Abstract
Background
Intrauterine growth restriction (IUGR) can cause lipid disorders in infants and have long-term adverse effects on their growth and development. Clostridium butyricum (C. butyricum), a kind of emerging probiotics, has been reported to effectively attenuate lipid metabolism dysfunctions. Therefore, the objective of this study was to investigate the effects of C. butyricum supplementation on hepatic lipid disorders in IUGR suckling piglets.
Methods
Sixteen IUGR and eight normal birth weight (NBW) neonatal male piglets were used in this study. From d 3 to d 24, in addition to drinking milk, the eight NBW piglets (NBW-CON group, n = 8) and eight IUGR piglets (IUGR-CON group, n = 8) were given 10 mL sterile saline once a day, while the remaining IUGR piglets (IUGR-CB group, n = 8) were orally administered C. butyricum at a dose of 2 × 108 colony-forming units (CFU)/kg body weight (suspended in 10 mL sterile saline) at the same frequency.
Results
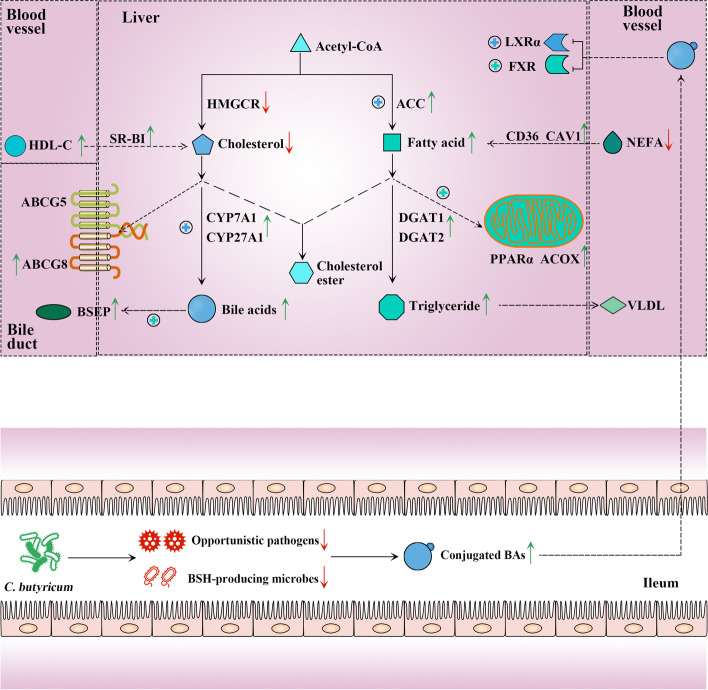
The IUGR-CON piglets exhibited restricted growth, impaired hepatic morphology, disordered lipid metabolism, increased abundance of opportunistic pathogens and altered ileum and liver bile acid (BA) profiles. However, C. butyricum supplementation reshaped the gut microbiota of the IUGR-CB piglets, characterized by a decreased abundance of opportunistic pathogens in the ileum, including Streptococcus and Enterococcus. The decrease in these bile salt hydrolase (BSH)-producing microbes increased the content of conjugated BAs, which could be transported to the liver and function as signaling molecules to activate liver X receptor α (LXRα) and farnesoid X receptor (FXR). This activation effectively accelerated the synthesis and oxidation of fatty acids and down-regulated the total cholesterol level by decreasing the synthesis and promoting the efflux of cholesterol. As a result, the growth performance and morphological structure of the liver improved in the IUGR piglets.
Conclusion
These results indicate that C. butyricum supplementation in IUGR suckling piglets could decrease the abundance of BSH-producing microbes (Streptococcus and Enterococcus). This decrease altered the ileum and liver BA profiles and consequently activated the expression of hepatic LXRα and FXR. The activation of these two signaling molecules could effectively normalize the lipid metabolism and improve the growth performance of IUGR suckling piglets.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40104-023-00828-1.
Keywords: Bile acid, Clostridium butyricum, Gut microbiota, Intrauterine growth restriction, Lipid metabolism, Suckling piglet
Background
From the moment of birth, a newborn must begin adapting to a different nutritional environment and obtaining energy from milk [1]. From d 3 to weaning, fat predominates in porcine milk. Due to its high energy value, this fat provides approximately 60% of the energy required for the growth of newborn piglets [2, 3]. Thus, a functional and efficient lipid metabolic system is crucial for the growth and development of newborns during the suckling period. However, piglets with intrauterine growth restriction (IUGR) show abnormal lipid metabolism and impaired growth performance, which severely impacts their health and results in considerable losses in animal production [4, 5]. Therefore, it is necessary to identify a method to regulate lipid metabolism in IUGR suckling piglets.
Emerging as a kind of probiotic, C. butyricum is a Gram-positive anaerobe that produces butyric acid. It is one of the earliest microbial colonizers in infants and primarily exists in the distal small intestine and colon of animals [6–8]. C. butyricum also exhibits resistance to acidic pH levels, high temperature and bile salts. Therefore, C. butyricum is regarded as a useful and safe additive [9], and previous studies have shown that it can improve growth performance, protect against pathogenic bacteria and strengthen immunity in weaned piglets [10–12].
Additionally, C. butyricum plays a role in the regulation of lipid metabolism, and this feature has been demonstrated in models of aged laying hens, high fat diet (HFD) mice and corticosterone-challenged ducks [13–15]. These previous studies showed that C. butyricum could regulate fatty acid (FA) metabolism by modifying the expression of lipogenesis-related genes, such as acetyl-CoA carboxylase (ACC), and lipolysis-related genes, such as peroxisome proliferator activated receptor alpha (PPARα) [14, 16]. C. butyricum has also been shown to modulate cholesterol metabolism by elevating the mRNA expression of CYP7A1 and CYP8B1 to increase cholesterol efflux [15]. However, it remains unclear whether C. butyricum supplementation could relieve the disordered lipid metabolism of IUGR suckling piglets.
The gut microbiota, as a crucial regulator of host metabolism, has the capacity to produce or modulate metabolites that function as metabolic substrates and signaling molecules in the host [17]. Disruptions to the gut microbiota may lead to various metabolic disorders including obesity, type 2 diabetes and malnutrition [18]. Previous studies revealed that IUGR can disturb the micro-ecological equilibrium of the gut and, as a result, negatively impact normal metabolic pathways [19, 20].
An increasing body of evidence indicates that the metabolic regulation of the gut microbiota is realized through the gut-liver axis [21], and as an important metabolite of the gut microbiota, bile acid (BA) can function as a signaling molecule and exert an impact on host metabolism [22]. During BA metabolism, the bile acid-activated receptors farnesoid X receptor (FXR) and liver X receptor (LXR) are highly expressed in the enterohepatic tissues, and both of these intracellular sensors can be activated to maintain lipid homeostasis through the gut-liver axis [23, 24]. In addition, others have shown that C. butyricum treatment can alter the BA profile of the liver and ileum and simultaneously affect the intestinal microbiota composition of the host [14, 15]. These substantial findings suggest that the addition of C. butyricum may exert an effect on BA metabolism via the gut microbiota. Nevertheless, how C. butyricum supplementation influences lipid metabolism and the gut microbiota–BA metabolism relationship still requires further exploration.
Therefore, in the present study, the aims were to determine whether C. butyricum supplementation could be an effective means of regulating lipid metabolism in IUGR piglets during the suckling period and to explore the underlying mechanism from the perspective of the gut-liver axis.
Materials and methods
Animals and experimental design
All experiments were conducted in accordance with the guidelines of the Institutional Animal Care and Use Committee of Nanjing Agricultural University. Forty healthy sows (Landrace × Yorkshire) in their third parity and with similar expected dates of confinement (≤ 3 d) were initially selected. After screening, eight sows that had similar litter sizes (12.13 ± 0.60) and met the selection criteria for IUGR were selected. The newborn piglets (Duroc × [Landrace × Yorkshire]) that weighed within 0.5 standard deviation (SD) of the mean birth weight (BW) of the littermates were defined as normal birth weight (NBW), whereas those with 2 SD lower BW were defined as IUGR [25, 26]. According to this criterion, two IUGR (0.90 ± 0.08 kg) and one NBW (1.62 ± 0.10 kg) male piglets were chosen from each sow. The sixteen IUGR and eight NBW piglets were then randomly allocated to three groups: the NBW-CON group (NBW piglets that received 10 mL sterile saline per day, n = 8), the IUGR-CON group (IUGR piglets that received 10 mL sterile saline per day, n = 8) and the IUGR-CB group (IUGR piglets that received 10 mL bacterial fluid per day, n = 8). After colostrum feeding, all piglets were randomly assigned to four sows (6 piglets/sow; NBW-CON = 2, IUGR-CON = 2, IUGR-CB = 2) with similar physiological condition for lactation. When 2 d of adaptation finished, the gavage trial was conducted from d 3 to d 24. The dose of C. butyricum in bacterial fluid was 2 × 108 CFU/kg BW, and the BW of the piglets was measured every 3 d. All piglets were kept in lactation crates and nursed by sows, and sow milk was the only available dietary sustenance for the piglets during the study.
The C. butyricum used in the study was provided by Qingdao Vland Biological Technology Co., Ltd. (Qingdao, Shandong, China). The spore count was 5 × 109 CFU/g. The strain was C. butyricum wl-53, which was initially isolated from the feces of healthy chickens and was conserved in the China Center for Type Culture Collection (CCTCC No. M2019252, Wuhan, Hubei, China).
Sample collection
Early in the morning of d 24, the piglets were weighed and the measurements were recorded as the final body weight (FBW) before blood collection. Then, blood sample was collected from the precaval vein of each piglet before sacrifice. Plasma was obtained by centrifugation at 3000 × g for 15 min at 4 °C, and stored at −80 °C for subsequent analysis. All piglets were killed by exsanguination after electrical stunning, after which fresh samples of liver and ileum chyme were immediately collected. After flushing the liver with saline, liver samples about 1 cm3 in size were collected from the left lobe and fixed in 4% paraformaldehyde solution for histological analysis. The remaining parts of the liver and the samples of chyme collected from the ileum were snap-frozen in liquid nitrogen and then stored at −80 °C for further analysis.
Histopathology
After being fixed in 4% paraformaldehyde for 24 h, the liver samples were dehydrated using an ethanol concentration gradient and then embedded in paraffin. These paraffin blocks were sliced into 5 μm sections, and the sections were stained with hematoxylin and eosin. The hepatic morphology was observed using a light microscopy (Nikon 80i, Tokyo, Japan).
Biochemical assay of serum samples
Commercial assay kits were used to determine the triglyceride (TG; #A110-1-1), nonesterified free fatty acids (NEFA; #A042-1-1), total cholesterol (TC; #A111-1-1), total bile acid (TBA; #E003-2-1), high-density lipoprotein cholesterol (HDL-C; #A112-1-1), low-density lipoprotein cholesterol (LDL-C; #A113-1-1) and glucose (GLU; #A154-1-1) content, according to the manufacturer’s instructions (Nanjing JianCheng Bioengineering Institute, Nanjing, Jiangsu, China).
Determination of hepatic metabolite concentration
Commercial assay kits were used to determine the TG (#A110-1-1), lipoprotein lipase (LPL; #A067-1-2), hepatic lipase (HL; #A067-1-2), TC (#A111-1-1), TBA (#E003-2-1) and total protein (TP; #A045-4-2) content, according to the manufacturer’s instructions (Nanjing Jiancheng Bioengineering Institute).
The 3-hydroxy-3-methylglutaryl-CoA reductase (HMGCR; #RX500243P) and very low-density lipoprotein (VLDL; #RX500284P) levels were detected using enzyme-linked immunoassay (ELISA) kits for swine from Quanzhou Ruixin Biological Technology Co., Ltd. (Quanzhou, Fujian, China), following the manufacturer’s instructions.
RNA isolation and quantitative real-time polymerase chain reaction (PCR) analysis
Total RNA was extracted from the ileum (mucosal) and liver samples using the Total RNA Extraction Reagent (Vazyme Biotechnology, Nanjing, Jiangsu, China) and quantified using an ND-2000 micro spectrophotometer (Thermo Fisher Scientific, Waltham, MA, USA). After the determination of RNA quality and concentration, 1 µg of total RNA was reverse-transcribed into complementary DNA (cDNA) using the HiScript III RT SuperMix Reagent (Vazyme Biotechnology), following the manufacturer’s instructions. The mRNA expression levels of specific genes were quantified via real-time polymerase chain reaction (PCR) using the SYBR qPCR Master Mix (Vazyme Biotechnology) and the QuantStudio 5 Real-Time PCR System (Thermo Scientific, Wilmington, DE, USA). The SYBR Green PCR reaction mixture consisted of 10 µL TB Green Premix Ex Taq, 0.4 µL ROX Reference Dye II, 2 µL cDNA template, 0.4 µL of each primer (total 0.8 µL, 10 µmol/L) and 6.8 µL of double-distilled H2O. The reaction conditions were as follows: pre-run at 95 °C for 30 s, 40 denaturation cycles at 95 °C for 10 s and annealing at 60 °C for 30 s. Each sample was run in triplicate. The relative mRNA expression levels were analyzed via the 2−ΔΔCt method after normalization against β-actin, and the results displayed a similar trend when GAPDH served as the housekeeping gene.
Protein extraction and western blot assay
TP was isolated from the frozen liver samples using a lysis buffer containing protease inhibitors (Beyotime Institute of Biotechnology, Nantong, Jiangsu, China). The protein concentration was measured using a BCA Protein Assay Kit (Beyotime Institute of Biotechnology). Equal amounts of TP (20 µg) were subjected to electrophoresis in 4%–20% SDS-PAGE and then transferred to PVDF membranes activated by methanol. After blocking with 5% fat-free dry milk in TBST (0.05% Tween-20, 100 mmol/L Tris–HCl, and 150 mmol/L NaCl, pH 7.5) at room temperature for 2 h, the membranes were incubated overnight at 4 °C with primary antibodies that target specific proteins, including β-actin (#20536-1-AP; Proteintech, Chicago, IL, USA), NR1H4 (#25055-1-AP; Proteintech), NR1H3 (#14351-1-AP; Proteintech), PPARα (#66826-1-Ig; Proteintech) and CYP7A1(#AF6657; Beyotime Institute of Biotechnology) and CYP27A1(#14739-1-AP; Proteintech). The blots were washed in TBST three times and incubated for 1.5 h at room temperature with a secondary antibody: alkaline phosphatase-conjugated goat anti-rabbit IgG or anti-mouse IgG (#BL023A and #BL021A; Biosharp, Hefei, Anhui, China). Finally, the blots were washed with TBST three times before protein detection using an enhanced chemiluminescence reagent (#BL520A; Biosharp) and visualisation on a ChemiDocTM Imaging System (BIO-RAD, Hercules, CA, USA). Protein band intensity was quantified using ImageJ 1.42 q software (NIH, Bethesda, MD, USA).
16S rRNA analysis of the ileal microbial community
Total bacterial DNA was extracted from the ileum chyme samples using the TIANamp Stool DNA Kit (Tiangen Biotech, Beijing, China), according to the manufacturer’s guidance. The V3–V4 region of the bacterial 16S rRNA genes was amplified using the specific primers 341 F/806R (341 F: 5’-ACTCCTACGGGAGGCAGCAG-3’; 806R: 5’-GGACTACHVGGGTWTCTAAT-3’). The PCR reaction involved a thermal cycle consisting of initial denaturation at 94 °C for 3 min, then 30 cycles of 94 ℃ for 30 s, 56 °C for 45 s, and 72 °C for 45 s, and a final extension step for 10 min at 72 °C. PCR enrichment was performed in a 50-µL reaction containing 30 ng template, fusion PCR primer and PCR master mix. The PCR products were purified with AmpureXP beads and eluted in an elution buffer. Libraries were qualified using the Agilent 2100 Bioanalyzer (Agilent, Santa Clara, CA, USA). The validated libraries were sequenced using the Illumina MiSeq platform (BGI, Shenzhen, Guangdong, China), following the standard pipelines of Illumina and generating 2 × 300 bp paired-end reads.
Raw reads were filtered to remove adaptors and low-quality ambiguous bases, and then paired-end reads were added to tags by the Fast Length Adjustment of Short reads program (V 1.2.11) to generate the tags. Subsequently, the clean tags were assigned to operational taxonomic units with a threshold of 97% identity by UPARSE (V 7.0.1090), and the chimeric sequences were identified and eliminated using UCHIME (V 4.2.40). Species annotation analysis was performed by an RDP Classifier (V 2.2) based on the Greengene database (V 201,305) with a minimum confidence threshold of 80%. The rarefaction curve, species accumulation curve and Shannon, Simpson and Chao indices were calculated using RStudio software (V 3.5.3) with the vegan package. To estimate beta diversity, principal coordinates analysis (PCoA) based on the Bray-Curtis distance and an analysis of similarities (ANOSIM) were conducted to compare the differences between the treatments using RStudio software (V 3.5.3).
Targeted metabolome analysis of intestinal and liver bile acids (BAs)
The BA content of the ileal chyme and the liver was determined using ultra-high performance liquid chromatography–mass spectrometry (UPLC/MS, ACQUITY UPLC-Xevo TQ-S, Waters Corp., Milford, MA, USA). In brief, approximately 10 mg of each freeze-dried sample was added to an Eppendorf tube along with 10 µL internal standard, 190 µL acetonitrile/methanol (v/v = 8:2) and 25 mg pre-cooling grinding beads. The sample was homogenized, and the homogenate was centrifuged at 13,500 r/min for 20 min at 4 ℃ (Microfuge 20R, Beckman Coulter, Inc., Indianapolis, IN, USA). Next, 10 µL of the resultant supernatant was removed and diluted with 45 µL acetonitrile/methanol (v/v = 8:2) and ultrapure water. Then, 5 µL of the diluent was applied to the UPLC/MS system for BA quantification. An ACQUITY UPLC Cortecs C18 1.6 μm analytical column (2.1 mm × 100 mm) heated to 30 ℃ was used for chromatographic separation. The gradient system consisted of Solvent A (10 mmol/L ammonium acetate with 0.25% acetate acid) and Solvent B (acetonitrile:methanol:isopropanol = 8:1:1) at a flow rate of 0.4 mL/min. The other parameters were set as follows: capillary voltage = 2.0 kV, ion source temperature = 150 ℃, desolvation temperature = 550 ℃, desolvation flow = 1000 L/h. BA standards were purchased from Steraloids, Co. Ltd (Newport, RI, USA) and TRC Chemicals, Co. Ltd (Toronto, ON, Canada). The mixed reference standards were obtained by dissolving each BA reference standard in methanol.
Statistical analysis
The data were analyzed using SPSS 25.0 statistical software (ver. 25.0 for Windows, SPSS Inc., Chicago, IL, USA). Statistical differences in serum and hepatic biochemical indices, hepatic gene and protein expression levels and intestinal and hepatic BA contents were determined by one-way ANOVA followed by Tukey’s test when F was significant. The Kruskal–Wallis test was used to detect differences in the relative abundance of bacteria among these groups. A P-value < 0.05 was considered statistically significant. The results are presented as mean ± SE.
Results
Growth performance
The piglets in the IUGR-CON group had lower FBWs than those in the NBW-CON group (P < 0.05), indicating that IUGR decreased the FBW. In contrast, in the IUGR-CB group, C. butyricum supplementation improved (P < 0.05) the growth performance of these piglets, and the average daily gain (ADG) and FBW were increased by 41.60% and 30.57%, respectively (Table 1).
Table 1.
Effect of supplemental C. butyricum on the growth performance of IUGR suckling piglets from 3 to 24 days of age
| Items1 | NBW-CON2 | IUGR-CON | IUGR-CB | P-values | ||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | ||||
| IBW, kg | 2.24 ± 0.03 | 1.51 ± 0.11* | 1.52 ± 0.12* | < 0.001 | < 0.001 | 0.998 |
| FBW, kg | 7.16 ± 0.19 | 5.66 ± 0.40* | 7.39 ± 0.26# | 0.005 | 0.847 | 0.001 |
| ADG, g/d | 234.11 ± 8.56 | 197.32 ± 16.42 | 279.40 ± 9.77*# | 0.103 | 0.038 | < 0.001 |
All data are presented as mean ± SE (n = 8). Significant difference is depicted as *P < 0.05 when compared with NBW-CON group, #P < 0.05 when compared with IUGR-CON group. Contrast: (1) NBW-CON versus IUGR-CON; (2) NBW-CON versus IUGR-CB; (3) IUGR-CON versus IUGR-CB
1IBW, initial body weight; FBW, final body weight; ADG, average daily gain
2NBW-CON, piglets with normal birth weight; IUGR-CON, piglets with intrauterine growth restriction; IUGR-CB, piglets with intrauterine growth restriction supplemented with Clostridium butyricum
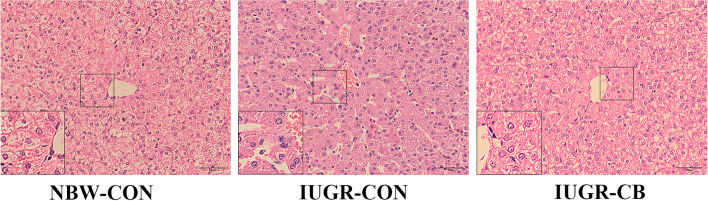
Histopathological analysis
As shown in Fig. 1, liver samples from IUGR-CON group piglets exhibited a congestive central vein, loosely arranged cords, dilated sinusoids and fewer lipid droplets in the hepatic lobule. However, C. butyricum supplementation effectively ameliorated these conditions, and normally oriented liver morphology was observed in the liver samples from IUGR-CB group piglets.
Fig. 1.
Effect of supplemental C. butyricum on hepatic histomorphology of IUGR suckling piglets. All samples were stained with hematoxylin and eosin (Low magnification: ×400, High magnification: ×800, Bars: 50 μm). NBW-CON, piglets with normal birth weight; IUGR-CON, piglets with intrauterine growth restriction; IUGR-CB, piglets with intrauterine growth restriction supplemented with Clostridium butyricum
Fatty acid (FA) metabolism
Alterations in the FA metabolites content and the corresponding enzymes in the serum and liver
As shown in Table 2, a higher (P < 0.05) level of serum NEFA and lower (P < 0.05) hepatic HL and TL levels were found in the IUGR-CON group compared to the NBW-CON group, indicating that IUGR induced these conditions. However, in the IUGR-CB group, C. butyricum treatment resulted in significantly less (P < 0.05) NEFA accumulation in the serum and elevated (P < 0.001) hepatic levels of TG and HL.
Table 2.
Effect of supplemental C. butyricum on the content of FA metabolites and their corresponding enzymes in the serum and liver of IUGR suckling piglets
| Items1 | NBW-CON2 | IUGR-CON | IUGR-CB | P-values | ||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | ||||
| Serum | ||||||
| TG, mmol/L | 1.27 ± 0.10 | 1.25 ± 0.18 | 1.25 ± 0.07 | 0.993 | 0.991 | 1.000 |
| NEFA, µmol/L | 1.49 ± 0.14 | 1.94 ± 0.04* | 0.95 ± 0.11*# | 0.027 | 0.005 | < 0.001 |
| Liver | ||||||
| TG, µmol/gprot | 89.66 ± 4.53 | 74.37 ± 5.92 | 108.83 ± 3.98*# | 0.092 | 0.029 | < 0.001 |
| HL, U/gprot | 580.11 ± 14.66 | 502.69 ± 9.49* | 621.34 ± 5.99*# | < 0.001 | 0.045 | < 0.001 |
| LPL, U/gprot | 679.73 ± 14.25 | 675.03 ± 17.36 | 694.09 ± 20.13 | 0.980 | 0.830 | 0.723 |
| TL, U/gprot | 1259.84 ± 19.35 | 1177.72 ± 11.57* | 1315.43 ± 24.70# | 0.018 | 0.128 | < 0.001 |
| VLDL, mmol/gprot | 0.57 ± 0.04 | 0.52 ± 0.02 | 0.57 ± 0.02 | 0.537 | 0.996 | 0.587 |
All data are presented as mean ± SE (n = 8). Significant difference is depicted as *P < 0.05 when compared with NBW-CON group, #P < 0.05 when compared with IUGR-CON group. Contrast: (1) NBW-CON versus IUGR-CON; (2) NBW-CON versus IUGR-CB; (3) IUGR-CON versus IUGR-CB
1TG, triglyceride; NEFA, non-esterified fatty acid; HL, hepatic lipase; LPL, lipoprotein lipase; TL, total lipase; VLDL, very low-density lipoprotein
2NBW-CON, piglets with normal birth weight; IUGR-CON, piglets with intrauterine growth restriction; IUGR-CB, piglets with intrauterine growth restriction supplemented with Clostridium butyricum
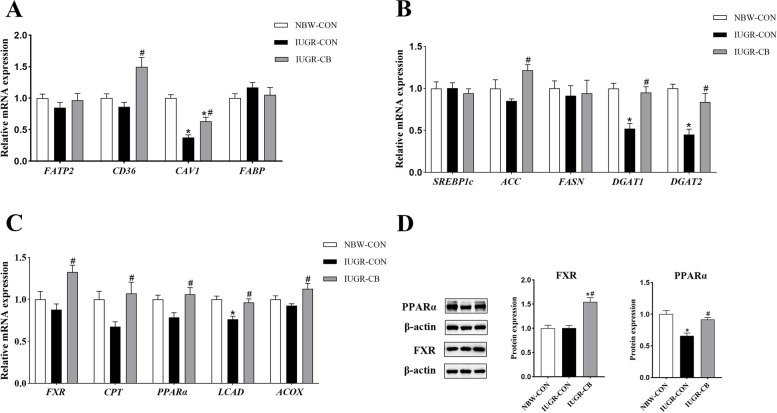
Gene expression involved in FA uptake, synthesis and oxidation
Regarding FA uptake, piglets in the IUGR-CON group had lower (P < 0.05) CAV1 mRNA expression levels than piglets in the NBW-CON group. Piglets in the IUGR-CB group had significantly higher (P < 0.05) levels of CD36 and CAV1 mRNA expression compared to piglets in the IUGR-CON group (Fig. 2A).
Fig. 2.
Effect of supplemental C. butyricum on FA metabolism of IUGR suckling piglets. A The mRNA abundance of genes related to FA uptake and transport. B The mRNA abundance of genes related to FA synthesis. C The mRNA abundance of genes related to FA oxidation. D The protein levels of FXR and PPARα. The column and its bar represented the means value and SE (n = 8), respectively. Significant difference is depicted as *P < 0.05 when compared with NBW-CON, #P < 0.05 when compared with IUGR-CON group. FATP2, fatty acid transport protein 2; CD36, cluster of differentiation 36; CAV1, caveolin 1; FABP, fatty acid binding protein; SREBP1c, sterol regulatory element-binding protein 1c; ACC, acetyl-CoA carboxylase; FASN, fatty acid synthase; DGAT1, diacylglycerol transferase 1; DGAT2, diacylglycerol transferase 2; FXR, farnesoid X receptor; CPT1, carnitine palmitoyltransferase 1; PPARα, peroxisome proliferator-activated receptor α; LCAD, long-chain acyl-CoA dehydrogenase; ACOX, acyl-CoA oxidase; NBW-CON, piglets with normal birth weight; IUGR-CON, piglets with intrauterine growth restriction; IUGR-CB, piglets with intrauterine growth restriction supplemented with Clostridium butyricum
Regarding FA synthesis, IUGR significantly decreased the gene expression of DGAT1 and DGAT2 (IUGR-CON group vs. NBW-CON group), and C. butyricum supplementation resulted in increased expression of ACC, DGAT1 and DGAT2 in the IUGR-CB group (Fig. 2B).
In terms of fatty acid oxidation (FAO), LCAD mRNA expression was significantly lower in the IUGR-CON group compared to that in the NBW-CON group. In contrast, compared to the IUGR-CON group, expression of FXR, CPT1, PPARα, LCAD and ACOX were all significantly higher in the IUGR-CB group (P < 0.05) (Fig. 2C).
Protein expression related to FA transport and metabolism
As shown in Fig. 2D, the expression of PPARα was significantly lower (P < 0.05) in the IUGR-CON group compared to that in the NBW-CON group. In contrast, IUGR piglets treated with C. butyricum exhibited higher (P < 0.05) expression of FXR and PPARα than IUGR piglets that did not receive C. butyricum.
Cholesterol and BA metabolism
Alterations in cholesterol and BA metabolites in serum and liver
As shown in Table 3, the IUGR-CON group piglets had significantly lower (P < 0.05) serum HDL-C and hepatic TBA concentrations and higher (P < 0.05) hepatic TC levels than the NBW-CON group piglets. In contrast, piglets that received C. butyricum had elevated (P < 0.05) serum HDL-C and hepatic TBA concentrations and lower (P < 0.05) hepatic TC levels, compared to the IUGR-CON group piglets.
Table 3.
Effect of supplemental C. butyricum on the content of TC and its metabolite in the serum and liver of IUGR suckling piglets
| Items1 | NBW-CON2 | IUGR-CON | IUGR-CB | P-values | ||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | ||||
| Serum | ||||||
| TC, mmol/L | 6.83 ± 0.57 | 5.28 ± 0.72 | 6.38 ± 0.57 | 0.208 | 0.865 | 0.443 |
| HDL-C, mmol/L | 3.28 ± 0.17 | 2.47 ± 0.19* | 3.54 ± 0.23# | 0.022 | 0.636 | 0.003 |
| LDL-C, mmol/L | 3.55 ± 0.31 | 2.80 ± 0.29 | 2.83 ± 0.23 | 0.165 | 0.186 | 0.997 |
| Liver | ||||||
| TC, mmol/gprot | 56.27 ± 3.62 | 72.54 ± 2.54* | 58.11 ± 3.12# | 0.004 | 0.910 | 0.010 |
| TBA, µmol/gprot | 7.12 ± 0.48 | 5.62 ± 0.33* | 7.21 ± 0.40# | 0.041 | 0.988 | 0.030 |
All data are presented as mean ± SE (n = 8). Significant difference is depicted as *P < 0.05 when compared with NBW-CON, #P < 0.05 when compared with IUGR-CON group. Contrast: (1) NBW-CON versus IUGR-CON; (2) NBW-CON versus IUGR-CB; (3) IUGR-CON versus IUGR-CB
1TC, total cholesterol; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; TBA, total bile acid
2NBW-CON, piglets with normal birth weight; IUGR-CON, piglets with intrauterine growth restriction; IUGR-CB, piglets with intrauterine growth restriction supplemented with Clostridium butyricum
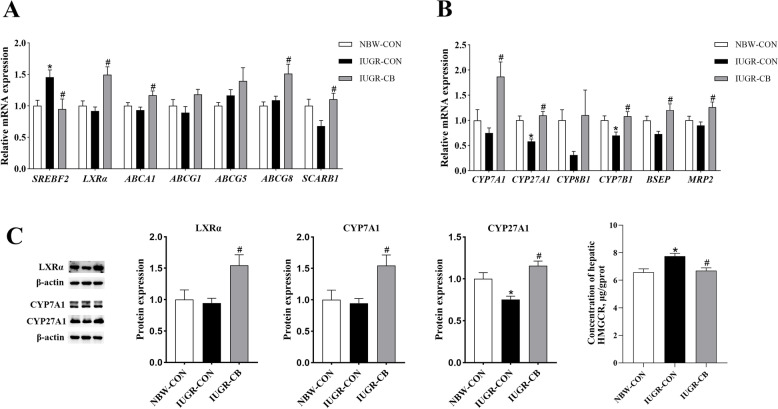
Expression of genes associated with cholesterol and BA metabolism
Compared with the NBW-CON group, the IUGR-CON groups showed significantly higher (P < 0.05) SREBF2 mRNA expression. However, C. butyricum supplementation resulted in significantly lower (P < 0.05) SREBF2 expression and, at the same time, higher (P < 0.05) expression of genes involved in reverse cholesterol transport and cholesterol efflux, such as LXRα, ABCA1, SCARB1 and ABCG8 (Fig. 3A).
Fig. 3.
Effect of supplemental C. butyricum on cholesterol and BA metabolism of IUGR suckling piglets. A The mRNA abundance of genes related to cholesterol synthesis and efflux. B The mRNA abundance of genes related to BA synthesis and excretion. C The protein levels of LXRα, CYP7A1 and CYP27A1. The column and its bar represented the means value and SE (n = 8), respectively. Significant difference is depicted as *P < 0.05 when compared with NBW-CON, #P < 0.05 when compared with IUGR-CON group. SREBF2, sterol-regulatory element binding factor 2; LXRα, liver X receptor α; ABCA1, ATP-binding cassette transporter A1; ABCG1, ATP-binding cassette transporter G1; ABCG5, ATP-binding cassette transporter G5; ABCG8, ATP-binding cassette transporter G8; SCARB1, scavenger receptor B class I; CYP7A1, cholesterol 7 α-hydroxylase; CYP27A1, cholesterol 27 α-hydroxylase; CYP7B1, Cytochrome P450 Family 7 Subfamily B Member 1; CYP8B1, Cytochrome P450 Family 8 Subfamily B Member 1; BSEP, bile salt export pump; MRP2, multidrug resistance associated protein 2; NBW-CON, piglets with normal birth weight; IUGR-CON, piglets with intrauterine growth restriction; IUGR-CB, piglets with intrauterine growth restriction supplemented with Clostridium butyricum
Regarding BA metabolism, the IUGR-CON group exhibited significantly lower (P < 0.05) CYP27A1 mRNA expression compared to the NBW-CON group. However, C. butyricum supplementation resulted in higher (P < 0.05) expression of genes related to BA synthesis, such as CYP7A1, CYP27A1 and CYP7B1, and upregulation (P < 0.05) of genes associated with BA excretion, such as BSEP and MRP2 (Fig. 3B).
Expression and enzymatic activity of proteins involved in cholesterol metabolism and BA synthesis
Piglets in the IUGR-CON group exhibited lower (P < 0.05) HMGCR activity and CYP27A1 expression in the liver compared to piglets in the NBW-CON group. Piglets in the IUGR-CB group exhibited not only elevated (P < 0.05) HMGCR activity, but also higher (P < 0.05) expression of LXRα, CYP7A1 and CYP27A1 (Fig. 3C).
Microbial composition of the ileal chyme samples
As is shown in Additional file 2: Table S2, there was no significant difference noted in the α-diversity among the three groups, including in the Sobs index, Chao index, Ace index and Shannon index. However, the IUGR-CB group’s Simpson index was lower (P < 0.05) than that of the NBW-CON group. Although no obvious separation was observed between the NBW-CON and IUGR-CON groups, C. butyricum treatment did make a difference (P < 0.05), as shown in the PCoA (Additional file 4: Fig. S1A) and ANOSIM results (Additional file 4: Fig. S1B).
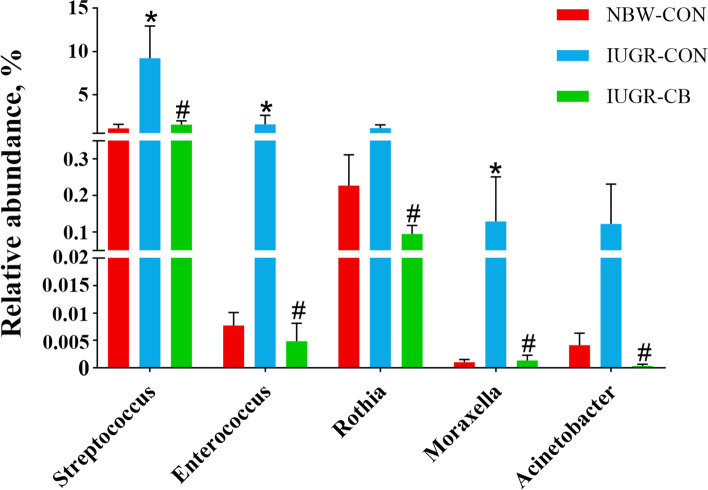
At the phylum level (Additional file 4: Fig. S1C), Firmicutes, Proteobacteria and Bacteroidetes predominantly constituted the ileal microbiota of the piglets, and no significant difference was found among the groups. At the genus level (Additional file 4: Fig. S1D), Lactobacillus, Veillonella and Actinobacillus were the dominant genera in the NBW-CON group, while in the IUGR-CON group, Lactobacillus, Streptococcus and Escherichia accounted for the majority of the bacteria. In the IUGR-CB group, the Lactobacillus, Actinobacillus and Escherichia genera dominated. Compared to the NBW-CON group, the IUGR-CON group had a relatively higher abundance of Streptococcus, Enterococcus and Moraxella (P < 0.05); however, piglets that received C. butyricum had clearly less (P < 0.05) Streptococcus, Enterococcus, Rothia, Moraxella and Acinetobacter compared to piglets in the IUGR-CON group (Fig. 4).
Fig. 4.
Differences in the relative abundance (> 0.1%) of the piglets’ ileal microbiota at the genus level. The column and its bar represented the means value and SE (n = 6), respectively. Significant difference is depicted as *P < 0.05 when compared with NBW-CON, #P < 0.05 when compared with IUGR-CON group. Streptococcus, Enterococcus, Rothia, Moraxella and Acinetobacter are all opportunistic pathogens. Thereinto, Streptococcus and Enterococcus are BSH-producing microbes. NBW-CON, piglets with normal birth weight; IUGR-CON, piglets with intrauterine growth restriction; IUGR-CB, piglets with intrauterine growth restriction supplemented with Clostridium butyricum
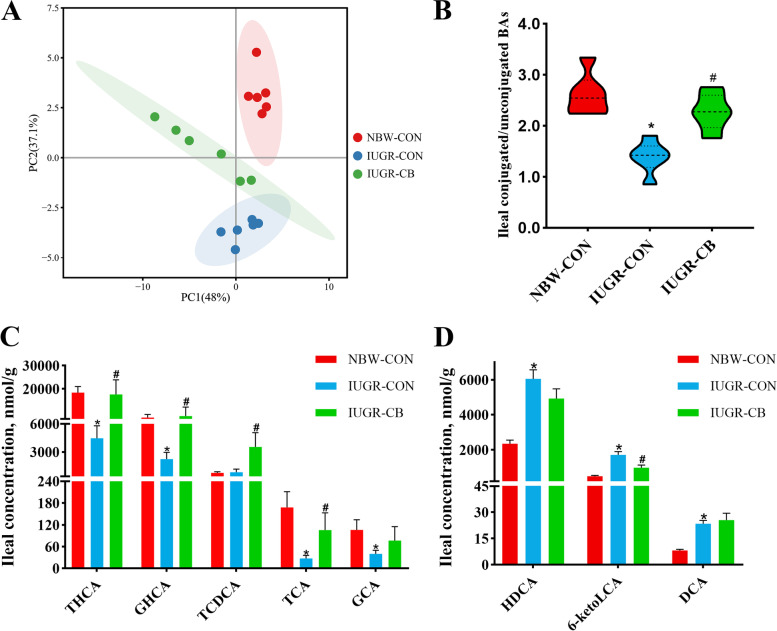
Intestinal and hepatic BA profiles
The principal component analysis (PCA) of the ileum samples revealed that there were differences in the ileal BA profiles of the three groups (Fig. 5A). Taurohyocholic acid (THCA), taurohyodeoxycholic acid (THDCA), glycohyocholate (GHCA) and glycohyodeoxycholic acid (GHDCA) accounted for the largest proportion of conjugated BAs in the ileum, while hyocholic acid (HCA), hyodeoxycholic acid (HDCA), and chenodeoxycholic acid (CDCA) represented the major unconjugated BAs in the ileum (Additional file 5: Fig. S2A). Compared to the NBW-CON group piglets, the IUGR-CON group piglets had significantly lower (P < 0.05) ratios of conjugated BAs, such as THCA, GHCA, taurocholic acid (TCA) and glycocholic acid (GCA), and higher (P < 0.05) levels of unconjugated BAs, such as HDCA, 6-ketolithocholic acid (6-ketoLCA) and deoxycholic acid (DCA) (Fig. 5C, D). As a result, the ratio of conjugated BAs to unconjugated BAs in the ileum of IUGR-CON group piglets decreased significantly (Fig. 5B). Piglets that received C. butyricum had dramatically higher (P < 0.05) levels of conjugated BAs (THCA, GHCA, taurochenodeoxycholic acid [TCDCA] and TCA), lower (P < 0.05) levels of unconjugated BAs (6-ketoLCA), and as a result, a higher ratio between conjugated and unconjugated BAs (Fig. 5B, C, D).
Fig. 5.
Effect of supplemental C. butyricum on ileal BA contents of IUGR suckling piglets. A Principal component analysis (PCA) of ileal BAs. B The ratio of the content of conjugated BAs to unconjugated BAs. C Differential metabolites of conjugated BAs. D Differential metabolites of unconjugated BAs. The column and its bar represented the means value and SE (n = 6), respectively. Significant difference is depicted as *P < 0.05 when compared with NBW-CON, #P < 0.05 when compared with IUGR-CON group. THCA, taurohyocholic acid; GHCA, glycohyocholate; TCDCA, taurochenodeoxycholic acid; TCA, taurocholic acid; GCA, glycocholic acid; HDCA, hyodeoxycholic acid; 6-ketoLCA, 6-ketolithocholic acid; DCA, deoxycholic acid. NBW-CON, piglets with normal birth weight; IUGR-CON, piglets with intrauterine growth restriction; IUGR-CB, piglets with intrauterine growth restriction supplemented with Clostridium butyricum
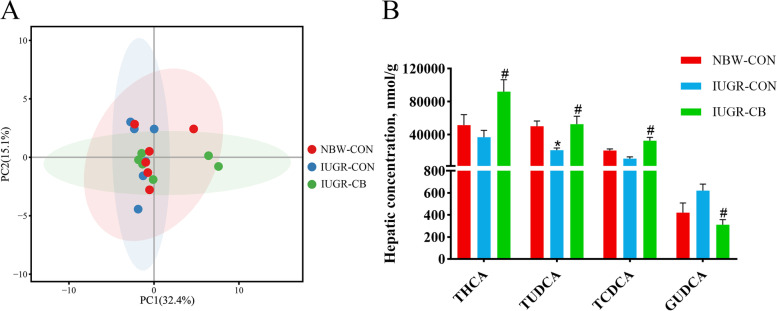
The PCA of the liver samples showed that there was no significant difference among the three groups and that the majority of the hepatic BAs were conjugated BAs (Fig. 6A). GHDCA, GHCA, glycochenodeoxycholic acid (GCDCA), THCA, tauroursodeoxycholic acid (TUDCA), TCDCA and GCA were the primary conjugated BAs found (Additional file 5: Fig. S2B). It was also found that piglets in the IUGR-CON group had significantly lower (P < 0.05) TUDCA levels than piglets in the NBW-CON group. In addition, the THCA, TUDCA and TCDCA levels were higher (P < 0.05) and the glycoursodeoxycholic acid (GUDCA) level was lower (P < 0.05) in the IUGR-CB group compared to the IUGR-CON group (Fig. 6B).
Fig. 6.
Effect of supplemental C. butyricum on hepatic BA contents of IUGR suckling piglets. A Principal component analysis (PCA) of ileal BAs. B Differential metabolites of hepatic BAs. The column and its bar represented the means value and SE (n = 6), respectively. Significant difference is depicted as *P < 0.05 when compared with NBW-CON, #P < 0.05 when compared with IUGR-CON group. THCA, Taurohyocholic acid; TUDCA, tauroursodeoxycholic acid; TCDCA, taurochenodeoxycholic acid; GUDCA, glycoursodeoxycholic acid. NBW-CON, piglets with normal birth weight; IUGR-CON, piglets with intrauterine growth restriction; IUGR-CB, piglets with intrauterine growth restriction supplemented with Clostridium butyricum
Discussion
A great deal of evidence shows that the BW of IUGR neonates is significantly lower than that of normal neonates in mammals, and the syndrome has an adverse impact on health over a long period [27]. In the present study, the serum GLU levels (Additional file 3: Table S3) and the FBWs of the IUGR-CON group piglets were significantly lower than those of the NBW-CON group piglets. It is well known that, maintaining serum GLU levels within an appropriate range is necessary for an organism’s metabolic and energy systems to function effectively [28, 29]. Therefore, we could infer that the IUGR-CON group piglets were in a low energy state during the suckling period, and as a result, their growth performance was restricted. Indeed, malnutrition is considered as a leading cause of growth restriction in mammals. When the lacking factor is replenished, spontaneous catch-up growth usually occurs, and brings the individual back to its original growth trajectory [30]. In our study, C. butyricum treatment resulted in significantly higher serum GLU levels (Additional file 3: Table S3) compared to the levels in the IUGR-CON piglets, indicating a recovery of the energy supply. As a consequence, the FBWs of the IUGR-CB piglets caught up. Given that the IBWs of IUGR-CB piglets were significantly lower than those of the NBW-CON piglets, the ADGs of IUGR-CB piglets were even higher than those of the NBW-CON piglets. Similarly, other studies have concluded that C. butyricum supplementation can effectively improve the growth performance of broilers, weanling pigs and Holstein heifers [31–33].
As a central regulator of lipid homeostasis, the liver is responsible for the de novo synthesis, oxidation and export of FAs; it also controls the biosynthesis and efflux of cholesterol [34, 35]. Maldevelopment of the liver has been observed in IUGR newborns, and this study’s findings of severe damage to the hepatic morphological structure in IUGR infants aligns with those of a previous study [5]. This damage may in turn lead to considerable dysfunction in the lipid metabolism system. Indeed, higher TC levels and lower TBA levels were observed in the livers of the IUGR-CON piglets. BAs are the end products of cholesterol catabolism, and the conversion of cholesterol to BAs accounts for the daily turnover of a major fraction of cholesterol in mammals [36]. These results indicate that IUGR could reduce the transformation of BAs and lead to an excessive accumulation of cholesterol.
Although no significant difference in TG levels was found in either the liver or serum samples, the serum NEFA concentration was notably higher in the IUGR-CON piglets. There is growing evidence that the accumulation of NEFAs is closely associated with a series of health problems, such as obesity, insulin resistance and vascular disease [37–39]. Thus, the elevated NEFA level is likely to have negative effects on the growth and development of these piglets.
In addition, the activity of hepatic HL and the level of serum HDL-C were both lower in the IUGR-CON piglets. HL plays a critical role in the hydrolysis of TGs and promotes the uptake of HDL-C in circulating blood [40, 41]. HDL-C is involved in the reverse cholesterol transport (RCT) pathway, via which excess cholesterol can be transported from the periphery to the liver for clearance [42]. Together, these findings suggest that the ability to clear excess lipids was weakened in the IUGR piglets, which may have increased the risk of developing diseases related to lipid accumulation.
On the contrary, the morphological structure of the liver was normalized in the IUGR-CB piglets. The addition of C. butyricum also resulted in less deposition of excess lipids, such as TC and NEFAs, and a simultaneous higher efflux of lipids due to high levels of hepatic TBA, HL and serum HDL-C. Similar effects of C. butyricum have been confirmed in HFD mice, indicating that C. butyricum intake could effectively improve the HFD-induced accumulation of lipid droplets in hepatocytes and decrease the content of hepatic TC and NEFAs in mice [15]. Intriguingly, we also found that hepatic TG levels in the IUGR-CB group were elevated compared to those in the other two groups. We inferred that this was likely due to a type of feedback mechanism triggered by a high cholesterol level. Because cholesterol esters are less toxic than free cholesterol, the promotion of FA synthesis plays a role in cholesterol homeostasis, with FAs being used as substrates for cholesterol esterification [43]. Hence, as shown above, supplemental C. butyricum could effectively regulate the disordered lipid metabolism of IUGR suckling piglets.
To further explore the molecular mechanism of lipid regulation utilized by C. butyricum, we detected the levels of genes and proteins associated with FA and cholesterol metabolism. As an important energy substrate, plasma NEFA can provide fuel for mitochondria, the engine of the body, to generate adenosine triphosphate (ATP) [44]. The uptake of circulating FAs by the liver is largely dependent on three major FA transporters located in the hepatocyte plasma membrane: fatty acid transport proteins (FATP), cluster of differentiation 36 (CD36) and caveolins [45, 46]. Following uptake, hydrophobic FAs cannot freely diffuse in the cytosol and must instead be shuttled between different organelles by fatty acid binding proteins (FABP) [45]. In this study, although no significant difference was observed in the expression of FATP2, CD36 and FABP1 between the NBW-CON and IUGR-CON groups, the expression of CAV1 mRNA in the IUGR-CON piglets was markedly lower than that in the NBW-CON piglets. However, treatment with C. butyricum resulted in not only higher CAV1 expression, but also higher CD36 expression. Given that CAV1 contributes to lipid trafficking and lipid droplet formation and that CD36 facilitates long-chain FA (LCFA) transport [46, 47], it could be inferred that the IUGR-CON piglets could not obtain enough materials to generate ATP for their growth and development. However, C. butyricum intervention could effectively rectify this issue.
The de novo biogenesis of FAs is mainly controlled by sterol regulatory element-binding protein 1c and its downstream targets ACC and FASN [34]. Thereinto, ACC is the first rate-limiting enzyme that converts acetyl-CoA to malonyl-CoA, and FASN is a key lipogenic enzyme that catalyzes the terminal steps of FAs synthesis [48, 49]. The newly synthesized FAs are then used in TG synthesis, and DGAT1 and DGAT2 catalyze the final step [50]. In the current study, IUGR had no great impact on the de novo synthesis of FAs; however, it reduced the storage of FAs as non-toxic TGs (IUGR-CON group vs. NBW-CON group). In contrast, IUGR piglets treated with C. butyricum exhibited increased biosynthesis of FAs and TGs. The reason for this phenomenon could be that IUGR impaired the uptake of FAs, which are an important substrate for TG synthesis. Nevertheless, C. butyricum supplementation effectively corrected this and simultaneously promoted FA synthesis. Previous studies have similarly reported that the addition of C. butyricum could increase the expression of genes related to FA synthesis in chickens [14, 16].
Following uptake, FAs are utilized by hepatocytes to generate ATP by means of β-oxidation. As the rate-limiting enzyme of FAO, carnitine palmitoyltransferase I (CPT1) catalyzes the conversion of acetyl-CoAs into acyl-carnitines, following which they can cross membranes to enter the mitochondria [51]. PPARα is an FA-activated nuclear receptor that plays a key role in the transcriptional regulation of genes involved in peroxisomal and mitochondrial FAO, such as ACOX and LCAD [52–54]. In line with the decreased uptake of FAs, the expression of PPARα and its target gene LCAD were down-regulated in the IUGR-CON group. Hence, we could infer that the elevated serum NEFA levels probably resulted from the weakened uptake and utilization of FAs in the IUGR-CON piglets. Given the involvement of FAO in energy generation, the growth performance of the IUGR-CON piglets could have been restricted by adverse effects on FAO. However, C. butyricum treatment resulted in higher expression of FXR and PPARα and its target genes involved in FAO. As a nuclear receptor, FXR is mainly expressed in the liver and intestine and has a comprehensive effect on lipid metabolism [55]. Similarly, Wang et al. found that C. butyricum supplementation could stimulate peroxisomal FA β-oxidation, possibly through the FXR–PPARα–ACOX pathway in hens [14]. Another study with human cells also found that FXR activation induced the expression of PPARα and its downstream genes involved in FAO [56]. It is interesting to note that although mitochondrial FAO was impaired in the IUGR piglets, C. butyricum addition improved peroxisomal and mitochondrial FAO both. Substantial evidence supports the notion that mitochondria and peroxisomes exhibit a close functional interplay in the β-oxidation of FAs to maintain lipid homeostasis [57]. Thus, we concluded that the C. butyricum treatment greatly improved FAO in the IUGR piglets, and as a result, the serum GLU level was raised and more energy was produced for their growth. To obtain more materials for FAO, the uptake of FAs was accordingly boosted, which likely reduced the serum NEFA content in the IUGR-CB piglets compared to the IUGR-CON piglets and even the NBW-CON piglets.
In cholesterol metabolism, LXRs work together with the sterol regulatory element-binding protein 2 (SREBP2) pathway to maintain cellular and systemic sterol levels [58]. On the one hand, LXRs can facilitate the elimination of excess cholesterol by stimulating biliary cholesterol excretion through the target genes ABCG5 and ABCG8 [59]. On the other hand, SREBP2 can boost cholesterol biosynthesis by activating the transcription of the gene that encodes the rate-limiting enzyme HMGCR [60]. The higher expression of SREBF2 and the activity of HMGCR in the IUGR-CON group compared with that in the NBW-CON group suggested that IUGR promotes cholesterol synthesis, whereas the addition of C. butyricum downregulated cholesterol synthesis by decreasing SREBF2 expression and upregulating its efflux by elevating the expression of LXRα and its downstream target ABCG8. LXRα is one isoform of the LXR family that is highly expressed in metabolically active tissues, such as the liver and intestine.
Moreover, LXRα also plays a critical role in promoting RCT, through which excess cholesterol in peripheral tissues can be transferred to HDL and then transported to the liver for BA synthesis and excretion [58]. In this process, downstream genes of LXRα, such as ABCA1, ABCG1 and SR-BI, work together to drive the assembly of HDL to initiate RCT [61–63]. Then, the excess cholesterol transported by HDL-C is used for BA synthesis, which is critical for maintaining cholesterol homeostasis and preventing the accumulation of cholesterol in the liver [36].
BAs are synthesized by multi-step reactions catalyzed in hepatocytes via two distinct routes: the “classical” (neutral) pathway and the “alternative” (acidic) pathway. The classic pathway is initiated by 7α-hydroxylation of cholesterol catalyzed by the rate-limiting enzyme CYP7A1, followed by further transformations of the steroid nucleus and oxidative cleavage of the side chain involving CYP8B1 [64]. The alternative pathway is initiated by sterol 27-hydroxylase (CYP27A1). This reaction is followed by oxysterol 7α-hydroxylation, which is primarily mediated by CYP7B1 [65]. Finally, the synthesized BAs are secreted through the bile canalicular membrane by two ABC transporters (BSEP and MRP2) into the canalicular lumen [66]. Consistent with the variation in hepatic TBA levels, the expression of CYP27A1 and CYP7B1 was lower in the IUGR-CON group compared to that in the NBW-CON group. In the IUGR-CB group, expression of CYP7A1 and CYP27A1 and its downstream gene CYP7B1 was markedly higher, and BSEP and MRP2 expression were both increased accordingly. These results revealed that the reduced BA levels in the IUGR-CON group were likely the result of an impaired alternative pathway, and that C. butyricum treatment could effectively restore BA content to normal levels by promoting the classic and alternative pathways. A study that focused on oxysterol 7α-hydroxylase, an important enzyme in the alternative pathway, confirmed the quantitative importance of the alternative pathway in early life in humans [67], suggesting that the alternative pathway might be the major route of BA synthesis in infants. Given the specific period of suckling, malfunction of the alternative pathway would consequently lead to considerable disruption of cholesterol metabolism. Moreover, previous studies have similarly indicated that increases in CYP27A1 activity could downregulate cholesterol synthesis through the SREBP pathway as well as enhance the efflux and elimination of cholesterol via LXR [68].
There is a plethora of evidence confirming that the composition of the gut microbiota can have profound effects on the host [69, 70]. In our study, no significant difference was found in the microbial α-diversity among the three groups except for a decreased Simpson index in the IUGR-CB group compared to the NBW-CON group. Hence, it could be inferred that the addition of C. butyricum affected the homogeneity of the gut microbiota by modulating its composition. To further investigate the connection between the change in the gut microbiota and the effect of lipid regulation in the IUGR-CB group, we analyzed the differences in the bacteria among the groups at the phylum and genus levels. Although no significant difference was found at the phylum level, piglets in the IUGR-CON group had significantly more opportunistic pathogens, such as Streptococcus, Enterococcus and Moraxella, which increases the risk of developing an inflammatory response and associated impairment of normal liver function [71–73]. Intriguingly, C. butyricum treatment resulted in not only lower relative abundance of the bacteria mentioned above but also lower relative abundance of Rothia and Acinetobacter, which are also considered opportunistic pathogens that could have negative effects on the host’s health [74, 75]. Hence, the modulation of the gut microbiota caused by C. butyricum might have effectively protected the IUGR piglets against pathogen invasion, and this is supported by the observed recovery of congestion in the liver portal vein and sinusoids.
Of note, among the changed microbes, Streptococcus and Enterococcus are BSH-producing microbes; BSH catalyzes the deconjugation of glycine- or taurine-conjugated BAs to form unconjugated BAs [76, 77]. As a result, the ileal BA profiles of the IUGR-CON piglets were altered compared with those of the NBW-CON piglets, and the profiles were characterized by lower levels of conjugated BAs and higher levels of unconjugated BAs. It is well known that BAs can function as endogenous signaling molecules by binding to BA receptors, such as FXR and LXRα, to regulate BA homeostasis in enterohepatic circulation and to modulate cholesterol and TG metabolism [36, 78]. In the current study, C. butyricum treatment was found to elevate the proportion of conjugated BAs in the ileum, and the THCA, TCDCA and TCA levels were dramatically increased. THCA is a known LXRα agonist, and TCA and TCDCA are known FXR agonists [23, 79]. Therefore, these signaling molecules might be transported to the liver via enterohepatic circulation and then play an important role in regulating lipid metabolism. To confirm this, we also analyzed the BA profile in the liver. In line with the results derived from the ileum, C. butyricum supplementation increased the levels of the LXRα agonist THCA and the FXR agonist TCDCA. Meanwhile, GUDCA, an FXR antagonist [80], was also decreased in the IUGR-CB group compared with the IUGR-CON group. Hence, FXR and LXRα may have been simultaneously activated to affect lipid metabolism in the liver.
Although FXR activation can repress BA synthesis, it relies on the effect of small heterodimer partner (SHP). The importance of SHP in the feedback regulation of BA synthesis was demonstrated in SHP−/− mice, in which the repression of CYP7A1 was dismissed and the size of the BA pool was enlarged [81]. In our study, despite the activation of FXR, no significant difference in SHP expression was observed in the IUGR-CB group compared to the IUGR-CON group. As a result, BA synthesis may not have been repressed. Conversely, the synthesis of BAs may have been upregulated by the activation of LXRα. As a type of hydrophilic BA used to treat hepatobiliary disorders, TUDCA can penetrate into the cell membrane and help transfer cholesterol from the cell membrane to HDL [82, 83]. A previous study showed that TUDCA treatment could effectively decrease serum and hepatic TC levels and increase the mRNA expression of CYP27A1 in a model of cholesterol gallstones [84]. Similarly, in our study, and consistent with the lower hepatic TUDCA levels in the IUGR piglets, the serum HDL-C level was lower and the hepatic TC level was higher in the IUGR-CON group than in the NBW-CON group. However, C. butyricum supplementation resulted in significantly higher hepatic TUDCA levels and, at the same time, promoted cholesterol efflux by increasing the serum HDL-C level to drive the transport of cholesterol and upregulating the expression of CYP27A1 to accelerate BA synthesis (Fig. 7).
Fig. 7.
Supplemental C. butyricum could effectively improve lipid disorders of IUGR suckling piglets. C. butyricum treatment modulated the gut microbiota to reduce the relative abundance of opportunistic pathogens in IUGR piglets. Therein, Streptococcus and Enterococcus are BSH-producing microbes, so that some conjugated BAs function as signaling molecules were increased in the ileum. Via enterohepatic circulation, these signaling molecules could be transported to the liver to activate LXRα and FXR. The activation of LXRα could promote the synthesis of FAs and the transformation of cholesterol to BAs, and the activation of FXR could increase the β-oxidation of FAs and the excretion of BAs.
Conclusion
Based on the findings of this study, we concluded that providing C. butyricum to IUGR suckling piglets might result in modulation of the gut microbiota; specifically, a reduction in the relative abundance of BSH-producing microbes, such as Streptococcus and Enterococcus. Thus, the levels of some conjugated BAs that function as signaling molecules were increased in the ileum. Via enterohepatic circulation, these signaling molecules could be transported to the liver and further regulated hepatic lipid metabolism by activating LXRα and FXR. As a result, the lipid metabolism was normalized and the growth performance was improved in the IUGR suckling piglets.
Supplementary Information
Additional file 1: Table S1. Sequences for real-time PCR primers.
Additional file 2: Table S2. Effect of supplemental C. butyricum on alpha diversity of ileal microbiota in IUGR suckling piglets.
Additional file 3: Table S3. Effect of supplemental C. butyricum on serum GLU of IUGR suckling piglets.
Additional file 4: Fig. S1. Effect of supplemental C. butyricum on the microbial structure of the ileum in IUGR suckling piglets.
Additional file 5: Fig. S2. Effect of supplemental C. butyricum on BAs composition of the ileum and liver.
Acknowledgements
This research was funded by the National Natural Science Foundation of China (No. 31802101) and the Fundamental Research Funds for the Central Universities (No. KJQN201935). We also would like to thank Scribendi (www.scribendi.com) for English language editing.
Abbreviations
- ABCA1
ATP-binding cassette transporter A1
- ABCG1
ATP-binding cassette transporter G1
- ABCG5
ATP-binding cassette transporter G5
- ABCG8
ATP-binding cassette transporter G8
- ACC
Acetyl-CoA carboxylase
- ACOX
Acyl-CoA oxidase
- ADG
Average daily gain
- BA
Bile acids
- BSEP
Bile salt export pump
- BSH
Bile salt hydrolase
- CAV1
Caveolin 1
- C. butyricum
Clostridium butyricum
- CD36
Cluster of differentiation 36
- CPT1
Carnitine palmitoyltransferase 1
- CYP27A1
Cholesterol 27 α-hydroxylase
- CYP7A1
Cholesterol 7alpha-hydroxylase
- CYP7B1
Cytochrome P450 Family 7 Subfamily B Member 1
- CYP8B1
Cytochrome P450 Family 8 Subfamily B Member 1
- DGAT1
Diacylglycerol acyltransferase 1
- DGAT2
Diacylglycerol acyltransferase 2
- FA
Fatty acid
- FABP
Fatty acid binding protein
- FASN
Fatty acid synthase
- FBW
Final body weight
- FXR
farnesoid X receptor
- GHCA
Glycohyocholate
- GUDCA
Glycoursodeoxycholic acid
- HDL-C
High-density lipoprotein cholesterol
- HL
Hepatic lipase
- HMGCR
3-hydroxy-3-methylglutaryl-CoA reductase
- IUGR
Intrauterine growth retardation
- LCAD
Long-chain acyl-CoA dehydrogenase
- LXRα
Liver X receptor alpha
- MRP2
Multidrug resistance associated protein 2
- NBW
Normal birth weight
- NEFA
Nonesterified free fatty acids
- PPARα
peroxisome proliferator activated receptor alpha
- SREBF2
Sterol-regulatory element binding factor 2
- TC
Total cholesterol
- TCA
Taurocholic acid
- TCDCA
Taurochenodeoxycholic acid
- TG
Triglyceride
- THCA
Taurohyocholic acid
- TUDCA
Tauroursodeoxycholic acid
Authors’ contributions
XZ1 and LZ conceived and designed the experiment; XZ1, YY, SJ, GY, ZX, HZ, XZ2 and TW conducted the experiment and statistical analysis; ZL and YY provided helps in experimental ideas; XZ1 wrote the manuscript; LZ reviewed the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (No. 31802101) and the Fundamental Research Funds for the Central Universities (No. KJQN201935).
Availability of data and materials
The datasets generated and/or analyzed during the present study are only available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
All procedures in the animal experiments followed the Guide published by the Institutional Animal Care and Use Committee of Nanjing Agricultural University (Permit No. SYXK-2017-0027).
Consent for publication
Not applicable.
Competing interests
The authors declare there are no conflict of interest.
References
- 1.Ferré P, Decaux JF, Issad T, Girard J. Changes in energy metabolism during the suckling and weaning period in the newborn. Reprod Nutr Dev. 1986;26(2b):619–31. doi: 10.1051/rnd:19860413. [DOI] [PubMed] [Google Scholar]
- 2.Odle J, Lin X, Jacobi SK, Kim SW, Stahl CH. The suckling piglet as an agrimedical model for the study of pediatric nutrition and metabolism. Annu Rev Anim Biosci. 2014;2:419–44. doi: 10.1146/annurev-animal-022513-114158. [DOI] [PubMed] [Google Scholar]
- 3.Zhang S, Chen F, Zhang Y, Lv Y, Heng J, Min T, et al. Recent progress of porcine milk components and mammary gland function. J Anim Sci Biotechnol. 2018;9:77. doi: 10.1186/s40104-018-0291-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu G, Bazer FW, Wallace JM, Spencer TE. Board-invited review: intrauterine growth retardation: implications for the animal sciences. J Anim Sci. 2006;84(9):2316–37. doi: 10.2527/jas.2006-156. [DOI] [PubMed] [Google Scholar]
- 5.He J, Dong L, Xu W, Bai K, Lu C, Wu Y, et al. Dietary tributyrin supplementation attenuates insulin resistance and abnormal lipid metabolism in suckling piglets with intrauterine growth retardation. PLoS ONE. 2015;10(8):e0136848. doi: 10.1371/journal.pone.0136848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stoeva MK, Garcia-So J, Justice N, Myers J, Tyagi S, Nemchek M, et al. Butyrate-producing human gut symbiont, Clostridium butyricum, and its role in health and disease. Gut Microbes. 2021;13(1):1–28. doi: 10.1080/19490976.2021.1907272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mountzouris KC, McCartney AL, Gibson GR. Intestinal microflora of human infants and current trends for its nutritional modulation. Br J Nutr. 2002;87(5):405–20. doi: 10.1079/BJN2002563. [DOI] [PubMed] [Google Scholar]
- 8.Sato R, Tanaka M. Intestinal distribution and intraluminal localization of orally administered Clostridium butyricum in rats. Microbiol Immunol. 1997;41(9):665–71. doi: 10.1111/j.1348-0421.1997.tb01909.x. [DOI] [PubMed] [Google Scholar]
- 9.Kong Q, He GQ, Jia JL, Zhu QL, Ruan H. Oral administration of Clostridium butyricum for modulating gastrointestinal microflora in mice. Curr Microbiol. 2011;62(2):512–7. doi: 10.1007/s00284-010-9737-8. [DOI] [PubMed] [Google Scholar]
- 10.Wang K, Cao G, Zhang H, Li Q, Yang C. Effects of Clostridium butyricum and Enterococcus faecalis on growth performance, immune function, intestinal morphology, volatile fatty acids, and intestinal flora in a piglet model. Food Funct. 2019;10(12):7844–54. doi: 10.1039/c9fo01650c. [DOI] [PubMed] [Google Scholar]
- 11.Chen L, Li S, Zheng J, Li W, Jiang X, Zhao X, et al. Effects of dietary Clostridium butyricum supplementation on growth performance, intestinal development, and immune response of weaned piglets challenged with lipopolysaccharide. J Anim Sci Biotechnol. 2018;9:62. doi: 10.1186/s40104-018-0275-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang K, Chen G, Cao G, Xu Y, Wang Y, Yang C. Effects of Clostridium butyricum and Enterococcus faecalis on growth performance, intestinal structure, and inflammation in lipopolysaccharide-challenged weaned piglets. J Anim Sci. 2019;97(10):4140–51. doi: 10.1093/jas/skz235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu Y, Liu C, Huang L, Xia Z. A discovery of relevant hepatoprotective effects and underlying mechanisms of dietary Clostridium butyricum against corticosterone-induced liver injury in Pekin ducks. Microorganisms. 2019;7(9):358. doi: 10.3390/microorganisms7090358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang WW, Wang J, Zhang HJ, Wu SG, Qi GH. Supplemental Clostridium butyricum modulates lipid metabolism through shaping gut microbiota and bile acid profile of aged laying hens. Front Microbiol. 2020;11:600. doi: 10.3389/fmicb.2020.00600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seo M, Inoue I, Tanaka M, Matsuda N, Nakano T, Awata T, et al. Clostridium butyricum MIYAIRI 588 improves high-fat diet-induced non-alcoholic fatty liver disease in rats. Dig Dis Sci. 2013;58(12):3534–44. doi: 10.1007/s10620-013-2879-3. [DOI] [PubMed] [Google Scholar]
- 16.Zhao X, Guo Y, Guo S, Tan J. Effects of Clostridium butyricum and Enterococcus faecium on growth performance, lipid metabolism, and cecal microbiota of broiler chickens. Appl Microbiol Biotechnol. 2013;97(14):6477–88. doi: 10.1007/s00253-013-4970-2. [DOI] [PubMed] [Google Scholar]
- 17.Schoeler M, Caesar R. Dietary lipids, gut microbiota and lipid metabolism. Rev Endocr Metab Disord. 2019;20(4):461. doi: 10.1007/s11154-019-09512-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fan Y, Pedersen O. Gut microbiota in human metabolic health and disease. Nat Rev Microbiol. 2021;19(1):55–71. doi: 10.1038/s41579-020-0433-9. [DOI] [PubMed] [Google Scholar]
- 19.Zhang W, Ma C, Xie P, Zhu Q, Wang X, Yin Y, et al. Gut microbiota of newborn piglets with intrauterine growth restriction have lower diversity and different taxonomic abundances. J Appl Microbiol. 2019;127(2):354–69. doi: 10.1111/jam.14304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang S, Li N, Liu C, Li T, Wang W, Jiang L, et al. Characteristics of the gut microbiota colonization, inflammatory profile, and plasma metabolome in intrauterine growth restricted piglets during the first 12 hours after birth. J Microbiol. 2019;57(9):748–58. doi: 10.1007/s12275-019-8690-x. [DOI] [PubMed] [Google Scholar]
- 21.Albillos A, de Gottardi A, Rescigno M. The gut-liver axis in liver disease: pathophysiological basis for therapy. J Hepatol. 2020;72(3):558–77. doi: 10.1016/j.jhep.2019.10.003. [DOI] [PubMed] [Google Scholar]
- 22.Tang Y, Zhang J, Li J, Lei X, Xu D, Wang Y, et al. Turnover of bile acids in liver, serum and caecal content by high-fat diet feeding affects hepatic steatosis in rats. Biochim Biophys Acta Mol Cell Biol Lipids. 2019;1864(10):1293–304. doi: 10.1016/j.bbalip.2019.05.016. [DOI] [PubMed] [Google Scholar]
- 23.Mencarelli A, Renga B, D’Amore C, Santorelli C, Graziosi L, Bruno A, et al. Dissociation of intestinal and hepatic activities of FXR and LXRα supports metabolic effects of terminal ileum interposition in rodents. Diabetes. 2013;62(10):3384–93. doi: 10.2337/db13-0299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kalaany NY, Mangelsdorf DJ. LXRS and FXR: the yin and yang of cholesterol and fat metabolism. Annu Rev Physiol. 2006;68:159–91. doi: 10.1146/annurev.physiol.68.033104.152158. [DOI] [PubMed] [Google Scholar]
- 25.D’Inca R, Kloareg M, Gras-Le Guen C. Le Huërou-Luron. Intrauterine growth restriction modifies the developmental pattern of intestinal structure, transcriptomic profile, and bacterial colonization in neonatal pigs. J Nutr. 2010;140(5):925–31. doi: 10.3945/jn.109.116822. [DOI] [PubMed] [Google Scholar]
- 26.Wang T, Huo YJ, Shi F, Xu RJ, Hutz RJ. Effects of intrauterine growth retardation on development of the gastrointestinal tract in neonatal pigs. Biol Neonate. 2005;88(1):66–72. doi: 10.1159/000084645. [DOI] [PubMed] [Google Scholar]
- 27.Darendeliler F. IUGR: genetic influences, metabolic problems, environmental associations/triggers, current and future management. Best Pract Res Clin Endocrinol Metab. 2019;33(3):101260. doi: 10.1016/j.beem.2019.01.001. [DOI] [PubMed] [Google Scholar]
- 28.Sohn JW, Ho WK. Cellular and systemic mechanisms for glucose sensing and homeostasis. Pflugers Arch. 2020;472(11):1547–61. doi: 10.1007/s00424-020-02466-2. [DOI] [PubMed] [Google Scholar]
- 29.López-Gambero AJ, Martínez F, Salazar K, Cifuentes M, Nualart F. Brain glucose-sensing mechanism and energy homeostasis. Mol Neurobiol. 2019;56(2):769–96. doi: 10.1007/s12035-018-1099-4. [DOI] [PubMed] [Google Scholar]
- 30.Gat-Yablonski G, Phillip M. Nutritionally-induced catch-up growth. Nutrients. 2015;7(1):517–51. doi: 10.3390/nu7010517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li Y, Wang Y, Lv J, Dou X, Zhang Y. Effects of dietary supplementation with Clostridium butyricum on the amelioration of growth performance, rumen fermentation, and rumen microbiota of Holstein heifers. Front Nutr. 2021;8:763700. doi: 10.3389/fnut.2021.763700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li W, Xu B, Wang L, Sun Q, Deng W, Wei F, et al. Effects of Clostridium butyricum on growth performance, gut microbiota and intestinal barrier function of broilers. Front Microbiol. 2021;12:777456. doi: 10.3389/fmicb.2021.777456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Casas GA, Blavi L, Cross TL, Lee AH, Swanson KS, Stein HH. Inclusion of the direct-fed microbial Clostridium butyricum in diets for weanling pigs increases growth performance and tends to increase villus height and crypt depth, but does not change intestinal microbial abundance. J Anim Sci. 2020;98(1):kz372. doi: 10.1093/jas/skz372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ipsen DH, Lykkesfeldt J, Tveden-Nyborg P. Molecular mechanisms of hepatic lipid accumulation in non-alcoholic fatty liver disease. Cell Mol Life Sci. 2018;75(18):3313–27. doi: 10.1007/s00018-018-2860-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Luo J, Yang H, Song BL. Mechanisms and regulation of cholesterol homeostasis. Nat Rev Mol Cell Biol. 2020;21(4):225–45. doi: 10.1038/s41580-019-0190-7. [DOI] [PubMed] [Google Scholar]
- 36.Chiang JY. Bile acid metabolism and signaling. Compr Physiol. 2013;3(3):1191. doi: 10.1002/cphy.c120023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Björntorp P, Bergman H, Varnauskas E. Plasma free fatty acid turnover rate in obesity. Acta Med Scand. 1969;185(4):351–6. doi: 10.1111/j.0954-6820.1969.tb07347.x. [DOI] [PubMed] [Google Scholar]
- 38.Boden G. Effects of free fatty acids (FFA) on glucose metabolism: significance for insulin resistance and type 2 diabetes. Exp Clin Endocrinol Diabetes. 2003;111(3):121–4. doi: 10.1055/s-2003-39781. [DOI] [PubMed] [Google Scholar]
- 39.Carlsson M, Wessman Y, Almgren P, Groop L. High levels of nonesterified fatty acids are associated with increased familial risk of cardiovascular disease. Arterioscler Thromb Vasc Biol. 2000;20(6):1588–94. doi: 10.1161/01.atv.20.6.1588. [DOI] [PubMed] [Google Scholar]
- 40.Connelly PW, Hegele RA. Hepatic lipase deficiency. Crit Rev Clin Lab Sci. 1998;35(6):547–72. doi: 10.1080/10408369891234273. [DOI] [PubMed] [Google Scholar]
- 41.Perret B, Mabile L, Martinez L, Tercé F, Barbaras R, Collet X. Hepatic lipase: structure/function relationship, synthesis, and regulation. J Lipid Res. 2002;43(8):1163–9. doi: 10.1194/jlr.R100020-JLR200. [DOI] [PubMed] [Google Scholar]
- 42.März W, Kleber ME, Scharnagl H, Speer T, Zewinger S, Ritsch A, et al. HDL cholesterol: reappraisal of its clinical relevance. Clin Res Cardiol. 2017;106(9):663–75. doi: 10.1007/s00392-017-1106-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Calkin AC, Tontonoz P. Transcriptional integration of metabolism by the nuclear sterol-activated receptors LXR and FXR. Nat Rev Mol Cell Biol. 2012;13(4):213–24. doi: 10.1038/nrm3312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stich V, Berlan M. Physiological regulation of NEFA availability: lipolysis pathway. Proc Nutr Soc. 2004;63(2):369–74. doi: 10.1079/PNS2004350. [DOI] [PubMed] [Google Scholar]
- 45.Mashek DG. Hepatic fatty acid trafficking: multiple forks in the road. Adv Nutr. 2013;4(6):697–710. doi: 10.3945/an.113.004648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Koo SH. Nonalcoholic fatty liver disease: molecular mechanisms for the hepatic steatosis. Clin Mol Hepatol. 2013;19(3):210–5. doi: 10.3350/cmh.2013.19.3.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Silverstein RL, Febbraio M. CD36, a scavenger receptor involved in immunity, metabolism, angiogenesis, and behavior. Sci Signal. 2009;2(72):re3. doi: 10.1126/scisignal.272re3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Numa S, Nakanishi S, Hashimoto T, Iritani N, Okazaki T. Role of acetyl coenzyme a carboxylase in the control of fatty acid synthesis. Vitam Horm. 1970;28:213–43. doi: 10.1016/s0083-6729(08)60895-x. [DOI] [PubMed] [Google Scholar]
- 49.Menendez JA, Lupu R. Fatty acid synthase and the lipogenic phenotype in cancer pathogenesis. Nat Rev Cancer. 2007;7(10):763–77. doi: 10.1038/nrc2222. [DOI] [PubMed] [Google Scholar]
- 50.McFie PJ, Chumala P, Katselis GS, Stone SJ. DGAT2 stability is increased in response to DGAT1 inhibition in gene edited HepG2 cells. Biochim Biophys Acta Mol Cell Biol Lipids. 2021;1866(9):158991. doi: 10.1016/j.bbalip.2021.158991. [DOI] [PubMed] [Google Scholar]
- 51.Schlaepfer IR, Joshi M. CPT1A-mediated fat oxidation, mechanisms, and therapeutic potential. Endocrinology. 2020;161(2):bqz046. doi: 10.1210/endocr/bqz046. [DOI] [PubMed] [Google Scholar]
- 52.Gao Q, Jia Y, Yang G, Zhang X, Boddu PC, Petersen B, et al. PPARα-deficient ob/ob obese mice become more obese and manifest severe hepatic steatosis due to decreased fatty acid oxidation. Am J Pathol. 2015;185(5):1396–408. doi: 10.1016/j.ajpath.2015.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fan CY, Pan J, Chu R, Lee D, Kluckman KD, Usuda N, et al. Hepatocellular and hepatic peroxisomal alterations in mice with a disrupted peroxisomal fatty acyl-coenzyme A oxidase gene. J Biol Chem. 1996;271(40):24698–710. doi: 10.1074/jbc.271.40.24698. [DOI] [PubMed] [Google Scholar]
- 54.Knottnerus SJG, Bleeker JC, Wüst RCI, Ferdinandusse S, L IJ, Wijburg FA, et al. Disorders of mitochondrial long-chain fatty acid oxidation and the carnitine shuttle. Rev Endocr Metab Disord. 2018;19(1):93–106. doi: 10.1007/s11154-018-9448-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Panzitt K, Wagner M. FXR in liver physiology: multiple faces to regulate liver metabolism. Biochim Biophys Acta Mol Basis Dis. 2021;1867(7):166133. doi: 10.1016/j.bbadis.2021.166133. [DOI] [PubMed] [Google Scholar]
- 56.Pineda Torra I, Claudel T, Duval C, Kosykh V, Fruchart JC, Staels B. Bile acids induce the expression of the human peroxisome proliferator-activated receptor alpha gene via activation of the farnesoid X receptor. Mol Endocrinol. 2003;17(2):259–72. doi: 10.1210/me.2002-0120. [DOI] [PubMed] [Google Scholar]
- 57.Schrader M, Costello J, Godinho LF, Islinger M. Peroxisome-mitochondria interplay and disease. J Inherit Metab Dis. 2015;38(4):681–702. doi: 10.1007/s10545-015-9819-7. [DOI] [PubMed] [Google Scholar]
- 58.Wang B, Tontonoz P. Liver X receptors in lipid signalling and membrane homeostasis. Nat Rev Endocrinol. 2018;14(8):452–63. doi: 10.1038/s41574-018-0037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yu L, York J, von Bergmann K, Lutjohann D, Cohen JC, Hobbs HH. Stimulation of cholesterol excretion by the liver X receptor agonist requires ATP-binding cassette transporters G5 and G8. J Biol Chem. 2003;278(18):15565–70. doi: 10.1074/jbc.M301311200. [DOI] [PubMed] [Google Scholar]
- 60.Horton JD, Shah NA, Warrington JA, Anderson NN, Park SW, Brown MS, et al. Combined analysis of oligonucleotide microarray data from transgenic and knockout mice identifies direct SREBP target genes. Proc Natl Acad Sci U S A. 2003;100(21):12027–32. doi: 10.1073/pnas.1534923100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vedhachalam C, Duong PT, Nickel M, Nguyen D, Dhanasekaran P, Saito H, et al. Mechanism of ATP-binding cassette transporter A1-mediated cellular lipid efflux to apolipoprotein A-I and formation of high density lipoprotein particles. J Biol Chem. 2007;282(34):25123–30. doi: 10.1074/jbc.M704590200. [DOI] [PubMed] [Google Scholar]
- 62.Wang N, Ranalletta M, Matsuura F, Peng F, Tall AR. LXR-induced redistribution of ABCG1 to plasma membrane in macrophages enhances cholesterol mass efflux to HDL. Arterioscler Thromb Vasc Biol. 2006;26(6):1310–6. doi: 10.1161/01.ATV.0000218998.75963.02. [DOI] [PubMed] [Google Scholar]
- 63.Gao F, Feng GJ, Li H, Qin WW, Xiao CS. Scavenger receptor BI induced by HDL from coronary heart disease may be related to atherosclerosis. Clin Appl Thromb Hemost. 2021;27:10760296211029710. doi: 10.1177/10760296211029710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jia W, Wei M, Rajani C, Zheng X. Targeting the alternative bile acid synthetic pathway for metabolic diseases. Protein Cell. 2021;12(5):411–25. doi: 10.1007/s13238-020-00804-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Russell DW. The enzymes, regulation, and genetics of bile acid synthesis. Annu Rev Biochem. 2003;72:137–74. doi: 10.1146/annurev.biochem.72.121801.161712. [DOI] [PubMed] [Google Scholar]
- 66.Ding L, Yang L, Wang Z, Huang W. Bile acid nuclear receptor FXR and digestive system diseases. Acta Pharm Sin B. 2015;5(2):135–44. doi: 10.1016/j.apsb.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Setchell KD, Schwarz M, O’Connell NC, Lund EG, Davis DL, Lathe R, et al. Identification of a new inborn error in bile acid synthesis: mutation of the oxysterol 7alpha-hydroxylase gene causes severe neonatal liver disease. J Clin Invest. 1998;102(9):1690–703. doi: 10.1172/JCI2962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fu X, Menke JG, Chen Y, Zhou G, MacNaul KL, Wright SD, et al. 27-hydroxycholesterol is an endogenous ligand for liver X receptor in cholesterol-loaded cells. J Biol Chem. 2001;276(42):38378–87. doi: 10.1074/jbc.M105805200. [DOI] [PubMed] [Google Scholar]
- 69.Saffouri GB, Shields-Cutler RR, Chen J, Yang Y, Lekatz HR, Hale VL, et al. Small intestinal microbial dysbiosis underlies symptoms associated with functional gastrointestinal disorders. Nat Commun. 2019;10(1):2012. doi: 10.1038/s41467-019-09964-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lynch SV, Pedersen O. The human intestinal microbiome in health and disease. N Engl J Med. 2016;375(24):2369–79. doi: 10.1056/NEJMra1600266. [DOI] [PubMed] [Google Scholar]
- 71.Haenni M, Lupo A, Madec JY. Antimicrobial resistance in Streptococcus spp. Microbiol Spectr. 2018;6(2):6. doi: 10.1128/microbiolspec.ARBA-0008-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Torres C, Alonso CA, Ruiz-Ripa L, León-Sampedro R, Del Campo R, Coque TM. Antimicrobial resistance in Enterococcus spp. of animal origin. Microbiol Spectr. 2018;6(4):6. doi: 10.1128/microbiolspec.ARBA-0032-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ren D, Pichichero ME. Vaccine targets against Moraxella catarrhalis. Expert Opin Ther Targets. 2016;20(1):19–33. doi: 10.1517/14728222.2015.1081686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fatahi-Bafghi M. Characterization of the Rothia spp. and their role in human clinical infections. Infect Genet Evol. 2021;93:104877. doi: 10.1016/j.meegid.2021.104877. [DOI] [PubMed] [Google Scholar]
- 75.Bergogne-Bérézin E, Towner KJ. Acinetobacter spp. as nosocomial pathogens: microbiological, clinical, and epidemiological features. Clin Microbiol Rev. 1996;9(2):148–65. doi: 10.1128/CMR.9.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Huang F, Zheng X, Ma X, Jiang R, Zhou W, Zhou S, et al. Theabrownin from Pu-erh tea attenuates hypercholesterolemia via modulation of gut microbiota and bile acid metabolism. Nat Commun. 2019;10(1):4971. doi: 10.1038/s41467-019-12896-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wahlström A, Sayin SI, Marschall HU, Bäckhed F. Intestinal crosstalk between bile acids and microbiota and its impact on host metabolism. Cell Metab. 2016;24(1):41–50. doi: 10.1016/j.cmet.2016.05.005. [DOI] [PubMed] [Google Scholar]
- 78.Houten SM, Watanabe M, Auwerx J. Endocrine functions of bile acids. Embo j. 2006;25(7):1419–25. doi: 10.1016/j.cmet.2016.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Vaquero J, Monte MJ, Dominguez M, Muntané J, Marin JJ. Differential activation of the human farnesoid X receptor depends on the pattern of expressed isoforms and the bile acid pool composition. Biochem Pharmacol. 2013;86(7):926–39. doi: 10.1016/j.bcp.2013.07.022. [DOI] [PubMed] [Google Scholar]
- 80.Sun L, Xie C, Wang G, Wu Y, Wu Q, Wang X, et al. Gut microbiota and intestinal FXR mediate the clinical benefits of metformin. Nat Med. 2018;24(12):1919–29. doi: 10.1038/s41591-018-0222-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wang L, Lee YK, Bundman D, Han Y, Thevananther S, Kim CS, et al. Redundant pathways for negative feedback regulation of bile acid production. Dev Cell. 2002;2(6):721–31. doi: 10.1016/s1534-5807(02)00187-9. [DOI] [PubMed] [Google Scholar]
- 82.Arai Y, Choi B, Kim BJ, Rim W, Park S, Park H, et al. Tauroursodeoxycholic acid (TUDCA) counters osteoarthritis by regulating intracellular cholesterol levels and membrane fluidity of degenerated chondrocytes. Biomater Sci. 2019;7(8):3178–89. doi: 10.1039/c9bm00426b. [DOI] [PubMed] [Google Scholar]
- 83.Vlahcevic ZR, Gurley EC, Heuman DM, Hylemon PB. Bile salts in submicellar concentrations promote bidirectional cholesterol transfer (exchange) as a function of their hydrophobicity. J Lipid Res. 1990;31(6):1063–71. doi: 10.1016/S0022-2275(20)42746-4. [DOI] [PubMed] [Google Scholar]
- 84.Lu Q, Jiang Z, Wang Q, Hu H, Zhao G. The effect of tauroursodeoxycholic acid (TUDCA) and gut microbiota on murine gallbladder stone formation. Ann Hepatol. 2021;23:100289. doi: 10.1016/j.aohep.2020.100289. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Sequences for real-time PCR primers.
Additional file 2: Table S2. Effect of supplemental C. butyricum on alpha diversity of ileal microbiota in IUGR suckling piglets.
Additional file 3: Table S3. Effect of supplemental C. butyricum on serum GLU of IUGR suckling piglets.
Additional file 4: Fig. S1. Effect of supplemental C. butyricum on the microbial structure of the ileum in IUGR suckling piglets.
Additional file 5: Fig. S2. Effect of supplemental C. butyricum on BAs composition of the ileum and liver.
Data Availability Statement
The datasets generated and/or analyzed during the present study are only available from the corresponding author on reasonable request.