Abstract
PURPOSE:
The purpose of this study was to evaluate associations of ethnicity and adaptive function with health-related quality of life (HRQOL) in youths with spina bifida myelomeningocele (SBM).
METHODS:
Participants included Hispanic (n = 75) and non-Hispanic White (n = 86) children and adolescents with SBM. Participants completed ratings of adaptive function and SBM-specific HRQOL. A series of linear multiple regression models was computed to investigate whether ethnicity moderates the relation between adaptive function and HRQOL.
RESULTS:
Results showed that greater adaptive function was associated with higher HRQOL. While no relations were found between ethnicity and HRQOL, a significant interaction was observed between adaptive function and ethnicity over and above other terms. Although groups did not differ on HRQOL at lower levels of adaptive function, Hispanic participants rated higher HRQOL relative to non-Hispanic White participants at higher levels of adaptive function. Further analysis showed this was true of both nonmotor and motor aspects of adaptive function.
CONCLUSION:
Results suggested complex relations between ethnicity and adaptive function with HRQOL, highlighting the importance of optimizing adaptive functioning in youth with SBM.
Keywords: Myelomeningocele, adaptive functioning, minoritized health
1. Background
1.1. Introduction
Spina bifida is a neural tube defect characterized by incomplete closure of the spinal cord that is estimated to affect 1,500 to 2,000 babies born each year [1]. Of the major types of spina bifida, myelomeningocele (SBM) is the most severe form and can cause functional impairment in cognition, mobility, and bladder/bowel control [2]. SBM is associated with several neurological complications, including Chiari II malformation and hydrocephalus, and thus is frequently associated with impairments in cognitive and psychosocial functioning, with greater severity and economic disadvantage predicting more severe impairments [3, 4]. Children and adolescents with more severe impairments (e.g., limited mobility and/or impaired cognitive skills) report lower quality of life [5].
1.2. Socioeconomic status (SES) and ethnicity
SBM is hypothesized to occur via a complex interplay of genetic and environmental factors, of which sociodemographic variables (including SES and ethnicity) are among the most studied [6]. Socioeconomic factors (e.g., neighborhood income, maternal education, obesity, malnutrition, reduced access to prenatal care) serve as multiplicative risk factors for SBM incidence, such that mothers residing in low SES neighborhoods are about twice as likely to have a child with SBM as socially-advantaged mothers [5].
Although controlling for SES substantially reduces the effect of race and ethnicity on SBM prevalence, racial prevalence differences have repeatedly been demonstrated to extend beyond SES. This point is particularly salient in consideration of the difference between prevalence rates among Hispanic and Black mothers, both of whom disproportionately belong to lower-SES groups. Compared to White women, Hispanic mothers are 1.2 times more likely to have a child with SBM [7]. By contrast, Black mothers have an SBM incidence at only .90 times that of their White counterparts. Reasons for heightened risk of SBM incidence among Hispanics remain unclear. Proposed explanations have included reduced folic acid intake via both traditional diet and supplemental intake, immigrant status, relatively higher proportions of visceral adipose tissue, and underlying genetic or epigenetic differences [8, 9]. Despite efforts that have been made in recent years to implement public health interventions to reduce racial/ethnic disparities in SBM prevalence (e.g., folic acid fortification in common cereals and grains), higher prevalence of SBM among Hispanic populations persists.
1.3. Health-related quality of life (HRQOL) and adaptive functioning (AF)
Early studies on the association of SBM with SES and race/ethnicity focused upon prevention efforts. More recent research has been conducted on the association between minoritized status and other psychosocial variables, such as HRQOL [10–12]. HRQOL is defined here as a person’s perception of the influence of a chronic health condition on their physical and psychosocial functioning [13]. Among younger children, HRQOL has historically been rated by proxy (i.e., caregivers) due to children’s perceived difficulty in responding directly, although self-ratings are encouraged among adolescents when possible [14]. HRQOL ratings of youth with SBM are often lower than those of their typically-developing peers, with specific predictors including medical and psychosocial variables [14–18]. However, this may be partially confounded by differences between parental report and self-report, such that adolescents often report higher HRQOL than their parents [18].
AF (here defined as one’s capacity to habitually function independently according to community standards across a broad variety of domains) is particularly relevant to HRQOL in the SBM population [19]. The modal SBM adaptive behavior profile is characterized by relatively high Social/Communication functioning, severe impairments in the Motor domain, and lesser impairments in the Personal Living and Community Living domains [19]. As such, the majority of SBM research regarding the associations between HRQOL and AF has focused upon motor function, with specific emphasis on urologic functioning and ambulatory status. Poorer motor AF is robustly associated with poorer HRQOL [15, 18, 20, 21]. The few studies that have examined nonmotor domains of AF in relation to HRQOL have shown mixed results [15, 18]. In their review, Sawin and Bellin [22] suggested that motor functioning may be specifically related to physical domains of HRQOL, while other psychosocial factors (e.g., caregiver hope, attitude) are more broadly related to overall HRQOL. However, as has been previously acknowledged, most of this literature has used HRQOL measures that are not specific to spina bifida (e.g., PedsQL), which have not been adapted for youth with physical disabilities, thereby limiting generalization to an SBM population [22].
1.4. Association of ethnicity with HRQOL and AF
While the association between AF and HRQOL seems clear, cultural differences in goals and priorities for AF may in turn be associated with relative differences in association with HRQOL. In the United States, the disability rights movement has historically prioritized “benchmarks” of success that reflect a primarily Anglo-centric value system; these benchmarks include the person with disabilities moving out of their family home, earning a salary at a traditional job, and creating nuclear families of their own [23]. Among many Hispanic families, primary caregiver goals for children with disabilities are not necessarily for independent residence. Instead, they wish to ensure that the young person develops the independence to make meaningful contributions within the family unit and in their community [23, 24]. This difference may be partially related to the heightened value placed on familial interdependence and cohesion among many Hispanic cultures [25]. Additional relevant cultural values may include differences in behaviors of seeking help from governmental authorities and religious and spiritual beliefs related to coping with disability [23].
1.5. The present study
As noted by Holmbeck et al., “Hispanic/Latino families are understudied in [the SBM] literature… [which] is surprising given the high prevalence rates of spina bifida in this population” [26]. Although several studies examining the complex relations of sociodemographic variables with other psychosocial/cognitive outcomes in SBM have been published recently, no studies have yet examined whether the association between HRQOL and AF differs by ethnicity and SES [12, 27, 28]. Given previously documented cultural differences in goals for AF and independence in youth with disabilities, as well as increased prevalence rates of SBM among the Hispanic population in North America, this study focused on exploring the role of ethnicity as a moderator of the association between total AF and HRQOL in an SBM population. More specifically, the study examined whether the role of ethnicity as a moderator changed when looking at relative importance of AF sub-domains (motor and nonmotor aspects of AF) on HRQOL.
2. Methods
2.1. Participants
The sample was drawn froma larger pool (N = 665) of infants, children, adolescents, and adults with SBM who were recruited as research volunteers from three primary sites (the Spina Bifida Clinic at Texas Children’s Hospital in Houston, Shriner’s Hospital for Children in Houston, and the Hospital for Sick Children and surrounding areas in Toronto) between 1998–2010. The present sample included 161 children and adolescents aged 5 to 20 (M = 13.1, SD = 3.4) with SBM and either shunted or arrested hydrocephalus. Any child or young adult who met these criteria was included in the initial screening. Children below age 5 and adults above age 20 as well as children with neurological disorders unrelated to SBM (e.g., brain tumors, regular seizure occurrence that was either not medicated or poorly managed with medication at the time of enrollment), sensory disorders (e.g., deafness or blindness), and neurodevelopmental disorders (e.g., autism spectrum disorder) were excluded. To focus on ethnic groups at highest risk of SBM, patients not belonging to the Hispanic or non-Hispanic White groups were also excluded (i.e., individuals identifying as Black, Asian, American Indian, or Mixed Race were removed for the purposes of focusing on the at-risk Hispanic subgroup). To reduce the heterogeneity of the Hispanic group, the focus was on individuals with Mexican and Central American backgrounds. Genetic admixture studies show that this is a relatively ethnically homogeneous group among Hispanic individuals and have also found that this population has a higher incidence of SBM among individuals in North America [29].
The sample included 75 Hispanic and 86 non-Hispanic White children and adolescents. The Hispanic sample (as determined by caregiver self-report) was primarily comprised of first- and second-generation immigrants living in Houston and Toronto. Nationality of familial origin was primarily Mexican, although Central American families were also included. Although children were recruited and identified under the label “Hispanic,” it is acknowledged that this term encompasses a diverse group of individuals who may prefer to identify themselves by country of origin or the umbrella term “Latino” or “Latinx.”
2.2. Assessment measures
SES was measured by the Hollingshead 4-Factor Scale, which classifies SES by caregiver education and occupational status [30]. A single score was calculated for each caretaker in the home. Scores were averaged to create a single SES index in families with several caretakers. Scores were calculated as a continuous variable, with higher scores associated with higher SES.
An HRQOL instrument specifically created for use in a spina bifida population (the HRQOL-SB) was administered in an effort to capture the unique concerns relevant to this population [22, 31]. The HRQOL-SB includes two forms: a 44-question caregiver scale for children ages 5–12 and a 47-question self-report scale for adolescents ages 13 and older. The caregiver scale explicitly instructs respondents to consider quality of life from the child’s viewpoint. All questions in both versions use a 5-point Likert scale, and higher HRQOL-SB scores indicate greater reported HRQOL. Both versions have high reliability in this sample, with Cronbach alpha scores of .92 and .87 for the caregiver and adolescent scales, respectively. Scores were obtained by summing each individual item, including those which were reverse-scored. As the adolescent scale includes three more questions than the caregiver counterpart, each sum total was divided by the total number of items completed to create a point average for ease of comparison. As differences in caregiver (M = 3.9, SD = 0.1) and adolescent self-report (M = 4.0, SD = 0.4) computed averages were not statistically significant, t(133) = –1.78, p = .08, and as no caregiver proxy measure is available for adolescents, scores on both measures were collapsed across age groups to create a combined HRQOL score. In other words, scores were examined as a single variable independent of rater type.
AF was measured via the Scales of Independent Behavior-Revised (SIB-R) [31]. Administered as a structured caregiver interview, the SIB-R asks caregivers to rate the ability of the child to perform adaptive behaviors in three categories (“independently,” “with assistance,” or “unable to perform”) across four clusters: Motor, Social Interaction and Communication, Personal Living, and Community Living. Split-half coefficients for these clusters range from the high .80s to low .90s [32]. A total AF score (i.e., the standard score across all domains of AF) was calculated for each participant. To explore the relative role of motor skills in AF, motor AF was compared to an on motor AF composites core in follow-up analyses, which were created by averaging scores on domains with relatively reduced motor demands (i.e., Social, Personal, and Community Living). This approach was taken to ensure that the nonmotor AF contribution was not overshadowed by motor functioning. It should be noted that although there is no overlap at the item level, some items in the nonmotor AF require motor functioning (e.g., bowel and bladder control), and it is acknowledged that these domains are not fully independent. The correlation between nonmotor AF and motor AF scores in this sample was .60.
2.3. Procedure
The original study was approved by institutional review boards in Houston and Toronto, and appropriate written informed consent and assent were provided by participants and their caregivers. Participants’ AF and HRQOL scores were measured as part of a larger assessment battery in two hospital-affiliated clinics in Houston and Toronto. Caregiver measures were administered in the preferred language (English or Spanish) and by native speakers when possible. Approximately 9% of participants were evaluated in Spanish by a bilingual native speaker using aversion in which the items were translated and adapted for a Spanish dialect appropriate for this ethnic group.
2.4. Statistical analyses
Lesion level (anatomic, as determined by imaging), ambulatory status, lifetime shunt placement, number of shunt revisions (as determined by available medical records), sex, and age were considered as potential covariates in the models, as was reporter type (i.e., self-report vs parent-proxy). To yield a meaningful interpretation of regression coefficients, all continuous variables were standardized. The PROC GLM procedure in SAS software (version 9.4) was utilized to compute models.
Although the study focused on exploring the role of ethnicity as a moderator of the association between AF and HRQOL in an SBM population, the analyses included fixed main effects models (five models in total) that separately examined the effects of AF (total, motor, and nonmotor) and ethnicity on HRQOL, controlling for covariates. The primary analysis involved a series of linear multiple regressions with fixed nested effects to investigate whether ethnicity moderated the relation between total AF and HRQOL. Additional analyses were computed to examine whether findings differed depending on the AF sub-domains (motor, nonmotor). In other words, the study examined whether ethnicity moderated relations between motor AF and HRQOL, as well as nonmotor AF and HRQOL. Each AF score was nested within ethnicity in three separate models. Of note, models with fixed nested effects never include main effects of nested variables. In other words, nested variables do not appear as main effects in the model [33]. In this case, AF variables were treated as nested variables, and therefore their main effects were not computed in estimated models. To further improve clarity, a simplified (not including covariates) example of a computed model follows:
HRQOL=ethnicity+ethnicity(total/nonmotor/motor AF), with total/nonmotor/motor AF nested with in ethnicity
The above formulation is equivalent to:
HRQOL=ethnicity+ethnicity*total/nonmotor/motor AF, omitted main effect of total/nonmotor/motor AF function
Models with nested fixed effects are advantageous in studies with a small sample, as they reduce the degrees of freedom by the number of fixed effects that are estimated relative to models with crossed (interactive) effects and consequently provide more power for testing interactive effects. Line plots were used to depict statistically significant interactive effects. The plots were generated in SAS. 9.4 using the PROC SGPLOT procedure.
3. Results
3.1. Demographic comparisons
Participant sociodemographic and medical variables grouped by ethnicity are presented in Table 1. No statistically significant group differences were noted in age, t(159) = 0.21, p = .84, sex, χ2(1) = 0.02, p =.88, or reporter type, χ2(1) = 1.44, p = .23. Similarly, no statistically significant differences were found in any of the measured medical variables, including lesion level, χ2(2) = 0.13, p =.94, ambulatory status, χ2(3) = 0.78, p = .85, shunt placement for hydrocephalus, χ2(1) = 2.91, p = .09, or lifetime number of shunt revisions, t(140) = 0.84, p = .40. A statistically significant difference was noted in SES, t(158) = 8.77, p<.001, with lower mean SES scores (M = 27.2, SD = 7.9) in Hispanic participants relative to non-Hispanic Whites (M = 41.9,SD = 12.3). Due to lack of statistically significant differences, all potential covariates analyzed except SES were trimmed from subsequent analyses.
Table 1.
Sociodemographic and medical information by ethnicity
| Ethnicity | ||
|---|---|---|
|
|
||
| Non-Hispanic White | Hispanic | |
|
| ||
| N | 86 | 75 |
| Age, yrs: M (SD) | 13.17 (3.47) | 13.05(3.26) |
| Reporter Type | ||
| Parent Proxy | 52 (32%) | 43 (27%) |
| Self-Report | 34 (21%) | 32 (20%) |
| Sex—n (%) | ||
| Male | 46 (53%) | 41 (55%) |
| Female | 40 (47%) | 34 (45%) |
| SES: M (SD)a,*,† | 41.92 (12.29) | 27.20 (7.85) |
| Lesion—n (%)b | ||
| Lumbar | 58 (67%) | 50 (67%) |
| Sacral | 7 (8%) | 5 (7%) |
| Thoracic | 21 (24%) | 19 (25%) |
| Amb Stat—n (%)c | ||
| No Assistance | 3 (3%) | 2 (3%) |
| Independent | 17 (20%) | 15 (20%) |
| Partial | 28 (33%) | 21 (28%) |
| Non-Ambulator | 28 (33%) | 29 (39%) |
| Shunt Placedd,†† | 81 (94%) | 68 (91%) |
| Shunt Revs: M (SD) | 2.51 (2.85) | 2.15 (2.13) |
Note.
SES = Socioeconomic status as measured by the Hollingshead 4-Factor SES score. Ratings calculated for primary caregivers in home, with higher scores indicating higher SES.
Lesion = Level of spinal lesion.
Amb Stat = Ambulatory Status (No Assistance = walks independently without ambulatory aids; Independent = ambulates independently with aids; Partial = ambulates independently some of the time with ambulatory aids but requires significant caregiver support; Non-Ambulator = requires caregiver support to ambulate most of the time).
Shunt Revs = Number of lifetime shunt revisions per available medical records.
p < .05.
SES data missing for 18 participants
Shut Placement data missing for 12 participants.
3.2. Adaptive function is associated with HRQOL
As seen in Table 2, results suggested that total AF was positively associated with HRQOL, β = 0.01, F(1, 124) = 14.84, p < .001. Both nonmotor AF, β = 0.40, F(1, 129) = 21.90, p < .001, and motor AF, β = 0.31, F(1,129) = 12.48, p < .001, were positively associated with HRQOL.
Table 2.
Model results for the effect of total, nonmotor, and motor domains of AF on HRQOL
| Predictor variable | R 2 | F | β | SE | t | p-value |
|---|---|---|---|---|---|---|
|
| ||||||
| Total AF | .11 | 14.84 | 0.01 | 0.00 | 3.85 | <001*** |
| Motor AF | .09 | 12.48 | <001*** | |||
| Motor | 0.31 | 0.09 | 3.53 | |||
| Nonmotor AF | .14 | 21.26 | <001*** | |||
| Nonmotor | 0.40 | 0.09 | 4.61 | |||
Note. AF = Adaptive Functioning.
p < .05
p < .01
p < .001.
3.3. Ethnicity alone is not associated with HRQOL
As reported in Table 3, no statistically significant relation was found between ethnicity and HRQOL after controlling for SES, β = 0.22, F(1, 131) = 0.53, p = 0.468.
Table 3.
Model results for the effect of ethnicity on HRQOL after controlling for SES
| Predictor variable | R 2 | F | β | SE | t | p-value |
|---|---|---|---|---|---|---|
|
| ||||||
| Ethnicity and SES | ||||||
| Omnibus | .004 | 0.28 | .759 | |||
| Ethnicity | 0.53 | .468 | ||||
| Hispanic | 0.16 | 0.22 | 0.73 | |||
| SES | 0.11 | 0.03 | 0.11 | 0.33 | .740 | |
Note. SES = Socioeconomic status; HRQOL = Health-Related Quality of Life.
3.4. Ethnicity moderates the relation between AF and HRQOL
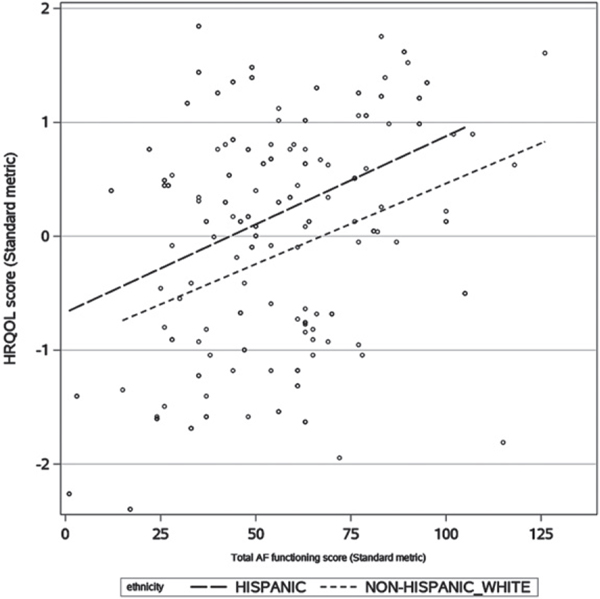
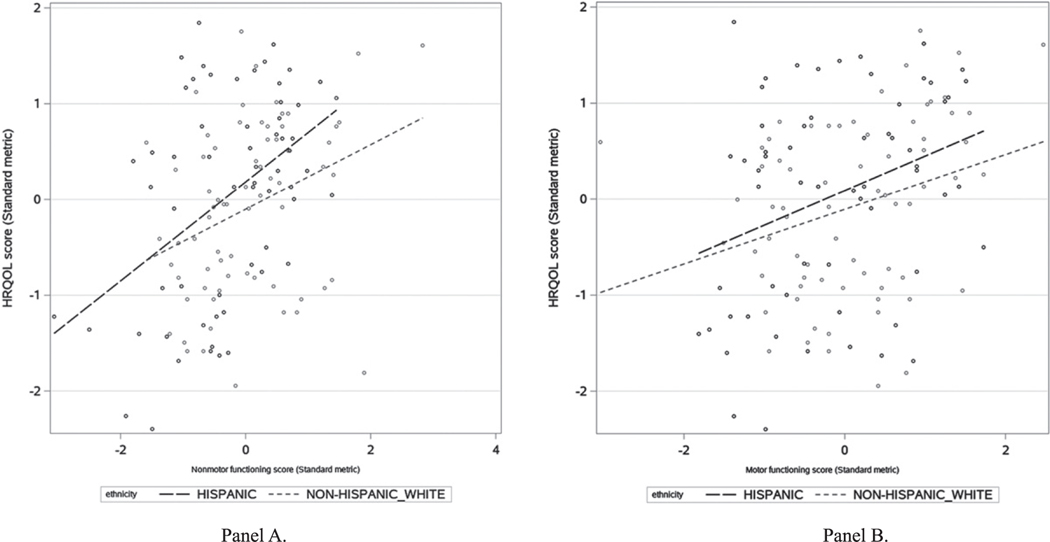
Results of the moderation analysis are presented in Table 4. Findings suggested a statistically significant interaction between total AF and ethnicity, F(2, 120) = 8.68, p < .001, controlling for SES. As presented in Fig. 1, the interaction was dominated by a main effect of ethnicity, such that Hispanic participants (depicted with a long-dashed line) had higher levels of HRQOL (β = 0.02, SE = 0.01) relative to non-Hispanic Whites (depicted with a short-dashed line, β = 0.01,SE = 0.00). In addition to the main effect of ethnicity described above, it was observed that the difference in HRQOL between Hispanics and non-Hispanic Whites was larger at higher levels of AF than at lower levels. This ordinal interaction is demonstrated in follow-up analyses showing statistically significant interactions between both nonmotor, F(2, 125) = 11.99, p < .001, and motor, F(2, 125) = 6.05, p = .002, aspects of AF and ethnicity. As observed in Fig. 2, relations between AF and HRQOL for Hispanics and non-Hispanic Whites were very similar at a lower level of nonmotor (Panel A) and motor (Panel B) AF, but not at a higher level. At the higher levels of nonmotor and motor AF, differences in these relations were much more pronounced. Specifically, Hispanics rated higher HRQOL at higher levels of nonmotor AF(β = 0.52, SE = 0.13) than non-Hispanic Whites (β = 0.33, SE = 0.13), with a similar pattern observed for motor AF: Hispanics (β = 0.36, SE = 0.28) and non-Hispanic Whites (β = 0.26, SE = 0.12).
Table 4.
Model results for the interaction of ethnicity and total, nonmotor, and motor AF on HRQOL, after controlling for SES
| Predictor variable | R 2 | F | β | SE | t | p-value |
|---|---|---|---|---|---|---|
|
| ||||||
| Total AF | ||||||
| Omnibus Test | .14 | 4.75 | .001** | |||
| SES | 0.04 | 0.02 | 0.11 | 0.20 | .842 | |
| Ethnicity | 0.40 | .127 | ||||
| Hispanic | 0.27 | 0.43 | 0.63 | |||
| AF x Ethnicity | <0.01 | <001*** | ||||
| AF x Hispanic | 0.02 | 0.01 | 2.87 | .005** | ||
| AF x NHW | 0.01 | 0.00 | 2.97 | .004** | ||
| Nonmotor AF | ||||||
| Omnibus Test | .16 | 6.12 | <001*** | |||
| SES | 0.03 | 0.02 | 0.10 | 0.19 | .853 | |
| Ethnicity | 2.13 | .147 | ||||
| Hispanic | 0.30 | 0.21 | 1.46 | |||
| AF x Ethnicity | 11.99 | <001*** | ||||
| AF x Hispanic | 0.52 | 0.13 | 4.10 | <001*** | ||
| AF x NHW | 0.33 | 0.13 | 2.65 | .009** | ||
| Motor AF | ||||||
| Omnibus Test | .10 | 3.35 | .012* | |||
| SES | 0.01 | 0.01 | 0.11 | 0.11 | .916 | |
| Ethnicity | 0.90 | .344 | ||||
| Hispanic | 0.21 | 0.22 | 0.95 | |||
| AF x Ethnicity | 6.47 | .002** | ||||
| AF x Hispanic | 0.36 | 0.13 | 2.75 | .007** | ||
| AF x NHW | 0.28 | 0.12 | 2.29 | .023* | ||
Note. AF = Adaptive Functioning; SES = Socioeconomic status; HRQOL = Health-Related Quality of Life; NHW = Non-Hispanic White.
p < .05
p < .01
p < .001.
Fig. 1.
Line Plot Depicting Interaction of Total AF With Ethnicity on HRQOL. Note. AF=Adaptive Functioning; HRQOL=Health-Related Quality of Life.
Fig. 2.
Line Plots Depicting Interaction of Nonmotor AF (Panel A) and Motor AF (Panel B) With Ethnicity on HRQOL. Note. AF=Adaptive Functioning; HRQOL=Health-Related Quality of Life.
4. Discussion
The results suggested interesting relations among ethnicity, AF, and HRQOL in youth with SBM. Consistent with prior research, AF was positively associated with HRQOL [15, 18]. A significant interaction of ethnicity and AF in association with HRQOL was observed, such that Hispanic participants rated higher HRQOL than did non-Hispanic White participants at higher levels of AF. Of note, this relation was apparent for both motor and nonmotor aspects of AF. While skills assessed in nonmotor AF measures require motor skills, these results illustrated the importance of examining elements of AF beyond the purely motor domain when conceptualizing how individuals with SBM and their families rate their own HRQOL.
While these results are associational and it therefore cannot be directly inferred that increasing AF leads to higher HRQOL, one possible interpretation of the association is that cultural differences may not be clinically meaningful in ratings of HRQOL below a certain threshold of AF; it is possible that at relatively low levels of AF, achievement of functional independence (or lack thereof) is prioritized when considering qualitative satisfaction with life. However, once a certain degree of functional independence is achieved, cultural differences seem to emerge, as results suggested that Hispanic individuals with SBM and their families may value independence in completing daily living tasks more when rating HRQOL than their non-Hispanic White counterparts. While further research is necessary to examine specific reasons for these differences, one possible explanation is related to cultural differences in goals regarding over all independence. As previously noted, due to cultural expectations in many Hispanic families in which individuals with disabilities are not typically expected to live or work outside the home in adulthood, familial goals for the child may be primarily related to their ability to contribute to the family and community [23–25]. Participation could involve assisting with family chores, helping to care for another family member, or completing simple errands [23]. This is consistent with previous qualitative research that found that Hispanic caregivers frequently described goals related to successful integration in their home and community when asked about their child’s HRQOL [24]. It may be that incremental increases in both motor and nonmotor aspects of AF can more readily translate into ability to meet the family- and community-oriented goals commonly held by many Hispanic families than into outcome-related goals like moving out of the homeor earning a salary. There may also be more opportunities for meaningful contributions in this family-based model. Achievement of these family-focused goals may in turn result in higher HRQOL among a Hispanic population at higher levels of AF. However, it is acknowledged that improving AF alone may be insufficient to improve HRQOL, as it is possible that other variables not explicitly examined in this study (e.g., familism, spirituality, perceptions of hope) may be driving these associations between HRQOL and AF; further research into these variables is therefore recommended.
Several limitations should be noted in evaluating this study. A primary limitation is that AF and HRQOL are overlapping constructs. As is demonstrated in this study, however, they should not be considered synonymous constructs; the latter is more clearly related to subjective life satisfaction, while the former is an objective assessment of ability to complete various tasks without clear association to personal and familial goals. The two domains are only moderately correlated. Additionally, it is difficult to fully differentiate nonmotor AF from its motor counterpart. Several items included in nonmotor AF (e.g., those related to bladder and bowel independence or community living) are dependent upon motor functioning. Thus, nonmotor and motor AF are not truly independent.
Another limitation is that the HRQOL-SB measure does not permit self-report or caregiver-report ratings across all ages. This is particularly challenging because past research has suggested that caregivers tend to rate their child’s HRQOL lower than children do themselves on parallel self-report measures [14]. Although the current analyses suggested that there were no statistically significant differences between caregiver and self-report of HRQOL in the sample, the lack of a self-report option for participants of all ages remains an important limitation of the measure. Indeed, given emerging evidence that even young children can directly reflect on their own HRQOL, Sawin and Bellin [22] have suggested that self-report versions of the HRQOL-SB for younger children should be considered for ease of comparison. Further, given that measurement of HRQOL and AF both used caregiver ratings, common method variance may have affected the results. Although this study specifically examined the role of ethnicity and SES in HRQOL ratings, it is acknowledged that these sociodemographic variables are but two facets of social determinants of health. Finally, the available data regarding the Hispanic participants in this study were limited; more granular details on language spoken at home, acculturation and immigration status, and language of administration may have yielded interesting additional information. Similarly, further examination of the associations between SES and the variables of interest in future studies may provide additional information that can be used in clinical decision-making with this population.
This study suggests that clinicians should remain mindful of differences in how individuals with disabilities of different ethnic/cultural backgrounds may value aspects of AF as they conceptualize their patients’ own and their family members’ HRQOL. If, for example, a person or family member of an individual with SBM expresses interest in improving their AF, a clinician may instinctively and erroneously assume that the primary treatment focus should be on improving motor skills. Results of this study suggest that the prudent clinician will first complete a thorough assessment of the goals and values of the specific individual and family, while taking particular care to ask detailed questions regarding both motor and nonmotor components of independence to improve HRQOL. This is particularly relevant when working with Hispanic families of children with disabilities. One barrier that may prevent Hispanic families from seeking formal supports is a perception that traditional disability services do not sufficiently consult and collaborate with families about goals for their child [23]. Improvement of HRQOL in this population may be best accomplished via an interdisciplinary rehabilitation team approach (including physiatrists, rehabilitative therapists, psychologists, school teachers, social workers, families, and community leaders) that addresses numerous aspects of AF and incorporates a holistic assessment of the patient’s values and needs. Thoughtful assessment of cultural considerations will become increasingly necessary over the next few years as the population of children of Hispanic descent (and relatedly, the number of Hispanic children with SBM) continues to grow within North America.
Acknowledgments
This work was supported in part by grant P01HD35946 awarded from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NICHD or the National Institutes of Health.
Footnotes
Ethical considerations
This study (titled Spina Bifida: Cognitive and Neurobiological Variability) is exempt from Institutional Review Board review as no new data is being collected. The study approval number is CR0000064 and has been renewed from May 2, 2018 to May 1, 2023. Informed consent and assent was obtained for all participants in this study. Additional information is available upon request.
Conflict of interest
The authors have no conflicts of interest to report.
References
- [1].National Institute of Neurological Disorders and Stroke. Spina bifida fact sheet [Internet]. Bethesda (MD): National Institute of Health; 2020. [updated 2022 Jul 25; cited 2022 Nov 3]. Available from: https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Spina-Bifida-Fact-Sheet [Google Scholar]
- [2].Centers for Disease Control and Prevention. What is spina bifida? [Internet]. Centers for Disease Control and Prevention; 2020. [updated 2020 Sep 3; cited 2022 Nov 3]. Available from: https://www.cdc.gov/ncbddd/spinabifida/facts.html [Google Scholar]
- [3].Fletcher JM, Brei TJ. Introduction: spinabifida—a multidisciplinary perspective. Dev Disabil Res Rev. 2010;16(1):1–5. doi: 10.1002/ddrr.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Copp AJ, Adzick NS, Chitty LS, Fletcher JM, Holmbeck GN, Shaw GM. Spina bifida. Nat Rev Dis Primers. 2015;1:15007. doi: 10.1038/nrdp.2015.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Wasserman RM, Holmbeck GN. Profiles of neuropsychological functioning in children and adolescents with spina bifida: associations with biopsychosocial predictors and functional outcomes. J Int Neuropsychol Soc. 2016;22(8):804–15. doi: 10.1017/S135561771600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Schechter MS, Liu T, Soe M, Swanson M, Ward E, Thibadeau J. Sociodemographic attributes and spina bifida outcomes. Pediatrics. 2015;135(4):957–64. doi: 10.1542/peds.2014-2576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Canfield MA, Mai CT, Wang Y, et al. The association between race/ethnicity and major birth defects in the United States,1999–2007.AmJPublicHealth.2014;104(9):14–23. doi: 10.2105/AJPH.2014.302098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Williams LJ, Rasmussen SA, Flores A, Kirby RS, Edmonds LD. Decline in the prevalence of spina bifida and anencephaly by race/ethnicity: 1995–2002. Pediatrics. 2005;116(3):580–6. doi: 10.1542/peds.2005-0592 [DOI] [PubMed] [Google Scholar]
- [9].Smith K, Freeman KA, Neville-Jan A, Mizokawa S, Adams E. Cultural considerations in the care of children with spina bifida. Pediatr Clin North Am. 2010;57(4):1027–40. doi: 10.1016/j.pcl.2010.07.019 [DOI] [PubMed] [Google Scholar]
- [10].Centers for Disease Control and Prevention (CDC). Racial/ethnic differences in the birth prevalence of spina bifida – United States, 1995–2005 [Internet]. Atlanta (GA): Centers for Disease Control and Prevention (CDC); 2009 [updated 2009 Jan 7; cited 2022 Nov 3]. Available from: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5753a2.htm [Google Scholar]
- [11].Papadakis JL, Acevedo L, Ramirez S, Stern A, Driscoll CF, Holmbeck GN. Psychosocial and family functioning among Latino youth with spina bifida. J Pediatr Psychol. 2018;43(2):105–19. doi: 10.1093/jpepsy/jsx096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Castillo J, Gandy J, Viachaslau B, Castillo H. Language and Latino immigrants living with spina bifida: social determinants of health – the missing dimension in quality of life research. J Pediatr Rehabil Med. 2019;12(4):345–59. doi: 10.3233/PRM-180586 [DOI] [PubMed] [Google Scholar]
- [13].Rocque BG, Bishop ER, Scogin MA, et al. Assessing health-related quality of life in children with spina bifida. J Neurosurg Pediatr. 2015;15(2):144–9. doi: 10.3171/2014.10.PEDS1441 [DOI] [PubMed] [Google Scholar]
- [14].Murray CB, Holmbeck GN, Ros AM, Flores DM, Mir SA, Varni JW. A longitudinal examination of health-related quality of life in children and adolescents with spina bifida. J Pediatr Psychol. 2015;40(4):419–30. doi: 10.1093/jpepsy/jsu098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Bier J-AB, Prince A, Tremont M, Msall M. Medical, functional, and social determinants of health-related quality of life in individuals with myelomeningocele. Dev Med Child Neurol. 2005;47(9):609–12. doi: 10.1017/S0012162205001209 [DOI] [PubMed] [Google Scholar]
- [16].Karmur BS, Kulkarni AV. Medical and socioeconomic predictors of quality of life in myelomeningocele patients with shunted hydrocephalus. Childs Nerv Syst. 2018;34(4):741–7. doi: 10.1007/s00381-017-3691-8 [DOI] [PubMed] [Google Scholar]
- [17].Ramachandra P, Palazzi KL, Skalsky AJ, Marietti S, Chiang G. Shunted hydrocephalus has a significant impact on quality of life in children with spina bifida. PM R. 2013;5(10):825–31. doi: 10.1016/j.pmrj.2013.05.011 [DOI] [PubMed] [Google Scholar]
- [18].Schoenmakers MAGC Uiterwaal CSPM, Gulmans VAM Gooskens RHJM, Helders PJM. Determinants of functional independence and quality of life in children with spina bifida. Clin Rehabil. 2005;19(6):677–85. doi: 10.1191/0269215505cr865oa [DOI] [PubMed] [Google Scholar]
- [19].Fletcher JM. Alternative approaches to outcomes assessment: beyond psychometric tests. Pediatr Blood Cancer. 2014;61(10):1734–8. doi: 10.1002/pbc.24824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Danielsson AJ, Bartonek Å, Levey E, McHale K, Sponseller P, Saraste H. Associations between orthopaedic findings, ambulation and health-related quality of life in children with myelomeningocele. J Child Orthop. 2008;2(1):45–54. doi: 10.1007/s11832-007-0069-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Olesen JD, Kiddoo DA, Metcalfe PD. The association between urinary continence and quality of life in paediatric patients with spina bifida and tethered cord. Paediatr Child Health. 2013;18(7):32–8. doi: 10.1093/PCH/18.7.E32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Sawin KJ, Bellin MH. Quality of life in individuals with spina bifida: a research update. Dev Disabil Res Rev. 2010;16(1):47–59. doi: 10.1002/ddrr.96 [DOI] [PubMed] [Google Scholar]
- [23].Leydorf D, Martinez K, Savinar R. Latinos with disabilities in the United States [Internet]. Berkeley (CA): World Institute on Disability; 2006. [cited 2022 Nov 3]. Available from: https://worldinstituteondisabilityblog.files.wordpress.com/2016/01/latinos-with-disabilities-in-the-us-english.pdf [Google Scholar]
- [24].Blue-Banning M, Turnbull AP, Pereira L. Hispanic youth/young adults with disabilities: parents’ visions for the future. Res Pract Pers Sev Disabil. 2002;27(3):204–19. doi: 10.2511/rpsd.27.3.204 [DOI] [Google Scholar]
- [25].Groce NE, Zola IK. Multiculturalism, chronic illness, and disability. Pediatrics. 1993;91(5 Pt 2):1048–55. [PubMed] [Google Scholar]
- [26].Holmbeck GN, Greenley RN, Coakley RM, Greco J, Hagstrom J. Family functioning in children and adolescents with spina bifida: an evidence-based review of research and interventions. J Dev Behav Pediatr. 2006;27(3):249–77. doi: 10.1097/00004703-200606000-00012 [DOI] [PubMed] [Google Scholar]
- [27].Devine KA, Holbein CE, Psihogios AM, Amaro CM, Holmbeck GN. Individual adjustment, parental functioning, and perceived social support in Hispanic and non-Hispanic white mothers and fathers of children with spina bifida. J Pediatr Psychol. 2012;37(7):769–78. doi: 10.1093/jpepsy/jsr083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Swartwout MD, Garnaat SL, Myszka KA, Fletcher JM, Dennis M. Associations of ethnicity and SES with IQ and achievement in spina bifida meningomyelocele. J Pediatr Psychol. 2010;35(9):927–36. doi: 10.1093/jpepsy/jsq001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Au KS, Tran PX, Tsai CC, et al. Characteristics of a spina bifida population including North American Caucasian and Hispanic individuals. Birth Defects Res A Clin Mol Teratol. 2008;82(10):692–700. doi: 10.1002/bdra.20499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Hollingshead AA. Four-Factor Scale Index of Social Status. New Haven (CT):Yale University Department of Sociology; 1975. (Unpublished). [Google Scholar]
- [31].Parkin PC, Kirpalani HM, Rosenbaum PL, et al. Development of a health-related quality of life instrument for use in children with spin a bifida.QualLifeRes.1997;6(2):123–32.doi: 10.1023/a:1026486016212 [DOI] [PubMed] [Google Scholar]
- [32].Bruininks RH, Woodcock RW, Weatherman RF, Hill BK. Scales of Independent Behavior-Revised. Chicago (IL): Riverside Publishing Company; 1996. [Google Scholar]
- [33].Schielzeth H, Nakagawa S. Nested by design: model fitting and interpretation in a mixed model era. Methods in Ecology and Evolution. 2013;4(1):14–24. doi: 10.1111/j.2041-210x.2012.00251.x [DOI] [Google Scholar]
- [34].Hernandez B, Cometa MJ, Rosen J, Velcoff J, Schober D, Luna RD. Employment, Vocational Rehabilitation, and the Ticket to Ride Program: Perspectives of Latinos with Disabilities. J Appl Rehabil Couns. 2006;37(3). doi: 10.1891/0047-2220.37.3.13 [DOI] [Google Scholar]