diurnal patterns and affect in adolescence. Development and psychopathology, 30(5), 1977–1993. 10.1017/S0954579418001098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demeke HB, Zilversmit Pao L, Clark H, Romero L, Neri A, Shah R, … & Rose MA (2020). Telehealth practice among health centers during the COVID-19 pandemic - United States, July 11-17, 2020. Morbidity and Mortality Weekly Report, 69(50), 1902–1905. 10.15585/mmwrmm.6950a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DePasquale CE, Parenteau A, Kenney M, & Gunnar MR (2020). Brief stress reduction strategies associated with better behavioral climate in a crisis nursery: A pilot study. Children and Youth Services Review, 110, 104813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donagh B (2020). From unnoticed to invisible: The impact of COVID-19 on children and young people experiencing domestic violence and abuse. Child abuse review, 29, 387–391. 10.1002/car.2649 [DOI] [Google Scholar]
- Eckenrode J, Smith EG, McCarthy ME, & Dineen M (2014). Income inequality and child maltreatment in the United States. Pediatrics, 133(3), 454–461. 10.1542/peds.2013-1707 [DOI] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, & Anda RF (2003). Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: results from the adverse childhood experiences study. The American Journal of Psychiatry, 160(8), 1453–1460. 10.1176/appi.ajp.160.8.1453 [DOI] [PubMed] [Google Scholar]
- Eliacin J, Matthias MS, Cunningham B, & Burgess DJ (2020). Veterans’ perceptions of racial bias in VA mental healthcare and their impacts on patient engagement and patient-provider communication. Patient Education and Counseling, 103(9), 1798–1804. 10.1016/j.pec.2020.03.017 [DOI] [PubMed] [Google Scholar]
- Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, & Galea S (2020). Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open, 3(9), e2019686. doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans GW, & Kim P (2010). Multiple risk exposure as a potential explanatory mechanism for the socioeconomic status-health gradient. Annals of the New York Academy of Sciences, 1186, 174–189. 10.1111/j.1749-6632.2009.05336.x [DOI] [PubMed] [Google Scholar]
- Feldmeyer B, Madero-Hernandez A, Rojas-Gaona CE, & Sabon LC (2019). Immigration, collective efficacy, social ties, and violence: Unpacking the mediating mechanisms in immigration effects on neighborhood-level violence. Race and Justice, 9(2), 123–150. [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, … & Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Finch C, Emrich CT & Cutter SL (2010). Disaster disparities and differential recovery in New Orleans. Population and Environment, 31, 179–202. 10.1007/s11111-009-0099-8 [DOI] [Google Scholar]
- Fitzpatrick KM, Harris C, & Drawve G (2020). Fear of COVID-19 and the mental health consequences in America. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S17–S21. 10.1037/tra0000924 [DOI] [PubMed] [Google Scholar]
- Forde AT, Crookes DM, Suglia SF, & Demmer RT (2019). The weathering hypothesis as an explanation for racial disparities in health: A systematic review. Annals of Epidemiology, 33, 1–18.e3. doi: 10.1016/j.annepidem.2019.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fothergill A, & Peek LA (2004). Poverty and disasters in the United States: A review of recent sociological findings. Natural Hazards, 32, 89–110 (2004). 10.1023/B:NHAZ.0000026792.76181.d9 [DOI] [Google Scholar]
- Flentje A, Obedin-Maliver J, Lubensky ME, Dastur Z, Neilands T, & Lunn MR (2020). Depression and anxiety changes among sexual and gender minority people coinciding with onset of COVID-19 pandemic. Journal of General Internal Medicine, 1–3. 10.1007/s11606-020-05970-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French SE, Seidman E, Allen L, & Aber JL (2006). The development of ethnic identity during adolescence. Developmental Psychology, 42(1), 1–10. 10.1037/0012-1649.42.1.1 [DOI] [PubMed] [Google Scholar]
- Fuchs JD, Carter HC, Evans J, Graham-Squire D, Imbert E, Bloome J, … & Kanzaria HK (2021). Assessment of a hotel-based COVID-19 isolation and quarantine strategy for persons experiencing homelessness. JAMA Network Open, 4(3), e210490. doi: 10.1001/jamanetworkopen.2021.0490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadermann AC, Thomson KC, Richardson CG, Gagné M, McAuliffe C, Hirani S, & Jenkins E (2021). Examining the impacts of the COVID-19 pandemic on family mental health in Canada: findings from a national cross-sectional study. BMJ Open, 12, 11(1), e042871. doi: 10.1136/bmjopen-2020-042871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcini L, Murray K, Zhou A, Klonoff E, Myers M, & Elder J (2016). Mental health of undocumented immigrant adults in the United States: A systematic review of methodology and findings. Journal of Immigrant & Refugee Studies, 14(1), 1–25. [Google Scholar]
- Gato J, Barrientos J, Tasker F, Miscioscia M, Cerqueira-Santos E, Malmquist A, … & Wurm M, (2021) Psychosocial effects of the COVID-19 pandemic and mental health among LGBTQ+ young adults: A cross-cultural comparison across six nations. Journal of Homosexuality, 68(4), 612–630. doi: 10.1080/00918369.2020.1868186. [DOI] [PubMed] [Google Scholar]
- Gendron T, Maddux S, Krinsky L, White J, Lockerman K, Metcalfe Y, & Aggarwal S (2013). Cultural competence training for healthcare professionals working with LGBT older adults. Educational Gerontology, 39(6), 454–463. 10.1080/03601277.2012.701114 [DOI] [Google Scholar]
- Georgetown University Center on Education and the Workforce. (2021). Tracking COVID-19 Unemployment and Job Losses. https://cew.georgetown.edu/cew-reports/jobtracker/#tool-3-tracking
- Germani A, Buratta L, Delvecchio E, & Mazzeschi C (2020). Emerging adults and COVID-19: The role of individualism-collectivism on perceived risks and psychological maladjustment. International Journal of Environmental Research and Public Health, 17(10), 3497. 10.3390/ijerph17103497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT (1992). The weathering hypothesis and the health of African-American women and infants: Evidence and speculations. Ethnicity & Disease, 2(3), 207–221. [PubMed] [Google Scholar]
- Gilbert LK, Breiding MJ, Merrick MT, Thompson WW, Ford DC, Dhingra SS, & Parks SE (2015). Childhood adversity and adult chronic disease: An update from ten states and the District of Columbia, 2010. American Journal of Preventive Medicine, 48(3), 345–349. 10.1016/j.amepre.2014.09.006 [DOI] [PubMed] [Google Scholar]
- Glass VQ, & Bickler A (2021). Cultivating the therapeutic alliance in a telemental health setting. Contemporary Family Therapy, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldmann E, & Galea S (2014). Mental health consequences of disasters. Annual Reviews of Public Health, 35, 169–83. doi: 10.1146/annurev-publhealth-032013-182435. [DOI] [PubMed] [Google Scholar]
- Gonzales G, de Mola EL, Gavulic KA, McKay T, & Purcell C (2020). Mental health needs among lesbian, gay, bisexual, and transgender college students during the COVID-19 pandemic. Journal of Adolescent Health, 67(5), 645–648. doi: 10.1016/j.jadohealth.2020.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodsmith N, Ijadi-Maghsoodi R, Melendez RM, & Dossett EC (2021). Addressing the urgent housing needs of vulnerable women in the era of COVID-19: The Los Angeles county experience. Psychiatric Services,72(3), 349–352. doi: 10.1176/appi.ps.202000318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorczynski P, & Fasoli F (2020). LGBTQ+ focused mental health research strategy in response to COVID-19. The Lancet. Psychiatry, 7(8), e56. 10.1016/S2215-0366(20)30300-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould E, & Wilson V (2020, June 1). Black workers face two of the most lethal preexisting conditions for coronavirus—Racism and economic inequality. https://www.epi.org/publication/black-workers-covid/ [Google Scholar]
- Gunnar MR, & Hostinar CE (2015). The social buffering of the hypothalamic-pituitary-adrenocortical axis in humans: Developmental and experiential determinants. Social Neuroscience, 10(5), 479–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo J, Fu M, Liu D, Zhang B, Wang X, & van Ijzendoorn MH (2020). Is the psychological impact of exposure to COVID-19 stronger in adolescents with pre-pandemic maltreatment experiences? A survey of rural Chinese adolescents. Child Abuse and Neglect, 110, 10.1016/j.chiabu.2020.104667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hacker K, Anies M, Folb BL, & Zallman L (2015). Barriers to health care for undocumented immigrants: A literature review. Risk Management and Healthcare Policy, 8, 175–183. 10.2147/RMHP.S70173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handa S, Daidone S, Peterman A, Davis B, Pereira A, Palermo T, & Yablonski J (2018). Myth-busting? Confronting six common perceptions about unconditional cash transfers as a poverty reduction strategy in Africa. The World Bank Research Observer, 33(2), 259–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haushofer J, Ringdal C, Shapiro JP, & Wang XY, (2019). Income changes and intimate partner violence: Evidence from unconditional cash transfers in Kenya [Working paper]. National Bureau of Economic Research, 10.3386/w25627 [DOI] [Google Scholar]
- Hawkins D (2020). Differential occupational risk for COVID-19 and other infection exposure according to race and ethnicity. American Journal of Industrial Medicine, 63(9), 817–820. 10.1002/ajim.23145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herzog JI & Schmahl C (2018). Adverse childhood experiences and the consequences on the neurobiological, psychosocial, and somatic conditions across the lifespan. Frontiers in Psychiatry, 9. 10.3389/fpsyt.2018.00420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibel LC, Boyer CJ, Buhler-Wassmann AC, & Shaw BJ (2021). The psychological and economic toll of the COVID-19 pandemic on Latina mothers in primarily low-income essential worker families. Traumatology. Advance online publication. 10.1037/trm0000293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill TD, & Jorgenson A (2018). Bring out your dead! A study of income inequality and life expectancy in the United States, 2000-2010. Health & place, 49, 1–6. 10.1016/j.healthplace.2017.11.001 [DOI] [PubMed] [Google Scholar]
- Hoffman KM, Trawalter S, Axt JR, & Oliver MN (2016). Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proceedings of the National Academy of Sciences of the United States of America, 113(16), 4296–4301. 10.1073/pnas.1516047113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hostinar CE (2015). Recent developments in the study of social relationships, stress responses, and physical health. Current Opinion in Psychology, 5, 90–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hostinar CE, Lachman ME, Mroczek DK, Seeman TE, & Miller GE (2015). Additive contributions of childhood adversity and recent stressors to inflammation at midlife: Findings from the MIDUS study. Developmental psychology, 51(11), 1630–1644. 10.1037/dev0000049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hostinar CE, & Miller GE (2019). Protective factors for youth confronting economic hardship: Current challenges and future avenues in resilience research. American Psychologist, 74(6), 641–652. 10.1037/amp0000520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hostinar CE, Nusslock R, & Miller GE (2018). Future directions in the study of early-life stress, physical and emotional health: Implications of the neuroimmune network hypothesis. Journal of Clinical Child and Adolescent Psychology, 47(1), 142–156. doi: 10.1080/15374416.2016.1266647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hostinar CE, Swartz JR, Alen NV, Guyer AE, & Hastings PD (2021). The role of stress phenotypes in understanding childhood adversity as a transdiagnostic risk factor for psychopathology. Journal of Abnormal Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House JS, Landis KR, & Umberson D (1988). Social relationships and health. Science, 241, 540–545. [DOI] [PubMed] [Google Scholar]
- Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, … & Dunne MP (2017). The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. The Lancet. Public health, 2(8), e356–e366. 10.1016/S2468-2667(17)30118-4 [DOI] [PubMed] [Google Scholar]
- Hughes V, Delva S, Nkimbeng M, Spaulding E, Turkson-Ocran RA, Cudjoe J, … & Han HR (2020). Not missing the opportunity: Strategies to promote cultural humility among future nursing faculty. Journal of Professional Nursing, 36(1), 28–33. 10.1016/j.profnurs.2019.06.005 [DOI] [PubMed] [Google Scholar]
- Hurtado A (1989). Relating to Privilege: Seduction and Rejection in the Subordination of White Women and Women of Color. Signs: Journal of Women in Culture and Society, 14(4), 833–855. 10.1086/494546 [DOI] [Google Scholar]
- Hwang WC, & Goto S (2008). The impact of perceived racial discrimination on the mental health of Asian American and Latino college students. Cultural Diversity and Ethnic Minority Psychology, 14(4), 326. [DOI] [PubMed] [Google Scholar]
- Inzlicht M, Tullett AM, & Gutsell JN (2012). Stereotype threat spillover: The short- and long-term effects of coping with threats to social identity. In Inzlicht M & Schmader T (Eds.), Stereotype threat: Theory, process, and application (p. 107–123). Oxford University Press. [Google Scholar]
- Jaffe DH, Lee L, Huynh S, & Haskell TP (2020). Health inequalities in the use of telehealth in the United States in the lens of COVID-19. Population Health Management, 23(5), 368–377. 10.1089/pop.2020.0186 [DOI] [PubMed] [Google Scholar]
- John-Henderson NA (2020). Childhood trauma as a predictor of changes in sleep quality in American Indian adults during the COVID-19 pandemic. Sleep Health, 6, 718–722. 10.1016/j.sleh.2020.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- John-Henderson NA, & Ginty AT (2020). Historical trauma and social support as predictors of psychological stress responses in American Indian adults during the COVID-19 pandemic. Journal of Psychosomatic Research, 139, 110263. doi: 10.1016/j.jpsychores.2020.110263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones AD (2017). Food insecurity and mental health status: A global analysis of 149 countries. American Journal of Preventive Medicine, 53(2), 264–273. 10.1016/j.amepre.2017.04.008 [DOI] [PubMed] [Google Scholar]
- Kamal K, Li JJ, Hahm HC, & Liu CH (2021). Psychiatric impacts of the COVID-19 global pandemic on U.S. sexual and gender minority young adults. Psychiatry Research, 299, 113855. 10.1016/j.psychres.2021.113855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman EA, McDonell MG, Cristofalo MA, & Ries RK (2012). Exploring barriers to primary care for patients with severe mental illness: Frontline patient and provider accounts. Issues in Mental Health Nursing, 33(3), 172–180, 10.3109/01612840.2011.638415 [DOI] [PubMed] [Google Scholar]
- Kim SJ, & Bostwick W (2020). Social vulnerability and racial inequality in COVID-19 deaths in Chicago. Health Education & Behavior, 47(4), 509–513. 10.1177/1090198120929677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H, Rackoff GN, Fitzsimmons-Craft EE, Shin KE, Zainal NH, Schwob JT, Eisenberg D, … & Newman MG (2021). College Mental Health Before and During the COVID-19 Pandemic: Results From a Nationwide Survey. Cognitive therapy and research, 1–10. Advance online publication. 10.1007/s10608-021-10241-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinman G, Teoh K, & Harriss A (2020). Supporting the well-being of healthcare workers during and after COVID-19. Occupational Medicine, 70(5), 294–296. 10.1093/occmed/kqaa096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kneale D, & Bécares L (2021). Discrimination as a predictor of poor mental health among LGBTQ+ people during the COVID-19 pandemic: Cross-sectional analysis of the online Queerantine study. BMJ open, 11(6), e049405. 10.1136/bmjopen-2021-049405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotwal AA, Holt-Lunstad J, Newmark RL, Cenzer I, Smith AK, Covinsky KE, & Perissinotto CM (2021). Social isolation and loneliness among San Francisco Bay Area older adults during the COVID −19 shelter-in-place orders. Journal of the American Geriatrics Society, 69(1), 20–29. 10.1111/jgs.16865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer MR, & Hogue CR (2009). Is segregation bad for your health? Epidemiologic Reviews, 31(1), 178–194. 10.1093/epirev/mxp001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N (2020). Measures of Racism, Sexism, Heterosexism, and Gender Binarism for Health Equity Research: From Structural Injustice to Embodied Harm-An Ecosocial Analysis. Annual Reviews of Public Health, 41, 37–62. doi: 10.1146/annurev-publhealth-040119-094017. [DOI] [PubMed] [Google Scholar]
- Kugelmass H (2016). “Sorry, I’m not accepting new patients”: An audit study of access to mental health care. Journal of Health and Social Behavior, 57(2), 168–183. 10.1177/0022146516647098 [DOI] [PubMed] [Google Scholar]
- Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, … & Hu S (2020). Factors associated with mental health outcomes among health care workers exposed to Coronavirus Disease 2019. JAMA Network Open, 3(3), e203976. 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laster Pirtle WN, & Wright T (2021). Structural Gendered Racism Revealed in Pandemic Times: Intersectional Approaches to Understanding Race and Gender Health Inequities in COVID-19. Gender & Society, 35(2), 168–179. 10.1177/08912432211001302 [DOI] [Google Scholar]
- Lawson M, Piel MH, & Simon M (2020). Child maltreatment during the COVID-19 pandemic: Consequences of parental job loss on psychological and physical abuse towards children. Child Abuse & Neglect, 110(2), 104709. 10.1016/j.chiabu.2020.104709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee D (2020). The impact of natural disasters on neighborhood poverty rate: A neighborhood change perspective. Journal of Planning Education and Research, 40(4), 447–459. 10.1177/0739456X18769144 [DOI] [Google Scholar]
- Lee S, Chung JE, & Park N (2018). Network environments and well-being: An examination of personal network structure, social capital, and perceived social support. Health communication, 33(1), 22–31. [DOI] [PubMed] [Google Scholar]
- Lee SJ, Ward KP, Lee JY, & Rodriguez CM (2021). Parental social isolation and child maltreatment risk during the COVID-19 pandemic. Journal of Family Violence. 10.1007/s10896-020-00244-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leijten P, Shaw DS, Gardner F, Wilson MN, Matthys W, & Dishion TJ (2015). The Family Check-Up and service use in high-risk families of young children: A prevention strategy with a bridge to community-based treatment. Prevention Science, 16(3), 397–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levenson T (2020). Conservatives try to rebrand the coronavirus. http://www.theatlantic.com/ideas/archive/2020/03/stop-trying-make-wuhan-virus-happen/607786/. [Google Scholar]
- Leventhal T, & Brooks-Gunn J (2003). Moving to opportunity: An experimental study of neighborhood effects on mental health. American Journal of Public Health, 93(9), 1576–1582. 10.2105/ajph.93.9.1576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, & Van Dyke ME (2018). Discrimination and the Health of African Americans: The Potential Importance of Intersectionalities. Current Directions in Psychological Science, 27(3), 176–182. 10.1177/0963721418770442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, & Galea S (2020). Racism and the COVID-19 epidemic: Recommendations for health care workers. American Journal of Public Health, 110(7), 956–957. 10.2105/AJPH.2020.305698 [DOI] [Google Scholar]
- Lick DJ, Durso LE, & Johnson KL (2013). Minority stress and physical health among sexual minorities. Perspectives on Psychological Science, 8(5), 521–548. [DOI] [PubMed] [Google Scholar]
- Liem A, Andre MNR, Hannam K, Lam AIF, & Hall BJ (2021). Acculturative stress and coping among migrant workers: A global mixed-methods systematic review. Applied Psychology Health and Well-Being, Epub ahead of print, 1–27. [DOI] [PubMed] [Google Scholar]
- Link BG & Phelan JC (1995). Social conditions as fundamental causes of disease. Journal of Health and Social Behavior, 35, 80–94. 10.2307/2626958 [DOI] [PubMed] [Google Scholar]
- Liu CH, Erdei C, & Mittal L (2021). Risk factors for depression, anxiety, and PTSD symptoms in perinatal women during the COVID-19 Pandemic. Psychiatry Research, 295, 113552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu CH, Zhang E, Wong G, Hyun S, & Hahm HC (2020). Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry research, 290, 113172. 10.1016/j.psychres.2020.113172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loopstra R (2018). Interventions to address household food insecurity in high-income countries. The Proceedings of the Nutrition Society, 77(3), 270–281. 10.1017/S002966511800006X [DOI] [PubMed] [Google Scholar]
- Luchetti M, Lee JH, Aschwanden D, Sesker A, Strickhouser JE, Terracciano A, & Sutin AR (2020). The trajectory of loneliness in response to COVID-19. American Psychologist, 75(7), 897–908. 10.1037/amp0000690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludwig J, Duncan GJ, Gennetian LA, Katz LF, Kessler RC, Kling JR, & Sanbonmatsu L (2012). Neighborhood effects on the long-term well-being of low-income adults. Science, 337(6101), 1505–1510. 10.1126/science.1224648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Kumar NL, & Benoit R (2019). Toward fostering resilience on large scale: Connecting communities of caregivers. Development and Psychopathology, 31, 1813–1825. DOI: 10.1017/S0954579419001251 [DOI] [PubMed] [Google Scholar]
- Mackey K, Ayers CK, Kondo KK, Saha S, Advani SM, Young S, & Kansagara D (2020). Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: A systematic review. Annals of Internal Medicine, M20–6306. Advance online publication. 10.7326/M20-6306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maestripieri L (2021). The Covid-19 Pandemics: Why Intersectionality Matters. Frontiers in Sociology, 6, 642662. 10.3389/fsoc.2021.642662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahaffey BL, Levinson A, Preis H, & Lobel M (2021). Elevated risk for obsessive-compulsive symptoms in women pregnant during the COVID-19 pandemic. Archives of Women's Mental Health, 10.1007/s00737-021-01157-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maragh-Bass AC, Torain M, Adler R, Schneider E, Ranjit A, Kodadek LM, – & Haider AH (2017). Risks, benefits, and importance of collecting sexual orientation and gender identity data in healthcare settings: A multi-method analysis of patient and provider perspectives. LGBT Health, 4(2), 141–152. 10.1089/lgbt.2016.0107 [DOI] [PubMed] [Google Scholar]
- Marr C (2021). Biden-Harris Child Tax Credit Expansion Would Lift 10 Million Children Above or Closer to Poverty Line. Center on Budget and Policy Priorities. Retrieved from: www.cbpp.org/blog/biden-harris-child-tax-credit-expansion-would-lift-10-million-children-above-or-closer-to. [Google Scholar]
- Masten AS (2020). Resilience of children in disasters: A multisystem perspective. International Journal of Psychology. 10.1002/ijop.12737 [DOI] [PubMed] [Google Scholar]
- McCall L (2005). The complexity of intersectionality. Signs: Journal of women in culture and society, 30(3), 1771–1800. [Google Scholar]
- McEwen BS (2018). How are emotions organized and physically embodied? In The Nature of Emotion (Second Edition, pp. 299–302). Oxford University Press. [Google Scholar]
- McEwen BS & Chattarji S (2007). Neuroendocrinology of stress. In Handbook of neurochemistry and molecular neurobiology (3rd ed., pp. 572–593). Springer-Verlag. [Google Scholar]
- McEwen BS, & Gianaros PJ (2010). Central role of the brain in stress and adaptation: Links to socioeconomic status, health, and disease. Annals of the New York Academy of Sciences, 1186, 190–222. 10.1111/j.1749-6632.2009.05331.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS, & Gianaros PJ (2011). Stress- and allostasis-induced brain plasticity. Annual Review of Medicine, 62(1), 431–445. 10.1146/annurev-med-052209-100430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKnight-Eily LR, Okoro CA, Strine TW, Verlenden J, Hollis ND, Njai R, … & Thomas C (2021). Racial and ethnic disparities in the prevalence of stress and worry, mental health conditions, and increased substance use among adults during the COVID-19 pandemic - United States, April and May 2020. Morbidity and mortality weekly report, 70(5), 162–166. 10.15585/mmwr.mm7005a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mead A (2020, July 30). Mental health in a pandemic. Rural Health Voices. Retrieved from https://www.ruralhealthweb.org/blogs/ruralhealthvoices/july-2020/mental-health-in-a-pandemic-q-a-with-thomasine-he [Google Scholar]
- Melendez Guevara AM, Lindstrom Johnson S, Elam K, Hilley C, McIntire C, & Morris K (2021). Culturally responsive trauma-informed services: A multilevel perspective from practitioners serving Latinx children and families. Community Mental Health Journal, 57(2), 325–339. [DOI] [PubMed] [Google Scholar]
- Menon DU, & Belcher H (2020). COVID-19 pandemic health disparities and pediatric health care-The promise of telehealth. JAMA Pediatrics, 10.1001/jamapediatrics.2020.5097. Advance online publication. 10.1001/jamapediatrics.2020.5097 [DOI] [PubMed] [Google Scholar]
- Merino Y, Adams L, & Hall WJ (2018). Implicit bias and mental health professionals: Priorities and directions for research. Psychiatric Services, 69(6), 723–725. 10.1176/appi.ps.201700294 [DOI] [PubMed] [Google Scholar]
- Metzler M, Merrick MT, Klevens J, Ports KA, & Ford DC (2017). Adverse childhood experiences and life opportunities: Shifting the narrative. Children and Youth Services Review, 72, 141–149. 10.1016/j.childyouth.2016.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miconi D, Li ZY, Founfelker RL, Santavicca T, Cénat JM, Venkatesh V, & Rousseau C (2020). Ethno-cultural disparities in mental health during the COVID-19 pandemic: A cross-sectional study on the impact of exposure to the virus and COVID-19-related discrimination and stigma on mental health across ethno-cultural groups in Quebec (Canada). BJPsych Open, 7, e14. 10.1192/bjo.2020.146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millan JB, & Alvarez AN (2014). Asian Americans and internalized oppression: Do we deserve this? In David EJR (Ed.), Internalized oppression: The psychology of marginalized groups (p. 163–190). Springer Publishing Company. [Google Scholar]
- Miller GE, Chen E, & Parker KJ (2011). Psychological stress in childhood and susceptibility to the chronic diseases of aging: Moving toward a model of behavioral and biological mechanisms. Psychological Bulletin, 137(6), 959–997. doi: 10.1037/a0024768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monte LM (2020). New Census Household Pulse Survey Shows More Households with Children Lost Income, Experienced Food Shortages During Pandemic. U.S. Census Bureau, Washington, DC. [Google Scholar]
- Morris M, Cooper RL, Ramesh A, Tabatabai M, Arcury TA, Shinn M, … & Matthews-Juarez P (2019). Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: A systematic review. BMC Medical Education, 19, 325. 10.1186/s12909-019-1727-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyce S, Velazquez M, Claudio D, Thompson S, Metcalf M, Aghbashian E, Vanderwood K, & Sisson N (2021). Exploring a rural Latino community's perception of the COVID-19 pandemic. Ethnicity & Health, 26(1), 126–138. 10.1080/13557858.2020.1838456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray-Garcia JL, Harrell S, Garcia JA, Gizzi E, & Simms-Mackey P (2014). Dialogue as skill: Training a health professions workforce that can talk about race and racism. American Journal of Orthopsychiatry, 84(5), 590–596. [DOI] [PubMed] [Google Scholar]
- Nagata JM, Ganson KT, Whittle HJ, Chu J, Harris OO, Tsai AC, & Weiser SD (2021). Food insufficiency and mental health in the U.S. during the COVID-19 pandemic. American Journal of Preventative Medicine, S0749-3797(21)00012-X. doi: 10.1016/j.amepre.2020.12.004. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Bureau of Economic Research (NBER) (2020). US Business Cycle Expansions and Contractions. National Bureau of Economic Research, Cambridge, MA. [Google Scholar]
- New York Times (2021). How George Floyd died, and what happens next. Retrieved January 31, 2022 from https://www.nytimes.com/article/george-floyd.html
- Nguyen TT, Criss S, Dwivedi P, Huang D, Keralis J, Hsu E, … & Nguyen QC (2020). Exploring U.S. shifts in anti-Asian sentiment with the emergence of COVID-19. International Journal of Environmental Research and Public Health, 17(19), 7032. 10.3390/ijerph17197032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olneck-Brown B (2021). Public education’s response to the coronavirus (COVID-19) pandemic. National Conference of State Legislatures. https://www.ncsl.org/research/education/public-education-response-to-coronavirus-covid-19.aspx [Google Scholar]
- Onyeador IN, Wittlin NM, Burke SE, Dovidio JF, Perry SP, Hardeman RR, … &van Ryn M (2020). The Value of Interracial Contact for Reducing Anti-Black Bias Among Non-Black Physicians: A Cognitive Habits and Growth Evaluation (CHANGE) Study Report. Psychological Science, 31(1), 18–30. 10.1177/0956797619879139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortega G, Rodriguez JA, Maurer LR, Witt EE, Perez N, Reich A, & Bates DW(2020). Telemedicine, COVID-19, and disparities: Policy implications. Health policy and technology, 9(3), 368–371. 10.1016/j.hlpt.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page KR, Venkataramani M, Beyrer C, & Polk S (2020). Undocumented US immigrants and Covid-19. The New England Journal of Medicine, 382(21), e62. 10.1056/NEJMp2005953 [DOI] [PubMed] [Google Scholar]
- Parenteau AM, Alen NV, Deer LK, Nissen AT, Luck AT, & Hostinar CE (2020). Parenting matters: Parents can reduce or amplify children's anxiety and cortisol responses to acute stress. Development and Psychopathology, 32(5), 1799–1809. 10.1017/S0954579420001285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park SS (2021). Caregivers' mental health and somatic symptoms during COVID-19. Journal of Gerontolology. Series B: Psychological and Social Sciences, 76(4), e235–e240. doi: 10.1093/geronb/gbaa121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S, Stimpson JP, Pintor JK, Roby DH, McKenna RM, Chen J, & Ortega AN (2019). The effects of the affordable care act on health care access and utilization among Asian American subgroups. Medical Care, 57(11):861–868. doi: 10.1097/MLR.0000000000001202. [DOI] [PubMed] [Google Scholar]
- Parkinson D (2019). Investigating the Increase in Domestic Violence Post Disaster: An Australian Case Study. Journal of Interpersonal Violence, 34(11), 2333–2362. 10.1177/0886260517696876 [DOI] [PubMed] [Google Scholar]
- Parolin Z, Curran MA, & Wimer C (2020). The CARES Act and poverty in the COVID-19 crisis: Promises and pitfalls of the recovery rebates and expanded unemployment benefits. Poverty and Social Policy Brief, 4(8), 1–18. [Google Scholar]
- Peek ME, Kim KE, Johnson JK, & Vela MB (2013). “URM candidates are encouraged to apply”: A national study to identify effective strategies to enhance racial and ethnic faculty diversity in academic departments of medicine. Academic Medicine, 88(3), 405–412. 10.1097/ACM.0b013e318280d9f9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry N, Johnson A, Hostinar C, & Gunnar M (2021). Parental emotional support and social buffering in previously institutionalized and typically developing children and adolescents. Developmental psychobiology, 63(5), 1167–1176. 10.1002/dev.22067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan JC, Link BG, & Tehranifar P (2010). Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. Journal of Health Social Behavior, 51 Suppl, S28–40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- Phelan JC, Link BG, & Tehranifar P (2010). Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. Journal of Health and Social Behavior, 51(1_suppl), S28–S40. 10.1177/0022146510383498 [DOI] [PubMed] [Google Scholar]
- Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, & van Ryn M (2015). Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obesity Reviews, 16(4), 319–326. https://dx.doi.org/10.1111%2Fobr.12266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post RM, & Weiss SRB (1998). Sensitization and kindling phenomena in mood, anxiety, and obsessive-compulsive disorders: The role of serotonergic mechanisms in illness progression. Biological Psychiatry, 44(3), 193–206. doi: 10.1016/S0006-3223(98)00144-9. [DOI] [PubMed] [Google Scholar]
- Power K (2020) The COVID-19 pandemic has increased the care burden of women and families. Sustainability: Science, Practice and Policy, 16(1), 67–73. doi: 10.1080/15487733.2020.1776561 [DOI] [Google Scholar]
- Prasad K, McLoughlin C, Stillman M, Poplau S, Goelz E, Taylor S, … & Sinsky CA (2021). Prevalence and correlates of stress and burnout among U.S. healthcare workers during the COVID-19 pandemic: A national cross-sectional survey study. EClinicalMedicine, 35, 100879. 10.1016/j.eclinm.2021.100879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preis H, Mahaffey B, Heiselman C, & Lobel M (2020). Vulnerability and resilience to pandemic-related stress among U.S. women pregnant at the start of the COVID-19 pandemic. Social science & medicine, 266, 113348. 10.1016/j.socscimed.2020.113348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prentice D & Paluck EL (2020). Engineering social change using social norms: lessons from the study of collective action. Current Opinion in Psychology, 35(1), 138–142. 10.1016/j.copsyc.2020.06.012. [DOI] [PubMed] [Google Scholar]
- Priest N, Perry R, Ferdinand A, Paradies Y, & Kelaher M (2014). Experiences of racism, racial/ethnic attitudes, motivated fairness and mental health outcomes among primary and secondary school students. Journal of Youth and Adolescence, 43(10), 1672–1687. 10.1007/s10964-014-0140-9 [DOI] [PubMed] [Google Scholar]
- Priest N, Slopen N, Woolford S, Philip JT, Singer D, Kauffman AD, Mosely K, Davis M, Ransome Y, & Williams D (2018). Stereotyping across intersections of race and age: Racial stereotyping among White adults working with children. PLOS ONE, 13(9), e0201696. 10.1371/journal.pone.0201696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prime H, Wade M, & Browne DT (2020). Risk and resilience in family well-being during the COVID-19 pandemic. The American psychologist, 75(5), 631–643. 10.1037/amp0000660 [DOI] [PubMed] [Google Scholar]
- Purtle J (2020). COVID-19 and mental health equity in the United States. Social psychiatry and psychiatric epidemiology, 55(8), 969–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi M, Zhou SJ, Guo ZC, Zhang LG, Min HJ, Li XM, & Chen JX (2020). The effect of social support on mental health in chinese adolescents during the outbreak of COVID-19. Journal of Adolescent Health, 67(4), 514–518. 10.1016/j.jadohealth.2020.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reskin B (2012). The race discrimination system. Annual Review of Sociology, 38(1), 17–35. 10.1146/annurev-soc-071811-145508 [DOI] [Google Scholar]
- Ribeiro WS, Bauer A, Andrade M, York-Smith M, Pan PM, Pingani L, … & Evans-Lacko S (2017). Income inequality and mental illness-related morbidity and resilience: a systematic review and meta-analysis. The Lancet. Psychiatry, 4(7), 554–562. 10.1016/S2215-0366(17)30159-1 [DOI] [PubMed] [Google Scholar]
- Riehm KE, Holingue C, Smail EJ, Kapteyn A, Bennett D, Thrul J, Kreuter F, McGinty EE, Kalb LG, Veldhuis CB, Johnson RM, Fallin MD, & Stuart EA (2021). Trajectories of Mental Distress Among U.S. Adults During the COVID-19 Pandemic. Annals of behavioral medicine, 55(2), 93–102. 10.1093/abm/kaaa126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez CM, Silvia PJ, & Pu DF (2018). Predictors of change in mothers’ and fathers’ parent-child aggression risk. Child abuse & neglect, 86, 247–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers AA, Ha T, & Ockey S (2021). Adolescents' perceived socio-emotional impact of COVID-19 and implications for mental health: Results from a U.S.-based mixed-methods study. The Journal of adolescent health, 68(1), 43–52. 10.1016/j.jadohealth.2020.09.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubio A, Oyanedel JC, Bilbao M, Mendiburo-Seguel A, López V, & Páez D (2020). Suicidal ideation mediates the relationship between affect and suicide attempt in adolescents. Frontiers in psychology, 11, 524848. 10.3389/fpsyg.2020.524848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Runkle JD, Yadav S, Michael K, Green S, Weiser J, & Sugg MM (2022). Crisis response and suicidal patterns in U.S. youth before and during COVID-19: A latent class analysis. The Journal of Adolescent Health, 70(1), 48–56. 10.1016/j.jadohealth.2021.10.003 [DOI] [PubMed] [Google Scholar]
- Ruprecht MM, Wang X, Johnson AK, Xu J, Felt D, Ihenacho S, … & Phillips G(2021). Evidence of social and structural COVID-19 disparities by sexual orientation, gender identity, and race/ethnicity in an urban environment. Journal of Urban Health, 98, 27–40. 10.1007/s11524-020-00497-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salerno JP, Shrader CH, Algarin AB, Lee JY, & Fish JN (2021). Changes in alcohol use since the onset of COVID-19 are associated with psychological distress among sexual and gender minority university students in the US. Drug and alcohol dependence, 221, 108594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salerno JP, Williams ND, & Gattamorta KA (2020). LGBTQ populations: Psychologically vulnerable communitites in the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy, 12(1), 239–242. 10.1037/tra0000837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saw YE, Tan EY, Buvanaswari P, Doshi K, & Liu JC (2021). Mental health of international migrant workers amidst large-scale dormitory outbreaks of COVID-19: A population survey in Singapore. Journal of Migration and Health, 4, 100062. 10.1016/j.jmh.2021.100062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawyer PJ, Major B, Casad BJ, Townsend SSM, & Mendes WB (2012). Discrimination and the stress response: Psychological and physiological consequences of anticipating prejudice in interethnic interactions. American Journal of Public Health, 102(5), 1020–1026. 10.2105/AJPH.2011.300620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scaramella LV, Sohr-Preston SL, Callahan KL, & Mirabile SP (2008). A test of the Family Stress Model on toddler-aged children's adjustment among Hurricane Katrina impacted and nonimpacted low-income families. Journal of Clinical Child and Adolescent Psychology, 37(3), 530–541. 10.1080/15374410802148202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schanzenbach D, & Pitts A (2020). How Much Has Food Insecurity Risen? Evidence from the Census Household Pulse Survey. Institute for Policy Research, Northwestern University, Evanston, IL. [Google Scholar]
- Schwartz SJ, Weisskirch RS, Hurley EA, Zamboanga BL, Park IJK, Kim SY, … & Greene AD(2010). Communalism, familism, and filial piety: Are they birds of a collectivist feather? Cultural Diversity and Ethnic Minority Psychology, 16(4), 548–560. doi: 10.1037/a0021370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seddighi H, Salmani I, Javadi MH, & Seddighi S (2019). Child abuse in natural disasters and conflicts: A systematic review. Trauma, violence, & abuse, 22(1), 176–185. 10.1177/1524838019835973 [DOI] [PubMed] [Google Scholar]
- Selden TM, & Berdahl TA (2020). COVID-19 and racial/ethnic disparities in health risk, employment, and household composition: Study examines potential explanations for racial-ethnic disparities in COVID-19 hospitalizations and mortality. Health Affairs, 39(9), 1624–1632. [DOI] [PubMed] [Google Scholar]
- Serafini RA, Powell SK, Frere JJ, Saali A, Krystal HL, Kumar V, Yashaswini C, Hernandez J, Moody K, Aronson A, Meah Y, & Katz CL (2021). Psychological distress in the face of a pandemic: An observational study characterizing the impact of COVID-19 on immigrant outpatient mental health. Psychiatry Research, 295, 113595. 10.1016/j.psychres.2020.113595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serhan Y, & McLaughlin TO (2020, March 12). The other problematic outbreak. 10.1377/hlthaff.2020.00897 [DOI] [Google Scholar]
- Shaefer HL, Collyer S, Duncan G, Edin K, Garfinkel I, Harris D, … & Yoshikawa H(2018). A universal child allowance: A plan to reduce poverty and income instability among children in the United States. The Russell Sage Foundation Journal of the Social Sciences, 4(2), 22–42. 10.7758/RSF.2018.4.2.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shear MD, & Wright W (2021). In Atlanta, Biden Condemns Attacks on Asian-Americans. The New York Times, The New York Times, 26 Mar. 2021, www.nytimes.com/live/2021/03/19/us/atlanta-shootings-massage-spa. [Google Scholar]
- Simon NM, Saxe GN, & Marmar CR (2020). Mental health disorders related to COVID-19–related deaths. JAMA, 324(15), 1493. 10.1001/jama.2020.19632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sneed RS, Key K, Bailey S, & Johnson-Lawrence V (2020). Social and psychological consequences of the COVID-19 pandemic in African-American communities: Lessons from Michigan. Psychological Trauma: Theory, Research, Practice, and Policy, 12(5), 446–448. 10.1037/tra0000881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer SJ, Logel C, & Davies PG (2016). Stereotype threat. Annual Review of Psychology, 67(1), 415–437. 10.1146/annurev-psych-073115-103235 [DOI] [PubMed] [Google Scholar]
- Stevenson B (2020. The Initial Impact of COVID-19 on Labor Market Outcomes across Groups and the Potential for Permanent Scarring. The Hamilton Project, Brookings Institution, Washington, DC. [Google Scholar]
- Stuart EA (2021). Trajectories of mental distress among U.S. adults during the COVID-19 pandemic. Annals of Behavioral Medicine. doi: 10.1093/abm/kaaa126. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Use and Mental Health Services Administration (2020, November 03). Double Jeopardy: COVID-19 and Behavioral Health Disparities for Black and Latino Communities in the U.S. (Submitted by OBHE). https://www.samhsa.gov/sites/default/files/covid19-behavioral-health-disparities-black-latino-communities.pdf
- Swedo E, Idaikkadar N, Leemis R, Dias T, Radhakrishnan L, Stein Z, … & Holland K(2020). Trends in U.S. emergency department visits related to suspected or confirmed child abuse and neglect among children and adolescents aged <18 years before and during the COVID-19 pandemic -- United States, January 2019 - September 2020. Centers for Disease Control and Prevention. https://www.cdc.gov/mmwr/volumes/69/wr/mm6949a1.htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tervalon M, & Murray-Garcia J (1998). Cultural humility versus cultural competence: A critical distinction in defining physician training outcomes in multicultural education. Journal of Health Care for the Poor and Underserved, 9(2), 117–125. [DOI] [PubMed] [Google Scholar]
- Thompson MP, Kingree JB, & Lamis D (2019). Associations of adverse childhood experiences and suicidal behaviors in adulthood in a U.S. nationally representative sample. Child: Care, Health, and Development, 45, 121–128. 10.1111/cch.12617 [DOI] [PubMed] [Google Scholar]
- Townshend I, Awosoga O, & Kulig J (2015). Social cohesion and resilience across communities that have experienced a disaster. Natural Hazards, 76, 913–938 (2015). 10.1007/s11069-014-1526-4 [DOI] [Google Scholar]
- Tsur N & Abu-Raiya H (2020). COVID-19-related fear and stress among individuals who experience child abuse: The mediating effect of complex posttraumatic stress disorder. Child Abuse and Neglect, 110, 10.1016/j.chiabu.2020.104694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JS, D'Amico EJ, Pedersen ER, Garvey R, Rodriguez A, & Klein DJ (2020). Behavioral health and service usage during the COVID-19 pandemic among emerging adults currently or recently experiencing homelessness. Journal of Adolescent Health, 67(4), 603–605. doi: 10.1016/j.jadohealth.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umaña-Taylor AJ, Quintana SM, Lee RM, Cross WE, Rivas-Drake D, Schwartz SJ, … & Ethnic and Racial Identity in the 21st Century Study Group. (2014). Ethnic and racial identity during adolescence and into young adulthood: An integrated conceptualization. Child Development, 85(1), 21–39. 10.1111/cdev.12196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF (n.d.) Coronavirus (COVID-19) Parenting Tips. https://www.unicef.org/coronavirus/covid-19-parenting-tips
- Verdery AM, Smith-Greenaway E, Margolis R, & Daw J (2020). Tracking the reach of COVID-19 kin loss with a bereavement multiplier applied to the United States. Proceedings of the National Academy of Sciences, 117(30), 17695–17701. 10.1073/pnas.2007476117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victor CR, & Bowling A (2012). A longitudinal analysis of loneliness among older people in Great Britain. The Journal of Psychology, 146(3), 313–331. 10.1080/00223980.2011.609572 [DOI] [PubMed] [Google Scholar]
- Wade M, Prime H, Johnson D, May SS, Jenkins JM, & Browne DT (2021). The disparate impact of COVID-19 on the mental health of female and male caregivers. Social Science and Medicine, 275, 10.1016/j.socscimed.2021.113801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- War II. Retrieved from https://www.worldbank.org/en/news/press-release/2020/06/08/covid-19-to-plunge-global-economy-into-worst-recession-since-world-war-ii [Google Scholar]
- Weiner D, Heaton L, Stiehl M, Chor B, Kim K, Heisler K, Foltz R, & Farrell A (2020). Chapin Hall issue brief: COVID-19 and child welfare: Using data to understand trends in maltreatment and response. Chicago, IL: Chapin Hall at the University of Chicago. [Google Scholar]
- Welch M & Haskins R (2020). What COVID-19 means for America’s child welfare system. Brookings. https://www.brookings.edu/research/what-covid-19-means-for-americas-child-welfare-system/ [Google Scholar]
- White K, & Borrell LN (2011). Racial/ethnic residential segregation: Framing the context of health risk and health disparities. Health & Place, 17(2), 438–448. 10.1016/j.healthplace.2010.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widom CS, Czaja SJ, & Dutton MA (2008). Childhood victimization and lifetime revictimization. Child abuse & neglect, 32(8), 785–796. 10.1016/j.chiabu.2007.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiemers EE, Abrahams S, AlFakhri M, Hotz VJ, Schoeni RF, & Seltzer JA (2020). Disparities in vulnerability to complications from COVID-19 arising from disparities in preexisting conditions in the United States. Research in Social Stratification and Mobility, 69, 100553. 10.1016/j.rssm.2020.100553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildman J (2021). COVID-19 and income inequality in OECD countries. European Journal of Health Economics, 22(3), 455–462. doi: 10.1007/s10198-021-01266-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willging CE, Salvador M, & Kano M (2006). Unequal treatment: Mental health care for sexual and gender minority groups in a rural state. Psychiatric Services, 57(6), 867–870. [DOI] [PubMed] [Google Scholar]
- Williams DR (1997). Race and health: Basic questions, emerging directions. Annals of Epidemiology, 7(5), 322–333. 10.1016/S1047-2797(97)00051-3 [DOI] [PubMed] [Google Scholar]
- Williams DR, Lawrence JA, & Davis BA (2019). Racism and health: Evidence and needed research. Annual Review of Public Health, 40(1), 105–125. 10.1146/annurev-publhealth-040218-043750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams K, Ruiz F, Hernandez F, & Hancock M (2020). Home visiting: A lifeline for families during the COVID-19 pandemic. Archives of Psychiatric Nursing, 35(1), 129–133. 10.1016/j.apnu.2020.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams CYK, Townson AT, Kapur M, Ferreira AF, Nunn R et al. (2021). Interventions to reduce social isolation and loneliness during COVID-19 physical distancing measures: A rapid systematic review. PLOS ONE, 16(2), e0247139. 10.1371/journal.pone.0247139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson FA, & Stimpson JP (2020). US policies increase vulnerability of immigrant communities to the COVID-19 pandemic. Annals of Global Health, 86(1), 57. 10.5334/aogh.2897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wise PH, & Chamberlain LJ (2022). Adversity and opportunity-The pandemic’s paradoxical effect on child health and well-being. JAMA Pediatrics. doi: 10.1001/jamapediatrics.2022.0063 [DOI] [PubMed] [Google Scholar]
- Woo JKH, Ghorayeb SH, Lee CK, Sangha H, & Richter S (2004). Effect of patient socioeconomic status on perceptions of first-and second-year medical students. CMAJ-JAMC, 170(13), 1915–1919. https://doi.org/10.1503.cmaj.1031474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank (2020). COVID-19 to plunge global economy into worst recession since World World II. Retrieved from https://www.worldbank.org/en/news/press-release/2020/06/08/covid-19-to-plunge-global-economy-into-worst-recession-since-world-war-ii
- World Health Organization (2022). WHO Coronavirus Dashboard. Retrieved January 24, 2022 from https://covid19.who.int/ [Google Scholar]
- Wrigley-Field E (2020). US racial inequality may be as deadly as COVID-19. Proceedings of the National Academy of Sciences of the United States of America, 117(36), 21854–21856. 10.1073/pnas.2014750117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu SJ, & Paluck EL (2020). Participatory practices at work change attitudes and behavior toward societal authority and justice. Nature Communications, 11(1), 2633. 10.1038/s41467-020-16383-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu W, Xiang L, Proverbs D, & Xiong S (2020). The influence of COVID-19 on community disaster resilience. International Journal of Environmental Research and Public Health, 18(1), 88. 10.3390/ijerph18010088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yip T (2015). The effects of ethnic/racial discrimination and sleep quality on depressive symptoms and self-esteem trajectories among diverse adolescents. Journal of Youth and Adolescence, 44(2), 419–430. 10.1007/s10964-014-0123-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshikawa H, Aber JL, & Beardslee WR (2012). The effects of poverty on the mental, emotional, and behavioral health of children and youth: Implications for prevention. American Psychologist, 67(4), 272–284. 10.1037/a0028015 [DOI] [PubMed] [Google Scholar]
- Yoshikawa H, Wuermli AJ, Britto PR, Dreyer B, Leckman JF, Lye SJ, … & Stein A (2020). Effects of the global Coronavirus Disease-2019 pandemic on early childhood development: Short- and long-term risks and mitigating program and policy actions. Journal of Pediatrics, 223, 188–193. 10.1016/j.jpeds.2020.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Q, Salvador CE, Melani L, Berg MK, Neblett EW, & Kitayama S (2021). Racial residential segregation and economic disparity jointly exacerbate COVID-19 fatality in large American cities. Annals of the New York Academy of Sciences. Epub ahead of print. 10.1111/nyas.14567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamarro G, & Prados MJ (2021). Gender differences in couples' division of childcare, work and mental health during COVID-19. Review of Economics of the Household, 1–30. Advance online publication, 10.1007/s11150-020-09534-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeiders KH (2017). Discrimination, daily stress, sleep, and Mexican-origin adolescents’ internalizing symptoms. Cultural Diversity and Ethnic Minority Psychology, 23(4), 570–575. 10.1037/cdp0000159 [DOI] [PMC free article] [PubMed] [Google Scholar]