In their new paper,1 Zhao et al. present an elegant computational approach to estimate concentrations of exogenous chemicals in human blood and calculated corresponding toxic equivalencies to prioritize toxicity testing. Application of their new model identified a surprisingly high proportion of food additives, indirect additives, and food-contact substances predicted to have the highest total toxic equivalencies [referred to by Zhao et al. as bioanalytical equivalencies (BEQ%)] for the general population. Other predominant categories included industrial chemicals, pesticides, and household, fragrance, and personal care products.
Zhao et al. used biomonitoring2 and ExpoCast3 data for 216 compounds to train and test a machine learning algorithm. They employed the model to predict blood concentrations for 7,858 chemicals from ToxCast,4 which they used to calculate %BEQ for 12 endocrine-disruption assays. The authors listed the top 25 chemicals with the highest BEQ% for each of the assays, a total of 145 unique chemicals, in their Excel Table S8. I visualized these results in Figure 1 by summing BEQ% by application category and within each category by assay end point.
Figure 1.
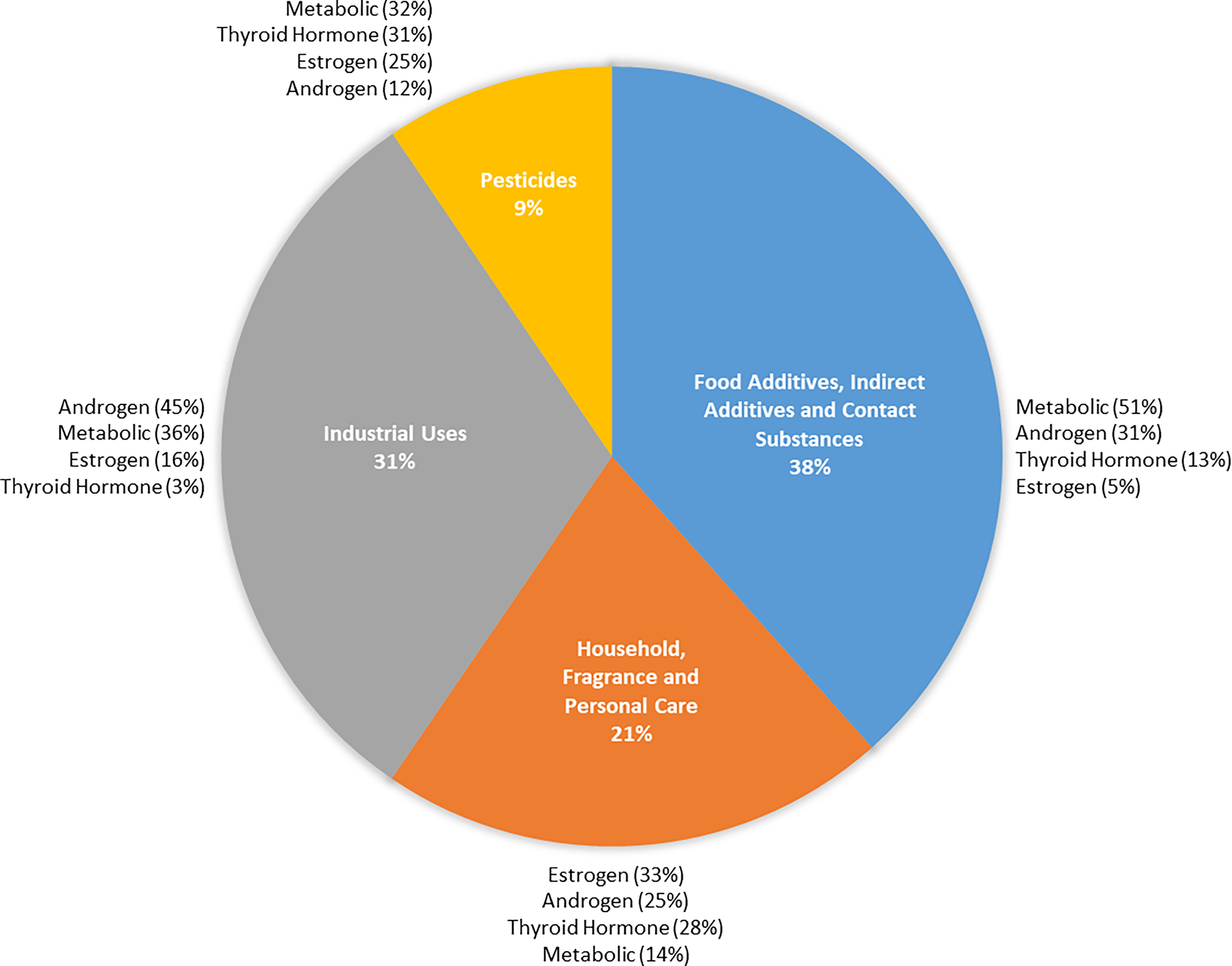
Proportional summed toxic equivalencies by application category and within each category by ToxCast end point (). Application categories derived by summing bioanalytic equivalencies () for chemicals within each category in Zhao et al., Excel Table S8.1
The unexpected predominance of the 50 food additives, indirect additives, and food-contact substances identified by this research highlights the need for comprehensive and agnostic approaches to toxicity testing prioritization. Resulting BEQ% were especially notable for two flavoring agents (2,3-butanedione and methyl formate), a colorant (FD&C Yellow 5), and three plasticizers used in food-contact substances (dimethyl isophthalate, diisobutyl phthalate, and diethyl phthalate), indicating the need to prioritize these chemicals for closer evaluation. Rigorous evaluation is also a priority among consumers, who are increasingly choosing organic foods and those with fewer ingredients and less packaging in an effort to avoid potentially harmful chemical exposures.5
Chemical production is on the rise,6 and only a small fraction of the estimated 350,000-plus chemicals in commerce have undergone careful screening or testing.7 Identification of harmful chemicals in commerce with widespread exposure has been ongoing for decades.8 Notorious examples include dichlorodiphenyltrichloroethane (DDT), lead, radium, dioxins, polybrominated diphenyl ethers, phthalates, bisphenols, and per- and polyfluoroalkyl substances.9,10 These discoveries have occurred alongside soaring rates of chronic diseases and conditions—including infertility, metabolic syndrome, thyroid disease, cancer, and neurodevelopmental and neurodegenerative conditions—that are not fully accounted for by genetic, lifestyle, or nutritional factors11 and that have been linked with exposure to many of these contaminants.12
The new model can also be used to screen alternatives that may have been introduced without adequate toxicity testing, potentially avoiding the continued use of regrettable substitutions. For example, one of the plasticizers identified by Zhao et al. for prioritization, diisobutyl phthalate, has been used as a replacement for di(2-ethylhexyl) phthalate.13 The authors also identified tri-isobutyl phosphate for prioritization; this compound is in the class of organophosphate flame retardants that have been widely used as replacements for polybrominated diphenyl ethers.14,15
Zhao et al. trained the model using biomonitoring data from the nationally representative National Health and Nutrition Examination Survey (NHANES),2 so it should be reasonably inclusive of communities with disparate burdens of chemical exposures. Improved chemical prioritization for toxicity testing is vital to better protect low-income communities and communities of color. A future evaluation of model performance could test the accuracy of predictions among vulnerable and sensitive populations. The authors noted several other ways to improve the model, such as use of more robust toxicity data and periodic future updates to incorporate new estimates of exposure and measured blood concentrations of chemicals.1
The task of predicting population blood concentrations for thousands of chemicals is seemingly impossible, yet it is a necessary step in overhauling current methods for prioritization of chemicals for toxicity testing. I applaud Zhao et al. for their innovative approach to tackling it.
Acknowledgments
C.C.C. is supported in part by the National Institute of Environmental Health Sciences, National Institutes of Health (R01ES028311), the U.S. Environmental Protection Agency National Priorities Program (No. 84025201 and Assistance Agreement No. R839482), and the U.S. Department of Agriculture National Institute of Food and Agriculture (Hatch Project MICL02565). This perspective has not been formally reviewed by the funding agencies. The views expressed in this document are solely from the author and do not necessarily reflect those of the funding agencies. The agencies do not endorse any products or commercial services mentioned in this paper.
Refers to https://doi.org.10.1289/EHP11305
References
- 1.Zhao F, Li L, Lin P, Chen Y, Xing S, Du H, et al. . 2023. HExpPredict: in vivo exposure prediction of human blood exposome using a random forest model and its application in chemical risk prioritization. Environ Health Perspect 131(3):037009, 10.1289/EHP11305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Calafat AM. 2012. The U.S. National Health and Nutrition Examination Survey and human exposure to environmental chemicals. Int J Hyg Environ Health 215(2):99–101, PMID: , 10.1016/j.ijheh.2011.08.014. [DOI] [PubMed] [Google Scholar]
- 3.Wambaugh JF, Rager JE. 2022. Exposure forecasting–ExpoCast–for data-poor chemicals in commerce and the environment. J Expo Sci Environ Epidemiol 32(6):783–793, PMID: , 10.1038/s41370-022-00492-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Richard AM, Huang R, Waidyanatha S, Shinn P, Collins BJ, Thillainadarajah I, et al. . 2021. The Tox21 10K compound library: collaborative chemistry advancing toxicology. Chem Res Toxicol 34(2):189–216, PMID: , 10.1021/acs.chemrestox.0c00264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crawford E. 2018. Eight trends that are reshaping the natural industry and opening doors in the conventional channel. Food Navigator USA. https://www.foodnavigator-usa.com/Article/2018/03/16/Eight-trends-that-are-reshaping-the-natural-industry-and-opening-doors-in-the-conventional-channel [accessed 19 December 2022]. [Google Scholar]
- 6.Bernhardt E, Rosi, E, Gessner, M. 2017. Synthetic chemicals as agents of global change. Front Ecol Environ 15(2):84–90, 10.1002/fee.1450. [DOI] [Google Scholar]
- 7.European Environment Agency. 2001. Late Lessons from Early Warnings: The Precautionary Principle 1896–2000. Luxembourg: Office for Official Publications of the European Communities. https://www.eea.europa.eu/publications/environmental_issue_report_2001_22#:∼:text=Late%20lessons%20from%20early%20warnings%20is%20about%20the%20gathering%20of,then%20living%20with%20the%20consequences [accessed 19 December 2022].
- 8.Wang Z, Walker GW, Muir DCG, Nagatani-Yoshida K. 2020. Toward a global understanding of chemical pollution: a first comprehensive analysis of national and regional chemical inventories. Environ Sci Technol 54(5):2575–2584, PMID: , 10.1021/acs.est.9b06379. [DOI] [PubMed] [Google Scholar]
- 9.Naidu R, Biswas B, Willett IR, Cribb J, Kumar Singh B, Paul Nathanail C, et al. . 2021. Chemical pollution: a growing peril and potential catastrophic risk to humanity. Environ Int 156:106616, PMID: , 10.1016/j.envint.2021.106616. [DOI] [PubMed] [Google Scholar]
- 10.Karlsson O, Rocklöv J, Lehoux AP, Bergquist J, Rutgersson A, Blunt MJ, et al. . 2021. The human exposome and health in the Anthropocene. Int J Epidemiol 50(2):378–389, PMID: , 10.1093/ije/dyaa231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sears ME, Genuis SJ. 2012. Environmental determinants of chronic disease and medical approaches: recognition, avoidance, supportive therapy, and detoxification. J Environ Public Health 2012:356798, PMID: , 10.1155/2012/356798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sly PD, Carpenter DO, Van den Berg M, Stein RT, Landrigan PJ, Brune-Drisse M-N, et al. . 2016. Health consequences of environmental exposures: causal thinking in global environmental epidemiology. Ann Glob Health 82(1):3–9, PMID: , 10.1016/j.aogh.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 13.Chiang C, Flaws JA. 2019. Subchronic exposure to di(2-ethylhexyl) phthalate and diisononyl phthalate during adulthood has immediate and long-term reproductive consequences in female mice. Toxicol Sci 168(2):620–631, PMID: , 10.1093/toxsci/kfz013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blum A, Behl M, Birnbaum LS, Diamond ML, Phillips A, Singla V, et al. . 2019. Organophosphate ester flame retardants: are they a regrettable substitution for polybrominated diphenyl ethers? Environ Sci Technol Lett 6(11):638–649, PMID: , 10.1021/acs.estlett.9b00582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang X, Sühring R, Serodio D, Bonnell M, Sundin N, Diamond ML. 2016. Novel flame retardants: estimating the physical–chemical properties and environmental fate of 94 halogenated and organophosphate PBDE replacements. Chemosphere 144:2401–2407, PMID: , 10.1016/j.chemosphere.2015.11.017. [DOI] [PubMed] [Google Scholar]


