Abstract
The COVID-19 pandemic has financial and emotional impacts on families. We explored how caregivers’ financial strain and mental health are associated with changes in their young children’s behavior during the pandemic. We additionally considered whether having a sense of purpose moderated these associations. Caregivers (n = 300) in the emergency department of a children’s hospital were surveyed anonymously about changes to their employment (e.g., reduced/increased hours and job loss), ability to pay for expenses and whether their child’s behavior had changed. Aligned with the Family Stress Model, caregivers’ financial strain was associated with poor mental health, inconsistent sleep routines, and changes in children’s problematic and prosocial behaviors. A sense of purpose buffered some of these relationships. Families are differently affected by the pandemic and our findings underscore the need for supporting caregivers’ mental health and connecting them with resources.
Keywords: COVID-19, Family Stress Model, parental mental health, stress, financial strain, sense of purpose, child development
Introduction
Parental stress has robustly been shown to be risky to the quality of parenting, family functioning and children’s development (Claessens, Engel, & Curran, 2015; Prickett, 2020; Priel, Djalovski, Zagoory-Sharon, & Feldman, 2019). The Family Stress Model posits that economic stress influences children’s developmental outcomes, largely through parental mental health and its impact on parenting practices (Masarik & Conger, 2017). The COVID-19 pandemic has greatly altered life, with likely differential impacts on parents (Brown, Doom, Lechuga-Peña, Watamura, & Koppels, 2020). While some adults have lost income, others have had no change or even increases in work (Kramer & Kramer, 2020). With most childcare settings closed, few ways to search for jobs, and increased expectations to work from home, caregivers may experience more stress and worse mental health. Such contextual stressors could affect children’s behaviors. Given the possible differential impact of the pandemic on families, we sought to understand how caregivers might be affected by the current pandemic and how those experiences relate to perceived changes in their children’s behavior. Drawing on extant research, especially the Family Stress Model (Masarik & Conger, 2017), and considering this unique time, we hypothesized that increased financial strain would be related to greater feelings of stress, sadness, and anxiety, which would be associated with lower-quality parenting practices and subsequently, increased behaviors problems for children.
Parental Financial Strain
Families with few financial resources often experience strain in meeting basic needs and psychological consequences related to worrying about household finances (Voydanoff, 1984). These financial strains can influence parents’ well-being, causing increased feelings of stress, sadness, and anxiety (Dijkstra-Kersten, Biesheuvel-Leliefeld, Wouden, Penninx, & Marwijk, 2015).
Financial strain is often more severe with rapid changes in income, such as the loss of employment. Involuntary job loss is an unexpected disruption for families that results in psychological tolls on parents (Brand, 2015). Importantly, there is a negative association between involuntary job loss and parental sensitivity to children (Prickett, 2020). This is especially important during the COVID-19 pandemic, when there were very rapid changes in employment for many parents, when the United States initiated shelter-in-place policies, followed by social-distancing practices that resulted in the continued closure of many places of employment. Emerging COVID-19 pandemic research has found financial concerns to be related to increased anxiety and worse mental health (Hertz-Palmor et al., 2021; Wilson et al., 2020), especially among those who have experienced a loss of employment. However, more research is needed to understand the extent and types of financial strain experienced specifically by parents of young children during this pandemic.
Parental Stress, Depression, and Anxiety
Financial strain is associated with worse mental health (Brand, 2015) and poor parental mental health influences the quality of parenting practices and children’s outcomes (Claessens et al., 2015; Priel et al., 2019). Elevated levels of stress, depressive symptoms, and anxiety are associated with less responsive and sensitive parenting, less stimulating home environments, and worse social, emotional, and academic outcomes for children (Carter, Garrity-Rokous, Chazan-Cohen, Little, & Briggs-Gowan, 2001; Conners-Burrow et al., 2014; Field, 2011; Tan, Wang, & Ruggerio, 2017). Importantly, sadness and anxiety below clinical thresholds are still related to lower-quality parenting practices and worse child outcomes (Brennan et al., 2000; Conners-Burrow et al., 2014; Goodman et al., 2011). Further, research finds the impacts of mental health issues on child outcomes to be stronger for families with few financial resources or more economic strain (Golberstein, Gonzales, & Meara, 2016; Masarik & Conger, 2017).
With the changes to daily life caused by the COVID-19 pandemic and potential financial impacts, caregivers could feel more stress, sadness, or angst, which could impact both their parenting and their children’s development.
Family Stress Model
Although largely applied to families with adolescents, the Family Stress Model (Conger, Rueter, & Conger, 2000) proposes a mediational model in which financial strain influences parental mental health, parenting practices, and child outcomes. Studies prior to the pandemic have supported the pathway of financial strain to parents’ poor mental health, which is predictive of lower parenting quality and negative child outcomes (Jackson, Brooks-Gunn, Huang, & Glassman, 2000). For instance, studies find that parents who report experiencing financial strain also report challenges with engaging in consistent and high quality parenting practices (e.g., consistent discipline and nutritious meals) (Marcil et al., 2020) and that parents’ increased stress, anxiety, and depression are associated with less stimulating and nurturing home environments (Carter et al., 2001; Conners-Burrow et al., 2014; Field, 2011; Tan et al., 2017). Studies of the Family Stress Model explicitly find a pathway from financial strain to poor child outcomes, mediated by parental mental health, coparenting conflict and low parental efficacy, harsh parenting, and less stimulation of the home (Neppl, Senia, & Donnellan, 2016; Nievar, Moske, Johnson, & Chen, 2014; Scaramella, Sohr-Preston, Callahan, & Mirabile, 2008). Nascent research during this pandemic has found support for some of these pathways. For instance, financial concerns are positively related to anxiety and worse mental health (Wilson et al., 2020) and children of parents experiencing financial strain and depression are at increased risk of psychological maltreatment (Lawson, Piel, & Simon, 2020). Although pandemic-related job loss and work-hour reductions are widespread in the United States (Wilson et al., 2020), few studies to date have investigated how this increase in financial strain relates to the development of young children, independently or in conjunction with poor mental health, and none have tested the Family Stress Model specifically.
Buffering Role of Sense of Purpose
Studies have shown that life’s stressors are often weathered more effectively by individuals who have a sense of purpose (Hill, Sin, Turiano, Burrow, & Almeida, 2018; Homan & Kong, 2020; Malin, Morton, Nadal, & Smith, 2019; Ryff, 1989). In the domain of parenting, interventions that promote a greater sense of purpose, such as mutual-aid groups, tend to reduce parental feelings of stress, depression, and loneliness (Dwivedi, 2000; Inagaki & O’rehek, 2017; Telleen, Herzog, & Kilbane, 1989). However, the potential moderating role of sense of purpose on family systems is not well studied, especially in periods of acute stress like the COVID-19 pandemic. Therefore, we consider whether feelings of purpose during this pandemic moderate the associations between financial and mental health stressors and children’s behavior problems.
Present Study
Given that the relationship between poor caregiver mental health and negative child outcomes may be stronger for those with financial strain from job loss, work-hour reductions, or concerns about being able to afford basic needs such as rent and food, we use the Family Stress Model to consider how pandemic-induced changes in caregiver mental health and financial strain relate to changes in parenting and children’s behavior during the COVID-19 pandemic. Additionally, given the benefits of having a sense of purpose (Hill et al., 2018; Homan & Kong, 2020; Malin et al., 2019; Ryff, 1989), we explore if it could buffer the associations between caregiver financial and emotional strain, parenting, and child behaviors.
Methods
From July 16, 2020 to September 1, 2020, 300 caregivers of children 8 years or younger in the emergency department of a children’s hospital in California completed an anonymous online survey examining their financial strain, stress, depression, and anxiety as well as changes in their child’s behaviors. During this time, the SARS-CoV-2 positivity rate per 100,000 with the testing capacity of the time was 5.1–7.5%.
Procedure
When caregivers were in a waiting area or exam room with a child 0–8 years old, they were asked by hospital staff (doctor, nurse, or technician) if they would be willing to complete an anonymous survey on one of the hospital iPads. If interested, they were asked to review the study information sheet on the tablet and select continue if consenting to participate. The consent document and survey were available in English and Spanish. All procedures and materials were approved by both a university and hospital Institutional Review Boards.
In total, 364 caregivers of a young child were approached about the study. Three hundred (82.4%) agreed to participate. Of these, seven did not complete the survey (2.3% attrition rate). As these are anonymous data, no details are available for comparison between participating and non-participating caregivers.
Participants
Respondents were primarily mothers (89.42%) and over half identified as Hispanic/Latine (58.70%). Most respondents reported annual household incomes of $40,000 or below (53.93%), and the majority had not earned a college degree (63.14%), although roughly a quarter (25.26%) had completed some college. Nearly three-quarters of respondents (72.35%) had a child 4 years or younger. More information about the sample is available in Table 1.
Table 1.
Sample Characteristics.
| % or M (SD) | N | |
|---|---|---|
| Relationship status to child | ||
| Mother | 89 | 262 |
| Father | 9 | 26 |
| Other | 2 | 5 |
| Relationship status | ||
| Never married/single | 27 | 78 |
| Married/living as married | 66 | 193 |
| Divorced/separated/widowed | 7 | 22 |
| Race/ethnicity | ||
| Hispanic/Latine | 59 | 172 |
| White/Caucasian | 22 | 65 |
| Asian/Asian-American | 7 | 22 |
| Other | 12 | 34 |
| Income (household/year) | ||
| Less than $20,000 | 24 | 69 |
| $21,000–$40,000 | 30 | 89 |
| $41,000–$60,000 | 18 | 53 |
| $61,000–$100,000 | 11 | 31 |
| More than $100,000 | 17 | 51 |
| Household crowding (room: people) | 2.28 (1.38) | 287 |
| Age of child brought to ER | ||
| Less than 1 year old | 18 | 53 |
| 1–2 years old | 33 | 96 |
| 3–4 years old | 21.5 | 63 |
| 5–6 years old | 16 | 47 |
| 7–8 years old | 11.5 | 34 |
| Education level | ||
| Less than high school | 39 | 111 |
| Some college/AA | 34 | 102 |
| Bachelor degree | 18 | 54 |
| Graduate degree | 9 | 26 |
| Language—survey | ||
| English | 89 | 262 |
| Spanish | 11 | 31 |
| Lost hours | 18 | 53 |
| Lost job | 22 | 65 |
| More difficulty with expenses | 38 | 112 |
| More difficulty in paying bills/basic needs | 37 | 108 |
Survey
The online survey was administered through the RedCap portal on iPads owned by the emergency department, which were sanitized between uses. The 39-item survey asked about demographic information (e.g., education level and income) and information related to experiences during the COVID-19 pandemic (e.g., financial strain, resources accessed, stress, and sense of purpose). Information was also collected to characterize the current routines of the children, as well as any behavioral changes observed since the onset of the COVID-19 pandemic.
Financial Strain
Respondents were asked whether their employment status had changed since onset of the COVID-19 crisis (e.g., job loss, new job, working from home, and number of hours worked) and whether the family was experiencing more, less, or the same amount of difficulty in keeping up with expenses (e.g., rent, bills, and food). A continuous variable was created for financial strain, with a maximum of three points: reduction in number of hours or loss of a job (1 point); increased difficulty in keeping up with bills and housing expenses (1 point); and increased difficulty in paying for basic needs like food (1 point).
Caregivers’ Mental Health Problems
Feelings of depression and anxiety were measured with the Patient Health Questionnaire-4 (PHQ-4) (Kroenke, Spitzer, Williams, & Löwe, 2009). Caregivers indicated how often in the past 2 weeks they experienced two indicators of depression (Cronbach’s α = .87) and two indicators anxiety (Cronbach’s α = .88) on a scale from 0 (not at all) to 3 (nearly every day). Scores were summed to create a depression and anxiety summary score, each from 0 to 6.
Stress was measured using the Perceived Stress Scale (Cohen, Kamarck, & Mermelstein, 1983). Only two of the four items were used due to lack of internally consistency for our sample (Cronbach’s α = .47). Factor analysis indicated two factors based on whether the items were reversed (Items 2 and 3) or not (1 and 4). Thus, we used the non-reversed, more highly correlated (r = .81) items. Respondents indicated on a 5-point Likert scale (0 = never to 4 = very often) whether they felt unable to control the important things in life and overwhelmed by difficulties in life. Items were transformed into a 4-point scale in order to match the scaling of the depression and anxiety scales for the purpose of creating a latent variable of parents’ mental health. A summary variable was created from these stress items (Cronbach’s α = .69; range 0–6).
Caregivers’ Sense of Purpose
Caregivers were asked to rate the degree to which they felt a sense of purpose (e.g., parental responsibility and role as an essential worker) during the pandemic on a scale of 0 (not at all) to 3 (very much). Nearly 80% of respondents reported “very much.” Due to the left-skewness of the data, we created a binary variable for parents’ sense of purpose with score of 3 (very much) indicating a high sense of purpose (n = 230) and scores from 0 (not at all) to 2 (sometimes) indicating a low sense of purpose (n = 63).
Family Sleep Routines
Caregivers were asked how often they had a consistent schedule for their children’s waking up, naptime, and bedtime in a week (Cronbach’s α = .75; 0 = not usually, 1 = most of the time, and 2 = always) and from this, we created a summary score with a total of six possible points if the respondent reported always having a consistent schedule for each item.
Children’s Behaviors
Caregivers rated if the frequency of negative and/or positive behaviors exhibited by the child they had brought to the hospital had changed since the start of the pandemic. Response options included: (1) a lot less, (2) a little less, (3) the same, (4) a little more, and (5) or a lot more. Four types of children’s behaviors were assessed. First, acting out included two items on hitting and having tantrums (each scored as 1 if occurring more), which were summed for a total acting out score (range 0–2). Second, regressing behaviors included two items on bedwetting/accidents and talking (for children 0–4 years, a score of 1 if talking the same or less and for children 5–8 if talking a little or a lot less), with a combined range of 0–2. Third, emotional coping included little or a lot more crying (score = 1), needing to be held more often (score = 1), and changes (more or less) in eating (score = 1) and sleeping (score = 1). Scores were then summed to create a composite score for behavior changes (range 0–4). Finally, positive behaviors included expressing affection and offering help a little or a lot more (range 0–2).
Covariates
To elucidate the association between caregivers’ feelings and changes in children’s behaviors, we controlled for child age, caretakers’ education level, household income, and household crowding (i.e., scored as the proportion of people to number of bedrooms in the home). Child age was a categorical variable (less than 1 year old, 1–2 years old, 3–4 years old, 5–6 years old, and 7–8 years old). Four levels (high school or less, some college, college degree (associate or bachelor), and graduate degree (master or doctoral) of education were used as a categorical variable as well as five categories of household income (less than $20,000 to more than $100,000). A people-to-bedroom ratio (i.e., household crowding) was calculated by dividing the number of family people living in the home by the number of bedrooms.
Analytic Plan
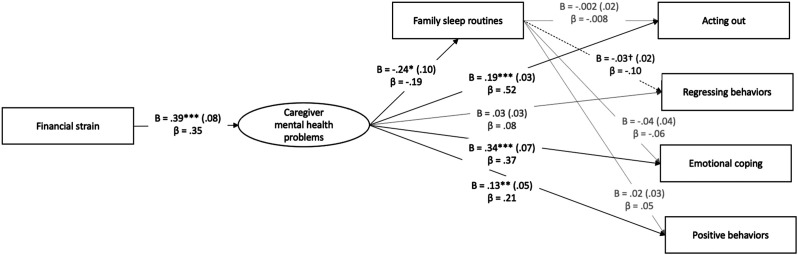
The current study tested the Family Stress Model using a structural equation modeling (SEM) framework in Mplus version 8.3. We estimated models to capture processes a) in the overall sample and b) in subgroups based on caregivers’ sense of purpose. Analyses were conducted across 293 participating caregivers, who all had complete data in the focal variables. As depicted in Figure 1, financial strain, sleep routines, and the four child behaviors (i.e., acting out, regressing, emotional coping, and positive behaviors) were estimated as measured variables. Caregivers’ mental health was estimated as a latent variable with indicators for depression, anxiety, and stress. We correlated the error terms for the depression and anxiety scales as they both originated from the PHQ-4 scale.
Figure 1.
Latent structural equation model for the relations between financial strain, caregivers’ mental health problems, family sleep routines, and children’s behaviors. Note. SEM Model includes pathways from parent education, people-to-room ratio, household income to each focal variable, as well as from child age to caregiver mental health, family sleep routines, and children’s behaviors. †p < .10. *p < .05. **p < .01. ***p < .001.
First, we estimated the overall structural processes outlined by the Family Stress Model. We estimated a direct effect of financial strain on caregivers’ mental health problems. Then, we estimated direct pathways from caregivers’ mental health problems to sleep routines and the four child behavior outcomes. Finally, we assessed the direct effects of sleep routines on child behaviors. Family covariates included parental education, household income, and people-to-bedroom ratio (household crowding) as predictors of family strain, caregivers’ mental health problems, sleep routines, and children’s behaviors. We also used children’s age as a covariate of caregivers’ mental health problems, sleep routines, and children’s behaviors. We examined several indices for overall model fit, including chi-square model fit test, RMSEA, CFI, TLI, and SRMR (Little, 2013).
Second, we estimated two mediational pathways through which caregivers’ financial strain may indirectly predict children’s behaviors. On one hand, caregivers’ mental health problems alone may mediate the associations between financial strain and children’s behaviors. On the other hand, financial strain may predict caregivers’ mental health, which predicts sleep routines; sleep routines then predict children’s behaviors in turn. We estimated these indirect effects using the MODEL INDIRECT command in Mplus v8.3 (Grimm, Ram, & Estabrook, 2016; Muthén & Muthén, 1998–2017). We examined the 95% confidence intervals (CIs) of the indirect effects, with CIs not encompassing zero indicating significant mediational pathways.
Finally, we tested the moderating role of caregivers’ sense of purpose in the Family Stress Model via multigroup analyses. We re-estimated a SEM model that freely estimated the focal pathways separately for caregivers with a high versus lower sense of purpose. Then, we estimated a nested model constraining all focal pathways to be equal across the two groups. Then, we examined the change in chi-square and compared the overall model fit between the two models. A non-significant chi-square indicated that all pathways were similar across groups. If the chi-square change was statistically significant, however, we examined each focal pathway to determine where relations differed between high and low purpose groups.
Results
About two-thirds of caregivers reported at least one type of financial strain related to the pandemic (job loss or reduced hours, difficulty in keeping up with household expenses (e.g., rent), difficulty in paying for basic needs. Approximately 40% reported losing hours or their job and over 1/3 reported more difficulty in paying for living expenses. Caregivers reported average levels of stress 7.75 (SD = 2.80), with many families feeling confident about handling their personal problems (61.44%). On average, caregivers reported limited feelings of sadness and anxiety (M = 2.54 of 12, SD = 3.01). Twenty-one percent reported feeling nervous, anxious, or on edge most to all of the time and another 17.7% reported not being able to stop or control worrying. With regards to sleep routines, caregivers reported moderate levels of consistent routines (M = 3.73 of 6, SD = 2.57), with about half always having a consistent bedtime (53.92%) and wake up time (47.78%) and less having a regular naptime (31.40%).
Approximately 30% of caregivers reported no increase in any of the concerning behaviors. Only 17% of children displayed four or more of the seven possible concerning behaviors (M=1.74, SD=1.64). Caregivers reported increased tantrums (13%), decreased child talking (or, if the child was under age 4, no growth in talking: 35%), increased need to be held (31%), changes in eating (27%), increased crying (28%), and changes in sleep (23%). Just under-half reported increases in affection and offers to help (47%).
Testing the Family Stress Model
As shown in Figure 1 and Table 2, the overall Family Stress Model yielded good to excellent fit to the data, χ2 (25) = 43.90, p < .05, RMSEA [90% CI] = .05 [.02; .08], CFI/TLI = .97/.92, SRMR = .03. All indicators of caregiver mental health problems significantly loaded on the latent variable, with standardized factor loadings falling between .70 and .75, p’s < .001. The pathways largely supported the Family Stress Model. Financial strain was positively associated with caregivers’ mental health problems (B = .39, SE = .08, p < .001, β = .35). In turn, caregivers’ mental health problems negatively predicted sleep routines (B = −.24, SE = .10, p < .05, β = −.19) and positively predicted children’s acting out (B = .19, SE = .03, p < .001, β = .52) and poor emotional coping (B = .34, SE = .07, p < .001, β = .37). Contrary to expectations, caregivers’ mental health problems also predicted children’s positive behaviors (B = .13, SE = .05, p < .01, β = .21) but not children’s regressing behaviors. Sleep routine also did not predict acting out, poor emotional coping, or positive behaviors and only marginally predicted regressing behaviors (B = −.03, SE = .03, p < .10, β = −.10).
Table 2.
Indirect Effects of Financial Strain on Child’s Behaviors.
| Effect | B | 95% CI |
|---|---|---|
| Financial strain → acting out | ||
| Total effect | .08 | [.04; .11] |
| Via parent mental health | .08 | [.04; .11] |
| Via parent mental health and family routines | .00 | [−.01; .004] |
| Financial strain → regressing behaviors | ||
| Total effect | .02 | [−.01; .04] |
| Via parent mental health | .01 | [−.01; .04] |
| Via parent mental health and family routines | .00 | [.00; .01] |
| Financial strain → emotional coping | ||
| Total effect | .14 | [.07; .22] |
| Via parent mental health | .13 | [.07; .21] |
| Via parent mental health and family routines | .00 | [−.003; .02] |
| Financial strain → positive behaviors | ||
| Total effect | .05 | [.01;.09] |
| Via parent mental health | .05 | [.01; .09] |
| Via Parent mental health and family routines | .00 | [−.01; .003] |
Note. All confidence intervals (CIs) are at 95%. CIs that do not encompass zero are statistically significant.
Tests of Mediation
In addition to direct effects, we found indirect effects in the associations between financial strain and children’s behaviors (Table 3). Overall, indirect associations between financial strain and children’s behaviors were largely accounted for by caregivers’ mental health alone. Caregivers’ mental health problems significantly mediated the links between financial strain and children’s acting out (B [95% CI] = 0.08 [0.04, 0.11]), poor emotional coping (B [95% CI] = .13 [.07, .21]), and positive behaviors (B [95% CI] = .05 [.01, .09]). Financial strain was not related to children’s behaviors via caregiver mental health and sleep routines.
Table 3.
Model Fit Comparisons from the Multigroup Analyses between High and Low Purpose Groups.
| Model | χ2 | df | p | Δχ2 | Δdf | p | RMSEA | 90% CI | CFI/TLI | SRMR |
|---|---|---|---|---|---|---|---|---|---|---|
| Freely estimated model | 69.16 | 54 | .080 | — | — | — | .04 | [.000; .072] | .977/.940 | .03 |
| All pathways equal | 101.54 | 64 | .002 | 32.39 | 10 | <.001 | .06 | [.039; .086] | .944/.874 | .05 |
| Mental health to child behaviors equal | 75.87 | 58 | .058 | 6.72 | 4 | .152 | .05 | [.000; .072] | .973/.934 | .04 |
| Routines to child behaviors equal | 92.36 | 58 | .003 | 23.20 | 4 | <.001 | .06 | [.038; .087] | .949/.873 | .04 |
| Routines to acting out equal | 79.67 | 55 | .017 | 10.51 | 1 | <.001 | .06 | [.024; .081] | .963/.904 | .04 |
| Routines to regressing equal | 70.18 | 55 | .082 | 1.02 | 1 | .312 | .04 | [.000; .071] | .977/.941 | .04 |
| Routines to emotional coping equal | 69.78 | 55 | .088 | .63 | 1 | .429 | .04 | [.000; .071] | .978/.943 | .04 |
| Routines to positive behaviors equal | 74.54 | 55 | .041 | 5.38 | 1 | .020 | .05 | [.011; .076] | .971/.924 | .04 |
| Mental health to routines | 74.08 | 55 | .044 | 4.92 | 1 | .027 | .05 | [.008; .075] | .972/.925 | .04 |
| Financial strain to mental health | 69.90 | 55 | .085 | .74 | 1 | .388 | .04 | [.000; .071] | .978/.942 | .04 |
| aFinal model | 76.44 | 61 | .088 | 7.28 | 7 | .400 | .04 | [.000; .068] | .977/.946 | .04 |
Note. Δχ2 and Δdf based on the differences in estimates from the freely estimated model.
aFinal model constrained all focal pathways to be equal across high and low purpose groups except for the pathways in bold.
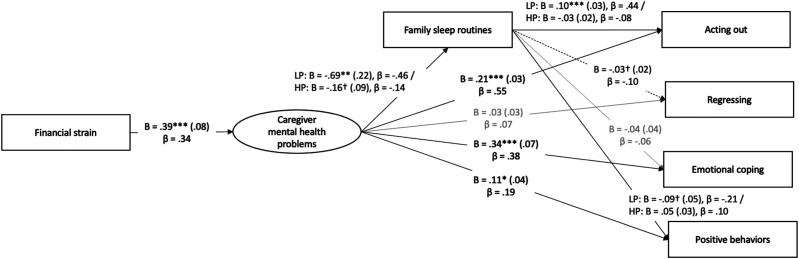
Sense of Purpose as a Moderator
Figure 2 presents the multigroup analysis results examining caregivers’ sense of purpose as a moderator. Relative to the model that freely estimated the focal pathways separately for the high and low purpose groups, constraining all focal pathways to be equal across groups led to a significant change in chi-square, Δχ2 (10) = 32.39, p < .001, and poorer model fit, χ2 (64) = 101.54, p < .01, RMSEA [90% CI] = .06 [.04; .09], CFI/TLI = .94/.87, SRMR = .05. That is, we found that one or more pathways were significantly different between the high and low purpose groups.
Figure 2.
Latent structural equation model including the moderated pathways by caregivers' sense of purpose. Note. LP = estimates for low purpose group. HP = estimates for high purpose group. SEM Model includes pathways from parent education, people-to-room ratio, household income to each focal variable, as well as from child age to caregiver mental health, sleep routines, and children’s behaviors. †p < .10. *p < .05. **p < .01. ***p < .001.
Further probes into group differences for each focal pathway led to a final SEM model indicating that caregivers’ sense of purpose moderated three specific pathways (see Figure 2). First, caregivers’ mental health problems negatively predicted sleep routines among caregivers with low sense of purpose (B = −.69, SE = .22, p < .01). However, caregivers’ mental health only marginally predicted sleep routines for caregivers with a higher sense of purpose (B= −.16, SE = .09, p < .10). The effects sizes were also larger for caregivers with a low (β = −.46), rather than those with a high (β = −.14), sense of purpose. Second, sleep routines moderately and positively predicted acting out among caregivers with a low sense of purpose (B = .10, SE = .03, p < .001, β = .44), but not among caregivers with a high sense of purpose. Finally, we found a small, negative trend of sleep routines on children’s positive behaviors among caregivers with a low (B = −.09, SE = .05, p < .10, β = −.21) but not high, sense of purpose.
Discussion
Research has robustly demonstrated the negative effects of financial strain and poor mental health on parenting practices and child outcomes (Carter et al., 2001; Claessens et al., 2015; Priel et al., 2019). The COVID-19 pandemic is resulting in many families experiencing job loss, economic strain (Barrero, Bloom, & Davis, 2020), and mental health challenges (Brown et al., 2020; Fitzpatrick, Harris, & Drawve, 2020), which our data demonstrate as well. Although a unique time in history, our data fit the Family Stress Model (Conger et al., 2000; Masarik & Conger, 2017) well, with financial strain significantly related to parents’ poor mental health, inconsistent sleep routines and changes in children’s behavior. Parental mental health was significantly related to changes in children’s behaviors, specifically more acting out (e.g., crying and tantrums) and poor emotional coping (e.g., changes in eating and sleeping patterns), and increased positive behaviors. Such findings align with emerging research in the United States and other countries that have implemented social-distancing policies, where parents report struggles with mental health (Fontanesi et al., 2020; Lawson et al., 2020; Romero, López-Romero, Domínguez-Álvarez, Villar, & Gómez-Fraguela, 2020). This is especially concerning given the relationship between parental burn-out, stress, and child maltreatment (Griffith, 2020; Lawson et al., 2020).
Previous research on natural disasters find acute increases in stress, anxiety, and depression as well as persistent mental health problems well after the disaster has resolved (Freedy, Saladin, Kilpatrick, Resnick, & Saunders, 1994; Norris, Perilla, Riad, Kaniasty, & Lavizzo, 1999) and that such psychological distress is associated with changes in parenting quality and child wellbeing (Cobham & McDermott, 2014; Felix, You, Vernberg, & Canino, 2013; Takahiro et al., 2019). The COVID-19 pandemic is a different type of natural disaster, with differential impacts on families’ employment, feelings of social isolation and purpose, and coping. As such, it is not surprising that patterns of family stress differ across our sample.
Interestingly, caregivers who reported more financial strain, poor mental health, and low sense of purpose also reported that their children displayed more helping and affectionate behaviors since the pandemic began. Studies with adolescents have found similar patterns in which financial strain and parental stress predict greater prosocial behavior (Carlo, Padilla-Walker, & Day, 2011; Tsai, Telzer, Gonzales, & Fuligni, 2013), which authors have attributed to youth’s desire to reduce family strain and support interpersonal trust, intimacy, and social competence (Carlo et al., 2011; Davis, Carlo, & Crockett, 2020; Davis, Carlo, Streit, & Crockett, 2018). Those studies focused exclusively on Latine families and our largely Latine (59%) sample suggest there may be important cultural differences for how families cope with stress and ways in which children can be more resilient. More research should explore these patterns. Given the high prevalence of prosocial behavior in early childhood (Thompson & Newton, 2012), it is possible that young children are more likely to help when they are aware that their caregivers are experiencing financial and affective strain.
Limitations
This study has some notable limitations. First, this was a cross-sectional survey study; thus, the direction of effects may be inverse to those posited or caused by other, unmeasured variables. Next, in order to collect data anonymously, we did not ask about the reason for the emergency visit, as some reasons (e.g., abuse and COVID-19 diagnosis) may have prevented participants from remaining anonymous. This limited our ability to assess how COVID-19 exposure might have related to family stressors and outcomes. Additionally, we only measured family sleep routines as a parenting behavior and a small set of child behaviors, given the need for brevity and anonymity. Future research should explore how family stressors contribute to other forms of parenting and children’s development. Last, generalizability should be considered as responses from caregivers in California may not represent caregivers in other regions of the country. Furthermore, caregivers who seek emergency medical attention for their child may differ from those who do not.
Conclusion
The COVID-19 pandemic is affecting families differently, with some having little to no change in financial security and others feeling high levels of financial strain. Some caregivers are struggling with heightened stress, depression, and anxiety, while others are not. Most children are doing well, with no increase in concerning behavior and notable increases in displays of affection and helpfulness. However, a sizable proportion of children are exhibiting undesirable changes in behavior. The risk for such behavioral difficulties is significantly related to caregivers’ mental health and financial strain. Thus, professionals concerned with family functioning should talk with caregivers about their feelings, connect them with resources, and pay attention to behavioral problems that arise during this unprecedented time. Because having a high sense of purpose seems to moderate the relationship between caregiver strain and child outcomes, efforts should be made to help caregivers focus on the valuable role they play in the lives of others (e.g., caring for children and keeping the family safe and healthy). Further, in some families with these contextual and individual stressors, children are demonstrating more affectionate and helpful behaviors. Investigating such patterns could offer insights into what helps children be more resilient. Our findings suggest that providing support for financial needs and mental health may help families to thrive during this challenging time.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Partial funding provided by the National Institute of Child Health and Human Development (#R01HD078547).
ORCID iD
Stephanie M. Reich https://orcid.org/0000-0002-8799-5236
References
- Barrero J., Bloom N., Davis S. (2020). COVID-19 is also a reallocation shock. Cambridge, MA: National Bureau Of Economic Research. Retrieved fromhttps://www.nber.org/papers/w27137 [Google Scholar]
- Brand J. (2015). The far-reaching impact of job loss and unemployment. Annual Review of Sociology, 41, 359–375. 10.1146/annurev-soc-071913-043237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan P. A., Hammen C., Andersen M. J., Bor W., Najman J. M., Williams G. M. (2000). Chronicity, severity, and timing of maternal depressive symptoms: relationships with child outcomes at age 5. Developmental Psychology, 36, 6. 10.1037//0012-1649.36.6.759 [DOI] [PubMed] [Google Scholar]
- Brown S., Doom J., Lechuga-Peña S., Watamura A., Koppels T. (2020). Stress and parenting during the global COVID-19 pandemic. Child Abuse & Neglect, 110(2), 104699. 10.1016/j.chiabu.2020.104699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlo G., Padilla-Walker L., Day R. (2011). A test of the economic strain model on adolescents’ prosocial behaviors. Journal of Research in Adolescence, 21(4), 842–848. 10.1111/j.1532-7795.2011.00742.x [DOI] [Google Scholar]
- Carter A.-S., Garrity-Rokous F. E., Chazan-Cohen R., Little C., Briggs-Gowan M.-J. (2001). Maternal depression and comorbidity: Predicting early parenting, attachment security, and toddler social-emotional problems and competencies. Journal of the American Academy of Child and Adolescent Psychiatry, 40(1), 18–26. 10.1097/00004583-200101000-00012 [DOI] [PubMed] [Google Scholar]
- Claessens A., Engel M., Curran C. (2015). The effects of maternal depression on child outcomes during the first years of formal schooling. Early Childhood Research Quarterly, 32, 80–93. 10.1016/j.ecresq.2015.02.003 [DOI] [Google Scholar]
- Cobham V., McDermott B. (2014). Perceived parenting change and child posttraumatic stress following a natural disaster. Journal of Child and Adolescent Psychopharmacology, 24(1), 18–23. 10.1089/cap.2013.0051 [DOI] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Conger K., Rueter M., Conger R. (2000). The role of economic pressure in the lives of parents and their adolescents: The Family Stress Model. In Crockett L. J., Silbereisen R. K. (Eds.), Negotiating adolescence in times of social change (pp. 201–223). New York, NY: Cambridge University Press. [Google Scholar]
- Conners-Burrow N., Bokony P., Whiteside-Mansell L., Jarret D., Kraleti S., McKelvey L., Kyzer A. (2014). Low-level depressive symptoms reduce maternal support for child cognitive development. Journal of Pediatric Health Care, 28(5), 404–412. 10.1016/j.pedhc.2013.12.005 [DOI] [PubMed] [Google Scholar]
- Davis A., Carlo G., Crockett L. J. (2020). The role of economic stress in parents’ depression and warmth. Peace and conflict: Journal of Peace Psychology, 26, 162–170. 10.1037/pac0000406 [DOI] [Google Scholar]
- Davis A., Carlo G., Streit C., Crockett L. (2018). Considering economic stress and empathic traits in predicting prosocial behaviors among U.S. Latino adolescents. Social Development, 27(1), 58–72. 10.1111/sode.12249 [DOI] [Google Scholar]
- Dijkstra-Kersten S. M. A., Biesheuvel-Leliefeld K. E. M., Wouden J. C. V. d., Penninx B. W. J. H., Marwijk H. W. J. V. (2015). Associations of financial strain and income with depressive and anxiety disorders. Journal of Epidemiological Community Health, 69, 660–665. 10.1136/jech-2014-205088 [DOI] [PubMed] [Google Scholar]
- Dwivedi K. (2000). Enhancing parenting skills. In Murray M., Reed C. (Eds.), Promotion of mental health (Vol. 7). NY, NY: Routledge. [Google Scholar]
- Felix E., You S., Vernberg E., Canino G. (2013). Family influences on the long term post-disaster recovery of puerto rican youth. Journal of Abnormal Child Psychology, 41, 111–124. 10.1007/s10802-012-9654-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field T. (2011). Prenatal depression effects on early development: A review. Infant Behavior & Development, 34, 1–14. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick K., Harris C., Drawve G. (2020). Fear of COVID-19 and mental health consequences in America. Psycholoigcal Trauma: Theory, Research, Practice, and Policy, 12(S1), S7–S21. 10.1037/tra0000924 [DOI] [PubMed] [Google Scholar]
- Fontanesi L., Marchetti D., Mazza C., Di Giandomenico S., Roma P., Verrocchio M. (2020). The effect of the COVID-19 lockdown on parents: A call to adopt urgent measures. Psychological Trauma: Theory, Research, Practice, and Policy, 12, S79–S81. 10.1037/tra0000672 [DOI] [PubMed] [Google Scholar]
- Freedy J. R., Saladin M. E., Kilpatrick D. G., Resnick H. S., Saunders B. E. (1994). Understanding acute psychological distress following natural disaster. Journal of Traumatic Stress, 7(2), 257–273. [DOI] [PubMed] [Google Scholar]
- Golberstein E., Gonzales G., Meara E. (2016). Economic conditions and children’s mental health. Cambridge, MA: National Bureau of Economic Research. [Google Scholar]
- Goodman S., Rouse M., Connell A., Broth M., Hall C., Heyward D. (2011). Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review, 14, 1–27. 10.1007/s10567-010-0080-1 [DOI] [PubMed] [Google Scholar]
- Griffith A. (2020). Parental burnout and child maltreatment during the COVID-19 pandemic. Journal of Family Violence. Online ahead of print, 1–7. 10.1007/s10896-020-00172-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimm K. J., Ram N., Estabrook R. (2016). Growth modeling: Structural equation and multilevel modeling approaches (Vol. 24). New York, NY: Guilford Press. [Google Scholar]
- Hertz-Palmor n., Moore T., Gothelf G., DiDomenico G., Dekel I., Greenberg D., Barzilay R. (2021). Association among income loss, financial strain and depressive symptoms during COVID-19: Evidence from two longitudinal studies. Journal of Affective Disorders, 291, 1–8. 10.1016/j.jad.2021.04.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill P., Sin N., Turiano N., Burrow A., Almeida D. (2018). Sense of purpose moderates the associations between daily stressors and daily well-being. Annals of Behavioral Medicine, 52(8), 724–729. 10.1093/abm/kax039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homan K., Kong J. (2020). Longitudinal health consequences of child adversity: The mediating role of purpose in life. Journal of Gerontoloical Social Work. Online Pre-Release. 10.1080/01634372.2020.1808140 [DOI] [PubMed] [Google Scholar]
- Inagaki T., O’rehek E. (2017). On the benefits of giving social support: When, why, and how support providers gain by caring for others. Current Directions in Psychological Science, 26(2), 109–113. 10.1177/0963721416686212 [DOI] [Google Scholar]
- Jackson A. P., Brooks-Gunn J., Huang C., Glassman M. (2000). Single mothers in low-wage jobs: Financial strain, parenting, and preschoolers’ outcomes. Child Development, 71(5), 1409–1423. 10.1111/1467-8624.00236 [DOI] [PubMed] [Google Scholar]
- Kramer A., Kramer J. Z. (2020). The potential impact of the COVID-19 pandemic on occupational status, work from home, and occupational mobility. Journal of Vocational Behavior, 119, 103442. 10.1016/j.jvb.2020.103442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R., Williams J., Löwe B. (2009). An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics, 50(6), 613–621. 10.1176/appi.psy.50.6.613 [DOI] [PubMed] [Google Scholar]
- Lawson M., Piel M., Simon M. (2020). Child maltreatment during the COVID-19 pandemic: Consequences of parental job loss on psychological and physical abuse towards children. Child Abuse & Neglect. Pre-release online version. 10.1016/j.chiabu.2020.104709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little T. D. (2013). Longitudinal structural equation modeling. New Jersey, NJ: Guilford Press. [Google Scholar]
- Malin H., Morton E., Nadal A., Smith A. N. (2019). Purpose and coping with adversity: A repeated measures, mixed-methods study with young adolescents. Journal of Adolescence, 76, 1–11. 10.1016/j.adolescence.2019.07.015 [DOI] [PubMed] [Google Scholar]
- Marcil L., Campbell J., Silva K., Hughes D., Salim S., Nguyen K., Kistin C. (2020). Women’s experiences of the effect of financial strain on parenting and mental health. Journal of Obstetric, Gynecologic & Neonatal Nursing. Online Pre-lease. 10.1016/j.jogn.2020.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masarik A., Conger R. (2017). Stress and child development: A review of the Family Stress Model. Current Opinion in Psychology, 13, 85–90. 10.1016/j.copsyc.2016.05.008 [DOI] [PubMed] [Google Scholar]
- Muthén L. K., Muthén B. O. (1998–2017). Mplus user’s guide (8th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Neppl T., Senia J., Donnellan M. (2016). Effects of economic hardship: Testing the family stress model over time. Journal of Family Psychology, 30, 12–21. 10.1037/fam0000168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nievar M., Moske A., Johnson D., Chen Q. (2014). Parenting practices in preschool leading to later cognitive competence: A family stress model. . Early Education & Development, 25, 318–337. 10.1080/10409289.2013.788426 [DOI] [Google Scholar]
- Norris F. H., Perilla J. L., Riad J. K., Kaniasty K., Lavizzo E. A. (1999). Stability and change in stress, resources, and psychological distress following natural disaster: Findings from hurricane Andrew. Anxiety, Stress & Coping, 12(4), 363–396. 10.1080/10615809908249317 [DOI] [PubMed] [Google Scholar]
- Prickett K. (2020). Mothers’ job loss and their sensitivity to young children’s development. Child Development. Online pre-release. 10.1111/cdev.13398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Priel A., Djalovski A., Zagoory-Sharon O., Feldman R. (2019). Maternal depression impacts child psychopathology across the first decade of life: Oxytocin and synchrony as markers of resilience. Journal of Child Psychology and Psychiatry, 60(1), 30–42. 10.1111/jcpp.12880 [DOI] [PubMed] [Google Scholar]
- Romero E., López-Romero L., Domínguez-Álvarez B., Villar P., Gómez-Fraguela J. A. (2020). Testing the effects of COVID-19 confinement in Spanish children: The role of parents’ distress, emotional problems and specific parenting. International Journal of Environmental Research and Public Health, 17, 6975–6998. 10.3390/ijerph17196975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryff C. (1989). Happiness is everything, or is it? Explorations on the meaning of psychological well-being. Journal of Personality and Social Psychology, 57(6), 1069–1081. [Google Scholar]
- Scaramella L. V., Sohr-Preston S. L., Callahan K. L., Mirabile S. P. (2008). A test of the family stress model on toddler-aged children's adjustment among hurricane Katrina impacted and nonimpacted low-income families. Journal of Clinical Child & Adolescent Psychology, 37(3), 530–541. 10.1080/15374410802148202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahiro M., Takeo F., Junko Y., Hiroaki H., Hirobumi M., Keizo N., Makiko O. (2019). Impact of parenting style on clinically significant behavioral problems among children aged 4–11 years old after disaster: A follow-up study of the great East Japan earthquake. Frontiers in Psychiatry, 10, 45. 10.3389/fpsyt.2019.00045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan T., Wang Y., Ruggerio A. (2017). Childhood adversity and children’s academic functioning: Roles of parenting stress and neighborhood support. Journal of Child and Family Studies, 26, 2742–2752. 10.1007/s10826-017-0775-8 [DOI] [Google Scholar]
- Telleen S., Herzog A., Kilbane T. (1989). Impact of a family support program on mothers’ social support and parenting stress. American Journal of Orthopsychiatry, 59(3), 410–419. 10.1111/j.1939-0025.1989.tb01676.x [DOI] [PubMed] [Google Scholar]
- Thompson R., Newton E. (2012). Baby altruists? Examining the complexity of prosocial motivation in young children. Infancy, 18(1), 120–133. 10.1111/j.1532-7078.2012.00139.x [DOI] [Google Scholar]
- Tsai K., Telzer E., Gonzales N. A., Fuligni A. (2013). Adolescents' daily assistance to the family in response to maternal need. Journal of Marriage and Family, 75(4), 964–980. 10.1111/jomf.12035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voydanoff P. (1984). Economic distress and families: Policy issues. Journal of Family Issues, 5(2), 273–288. [Google Scholar]
- Wilson J., Lee J., Fitzgerald H., Oosterhoff B., Sevi B., Shook N. (2020). Job insecurity and financial concern during the COVID-19 pandemic are associated with worse mental health. Journal of Occupational and Environmental Medicine, 62(9), 686–691. 10.1097/JOM.0000000000001962 [DOI] [PubMed] [Google Scholar]