Abstract
To disseminate, educate, and validate psychiatric clinical practice guidelines, the Effectiveness of Guidelines for Dissemination and Education in Psychiatric Treatment (EGUIDE) project was launched in 2016. In this study, we investigated whether the web‐based courses offered by this project would be as effective as the face‐to‐face courses. We analyzed and compared survey answers about overall participant satisfaction with the course and answers regarding clinical knowledge of schizophrenia and major depressive disorder between 170 participants who took the web‐based courses in 2020 and 689 participants who took the face‐to‐face courses from 2016 to 2019. The web‐based course participants completed the survey questions about satisfaction with the web‐based courses. The web‐based courses were conducted using a combination of web services to make it as similar as possible to the face‐to‐face courses. The degree of satisfaction assessed by the general evaluation of the web‐based courses was higher than what was expected from the face‐to‐face courses. The degree of satisfaction was similar for the courses on schizophrenia and major depressive disorder. In addition, there were no significant differences in overall satisfaction and clinical knowledge between web‐based and face‐to‐face courses. In conclusion, the web‐based courses on clinical practice guidelines provided by the EGUIDE project were rated as more satisfying than the face‐to‐face course that the participants expected to take and no differences in the effectiveness of either course. The results suggest that, after the COVID‐19 pandemic, it would be possible to disseminate this educational material more widely by adopting web‐based courses additionally face‐to‐face courses.
Keywords: clinical practice guideline, EGUIDE, evidence‐practice gap, face‐to‐face, web‐based
We examined how the participants evaluated the web‐based courses on clinical practice guidelines provided by the EGUIDE project and how it differed from the face‐to‐face courses that were provided in the past. The web‐based courses were rated as more satisfying than the face‐to‐face course that the participants expected to take and no differences in the effectiveness of either course.
1. INTRODUCTION
It is essential to provide treatment based on the best available evidence for a particular disease in medical practice. Clinical practice guidelines are recommendations for optimizing patient care and are developed based on evaluating the whole body of evidence through systematic reviews and the assessment of benefits and harms. 1 However, clinical practice guidelines are not sufficiently applied in clinical practice. There is a gap between scientific evidence and actual clinical practice, known as the evidence‐practice gap. 2 Multifactorial barriers related to knowledge, attitudes, and external factors have been reported regarding the implementation of guidelines. 3 , 4 It has become clear that the process of evidence dissemination and practice is not passive but requires active strategies to ensure that evidence is effectively understood, adopted, practiced, and maintained. 5 Despite this situation, there are no established methodologies.
In the area of mental health, schizophrenia (SZ) and major depressive disorder (MDD) are major mental disorders, and international treatment guidelines have been published by the American Psychiatric Association 6 and the National Institute for Health and Clinical Excellence. 7 In Japan, the Japanese Society of Mood Disorders published the Treatment Guideline: Major Depressive Disorder in 2012, 8 and the Japanese Society of Neuropsychopharmacology published the Guideline for Pharmacological Therapy for Schizophrenia in 2015. 9 It has been reported that there are evidence‐practice gaps for psychiatric disorders. For example, despite the existence of treatment guidelines, there are significant differences among treatment facilities due to a lack of sufficient practice and because treatment is not standardized. 10 , 11 , 12 , 13 However, no strategy for disseminating and adopting practice guidelines has been established to date. 14
To bridge this evidence‐practice gap, it is necessary to disseminate, educate, and validate psychiatric clinical practice guidelines; thus, the Effectiveness of Guidelines for Dissemination and Education in Psychiatric Treatment (EGUIDE) project was launched in 2016. 10 , 11 , 12 , 15 The EGUIDE project started with the cooperation of 22 hospitals, and as of 2021, more than 240 hospitals (44 universities) are participating in the project, which provides educational courses for psychiatrists on treatment guidelines for SZ and for MDD throughout Japan. The project evaluates and verifies three quality indicators: the level of understanding of the guidelines, the level of their implementation, and the prescribing behavior of each psychiatrist. In psychiatry, there have been few studies that have examined the effects of clinical practice guidelines, but we recently reported a significant improvement in the level of understanding from before to after the course. 15 The courses in the EGUIDE project were conducted face‐to‐face to promote understanding and then the group discussions were used to reinforce that knowledge. However, in 2020, courses were conducted completely through the web to prevent the spread of COVID‐19. Therefore, we adapted the course by combining web services such that the web course could be as understandable as the face‐to‐face course. Although there have been various studies on the effectiveness of learning in online settings, 16 there have been no reports on training with reference to clinical practice guidelines. In face‐to‐face courses, it is considered possible to provide a concentrated course through direct teaching, and it can be conducted without the IT literacy and equipment required for web‐based courses; however, it does require the participants to travel to the course location. On the other hand, although web‐based courses require IT literacy and equipment, they have the advantage that they can be conducted anywhere. However, since the course is conducted via the web, communication may be more difficult than in face‐to‐face courses. Although different courses may have particular characteristics, there have been no studies that compared the level of satisfaction and understanding of the participants, although these two factors are considered to significantly impact the dissemination of courses.
In this study, we examined how the participants evaluated the web‐based courses on clinical practice guidelines provided by the EGUIDE project and how it differed from the face‐to‐face courses that were provided in the past. Note that the questionnaire used in this study to evaluate the web‐based courses was set up for this study and has not been used in previous face‐to‐face courses. And we did not directly compare the web‐based course and the face‐to‐face course.
2. MATERIAL AND METHODS
From October to December 2020, we conducted a total of 18 (ie 9 for each topic) web‐based courses on the Guideline for Pharmacological Therapy for Schizophrenia and Treatment Guideline: Major Depressive Disorder, with a total of 170 participants from 49 medical institutions participating in the web‐based courses. We defined the controls as 689 participants who participated in face‐to‐face courses from 2016 to 2019 (169 participants in 2016, 176 participants in 2017, 185 participants in 2018, and 159 participants in 2019). Written informed consent was obtained from all participants after a complete explanation of the procedures.
In Japan, physicians who graduate from medical school and obtain a medical license first undergo a 2‐year clinical internship to acquire basic primary care skills. After that, they become specialists in a specialized area of psychiatry and spend 3 years or more in training to obtain a specialist license.
The course was conducted by “lecturers” from the EGUIDE project who met the following requirements:
They had completed the EGUIDE project courses.
They were qualified as psychiatrists as defined by the Japanese Society of Psychiatry and Neurology.
They had sufficient knowledge of clinical practice guidelines as well as their implementation.
They had prepared the course materials and facilitated the course at least twice.
Most of the lecturers were psychiatrists with more than 15 years of experience. The lecturer had the role of facilitator of the lectures and group discussions in the courses.
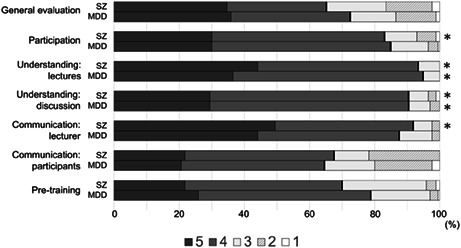
The schedules of the face‐to‐face and web‐based courses are shown in Figure 1. The overall schedule for both face‐to‐face and web‐based courses was as follows. First, the participants and the lecturers introduced themselves to each other, and then the lecturer explained that the purpose of the course involved the clinical practice guidelines. After that, participants took a pretest to assess their knowledge of the guidelines. After the test, the lecturer gave a six‐part lecture of approximately 20 min on the content of the guidelines. In the afternoon after a lunch break, the participants had group discussions on how to use the guidelines through case studies because learning the guidelines alone is not enough to understand how to use them in clinical practice. A lecturer facilitated groups of five to six participants, and the participants were assigned as moderators, minute takers, and presenters. There were two cases (a typical case and a severe case) related to the guidelines for both SZ and MDD, and the participants learned how to apply the guidelines in actual clinical practice. After the discussion, each group presented to all the individuals in the course how their group discussed the issues, which enhances understanding. Afterward, the participants took a posttest to assess their knowledge of the guidelines (this test was the same as the pretest) and answered survey questions to assess their overall satisfaction with the course. Then, the lecturer discussed the answers to the test on knowledge of the guidelines and commented on the EGUIDE project outcomes that had been obtained to date. The course ended with a question‐and‐answer session.
FIGURE 1.
Timetable of the training course. There are two courses, the schizophrenia course and the major depressive disorder course, and both progress back and forth between plenary and individual sessions. The left column shows the plenary sessions for the schizophrenia course, the middle column shows the plenary sessions for the major depressive disorder course, and the right column shows the individual sessions for both courses. MDD, major depressive disorder.
2.1. Devices for web‐based training
We constructed the courses using the following services to ensure that the web‐based courses were conducted in the same format as the face‐to‐face course. The web‐based courses were conducted using Zoom, a web conferencing service, and Google Slides, a free web‐based presentation program provided by Google. To standardize the web environment, both the lecturers and the participants were required to use a PC and to take the course at a location with a stable internet environment. To standardize the skills of the lecturers needed for the web‐based course, we developed a manual for web course facilitation, and the lecturer had to pass at least three pretraining sessions. All participants were required to take and pass the pretraining session on Zoom at least 1 week before the course showing that they could participate in the web‐based course using Zoom and Google Slides.
Just before the course started, we performed a 10‐min presystem check to ensure that there were no problems with the use of Zoom. A short survey using the polling feature in Zoom was conducted to ensure that the participants were listening during the lectures. Group discussions during the courses were conducted by dividing the entire class into small groups using Zoom breakout rooms. We expected that interactive discussions would be difficult in a web‐based course; the lecturer acted as a moderator to ensure smooth communication. In addition, Google Slides, which allows online collaborative editing, was used to record the discussions as they proceeded. The level of understanding and satisfaction with the courses were assessed by web questionnaires using Google Forms, and a questionnaire on the level of satisfaction with the web‐based nature of the course was also completed by those in the web‐based courses. Links to the Google Slides and the web questionnaires using Google Forms were sent to the participants using the chat function in Zoom.
2.2. Evaluation
All evaluations were conducted using self‐administered questionnaires. After the face‐to‐face courses in 2016–2019 had been completed, we conducted a survey with questions about the subjective assessments of the participants in the guideline programs to measure the degree of satisfaction with the courses themselves (Table S1). 17 The questions were as follows: How was the content of this course? Would you recommend this course to your colleagues or juniors? Did this course improve your knowledge about the treatment of schizophrenia/major depressive disorder? Did this course improve your skills in treating schizophrenia/major depressive disorder? How confident are you in your ability to properly treat schizophrenia/major depressive disorder? Will you follow the guidelines in treatment for schizophrenia/major depressive disorder?
For those in the web‐based courses conducted in 2020, in addition to the original survey, we also conducted a survey with questions about the satisfaction of the participants with the web‐based nature of the course to measure the degree of satisfaction with the web‐based courses compared to their expectations of a face‐to‐face course (Table S2). The questions were as follows: Which would you prefer to participate in, a web‐based course or a general face‐to‐face course? How was the web‐based course easy to participate? How do you understand the morning lectures on the guideline in the web‐based course? How do you understand the afternoon discussion of a clinical case in the web‐based course? How was the communication with the lecturer in the web‐based course? How was the communication with other participants in the web‐based course? How useful was the pre‐training session in preparation for the web‐based course?
A survey with questions regarding knowledge of SZ and MDD was completed before and after the course to determine the level of understanding of the guidelines in individuals taking web‐based and face‐to‐face courses (Table S3). The content validity of all questionnaires was assessed by all project members.
The six items on the “Survey questions about the subjective assessment of participants in the guideline programs” were rated on a 5‐point Likert scale (higher scores on a scale indicated greater satisfaction for that item). We compared the scores for each question between the web‐based courses and each year of the face‐to‐face courses.
The seven items on the “Survey questions about the satisfaction of participants with the web‐based course” were rated on a 5‐point Likert scale (higher scores on a scale indicated greater satisfaction for that item). The statistical analysis categorized the data into two groups: Likert scores 4 and 5 (favorable to the web‐based course) and 1–3 (less favorable to the web‐based course). The distributions into these two groups were compared between the SZ course and MDD course for each individual question and between “general evaluation” and the six other questions (“participation,” “understanding: lectures,” “understanding: discussion,” “communication: lecturer,” “communication: participants,” and “pretraining”) in the same course.
The “Questions regarding knowledge of SZ and MDD” were self‐administered questionnaires consisting of 37 items (a total of 37 points) for both the SZ course and MDD course. The baseline and postcourse scores, the change from baseline to postcourse scores, and the percentage of correct answers for each question were compared for each year of the web‐based and face‐to‐face courses.
Statistical analysis was performed using IBM SPSS Statistics (Version 27). Fisher's exact tests were used to compare the sex of the participants between web‐based courses and face‐to‐face courses and the distribution of answers on the “Survey questions about the satisfaction of participants with the web‐based course.” The age, experience as a physician, and experience as a psychiatrist of the participants, the scores and changes in scores for the “Questions regarding knowledge of SZ and MDD,” and the points on the “Survey questions about the subjective assessment of participants in the guideline programs” were statistically compared using Mann–Whitney U tests to compare the web‐based course with the face‐to‐face course. In cases with multiple comparisons, the Bonferroni method was applied to correct for multiple comparisons.
This study was approved by the Research Ethics Review Committee of the National Center of Neurology and Psychiatry and each participating facility.
3. RESULTS
The demographic characteristics of the participants are shown in Table 1. The distribution of participants by age and years of psychiatric experience is shown in Figure S1. The participants in the web‐based courses were significantly younger and had less experience as physicians and psychiatrists than the participants in the face‐to‐face courses. This may be because, in the first year of the course, some participants were older and had more years of experience, but in the second and subsequent years, the participants were mainly composed of newcomers at the same facilities.
TABLE 1.
Demographic characteristics of the course participants
| Web‐based | Face‐to‐face | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2020 (n = 170) | 2016 (n = 169) | 2017 (n = 176) | 2018 (n = 185) | 2019 (n = 159) | ||||||||||
| Mean | SD | Mean | SD | p‐value | Mean | SD | p‐value | Mean | SD | p‐value | Mean | SD | p‐value | |
| Age | 32.2 | 7.3 | 33.8 | 6.7 | 5.2 × 10 −5 | 33.7 | 7.1 | 1.3 × 10 −3 | 33.9 | 8.0 | 1.2 × 10−2 | 32.6 | 6.4 | 3.5 × 10−2 |
| Sex (male/female) | 111/59 | 118/51 | 0.42 | 139/37 | 3.6 × 10−2 | 124/61 | 0.74 | 119/40 | 7.1 × 10−2 | |||||
| Experience as a physician (years) | 5.5 | 5.8 | 7.5 | 5.7 | 5.1 × 10 −15 | 7.7 | 6.4 | 2.7 × 10 −7 | 7.5 | 7.1 | 2.3 × 10 −4 | 5.6 | 5.1 | 5.1 × 10−2 |
| Experience as a psychiatrist (years) | 3.0 | 5.4 | 4.9 | 5.5 | 2.2 × 10 −18 | 5.3 | 6.6 | 1.2 × 10 −8 | 5.2 | 7.1 | 1.2 × 10 −5 | 3.1 | 4.8 | 3.6 × 10−2 |
Note: The mean and SD of the participant's age, experience as a physician (years), experience as a psychiatrist (years), and the number of participants by sex for courses in each year are shown. We compared the differences in age, experience as a physician (years), and experience as a psychiatrist (years) between the web‐based courses (2020) and the face‐to‐face courses for each year (2016–2019) using Mann–Whitney U tests. We also compared the difference in the distribution of sex between the web‐based courses (2020) and the face‐to‐face courses in each year (2016–2019) using Fisher's exact tests. Since there were multiple comparisons, the Bonferroni method was applied for correction, with two‐sided p < 3.1 × 10−3. Significant p‐values are shown in bold and underlined.
Abbreviations SD, standard deviation.
Table 2, Tables S4 and S5 show the subjective assessment of participants and understanding of the guidelines for the face‐to‐face and web‐based training courses. After correcting for multiple comparisons, none of the results were significant, with the exception of satisfaction with the recommendations among the SZ course participants in 2017 (Table 2; web‐based course: 4.2 ± 0.7 SD vs. face‐to‐face course: 4.5 ± 0.5 SD, p = 6.5 × 10−5).
TABLE 2.
Scores for the survey questions regarding the subjective assessment of participants in the guideline programs
| Web‐based | Face‐to‐face | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2020 (n = 170) | 2016 (n = 169) | 2017 (n = 176) | 2018 (n = 185) | 2019 (n = 159) | ||||||||||
| Mean | SD | Mean | SD | p‐value | Mean | SD | p‐value | Mean | SD | p‐value | Mean | SD | p‐value | |
| Schizo‐phrenia | ||||||||||||||
| Contents | 4.4 | 0.6 | 4.5 | 0.5 | 2.5 × 10−2 | 4.5 | 0.5 | 2.7 × 10−2 | 4.5 | 0.5 | 2.4 × 10−2 | 4.4 | 0.5 | 0.49 |
| Recommend | 4.2 | 0.7 | 4.4 | 0.6 | 1.0 × 10−2 | 4.5 | 0.5 | 6.5 × 10 −5 | 4.4 | 0.6 | 3.0 × 10−3 | 4.3 | 0.6 | 5.3 × 10−2 |
| Knowledge | 4.3 | 0.5 | 4.2 | 0.5 | 0.16 | 4.3 | 0.5 | 0.90 | 4.4 | 0.5 | 0.25 | 4.3 | 0.5 | 0.82 |
| Skills | 4.2 | 0.6 | 4.1 | 0.5 | 0.16 | 4.2 | 0.5 | 0.56 | 4.2 | 0.5 | 0.97 | 4.1 | 0.5 | 0.23 |
| Confident | 3.3 | 0.7 | 3.5 | 0.6 | 0.10 | 3.3 | 0.7 | 0.45 | 3.4 | 0.7 | 0.31 | 3.3 | 0.7 | 0.96 |
| Follow | 4.3 | 0.5 | 4.1 | 0.4 | 2.5 × 10−4 | 4.2 | 0.4 | 3.5 × 10−2 | 4.1 | 0.4 | 1.5 × 10−2 | 4.1 | 0.5 | 3.5 × 10−3 |
| Major depressive disorder | ||||||||||||||
| Contents | 4.4 | 0.6 | 4.4 | 0.6 | 0.95 | 4.4 | 0.5 | 0.69 | 4.5 | 0.5 | 0.10 | 4.5 | 0.6 | 0.11 |
| Recommend | 4.2 | 0.6 | 4.3 | 0.6 | 0.78 | 4.4 | 0.5 | 0.059 | 4.4 | 0.6 | 2.1 × 10−2 | 4.3 | 0.6 | 8.4 × 10−2 |
| Knowledge | 4.4 | 0.5 | 4.3 | 0.5 | 7.5 × 10−3 | 4.4 | 0.5 | 0.33 | 4.4 | 0.6 | 0.74 | 4.4 | 0.5 | 0.65 |
| Skills | 4.2 | 0.6 | 4.1 | 0.6 | 1.3 × 10−2 | 4.1 | 0.5 | 0.10 | 4.2 | 0.6 | 0.92 | 4.2 | 0.6 | 0.58 |
| Confident | 3.4 | 0.6 | 3.4 | 0.7 | 0.28 | 3.4 | 0.6 | 0.88 | 3.5 | 0.6 | 9.0 × 10−2 | 3.5 | 0.7 | 0.21 |
| Follow | 4.3 | 0.5 | 4.2 | 0.4 | 1.9 × 10−2 | 4.2 | 0.5 | 2.2 × 10−2 | 4.2 | 0.4 | 2.7 × 10−2 | 4.2 | 0.5 | 6.1 × 10−2 |
Note: The scores on the six‐item satisfaction questionnaire are shown for the schizophrenia and major depressive disorder courses. Each question is shown in Table S1. Each question was rated on a scale ranging from 1 to 5, with higher values indicating better evaluation. For each question, Mann–Whitney U test was used to compare the scores between the web‐based courses (2020) and the face‐to‐face courses (2016–2019). Because of multiple comparisons, the Bonferroni method was applied for correction, with two‐sided p < 1.36 × 10−4. Significant p‐values are shown in bold and underlined.
Abbreviation: SD, standard deviation.
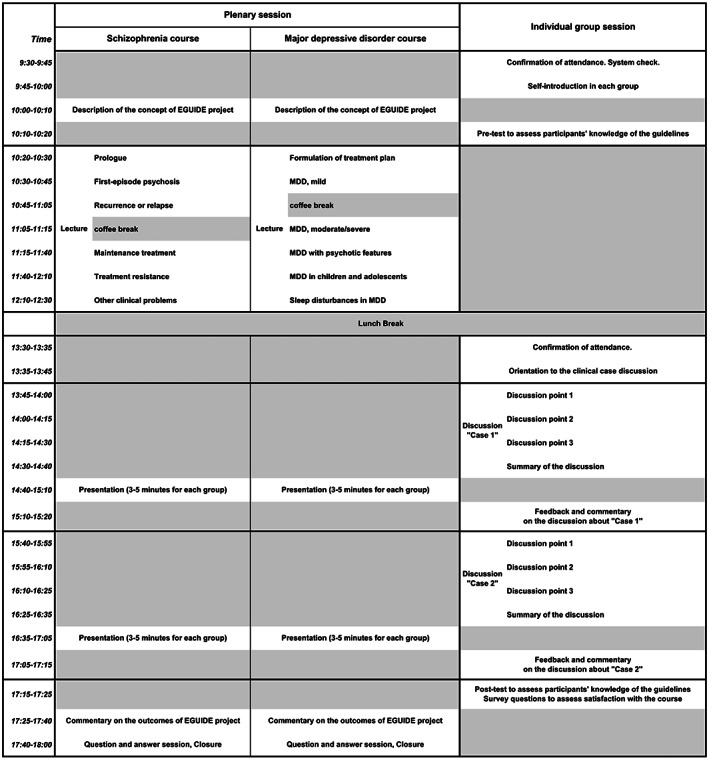
Figure 2 shows the results of the “Survey questions about the satisfaction of participants with the web‐based course.” For the SZ course, regarding the “general evaluation,” 65.3% of the participants preferred the web‐based course (5 and 4), 18.2% preferred neither (3), and 16.5% preferred the face‐to‐face course (2 and 1). More than 80% of the participants preferred the web‐based course based on questions regarding “participation,” “understanding: lectures,” “understanding: discussion,” and “communication: lecturer.” On the other hand, 67.6% of the participants preferred the web‐based course for “communication: participants,” and 70.0% of the participants preferred the web‐based training for “pretraining.” In the statistical comparisons, the percentages of participants who preferred the web‐based course were significantly higher for “participation,” “understanding: lectures,” “understanding: discussions,” and “communication: lecturer” than for “general evaluation.”
FIGURE 2.
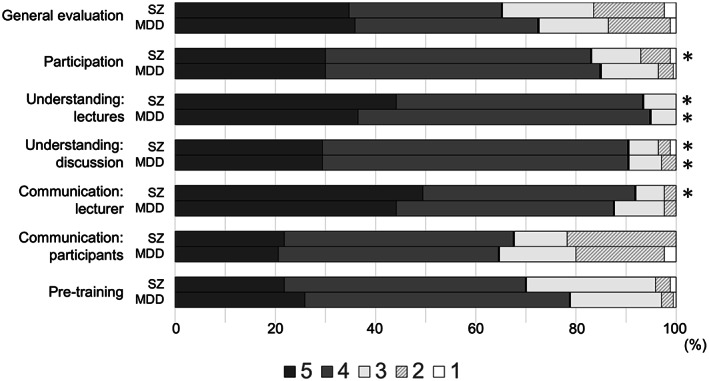
Percentage of responses to survey questions about the satisfaction of the participants with the web‐based courses. The figure shows the percentage of respondents for each survey question regarding satisfaction with the web‐based courses. The questionnaire contained seven questions answered by the same 170 participants in both the schizophrenia and major depressive disorder courses. Each question is shown in Table S3. Each question was rated on a scale ranging from 1 to 5 for all questions, with higher values indicating better evaluation or preference for the web‐based course over the face‐to‐face course. The five levels were categorized into two groups of scores, namely, 1–3 and 4–5, and analyzed with Fisher's exact test. The statistical comparisons were between the percentage of responses to the “general evaluation” and the percentage of responses to other questions in the same course and between the percentage of responses to the same questions in the schizophrenia and major depressive disorder courses. Since there were multiple comparisons, the Bonferroni method was applied for correction, with two‐sided p < 1.02 × 10−3. Statistically significant differences in the percentage of responses to a particular question compared to the percentage of responses to “general evaluation” in the same course are indicated by *. In the schizophrenia course, there were more favorable responses to the web‐based course in “participation,” “understanding: lectures,” “understanding: discussion,” and “communication: lecturer” to “general evaluation.” In the major depressive disorder course, there were more favorable responses to the web‐based course in “understanding: lectures,” “understanding: discussion,” and “general evaluation.” There were no significant differences between the percentage of responses for the same question across the schizophrenia course and the major depressive disorder course.
For the MDD course, regarding the “general evaluation,” 72.4% of the participants preferred the web‐based course, 14.1% preferred neither, and 13.5% preferred the face‐to‐face course. More than 80% of the participants preferred the web‐based course for “participation,” “understanding: lectures,” “understanding: discussion,” and “communication: lecturer.” On the other hand, 64.7% of the participants preferred the web‐based course for “communication: participants” and 78.8% of the participants preferred the web‐based training for “pretraining.” In the statistical comparisons, the percentages of participants who preferred the web‐based course were significantly higher for “understanding: lectures” and “understanding: discussions” than for “general evaluation.”
There were no significant differences between the percentages of the two groups between the SZ and MDD courses.
4. DISCUSSION
In this study, we assessed whether there was a difference in participant satisfaction in a fully web‐based course designed to enhance the dissemination, education, and validation of psychiatric clinical practice guidelines compared to what was expected from a face‐to‐face course. To the best of our knowledge, this is the first study of web‐based courses focused on clinical practice guidelines. The degree of satisfaction based on the overall evaluation was higher with the web‐based courses than with the face‐to‐face courses. In addition, compared to the overall evaluation, the items for ease of participation, understanding of lectures and group discussions, and communication with the lecturers had a higher percentage of participants who preferred the web‐based course. The secondary analysis showed no difference in the level of understanding of the clinical practice guidelines between the web‐based courses and the previous face‐to‐face courses.
A systematic review comparing online and offline learning in medical education showed that online learning was significantly better than offline learning in comprehension. 18 However, most of the studies included in this review found that online learning did not provide the same content as offline learning; rather, the content was modified for online presentation and evaluated as knowledge was gained. The present study used a new approach by adapting the web courses to be as similar as possible to the face‐to‐face courses using web tools. Furthermore, this study was not intended for medical students but for psychiatrists who are already engaged in clinical practice. The average working hours of physicians are long, but they must spend time within those working hours to learn and continue their lifelong education. As shown in this study, it would be very beneficial to provide a 1‐day course that improved the understanding of the content related to clinical practice guidelines. Compared to face‐to‐face courses, web‐based courses have been reported to reduce participants' motivation to learn due to a weaker learning process, lack of familiarity with the educational media, and dependence on the internet environment. 16 Since we have been conducting face‐to‐face courses, we have been using case discussions and lectures to improve our level of understanding. It has been challenging to reproduce these discussions from face‐to‐face courses in the web‐based courses, but we believe it is now possible using various web services.
Participant satisfaction with communication with other participants was lower than in the other categories. It has been reported that online learning results in difficulty achieving interactive communication between instructors and participants and between participants, which can be done in offline learning. 16 In this study, we prepared a manual for the lecturers in the web course to help them communicate well with the participants, and it was required for the lecturers to practice several times in advance. As a result, the communication between the lecturers and the participants was satisfactory. However, as we expected, communication between participants in the web course was difficult. In a face‐to‐face course, there is a possibility of building a network by exchanging information through direct communication between participants. However, building such a network in web‐based courses is thought to be challenging, and this is an essential issue to address in the future.
If a course on clinical practice guidelines can be conducted online, it will be easier for doctors who cannot participate in the course due to distance to participate. Another advantage is that it does not put pressure on clinical practice time because it does not involve the need to travel. Regarding the degree of overall satisfaction with the courses, there was a significant difference between the 2017 face‐to‐face course and the current web‐based course in terms of the course being “recommended,” but there were no differences in the other years, and the results were not consistent. The degree of overall satisfaction with the course was high for the previous face‐to‐face courses, and it was also high for the current web‐based courses. If there is no difference in the degree of overall satisfaction between the courses, then the web‐based course may have the added benefit of simply being a web‐based course. However, the bottleneck is that IT literacy, equipment, and other conditions need to be in place to make the web‐based course feasible.
Limitations of this study include the results of this study are based on only subjective satisfaction with the web‐based courses and did not directly compare the web‐based course and the face‐to‐face course. If we compared them directly, it is possible that the information in the face‐to‐face course was easier to understand than the web‐based course or that communication among the participants was more accessible. In addition, we did not examine the effectiveness of the course in terms of long‐term changes. We should consider making such comparisons in the future when the COVID‐19 situation has been resolved, and face‐to‐face courses can be conducted without problems.
5. CONCLUSION
We found that the degree of satisfaction with web‐based courses was higher than what the participants expected from the face‐to‐face course. In addition, the web‐based courses were as effective as the face‐to‐face courses, suggesting that web‐based courses can also improve clinical knowledge of clinical practice guidelines. After the COVID‐19 pandemic, it is possible that we can contribute to reducing the evidence‐practice gap by disseminating education regarding these guidelines more widely through the choice of a face‐to‐face or web‐based course depending on the individual's preference.
AUTHOR CONTRIBUTIONS
HI and TOka were involved in data collection and data analysis and wrote the first draft of the manuscript. KN, NHase, SN, and KOga were involved in the data analysis and contributed to the interpretation of the data and writing the manuscript. KM, JM, HH, JI, KIchi, NHashi, HY, KOhi, NYF, KF, TT, MU, RF, YT, AH, HM, EK, TN, SO, HKoma, SK, MT, TOni, ST, CK, and HKawa contributed to the interpretation of the data and data collection. KIna and KW were involved in the study design and contributed to the interpretation of the data. RH supervised the entire project, collected the data, and was involved in the design, analysis, and interpretation of the data. All authors contributed to revising the manuscript critically for important intellectual content and gave final approval of the version to be published and had an agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
FUNDING INFORMATION
This study was supported by the Japan Agency for Medical Research and Development (AMED) under grant numbers JP18dk0307060, JP19dk0307083, and JP20dk0307081, Health and Labor Sciences Research Grants (H29‐Seishin‐Ippan‐001 and 19GC1201), the Japanese Society of Neuropsychopharmacology, and the Japanese Society of Mood Disorders. The funders had no role in the study design, data collection, analysis, decision to publish, or manuscript preparation.
CONFLICT OF INTEREST
The author(s) reports no conflicts of interest in this work.
APPROVAL OF THE RESEARCH PROTOCOL BY AN INSTITUTIONAL REVIEW BOARD
This study was approved by the ethics committees of the National Center of Neurology and Psychiatry (A2017‐105) and each participating university, hospital, and clinic.
INFORMED CONSENT
All participants provided their written informed consent. The public availability of raw data was not planned in the research protocol that was approved by an Institutional Review Board. We did not obtain informed consent for public availability.
REGISTRY AND THE REGISTRATION NO. OF THE STUDY/TRIAL
Trial registration: The Effectiveness of Guidelines for Dissemination and Education in Psychiatric Treatment, UMIN000022645, Registered June 15, 2016, https://center6.umin.ac.jp/cgi‐open‐bin/ctr_e/ctr_view.cgi?recptno=R000026044
ANIMAL STUDIES
Not available.
Supporting information
Tables S1‐S5
Figure S1
ACKNOWLEDGMENTS
We appreciate the cooperation of all the individuals who participated in this study.
Iida H, Okada T, Nemoto K, Hasegawa N, Numata S, Ogasawara K, et al. Satisfaction with web‐based courses on clinical practice guidelines for psychiatrists: Findings from the “Effectiveness of Guidelines for Dissemination and Education in Psychiatric Treatment (EGUIDE)” project. Neuropsychopharmacol Rep. 2023;43:23–32. 10.1002/npr2.12300
DATA AVAILABILITY STATEMENT
The data are not publicly available due to privacy and ethical restrictions (ie, we did not obtain informed consent on the public availability of raw data).
REFERENCES
- 1. Institute of Medicine (US) Committee on Standards for Developing Trustworthy Clinical Practice Guidelines . In: Graham R, Mancher M, Miller Wolman D, Greenfield S, Steinberg E, editors. Clinical practice guidelines we can trust. Washington, DC: National Academies Press (US); 2011. [PubMed] [Google Scholar]
- 2. Elliott JH, Turner T, Clavisi O, Thomas J, Higgins JPT, Mavergames C, et al. Living systematic reviews: an emerging opportunity to narrow the evidence‐practice gap. PLoS Med. 2014;11(2):e1001603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–65. [DOI] [PubMed] [Google Scholar]
- 4. Fischer F, Lange K, Klose K, Greiner W, Kraemer A. Barriers and strategies in guideline implementation‐a scoping review. Healthcare. 2016;4(3):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Proctor EK. Leverage points for the implementation of evidence‐based practice. Brief Treat Crisis Interv. 2004;4(3):227–42. [Google Scholar]
- 6. American Psychiatry Association . Practice guideline for the treatment of patients with major depressive disorder. 3rd ed. Arlington, VA: American Psychiatric Association; 2010. [Google Scholar]
- 7. National Institute for Health and Clinical Excellence (NICE) . The treatment and management of depression in adults (updated edition)‐National Clinical Practice Guideline. Leicestar, UK: British Psychological Society; 2010. [PubMed] [Google Scholar]
- 8. Japanese Sociaty of Mood Disorders . Treatment Guideline: Major Depressive Disorder. Tokyo: Igakusyoin; 2012. (in Japanese). [PubMed] [Google Scholar]
- 9. Japanese Society of Neuropsychopharmacology . Guideline for pharmacological therapy of schizophrenia. Neuropsychopharmacol Rep. 2021;41(3):266–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ichihashi K, Hori H, Hasegawa N, Yasuda Y, Yamamoto T, Tsuboi T, et al. Prescription patterns in patients with schizophrenia in Japan: first‐quality indicator data from the survey of “effectiveness of guidelines for dissemination and education in psychiatric treatment (EGUIDE)” project. Neuropsychopharmacol Rep. 2020;40(3):281–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Iida H, Iga J, Hasegawa N, Yasuda Y, Yamamoto T, Miura K, et al. Unmet needs of patients with major depressive disorder ‐ findings from the ‘Effectiveness of guidelines for dissemination and education in psychiatric treatment (EGUIDE)’ project: a nationwide dissemination, education, and evaluation study. Psychiatry Clin Neurosci. 2020;74(12):667–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hashimoto N, Yasui‐Furukori N, Hasegawa N, Ishikawa S, Numata S, Hori H, et al. Characteristics of discharge prescriptions for patients with schizophrenia or major depressive disorder: real‐world evidence from the effectiveness of guidelines for dissemination and education (EGUIDE) psychiatric treatment project. Asian J Psychiatr. 2021;63:102744. [DOI] [PubMed] [Google Scholar]
- 13. Park SC, Jang EY, Xiang YT, Kanba S, Kato TA, Chong MY, et al. Network analysis of the depressive symptom profiles in Asian patients with depressive disorders: findings from the research on Asian psychotropic prescription patterns for antidepressants (REAP‐AD). Psychiatry Clin Neurosci. 2020;74(6):344–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bighelli I, Ostuzzi G, Girlanda F, Cipriani A, Becker T, Koesters M, et al. Implementation of treatment guidelines for specialist mental health care. Cochrane Database Syst Rev. 2016;12(12):CD009780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Takaesu Y, Watanabe K, Numata S, Iwata M, Kudo N, Oishi S, et al. Improvement of psychiatrists' clinical knowledge of the treatment guidelines for schizophrenia and major depressive disorders using the ‘Effectiveness of guidelines for dissemination and education in psychiatric treatment (EGUIDE)’ project: a nationwide dissemination, education, and evaluation study. Psychiatry Clin Neurosci. 2019;73(10):642–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Paul J, Jefferson F. A comparative analysis of student performance in an online vs. face‐to‐face environmental science course from 2009 to 2016. Front Comput Sci. 2019;1(7):1–9. 10.3389/fcomp.2019.00007 [DOI] [Google Scholar]
- 17. Ogasawara K, Numata S, Hasegawa N, Makinodan M, Ohi K, Takeshima M, et al. The subjective assessment of participants in education programs on clinical practice guidelines in the field of psychiatry. Neuropsychopharmacol Rep. 2022;42(2):221–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pei L, Wu H. Does online learning work better than offline learning in undergraduate medical education? A systematic review and meta‐analysis. Med Educ Online. 2019;24(1):1666538. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1‐S5
Figure S1
Data Availability Statement
The data are not publicly available due to privacy and ethical restrictions (ie, we did not obtain informed consent on the public availability of raw data).


