Abstract
Background:
Despite growing evidence of the impact that clinical academic (CA) staff have on patient care and clinical practice, there are disproportionately low numbers of nurses, allied health professionals (AHPs) and other healthcare professionals in CA joint roles, compared to their medical colleagues.
Aim:
To describe the initial development of a CA career pathway for nurses, AHPs and other healthcare professionals in a Community and Mental Health NHS Trust.
Methods:
Kotter’s 8-Step Change Model was used to expand opportunities and research culture across an NHS Trust.
Results:
A variety of capacity and capability initiatives at different academic levels were created to support CA development and to complement those available externally. These opportunities were underpinned by a research and development strategy, senior leadership buy-in, manager and clinical staff support, and targeted organisation-wide communication.
Conclusion:
The ongoing development of innovative CA opportunities in the Trust, alongside greater support for staff interested in pursuing CA careers, has resulted in a growing number of individuals successful in developing as CAs. This has led to a growth in research culture in the organisation and a greater understanding of what CA staff can bring to patient care, the clinical service and the wider organisation.
Keywords: allied health professionals, career pathway, clinical academic, NHS, nursing
Introduction
The development of clinical academic (CA) roles and career opportunities for professions outside of medicine and dentistry in England, Scotland and Wales has gained traction over the last decade. However, despite these developments, the proportion of nurses, midwives and allied health professions (AHPs) in CA roles remains disproportionately low at 0.1% of the workforce, compared to 4.6% of the medical workforce in the United Kingdom (UK) (Council of Deans of Health, 2018; Medical Research Council (MRC), 2017). To bridge this gap and to achieve the Association of UK University Hospitals (AUKUH) ambition of 1% of nurses, midwives and AHPs in CA roles by 2030, further development opportunities and initiatives are required to improve capability and capacity in these professional groups (AUKUH Clinical Academic Roles Development Group, 2016).
Background
A CA is described as a ‘clinically active health researcher’ who combines their clinical role with research activity that is grounded in clinical practice, allowing them to address the issues that are relevant to both patients and their organisation (Department of Health, 2012; National Institute of Health Research (NIHR), 2016). The role of the CA, their research engagement and activity are essential to provide transformative and sustainable health and social care services that meet the needs of an aging population with increasing complex needs (NHS England, 2014). An increasing body of evidence demonstrates that research-active organisations are associated with improved quality of care, enhanced patient experience and improved patient outcomes (Boaz et al., 2015; Hanney et al., 2013). CAs also impact on staff recruitment and retention, knowledge exchange and raising the profile of their organisations through presentations, publications and awards (Newington et al., 2021).
Notwithstanding the contribution of doctoral qualified nurses, AHPs and other clinically qualified professions to improving clinical practice standards (Andreassen et al., 2018), there remains a lack of appreciation of the value that they bring (Trusson et al., 2019; Van Oostveen et al., 2017). This is often associated with senior clinicians’ and managers’ lack of knowledge and understanding of what the role entails, rather than pure unwillingness to offer such a role (Van Oostveen et al., 2017). This can also be exacerbated by a lack of leadership, mentorship, guidance and limited organisational support (Trusson et al., 2019).
Regardless of the progress in the development of CA roles over the last decade, funding and CA pathways are still insufficient to enable adequate capacity and capability (Carrick-Sen et al., 2019). The Health Education England (HEE)-National Institute for Health and Care Research (NIHR) Integrated Clinical and Practitioner Academic (ICA) Programme was established to address this shortfall; however, these schemes are highly competitive and frontline clinicians are further challenged by limited opportunities to experience the demands of combining clinical and academic components of a CA role outside of these schemes (Bramley et al., 2018).
A key approach to increase the percentage of nurses and AHPs in CA roles, and to overcome the barriers to successful and sustainable CA careers, is the development of local and regional initiatives enhancing the development and growth of communities of CAs (Bramley et al., 2018; Roddam et al., 2019). Essential to these initiatives is the development of strong collaboration and sustainable partnership between higher education institutions (HEIs) and NHS organisations (Westwood et al., 2018).
The aim of this paper is to describe the development of a CA pathway, and local research capacity and capability initiatives, in a Community and Mental Health NHS Trust through collaboration and partnership with an HEI.
Local context
Leicestershire Partnership NHS Trust (LPT) is a Community and Mental Health NHS Trust with over 5500 substantive employees comprising 3.7% medical staff, 48.4% nursing, AHP or other qualified clinical staff and 24.1% non-registered clinical staff. Formal CA positions or opportunities are not proportionally reflected across these groups, with a far lower proportion of CA positions for clinical professions outside of medicine, compared to those held by medical staff.
To increase research capacity, improve patient care and outcomes, and to aid staff recruitment and retention, LPT aimed to develop a sustainable career pathway for nurses, AHPs, pharmacists and psychologists. The development of new CA roles in LPT was initiated by the Head of Research and Development (R&D), an occupational therapist by clinical background. Development of these innovative roles required close collaboration with local HEIs such as the University of Leicester and De Montfort University (DMU). Although LPT and the University of Leicester already had established several joint CA posts for medical staff, the development of new collaborative relationships with academics at DMU was instrumental in establishing several new initiatives aimed at other registered healthcare professionals in the Trust. These partnerships offered not only academic opportunities for clinical staff, but also an opportunity for academic staff at DMU to build links with clinical services and create opportunities for collaboration.
The Head of R&D and the Executive Director of Community Health Services in LPT, in conjunction with the Dean of Health and Life Sciences and a Professor of Nursing in DMU, were the driving force behind this strong collaborative relationship and innovative CA initiatives. Since 2020, the ongoing development of CA initiatives and the implementation of the recently launched Chief Nursing Officer of England’s Strategic Plan for Nursing Research and the Allied Health Professions’ Research and Innovation Strategy for England are driven by the Executive Director of Nursing (DoN), AHPs and quality in LPT.
Underpinning cultural change – Kotter’s 8-Step Change Model
Kotter’s (1996) 8-Step Change Model was used to inform and facilitate the desired transformational change. With growing evidence of improved healthcare performance and patient outcomes in research-engaged organisations (Boaz et al., 2015), it was imperative to bring change to an organisation with minimal research activity. Existing research was primarily led by medical staff, and the tradition of research being core business within healthcare was not yet established as the norm for nurses, AHPs, pharmacists and clinical psychologists. Multiple barriers, including the pressures within services, limited access to training and lack of confidence, were likely contributing factors (Harris et al., 2020).
The eight steps of Kotter’s (1996) Change Model, the organisational starting point in 2013 and some of the steps taken are outlined in Table 1. Although the model suggests a linear process, Rose (2019) emphasised the importance of ‘short-term wins’ which not only help progress as stepping-stones, but also underpin the longer-term vision and help sustain the effort needed to embed the change.
Table 1.
Kotter’s 8-Step Change Model and its application within LPT.
| Kotter’s 8 steps | LPT starting position | Actions taken |
|---|---|---|
| 1. Create a sense of urgency (2013–2014) | • Limited research culture • Limited understanding of benefits of research to the organisation, staff and patients • Lack of awareness of and applications for national and local CA opportunities |
• Discussed with Trust Board the benefits of research, deficit of staff with CA skills and opportunities available to develop CA careers • Sought and learnt from examples of success regionally and nationally |
| 2. Build a guiding coalition (2014–2017) | • Lack of internal and external research supporters, champions and enablers | • Identified research allies (including academic partners) and established strategic and operational leadership groups • Ensured influencers and academic partners were contributors to the development of new CA opportunities |
| 3. Form a strategic vision and initiatives (2014–2018) | • Absence of a current R&D strategy | • Developed a 5-year R&D strategy which included a specific aim to develop CA careers for all professions • Aims of the new strategy were shared with the Trust Board and Clinical Effectiveness Committee |
| 4. Communicate the vision (2018) | • Very limited visibility of research within the organisation | • Raised the profile of research in the Trust through social media platforms and newsletters • Developed a programme of research forums |
| 5. Enable action by removing barriers (2016) | • Lack of managerial understanding of the benefits of research and of supporting staff to pursue CA careers • Managers were challenged with covering clinical service needs when releasing staff to undertake CA training |
• Engaged with senior managers to support with, for example, staff release from clinical practice • Developed a buddy system and a peer support network • Offered mentoring and coaching to aspiring CAs |
| 6. Generate short-term wins (2016) | • Limited number of staff expressing interest in seeking CA opportunities • Lack of managerial insight and support |
• CA opportunities were more widely publicised within the organisation • Specific support was offered to staff to strengthen applications submitted for CA opportunities • Provided support to line managers of staff applying for CA opportunities • Built collaborative relationships with DMU • Secured charitable funds to support PhDs and Masters in Research (2016) • Developed a programme of research skills workshops |
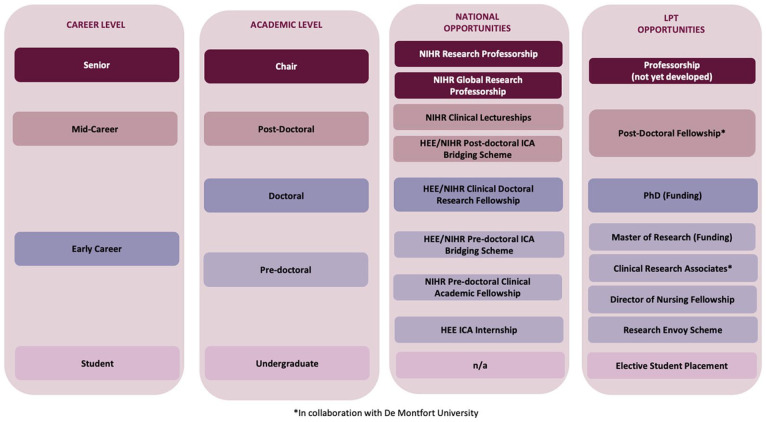
| 7. Revise, refine, scale and build on the change (2017 to date) | • An identified need to build greater research capacity and capability throughout the organisation | • Developed internal opportunities for CA progression (see Figure 1). • Developed the Research Envoy scheme (2017) to raise the profile of research and establish research champions in clinical services. • Introduced early career nursing staff to research and CA careers through the Director of Nursing Fellowship scheme (2021), and introduction of elective student nursing research placements (2022) |
| 8. Anchor the changes (2019 to date) | • Need for research to become accepted as part of day-to-day business in the organisation for all clinical staff • Mechanisms required to support staff to be research active, engaged and to develop future research leaders |
• Established a ‘Research Award’ within the annual organisational award ceremony • Ongoing support of CA opportunities in the Trust • Expansion of initial internal pilot CA opportunities to all areas of the Trust • Building on increased awareness and evidence of a research culture within the Trust |
CA: clinical academic; DMU: De Montfort University; LPT: Leicestershire Partnership NHS Trust; R&D: Research and Development.
Prior to developing LPT-specific CA programmes, opportunities such as the HEE-NIHR Internship and Predoctoral Bridging awards were highlighted to staff. To enable successful applications of these opportunities, the Head of R&D supported staff to develop their research ideas and facilitated conversations about research and CA development between prospective applicants and their line managers.
It was clear early in the organisation’s journey that there was a need to develop an innovative and collaborative approach with an academic partner. Through in-depth discussions with senior academic staff at DMU, a shared vision emerged. A pivotal event that changed views and gained commitment was a joint visit to a large acute teaching Trust by the Head of R&D, a Trust Executive Director and the Dean of the Faculty of Health and Life Sciences at DMU. This offered the opportunity to hear, see, meet, question and understand what difference and impact research-engaged and research-active nurses, midwives and AHPs had on patient care, the research culture of the organisation, career development opportunities and staff retention. The shared understanding gained that day, for both LPT and DMU, cemented commitment, allowed LPT’s vision to grow and enabled the Executive Director, a nurse by clinical background, to champion the vision, secure reinforcement within the organisation and assist with navigating barriers. This proved critical to building a successful foundation to grow from.
Following this visit, an organisational R&D strategy was developed for 2014–2018 which included the goal of ‘Building research capacity’ within the workforce, and the subsequent 5-year strategy, built on this work with the goal to ‘attract, develop and retain research leadership and skills’.
Since then, a variety of CA opportunities, complementary to the Hee-NIHR ICA programme pathway, have been developed at different academic levels for all clinical professions outside of medicine and are outlined in Figure 1. The intention was, and remains, to provide a clear progression through internal and external schemes to enable staff to develop as CAs and independent researchers.
Figure 1.
National and LPT CA development opportunities.
CA: clinical academic; HEE: Health Education England; ICA: integrated clinical academic; LPT: Leicestershire partnership NHS trust; n/a: not applicable; NIHR: National Institute for Health Research.
Local CA initiatives
Master’s and PhD funding and supervision
Securing funds from the Trust’s charity ‘Raising Health’ in 2016 to support PhD study was a key strategy to support the growth of research capacity in the Trust. Three staff were offered funding to support mainly PhD fees and/or back-fill. It was up to the member of staff if they preferred to undertake part-time or full-time PhD study. Of the three members of staff, two selected part-time and one full-time study. Because the funding was partial, most individuals sought additional funding elsewhere (e.g. through an additional PhD studentship). A further member of staff was also supported to secure partial PhD funding in 2021 from the local NIHR Collaboration for Leadership in Applied Health Research and Care (now known as Applied Research Collaboration), in addition to that provided from the charitable funds. PhD funding support from charitable funds was offered as a once-off and ongoing support sought through other local, regional and national PhD studentships and relevant funding streams.
It was evident that growing the future cohort of staff undertaking PhDs needed investment at Master’s degree level. Several staff were supported in applications to the NIHR-funded Master’s in Applied Research, but when this scheme changed to the NIHR Pre-Doctoral Clinical Academic Fellowship, the application process became extremely competitive and challenging for staff to succeed. Therefore, additional funding was secured from the Raising Health charity in 2014, to cover the fees for Master’s in Research Methods. It was up to the individual member of staff if they preferred to undertake part-time or full-time study. The funding was for fees only. Backfill or study leave was not funded. Charitable funds were also secured to support conference attendance and presentation and other research-related activities, such as printing posters.
Academic supervision for staff undertaking Master’s or PhD has been provided by partner HEIs as appropriate. The close collaborative relationship with DMU has been further extended not only though academic supervision, but also via provision of fee waivers for PhD students in some cases. These relationships have since built further opportunities for collaboration in research with several of these academic partners.
The Research Envoy scheme
The Research Envoy scheme originated in 2017 following a joint venture between the local Clinical Research Network (CRN), the University Hospitals of Leicester NHS Trust, and LPT (Melvin et al., 2018). The scheme aimed to give patient-facing staff, from all professions and levels, a basic understanding of the role of research in the NHS and equip them with skills and knowledge to champion and facilitate research in their clinical service, both with service users and colleagues. Initially, it involved 20 protected days over 6 months and included taught elements (some delivered by the local CRN), shadowing researchers, and a project to raise the profile of research in their clinical area. The first iteration of the Envoy scheme, funded by the CRN East Midlands, was offered as a once-off opportunity in 2017. Following its success, it was decided to offer a similar training programme within LPT with some adaptations such as fewer training days (12 days over 6 months) based on feedback that this would make it more accessible to staff who would need to be released from their clinical role to undertake the training. The programme continues to be offered annually.
Clinical Research Associate secondments
The Clinical Research Associate (CRA) secondments originated through collaboration between R&D, Community Health Services in LPT and the Faculty of Health and Life Sciences at DMU. These secondments are joint funded by the two organisations. Two members of non-medical staff are awarded a 2-year 0.5 WTE secondment to undertake a research project relevant to their clinical area. The CRAs receive academic supervision from senior academics at DMU and access to university facilities and resources. Further support is provided by LPT R&D and a clinical mentor. The initiative started in 2017 and thus far is open to all nurses and AHPs who work in a patient-facing role in the Community Health Services directorate. Applicants can be of any level of research experience and the training and support they receive are tailored to their level of research and academic experience and their academic aspirations. This opportunity has been available for two successive 2-year periods and has led to patient-focussed research which has been disseminated at national conferences, raised the profile of research in the CRA’s service and increased links and collaboration between the Trust and DMU. Funding and support for Cohort 3 of the CRA secondment opportunity have been agreed and this CA development opportunity expanded to all three clinical directorates in LPT.
The Director of Nursing (DoN) Fellowship programme
The DoN Fellowship programme offers a bespoke development opportunity for Band 5 nurses in clinical practice. Based on the Chief Nurse Fellow Model (Bramley et al., 2018), the fellowship aims to empower frontline nurses to make a difference to patient care through a quality improvement project whilst developing leadership and academic skills.
The first cohort of the DoN fellowship programme launched in September 2021 and consists of a taught element, insight opportunities and a quality improvement project relevant to their clinical areas. The taught elements of the programme were developed and delivered by the LPT Organisational Development Team (leadership), Quality Improvement Core Team (quality improvement) and R&D Team (research and academic skills). Invited guests from other services, such as local universities, library services and the Care Quality Commission, also contributed. There was no specific funding allocated for the development and delivery of the DoN fellowship programme. Existing organisational resources (training and project support) were utilised for the delivery of the programme and clinical services agreed to release their fellow for 1 day a week for the duration of the 1-year fellowship, without any backfill funding.
The programme offers one day a week out of clinical practice for a period of 1 year to undertake learning activities and their quality improvement projects whilst supported by a clinical and an academic mentor and engaging in six weekly action learning sets. Clinical mentoring and facilitation of the action learning sets are supported by the relevant Deputy Heads of Nursing in the fellow’s clinical area. Academic mentoring is supported by multi-professional members of staff who are currently undertaking or have completed PhD/Doctoral study. Furthermore, fellows have a quarterly coaching session with the DoN. It is anticipated that the programme will be offered on an annual basis with the intention to expand this opportunity to AHPs in future cohorts.
Postdoctoral fellowship
A university-funded 12-month secondment opportunity was developed in a collaboration with DMU for a postdoctoral nurse or AHP researcher. The fellowship, due to start 2022/2023, aims to bridge the doctoral–postdoctoral gap by providing the fellow bespoke support to develop as an independent CA researcher and work towards being a Chief Investigator/Principal Investigator on collaborative research grant applications, and/or to develop early papers and research grant applications relevant to practice in LPT. The postdoctoral fellowship is a new CA opportunity that will be evaluated at the end of the secondment with the view to offer it on an annual basis.
Peer support network
To support and empower staff undertaking or aspiring to undertake a PhD, a CA peer support network was created. Quarterly meetings were hosted by the Head of R&D and included invitations to members of the Executive board. Their attendance enabled them to understand and see the ongoing growth of these staff and help build a vision for how they could be retained, and their advanced skills utilised within the Trust once their studies were complete.
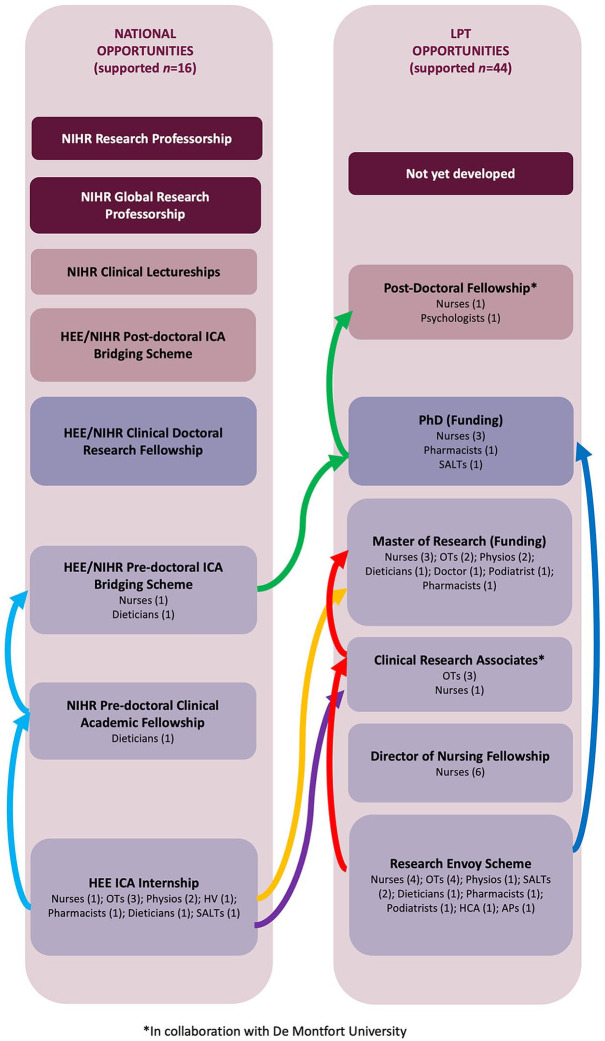
Success of internal opportunities
Since 2014, the new LPT-specific CA initiatives have been successful in supporting numerous staff to build on their research interests, to develop their knowledge and skills, and progress as CA researchers. These opportunities have engaged staff from a range of professions (nurses, dieticians, occupational therapists, psychologists, physiotherapists, speech and language therapists, pharmacists, podiatrists, assistant practitioners, healthcare assistants) and across varying levels of seniority in the organisation. It has become evident that staff are able to progress through the internal and external CA opportunities available to advance as researchers and develop their CA career. Figure 2 illustrates a range of professionals successful at each of the opportunities as well as examples of the progress of several individual staff (indicated by different coloured arrows). This demonstrates that staff can join the pathway at the right point for them and can progress to the next appropriate internal or external CA opportunity.
Figure 2.
Examples of CA support and progression in LPT.
APs: assistant practitioner; ARC: Applied Research Collaboration; CA: clinical academic; HEE: Health Education England; HCA: healthcare assistant; HV: health visitor; ICA: integrated clinical academic; LPT: Leicestershire partnership NHS trust; n/a: not applicable; NIHR: National Institute of Health Research; OTs: occupational therapists; Physios: physiotherapists; SALTs: speech and language therapists.
Discussion
This paper has described the development of a CA pathway, and local research capacity and capability initiatives, in a Community and Mental Health NHS Trust through collaboration and partnership with an HEI and the local CRN.
Successes
Kotter’s (1996) model for change provided a helpful framework for the desired transformational change. It was used in cycles with regular new activities being embedded as standard practice.
Over time, there were staff in the Trust who had been successful in pursuing CA opportunities who were willing to support others by sharing their applications as examples and advising prospective applicants. Marie Wilson (2011) is quoted as saying ‘you can’t be what you can’t see’ and it was recognised that a benefit to this work would be to create role models for staff to aspire to. Likewise for managers, who could then see how other managers were supporting their staff to become research active and for clinical staff who could see their peers succeeding in internship schemes or undertaking higher degrees.
To raise visibility of research-engaged and research-active staff and to showcase and role model that ‘this is what you can be’ within LPT, several strategies have been adopted which included celebration of staff achievements through the Trust weekly newsletter and social media, introducing a research award at the Trust’s annual celebration awards, and inviting Executive Board members to key events celebrating the internal CA opportunities.
Other strategies include offering a buddy system, providing coaching to emerging research leaders and hosting workshops for applicants and their managers. Early engagement between R&D and line managers helped them to fully understand the support their staff required. It also allowed managers to be linked, enabling them to learn from others and understand the wide range of benefits of having research-active and research-engaged staff within their teams.
Securing income to support CA development has been crucial to enabling managers to release staff from clinical practice to undertake research activities. Funding of opportunities (from NIHR and HEE initiatives, the Trust’s charitable funds, and match funding from local HEI and LPT) has equalled over £840k since 2014.
Continuing benefits of having CA staff in a clinical service have been the growth of research culture in the team and increased opportunities for staff and service users as participants in research. Additionally, CA staff have generated publications and conference presentations that have raised the profile of the Trust and clinician-led research.
Challenges
This work has not been without significant challenges, some of which remain. LPT is a large Community and Mental Health NHS Trust, and staff are located across more than 120 bases. Prior to the COVID-19 pandemic, the geographical dispersal of staff posed significant challenges in terms of communication and bringing individuals together; however, the increased use of online platforms for meetings and training events has bridged this gap, and attendance at research events has greatly increased.
LPT services are configured into three clinical directorates with varying levels of research commitment, engagement and opportunities. At times, this has led to disparate uptake of CA opportunities and therefore required bespoke approaches for each Directorate. The Trust includes a large range of different services with pockets of research excellence and role models; however, embedding a consistent approach across directorates has been difficult.
At times, the experience of staff undertaking CA or research activity was that they were not valued and supported at a local team level. In some cases, managers or service leads lacked understanding of the research process and general appreciation of the relevance of research to evidence-based care. Challenges of service delivery, especially during the COVID pandemic, have required flexibility and good communication between the CA and their clinical team. If this is done well, it can result in increased understanding of research and what it brings to clinical care.
Next steps
A key step to further development and consolidation of the CA career pathway has been the recent appointment of a full-time Clinical Academic Careers Pathway Lead. This has already been instrumental in progressing the development of the DoN Fellowship programme and facilitating plans for a new student placement with the research team.
It is intended that the CRA secondment and DoN fellowship opportunities will be available more widely across all clinical directorates and to all nursing and AHP staff groups. The aspiration is to develop further CA opportunities whilst recognising that innovative approaches will be required to overcome resource limitations and to match the requirements to the capacity of our partner HEIs to support them. Discussions to develop a collaborative relationship and similar CA opportunities with the University of Leicester are positive and ongoing.
It is recognised that there are disparities in the uptake of CA opportunities across the clinical directorates, across professional groups and personal characteristics of staff which will be explored and addressed as a priority.
The Chief Nursing Officer for England’s Strategic Plan for Nursing Research and the Allied Health Professions’ Research and Innovation Strategy for England set out policy frameworks for the development and investment in Nursing and AHP research. Implications for effective implementation of these national strategies are being explored.
Conclusion
The transformational changes described in this paper represent the initial steps in the development of a structured local CA career pathway that is aimed to complement regional and national schemes. It is anticipated that by building on this the Trust will, in time, achieve the target of 1% of non-medical staff in CA roles. Building a critical mass of CAs in a Community and Mental Health NHS Trust has considerable challenges but is required to gain the benefits of improved patient care and outcomes.
Key points for policy, practice and/or research.
Innovative CA opportunities, outside of regional and national schemes, are essential to build local research and academic capacity and capability.
Strong partnership with Higher Education Institutions is essential to the development of a local CA pathway.
The support of line managers is essential to enable staff to pursue CA development opportunities and careers.
It is important to develop opportunities to support staff at different stages of their CA career.
Biography
Lizelle Bernhardt is the Clinical Academic Careers Pathway Lead in Leicestershire Partnership NHS Trust. Her role is to develop research capacity and capability for nurses, allied health professionals and other qualified staff and to develop and embed clinical academic roles within the organisation.
Sarah Baillon is a Senior Research Associate at Leicestershire Partnership NHS Trust. Part of her role is to support clinical staff to engage in research including pursuing clinical academic careers.
Susan M Corr is an independent coach/consultant specialising in clinical academic careers. Former roles include Head of Research and Development at Leicestershire Partnership NHS Trust and Professor of Occupational Therapy at the University of Northampton.
Kay de Vries is a Professor of Older Peoples Health at De Montfort University Faculty of Health & Life Sciences. She is an experienced nurse researcher and a PhD supervisor, primarily in the field of old age, dementia and end-of-life care.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Not applicable.
ORCID iD: Lizelle Bernhardt  https://orcid.org/0000-0002-6010-3955
https://orcid.org/0000-0002-6010-3955
Contributor Information
Lizelle Bernhardt, Clinical Academic Careers Pathway Lead, Leicestershire Partnership NHS Trust, Leicester, UK; Department of Cardiovascular Sciences, University of Leicester, Leicester, UK.
Sarah Baillon, Senior Research Associate, Leicestershire Partnership NHS Trust, Leicester, UK; Department of Health Sciences, University of Leicester, Leicester, UK.
Susan M Corr, Independent Coach/Consultant specialising in Clinical Academic Careers; Former Head of Research and Development, Leicestershire Partnership NHS Trust (formerly), Leicester, UK.
Kay de Vries, Professor of Older Peoples Health, De Montfort University, Leicester, UK.
References
- Andreassen P, Christensen MK. (2018) “We’re at a watershed”: The positioning of PhD nurses in clinical practice. Journal of Advance Nursing 74: 1908–1918. [DOI] [PubMed] [Google Scholar]
- AUKUH Clinical Academic Roles Development Group (2016) Transforming Healthcare Through Clinical Academic Roles in Nursing, Midwifery and Allied Health Professions. A Practical Resource for Healthcare Provider Organisations. AUKUH Clinical Academic Roles Development Group. Available at: http://www.medschools.ac.uk/SiteCollectionDocuments/Transforming-Healthcare.pdf [Google Scholar]
- Boaz A, Hanney S, Jones T, et al. (2015) Does the engagement of clinicians and organisations in research improve healthcare performance: A three-stage review. BMJ Open 5: 3009415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bramley L, Manning JC, Cooper J. (2018) Engaging and developing front-line clinical nurses to drive care excellence: Evaluating the Chief Nurse Excellence in Care Junior Fellowship initiative. Journal of Research in Nursing 23: 678–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrick-Sen DM, Moore A. (2019) Improving care and outcome through NMAHP research-focused clinical academic roles – an international perspective. International Journal of Practice-Based Learning in Health and Social Care 7: ii–vi. [Google Scholar]
- Council of Deans of Health (2018) Nursing, Midwifery and Allied Health Clinical Academic Research Careers in the UK. Council of Deans of Health. Available at: https://councilofdeans.org.uk/wp-content/uploads/2018/08/Nursing-midwifery-and-allied-health-clinical-academic-research-careers-in-the-UK.pdf [Google Scholar]
- Department of Health (2012) Developing the Role of the Clinical Academic Researcher in the Nursing, Midwifery and Allied Health Professions. Department of Health. Available at: https://www.gov.uk/government/publications/developing-the-role-of-the-clinical-academic-researcher-in-the-nursing-midwifery-and-allied-health-professions [Google Scholar]
- Hanney S, Boaz A, Jones T, et al. (2013) Engagement in Research: An Innovative Three-Stage Review of the Benefits for Health-Care Performance. Southampton (UK): NIHR Journals Library. [PubMed] [Google Scholar]
- Harris J, Grafton K, Cooke J. (2020) Developing a consolidated research framework for clinical allied health professionals practising in the UK. BMC Health Services Research 20: 852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotter JP. (1996) Leading Change. Boston, MA: Harvard Business School Press. [Google Scholar]
- Medical Research Council (2017) 2017 UK-Wide survey of clinical and health research fellowships. Available at: https://mrc.ukri.org/publications/browse/clinical-and-health-research-fellowships-survey-2017/.
- Melvin G, Patel R. (2018) Evaluation of a Pilot Internship Programme to Create Research Envoys; NHS Clinical Staff Who Can Spread the Research Message. Clinical Research Network East Midlands. Available at: https://www.nihr.ac.uk/documents/pilot-internship-programme-to-create-research-envoys/21947 [Google Scholar]
- National Institute of Health Research (NIHR) (2016) Building a Research Career Handbook. Available at: http://www.nihr.ac.uk/documents/faculty/Building-a-research-careerhandbook.pdf (accessed January 2022).
- Newington L, Wells M, Adonis A, et al. (2021) A qualitative systematic review and thematic synthesis exploring the impacts of clinical academic activity by healthcare professionals outside medicine. BMC Health Services Research 21: 400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHS England (2014) Five year forward view. Available at: https://www.england.nhs.uk/ourwork/futurenhs/ (accessed January 2022).
- Roddam H, Cross L, Georgiou R, et al. (2019) Developing clinical academic researchers: Insights from practitioners and managers in nursing, midwifery, and allied health. British Journal of Healthcare Management 25: 282–292. [Google Scholar]
- Rose KH. (2019) Leading change: A model by John Kotter. http://www.siriusmeetings.com/articles/article-leading-change.
- Trusson D, Rowley E, Barratt J. (2021) Multi-methods study comparing the experiences of medical clinical academics with nurses, midwives and allied health professionals pursuing a clinical academic career. BMJ Open 11: e043270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trusson D, Rowley E, Bramley L. (2019) A mixed-methods study of challenges and benefits of clinical academic careers for nurses, midwives, and allied health professionals. BMJ Open 9: e030595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Oostveen C, Goedhart NS, Francke AL, et al. (2017) Combining clinical practice and academic work in nursing: A qualitative study about perceived importance, facilitators, and barriers regarding clinical academic careers for nurses in university hospitals. Journal of Clinical Nursing 26: 23–24. [DOI] [PubMed] [Google Scholar]
- Westwood G, Richardson A, Latter S, et al. (2018) Building clinical academic leadership capacity: Sustainability through partnership. Journal of Research in Nursing 23: 346–357. [DOI] [PMC free article] [PubMed] [Google Scholar]