Yamada Y. The studies on lymphatic venous anastomosis in lymphedema. Nagoya J Med Sci. 1969;32(1):1–21.
Although a considerable number of publications about the treatment of lymphedema has been appeared in recent years, an effective method for surgical treatment has not yet been established. In legs of adult mongrel dogs the author made a lymphatic venous end-to-end anastomosis with 4 to 6 evenly-spaced, interrupted sutures of No. 10-0 black tetron monofflament. All branches of the sapheneus vein were ligated and cut off to prevent venous blood inflow. Consequently the saphenous vein was transformed into a lymphatic channels. At the site of the anastomosis, the author amputated the lymphatic venous anastomosed leg and the control leg except their bones, arteries, veins and nerves and relsutured them respectively for formation of lymphedema. The author examined the relationship between lymphatic and venous pressure at rest or in the manual pumping procedures. In the present study, lymphpressure ascended abruptly during manual pumping more than venous pressure. In the amputated leg having an end-to-end anastomosis, the author succeeded to demonstrate the passage of a contrast medium through the anastomosis by indirect lymphangiography, and circumferences of the lymphatic venous anastomosed leg were less than those of the control leg. The main cause of failure of anastomosis was presence of excess granulation tissue at the anastomotic site and anastomotic disruption. By using No. 10-0 black tetron monofilament, however, the granulation was not prominent histologically. Therefore, the author applied this method to a patient with lymphedema clinically, and obtained considerable effects.
The manuscript “The studies on lymphatic venous anastomosis in lymphedema” by Yamada in 1969,1 played an extremely important role in the treatment of lymphedema by advocating direct anastomosis of lymphatic vessels, which was an active topic of research at the time. His suggested surgical technique changed the direction of lymphedema treatment and has become the established lymphedema treatment of today. This paper describes its historical significance.
Lymphedema is a condition in which the lymphatic system does not function properly and fluid containing high concentrations of protein accumulates in the interstitium instead of being collected by the lymph vessels. Lymphedema can be broadly classified into primary and secondary lymphedema and most cases are secondary. The pathogenesis of secondary lymphedema is acquired damage to the lymphatic system, which is most often infection, trauma, or treatment for tumors. Lymphedema occurs more often in the extremities than in the head and neck or trunk. Worldwide, lymphedema is most commonly caused by filariasis. However, in developed nations, including Japan, it occurs more often following treatment for malignancy, with typical cases of edema in either one upper or lower extremity after surgery. In addition, radiation therapy and chemotherapy for breast or uterine cancer are also common causes of lymphedema in many areas of the developed world.
Historically, treatment for lymphedema was primarily nonoperative physiotherapy, such as manual drainage and bandage compression. Surgical therapy included excision of the skin and subcutaneous tissue, including skin flap procedures, skin graft operations, and transfer of the omentum or part of the intestinal tract as a drainage route.2 However, these procedures were often associated with complications, such as long surgical scars, postoperative infections, inadequate wound healing, and chronic pain. The pathophysiology of lymphedema itself is relatively simple, and the most physiologic surgical approach is to drain excess lymphatic fluid into healthy lymph vessels or veins. In the 1960s, many studies were conducted on anastomosis of blood vessels that had a diameter of a few millimeters or less and, in 1968, Komatsu and Tamai reported the world’s first successful case of replantation of an amputated thumb.3 In a similar vein, anastomoses between lymphatic vessels, and between a lymphatic vessel and a vein were also studied. However, stable results were not obtained because the caliber of lymphatic vessels is usually small and their walls are extremely thin, which makes anastomosis difficult. Therefore, the focus of research was basically anastomoses of veins to lymph nodes and not lymphatic vessels.4
Yamada’s report and findings from his experiments on dog’s hind legs had a global impact. His research resulted in two important discoveries. The first was that lymphatic vessels and veins in the limbs could be anastomosed using a technique developed at the time for vascular anastomosis research, and the second was that lymphatic fluid could be drained into the venous system at these anastomosed sites. Lymphangiography that was performed two weeks after the operation confirmed the patency of the anastomoses and the lymphedema created in the dogs’ hind legs was markedly reduced. Furthermore, this surgical technique was applied to a clinical human case and the edema reduction effect lasted at least several months. The surgical procedure and results were very revealing in that they showed that lymphatic venous anastomosis, a physiological surgical approach for lymphedema, was feasible with the suture threads and needles and operating microscopes of the time.
There were no subsequent reports on lymphatic venous anastomosis for lymphedema until 1977, which is when O’Brien et al reported some clinical results.5 O’Brien’s report led to the wider use of lymphatic venous anastomosis for lymphedema worldwide and further important research on the topic. It was later discovered that, in some instances, excessive venous pressure in the veins of extremities with a caliber larger than 1 to 1.5 mm caused venous blood to flow back into the lymphatic system, and the desired effect could not be ultimately achieved.6 Interestingly, Yamada measured the levels of pressures and described this pressure gradient between the lymphatic and venous systems in his paper. Subsequent developments in surgical techniques made it possible to anastomose lymphatic and venous vessels with a caliber of 1 mm or less7 (Fig. 1), and the number of cases where this method is indicated has increased. Lymphatic venous anastomosis is now the first choice of surgery for lymphedema.
Fig. 1.
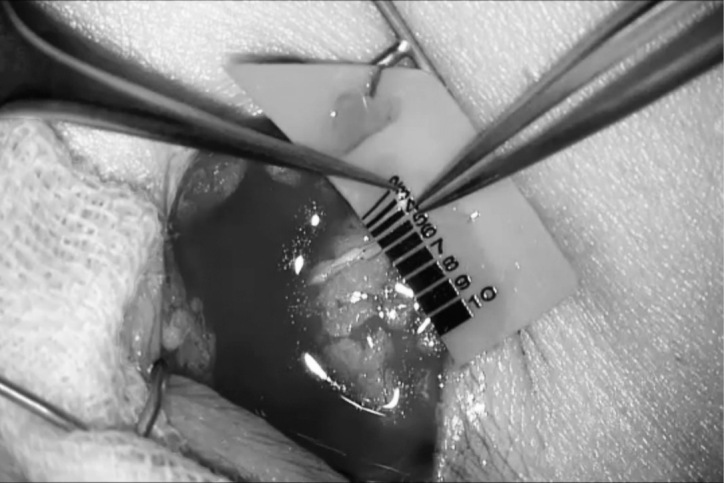
Lymphatic venous anastomosis
This figure shows a lymphatic venous anastomosis performed in the inguinal region. Each bar on the sheet represents a width of less than 1 mm. A vein with a caliber of 0.5 mm is shown on the left side of the figure, and a lymphatic vessel with a caliber of 0.5 mm is shown on the right side of the figure.
In conclusion, Yamada’s description of lymphedema was of considerable importance. His research demonstrated the feasibility of lymphedema treatment by lymphatic anastomosis and generated further international study and discussion on the topic. This had great influence on the development of new treatment methods. His research became the origin of current surgical procedures for lymphedema.
CONFLICTS OF INTEREST
The authors have no conflicts of interest associated with this article.
REFERENCES
- 1.Yamada Y. The studies on lymphatic venous anastomosis in lymphedema. Nagoya J Med Sci. 1969;32(1):1–21.
- 2.Clodius L. Lymphedema. In: McCarthy JG, ed. Plastic Surgery. Philadelphia: W.B. Saunders Company; 1990: Chapter 83.
- 3.Komatsu S, Tamai S. Successful replantation of completely cut-off thumb. Plast Reconstr Surg. 1968;42(4):374–377.
- 4.Nielubowicz J, Olszewski W. Surgical lymphaticovenous shunts in patients with secondary lymphoedema. Br J Surg. 1968;55(6):440–442. doi: 10.1002/bjs.1800550609. [DOI] [PubMed]
- 5.O’Brien BM, Sykes P, Threlfall GN, Browning FS. Microlymphaticovenous anastomoses for obstructive lymphedema. Plast Reconstr Surg. 1977;60(2):197–211. doi: 10.1097/00006534-197708000-00006. [DOI] [PubMed]
- 6.Baumeister RG, Siuda S. Treatment of lymphedemas by microsurgical lymphatic grafting: what is proved? Plast Reconstr Surg. 1990;85(1):64–74; discussion 75–76. doi: 10.1097/00006534-199001000-00012. [DOI] [PubMed]
- 7.Koshima I, Inagawa K, Etoh K, Moriguchi T. Supramicrosurgical lymphaticovenular anastomosis for the treatment of lymphedema in the extremities [in Japanese]. Nihon Geka Gakkai Zasshi. 1999;100(9):551–556. [PubMed]


