Dear Editor,
Erlotinib is an epidermal growth factor receptor (EGFR) inhibitor used in the treatment of non-small cell lung cancer. Common side effects of erlotinib include rash and diarrhea, while eyelash trichomegaly and hair disorder are rarely reported, and corneal ulcer is less than 0.1%[1]. To our best knowledge, this the first such case so far. The patient developed metastasis during the treatment with erlotinib in pulmonary carcinoma. The clinical manifestations were peripheral corneal ulcer and eyelash trichomegaly. The patient successfully underwent epilation, bandage contact lens, topical steroid and lubrication therapy. Subsequently, the patient developed herpes simplex virus epithelial keratitis and acute anterior uveitis (AAU).
This case report was approved by Kiang Wu Hospital. Written informed consent to participate and publication was obtained from the patient. The study was conducted in accordance with the principles of the Declaration of Helsinki.
CASE REPORT
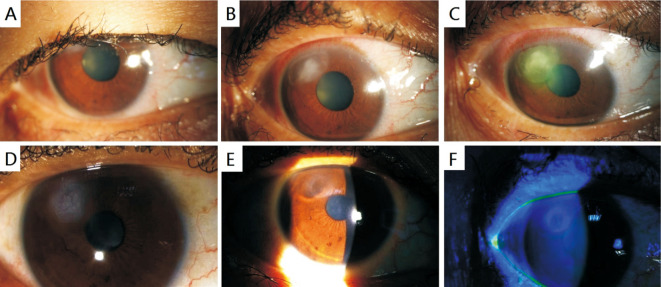
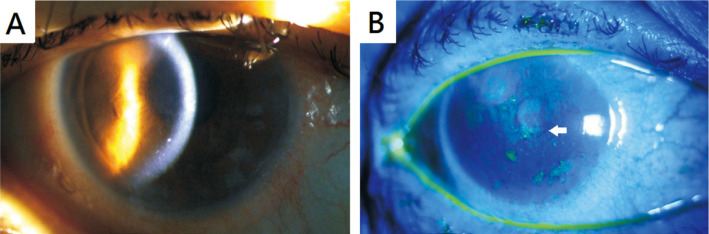
A 52-year-old female have received the treatment with Erlotinib due to the bone metastasis originated from pulmonary carcinoma for about half a year, presenting with eyelash trichomegaly (Figure 1A). She complained of mild foreign body sensation without redness, pain, photophopia and ocular discharge in her right eye. No history of eye disease, contact len use or autoimmune disease. Slit-lamp examination showed mild conjunctival injection. Peripheral corneal ulcer occurred on the cornea at around 11 o'clock, and was separated from it at lucid interval in the right eye (Figure 1B). Her intensely matted clumped eyelashes would contact to the corneal ulcer. Blood investigatins revealed white blood cell count: 3.17×109/L and hemoglobin: 106 g/L. Urine, liver and kidney function were normal. Herpes simplex virus immunoglobulin M, C-reactive protein, and erythrocyte sedimentation rate were normal with normal chest radiography. Initially, the patient was given topical antibiotics and lubrication with epilation for about 5d. However, her condition failed to respond to the treatment, the corneal ulcer expanded (Figure 1C). After stopped application of antibotic, with the addition of topical steroid, the lesion gradually shrank, but the healing process remained slow. During the follow-up, the deciduous eyelashes were found adhered to the corneal ulcer, affecting the healing of the lesion (Figure 1D). Finally, the patient successfully underwent epilation, bandage contact lens, topical steroid and lubrication treatment without discontinuing erlotinib (Figure 1E, 1F). However, 3wk after the recovery from corneal ulcer, the patient developed dendritic epithelial ulcer and AAU. The dendritic epithelial ulcer was located in the center of the cornea, AAU was accompanied with granulomatous and small keratic precipitates (Figure 2B), and mild inflammation occurred in the anterior chamber. After oral and topical antiviral drugs, dendrite keratopathy (Figure 2A) reduced and recovered. AAU improved after 2mo of topical steroid treatment.
Figure 1. The slit-lamp examination.
A: There was mild conjunctival hyperaemia and eyelash trichomegaly; B: At 11 o'clock, there was a corneal infiltration and epithelial defect; C: After 5d treatment without topical sterioid application, the corneal ulcer was expanded; D: During treatment, detached eyelashes are sometimes observed adhering to corneal ulcer; E: After bandage contact lens and topical steroid, the corneal epithelium regenerated and the defect became scarred; F: The corneal epithelium was not stained with fluorescein.
Figure 2. The slit-lamp photography.
A: Herpes simplex virus acute anterior uveitis with granulomatous and small keratic precipitates; B: After antiviral treatment, fluroescein-stained cornea: dendritic corneal epithelial lesions (white arrow) were reduced until complete recovery.
DISCUSSION
Erlotinib is a tyrosine kinase inhibitor of EGFR. EGFR is widely expressed on the ocular surface and periocular adnexa. Systemic administration of EGFR inhibitors may therefore lead to adverse reactions to ocular epithelial tissue regeneration and periocular adnexa. Clinically reported ocular adverse reactions of erlotinib include eyelash trichomegaly[2], blepharitis, corneal epithelial defect[3], infectious corneal ulcer[1],[4], and even corneal perforation[4]. Symptoms of eyelash trichomegaly include curly, irregular, excessively long and brittle eyelashes. In our case, the factors of corneal ulcer formation were considered as follows: A: Erlotinib inhibited corneal epithelial regeneration and healing; B: Matted clumped eyelashes in contact with cornea can cause mechanical injury. Interestingly, brittle eyelash will adhere to corneal lesions and interfere with the healing of corneal ulcer. In this case, despite of epilation, antibiotics and artificial tears, the lesion of the patient remained enlarged, but she was then cured through epilation, bandage contact lens, topical steroids and artificial tears without discontinuing erlotinib. Although discontinuing erlotinib and topical medicine have been reported to be capable of curing keratopathy in several literatures[1],[5], the progression of the primary disease may be prompted instead. Erlotinib is not considered to be the cause of advanced herpes simplex virus epithelial keratitis and AAU. Probably, the compromised immune system of carcinoma patient may lead to the underlying viral attack. Consequently, the significance of the potential peripheral corneal ulcer in patients treated with erlotinib should be highlighted in ophthalmologists. In addition, bandage contact lens and topical steroid may be conducive to the healing of such corneal ulcer, despite the continuous administration of erlotinib.
Acknowledgments
Conflicts of Interest: Tam KM, None; Lai IF, None.
REFERENCES
- 1.Tamura M, Takai Y, Nakamura S, Ohira A. A case report of pseudo-exfoliation syndrome with prolonged corneal epithelial regeneration because of erlotinib-induced unilateral corneal ulcer and anterior uveitis. Acta Ophthalmol. 2020;98(8):e1055–e1056. doi: 10.1111/aos.14454. [DOI] [PubMed] [Google Scholar]
- 2.Hutchison DM, Duffens A, Yale K, Park A, Cardenas K, Mesinkovska NA. Eyelash trichomegaly: a systematic review of acquired and congenital aetiologies of lengthened lashes. J Eur Acad Dermatol Venereol. 2022;36(4):536–546. doi: 10.1111/jdv.17877. [DOI] [PubMed] [Google Scholar]
- 3.Johnson KS, Levin F, Chu DS. Persistent corneal epithelial defect associated with erlotinib treatment. Cornea. 2009;28(6):706–707. doi: 10.1097/ICO.0b013e31818fdbc6. [DOI] [PubMed] [Google Scholar]
- 4.Sobol EK, Ahmad S, Ibrahim K, Alfaro C, Pakett J, Esquenazi K, Della Rocca D, Ginsburg R. Rapidly progressive streptococcus dysgalactiae corneal ulceration associated with erlotinib use in stage IV lung cancer. Am J Ophthalmol Case Rep. 2020;18:100630. doi: 10.1016/j.ajoc.2020.100630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kau HC, Tsai CC. Erlotinib-related keratopathy in a patient underwent laser in situ keratomileusis. Cutan Ocular Toxicol. 2016;35(3):257–259. doi: 10.3109/15569527.2015.1072546. [DOI] [PubMed] [Google Scholar]