ABSTRACT
Cervical laminoplasty is a safe and effective treatment for cervical myelopathy. However, it has a higher frequency of postoperative axial pain than other methods. A variety of causes of postoperative axial pain have been reported, but these have not been fully elucidated. This study aimed to investigate the association between postoperative axial pain and changes in the posterior neck muscles before and after surgery. The study included 93 patients with cervical myelopathy who underwent surgery at our institute between June 2010 and March 2013. The patients with greater preoperative and 1-year postoperative neck pain visual analog scale scores comprised the neck pain group. The cross-sectional area of the cervical posterior extensor muscles and the trapezius muscle were measured by magnetic resonance imaging before and 1 year after surgery at the C3/4, C4/5, and C5/6 levels to compare with neck pain. The total cross-sectional area atrophy rate (C3/C4, C4/C5, and C5/C6) of the trapezius muscle was significantly larger in patients with neck pain (12.8 ± 13.2) than in those without (6.2 ± 14.4; p<0.05). The cross-sectional area atrophy rate of the trapezius muscle at only the C5/6 level was significantly higher in patients with neck pain (16.7 ± 11.7) compared to those without (3.3 ± 14.4; p<0.001). No significant differences were found in the cross-sectional areas of the cervical posterior extensor muscles. Trapezius atrophy, especially at the lower cervical vertebrae, was associated with neck pain after cervical laminoplasty.
Key Words: trapezius muscle, neck pain, cervical myelopathy, cervical laminoplasty, cross-sectional areas
INTRODUCTION
Degenerative cervical myelopathy (DCM) is the most common cause of spinal cord dysfunction in the elderly.1 Chronic spinal cord compression is caused by degeneration of the cervical spine, such as spondylolisthesis, herniated discs, and ossification of the posterior longitudinal ligament. This disease usually progresses slowly and in stages, with gradually worsening symptoms such as gait abnormalities, muscle weakness, and sensory changes.2 For patients with severe or progressive symptoms, current clinical practice recommends surgical decompression to reverse further neurological deterioration.3,4
Cervical laminoplasty is a widely used surgical technique to treat DCM. Laminoplasty provides safe and effective posterior decompression for multistage lesions while preserving the posterior elements of the cervical spine. Postoperative complications of laminoplasty have been reported, including C5 palsy, axial pain, motor deficits, and loss of lordosis. Recent meta-analyses have shown that in the treatment of multilevel cervical myelopathy, the incidence of surgery-related complications after laminoplasty is significantly lower after laminectomy with fusion than after anterior decompression and fusion5,6; however, laminoplasty tends to have a higher frequency of postoperative axial pain compared to other surgeries.6,7 Hosono et al8 have previously reported a significantly higher incidence of neck pain in patients who underwent laminoplasty compared with those who underwent anterior fusion (60% and 19%, respectively). Postoperative axial neck pain occurred in 26% of patients who underwent laminoplasty, had persisted for an average of 5.5 months, and was reduced within 1 to 1.5 years postoperatively.
Although axial pain is not a major symptom of DCM, preventing axial pain may play a key role in improving surgical outcomes, as persistent axial pain can have a significant negative impact on the patient’s quality of life.9
Many prior studies have investigated the causes of axial pain after laminoplasty.8,10 Recently, some studies have reported that the muscles attached to C2 or C7, such as the posterior deep extensor and trapezius muscles, are related to postoperative axial pain.10-12 However, it is not known which muscles actually change from pre-operation to post-operation, or to what extent. Regarding residual neck pain, gaining an understanding of which muscles are atrophied may be useful in predicting the surgical procedure, preoperative planning, and postoperative rehabilitation. Thus, in this study, we sought to investigate the association between postoperative axial pain and changes in the posterior neck muscles before and after surgery. To achieve our aim, we measured the area of the posterior deep extensor and trapezius muscles before and after laminoplasty and investigated their relationship with neck pain.
MATERIALS AND METHODS
This study was conducted in compliance with the principles of the Declaration of Helsinki, with the approval of the Research Ethics and Conflicts Committee of the authors’ affiliated institution. All participants provided informed consent for participation in the study.
Participants
Individuals who underwent double-door laminoplasty using hydroxyapatite spacers for cervical myelopathy at our institute were consecutively enrolled from June 2010 to March 2013. The diagnosis of myelopathy was confirmed with a thorough neurological examination and the imaging findings of spinal cord compression, which were generally associated with an intramedullary high-intensity area on T2-weighted magnetic resonance imaging (MRI). Spinal surgeons at our institute determined the surgical indications based on the symptoms and medical images of patients with cervical myelopathy.
The surgical procedure for conventional double-door laminoplasty has previously been described in detail.13 Midline spinous processes were split with a high-speed burr under microscopy. Hydroxyapatite spacers (Apacerum; Asahi Optical Co, Ltd, Tokyo, Japan) were placed between the split laminae and fixed with non-absorbable sutures to maintain an enlarged spinal canal. Patients wore a cervical orthosis for 2 weeks after surgery.14
The surgery was performed at the C3-C7 level in which stenosis was noted. The inclusion criteria were as follows: patients who underwent C3-C6, C3-C7, C4-C6, and C4-C7 laminoplasty. The exclusion criteria were as follows: those who had undergone prior cervical spine surgery, and individuals for whom we could not obtain preoperative and 1-year postoperative visual analogue scale (VAS) scores and MRI.
Measurements
We evaluated neck pain using the VAS scores obtained preoperatively and 1 year postoperatively. Patients with greater postoperative VAS scores compared with preoperative scores were defined as the prolonged postoperative neck pain group.
We assessed the cervical posterior extensor muscles and trapezius muscle mass using a 1.5-T MRI scanner. Axial T2-weighted slices at the C3/C4, C4/C5, and C5/C6 intervertebral levels were obtained to measure the cross-sectional area (CSA) of the cervical posterior extensor muscles (multifidus, semispinalis cervicis, semispinalis capitis, splenius capitis, and trapezius muscles) (Fig. 1). The CSAs of these muscles, measured using area calculation software (SYNAPSE; Fujifilm Medical, Tokyo, Japan) and obtained from the right and left sides were combined for each participant. Measurements of the CSAs were conducted by one investigator who manually traced the defined region of interest within the fascial border of each muscle (bilaterally) on the T2-weighted images. The measurement was repeated twice, and the results were averaged. To assess the intra- and interobserver error, five randomly chosen MR images were measured independently by the first investigator, and again by a second investigator.15 In addition, we calculated each muscle’s CSA atrophy rate as follows: (preoperative CSA – postoperative CSA)/preoperative CSA×100.
Fig. 1.
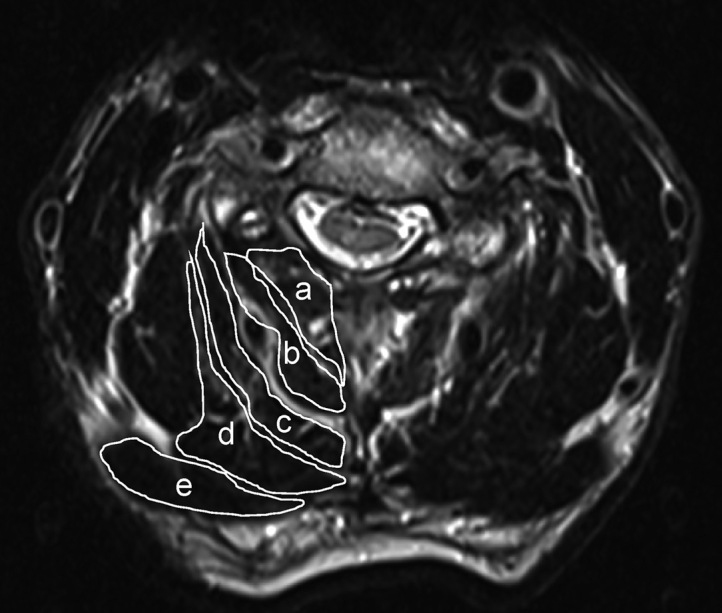
Using preoperative MRI, the cross-sectional areas of the trapezius muscle at C3-4, C4-5 and C5-6 intervertebral levels were measured on T2-weighted axial images
a: multifidus
b: semispinalis cervicis
c: semispinalis capitis
d: splenius capitis
e: trapezius
We assessed the Japanese Orthopaedic Association (JOA) score, cervical lordosis, and range of motion on radiographs preoperatively and 1 year postoperatively. Cervical lordosis was defined as the Cobb angle from C2 to C7 (C2-7 angle), which was defined as the angle between the inferior endplates of C2 and C7 on standing lateral radiographs. Range of motion was defined as follows: the C2-7 angle in extension position – the C2-7 angle in the flexion position.
Statistical analysis
Participant demographics, follow-up duration, JOA score, cervical lordosis, and range of motion measurements on radiographs were compared between patients with and without neck pain using a chi-squared test or Student’s t-test, as appropriate. The muscle mass of the cervical posterior extensor muscles, trapezius muscles were compared between patients with and without neck pain using the analysis of covariance (ANCOVA) adjusted for BMI. Logistic regression analysis was used to examine the risk factors of neck pain and was performed for items that were significantly different (p-value <0.05) on univariate analysis. Each analysis was performed separately for patients under 65 years of age (non-elderly) and those over 65 years of age (elderly). SPSS Statistics 22 software (IBM, Armonk, NY) was used for data aggregation and analyses with p < 0.05 indicating statistical significance.
RESULTS
Our study included 93 participants who had undergone surgery for cervical myelopathy between June 2010 and March 2013. The average age at the time of surgery was 72.6 ± 8.7 years. Thirty patients underwent C3-C6 laminoplasty, thirty-six underwent C3-C7 laminoplasty, eight underwent C4-C6 laminoplasty, and nineteen underwent C4-C7 laminoplasty. There were 29 participants with neck pain and 64 without. No significant differences were observed between groups regarding sex, age, height, body weight, preoperative range of motion, preoperative cervical lordosis, JOA score, or the CSAs of the cervical posterior extensor muscles and trapezius muscle (Tables 1 and 2). The postoperative cervical range of motion was significantly narrower in patients with neck pain than in those without (neck pain, 24.3 ± 9.8; no neck pain, 30.0 ± 11.3; p < 0.05; Table 3). No significant differences were observed between groups in terms of follow-up duration, postoperative cervical lordosis, JOA score, or the CSAs of the cervical deep extensor muscles and trapezius muscle (Tables 3 and 4).
Table 1.
Preoperative demographics and clinical characteristics
| All | Neck pain (+) | Neck pain (–) | p | |
| No | 93 | 29 | 64 | |
| Male/Female | 60/33 | 19/10 | 41/23 | 0.542 |
| Age (years) | 72.6±8.7 | 72.4±8.6 | 72.6±8.8 | 0.914 |
| Height (cm) | 157.4±11.1 | 156.3±11.8 | 157.9±10.8 | 0.526 |
| Weight (kg) | 59.6±9.8 | 60.7±10.2 | 59.1±9.6 | 0.47 |
| VAS | 4.7±2.9 | 2.4±2.1 | 5.7±2.6 | <0.001 |
| Cervical ROM (degree) | 35.8±14.3 | 37.1±15.8 | 35.3±13.6 | 0.572 |
| CL (degree) | 15.7±11.4 | 15.3±7.2 | 15.8±12.9 | 0.822 |
| JOA score | 11.7±2.6 | 12±2.4 | 11.6±2.6 | 0.464 |
Values are mean ± SD for each group.
VAS: visual analog scale
Cervical ROM: cervical range of motion
CL: cervical lordosis
JOA score: Japanese Orthopaedic Association score
Table 2.
Preoperative cross-sectional area
| All | Neck pain (+) | Neck pain (-) | p | |
| All | Neck pain (+) | Neck pain (-) | p | |
| CPEMs at C3/4 level | 1918.8±431.7 | 1895.6±506 | 1929.3±397.5 | 0.73 |
| CPEMs at C4/5 level | 1844.4±374.5 | 1831.2±463 | 1850.3±330.9 | 0.821 |
| CPEMs at C5/6 level | 1792±351.6 | 1804.3±427 | 1786.5±315.2 | 0.822 |
| Total CPEMs | 5555.2±1090.1 | 5531.1±1334.4 | 5566.1±971.3 | 0.887 |
| Trapezius at C3/4 level | 201.2±81.5 | 186.9±81.5 | 207.6±81.4 | 0.26 |
| Trapezius at C4/5 level | 277.5±126.5 | 265±116.3 | 283.2±131.4 | 0.524 |
| Trapezius at C5/6 level | 605±240.4 | 568.9±211.1 | 621.3±252.5 | 0.333 |
| Total trapezius | 1083.7±351.6 | 1020.9±329.4 | 1112.1±360.2 | 0.249 |
Values are mean ± SD for each group.
The Cross-sectional area (CSA) is shown as mm2.
CPEMs: cervical posterior extensor muscles
Total: C3/4+C4/5+C5/6
Table 3.
Postoperative demographics and clinical characteristics
| All | Neck pain (+) | Neck pain (–) | p | |
| No | 93 | 29 | 64 | |
| VAS | 3.4±2.4 | 4.8±2.5 | 2.7±2.2 | <0.001 |
| Cervical ROM (degree) | 28.2±11.1 | 24.3±9.8 | 30.0±11.3 | 0.021 |
| CL (degree) | 9.2±13.6 | 6.3±10.6 | 10.5±14.6 | 0.176 |
| JOA score | 14.5±2.1 | 14±2.4 | 14.7±1.9 | 0.186 |
Values are mean ± SD for each group.
Cervical ROM: cervical range of motion
CL: cervical lordosis
JOA score: Japanese Orthopaedic Association score
Table 4.
Postoperative cross-sectional area
| All | Neck pain (+) | Neck pain (–) | p | |
| CPEMs at C3/4 level | 1909.3±450.1 | 1874.9±458.4 | 1924.9±449.1 | 0.623 |
| CPEMs at C4/5 level | 1847.9±483.8 | 1744.7±455 | 1894.7±492.7 | 0.168 |
| CPEMs at C5/6 level | 1713.7±413.3 | 1681.3±437.7 | 1728.3±404.4 | 0.614 |
| Total CPEMs | 5470.9±1270.4 | 5301±1291.3 | 5547.9±1263.5 | 0.388 |
| Trapezius at C3/4 level | 234.6±102.6 | 216.9±85.3 | 242.7±109.2 | 0.264 |
| Trapezius at C4/5 level | 298.8±126.6 | 280.2±112.3 | 307.3±132.5 | 0.343 |
| Trapezius at C5/6 level | 653.8±229.7 | 671.7±199.4 | 645.7±243.2 | 0.616 |
| Total trapezius | 1187.3±357.6 | 1168.8±328.9 | 1195.6±372.1 | 0.739 |
Values are mean ± SD for each group.
The cross-sectional area is shown as mm2.
CPEMs: cervical posterior extensor muscles
Total: C3/4+C4/5+C5/6
With respect to pre- and post-operative changes, the JOA recovery rate was significantly lower in patients with neck pain than in those without (neck pain, 40.0 ± 44.8; no neck pain, 58.3 ± 30.8; p < 0.05; Table 5). The total CSA atrophy rate (C3/C4, C4/C5, and C5/C6) of the trapezius muscle was significantly higher in patients with neck pain than in those without (neck pain, 12.8 ± 13.2; no neck pain, 6.2 ± 14.4; p < 0.05; Table 5). The CSA atrophy rate of the trapezius muscle specifically at the C5/6 level was significantly higher only in patients with neck pain (neck pain, 16.7 ± 11.7; no neck pain, 3.3 ± 14.4; p < 0.001; Table 5). No significant differences were found in the CSAs of the cervical posterior extensor muscles (Table 5).
Table 5.
Preoperative and postoperative changes
| Pre- Postoperative changes | All | Neck pain (+) | Neck pain (–) | p |
| Change in VAS (cm) | –1.3±3.5 | 2.4±2.3 | –2.9±2.6 | <0.001 |
| JOA recovery rate (%) | 52.6±36.5 | 40±44.8 | 58.3±30.8 | 0.024 |
| CSA atrophy rate (%) | ||||
| CPEMs at C3/4 level | 2.9±29.8 | 1.8±23.7 | 3.5±32.3 | 0.798 |
| CPEMs at C4/5 level | 2.4±29.1 | –3.7±18.4 | 5.2±32.6 | 0.176 |
| CPEMs at C5/6 level | –2.6±25.4 | –6.6±12.5 | –0.7±29.3 | 0.299 |
| Total CPEMs | 0.5±25.8 | –3.3±15.2 | 2.2±29.3 | 0.344 |
| Trapezius at C3/4 level | 12.1±22.8 | 16±21.8 | 10.4±23.3 | 0.276 |
| Trapezius at C4/5 level | 4.1±26.1 | 4.1±22.3 | 4.1±27.8 | 0.994 |
| Trapezius at C5/6 level | 7.5±14.9 | 16.7±11.7 | 3.3±14.4 | <0.001 |
| Total trapezius | 8.3±14.3 | 12.8±13.2 | 6.2±14.4 | 0.041 |
Values are mean ± SD for each group.
Change in VAS: postoperative VAS – preoperative VAS
JOA recovery rate: (postoperative JOA – preoperative JOA)/(17- preoperative JOA)×100
CSA atrophy rate: (preoperative CSA – postoperative CSA)/preoperative CSA×100
Total: C3/4+C4/5+C5/6
JOA score: Japanese Orthopaedic Association score
CSA: cross-sectional area
CPEMs: cervical posterior extensor muscles
VAS: visual analog scale
Logistic regression analysis was performed on the items found to be significantly different (postoperative cervical range of motion, JOA recovery rate, total CSA atrophy rate, and CSA at the C5/6 level of the trapezius muscle). Only the CSA atrophy rate at the C5/6 level of the trapezius muscle was significantly different, and was considered to be a risk factor for neck pain (p = 0.001, odds ratio 0.881, 95% confidence interval: 0.818–0.948; Table 6).
Table 6.
Logistic regression analysis for risk factors of neck pain
| β | SE | Wald | p | OR | 95%CI | |
| JOA recovery rate | -0.019 | 0.01 | 3.55 | 0.06 | 0.982 | 0.963-1.001 |
| Postoperative cervical ROM (degree) | 0.045 | 0.032 | 1.996 | 0.158 | 1.046 | 0.983-1.114 |
| CSA atrophy rate of total trapezius (%) | -0.043 | 0.026 | 2.709 | 0.1 | 0.958 | 0.909-1.008 |
| CSA atrophy rate of trapezius at C5/6 level (%) | -0.127 | 0.038 | 11.485 | 0.001 | 0.881 | 0.818-0.948 |
JOA recovery rate: Japanese Orthopaedic Association recovery rate
ROM: range of motion
CSA: cross-sectional area
SE: standard error
OR: odds ratio
95%CI: 95% confidence interval
The estimated intra-class correlation for intra-observer error was 0.840, and the inter-observer error was 0.830. The independent findings showed good agreement.
DISCUSSION
In the present study, the cervical posterior extensor muscles were not clearly associated with postoperative neck pain. Rather, decreased trapezius muscle mass, especially in the lower cervical spine, was associated with postoperative neck pain. Various studies have reported that the causes of axial pain may be postoperative complications of cervical laminoplasty.11,16-18 However, to the best of our knowledge, this study is the first to show an association between pre- and postoperative muscle mass and postoperative neck pain by MRI evaluation of muscle CSA.
One recent study reported on the effect of muscle changes on axial pain after cervical laminoplasty. Preservation of the cervical semispinalis muscles has been reported to reduce postoperative neck pain.19 In addition, it has been reported that preserving the C2, to which the cervical semispinalis muscles are attached, reduces postoperative neck pain.20 Preservation of the C7 spinous process has further been reported to reduce postoperative neck pain by preserving the attachment of the trapezius and rhomboid minor muscles to C7.12 In many instances, the midline of the trapezius muscle is also attached to C6, and preservation of this muscle is reported to reduce neck pain.21
In the present study, trapezius muscle atrophy, especially in the lower trapezius muscle, was associated with residual neck pain. Cervical semispinalis muscle atrophy was found not to play a role in this study. An imbalance between the upper and lower trapezius muscles has been reported to cause neck pain.22-25 In this study, cervical laminoplasty had damaged and atrophied the upper trapezius muscle, and the degree of atrophy was more unbalanced because a greater degree of atrophy resulted in neck pain. Decreased mobility of the cervical spine has also been reported to cause cervical pain.26,27 In this study, postoperative decreased range of motion of the cervical spine was also associated with cervical pain.
The attachment of the trapezius ranges widely from the occipital bone to the T-12 spinous process. In particular, the middle fibers of the trapezius are very strong due to the presence of a very strong tendinous component. In an anatomical study of 50 cadavers, Ono et al28 reported that the middle fibers of the trapezius are attached to the spinous process between C3 and T3, and its center was located at the C7 spinous process in more than half of the individuals. The C6 spinous process is the second longest spinous process other than C7 in the cervical region, and it plays a role as an attachment point for these muscles. In this study, atrophy of the trapezius muscle at the C5-6 level in the lower cervical area was associated with postoperative axial pain, and the middle fibers of the trapezius muscle at the lower cervical level may have played an important role in postoperative axial pain.
Preservation of the deep cervical extensor muscles does not play an important role in reducing axial neck pain after cervical laminoplasty, and these adverse effects after laminoplasty are reported to be mainly due to detachment of the C2 and C7 spinous processes.29 Similarly, cervical posterior extensor muscle mass was not associated with postoperative neck pain in the present study.
The results of this study suggest that preservation of the trapezius muscle may be desirable for the prevention of neck pain after cervical laminoplasty. One solution may be to perform lumbar spinous process-splitting laminectomy, as is performed for lumbar canal stenosis in the lumbar spine, in cervical laminoplasty.30 However, in this study, it is unclear whether muscle atrophy is a risk factor in the development of postoperative neck pain. The reason for this is that muscle atrophy may occur as a result of disuse due to the limited range of motion caused by postoperative neck pain. Therefore, future consideration and prospective investigation of such an approach may lead to a reduction in future postoperative neck pain.
This study has some limitations. We believe that our assessment of axial pain was inadequate based on several factors, including cervical pathology and psychological issues. The postoperative follow-up period of 1 year is also fairly short. There were variations in the number of cervical laminae that were operated on; nevertheless, the surgical procedure was uniform. Although the effect of cervical alignment may cause differences in the CSAs of the muscles in each individual, the rate of atrophy is calculated for each individual with respect to the pre- and postoperative comparisons. Thus, the cervical alignment is thought to be corrected.
CONCLUSION
Cervical range of motion, postoperative outcomes, and trapezius muscle atrophy, especially of the lower cervical vertebrae, are associated with neck pain after cervical laminoplasty. Trapezius atrophy, especially of the lower cervical vertebrae, is associated with postoperative neck pain.
DATA AVAILABILITY
The data used in this study are available from the corresponding author upon request.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest regarding this paper.
FUNDING STATEMENT
This work has not been supported by any specific grant from any funding agency in the public, commercial or non-profit sectors.
ACKNOWLEDGMENTS
The authors gratefully acknowledge the contributions of the clinical investigators and staff who were involved in data collection of this study.
Abbreviations
- DCM
degenerative cervical myelopathy
- MRI
magnetic resonance imaging
- VAS
visual analog scale
- CSA
cross-sectional area
- JOA
Japanese Orthopaedic Association
- C2-7 angle
Cobb angle from C2 to C7
REFERENCES
- 1.Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG. Degenerative cervical myelopathy: epidemiology, genetics, and pathogenesis. Spine (Phila Pa 1976). 2015;40(12):E675-E693. doi: 10.1097/BRS.0000000000000913. [DOI] [PubMed]
- 2.Emery SE. Cervical spondylotic myelopathy: diagnosis and treatment. J Am Acad Orthop Surg. 2001;9(6):376–388. doi: 10.5435/00124635-200111000-00003. [DOI] [PubMed]
- 3.Rhee JM, Shamji MF, Erwin WM, et al. Nonoperative management of cervical myelopathy: a systematic review. Spine (Phila Pa 1976). 2013;38(22 Suppl 1):S55-S67. doi: 10.1097/BRS.0b013e3182a7f41d. [DOI] [PubMed]
- 4.Sampath P, Bendebba M, Davis JD, Ducker TB. Outcome of patients treated for cervical myelopathy. a prospective, multicenter study with independent clinical review. Spine (Phila Pa 1976). 2000;25(6):670–676. doi: 10.1097/00007632-200003150-00004. [DOI] [PubMed]
- 5.Adogwa O, Huang K, Hazzard M, et al. Outcomes after cervical laminectomy with instrumented fusion versus expansile laminoplasty: a propensity matched study of 3185 patients. J Clin Neurosci. 2015;22(3):549–553. doi: 10.1016/j.jocn.2014.10.001. [DOI] [PubMed]
- 6.Liu X, Wang H, Zhou Z, Jin A. Anterior decompression and fusion versus posterior laminoplasty for multilevel cervical compressive myelopathy. Orthopedics. 2014;37(2):e117-e122. doi: 10.3928/01477447-20140124-12. [DOI] [PubMed]
- 7.Woods BI, Hohl J, Lee J, Donaldson W 3rd, Kang J. Laminoplasty versus laminectomy and fusion for multilevel cervical spondylotic myelopathy. Clin Orthop Relat Res. 2011;469(3):688–695. doi: 10.1007/s11999-010-1653-5. [DOI] [PMC free article] [PubMed]
- 8.Hosono N, Yonenobu K, Ono K. Neck and shoulder pain after laminoplasty. a noticeable complication. Spine (Phila Pa 1976). 1996;21(17):1969–1973. doi: 10.1097/00007632-199609010-00005. [DOI] [PubMed]
- 9.Kimura A, Endo T, Inoue H, Seichi A, Takeshita K. Impact of axial neck pain on quality of life after laminoplasty. Spine (Phila Pa 1976). 2015;40(24):E1292-E1298. doi: 10.1097/BRS.0000000000001167. [DOI] [PubMed]
- 10.Riew KD, Raich AL, Dettori JR, Heller JG. Neck pain following cervical laminoplasty: does preservation of the C2 muscle attachments and/or C7 matter? Evid Based Spine Care J. 2013;4(1):42–53. doi: 10.1055/s-0033-1341606. [DOI] [PMC free article] [PubMed]
- 11.Kato M, Nakamura H, Konishi S, et al. Effect of preserving paraspinal muscles on postoperative axial pain in the selective cervical laminoplasty. Spine (Phila Pa 1976). 2008;33(14):E455-E459. doi: 10.1097/BRS.0b013e318178e607. [DOI] [PubMed]
- 12.Hosono N, Sakaura H, Mukai Y, Fujii R, Yoshikawa H. C3-6 laminoplasty takes over C3-7 laminoplasty with significantly lower incidence of axial neck pain. Eur Spine J. 2006;15(9):1375–1379. doi: 10.1007/s00586-006-0089-9. [DOI] [PMC free article] [PubMed]
- 13.Kimura A, Seichi A, Inoue H, Hoshino Y. Long-term results of double-door laminoplasty using hydroxyapatite spacers in patients with compressive cervical myelopathy. Eur Spine J. 2011;20(9):1560–1566. doi: 10.1007/s00586-011-1724-7. [DOI] [PMC free article] [PubMed]
- 14.Kimura A, Shiraishi Y, Inoue H, Endo T, Takeshita K. Predictors of persistent axial neck pain after cervical laminoplasty. Spine (Phila Pa 1976). 2018;43(1):10–15. doi: 10.1097/BRS.0000000000002267. [DOI] [PubMed]
- 15.Okada E, Matsumoto M, Ichihara D, et al. Cross-sectional area of posterior extensor muscles of the cervical spine in asymptomatic subjects: a 10-year longitudinal magnetic resonance imaging study. Eur Spine J. 2011;20(9):1567–1573. doi: 10.1007/s00586-011-1774-x. [DOI] [PMC free article] [PubMed]
- 16.Zhang H, Lu S, Sun T, Yadav SK. Effect of lamina open angles in expansion open-door laminoplasty on the clinical results in treating cervical spondylotic myelopathy. J Spinal Disord Tech. 2015;28(3):89–94. doi: 10.1097/BSD.0b013e3182695295. [DOI] [PubMed]
- 17.Motosuneya T, Maruyama T, Yamada H, Tsuzuki N, Sakai H. Long-term results of tension-band laminoplasty for cervical stenotic myelopathy: a ten-year follow-up. J Bone Joint Surg Br. 2011;93(1):68–72. doi: 10.1302/0301-620X.93B1.24532. [DOI] [PubMed]
- 18.Fujibayashi S, Neo M, Yoshida M, Miyata M, Takemoto M, Nakamura T. Neck muscle strength before and after cervical laminoplasty: relation to axial symptoms. J Spinal Disord Tech. 2010;23(3):197–202. doi: 10.1097/BSD.0b013e3181a1a73e. [DOI] [PubMed]
- 19.Kotani Y, Abumi K, Ito M, et al. Minimum 2-year outcome of cervical laminoplasty with deep extensor muscle-preserving approach: impact on cervical spine function and quality of life. Eur Spine J. 2009;18(5):663–671. doi: 10.1007/s00586-009-0892-1. [DOI] [PMC free article] [PubMed]
- 20.Takeuchi K, Yokoyama T, Aburakawa S, et al. Axial symptoms after cervical laminoplasty with C3 laminectomy compared with conventional C3–C7 laminoplasty: a modified laminoplasty preserving the semispinalis cervicis inserted into axis (Presented at the 2004 CSRS Meeting). Spine(Phila Pa 1976). 2005;30(22):2544–2549. doi: 10.1097/01.brs.0000186332.66490.ba [DOI] [PubMed]
- 21.Mori E, Ueta T, Maeda T, Yugué I, Kawano O, Shiba K. Effect of preservation of the C-6 spinous process and its paraspinal muscular attachment on the prevention of postoperative axial neck pain in C3–6 laminoplasty. J Neurosurg Spine. 2015;22(3):221–229. doi: 10.3171/2014.11.SPINE131153. [DOI] [PubMed]
- 22.Wright EF, Domenech MA, Fischer JR Jr. Usefulness of posture training for patients with temporomandibular disorders. J Am Dent Assoc. 2000;131(2):202–210. doi: 10.14219/jada.archive.2000.0148. [DOI] [PubMed]
- 23.Page P. Shoulder muscle imbalance and subacromial impingement syndrome in overhead athletes. Int J Sports Phys Ther. 2011;6(1):51–58. [PMC free article] [PubMed]
- 24.Mekhora K, Liston CB, Nanthavanij S, Cole JH. The effect of ergonomic intervention on discomfort in computer users with tension neck syndrome. Int J Ind Ergon. 2000;26(3):367–379. doi: 10.1016/S0169-8141(00)00012-3. [DOI]
- 25.Park SH, Lee MM. Effects of lower trapezius strengthening exercises on pain, dysfunction, posture alignment, muscle thickness and contraction rate in patients with neck pain; randomized controlled trial. Med Sci Monit. 2020;26:e920208. doi: 10.12659/MSM.920208. [DOI] [PMC free article] [PubMed]
- 26.Kanchanomai S, Janwantanakul P, Pensri P, Jiamjarasrangsi W. Prevalence of and factors associated with musculoskeletal symptoms in the spine attributed to computer use in undergraduate students. Work. 2012;43(4):497–506. doi: 10.3233/WOR-2012-1387. [DOI] [PubMed]
- 27.Falla D, Jull G, Russell T, Vicenzino B, Hodges P. Effect of neck exercise on sitting posture in patients with chronic neck pain. Phys Ther. 2007;87(4):408–417. doi: 10.2522/ptj.20060009. [DOI] [PubMed]
- 28.Ono A, Tonosaki Y, Yokoyama T, et al. Surgical anatomy of the nuchal muscles in the posterior cervicothoracic junction: significance of the preservation of the C7 spinous process in cervical laminoplasty. Spine(Phila Pa 1976). 2008;33(11):E349-E354. doi: 10.1097/BRS.0b013e31817152cc. [DOI] [PubMed]
- 29.Sakaura H, Hosono N, Mukai Y, Fujimori T, Iwasaki M, Yoshikawa H. Preservation of muscles attached to the C2 and C7 spinous processes rather than subaxial deep extensors reduces adverse effects after cervical laminoplasty. Spine(Phila Pa 1976). 2010;35(16):E782-E786. doi: 10.1097/BRS.0b013e3181d34614. [DOI] [PubMed]
- 30.Watanabe K, Hosoya T, Shiraishi T, Matsumoto M, Chiba K, Toyama Y. Lumbar spinous process-splitting laminectomy for lumbar canal stenosis. Technical note. J Neurosurg Spine. 2005;3(5):405–408. doi: 10.3171/spi.2005.3.5.0405. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used in this study are available from the corresponding author upon request.


