Abstract
Background
Neck of femur fractures result in impaired function for older people. Despite surgery, many patients experience a decrease in functional level and poorer health status after the injury. The objectives of this study were (1) to determine the short-term mobility and hip function of geriatric patients who underwent hip replacement surgery for a displaced neck of femur fracture in our local population and (2) to identify factors which affect the functional outcome of these patients.
Methods
Patients aged 60 years and above, who were admitted for neck of femur fracture from January 2017 to December 2020, and treated surgically with arthroplasty, were included. Information on patient demography, comorbidities, perioperative data, mobility, hip function and complications were retrospectively collected. Outcome measures used were independent ambulation and recovery of pre-fracture mobility at 1 year after surgery while hip function was assessed using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) total, pain, stiffness, and physical function scores. Factors associated with these outcomes were analyzed.
Results
168 patients with a mean age of 75.2 (SD 8.4) years met the inclusion criteria. 32.1% of patients regained their pre-fracture mobility and 59.6% remained independent 1 year after surgery. Logistic regression analysis identified age, gender, surgical procedure, and time to surgery as significant contributors to recovery of pre-fracture mobility. Older age and increasing requirement for postoperative ambulatory aid resulted in worse WOMAC total and physical function scores. No significant differences were observed in patient-reported hip function between those who had a total hip arthroplasty and those who had a hemiarthroplasty.
Conclusion
Most geriatric patients with displaced neck of femur fractures did not regain pre-fracture mobility despite surgical treatment with arthroplasty.
Keywords: mobility, hip function, geriatric, neck of femur fracture, arthroplasty
Introduction
Neck of femur fractures remain a global public health concern. With an increasingly aged population worldwide, the incidence is expected to rise in tandem alongside healthcare costs and expenditure.1 Most neck of femur fractures are a result of low-energy trauma in osteoporotic bone and is therefore unsurprisingly more common in the geriatric age group.2
Sustaining a neck of femur fracture is a debilitating and potentially fatal injury for older people, resulting in impaired function, and a high morbidity and mortality. The goal of treatment is to get the patient up on their feet as soon as possible. Surgery allows for early mobilization and ambulation, accelerated rehabilitation and maintenance of independent living, and remains the mainstay of treatment as a conservative approach is associated with an increased mortality rate.3,4 Despite this, many patients experience a decrease in functional level and poorer health status after the injury.5,6 Published research has shown that up to 50% of older people with hip fractures do not reach their pre-fracture levels of functioning 1 year after injury.7
This study presents new data on the short-term mobility and hip function of geriatric patients who underwent hip replacement surgery for a displaced neck of femur fracture in our local population and factors which affect the functional outcome of these patients.
Methods
This study was approved by the Medical Research and Ethics Committee (MREC) of the Malaysian Ministry of Health (NMRR ID-22-01674-PNB). The medical records of all patients who were admitted to the authors’ institution for neck of femur fracture from January 2017 to December 2020 were retrospectively analyzed. Patients aged 60 years and above, who sustained a displaced fracture of the femoral neck, and treated surgically with arthroplasty, were included in this study. Patients who were younger than 60 years old, treated with internal fixation, refused surgical treatment, or had a pathological fracture other than osteoporosis were excluded.
Information was retrieved from inpatient notes, operation theatre records and clinic notes on patient demography, American Society of Anesthesiologists (ASA) status, peri-operative data, preoperative mobility, postoperative mobility, and functional status, as well as complications. Acute fractures were defined as fractures that presented within 3 weeks from the date of injury while neglected fractures were defined as those that presented after 3 weeks. Time to surgery was the duration taken from occurrence of fracture to surgical intervention.
The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) total score (range, 0 to 96), pain score (range, 0 to 20), stiffness score (range, 0 to 8), and physical function score (range, 0 to 68) was used to assess hip function in the outpatient clinic at 1 year follow-up, with higher scores indicating worse pain, stiffness, and functional limitations. The postoperative ambulatory status at 1 year was also recorded routinely. Multiple studies have demonstrated no difference in patient-reported outcome measures (PROMs) between 1 and 2 years.8,9 Therefore, 1 year follow-up data is reasonable for PROMs, rather than the required minimum 2-year data used for survivorship studies.
Sample size was calculated a priori using G*Power software, Germany (version 3.1.9.6). Considering 5% marginal error, 80% power of study and medium effect size, 128 subjects were needed to detect the mean of outcome variables. All data analysis was performed using SPSS version 26.0 (IBM Corp, Armonk, NY, USA) and statistical significance was defined as P < .05. Multiple imputation was used to treat missing data, which were missing at random. Normality was assessed using the Kolmogorov-Smirnov and Shapiro-Wilk tests. To compare between groups, the independent samples t-test, Pearson’s chi-square test, Fisher’s exact test and one-way ANOVA were used, while the Pearson correlation coefficient was used to determine correlation between continuous variables and outcome scores.
Univariate and multivariate logistic regression models were fitted to examine relationships between variables. The multivariate regression model was constructed with purposeful selection of variables, after initially performing univariate analysis on each variable and selecting candidates based on a P-value cut-off point of .25. The performance of the models was assessed using goodness-of-fit tests.
Results
168 patients who fit the inclusion criteria were identified, of which 50 (29.8%) were male and 118 (70.2%) were female (Table 1). The mean age was 75.2 years (SD 8.4; range, 60 to 94), where the vast majority (73.3%) were aged 70 years and above, with the largest age group being 70-79 years old (38.7%). The mean age for males and females were similar (P = .95). Most patients had an ASA 2 status (58.9%), regardless of age group, while 31.0% had an ASA 3 status. 89.3% of patients presented to us with an acute fracture.
Table 1.
Patient Characteristics and Clinical Details (n = 168).
| Gender | |
| Male | 50 (29.8%) |
| Female | 118 (70.2%) |
| Age (years) | 75.2 (8.4) |
| Male | 75.1 (7.9) |
| Female | 75.2 (8.6) |
| Age group | |
| 60-69 years | 45 (26.8%) |
| 70-79 years | 65 (38.7%) |
| 80-89 years | 51 (30.4%) |
| 90-99 years | 7 (4.2%) |
| ASA status | |
| 1 | 17 (10.1%) |
| 2 | 99 (58.9%) |
| 3 | 52 (31.0%) |
| Fracture presentation | |
| Acute | 150 (89.3%) |
| Chronic | 18 (10.7%) |
| Surgical procedure | |
| THA | 74 (44%) |
| HA | 94 (56%) |
| Mode of anaesthesia | |
| General anaesthesia | 112 (66.7%) |
| Regional anaesthesia | 56 (33.3%) |
| Non-hip complications | |
| None | 110 (65.5%) |
| 1 | 46 (27.4%) |
| 2 or more | 12 (7.1%) |
| Hip complications | |
| None | 157 (93.5%) |
| 1 or more | 11 (6.5%) |
| Time to surgery (days) | 19.8 (1.4) |
| Length of stay (days) | 16.9 (8.8) |
| Duration of surgery (mins) | 115.6 (30.6) |
| EBL (ml) | 507.0 (233.6) |
Values for age, time to surgery, length of stay, duration of surgery and EBL are presented as mean (SD). All other values are presented as frequency (percentage). Chronic fractures are defined as those that presented after 3 weeks. ASA: American Society of Anesthesiologists. THA: total hip arthroplasty. HA: hemiarthroplasty. EBL: Estimated blood loss.
44.0% of patients underwent total hip arthroplasty and 56.0% underwent hemiarthroplasty, with the majority subjected to general anesthesia (66.7%). The lateral approach and cemented femoral stems were used in all cases. Cemented acetabular cups were used in all total hip arthroplasties. The mean time to surgery, length of stay, duration of surgery and estimated blood loss (EBL) were 19.8 (SD 1.4) days, 16.9 (SD 8.8) days, 115.6 (SD 30.6) minutes and 491.9 (SD 233.6) ml, respectively. 34.5% of patients experienced 1 or more non-hip related adverse events during their hospital stay, while 6.5% of patients had at least 1 hip complication after surgery.
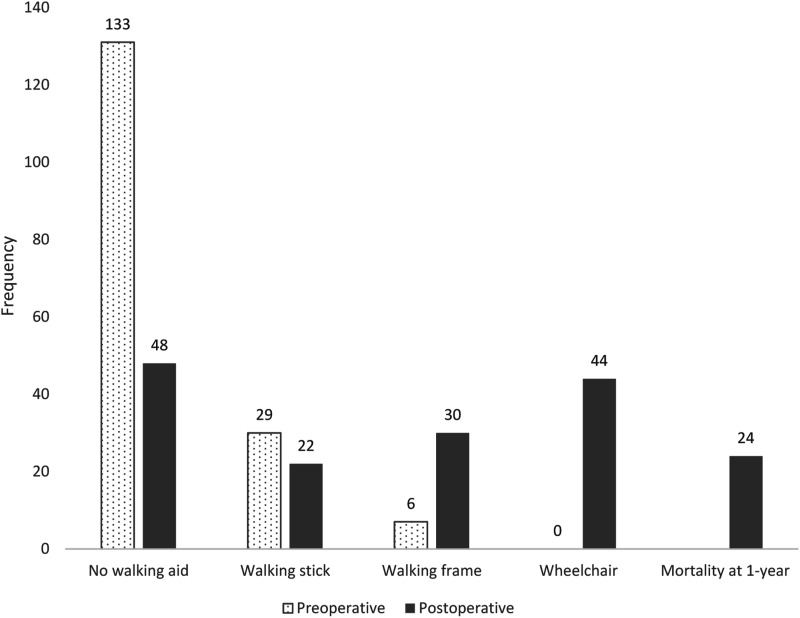
Preoperatively, all patients were able to ambulate independently. 79.1% of patients did not require a walking aid, 17.3% required a walking stick and 3.6% required a walking frame (Table 2, Figure 1). Postoperatively, 59.6% of patients remained independent and 28.6% of patients retained the ability to ambulate without a walking aid. 32.1% of patients regained pre-fracture mobility status. Patients who had a total hip arthroplasty and who did not require a walking aid before surgery were more likely to remain independent 1 year after surgery (Table 3) while patients who regained pre-fracture mobility were more likely to be younger, had an ASA 1 status, underwent total hip arthroplasty, had no non-hip related adverse events during their hospital stay, and did not require a walking aid prior to the injury.
Table 2.
Comparison Between Preoperative and Postoperative Mobility.
| Preoperative | Postoperative (1-year) | Total | ||||
|---|---|---|---|---|---|---|
| Independent | Dependent | Mortality at 1 year | ||||
| No Walking Aid | Walking Stick | Walking Frame | Wheelchair | |||
| No walking aid | 48 | 19 | 17 | 30 | 19 | 133 (79.1%) |
| Walking stick | 0 | 3 | 10 | 11 | 5 | 29 (17.3%) |
| Walking frame | 0 | 0 | 3 | 3 | 0 | 6 (3.6%) |
| Wheelchair | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 48 (28.6%) | 22 (13.1%) | 30 (17.9%) | 44 (26.1%) | 24 (14.3%) | 168 |
Figure 1.
Preoperative and postoperative ambulation, including mortality at 1-year.
Table 3.
Association Between Variables and Postoperative Ambulation at 1-year.
| Variable | Total | Independent Ambulation at 1-year | Recovery of Pre-fracture Mobility | ||||
|---|---|---|---|---|---|---|---|
| Yes | No | P-Value | Yes | No | P-Value | ||
| Overall | 144 | 100 (59.6%) | 44 (26.1%) | 54 (32.1%) | 90 (53.6%) | ||
| Gender | .82a | .12a | |||||
| Male | 44 (30.6%) | 32 (32.0%) | 12 (27.3%) | 14 (25.9%) | 30 (33.3%) | ||
| Female | 100 (69.4%) | 68 (68.0%) | 32 (72.7%) | 40 (74.1%) | 60 (66.7%) | ||
| Age (years) | 74.3 (8.3) | 77.8 (9.1) | .10b | 71.4 (7.1) | 77.7 (8.6) | .00b | |
| Age group | .05c | .00c | |||||
| 60-69 years | 41 (28.4%) | 32 (32.0%) | 9 (20.5%) | 23 (42.6%) | 18 (20.0%) | ||
| 70-79 years | 54 (37.5%) | 37 (37.0%) | 17 (38.6%) | 24 (44.4%) | 30 (33.3%) | ||
| 80-89 years | 44 (30.6%) | 30 (30.0%) | 14 (31.8%) | 7 (13.0%) | 37 (41.1%) | ||
| 90-99 years | 5 (3.5%) | 1 (1.0%) | 4 (9.1%) | 0 | 5 (5.6%) | ||
| ASA status | .11c | .00c | |||||
| 1 | 15 (10.4%) | 12 (12.0%) | 3 (6.8%) | 11 (20.4%) | 4 (4.4%) | ||
| 2 | 88 (61.1%) | 61 (61.0%) | 27 (61.4%) | 32 (59.2%) | 56 (62.2%) | ||
| 3 | 41 (28.5%) | 27 (27.0%) | 14 (31.8%) | 11 (20.4%) | 30 (33.3%) | ||
| Fracture presentation | .19a | .47a | |||||
| Acute | 111 (77.1%) | 82 (82.0%) | 29 (65.9%) | 43 (79.6%) | 68 (75.6%) | ||
| Chronic | 33 (22.9%) | 8 (8.0%) | 5 (11.4%) | 11 (20.4%) | 22 (24.4%) | ||
| Surgical procedure | .00a | .00a | |||||
| THA | 63 (43.8%) | 50 (50.0%) | 13 (29.5%) | 32 (59.3%) | 31 (34.4%) | ||
| HA | 81 (56.3%) | 50 (50.0%) | 31 (70.5%) | 22 (40.7%) | 59 (65.6%) | ||
| Mode of anaesthesia | .39a | .42a | |||||
| General anaesthesia | 92 (63.9%) | 64 (64.0%) | 28 (63.6%) | 39 (72.2%) | 53 (58.9%) | ||
| Regional anaesthesia | 52 (36.1%) | 36 (36.0%) | 16 (36.4%) | 15 (27.8%) | 37 (41.1%) | ||
| Non-hip complications | .31a | .02c | |||||
| None | 79 (54.9%) | 59 (59.0%) | 20 (45.5%) | 38 (70.4%) | 41 (45.6%) | ||
| 1 | 46 (31.9%) | 32 (32.0%) | 14 (31.8%) | 13 (24.1%) | 33 (36.7%) | ||
| 2 or more | 19 (13.2%) | 9 (9.0%) | 10 (22.7%) | 3 (5.6%) | 16 (17.8%) | ||
| Hip complications | .75c | .78c | |||||
| None | 138 (95.8%) | 96 (96.0%) | 42 (95.5%) | 51 (94.4%) | 87 (96.7%) | ||
| 1 or more | 6 (4.2%) | 4 (4.0%) | 2 (4.5%) | 3 (5.6%) | 3 (3.3%) | ||
| Preoperative ambulation | .01c | .00c | |||||
| No walking aid | 114 (79.1%) | 84 (84.0%) | 30 (68.2%) | 48 (88.9%) | 66 (73.3%) | ||
| Walking stick | 24 (16.7%) | 13 (13.0%) | 11 (25.0%) | 3 (5.6%) | 21 (23.3%) | ||
| Walking frame | 6 (4.2%) | 3 (3.0%) | 3 (6.8%) | 3 (5.6%) | 3 (3.3%) | ||
| Time to surgery (days) | 19.6 (17.0) | 19.2 (16.8) | 20.8 (19.4) | .67b | 16.2 (9.6) | 16.7 (7.7) | .84b |
| Length of stay (days) | 16.5 (8.5) | 16.2 (8.9) | 17.2 (7.9) | .57b | 19.3 (16.2) | 19.9 (17.8) | .72b |
| Duration of surgery (mins) | 116.7 (30.9) | 118.4 (30.0) | 111.9 (35.1) | .33b | 123.3 (29.0) | 112.7 (32.0) | .07b |
| EBL (ml) | 507.1 (240.5) | 493.9 (243.4) | 536.9 (253.2) | .55b | 490.6.0 (247.6) | 517.6 (250.9) | .70b |
Values for age, time to surgery, length of stay, duration of surgery and EBL are presented as mean (SD). All other values are presented as frequency (percentage). Chronic fractures are defined as those that presented after 3 weeks. ASA: American Society of Anesthesiologists. THA: total hip arthroplasty. HA: hemiarthroplasty. EBL: Estimated blood loss.
aP-value determined by Pearson’s chi-square test.
bP-value determined by independent samples t-test.
cP-value determined by Fisher’s exact test.
Logistic regression models assessing the relationship of selected variables and 1-year postoperative ambulation are presented for independent ambulation and recovery of pre-fracture mobility (Table 4). In the independent ambulation model, those who underwent total hip arthroplasty had higher odds of being able to ambulate independently 1 year after surgery while those who received regional anesthesia had lower odds. In the recovery of pre-fracture mobility model, increasing age and longer time to surgery had higher odds of being able to retain pre-fracture mobility while being female and having a hemiarthroplasty had lower odds.
Table 4.
Multivariate Logistic Regression Models for Independent Ambulation and Recovery of Pre-Fracture Mobility at 1-Year.
| Variable | Independent Ambulation at 1-year | Recovery of Pre-fracture Mobility | ||
|---|---|---|---|---|
| OR (95% CI) | P-Value | OR (95% CI) | P-Value | |
| Age | 1.02 (.93, 1.11) | .75 | 1.17 (1.02, 1.34) | .02 |
| Gender | ||||
| Male | — | — | Ref | |
| Female | — | — | .01 (.00, .34) | .01 |
| Surgical procedure | ||||
| THA | Ref | Ref | ||
| HA | .03 (.00, .29) | .00 | .00 (.00, .16) | .00 |
| Mode of anaesthesia | ||||
| General anaesthesia | Ref | Ref | ||
| Regional anaesthesia | .08 (.01, .59) | .01 | .38 (.04, 3.96) | .42 |
| Preoperative ambulation | ||||
| No walking aid | Ref | — | — | |
| Walking stick | 3.03 (.55, 16.54) | .20 | — | — |
| Walking frame | 4.28 (.38, 48.23) | .24 | — | — |
| Non-hip complications | ||||
| None | Ref | Ref | ||
| 1 | 4.15 (.64, 27.00) | .14 | 3.22 (.90, 11.56) | .07 |
| 2 or more | 2.09 (.26, 16.98) | .49 | 2.84 (.23, 35.71) | .42 |
| Time to surgery (days) | — | — | 1.10 (1.01, 1.20) | .02 |
| Duration of surgery (mins) | — | — | 1.00 (.97, 1.02) | .77 |
| EBL (ml) | — | — | 1.00 (1.00, 1.00) | .91 |
| Goodness-of-fit statistics | ||||
| Hosmer-lemeshow | P = .75 | P = .925 | ||
| R-square | .24 | .68 | ||
OR: odds ratio. CI: confidence interval. THA: total hip arthroplasty. HA: hemiarthroplasty.
No multicollinearity present in this model.
The average postoperative 1-year WOMAC total, pain, stiffness and physical function scores were 12.7 (SD 11.8), .6 (SD 1.6), .5 (SD 1.5) and 11.7 (SD 11.8) respectively. No differences were observed between groups for all variables in terms of WOMAC pain and stiffness scores (Table 5). However, being older and requiring increasing levels of walking aid postoperatively resulted in worse WOMAC total and physical function scores. There were no correlations found between WOMAC physical function scores and age, time to surgery, length of stay, duration of surgery and EBL.
Table 5.
Difference Between Groups and 1-Year Postoperative WOMAC Scores.
| WOMAC Score | P-value | |||
|---|---|---|---|---|
| Total | Pain | Stiffness | Physical Function | |
| Gendera | .53 | .25 | .99 | .51 |
| Age groupb | .02 | .69 | .07 | .02 |
| ASA statusb | .08 | .82 | .44 | .08 |
| Fracture presentationa | .69 | .70 | .19 | .83 |
| Surgical procedurea | .10 | .57 | .73 | .09 |
| Mode of anaesthesiaa | .68 | .77 | .32 | .75 |
| Non-hip complicationsb | .79 | .85 | .69 | .71 |
| Hip complicationsa | .71 | .76 | .57 | .65 |
| Preoperative ambulationb | .03 | .51 | .71 | .05 |
| Postoperative ambulationb | .00 | .02 | .95 | .00 |
WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index. ASA: American Society of Anesthesiologists.
aP-value determined by independent samples t-test.
bP-value determined by one-way ANOVA.
Subgroup analysis of surgical procedure showed that patients who underwent total hip arthroplasty were significantly younger, subject to general anesthesia, experienced longer time to surgery, longer duration of surgery and a higher EBL (Table 6). Although WOMAC total, pain, stiffness and physical function scores were lower in the total hip arthroplasty group, these differences were not statistically significant. There was also no difference for hip-related complications between those who had a total hip arthroplasty and those who had a hemiarthroplasty.
Table 6.
Subgroup Analysis of Surgical Procedure.
| THA | HA | P-value | Mean Difference (95% CI) | |
|---|---|---|---|---|
| Overall | 74 (44%) | 94 (56%) | ||
| Gender | P = .18a | |||
| Male | 26 (35.1%) | 24 (25.5%) | ||
| Female | 48 (64.9%) | 70 (74.5%) | ||
| Age | 72.0 (7.0) | 77.7 (8.6) | P = .00b | −5.76 (−8.18, −3.35) |
| Age group | P = .00a | |||
| 60-69 years | 27 (60.0%) | 18 (40.0%) | ||
| 70-79 years | 35 (53.8%) | 30 (46.2%) | ||
| 80-89 years | 12 (23.5%) | 39 (76.5%) | ||
| 90-99 years | 0 (.0%) | 7 (100.0%) | ||
| ASA status | P = .21a | |||
| 1 | 10 (58.8%) | 7 (41.2%) | ||
| 2 | 38 (38.4%) | 61 (61.6%) | ||
| 3 | 26 (50.0%) | 26 (50.0%) | ||
| Fracture presentation | P = .08a | |||
| Acute | 63 (85.1%) | 87 (92.6%) | ||
| Chronic | 11 (14.9%) | 7 (7.4%) | ||
| Mode of anaesthesia | P = .00a | |||
| General anaesthesia | 64 (86.5%) | 48 (51.1%) | ||
| Regional anaesthesia | 10 (13.5%) | 46 (48.9%) | ||
| Non-hip complications | P = .13c | |||
| None | 54 (73.0%) | 56 (59.6%) | ||
| 1 | 18 (24.3%) | 28 (29.8%) | ||
| 2 or more | 2 (2.7%) | 10 (10.6%) | ||
| Hip complications | P = 1.00a | |||
| None | 69 (93.2%) | 88 (93.6%) | ||
| 1 or more | 5 (6.8%) | 6 (6.4%) | ||
| Time to surgery (days) | 20.3 (1.4) | 19.5 (1.3) | P = .00b | .79 (.34, 1.24) |
| Length of stay (days) | 18.4 (9.4) | 15.8 (8.2) | P = .09b | 2.57 (−.14, 5.55) |
| Duration of surgery (mins) | 137.3 (20.9) | 99.3 (26.5) | P = .00b | 37.97 (29.78, 46.16) |
| EBL (ml) | 575.6 (229.9) | 451.1 (224.2) | P = .02b | 124.48 (14.93, 234.02) |
| WOMAC physical function | 9.1 (13.8) | 13.8 (12.9) | P = .09b | −4.66 (−10.08, .76) |
Values for age, time to surgery, length of stay, duration of surgery and EBL are presented as mean (SD). Chronic fractures are defined as those that presented after 3 weeks. ASA: American Society of Anesthesiologists. THA: total hip arthroplasty. HA: hemiarthroplasty. EBL: Estimated blood loss.
aP-value determined by Pearson’s chi-square test.
bP-value determined by independent samples t-test.
cP-value determined by Fisher’s exact test.
The 1-year mortality rate was 14.3% where the majority were from the 70 to 79 years old age group and ASA 3 category. Within the 1-year postoperative period, 1 patient from the total hip arthroplasty group underwent revision for recurrent dislocation and 1 patient from the hemiarthroplasty group underwent revision for stem fracture. There were no other secondary hip procedures within the study interval. Other hip related problems included foot drop (2), heterotrophic ossification (2), aseptic loosening of stem (1), wound complications (3) and prosthetic joint infection (1).
Discussion
Demography of the study population was predominantly female, at a 2.36:1 ratio and is reflective of local5,10 and regional11 trends. However, these patients are relatively younger than those reported in other regions.12 The authors’ institution provides orthopedic services to an area with a radius of approximately 200 km and is the only arthroplasty centre within the state. There are many remote communities within this area and there exists specific challenges with regards to healthcare access, due to distance and nature. Coupled with operating time constraints, these factors inadvertently result in a delay in presentation, longer time to surgery and length of stay.
The most important finding from this study was that a substantial proportion of patients did not regain pre-fracture ambulatory ability. All patients were able to ambulate independently, with or without aid, prior to fracture. Considering the mortality rate of 14.3%, at 1 year after surgery, only 32.1% managed to regain pre-fracture mobility status while 26.1% of patients became dependent. Prior to fracture, 79.2% of the patients were able to ambulate without a walking aid but only 28.6% retained this ability 1 year after surgery. Possible reasons include increasing frailty, or the lack of effective rehabilitative measures and monitoring of care delivery after discharge.5 In 2019, Khor et al,13 had conducted a study at a tertiary centre in the capital city and found that 41.6% of patients with hip fractures managed to regain pre-fracture mobility and that age, length of hospitalization and pre-fracture mobility status were predictors of mobility recovery. In this study, regression analysis showed that age, gender, surgical procedure, and time to surgery were predictors of mobility recovery.
The mortality rate in this review was lower than reported in past studies.14,15 This could be attributed to confounding factors such as a small sample size, or improved quality of care within our healthcare system. Involvement of geriatricians in the orthogeriatric care model has been shown to reduce complications, mortality rate, time to surgery and functional deterioration16,17 while early geriatric intervention benefits older patients with poor functional status prior to fracture.18 Although surgeons are mostly concerned with surgery and implant related outcomes, it is important to note that better functional recovery leads to a better quality of life and thus, better overall results. Therefore, measures such as setting up a fracture liaison service, admission to a comprehensive geriatric care ward,16,19 improving time to surgery,20 improving access to the healthcare facility and rehabilitation services, as well as continuity of care after discharge, could be implemented to improve patient outcomes in this locality.
There is strong consensus in the literature that arthroplasty is associated with a lower re-operation rate and better function than internal fixation for patients with displaced intracapsular hip fractures.21,22 However, there is still no agreement with regards to whether a total hip arthroplasty or hemiarthroplasty is superior.22 Although multiple studies have favored total hip arthroplasty due to a lower revision risk, better function, and better quality of life,21,23,24 a recent randomized controlled trial has refuted this.25
Results from this study showed that patients who had a total hip arthroplasty were more likely to remain independent 1 year after surgery, more likely to regain pre-fracture mobility and continue ambulating without a walking aid. Although regression analysis favored those who had a total hip arthroplasty, this advantage could be a result of selection bias as patients at the authors’ institution were planned for total hip arthroplasty if there was preexisting hip pain or if the Sernbo score was more than 16 i.e., younger, and healthier subset of older people who can ambulate independently. In addition, better WOMAC scores were observed in the total hip arthroplasty group at 1 year follow-up. Interestingly, this difference in patient-reported outcome measures was not significant and did not meet the threshold for minimal clinically important difference,26 despite the selection bias and retrospective nature of this study.
The most common complications that these patients developed during their hospital stay were pressure sores followed by urinary tract infection. Analysis showed that this was not related to preoperative ambulatory ability, ASA status and time to surgery, nor did it have any significant association with postoperative independent ambulation and WOMAC scores. However, patients who regained pre-fracture mobility were less likely to have experienced these adverse events. Although not predictors for both regression models, this variable was included as it was found to be a significant confounding factor. In contrast, Hansson et al.27 reported that the presence of general complications was a major risk factor affecting functional outcome and together with local complications, affecting pain and satisfaction. In this review, the total hip arthroplasty and hemiarthroplasty groups displayed no difference with regards to hip-related complications. The effect of all these variables on mortality rate was not analyzed.
The mean age of patients in this study was 75.2 years old. With an average life span of 75.6 years in this population,28 and no significant differences in patient-reported hip function or complications after surgery in the short-term, it may be reasonable to choose hemiarthroplasty in this age group even when patients meet the criteria for total hip arthroplasty, especially if cost is a factor. Other advantages include shorter duration of surgery and less blood loss. However, the difference in transfusion requirement and long-term problems associated with hemiarthroplasty such as acetabular erosion and revision to total hip arthroplasty were not explored in this study. To the best of the authors’ knowledge, this is the first study to date on short-term mobility and hip function after geriatric neck of femur fractures treated with arthroplasty in this population.
Limitations
The main limitation of this study is that it is a retrospective review with a relatively small sample size. Therefore, patient groups or treatment modalities could not be compared objectively as the study subjects were not matched nor randomized. Furthermore, there is a lack of information regarding the rehabilitation process, which ostensibly could affect both mobility and hip function postoperatively.
Conclusion
A significant proportion of patients did not regain their pre-fracture mobility after sustaining a neck of femur fracture, despite surgical treatment with arthroplasty. In this retrospective review, there was no significant difference in patient-reported hip function between those who had a total hip arthroplasty and those who had a hemiarthroplasty.
Acknowledgments
We would like to thank the Director General of Health Malaysia for his permission to publish this article.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Jade Pei Yuik Ho https://orcid.org/0000-0002-0188-9687
References
- 1.Dieleman JL, Squires E, Bui AL, et al. Factors associated with increases in US health care spending, 1996-2013. JAMA. 2017;318(17):1668-1678. doi: 10.1001/jama.2017.15927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gallagher JC, Melton LJ, Riggs BL, Bergstrath E. Epidemiology of fractures of the proximal femur in Rochester, Minnesota. Clin Orthop Relat Res. 1980;150:163-171. [PubMed] [Google Scholar]
- 3.Frenkel Rutenberg T, Assaly A, Vitenberg M, et al. Outcome of non-surgical treatment of proximal femur fractures in the fragile elderly population. Injury. 2019;50(7):1347-1352. doi: 10.1016/j.injury.2019.05.022. [DOI] [PubMed] [Google Scholar]
- 4.Moulton LS, Green NL, Sudahar T, Makwana NK, Whittaker JP. Outcome after conservatively managed intracapsular fractures of the femoral neck. Ann R Coll Surg Engl. 2015;97(4):279-282. doi: 10.1308/003588415x14181254788809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lim HT, Chong E, Yau WK, Abdul-Halim H. Outcomes and impact of fragility fracture among geriatrics patients who underwent hip surgery in hospital Kuala Lumpur. Malays Orthop J. 2022;16(1):84-90. doi: 10.5704/moj.2203.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Laflamme GY, Rouleau DM, Leduc S, Roy L, Beaumont E. The timed up and go test is an early predictor of functional outcome after hemiarthroplasty for femoral neck fracture. J Bone Joint Surg Am. 2012;94(13):1175-1179. doi: 10.2106/jbjs.J.01952 [DOI] [PubMed] [Google Scholar]
- 7.Flikweert ER, Izaks GJ, Reininga IHF, Wendt KW, Stevens M. Evaluation of the effect of a comprehensive multidisciplinary care pathway for hip fractures: Design of a controlled study. BMC Musculoskelet Disord. 2013;14(1):291. doi: 10.1186/1471-2474-14-291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ramkumar PN, Navarro SM, Haeberle HS, Ng M, Piuzzi NS, Spindler KP. No difference in outcomes 12 and 24 months after lower extremity total joint arthroplasty: A systematic review and meta-analysis. J Arthroplasty. 2018;33(7):2322-2329. doi: 10.1016/j.arth.2018.02.056 [DOI] [PubMed] [Google Scholar]
- 9.Seetharam A, Deckard ER, Ziemba-Davis M, Meneghini RM. The AAHKS clinical research award: Are minimum two-year patient-reported outcome measures necessary for accurate assessment of patient outcomes after primary total knee arthroplasty? J Arthroplasty. 2022;37(8):S716-S720. doi: 10.1016/j.arth.2022.02.016 [DOI] [PubMed] [Google Scholar]
- 10.Ong T, Khor HM, Kumar CS, et al. The current and future challenges of hip fracture management in Malaysia. Malays Orthop J. 2020;14(3):16-21. doi: 10.5704/moj.2011.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tan WLB, Low SL, Shen L, Das De S. Osteoporotic hip fractures: 10-year review in a Singaporean hospital. J Orthop Surg. 2015;23(2):150-154. doi: 10.1177/230949901502300206. [DOI] [PubMed] [Google Scholar]
- 12.Vergara I, Vrotsou K, Orive M, Gonzalez N, Garcia S, Quintana JM. Factors related to functional prognosis in elderly patients after accidental hip fractures: A prospective cohort study. BMC Geriatr. 2014;14:124. doi: 10.1186/1471-2318-14-124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khor HM, Teh HX, Tan FC, et al. 66 short term outcomes following fragility HIP fracture in Malaysia. Age Ageing. 2019;48(4):iv13-iv17. doi: 10.1093/ageing/afz164.66 [DOI] [Google Scholar]
- 14.Penafort R, Hussein A, Sengupta S, Poi P. One year outcome of hip fractures in the elderly. Med J Malaysia. 2002;57:39-47. [Google Scholar]
- 15.Nanchappan NS, Chopra S, Samuel A, Therumurtei L, Ganapathy SS. Mortality rate and ten years survival of elderly patients treated with total hip arthroplasty for femoral neck fractures. Malays Orthop J. 2021;15(2):136-142. doi: 10.5704/moj.2107.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prestmo A, Hagen G, Sletvold O, et al. Comprehensive geriatric care for patients with hip fractures: A prospective, randomised, controlled trial. Lancet. 2015;385(9978):1623-1633. doi: 10.1016/s0140-6736(14)62409-0 [DOI] [PubMed] [Google Scholar]
- 17.Grigoryan KV, Javedan H, Rudolph JL. Orthogeriatric care models and outcomes in hip fracture patients: A systematic review and meta-analysis. J Orthop Trauma. 2014;28(3):e49-e55. doi: 10.1097/BOT.0b013e3182a5a045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Crego-Vita D, Sanchez-Perez C, Gomez-Rico JAO, De Arriba CC. Intracapsular hip fractures in the elderly. Do we know what is important? Injury. 2017;48(3):695-700. doi: 10.1016/j.injury.2017.01.022 [DOI] [PubMed] [Google Scholar]
- 19.Taraldsen K, Thingstad P, Sletvold O, et al. The long-term effect of being treated in a geriatric ward compared to an orthopaedic ward on six measures of free-living physical behavior 4 and 12 months after a hip fracture - a randomised controlled trial. BMC Geriatr. 2015;15:160. doi: 10.1186/s12877-015-0153-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sheehan KJ, Williamson L, Alexander J, et al. Prognostic factors of functional outcome after hip fracture surgery: A systematic review. Age Ageing. 2018;47(5):661-670. doi: 10.1093/ageing/afy057 [DOI] [PubMed] [Google Scholar]
- 21.Hopley C, Stengel D, Ekkernkamp A, Wich M. Primary total hip arthroplasty versus hemiarthroplasty for displaced intracapsular hip fractures in older patients: Systematic review. BMJ. 2010;340:c2332. doi: 10.1136/bmj.c2332 [DOI] [PubMed] [Google Scholar]
- 22.Tornetta P, Bhandari M, Devereaux PJ, et al. Operative management of displaced femoral neck fractures in elderly patients: An international survey. J Bone Joint Surg Am. 2005;87(9):2122-2130. [DOI] [PubMed] [Google Scholar]
- 23.Blomfeldt R, Törnkvist H, Eriksson K, et al. A randomised controlled trial comparing bipolar hemiarthroplasty with total hip replacement for displaced intracapsular fractures of the femoral neck in elderly patients. J Bone Joint Surg Br. 2007;89(2):160-165. doi: 10.1302/0301-620x.89b2.18576 [DOI] [PubMed] [Google Scholar]
- 24.Lewis DP, Wæver D, Thorninger R, Donnelly WJ. Hemiarthroplasty vs total hip arthroplasty for the management of displaced neck of femur fractures: A systematic review and meta-analysis. J Arthroplasty. 2019;34(8):1837-1843. doi: 10.1016/j.arth.2019.03.070 [DOI] [PubMed] [Google Scholar]
- 25.Bhandari M, Einhorn TA, Guyatt G, et al. Total hip arthroplasty or hemiarthroplasty for hip fracture. N Engl J Med. 2019;381(23):2199-2208. doi: 10.1056/NEJMoa1906190 [DOI] [PubMed] [Google Scholar]
- 26.MacKay C, Clements N, Wong R, Davis AM. A systematic review of estimates of the minimal clinically important difference and patient acceptable symptom state of the Western Ontario and McMaster Universities Osteoarthritis Index in patients who underwent total hip and total knee replacement. Osteoarthritis Cartilage. 2019;27(10):1408-1419. doi: 10.1016/j.joca.2019.05.002 [DOI] [PubMed] [Google Scholar]
- 27.Hansson S, Rolfson O, Åkesson K, Nemes S, Leonardsson O, Rogmark C. Complications and patient-reported outcome after hip fracture. A consecutive annual cohort study of 664 patients. Injury. 2015;46(11):2206-2211. doi: 10.1016/j.injury.2015.07.024 [DOI] [PubMed] [Google Scholar]
- 28.Mahidin MU. Launching of Report on the Key Findings Population and Housing Census of Malaysia; 2020. [Google Scholar]