Abstract
Objectives:
The COVID-19 Healthcare Personnel Study is a longitudinal survey to assess the changing impact of the COVID-19 pandemic on the New York State health care workforce. We analyzed results from a follow-up survey of physicians, nurse practitioners, and physician assistants on the availability of equipment and personnel, work conditions, physical and mental health of participants, and impact of the pandemic on commitment to their profession.
Methods:
We conducted an online survey of all licensed New York State physicians, nurse practitioners, and physician assistants in April 2020 (N = 2105) and a follow-up survey in February 2021 (N = 978). We analyzed changes in item responses from baseline to follow-up. We calculated survey-adjusted paired t tests and odds ratios (ORs) using survey-adjusted generalized linear models controlling for age, sex, region of practice, and hospital versus non–hospital-based practice.
Results:
Twenty percent of respondents expressed continuing concern about personnel shortages at both baseline and follow-up. Respondents reported working approximately 5 more hours on average during a 2-week period at follow-up compared with baseline (78.1 vs 72.6 hours; P = .008). For 20.4% (95% CI, 17.2%-23.5%) of respondents, mental health issues had become persistent. More than one-third (35.6%; 95% CI, 31.9%-39.4%) of respondents reported that they thought about leaving their profession more often than once per month. The association between persistent mental and behavioral health issues and contemplating leaving one’s profession was significant (OR = 2.7; 95% CI, 1.8-4.1; P < .001).
Conclusions:
Interventions such as decreasing the number of hours worked, ensuring health care professionals do not work directly with patients while ill, and addressing shortages of personal protective equipment can help address concerns of the health care workforce.
Keywords: COVID-19, health professions, survey, mental health and well-being, workforce
More than 2 years into the COVID-19 pandemic, health care workers continue to struggle to meet the demands placed on care systems and hospitals across the globe. The COVID-19 pandemic has been associated with high levels of anxiety, 1 feelings of isolation, 2 and concerns about family members among health care providers, 3 and health care workers treating patients with COVID-19 were “experiencing symptoms of depression, anxiety, insomnia, and distress.” 4 Many of these early studies were restricted to a single specialty or institution5,6 and used cross-sectional data.5,6
Among more recent longitudinal assessments, a single-institution survey found little or no decrease in levels of anxiety and worry in a follow-up study of 77 physicians 1 year into the pandemic. 7 Another, albeit shorter-term, single-institution longitudinal survey of 51 physicians reported evidence of resilience associated with medical specialty board certification, with more senior attending physicians than junior resident physicians demonstrating decreased perceived stress 4 weeks after a baseline survey in spring 2020. 8 This evidence of resiliency is consistent with a report that physicians with a previous exposure to similar traumatic events were 75% less likely than those who did not experience such events to experience fear during the COVID-19 pandemic. 2
Prepandemic estimates of some level of burnout have been reported in up to half of all US physicians 9 and may be exacerbated by the COVID-19 pandemic. In a 2021 national survey of physicians, 22% “were considering leaving their current jobs to pursue a nonclinical career.” 10 Most of these physicians “planned to make the change within 3 years.” 11
Results from a baseline survey of New York State physicians administered in April 2020 found significantly higher levels of hopelessness among physicians aged ≥50 years compared with younger physicians. 12 Most physicians, nurse practitioners, and physician assistants (57.6%; 95% CI, 55.2%-60.0%) reported a negative impact on their overall mental health. Negative mental health was associated with having become ill with COVID-19 (odds ratio [OR] = 1.7; 95% CI, 1.3-2.1) and redeployment to unfamiliar functions (OR = 1.3; 95% CI, 1.1-1.6).13,14
In the current study, we present and analyze results from a follow-up survey of physicians, nurse practitioners, and physician assistants who agreed to be part of a longitudinal survey administered in early 2021. We report on the availability of equipment and personnel, work conditions, physical and mental health of participants, and impact of the pandemic on commitment to their profession.
Methods
In early 2020, at the height of the COVID-19 pandemic in New York State, the COVID-19 Healthcare Personnel Study (CHPS) was launched to assess and help mitigate the adverse health impact of the COVID-19 pandemic on the health care workforce in New York State. 13 CHPS collaborators recruited members of multiple health care professions across the state to participate in a longitudinal cohort. Professions included physicians, nurses and nurse practitioners, medical residents, physician assistants, and other health professionals such as respiratory therapists, visiting nurses, home health care workers, and others. Participants were drawn from community-based settings, hospitals, and other institutional settings. The protocol was approved by the institutional review boards of Columbia University Medical Center, the New York State Psychiatric Institute, the City University of New York, New York University, and New York University School of Medicine.
The CHPS collaborative group conducted a survey in April 2020 and a follow-up survey in February 2021. The sampling frame of physicians, nurse practitioners, and physician assistants consisted of 103 103 physicians, 21 503 nurse practitioners, and 14 503 physician assistants, representing all licensed providers among those professions licensed to practice in New York State. We obtained email addresses from the New York State Department of Education, the professional licensing arm of New York State. In April 2020, an invitation to participate in the survey was sent from the office of the New York State Commissioner of Health. Of the 139 109 emails sent, 38 090 (27.4%) reached an intended recipient and were opened. Of these, 2105 physicians, nurse practitioners, and physician assistants completed the survey, for a response rate of 5.5%. In the baseline survey, we asked participants whether they would consent to be part of a longitudinal follow-up survey. Of the original 2105 physicians, nurse practitioners, and physician assistants at baseline, 1569 (74.5%) respondents consented to enter into the longitudinal survey. Of these, 978 (62.3%) submitted follow-up responses in 2021. We limited the results of the current study to the 978 physicians, nurse practitioners, and physician assistants who responded to both surveys.
The survey was administered by the Data Coordinating Center at the New York State Psychiatric Institute through REDCap version 12.4.0, a secure web application for building and managing online surveys and databases. We downloaded and read raw data using R version 4.2.1 (R Foundation for Statistical Computing), checked for outliers, and cleaned the data. We applied poststratification raking using the postStratify procedure in the R survey package version 4.2.1 (R Foundation for Statistical Computing) to assign survey weights for each respondent to represent a target population of physicians, nurse practitioners, and physician assistants based on age, sex, and geographic location across the 10 regions of New York State.15-18
Results were based on responses to questions about 5 mental and behavioral health conditions (nervousness/anxiety, worrying thoughts, feeling down or hopeless, lack of pleasure in previously enjoyable activities, and sleep disturbances), thoughts of leaving the medical profession, and 11 chronic medical conditions (heart disease, diabetes, chronic pulmonary disease, high blood pressure, active cancer in the past 5 years, chronic kidney disease, immune compromised condition, severe asthma, history of stroke, chronic liver disease, and depression).
Statistical analyses consisted of survey-adjusted weighted counts, proportions, and means with the range of uncertainty for point estimates in the survey data presented as 95% CIs using the R survey package. We calculated P values and 95% CIs for changes in item responses from the baseline survey to the follow-up survey using survey-adjusted paired t tests for dichotomous comparisons and the Pearson χ2 test for >2 categories. We calculated ORs for association using survey-adjusted generalized linear models controlling for baseline characteristics of age, sex, New York State region of practice, and hospital versus non–hospital-based practice. We considered P < .05 to be significant. The questionnaire is available on request from the CHPS Steering Committee.
Results
The sample of 978 longitudinal baseline and follow-up survey responses represented a weighted estimate of 48 486 (95% CI, 46 256-50 717) physicians, nurse practitioners, and physician assistants licensed in New York State, with a mean age of 50.6 (95% CI, 49.6-51.6) years, of whom 61.5% (95% CI, 57.7%-65.3%) were female. (Results of the unweighted analyses are available in the first section of the Supplemental Material and in eTable 1. A table of frequencies and weighted responses is available in eTable 2 of the Supplemental Material.)
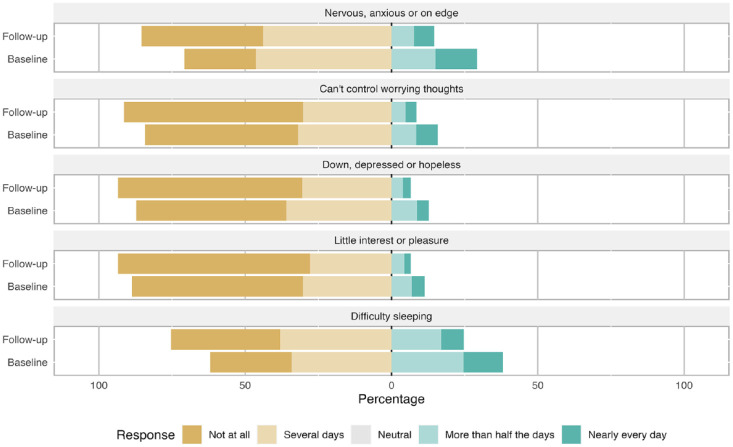
At baseline, 48.8% (95% CI, 44.9%-52.7%) of respondents reported at least 1 of 5 mental or behavioral health problems on half or more days during the previous 2 weeks. At follow-up, this proportion had declined significantly to 26.7% (95% CI, 23.2%-30.1%; P < .001). We found significant declines in the proportion of respondents with such mental or behavioral health issues across all domains from baseline to follow-up (Table 1, Figure 1).
Table 1.
Percentage of physicians, nurse practitioners, and physician assistants reporting half or more days of mental or behavioral health issues during the previous 2 weeks, New York State COVID-19 Healthcare Personnel Study a
| Condition | Baseline survey | Follow-up survey |
|---|---|---|
| Nervousness/anxious | 29.2 (25.7-32.8) | 14.6 (11.8-32.8) |
| Worrying thoughts | 15.8 (12.9-18.6) | 8.6 (6.3-18.6) |
| Feeling down or hopeless | 12.7 (10.0-15.5) | 6.6 (4.7-15.5) |
| Lack of pleasure in previously enjoyable activities | 11.3 (8.7-13.9) | 6.6 (4.8-13.9) |
| Sleep disturbances | 38.1 (34.2-41.9) | 17.5 (14.6-41.9) |
All values are percentage (95% CI). Participants (978 weighted responses) were surveyed at baseline (April 2020) and at follow-up (February 2021). The difference between baseline and follow-up for each condition was significant at P < .001, determined by survey-adjusted matched t test.
Figure 1.
Mental and behavioral health issues of physicians, nurse practitioners, and physician assistants at baseline (April 2020) and follow-up (February 2021) surveys, COVID-19 Healthcare Personnel Study, New York State. Data were based on 978 weighted responses.
At follow-up, 28.4% (95% CI, 25.0%-31.9%) of respondents who had reported mental or behavioral health problems at baseline no longer reported problems, 6.3% (95% CI, 4.6%-8.1%) reported new problems, and 20.4% (95% CI, 17.2%-23.5%) continued to report them. While we found a significant decrease in the proportion of respondents reporting receiving crisis counseling, from 11.6% (95% CI, 9.1%-14.0%) at baseline to 8.3% (95% CI, 6.3%-10.3%) at follow-up (P = .02), in a survey-adjusted generalized linear model controlling for age, sex, New York State region, and type of practice (hospital-based vs non–hospital-based), reporting any of 5 mental or behavioral health problems was associated with seeking crisis counseling at both baseline survey (OR = 2.2; 95% CI, 1.3-4.0) and follow-up (OR = 2.9; 95% CI, 1.6-5.3).
In stratified comparisons, respondents with persistent mental or behavioral health problems differed significantly in sex and in having their usual practice location in the New York City metropolitan area (Table 2). On survey-adjusted simple logistic regression, the OR for the association between working in the New York City metropolitan area during the baseline survey and the presence of persistent mental and behavioral health issues was 1.5 (95% CI, 1.1-2.2; P = .04). When adjusted for age and sex, this association was no longer significant.
Table 2.
Stratified comparison of persistent mental or behavioral health issues a from baseline to follow-up survey, New York State COVID-19 Healthcare Personnel Study b
| Characteristic | Mental or behavioral health issues | P value c | |
|---|---|---|---|
| None/resolved (n = 38 618.2) | Continuing (n = 9867.9) | ||
| Age group, y | .15 | ||
| 20-39 | 9112.4 (24.5) | 2957.3 (31.1) | |
| 40-59 | 16 331.1 (43.9) | 4301.4 (45.2) | |
| ≥60 | 11 784.8 (31.7) | 2248.0 (23.6) | |
| Sex | <.001 | ||
| Female | 22 543.7 (58.7) | 7299.4 (75.0) | |
| Male | 15 831.5 (41.3) | 2429.8 (25.0) | |
| Profession | .08 | ||
| Physician | 26 490.3 (68.6) | 5632.5 (57.1) | |
| Nurse practitioner | 6521.4 (16.9) | 2419.8 (24.5) | |
| Physician assistant | 5606.5 (14.5) | 1815.6 (18.4) | |
| No. of years in practice | .08 | ||
| <5 | 7560.9 (19.6) | 2511.0 (25.4) | |
| 5-15 | 9865.5 (25.5) | 2763.1 (28.0) | |
| 16-25 | 17 325.5 (44.9) | 3228.8 (32.7) | |
| >25 | 3866.4 (10.0) | 1365.0 (13.8) | |
| No. of patients who died from COVID-19 | .71 | ||
| <10 | 5350.3 (24.5) | 1164.3 (21.2) | |
| 10-20 | 3631.5 (16.6) | 700.2 (12.8) | |
| 21-50 | 3378.1 (15.5) | 922.5 (16.8) | |
| >50 | 9479.0 (43.4) | 2697.7 (49.2) | |
| Worked with COVID-19 patients in previous 2 weeks | 16 149.4 (84.5) | 4665.8 (82.9) | .76 |
| NYC metropolitan practice d | |||
| Baseline | 23 033.7 (60.1) | 6791.2 (69.3) | .04 |
| Follow-up | 19 670.0 (59.7) | 5907.6 (70.0) | .04 |
| NYC practice | |||
| Baseline | 10 536.4 (27.5) | 2987.4 (30.5) | .44 |
| Follow-up | 9635.2 (29.2) | 2478.9 (29.4) | .97 |
| Hospital-based practice | 17 171.9 (45.1) | 4974.8 (50.6) | .27 |
| Clinical specialty | .64 | ||
| Behavioral | 1833 (4.8) | 623 (6.3) | |
| Critical care | 1855 (4.9) | 804 (8.2) | |
| Emergency | 3769 (9.9) | 561 (5.7) | |
| Pediatrics | 6100 (16.0) | 1366 (13.9) | |
| Primary care | 9172 (24.0) | 2460 (25.0) | |
| Nonsurgical specialties | 2442 (6.4) | 692 (7.0) | |
| Surgery | 4698 (12.3) | 1143 (11.6) | |
| Other e | 8358.4 (21.9) | 2177.5 (22.2) | |
| Type of practice | .71 | ||
| Government | 4455.5 (11.6) | 1429.2 (14.5) | |
| Academic | 11 973.5 (31.1) | 2783.6 (28.2) | |
| Private/nonprofit | 17 847.7 (46.3) | 4738.9 (48.0) | |
| Other | 4277.1 (11.1) | 916.3 (9.3) | |
| Reassigned to other than usual duties/specialty | 715.7 (14.4) | 449.5 (22.2) | .34 |
| Worked excess hours at baseline | 12 066.9 (59.2) | 2472.0 (54.9) | .57 |
| Worked excess hours at follow-up | 15 535.0 (64.0) | 4189.2 (66.2) | .72 |
Abbreviation: NYC, New York City.
Mental or behavioral health issues were nervousness/anxiety, worrying thoughts, feeling down or hopeless, lack of pleasure in previously enjoyable activities, and sleep disturbances.
All values are number (percentage) unless otherwise indicated. Participants (978 survey weighted responses representing a weighted estimate of 48 486 [95% CI, 46 256-50 717] physicians, nurse practitioners, and physician assistants licensed in New York State) were surveyed at baseline 13 (April 2020) and follow-up (February 2021).
P value based on matched survey-adjusted t test for dichotomous comparisons and the Pearson χ2 test for >2 categories. P < .05 was considered significant.
Includes NYC metropolitan (“downstate”) area of NYC and Nassau, Suffolk, Westchester, and Rockland counties.
“Other” includes responses that did not fall into the previous 7 specialties.
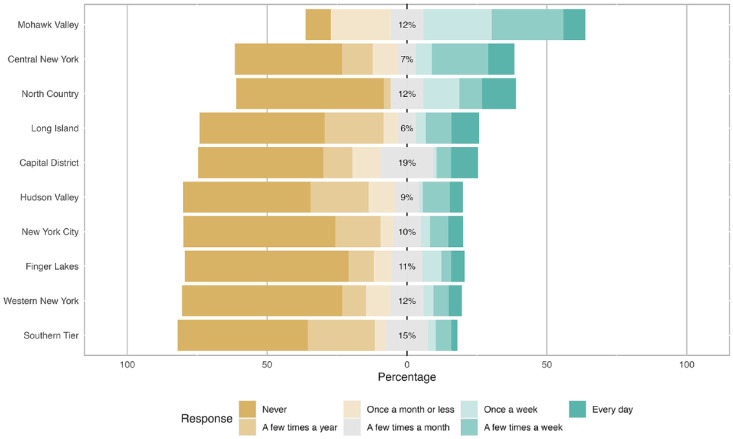
In a question not asked at baseline, more than one-third (35.6%; 95% CI, 31.9%-39.4%) of follow-up respondents reported that they thought about leaving their profession more often than once a month. In a survey-adjusted generalized linear model controlling for age, sex, New York State region, and type of practice (hospital-based vs non–hospital-based), we found a significant association between persistent mental and behavioral health issues and contemplating leaving one’s profession (OR = 2.9; 95% CI, 1.8-4.1; P < .001). The proportion of respondents contemplating leaving their profession varied across the New York State region (Figure 2).
Figure 2.
Responses from physicians, nurse practitioners, and physician assistants to the question, “Since 7/1/20, I’ve considered leaving my profession,” by New York State region, February 2021. The question was asked in a follow-up survey as part of the COVID-19 Healthcare Personnel Study. Data were based on 978 weighted responses.
At baseline, 33.0% (95% CI, 29.3%-36.6%) of respondents reported having any of 11 chronic medical conditions. At follow-up, 36.2% (95% CI, 32.4%-39.9%) reported a chronic medical condition. This increase was significant on the survey-adjusted paired t test (P = .03; Table 3). We found no significant differences in the percentage of respondents reporting any of the 11 chronic conditions from baseline to follow-up. The percentage of respondents reporting heart disease increased, but not significantly, from 3.9% (95% CI, 2.7%-5.3%) of respondents at baseline to 5.3% (95% CI, 3.5%-7.0%) of respondents at follow-up.
Table 3.
Survey-adjusted (weighted) percentage of participants reporting shortages of equipment during COVID-19 at baseline and follow-up surveys, New York State COVID-19 Healthcare Personnel Study a
| Item | Baseline survey | Follow-up survey | P value b |
|---|---|---|---|
| Test kits | 23.3 (20.0-26.5) | 4.4 (2.9-26.5) | <.001 |
| Face masks | 36.0 (32.2-39.8) | 9.8 (7.4-39.8) | <.001 |
| Ventilators | 1.5 (0.6-2.4) | 0.1 (0-2.4) | .005 |
| Beds | 4.3 (2.6-6.1) | 5.7 (3.9-6.1) | .25 |
| Personnel | 20.4 (17.1-23.7) | 18.9 (15.9-23.7) | .47 |
Participants (978 weighted responses from physicians, nurse practitioners, and physician assistants) were surveyed at baseline (April 2020) and follow-up (February 2021). 13
P value based on matched survey-adjusted t test, with P < .05 considered significant.
At baseline, 51.8% (95% CI, 47.9%-55.7%) of respondents reported working directly (in close physical contact) with COVID-19 patients. At follow-up, that proportion had increased to 61.3% (95% CI, 57.5%-65.5%). This 8.8% percentage-point increase was significant on the survey-adjusted paired t test (P < .001). Respondents reported a significant improvement in the availability of face masks, testing, and ventilators (Table 3). Respondents reported on average working approximately 5 more hours during a 2-week period at follow-up compared with baseline (78.1 vs 72.6 hours; P = .008).
Discussion
Our study contributes to accumulating evidence of the impact of the COVID-19 pandemic on health care professionals with a larger, more comprehensive longitudinal assessment than has previously been reported and includes multiple specialties and professions in a geographic region that was an early epicenter of the COVID-19 pandemic. Our results indicate a mixed and evolving picture. While evidence of distress is apparent, with one-third of respondents contemplating leaving their profession, we also found demonstrable declines in multiple measures of behavioral and mental health disorders.
Still, for 20% of physicians, nurse practitioners, and physician assistants, mental health concerns had become a persistent problem; those reporting mental and behavioral health problems were more than twice as likely to report taking advantage of crisis counseling than those who did not report mental and behavioral health problems. Our results are consistent with population estimates that 40% of all people in New York State reported “poor mental health” about the time this survey was administered. 19 In our survey sample, chronic psychological stress was related to burnout and wanting to leave one’s profession.
A nationwide survey of physicians in 2020 reported that 37% of those surveyed “would like to retire in the next year.” 20 While physician burnout is not a new phenomenon, addressing the continuing concerns and psychological stress among the health care workforce is a necessary part of any response to retaining highly trained and essential medical professionals. While some medical editorialists warn that the current stressors to “an already fragile workforce . . . have become insurmountable,” 21 some interventions may be within the means of managers and policy makers. In a recently published analysis by our group, 14 we reported that potentially modifiable occupational circumstances, such as working more hours than usual, working directly with patients while sick themselves, and having shortages of protective equipment and other items, were all associated with adverse mental health outcomes among health care workers during the initial COVID-19 pandemic wave in New York State.
In a March 2020 survey of emergency medicine physicians at 7 academic medical centers in the United States, 90.8% of 426 physicians surveyed were experiencing changes in their behavior toward family and friends. These physicians identified access to personal protective equipment and increased availability of COVID-19 testing as 2 measures that would help alleviate their stress and anxiety. 22 In our analyses, while concerns about the availability of testing kits and personal protective equipment declined, the decreased availability of personnel remained concerning.
Our follow-up survey illustrates how the impact of the COVID-19 pandemic on health care professionals continues to evolve and points out the importance of longitudinal assessments. We note that the proportion of respondents reporting they worked in close contact with COVID-19 patients increased significantly from baseline to follow-up. We believe this increase was largely the result of the follow-up survey coinciding with a second, large wave of infections that had expanded from the New York City area to encompass the entire state. Response bias may also have affected these results; physicians, nurse practitioners, and physician assistants working in settings with more COVID-19 patients may have been more likely than those for whom COVID-19 was less of an issue to participate in the follow-up survey.
Our results include a significant increase in the proportion of respondents reporting chronic medical conditions. While some of this increase may be attributed to the aging of health care workers in general, attrition and changes in the underlying relative demographic characteristics of health care professionals and some possibly as yet unrealized chronic effects of COVID-19 infections may have come into play. The potential for the COVID-19 pandemic to have a long-lasting effect on the health of medical workers is a critically important area of additional research to which surveys such as CHPS can contribute evidence.
Limitations
Our study had 2 limitations. First, these results apply narrowly to physicians, nurse practitioners, and physician assistants, whose demographic characteristics differ from other groups, including non-Hispanic Black/African American people who comprise a large proportion of people providing nonmedical direct services to COVID-19 patients in New York City. 23 Additional results from the CHPS sample of nonmedical providers can provide insight into this area of research. Second, while our response rate relative to the entire sampling frame was low, it is comparable with other recent studies of physicians. 24 We adjusted our survey sample to better match the target population on demographic and geographic measures, but biases in this group of clinicians who chose to participate are likely. The motivation of the initial group of respondents to join the longitudinal cohort, however, offers the opportunity to reliably track changes and trends in this sample.
Conclusion
We found evidence of both distress and resilience among physicians, nurse practitioners, and physician assistants responding to the COVID-19 pandemic in New York State. Our results indicate that concrete steps, such as limiting the number of hours worked, ensuring that clinicians are not compelled to work directly with patients while ill themselves, and addressing shortages of protective equipment and other items, may be taken by government and hospital administrations to help address their concerns and support their resilience.
Supplemental Material
Supplemental material, sj-docx-1-phr-10.1177_00333549231155473 for The New York State COVID-19 Healthcare Personnel Study: One-Year Follow-up of Physicians, Nurse Practitioners, and Physician Assistants, 2020-2021 by Charles DiMaggio, Ezra Susser, Spiros Frangos, David Abramson, Howard Andrews, Christina Hoven, Megan Ryan and Guohua Li in Public Health Reports
Acknowledgments
The authors thank Ms Barbara Lang for administrative support; Jennifer Norton, PhD, for data cleaning and preparation; and Howard Zucker, MD, JD, and the office of the New York State Commissioner of Health for inviting the New York State health care workforce to participate in this survey.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Dr Hoven’s efforts were supported in part by the New York State Office of Mental Health.
ORCID iDs: Charles DiMaggio, PhD, MPH  https://orcid.org/0000-0003-2356-6659
https://orcid.org/0000-0003-2356-6659
David Abramson, PhD, MPH  https://orcid.org/0000-0002-7846-3588
https://orcid.org/0000-0002-7846-3588
Supplemental Material: Supplemental material for this article is available online. The authors have provided these supplemental materials to give readers additional information about their work. These materials have not been edited or formatted by Public Health Reports’s scientific editors and, thus, may not conform to the guidelines of the AMA Manual of Style, 11th Edition.
References
- 1.Mosheva M, Hertz-Palmor N, Dorman Ilan S, et al. Anxiety, pandemic-related stress and resilience among physicians during the COVID-19 pandemic. Depress Anxiety. 2020;37(10):965-971. doi: 10.1002/da.23085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al Sulais E, Mosli M, AlAmeel T. The psychological impact of COVID-19 pandemic on physicians in Saudi Arabia: a cross-sectional study. Saudi J Gastroenterol. 2020;26(5):249-255. doi: 10.4103/sjg.SJG_174_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Uyaroğlu OA, Başaran NÇ, Ozisik L, et al. Evaluation of the effect of COVID-19 pandemic on anxiety severity of physicians working in the internal medicine department of a tertiary care hospital: a cross-sectional survey. Intern Med J. 2020;50(11):1350-1358. doi: 10.1111/imj.14981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodriguez RM, Medak AJ, Baumann BM, et al. Academic emergency medicine physicians’ anxiety levels, stressors, and potential stress mitigation measures during the acceleration phase of the COVID-19 pandemic. Acad Emerg Med. 2020;27(8):700-707. doi: 10.1111/acem.14065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kowalski LP, Imamura R, de Castro G, Jr, et al. Effect of the COVID-19 pandemic on the activity of physicians working in the areas of head and neck surgery and otorhinolaryngology. Int Arch Otorhinolaryngol. 2020;24(3):258-266. doi: 10.1055/s-0040-1712169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Uyaroğlu OA, Özdede M, Çalık Başaran N, Özışık L, Tanriover MD, Sain Güven G.“Anxiety is still ongoing!” Evaluation of the effect of the COVID-19 pandemic on anxiety severity of physicians working in the internal medicine department after 1 year: a collaborative cross-sectional study. Intern Med J. 2021;51(11):1940-1945. doi: 10.1111/imj.15558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dionisi T, Sestito L, Tarli C, et al. Risk of burnout and stress in physicians working in a COVID team: a longitudinal survey. Int J Clin Pract. 2021;75(11):e14755. doi: 10.1111/ijcp.14755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shanafelt TD, Dyrbye LN, West CP.Addressing physician burnout: the way forward. JAMA. 2017;317(9):901-902. doi: 10.1001/jama.2017.0076 [DOI] [PubMed] [Google Scholar]
- 10.Gleason C.1 in 5 physicians has considered quitting their current job, survey finds. Becker’s Hospital Review. October11, 2021. Accessed February 2, 2022. https://www.beckershospitalreview.com/hospital-physician-relationships/1-in-5-physicians-has-considered-quitting-their-current-job-survey-finds.html
- 11.Hurt A. Docs are leaving practice, but not only because of COVID-19, says new survey. Medscape. October8, 2021. Accessed February 2, 2022. https://www.medscape.com/viewarticle/960491#:~:text=The%20results%20were%20sobering.,53%25)%20are%20looking%20online
- 12.Johnson AA, Wallace BK, Xu Q, et al. Hopelessness in New York State physicians during the first wave of the COVID-19 outbreak. J Neurosurg Anesthesiol. 2022;34(1):152-157. doi: 10.1097/ANA.0000000000000808 [DOI] [PubMed] [Google Scholar]
- 13.DiMaggio C, Abramson D, Susser ES, et al. The COVID-19 Healthcare Personnel Study (CHPS): overview, methods, and preliminary findings. J Neurosurg Anesthesiol. 2022;34(1):148-151. doi: 10.1097/ANA.0000000000000813 [DOI] [PubMed] [Google Scholar]
- 14.Cheslack-Postava K, Bresnahan M, Ryan M, et al. Occupational conditions associated with negative mental health outcomes in New York State health professionals during the COVID-19 pandemic. J Occup Environ Med. 2022;64(7):e417-e423. doi: 10.1097/JOM.0000000000002566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Armstrong DP, Chung R, Daman S, Forte GJ.New York Physician Workforce Profile, 2014 Edition. Center for Health Workforce Studies, School of Public Health, SUNY Albany; 2015. Accessed July 15, 2020. https://www.chwsny.org/our-work/reports-briefs/r-2015-6 [Google Scholar]
- 16.Martiniano R, Wang S, Moore J.A Profile of New York State Nurse Practitioners, 2017. Center for Health Workforce Studies, School of Public Health, SUNY Albany; October2017. [Google Scholar]
- 17.Liu Y, Martiniano R, Moore J.A Comparative Analysis of New York’s Active Nurse Practitioners and Physician Assistants. Center for Health Workforce Studies, School of Public Health, SUNY Albany; 2018. [Google Scholar]
- 18.New York State Education Department. Licenses statistics. Accessed July 28, 2020. http://www.op.nysed.gov/prof/med/medcounts.htm
- 19.NY Health Foundation. Still recovering: mental health impact of the COVID-19 pandemic in New York State. 2021. Accessed February 18, 2022. https://nyshealthfoundation.org/resource/still-recovering-mental-health-impact-of-the-covid-19-pandemic-in-new-york-state
- 20.The Physicians Foundation. The Physicians Foundation 2020 survey of America’s physicians: COVID-19 impact edition. Accessed February 22, 2022. https://physiciansfoundation.org/wp-content/uploads/2020/12/2020-Survey-of-Americas-Physicians_Exec-Summary.pdf
- 21.Abbasi J.Pushed to their limits, 1 in 5 physicians intends to leave practice. JAMA. 2022;327(15):1435-1437. doi: 10.1001/jama.2022.5074 [DOI] [PubMed] [Google Scholar]
- 22.Rodriguez RM, Medak AJ, Baumann BM, et al. Academic emergency medicine physicians’ anxiety levels, stressors, and potential stress mitigation measures during the acceleration phase of the COVID-19 pandemic. Acad Emerg Med. 2020;27(8):700-707. doi: 10.1111/acem.14065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hong N.3 hospital workers gave out masks. Weeks later, they all were dead. The New York Times. May4, 2020. Accessed May 9, 2020. https://www.nytimes.com/2020/05/04/nyregion/coronavirus-ny-hospital-workers.html
- 24.West CP, Dyrbye LN, Sinsky C, et al. Resilience and burnout among physicians and the general US working population. JAMA Netw Open. 2020;3(7):e209385. doi: 10.1001/jamanetworkopen.2020.9385 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-phr-10.1177_00333549231155473 for The New York State COVID-19 Healthcare Personnel Study: One-Year Follow-up of Physicians, Nurse Practitioners, and Physician Assistants, 2020-2021 by Charles DiMaggio, Ezra Susser, Spiros Frangos, David Abramson, Howard Andrews, Christina Hoven, Megan Ryan and Guohua Li in Public Health Reports