Abstract
Background
COVID-19 vaccination refusal/hesitancy among patients with cancer has been reported to be high. This study aimed to assess vaccination status and attitudes towards COVID-19 vaccines in patients with cancer undergoing active treatment in a single center in Mexico.
Methods
A cross-sectional, 26-item survey evaluating vaccination status and attitudes towards COVID-19 vaccination was conducted among patients undergoing active cancer treatment. Descriptive statistics were used to analyze the sociodemographic characteristics, vaccination status, and attitudes. X2 tests and multivariate analysis were used to evaluate associations between characteristics and attitudes with adequate vaccination status.
Results
Of 201 respondents, 95% had received at least one dose, and 67% had adequate COVID-19 vaccination status (≥ 3 doses). Thirty-six percent of patients had at least one reason for doubting/rejecting vaccination, and the main reason was being afraid of side effects. On multivariate analysis, age ≥ 60 years (odds ratio (OR) 3.77), mass media as main source of information on COVID-19 (OR 2.55), agreeing vaccination against COVID-19 is safe in patients with cancer (OR 3.11), and not being afraid of the composition of the COVID-19 vaccines (OR 5.10) statistically increased the likelihood of adequate vaccination status.
Conclusions
Our study shows high vaccination rates and positive attitudes towards COVID-19 vaccines, with a significant proportion of patients undergoing active cancer treatment with adequate vaccination status (≥ 3 doses). Older age, use of mass media as main source of COVID-19 information, and positive attitudes towards COVID-19 vaccines were significantly associated with a higher likelihood of adequate COVID-19 vaccination status among patients with cancer.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00520-023-07667-w.
Keywords: COVID-19, Vaccines, Cancer, Acceptance, Hesitancy, Attitudes
Background
On January 30, 2020, the World Health Organization (WHO) declared a global state of emergency due to the pandemic spread of the new coronavirus (SARS-CoV-2), which causes the coronavirus disease (COVID-19) [1]. Multiple vaccines against COVID-19 have been proven to reduce the risk of serious illness and death [2]. Although a wide range of vaccines against COVID-19 have been approved and disseminated nationally since December 2020, Mexico still ranks second in global mortality with a fatality rate of 5.7% [3],[4]. Furthermore, the 2020 National Survey on Health and Nutrition (Encuesta Nacional de Salud y Nutricion 2020 [ENSANUT]) reported that the rate of acceptance, rejection, and doubt about vaccination against COVID-19 in the general population was 62.3%, 28.2%, and 9.5%, respectively. The main factors associated with rejection and doubt identified in this report were female sex, older age, lower educational level, lower socioeconomic level, and working in the informal sector [5].
Patients with cancer have been shown to be more susceptible to COVID-19 infection and have a higher risk of death from COVID-19 [6]. Therefore, different international organizations, such as the National Comprehensive Cancer Network [7], the American Society of Clinical Oncology [8], and the European Society for Medical Oncology, [9] recommend vaccination against COVID-19 in all adults diagnosed with cancer. Similarly, the Mexican Society of Oncology (SMEO) also recommends vaccination against COVID-19 in all adult patients with cancer [10]. Nonetheless, COVID-19 vaccination refusal or hesitancy among patients with cancer has been reported to be high [11].
In Mexico, data on vaccination acceptance against COVID-19 in patients with cancer is scarce. A prior survey of women with breast cancer living in Mexico showed that 34% were hesitant to be vaccinated, 4% would only do so if vaccination was compulsory, and 3% would refuse to be vaccinated altogether [12]. Therefore, the objective of this study was to assess the vaccination status against COVID-19 and analyze attitudes towards COVID-19 vaccines in patients with cancer undergoing active cancer treatment in a referral center in Mexico.
Methods
Study design and data collection
We designed a cross-sectional, web-based survey exploring vaccination status, attitudes, and reasons for hesitancy towards COVID-19 vaccination among patients undergoing active cancer treatment. The conduct and reporting of the study adhered to the Consensus-Based Checklist for Reporting of Survey Studies (CROSS) [13], which is included in Supplementary Appendix 1. The survey included four separate sections with 26 items addressing participants’ characteristics, previous experience with COVID-19, vaccination status, and attitudes towards COVID-19 vaccination. The survey was designed based on validated items and/or questions included in previous publications measuring vaccination attitudes towards COVID-19 vaccination among patients with cancer and general population [14–17]. The sociodemographic characteristics of patients, clinical characteristics, previous experience with COVID-19, vaccination status, and reasons for hesitancy towards COVID-19 vaccination were obtained through multiple-choice questions. Attitudes towards vaccination against COVID-19 were evaluated using a five-point Likert scale. The final version of the survey was pretested by the investigators, and reviewed and approved by a local panel of cancer specialists, which included one medical oncologist and two clinical researchers with experience in the field. The full survey is included in Supplementary Appendix 2.
Survey population and administration
The survey was created and answered by participants using the REDCap (Research Electronic Data Capture) electronic data capture tool hosted at the Instituto Nacional de Ciencias Medicas y Nutricion Salvador Zubiran (INCMNSZ). All consecutive patients undergoing active cancer treatment (chemotherapy and/or immunotherapy) at the Infusion Center at INCMNSZ were invited to participate in person before, during, or after the administration of systemic treatment. Participants were provided with a tablet to answer the web-based survey, and answers were collected from May 2nd, 2022, to July 22nd, 2022. Considering a prevalence of cancer in Mexico of 125,944 and considering an expected proportion of fully vaccinated individuals of 65%, a sample size of 207 would allow us to estimate the true population proportion with a margin of error of 6.5 and a 95% confidence level.
Ethical considerations
No identifying data were obtained from participants. All participants were informed about the purpose of the study. The invitation to participate in this study was also included in the heading of the questionnaire, and by accepting such an invitation, consent was implied. Study procedures were reviewed and approved by the Institutional Review Board at INCMNSZ.
Statistical analysis
Analyses were performed only on patients’ responses who answered the survey completely. Descriptive statistics, including means, medians, and standard deviations, were used to analyze the sociodemographic characteristics of patients, clinical characteristics, previous experience with COVID-19, vaccination status, and reasons for hesitancy towards COVID-19 vaccination. Vaccination status was considered adequate if patients had received ≥ 3 doses of COVID-19 vaccination (primary vaccination series plus at least one booster dose), as was recommended by the WHO at the time the survey was conducted [18]. In Mexico, four doses (or second booster) of COVID-19 vaccination became approved in April 2022, only for patients aged ≥ 60 years, those with comorbidities, and healthcare professionals [19]. Answers regarding attitudes were dichotomized into “agree” (“strongly agree” and “agree”) versus “disagree” (“neutral,” “disagree,” and “strongly disagree”) for comparing associations with vaccination status. X2 tests were used to evaluate associations between patients’ characteristics, previous experience with COVID-19, and attitudes towards COVID-19 vaccines with adequate vaccination status. Variables associated with univariable p value < 0.05 were evaluated in a multivariable logistic regression model. A p-value < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS (Statistical Package for the Social Sciences) v25.
Results
Respondents’ characteristics
Of the 245 eligible patients undergoing active cancer treatment with chemotherapy and/or immunotherapy in the Infusion Center at INCMNSZ, 39 patients did not attend their appointment or were not reached by the investigators. Among 206 (84.1%) patients invited to participate, a total of 201 (82%) answered the survey completely. The median age was 62 years (range 19–92 years), 58% were aged 60 years and older, 57% were women, and 50% lived in the Mexico City metropolitan area. Sixty percent were in a couple (married or in a domestic partnership), 38% had higher education (university or post-graduate studies), and 46% were unemployed. Regarding the type of healthcare coverage, 76% had governmental public healthcare (Instituto de Salud para el Bienestar [INSABI], Institute of Health for Wellbeing in English), 23% had social security (Instituto Mexicano del Seguro Social [IMSS], Mexican Institute of Social Security in English, or Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado [ISSSTE], Institute for Social Security and Services for State Workers in English), and only 1% had private insurance. Regarding most frequent tumor types, 16% had colorectal cancer, 14% breast cancer, 14% pancreatic cancer, and 7% prostate cancer. Fifty-two percent of patients had metastatic disease and the remaining 48% had localized disease. Regarding active cancer treatment, 86% of patients were receiving systemic chemotherapy, 9% concurrent chemo-radiotherapy, and 5% immunotherapy. General characteristics of the included respondents are shown in Table 1.
Table 1.
Respondents’ characteristics
| Characteristics | n = 201 (%) |
|---|---|
| Gender | |
| Male | 86 (42.8%) |
| Female | 115 (57.2%) |
| Age | |
| < 60 years | 89 (44.3%) |
| ≥ 60 years | 112 (55.7%) |
| Place of residence | |
| Mexico City | 101 (50.2%) |
| State of Mexico | 39 (19.4%) |
| Morelos | 12 (6.0%) |
| Other | 49 (24.4%) |
| Marital status | |
| Single | 44 (21.9%) |
| Married | 109 (54.2%) |
| Divorced | 22 (10.9%) |
| Widowed | 14 (7.0%) |
| Domestic partnership | 12 (6.0%) |
| Education level | |
| No education | 3 (1.5%) |
| Elementary school | 36 (17.9%) |
| Middle school | 38 (18.9%) |
| High school | 47 (23.4%) |
| University | 62 (30.8%) |
| Postgraduate | 15 (7.5%) |
| Occupation | |
| Student | 5 (2.5%) |
| Employed | 71 (35.3%) |
| Unemployed | 92 (45.8%) |
| Retired | 33 (16.4%) |
| Type of healthcare coverage | |
| IMSS | 29 (14.4%) |
| ISSSTE | 18 (9.0%) |
| INSABI | 152 (75.6%) |
| Private | 2 (1%) |
| Primary tumor | |
| Colorectal | 33 (16.4%) |
| Breast | 29 (14.4%) |
| Pancreas | 29 (14.4%) |
| Prostate | 14 (7.0%) |
| Others | 83 (41.3%) |
| Disease extension | |
| Localized | 97 (48.3%) |
| Metastatic | 104 (51.7%) |
| Active cancer treatment | |
| Chemotherapy | 172 (85.6%) |
| Concurrent chemo-radiotherapy | 19 (9.4%) |
| Immunotherapy | 10 (5.0%) |
Previous experience with COVID-19
Thirty-one percent (n = 62) of the participants had a personal history of COVID-19 infection prior to the survey, and 4% (n = 8) required in-hospital treatment for COVID-19. Seventy-four percent (n = 149) knew somebody who had had COVID-19 infection, and 38% (n = 77) knew somebody who had died because of COVID-19 infection. Patients reported using the following sources for obtaining information regarding COVID-19: mass media (newspapers or broadcast television) (82%), social media (23%), family members (15%), and healthcare professionals (5%).
Vaccination status against COVID-19
Ninety-five percent of included patients reported having received at least one dose of COVID-19 vaccination, with a median of 3 doses (range 0–4). At the moment of the survey, 56% had received three doses and 11% four doses, summing up to 67% of patients with adequate COVID-19 vaccination status (≥ 3 doses).
Attitudes towards COVID-19 vaccination
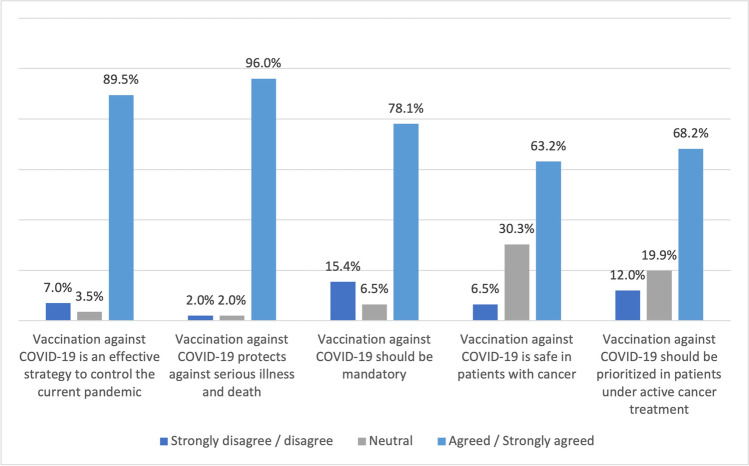
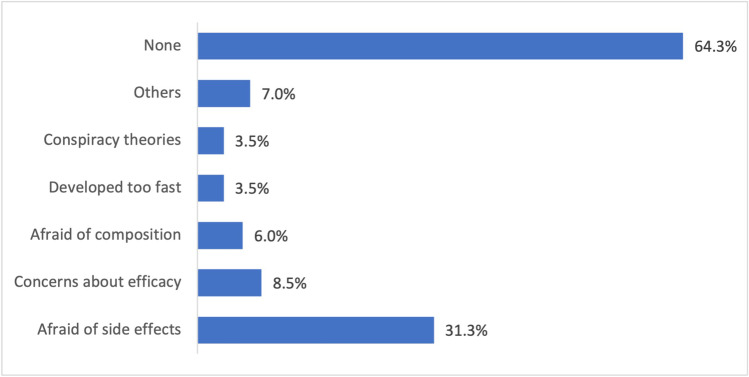
Ninety percent agreed/strongly agreed that vaccination against COVID-19 is an effective strategy to control the current pandemic, 96% agreed/strongly agreed that vaccination against COVID-19 reduces risk of complications and death, and 78% agreed/strongly agreed that COVID-19 vaccination should be mandatory for the general population. Sixty-three percent believed COVID-19 vaccines are safe in patients with cancer, and 68% that patients undergoing active cancer treatment should get vaccinated first. Attitudes towards COVID-19 vaccination are shown in Fig. 1. Thirty-six percent of the patients had at least one reason for doubting and/or rejecting vaccination against COVID-19. Main reasons for hesitancy included being afraid of the vaccines’ side effects (31%), concerns about the effectiveness of the vaccines (9%), and being afraid of the composition of the vaccine (6%). Figure 2 shows participants’ reasons for hesitancy to COVID-19 vaccinations.
Fig. 1.
Attitudes towards COVID-19 vaccination
Fig. 2.
Reasons for hesitancy towards COVID-19 vaccination
Associations between patients’ characteristics and attitudes with adequate vaccination status
On the univariate analysis, patients 60 years and older were more likely to have adequate COVID-19 vaccination status (≥ 3 doses) than patients younger than 60 years (80.4% vs 49.4%, p < 0.001, respectively). Other sociodemographic characteristics, including sex, place of residence, marital status, occupation, and educational level, were not associated with adequate COVID-19 vaccination status. Clinical characteristics, including primary tumor site, disease extension, and treatment type, were also not associated with adequate COVID-19 vaccination. Personal history of previous COVID-19 infection and knowing somebody who suffered from COVID-19 infection were also not associated with vaccination status. Patients who used mass media (p = 0.003) and those who did not use social media (p = 0.01) as main sources to obtain information about COVID-19 were more likely to have at least 3 vaccine doses against COVID-19 (Table 2).
Table 2.
Associations between patients’ characteristics, previous COVID experience, and sources of information regarding COVID-19 and adequate COVID-19 vaccination
| Total number of patients | < 3 doses | ≥ 3 doses | p | |||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Patients’ characteristics | ||||||
| Gender | ||||||
| Male | 86 | 26 | 30.2 | 60 | 69.8 | 0.42 |
| Female | 115 | 41 | 35.7 | 74 | 64.3 | |
| Age | ||||||
| < 60 years | 89 | 45 | 50.6 | 44 | 49.4 | < 0.001 |
| ≥ 60 years | 112 | 22 | 19.6 | 90 | 80.4 | |
| Place of residence | ||||||
| Mexico City | 101 | 30 | 29.7 | 71 | 70.3 | 0.27 |
| Other | 100 | 37 | 37.0 | 63 | 63.0 | |
| Marital status | ||||||
| Unpartnered | 80 | 30 | 37.5 | 50 | 62.5 | 0.31 |
| Partnered | 121 | 37 | 30.6 | 84 | 69.4 | |
| Education level | ||||||
| Low | 124 | 45 | 36.3 | 79 | 63.7 | 0.26 |
| Higher | 77 | 22 | 28.6 | 55 | 71.4 | |
| Occupation | ||||||
| Student | 5 | 4 | 80.0 | 1 | 20.0 | 0.06 |
| Employed | 71 | 25 | 35.2 | 46 | 64.8 | |
| Unemployed/retired | 125 | 38 | 30.4 | 87 | 69.6 | |
| Healthcare coverage | ||||||
| IMSS/ISSSTE | 46 | 12 | 26.1 | 34 | 73.9 | 0.49 |
| INSABI | 152 | 54 | 35.5 | 98 | 64.5 | |
| Private | 3 | 1 | 33.3 | 2 | 66.7 | |
| Primary tumor site | ||||||
| Colorectal | 33 | 11 | 33.3 | 22 | 66.7 | 0.35 |
| Breast | 29 | 11 | 38.9 | 18 | 61.1 | |
| Pancreas | 29 | 7 | 24.1 | 22 | 75.9 | |
| Prostate | 14 | 2 | 14.3 | 12 | 85.7 | |
| Others | 96 | 26 | 27.1 | 60 | 72.9 | |
| Disease extension | ||||||
| Localized | 97 | 27 | 27.8 | 70 | 72.2 | 0.11 |
| Metastatic | 104 | 40 | 38.5 | 54 | 61.5 | |
| Treatment type | ||||||
| Chemotherapy | 172 | 58 | 33.7 | 114 | 66.3 | 0.96 |
| Concurrent chemo-radiation | 19 | 6 | 31.6 | 13 | 68.4 | |
| Immunotherapy | 10 | 3 | 30.0 | 7 | 70.0 | |
| Previous experience with COVID-19 | ||||||
| Previous COVID-19 infection | ||||||
| No | 139 | 49 | 35.3 | 90 | 64.7 | 0.39 |
| Yes | 62 | 18 | 29.0 | 44 | 71.0 | |
| Previous hospitalization due to COVID-19 infection | ||||||
| No | 193 | 65 | 33.7 | 128 | 66.3 | 0.61 |
| Yes | 8 | 2 | 25.0 | 6 | 75.0 | |
| Knows somebody who experienced COVID-19 infection | ||||||
| No | 52 | 21 | 40.4 | 31 | 59.6 | 0.21 |
| Yes | 149 | 46 | 30.9 | 103 | 69.1 | |
| Knows somebody who died due to COVID-19 infection | ||||||
| No | 124 | 46 | 37.1 | 78 | 62.9 | 0.15 |
| Yes | 77 | 21 | 27.3 | 56 | 72.7 | |
| Sources to obtain information about COVID-19 | ||||||
| Mass media | ||||||
| No | 37 | 20 | 54.1 | 17 | 45.9 | 0.003 |
| Yes | 164 | 47 | 28.7 | 117 | 71.3 | |
| Social media | ||||||
| No | 154 | 44 | 28.7 | 110 | 71.3 | 0.01 |
| Yes | 47 | 23 | 48.9 | 24 | 51.1 | |
| Family members and acquaintances | ||||||
| No | 171 | 58 | 33.9 | 113 | 66.1 | 0.17 |
| Yes | 30 | 9 | 30.0 | 21 | 70.0 | |
| Healthcare professionals | ||||||
| No | 190 | 64 | 33.7 | 126 | 66.3 | 0.66 |
| Yes | 11 | 3 | 27.3 | 8 | 72.7 | |
Patients who believed vaccination against COVID-19 should be mandatory (p = 0.003) and those who considered it safe in patients with cancer (p < 0.001) were more likely to have received at least 3 doses. Patients not concerned by the side effects of the vaccines (p = 0.024), those not afraid of the composition of the vaccines (p = 0.002), and those who did not have any reason against vaccination (p = 0.013) were more likely to have adequate vaccination status against COVID-19 (Table 3).
Table 3.
Associations between attitudes towards COVID-19 vaccination and adequate COVID-19 vaccination
| Total number of patients | < 3 doses | ≥ 3 doses | p | |||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Attitudes towards COVID-19 vaccinations | ||||||
| Vaccination against COVID-19 is an effective strategy to control the current pandemic | ||||||
| Disagree | 21 | 11 | 52.4 | 10 | 47.6 | 0.05 |
| Agree | 180 | 56 | 31.1 | 124 | 68.9 | |
| Vaccination against COVID-19 reduces the risk of complications and death | ||||||
| Disagree | 8 | 5 | 62.5 | 3 | 37.5 | 0.07 |
| Agree | 193 | 62 | 32.1 | 131 | 67.9 | |
| Vaccination against COVID-19 should be mandatory | ||||||
| Disagree | 44 | 23 | 52.3 | 21 | 47.7 | 0.003 |
| Agree | 157 | 44 | 28.0 | 113 | 72.0 | |
| Vaccination against COVID-19 is safe in patients undergoing active cancer treatment | ||||||
| Disagree | 74 | 38 | 51.4 | 36 | 48.6 | < 0.001 |
| Agree | 127 | 29 | 22.8 | 98 | 77.2 | |
| Vaccination against COVID-19 should be prioritized in patients with cancer | ||||||
| Disagree | 64 | 26 | 40.6 | 38 | 59.4 | 0.13 |
| Agree | 137 | 41 | 29.9 | 96 | 70.1 | |
| Reasons for hesitancy towards COVID-19 vaccinations | ||||||
| Afraid of side effects | ||||||
| No | 138 | 39 | 28.3 | 99 | 71.7 | 0.02 |
| Yes | 63 | 28 | 44.4 | 35 | 55.6 | |
| Concerns about efficacy | ||||||
| No | 184 | 58 | 31.5 | 126 | 68.5 | 0.07 |
| Yes | 17 | 9 | 52.9 | 8 | 47.1 | |
| Afraid of the composition of the vaccines | ||||||
| No | 189 | 58 | 30.7 | 131 | 69.3 | 0.002 |
| Yes | 12 | 9 | 75.0 | 3 | 25.0 | |
| Vaccines were developed very fast | ||||||
| No | 194 | 64 | 33.0 | 130 | 67.0 | 0.59 |
| Yes | 7 | 3 | 42.9 | 4 | 57.1 | |
| Religious beliefs | ||||||
| No | 200 | 66 | 33.0 | 134 | 67.0 | 0.16 |
| Yes | 1 | 1 | 100 | 0 | 0.0 | |
| COVID-19 does not exist | ||||||
| No | 200 | 66 | 33.0 | 134 | 67.0 | 0.16 |
| Yes | 1 | 1 | 100 | 0 | 0.0 | |
| Conspiracy theories | ||||||
| No | 194 | 63 | 32.5 | 131 | 67.5 | 0.17 |
| Yes | 7 | 4 | 57.1 | 3 | 42.9 | |
| I do not need the vaccine because I have a low risk of contagion | ||||||
| No | 200 | 66 | 33.0 | 134 | 67.0 | 0.16 |
| Yes | 1 | 1 | 100 | 0 | 0.0 | |
| I do not have reasons for hesitancy | ||||||
| No | 72 | 32 | 44.4 | 40 | 55.6 | 0.01 |
| Yes | 129 | 35 | 27.1 | 94 | 72.9 | |
On the multivariate analysis, age 60 years or older (odds ratio (OR) 3.77, 95% confidence interval (CI) 1.87–7.60; p < 0.01), using mass media as the main source of information on COVID-19 (OR 2.55, CI 95% 1.03–6.33; p = 0.04), agreeing vaccination against COVID-19 is safe in patients with cancer (OR 3.11, 95% CI 1.52–6.46; p < 0.01), and not being afraid of the composition of the vaccines against COVID-19 (OR 5.10, 95% CI 1.12–23.3; p = 0.04) remained as statistically significant factors increasing the likelihood of having an adequate vaccination status against COVID-19 (Table 4).
Table 4.
Multivariate analysis on factors increasing the likelihood of adequate COVID-19 vaccination
| Factors | Odds ratio | 95% Confidence interval | p |
|---|---|---|---|
| Aged ≥ 60 years | 3.77 | 1.87–7.60 | < 0.01 |
| Uses mass media as main source for information on COVID-19 | 2.55 | 1.03–6.33 | 0.04 |
| Uses social media as main source for information on COVID-19 | 0.85 | 0.35–2.04 | 0.71 |
| Agrees vaccination against COVID-19 should be mandatory | 1.69 | 0.73–3.89 | 0.22 |
| Agrees vaccination against COVID-19 is safe in patients undergoing active cancer treatment | 3.11 | 1.52–6.36 | < 0.01 |
| Not afraid of side effects of the vaccines against COVID-19 | 1.60 | 0.77–3.34 | 0.21 |
| Not afraid of the composition of the vaccines against COVID-19 | 5.10 | 1.12–23.3 | 0.04 |
Discussion
The results of our study show that a vast proportion of patients undergoing active cancer treatment in our center have been vaccinated against COVID-19. Furthermore, approximately two-thirds of our patients complied with the recommendation by the WHO of at least one booster dose at the time this survey was conducted [18].
Despite high hesitancy/refusal rates previously reported in the general population in Mexico, our findings demonstrate high vaccination rates among patients undergoing active cancer treatment. According to the ENSANUT survey conducted prior to the implementation of the vaccination campaign against COVID-19 in Mexico (November 2020) among the general population, 38% of the participants were hesitant or refused COVID-19 vaccination [5]. These results contrast with our findings, in which 95% of the participants had received at least one vaccine dose. However, a more recent survey conducted during the early vaccination rollout period in Mexico City (May–June 2021) found that the prevalence of vaccine hesitancy was 6% among the general population [20], similar to the percentage of patients in our study who had not received any vaccine dose against COVID-19. Finally, a later survey conducted among healthy adults and adults with chronic diseases in Mexico City (December 2021) found that 10.3% of adults with chronic diseases were not vaccinated against COVID-19 [21]. Therefore, patients with cancer undergoing active cancer treatment in our center appear to be less reluctant to COVID-19 vaccination than expected.
Patients with cancer have been described to be more hesitant to undergo COVID-19 vaccination, as demonstrated by a global population-based study exploring factors associated with vaccination intention against COVID-19, which showed that more patients with a history of cancer in the past 5 years were unwilling to receive vaccination against COVID-19 (61%) vs those without a history of cancer (14%) [22]. A meta-analysis on COVID-19 vaccine acceptance and hesitancy among patients with cancer, including 29 studies, found a pooled prevalence of vaccine acceptance of 59% and a pooled prevalence of vaccine hesitancy due to fear of vaccine-related side-effects of 53% [11]. However, adequate vaccination rates against COVID-19 in our study reached 67%, similar to the reported prevalence of adequate vaccination against COVID-19 among patients with cancer in a large cross-sectional study in Bosnia and Herzegovina (64%) [23]. Thus, factors associated with acceptance or hesitance to vaccination against COVID-19 may vary across different populations.
In our survey, older age increased the likelihood of having an adequate vaccination status (≥ 3 doses) against COVID-19. Likewise, older age has been repeatedly associated with a higher likelihood of vaccine acceptance among patients with cancer in other studies [12, 14, 15, 23–32]. Interestingly, a single-center study in France evaluating acceptance rate of COVID-19 vaccination and vaccine safety among older patients with cancer (≥ 70 years) conducted in January 2021 found a vaccine acceptance rate of 82.6% and an adequate vaccination rate (2 doses) reached 75.3% [33]. These results suggest older age is a predictive factor for adequate vaccination against COVID-19 among patients with cancer. Furthermore, positive attitudes towards COVID-19 vaccines have also been associated with higher acceptance of COVID-19 vaccination in patients with cancer in other studies [26, 28–30, 34–37]. In our survey, positive attitudes, such as believing that COVID-19 vaccines are safe in patients with cancer also increased the likelihood of having an adequate vaccination status (≥ 3 doses). These findings highlight the importance of positive attitudes with actually undergoing vaccination against COVID-19 in patients under active cancer treatment.
Finally, sources on COVID-19 information may play an important role in acceptance or resistance to COVID-19 vaccination. As in our study, mass media has been reported as the main source of information on COVID-19 among patients with cancer in previous studies [35, 38, 39]. Contrary to our results, in a study by Lazar et al. among patients with cancer, more unvaccinated as compared to vaccinated patients used mass media as their main source of information on COVID-19 (72.4% vs. 29.7%, respectively) [27]. Notably, some evidence suggests that patients with cancer were more likely to accept COVID-19 vaccination if they were advised to receive it by their oncologists [12, 15, 23–25, 27, 30, 37]. However, only 5% of patients in our study reported healthcare professionals as their main source of information on COVID-19. Despite the importance of medical oncologists in promoting COVID-19 vaccine acceptance among patients with cancer in other regions, in our center vaccine acceptance was mainly driven by mass media. This reflects a less important role of attending physicians in guiding patients’ attitudes and behaviors toward COVID-19 vaccination in our center. Transforming the role of healthcare professionals as pivotal sources of information on COVID-19 may help patients doubting/refusing to accept vaccination, especially patients undergoing active cancer treatment at high risk of complications from COVID-19 infection.
Our study has some limitations. First, as our study was conducted in a single center, the results obtained by this survey might not portray the vaccination rate and attitudes of the general population of patients undergoing active cancer treatment in Mexico. Second, data on efficacy and safety as perceived by patients, including short- and long-term adverse events, post-vaccine COVID-19 infection, COVID-19 infection severity, other COVID-19-related complications, and death, were not assessed by this survey. Third, vaccination status was not confirmed by vaccine certificates; therefore, results regarding vaccination status and attitudes towards COVID-19 vaccines may not be representative of real life, as patients may have exhibited a response bias, modifying their answers in response to their awareness of being evaluated. Nevertheless, our study has several strengths. A wide range of patients were included regarding age (19–92 years), place of residence, and various tumor types. Also, our survey assessed actual vaccination status and attitudes rather than willingness to accept or refuse COVID-19 vaccines, as in most previously reported studies. Finally, we evaluated the prevalence of patients with adequate COVID-19 vaccination status, defined as primary vaccination series plus at least one booster dose, which indirectly measures adherence to the WHO’s recommendations on COVID-19 vaccination [18].
Conclusions
The results of our study show high rates of COVID-19 vaccination and positive attitudes towards COVID-19 vaccines with a significant proportion of patients undergoing active cancer treatment with adequate vaccination status (≥ 3 doses) in a referral center in Mexico. Older age, use of mass media as main source of COVID-19 information, and belief that vaccines against COVID-19 are safe among patients with cancer were positively associated with a higher likelihood of adequate COVID-19 vaccination status. However, a small proportion of patients remain reluctant and unvaccinated due primarily to fear or potential side effects associated with COVID-19 vaccines. Information regarding the safety of vaccines against COVID-19 provided by attending healthcare professionals, especially by treating oncologists, may help reach a complete COVID-19 vaccination rate in this population.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contribution
All authors were involved in the concept and design, writing, editing, and final approval of this manuscript.
Funding
This research was funded by the Beca Carlos Slim para el Impulso a la Investigacion en Salud 2022 (2022 Carlos Slim Grant for Boosting Health Research).
Data availability
Derived data supporting the findings of this study are available from the corresponding author on request.
Declarations
Ethical approval
Study procedures were reviewed and approved by the Institutional Review Board at INCMNSZ. No identifying data were obtained from participants. All participants were informed about the purpose of the study. The invitation to participate in this study was also included in the heading of the survey, and by accepting such an invitation, consent was implied.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization (WHO) (2020) WHO Director-General’s opening remarks at the briefing on COVID-19. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Accessed 9 Mar 2022
- 2.Delgado-Gallegos JL, Padilla-Rivas GR, Zúñiga-Violante E, et al. Determinants of COVID-19 vaccine hesitancy: a cross-sectional study on a Mexican population using an online questionnaire (COV-AHQ) Front Public Heal. 2021;9:728690. doi: 10.3389/fpubh.2021.728690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johns Hopkins University & Medicine (2022) Mortality analyses - Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/data/mortality. Accessed 9 Mar 2022
- 4.Secretaria de Relaciones Exteriores (2021) Mexico has one of the broadest vaccines portfolios in the world. https://www.gob.mx/sre/prensa/mexico-has-one-of-the-broadest-vaccine-portfolios-in-the-world. Accessed 9 Mar 2022
- 5.Carnalla M, Basto-Abreu A, Stern D, et al. Acceptance, refusal and hesitancy of Covid-19 vaccination in Mexico: Ensanut 2020 Covid-19. Salud Publica Mex. 2021;63:598–606. doi: 10.21149/12696. [DOI] [PubMed] [Google Scholar]
- 6.Yang L, Chai P, Yu J, Fan X. Effects of cancer on patients with COVID-19: a systematic review and meta-analysis of 63,019 participants. Cancer Biol Med. 2021;18:298–307. doi: 10.20892/j.issn.2095-3941.2020.0559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.NCCN Advisory Committee on Covid-19 Vaccination and Pre-exposure Prophylaxis (2022) Recommendations of the National Comprehensive Cancer Network® (NCCN®) Advisory Committee on COVID-19 vaccination and pre-exposure prophylaxis*. https://aonnonline.org/images/resources/navigation_tools/covid-19/vaccines/nccn_2021_covid-19_vaccination_guide_v5_2.pdf. Accessed 9 Mar 2022
- 8.American Society of Clinical Oncology (2022) COVID-19 vaccines & patients with cancer. https://www.asco.org/covid-resources/vaccines-patients-cancer. Accessed 9 Mar 2022
- 9.Castelo-Branco L, Cervantes A, Curigliano G, Garassino MC, Giesen N, Grivas P, Haanen J, Jordan K, Liebert UG, Lordick F, Lucibello F, Melero I, Mir O, Pentheroudakis G, Peters S, Pietsch C, Scotté F, Marie von Lilienfeld-Toal (2021) ESMO statements on vaccination against COVID-19 in people with cancer. European Society for Medical Oncology. https://www.esmo.org/covid-19-and-cancer/covid-19-vaccination. Accessed 9 Mar 2022
- 10.Soto-Perez-de-Celis E, Arrieta O, Bargalló-Rocha E, et al. COVID-19 vaccine guidance for patients with cancer in mexico: report from the working group of the Mexican Society of Oncology. Arch Med Res. 2021;53:223–227. doi: 10.1016/j.arcmed.2021.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prabani KIP, Weerasekara I, Damayanthi HDWT. COVID-19 vaccine acceptance and hesitancy among patients with cancer: a systematic review and meta-analysis. Public Health. 2022;212:66–75. doi: 10.1016/j.puhe.2022.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Villarreal-Garza C, Vaca-Cartagena BF, Becerril-Gaitan A, et al. Attitudes and factors associated with COVID-19 vaccine hesitancy among patients with breast cancer. JAMA Oncol. 2021;7:1242–1244. doi: 10.1001/jamaoncol.2021.1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharma A, Minh Duc NT, Luu Lam Thang T, et al. A consensus-based checklist for reporting of survey studies (CROSS) J Gen Intern Med. 2021;36:3179–3187. doi: 10.1007/s11606-021-06737-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nguyen M, Bain N, Grech L, et al. COVID-19 vaccination rates, intent, and hesitancy in patients with solid organ and blood cancers: a multicenter study. Asia Pac J Clin Oncol. 2022 doi: 10.1111/ajco.13754. [DOI] [PubMed] [Google Scholar]
- 15.Barrière J, Gal J, Hoch B, et al. Acceptance of SARS-CoV-2 vaccination among French patients with cancer: a cross-sectional survey. Ann Oncol. 2021;32:673–674. doi: 10.1016/j.annonc.2021.01.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peng X, Gao P, Wang Q, et al. Prevalence and impact factors of COVID-19 vaccination hesitancy among breast cancer survivors: a multicenter cross-sectional study in China. Front Med. 2021;8:741204. doi: 10.3389/fmed.2021.741204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Sousa MJ, Caramujo C, Júlio N, Magalhães JC, Basto R, Fraga T, Gomes IF, Monteiro AR, Pazos I, Sousa G (2022) Acceptance of SARS-CoV-2 vaccination among cancer patients in Portugal: attitudes and associated factors. Support Care Cancer (5):4565–4570. 10.1007/s00520-022-06886-x [DOI] [PMC free article] [PubMed]
- 18.World Health Organization (2021) Interim recommendations for an extended primary series with an additional vaccine dose for COVID-19 vaccination in immunocompromised persons: interim guidance. World Health Organization. https://apps.who.int/iris/handle/10665/347079. Accessed 9 Mar 2022
- 19.Brigada Correcaminos (2022) Operativo especial para la recuperación de cuberturas de refuerzos y esquemas primarios en adultos conforme a la Política Nacional de Vacunación contra el virus SARS-CoV-2 para la prevención de la COVID-19 en México. https://www.vacunacovid.gob.mx/documentos/operativo-especial-para-la-recuperacion-de-coberturas-de-refuerzos-y-esquemas-primarios-en-adultos-conforme-a-la-politica-nacional-de-vacunacion-contra-el-virus-sars-cov-2-para-la-prevencion-de-la-cov/Ciudad de México. Accessed 22 Dec 2022
- 20.Mongua-Rodríguez N, Rodríguez-Álvarez M, De-la-Rosa-Zamboni D, et al. Knowledge, attitudes, perceptions, and COVID-19 hesitancy in a large public university in Mexico city during the early vaccination rollout. BMC Public Health. 2022;22:1853. doi: 10.1186/s12889-022-14225-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.González-Block MÁ, Gutiérrez-Calderón E, Sarti E (2022) COVID-19 vaccination hesitancy in Mexico City among healthy adults and adults with chronic diseases: a survey of complacency, confidence, and convenience challenges in the transition to endemic control. Vaccines (Basel) 10(11):1944. 10.3390/vaccines10111944 [DOI] [PMC free article] [PubMed]
- 22.Huang J, Chan SC, Ko S, Wang HHX, Yuan J, Xu W, Zheng ZJ, Xue H, Zhang L, Jiang JY, Huang JLW, Chen P, Palaganas E, Viwattanakulvanid P, Somrongthong R, Caicedo A, Medina-Arellano MJ, Murphy JK, Paredes MBA, Withers M, Wong MCS (2022) Association of Pacific Rim Universities (APRU) Global Health Program. Factors associated with vaccination intention against the COVID-19 pandemic: a global population-based study. Vaccines (Basel) 10(9):1539. 10.3390/vaccines10091539 [DOI] [PMC free article] [PubMed]
- 23.Cerić T, Sokolović E, Pašić A, et al. Acceptance, effects, and tolerability in the vaccination process against SARS-CoV-2 among cancer patients in Bosnia and Herzegovina: a single-center cross-sectional study. Bosn J Basic Med Sci. 2022;22:833–842. doi: 10.17305/bjbms.2021.7134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.MatovinaBrko G, Popovic M, Jovic M, et al. COVID-19 vaccines and cancer patients: acceptance, attitudes and safety. J BUON. 2021;26:2183–2190. [PubMed] [Google Scholar]
- 25.Erdem D, Karaman I. Impact of corona-phobia on attitudes and acceptance towards COVID-19 vaccine among cancer patients: a single-center study. Futur Oncol. 2022;18:457–469. doi: 10.2217/fon-2021-1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hathaway CA, Siegel EM, Gonzalez BD, et al. Individual-level factors associated with COVID-19 vaccine acceptance among U.S. patients with cancer. Vaccine. 2022;40:6649–6657. doi: 10.1016/j.vaccine.2022.09.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lazar R, Oprean CM, Badau LM, et al. Attitudes towards COVID-19 vaccination in patients with cancer: a cross-sectional study of 12 oncology centers. Mol Clin Oncol. 2022;17:162. doi: 10.3892/mco.2022.2595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chun JY, Kim SI, Park EY, Park SY, Koh SJ, Cha Y, Yoo HJ, Joung JY, Yoon HM, Eom BW, Park CM, Han JY, Kim M, Lee DW, Kim JW, Keam B, Lee M, Kim TM, Choi YJ, Chang YJ, Lim MC (2021) Cancer patients’ willingness to take COVID-19 Vaccination: a Nationwide Multicenter Survey in Korea. Cancers (Basel) 13(15):3883. 10.3390/cancers13153883 [DOI] [PMC free article] [PubMed]
- 29.Khiari H, Cherif I, M’ghirbi F, et al. COVID-19 vaccination acceptance and its associated factors among cancer patients in Tunisia. Asian Pacific J Cancer Prev. 2021;22:3499–3506. doi: 10.31557/APJCP.2021.22.11.3499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brodziak A, Sigorski D, Osmola M, Wilk M, Gawlik-Urban A, Kiszka J, Machulska-Ciuraj K, Sobczuk P (2021) Attitudes of patients with cancer towards vaccinations-results of online survey with special focus on the vaccination against COVID-19. Vaccines (Basel) 9(5):411. 10.3390/vaccines9050411 [DOI] [PMC free article] [PubMed]
- 31.Mejri N, Berrazega Y, Ouertani E, et al. Understanding COVID-19 vaccine hesitancy and resistance: another challenge in cancer patients. Support Care Cancer. 2022;30:289–293. doi: 10.1007/s00520-021-06419-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bain N, Nguyen M, Grech L, Day D, McCartney A, Webber K, Kwok A, Harris S, Chau H, Chan B, Nott L, Hamad N, Tognela A, Underhill C, Loe BS, Freeman D, Segelov E (2022) On behalf of the canvaccs investigators. COVID-19 vaccine hesitancy in Australian patients with solid organ cancers. Vaccines (Basel) 10(9):1373. 10.3390/vaccines10091373 [DOI] [PMC free article] [PubMed]
- 33.Couderc A-L, Ninove L, Nouguerède E, et al. Acceptance, efficacy, and safety of COVID-19 vaccination in older patients with cancer. J Geriatr Oncol. 2022;13:850–855. doi: 10.1016/j.jgo.2022.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fu L, Wu S, Wang B, et al. COVID-19 vaccination perception and uptake among cancer patients in Guangzhou. China Hum Vaccin Immunother. 2022;18:2102329. doi: 10.1080/21645515.2022.2102329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hong J, Xu X-W, Yang J, et al. Knowledge about, attitude and acceptance towards, and predictors of intention to receive the COVID-19 vaccine among cancer patients in Eastern China: a cross-sectional survey. J Integr Med. 2022;20:34–44. doi: 10.1016/j.joim.2021.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.TadeleAdmasu F. Knowledge and proportion of COVID-19 vaccination and associated factors among cancer patients attending public hospitals of Addis Ababa, Ethiopia, 2021: a multicenter study. Infect Drug Resist. 2021;14:4865–4876. doi: 10.2147/IDR.S340324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marijanović I, Kraljević M, Buhovac T, Sokolović E. Acceptance of COVID-19 vaccination and its associated factors among cancer patients attending the oncology clinic of University Clinical Hospital Mostar, Bosnia and Herzegovina: a cross-sectional study. Med Sci Monit. 2021;27:e932788. doi: 10.12659/MSM.932788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moujaess E, Zeid NB, Samaha R, et al. Perceptions of the COVID-19 vaccine among patients with cancer: a single-institution survey. Futur Oncol. 2021;17:4071–4079. doi: 10.2217/fon-2021-0265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Heyne S, Esser P, Werner A, et al. Attitudes toward a COVID-19 vaccine and vaccination status in cancer patients: a cross-sectional survey. J Cancer Res Clin Oncol. 2022;148:1363–1374. doi: 10.1007/s00432-022-03961-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Derived data supporting the findings of this study are available from the corresponding author on request.