Abstract
Objective:
To measure changes in micronutrient adequacy and diet quality in healthcare and university employees who underwent a 10-week teaching kitchen program.
Methods:
Thirty-eight healthcare and university employees participated in a 10-week teaching kitchen program. Twenty-seven completed self-administered, 24-hour dietary recalls to measure dietary intake at baseline and 3-months. Micronutrient adequacy and diet quality was assessed using Dietary Reference Intakes (DRIs) and the Healthy Eating Index (HEI).
Results:
Seventy percent of participants were classified as low or moderate micronutrient adequacy at baseline. The proportion of participants with high micronutrient adequacy increased from 30% to 48% at 3-month follow-up. Total HEI and most HEI components increased at follow-up; with a statistically significant increase in seafood/plant protein score (P = .007).
Conclusions and Implications for Practice:
Our results suggest an inadequacy in micronutrient intake in university and healthcare employees and that teaching kitchens may help improve micronutrient adequacy and diet quality.
Keywords: ASA-24, diet quality, dietary recall, Healthy Eating Index, micronutrient adequacy, nutrition education, plant-based, teaching kitchen
Background
Over 40% of United States (US) adults have inadequate intakes of key micronutrients important for maintaining and promoting human health.1 Biochemical measures of micronutrient status suggest 30% of the US population are at risk of suffering from at least one vitamin deficiency, 6.3% are at risk of at least 2 vitamin deficiencies, and 1.7% are at risk of between 3 and 5 vitamin deficiencies.2,3 Micronutrient inadequacy contributes to poor disease outcomes and deficiencies of key micronutrients can disrupt system-wide biochemical functioning.4 Hence, it is important to improve adherence to specific micronutrient DRIs and identifying strategic methods for innovative, educational strategies to improve micronutrient intake and diet quality.5 Interventions aimed at improving healthy eating behaviors have demonstrated mixed results in terms of improving individual micronutrient adequacy.6,7
Teaching kitchens blend didactic and experiential learning techniques to enhance nutrition knowledge and cooking skills for promoting healthy eating strategies and improving health.8 Teaching kitchens vary in design and their curriculum often encompasses additional lifestyle components.8 Several studies that have reported improved diet quality in participants following participation in teaching kitchen programs.9-11 However, most previous literature on teaching kitchens measure nutrition-related outcomes through nutrition knowledge, cooking behavior, and eating habit questionnaires. Few have used validated nutritional intake methods to quantify nutrient intake and compare with national dietary recommendations and guidelines. Understanding whether teaching kitchens can improve adherence to dietary recommendations will help determine if they are effective strategies for improving health.
This study aims to evaluate changes in micronutrient adequacy in healthcare and university employees following participation in the Emory Healthy Kitchen Collaborative (EHKC) 10-week, plant-based teaching kitchen program. Additionally, we evaluate changes in diet quality. We hypothesized both micronutrient adequacy and diet quality would improve following the EHKC teaching kitchen program.
Methods
Study design
The EHKC teaching kitchen program consisted of a 20-hour, self-care curriculum, administered in five, 4-hour Saturday classes over the course of 10 weeks spanning August to October 2019.12 The nutrition component of the curriculum emphasized whole food, plant-based nutrition and included didactic instruction (3 hours of nutrition education, 1 of mindfulness-based eating, and 1 of ethnobotany) and experiential learning sessions (5 1-hour culinary skill-based instruction sessions with hands-on cooking demonstrations and 5 30-minute mindful eating sessions). Additional EHKC teaching kitchen sessions were held on physical activity, yoga, and stress management. The research study was conducted as a pilot study of a targeted convenience sample without a control group. As our primary outcome does not have established effect sizes, a power analysis was not performed.
Participants
Benefits-eligible Emory employees were eligible to participate in the EHKC teaching kitchen program. Employees interested in the program applied and were invited based on a priori selection criteria favoring those with an elevated body mass index (BMI), comorbid conditions, and exhibiting a high level of motivation for lifestyle change. Inclusion criteria required applicants agree to attend all classes and study visits and provide consent to video and photography throughout the program. Applicants with health conditions limiting their participation in the program were excluded. All enrolled participants provided written consent prior to participation in the program.
Measures
Participants completed a single, 24-hour dietary recall at baseline and again at 3-months follow-up using the Automated Self-Administered 24-hour (ASA24) dietary assessment tool.13 Micronutrient adequacy for 9 vitamins and 13 minerals were determined using the Dietary Reference Intake (DRI) guidelines and were defined as meeting their respective Estimated Average Requirement (EAR) or Adequate Intake (AI).14 The frequency and proportion of individuals meeting DRIs for each individual micronutrient were calculated. The total number of DRI’s achieved were determined for each participant and categorized into 3 adequacy groups classified as low adequacy (meeting ⩽7 of 22 micronutrient DRIs), moderate adequacy (meeting between 8 and 14 of 22 micronutrients) and high adequacy (meeting ⩾15 of 22 micronutrients). Diet quality was evaluated using the Healthy Eating Index (HEI), an indicator of adherence to the US Dietary Guidelines for Americans, but not specifically to plant-based diets.15,16
Statistical analysis
Descriptive statistics were performed on demographic characteristics. As not all 38 participants completed the ASA24, we assessed potential respondent bias in the subsample of teaching kitchen participants who completed the ASA24 data collection using two-sample t-tests and chi-square tests of the demographic characteristics between the ASA24 subsample and the non-respondent subsample. Fischer’s exact test was used for frequency counts of five or less. The paired t-test was used to determine differences among participants and the frequency of DRI’s met. The McNemar test was performed to evaluate differences in the proportion of participants meeting the EAR or AI for each individual micronutrient. The paired Wilcoxon signed-rank test was used to evaluate differences in HEI total scores and HEI component scores between baseline and 3-month follow-up points. Alpha values <0.05 were considered statistically significant. To adjust for multiple comparisons, false discovery rate (FDR) correction was applied using the Benjamini-Hochberg procedure and a q-value threshold of 0.1 was used.17 All data analysis was performed using StataSE 17 (StataCorp 2021). The study protocol was approved by the Emory University Institution Review Board (IRB 00109546) and registered with ClinicalTrials.gov (NCT04005495).
Results
Thirty-eight benefits-eligible Emory employees aged 26 to 63 participated in the EHKC teaching kitchen program. Twenty-seven completed both baseline and 3-month ASA24 dietary recalls and are the cohort presented in this study. Demographics and clinical characteristics did not differ between the participants completing the ASA24 (n = 27) dietary assessment and participants who did not complete the assessment (n = 11) (P > .05; Supplemental Appendix Table 1). The mean age of our cohort was 48.3 years (standard deviation (SD): ±10.4), mean BMI was 35.1 (SD: ±6.2), 93% were female, and 67% were African American. Most participants had a bachelor’s degree or higher (70%) and an income ranging between $25 000 and $99 999 (74%).
At baseline, 30% (n = 8) of participants had low micronutrient adequacy, 40% (n = 11) of participants had moderate micronutrient adequacy, and 30% (n = 8) of participants had high micronutrient adequacy (Table 1). The percent of participants with low and moderate micronutrient adequacy decreased to 19% (n = 5) and 33% (n = 9) respectively at 3-month follow-up. The percent of participants with high micronutrient adequacy increased to 48% (n = 13) at 3-month follow-up. There were no significant differences between the frequencies of DRI’s met at baseline compared to 3-month follow up. At neither timepoint did any participant meet all 22 micronutrient DRIs.
Table 1.
Percentages of Emory Healthy Kitchen Collaborative teaching kitchen participants for determined micronutrient intake categories at baseline and 3-month follow-up, August to October 2019.
| Micronutrient intake adequacy categoriesa | Baseline N (%) | Follow-up N (%) |
|---|---|---|
| Low adequacy: Meeting DRI for less than or equal to 7 micronutrients | 8 (30) | 5 (19) |
| Moderate adequacy: Meeting DRIs for 8-14 micronutrients | 11 (40) | 9 (33) |
| High adequacy: Meeting DRIs for greater than or equal to 15 micronutrients | 8 (30) | 13 (48) |
n = 27. *P = .071, *test statistic = −1.88 for paired t-test for differences among participants in frequencies of micronutrient DRI’s met at baseline and 3-month follow-up.
Categories developed using estimated average requirements and adequate intake values taken from the National Institutes of Health for specific sex and age categories. Zero participants met all individual micronutrient requirements at baseline or follow-up.
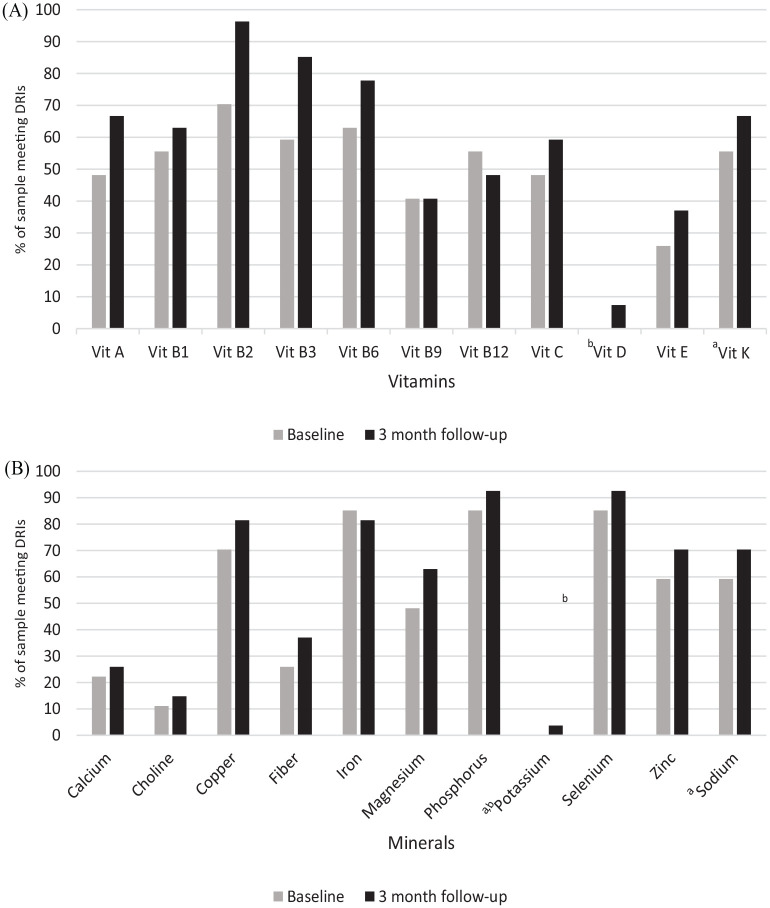
For specific micronutrients vitamin A, vitamin B1, vitamin B2, vitamin B3, vitamin B6, vitamin C, vitamin D, vitamin E, and vitamin K, calcium, choline, copper, fiber, magnesium, phosphorus, potassium, selenium, sodium, and zinc, the percent of participants meeting the DRI increased at 3-month follow-up; although increases were not statistically significant (P > .05; Figure 1). Compared to baseline, the percent of participants meeting the DRI for vitamin B12 and iron decreased at 3-month follow-up (P > .05; Figure 1). Vitamin B9 remained unchanged compared to baseline.
Figure 1.
Percent of Emory Healthy Kitchen Collaborative teaching kitchen participants meeting/exceeding the DRI recommendations for (A) vitamins and (B) minerals for baseline and 3-month follow-up, August to October 2019.
n = 27. Estimated average requirement and adequate intake values are taken from the National Institutes of Health for specific sex and age categories. No significant differences observed from the McNemar test for differences in proportions of dietary reference intake adequacy for paired sample.
aNot enough data exists to determine estimated average requirement value for these nutrients.
bBaseline values were essentially 0.
Adequate intake is used instead.
Mean HEI seafood and plant-protein’s component score significantly increased from 2.16 (SD: ±2.21) to 3.85 (SD: ±1.78) (mean change of 1.69; P = 0.007; Table 2). Compared to baseline, 3-month follow-up demonstrated increases in HEI total score (+7.17) and HEI adequacy component scores for total vegetables (+0.48), greens and beans (+0.35), total fruit (+0.50), whole fruit (+0.25), whole grains (+0.48), total dairy (+0.88), total protein (+0.71), and fatty acids (+0.14); however, these increases did not reach statistical significance (P > .05; Table 2). Mean changes in HEI moderation component scores increased for refined grains (+1.01) and sugars (+1.31), and decreased for sodium (−0.45), and saturated fat (−0.18) (P > .05; Table 2). Adequacy components are directly related to healthy eating index scoring; increased consumption yields higher component score. Moderation components are inversely related to healthy eating index scoring; increased consumption yields decreases in component score.
Table 2.
Comparisons of changes in Healthy Eating Index (HEI) total and component scores in Emory Healthy Kitchen Collaborative teaching kitchen participants between baseline and 3-month follow-up, August to October 2019.
| HEI Score/Component | Baseline mean ±SD | Follow-up mean ±SD | 3-month change |
|---|---|---|---|
| Total score | 54.94 ± 13.42 | 62.11 ± 13.32 | 7.17 |
| Adequacy Components a | |||
| Total vegetables | 3.69 ± 1.78 | 4.17 ± 1.45 | 0.48 |
| Greens and beans | 2.88 ± 2.37 | 3.23 ± 2.31 | 0.35 |
| Total fruit | 1.94 ± 2.22 | 2.44 ± 2.30 | 0.50 |
| Whole fruit | 2.10 ± 2.39 | 2.35 ± 2.33 | 0.25 |
| Whole grains | 3.76 ± 3.80 | 4.24 ± 3.87 | 0.48 |
| Total dairy | 3.43 ± 3.77 | 4.31 ± 3.84 | 0.88 |
| Total protein foods | 3.87 ± 1.69 | 4.58 ± 0.93 | 0.71 |
| Seafood/ and plant proteins | 2.16 ± 2.21 | 3.85 ± 1.78 | 1.69* |
| Fatty acids | 6.64 ± 3.57 | 6.78 ± 3.90 | 0.14 |
| Moderation components b | |||
| Sodium | 3.83 ± 3.99 | 3.38 ± 3.81 | –0.45 |
| Refined grains | 7.53 ± 3.30 | 8.54 ± 2.38 | 1.01 |
| Saturated fats | 5.99 ± 3.75 | 5.81 ± 3.80 | –0.18 |
| Added sugars | 7.12 ± 3.39 | 8.43 ± 2.88 | 1.31 |
n = 27. *P-value < .05, from the Wilcoxon-signed Rank test of means for a paired sample.
Adequacy components are directly related to healthy eating index scoring; increased consumption yields a higher component score.
Moderation components are inversely related to healthy eating index scoring; increased consumption yields a decreased component score.
Discussion
Following the EHKC teaching kitchen program, we observed an 18% increase in the percent of participants meeting high micronutrient adequacy. Although it was not statistically significant, we find this to be clinically meaningful. Seventy-percent of participants in this study demonstrated low and moderate-micronutrient adequacy at baseline, suggesting a substantial inadequacy in micronutrient intake in our study population. This aligns with data from the National Health and Nutrition Examination Survey (NHANES) suggesting the overall US population maintains inadequate intakes in 45% of micronutrients.18
When looking at micronutrients individually, we observed increases in the percent of our sample meeting DRI’s for vitamins A, C, D, E, and K, and calcium, magnesium, dietary fiber, potassium, and choline. These specific micronutrients have been previously reported as being under consumed by most of the US population.18 Lin et al similarly observed improved adherence to DRI recommendations for vitamins A, C, calcium, and magnesium in adults 25 years and older following a behavioral lifestyle intervention paired with the Dietary Approaches to Stop Hypertension (DASH) diet recommendation.19 The EHKC program emphasized plant-based nutrition education which may explain the decrease in meeting DRI’s for iron and vitamin B12 compared to baseline, as these are predominantly found in animal food. Our results suggest the EHKC teaching kitchen program may be useful for improving micronutrient adequacy overall by improving intake of certain micronutrients.
We observed a significant improvement in diet quality relating to seafood and plant protein’s HEI component score during follow-up. Additionally, HEI total score and component scores for total vegetables, greens and beans, total fruit, whole fruit, whole grains, total dairy, total protein, fatty acids, refined grains, and added sugars suggested improvements in diet quality that may be of clinical relevance. The program’s emphasis on plant-based nutrition strategies may explain the significant improvements seen in the intake of plant proteins. This is in line with prior studies that have reported improved diet quality in participants following participation in teaching kitchen programs.9-11 Razavi et al reported a significant increase in Mediterranean diet score in families following a 6-week Mediterranean diet-focused, randomized teaching kitchen intervention.11 Dexter et al reported a significant increase in the number of overweight and obese veterans who reported consumption of fruits, vegetables, fish, whole grains, liquid oils, and trans-fat free products following 5-weeks of a teaching kitchen program.9 Outcomes from our program are unique in that validated dietary intake methods were used to calculate nutrient intake and national dietary guidelines were used to evaluate diet quality. Considering higher HEI total scores are associated with a reduced risk for chronic disease such as cardiovascular disease, obesity, and depression, increases in HEI component scores may lead to improved health outcomes.20-22
Limitations
Limitations of the study include the relatively small sample size, assessment methods, and inability to determine long-term effects of the intervention. Although validated dietary assessment methods were used, single 24-hour recalls may not fully capture dietary patterns. Due to their inability to capture day-to-day variability in dietary intake, evaluation of “usual intake” through single 24-hour recalls report lower validity compared to multiple 24-hour recalls or semi-quantitative food frequency questionnaires.23 In addition, self-reported methods are commonly subject to response bias.23 The lack of a control group limits our ability to attribute changes strictly to the intervention. Lastly, follow-up occurred at the end of the 10-week course; therefore, long-term effects of the intervention on micronutrient adequacy and diet quality cannot be determined.
Implications for Research and Practice
This study demonstrated a substantial proportion of university and healthcare employees report inadequate micronutrient intakes of key micronutrients, and highlights the need for effective nutrition education strategies to improve micronutrient adequacy and diet quality. Our results suggest teaching kitchens may serve as an effective strategy for improving micronutrient adequacy and diet quality. Future studies using validated nutrient intake methods could incorporate larger, diverse samples to improve statistical power and generalizability, multiple 24-hour dietary recalls to account for usual intake, and longer follow-up to determine teaching kitchen’s effectiveness of improving long-term dietary intake.
Supplemental Material
Supplemental material, sj-docx-1-nmi-10.1177_11786388231159192 for A Teaching Kitchen Program Improves Employee Micronutrient and Healthy Dietary Consumption by Miranda A Moore, Benjamin A Cousineau, Krystyna Rastorguieva, Jonathan P Bonnet and Sharon H Bergquist in Nutrition and Metabolic Insights
Acknowledgments
We would like to thank the Seavey Clinic staff for facilitating the Emory Health Kitchen Collaborative program.
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study is supported by a grant from the Ardmore Institute of Health (Award ID 0000050387), the Seavey Clinic Director’s Fund, and the John and Mary Brock Diagnostic and Discovery Fund; the sponsors did not play a role in study design, data collection, interpretation, or manuscript preparation. Financial Disclosures Dr. Miranda Moore reports receiving funding from National Institutes of Health, Agency for Healthcare Research and Quality’s, Health Resources and Services Administration, Ardmore Institute of Health, Georgia State Department of Human Services, and the Alzheimer’s Association.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: Conception and design: SHB, KR, MAM, JPB. Collection and assembly of data: SHB, KR, MAM, JPB. Data analysis and interpretation: All Authors. Manuscript writing: All Authors. Final approval of manuscript: All Authors. Accountable for all aspects of the work: SHB, KR, MAM, JPB.
Data Availability: Deidentified data can be obtained from the authors upon email request.
ORCID iD: Miranda A Moore  https://orcid.org/0000-0002-1455-6099
https://orcid.org/0000-0002-1455-6099
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Agarwal S, Reider C, Brooks JR, Fulgoni VL. Comparison of prevalence of inadequate nutrient intake based on body weight status of adults in the United States: an analysis of NHANES 2001-2008. J Am Coll Nutr. 2015;34:126-134. [DOI] [PubMed] [Google Scholar]
- 2. Shenkin A. The key role of micronutrients. Clin Nutr. 2006;25:1-13. [DOI] [PubMed] [Google Scholar]
- 3. Bird JK, Murphy RA, Ciappio ED, McBurney MI. Risk of deficiency in multiple concurrent micronutrients in children and adults in the United States. Nutrients. 2017;9:655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hoeft B, Weber P, Eggersdorfer M. Micronutrients - a global perspective on intake, health benefits and economics. Int J Vitam Nutr Res. 2012;82:316-320. [DOI] [PubMed] [Google Scholar]
- 5. Burch GF, Giambatista R, Batchelor JH, Burch JJ, Hoover JD, Heller NA. A Meta-Analysis of the relationship between experiential learning and learning outcomes. Decis Sci J Innov Educ. 2019;17:239-273. [Google Scholar]
- 6. Jensen SK, Yates B, Lyden E, Krogstrand KS, Hanson C. Dietary micronutrient intake of participants in a “partners together in health” cardiac rehabilitation intervention. J Cardiopulm Rehabil Prev. 2018;38:388-393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ojeda-Rodríguez A, Zazpe I, Morell-Azanza L, Chueca MJ, Azcona-Sanjulian MC, Marti A. Improved diet quality and nutrient adequacy in children and adolescents with abdominal obesity after a lifestyle intervention. Nutrients. 2018;10:1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eisenberg DM, Imamura A. Teaching kitchens in the learning and work environments: the future is now. Glob Adv Health Med. 2020;9:2164956120962442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dexter AS, Pope JF, Erickson D, Fontenot C, Ollendike E, Walker E. Cooking education improves cooking confidence and dietary habits in veterans. Diabetes Educ. 2019;45:442-449. [DOI] [PubMed] [Google Scholar]
- 10. Miller MF, Li Z, Habedank M. A randomized controlled trial testing the effectiveness of coping with cancer in the kitchen, a nutrition education program for cancer survivors. Nutrients. 2020;12:3144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Razavi AC, Sapin A, Monlezun DJ, et al. Effect of culinary education curriculum on Mediterranean diet adherence and food cost savings in families: A randomised controlled trial. Public Health Nutr. 2021;24:2297-2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Munroe D, Moore MA, Bonnet JP, et al. Development of culinary and self-care programs in diverse settings: theoretical considerations and available evidence. Am J Lifestyle Med. 2022;16:672-683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. National Cancer Institute. Automated Self-Administered 24-Hour (ASA24) Dietary Assessment Tool. National Cancer Institute; 2018. [Google Scholar]
- 14. Institute of Medicine (US) Subcommittee on Interpretation and Uses of Dietary Reference Intakes, Institute of Medicine (US). Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. DRI Dietary Reference Intakes: Applications in Dietary Assessment. National Academies Press (US); 2000. Accessed October 24, 2021. http://www.ncbi.nlm.nih.gov/books/NBK222890/ [PubMed] [Google Scholar]
- 15. Kennedy ET, Ohls J, Carlson S, Fleming K. The Healthy Eating Index: Design and applications. J Am Diet Assoc. 1995;95:1103-1108. [DOI] [PubMed] [Google Scholar]
- 16. Krebs-Smith SM, Pannucci TE, Subar AF, et al. Update of the Healthy Eating Index: HEI-2015. J Acad Nutr Diet. 2018;118:1591-1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Glickman ME, Rao SR, Schultz MR. False discovery rate control is a recommended alternative to Bonferroni-type adjustments in health studies. J Clin Epidemiol. 2014;67:850-857. [DOI] [PubMed] [Google Scholar]
- 18. Dietary Guidelines Advisory Committee. Scientific Report of the 2020 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Agriculture and Secretary of Health and Human Services. U.S. Department of Agriculture, Agricultural Research Service; 2020. doi: 10.52570/DGAC2020 [DOI] [Google Scholar]
- 19. Lin PH, Appel LJ, Funk K, et al. The PREMIER intervention helps participants follow the dietary approaches to stop hypertension dietary pattern and the current dietary reference intakes recommendations. J Am Diet Assoc. 2007;107:1541-1551. [DOI] [PubMed] [Google Scholar]
- 20. Tande DL, Magel R, Strand BN. Healthy Eating Index and abdominal obesity. Public Health Nutr. 2010;13:208-214. [DOI] [PubMed] [Google Scholar]
- 21. Shan Z, Li Y, Baden MY, et al. Association between healthy eating patterns and risk of cardiovascular disease. JAMA Intern Med. 2020;180:1090-1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wang K, Zhao Y, Nie J, Xu H, Yu C, Wang S. Higher HEI-2015 score is associated with reduced risk of depression: result from NHANES 2005-2016. Nutrients. 2021;13:348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yuan C, Spiegelman D, Rimm EB, et al. Relative validity of nutrient intakes assessed by questionnaire, 24-hour recalls, and diet records as compared with urinary recovery and plasma concentration biomarkers: findings for women. Am J Epidemiol. 2018;187:1051-1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-nmi-10.1177_11786388231159192 for A Teaching Kitchen Program Improves Employee Micronutrient and Healthy Dietary Consumption by Miranda A Moore, Benjamin A Cousineau, Krystyna Rastorguieva, Jonathan P Bonnet and Sharon H Bergquist in Nutrition and Metabolic Insights