Abstract
Objectives
Paid care provided in the home includes important support services for older adults with dementia such as cleaning and personal care assistance. By reducing unmet needs, these services could delay the transition to residential long-term care, but access may differ across racial groups. This study examined the relationship between paid care and transitioning out of the community among Black and White older adults with dementia.
Methods
Using data from 303 participants (29.4% Black) with probable dementia in the 2011 National Health and Aging Trends Study, competing risk hazards models estimated the association between receiving paid care at baseline and the probability of transitioning out of the community over 8 years (through 2019). Covariate selection was guided by the Andersen model of health care utilization.
Results
Paid care was associated with lower risk of transitioning out of the community (subhazard ratios [SHR] = 0.70, 95% CI [0.50, 0.98]). This effect was similar after controlling for predisposing factors and most prominent after controlling for enabling and need for services factors (SHR = 0.65, 95% CI [0.44, 0.95]). There was no racial difference in the use of paid care despite evidence of greater care needs in Blacks. Furthermore, Black participants were less likely to transition out of the community than Whites.
Discussion
Paid care services may help delay transitions out of the community. Future research should seek to explain racial differences in access to and/or preferences for home-based, community-based, and residential care.
Keywords: Alzheimer’s disease, Caregiving, Long-term care, Minority aging
Meeting the care needs of older adults in the home can be challenging because caregivers often decrease their work hours and earning potential, placing them at risk for financial hardship (Johnson &Wang, 2019). Those with more needs, especially with high levels of functional impairment, often require additional care, which may be fulfilled using paid services, including personal care and housekeeping. Paid care in the home could also foster continued engagement of the older person with dementia in purposeful community activities including walking and visiting with friends (Reckrey, Federman, et al., 2020; Szanton et al., 2015). However, there may be racial disparities in access to paid care.
Older adults transition to residential long-term care (LTC) settings when medical, behavioral, or functional care needs exceed available services (Cloutier et al., 2019; Young et al., 2020). Paid care has the potential to support older adults with functional impairment in the home and decrease the need for residential LTC services (Thomeer et al., 2015). However, previous studies have documented racial differences in the use of residential LTC services (Aranda et al., 2021). In this article, we analyze the association between paid care and the transition to LTC institutions among non-Hispanic Black (hereafter “Black”) and non-Hispanic White (hereafter “White”) older adults with dementia.
Racial Disparities in Paid Care
Among people living with dementia, Blacks incur greater costs of care, including inpatient hospital stays and Alzheimer’s disease and related disorders-specific medications, than Whites or Hispanics (Gilligan et al., 2013). This trend may reflect structural racism in the health care system, such as inequities in access to preventative care, delayed diagnoses (Shiekh et al., 2021), and/or poorer care coordination (Hammonds & Reverby, 2019). The out-of-pocket cost incurred by the spouses or partners of those living with dementia can lead to significant financial burden (Johnson & Wang, 2019). Thus, considering the cost of services is important.
Paid care services can be cost-prohibitive. Few older adults with disabilities can afford paid care services on income alone, requiring spending down their assets (Johnson, 2019). Wealth gained through home equity could be tapped to finance the cost of paid care (Johnson & Wang, 2019). Although Medicaid policy protects home equity for spouses, some states tax the estate posthumously, influencing the inheritability of housing wealth if a nursing home stay is Medicaid financed. Furthermore, Blacks have historically been prevented from building generational wealth through home purchases (Kaufman et al., 2020). Policies creating geographical boundaries and redlining led to consistent undervaluing of homes owned by Blacks, further contributing to disparities in generational wealth (Aranda et al., 2021; Johnson & Wang, 2019; Kaufman et al., 2020). These disparities could also be attributed to structural violence, which includes pervasive social inequities and racism often faced by Blacks in relation to complex system-wide interactions, including political, educational, and economic structures (Dilts et al., 2012). The concept of structural violence makes common conditions that have led to forms of disparity more visible. Here, violence takes on a deeper meaning, encompassing physical, visible, and invisible harm; enacted and preserved through policies and other social structures leading to conditions such as poverty, poor health, and income inequality that span generations (Dilts et al., 2012).
Transitioning out of the Community
Racial differences have been documented in the utilization of assisted living and skilled nursing facility services (Aranda et al., 2021). Reasons underlying these racial differences include poor understanding and estimation of health care needs, leading to underutilization of these services among Black families compared with Whites (Black et al., 2019). Understanding the health care needs and concerns of White and Black older adults is an important factor to ensuring access and utilization of resources (Thoomer et al, 2015).
Cultural and familial perspectives on caregiving also influence the decision to provide care in the home for the person with dementia within Hispanic and Black families (Dilworth-Anderson et al., 2020). Intergenerational relationships within families can also lead to increased involvement of family members to support Black older adults with dementia (Brewster et al., 2020). Given that lack of availability of informal caregivers is one factor leading to transitioning out of the community (Reckrey, Morrison, et al., 2020), these intergenerational relationships may also contribute to observed racial differences. However, fewer studies have examined the relationship between receiving home-based paid care and transitions to LTC among racially diverse older adults.
Theoretical Framework
Andersen’s (2005) behavioral model of health service utilization guides the current study. Andersen’s model has been used to investigate how three domains may determine transition to LTC: (a) predisposing factors, (b) enabling factors, and (c) need factors (Babitsch et al., 2012; Casanova, 2021). First, Andersen’s model suggests that exogenous factors may contribute to health service utilization, including demographic characteristics (e.g., age, sex/gender, race/ethnicity) and attitudes/beliefs toward health services. Given the mixed results in sociodemographic characteristics and contextual factors associated with nursing home admission (Gaugler et al., 2009; Moon et al., 2018), this study incorporates the key variables of age, sex, and race/ethnicity as predisposing factors.
Second, enabling factors, which are available resources at the individual, family, and community levels, could help prevent or delay institutional placement. For example, previous research has shown that lack of paid care utilization, as well as insurance coverage for LTC and social support, are associated with the increased likelihood of LTC admission (Cohen & Bulanda, 2016; Luppa et al., 2010; Moon et al., 2018). In this study, resources garnered over the life course, including socioeconomic status (i.e., education, income, home ownership), marital status, number of adult children, and health insurance, which can provide access to services such as home health, are considered as enabling factors, in addition to the primary exposure of interest: paid care.
Finally, the need domain contains individuals’ perceived and actual service needs reflecting health problems (i.e., activity limitations, chronic health conditions, cognitive impairment). For example, previous studies indicate that older adults with limitations in activities of daily living, multiple comorbidities, reduced mobility, cognitive impairment, or fall episodes may be at greater risk for institutional placement (Cloutier et al., 2019; Gaugler et al., 2009). Therefore, we include the number of individuals assisting with mobility, transportation, self-care or medical care, fall injury, limitations in self-care, mobility and household activities, chronic conditions, the need for a proxy respondent due to medical reasons, and severity of cognitive impairment as need factors.
Purpose of the Study
Understanding how paid care, which is conceptualized as an enabling factor based on Anderson’s model (1973; Gelberg et al., 2000), influences the transition out of the community requires further investigation. Studies have examined the lifetime cost of care for people with dementia (Kelley et al., 2015), others have evaluated the use of LTC by White older adults with dementia versus Blacks and other diverse ethnic populations (Aranda et al., 2021). Lastly, several studies have attempted to understand the factors that indicate a need for admission to LTC (Yan et al., 2021). Few have attempted to address the association between paid care services and the transition to institutionalized care. Thus, the extent to which paid care influences transitions from the community to LTC for older adults with dementia including Black and White older adults is not well understood.
In this study we sought to answer the following research questions: First, what are the racial differences in paid care among Black and White participants? Based on the conceptualization of race/ethnicity as a predisposing factor in the Andersen model, as well as empirical studies showing racial disparities in various paid services such as respite care (Fabius & Thomas, 2019), we expect that Black older adults with dementia would be less likely to use paid care than their White counterparts. Second, is there a relationship between receiving paid care and transitioning out of the community? Based on our conceptualization of paid care as an enabling factor in the Andersen model, we expect that paid care would delay the need for institutionalization in older adults with dementia. We also expect that Black older adults with dementia would be less likely to transition out of the community than White older adults with dementia.
Method
Data and Sample
This study used data from Rounds 1–9 (2011–2019) of National Health and Aging Trends Study (NHATS), a national survey of U.S. adults 65 years and older, sponsored by the National Institute on Aging (grant NIA U01AG032947). The study design and data collection procedures were described previously (Kasper & Freedman, 2021; Montaquila et al., 2012). The analytic sample consisted of 303 community-dwelling participants with probable dementia at study entry in 2011 (baseline). We examined transitions to nursing homes or residential care facilities through 2019. Probable dementia was defined in NHATS based on any one of the following: self or proxy report of medical diagnosis of dementia/Alzheimer’s disease, scoring 1.5 SD or more below the mean in at least two cognitive domains (i.e., memory, orientation, executive functioning) assessed by a battery of neuropsychological tests or a probable dementia score (≥2) on the proxy-completed AD8 Dementia Screening Interview (Kasper et al., 2015).
Measures
Outcome
The primary outcome was time to placement in nursing homes or residential care facilities between 2012 and 2019. Residential care facilities included assisted living facilities, continuing care retirement communities, adult family care homes, group homes, and board and care homes. In contrast, independent living facilities, retirement communities, and senior housing were considered community living settings.
Exposure
The primary predictor of interest was the presence of paid care at baseline (2011). Paid care was a derived variable (yes/no) from the other person (OP) File. The OP File contains a list of all persons who have the following roles to the NHATS participant: a proxy respondent; spouse/partner; household member; child or stepchild not in sample person (SP)’s household; social network member; helper with mobility, driving and transportation, self-care, household activities, medical care activities; a person SP takes care of; and a contact person outside of SP household (Kasper & Freedman, 2021). Among OP respondents, people were identified as helpers if they helped with at least one of the following daily activities: mobility (getting around inside or outside, getting out of bed); transportation; household activities (laundry, grocery shopping, preparing hot meals, handling bills/banking); self-care activities (eating, toileting, dressing, bathing); and medical care (medication assistance, going to doctor visits, and making decisions about insurance). This help could have been provided in or out of the home. Receiving paid help was coded as “yes” if any helper in the OP file answered yes to the question, “Is {OP respondent} paid to provide this help?” The stand-alone question on respite care was not included in the exposure.
Covariates
All covariates were measured at baseline. We included the following covariates based on the theoretical framework: (a) predisposing factors (age, sex [0 male, 1 female], race/ethnicity [non-Hispanic White, non-Hispanic Black, Hispanic, other]); (b) enabling factors (number of children, education [0 below high school graduate, 1 high school graduate and above], marital status [0 never married/separated/divorced/widowed, 1 married/living with a partner], home ownership [0 own, 1 rent/other arrangement], income, insurance coverage [0 not insured, 1 insured]); and (c) need factors (number of helpers, recent fall [0 have not fallen in the last year, 1 fallen in the last year], activity limitations, multimorbidity [0 less than two health conditions, 1 two or more health conditions], proxy respondent [0 participants responded, 1 proxy responded]). Income was a continuous variable from NHATS, imputed from several income sources or total income from all sources (Montaquila et al., 2012). The income distribution was positively skewed, so we log-transformed income for our analyses. Three types of insurance were included Medicaid, TriCare (an insurance plan for military service members), and private LTC insurance for nursing homes/assisted living/home health providers. The total number of helpers was the sum of all paid and unpaid helpers from OP File. The number of activity limitations was a derived variable based on the total sum of self-care (needing help eating, toileting, bathing, or dressing), mobility (needing help getting out of bed, moving inside, or going outside), and household activities (having difficulty with laundry, shopping, handling bills, making meals, tracking medications) where the individual needed help, and a higher number indicated more activity limitations. The dichotomous multimorbidity considered the following health conditions: heart attack, heart disease, hypertension, arthritis, osteoporosis, diabetes, lung disease, stroke, and cancer. Cognitive functioning was considered as an additional need factor in sensitivity analyses. Detailed information about how a harmonized cognition variable was computed across objective cognitive assessments and proxy-reported cognitive status is provided in Supplementary Material.
Statistical Analysis
We used standard descriptive statistics and independent-samples t-tests to summarize baseline characteristics of NHATS participants. To compare the characteristics between White and Black older adults, we calculated the effect sizes of Cohen’s d for continuous variables and phi coefficient for binary variables. The Fine and Gray hazards model was used to estimate the time to institutionalization (Fine & Gray, 1999). This model allows for the existence of a competing event (death) that renders a participant unable to experience the event of interest (institutionalization). Participants were censored if they were alive in the community in 2019 or lost to follow-up in the years before 2019. We used subhazard ratios (SHR) to determine the unadjusted and adjusted association between predictors and institutionalization, which changes the interpretation of the findings compared with a traditional hazard model. The subdistribution hazard of institutionalization is reported, which is the rate of nursing home placement among the subset of participants who have not yet moved to a nursing home or died.
We conducted four competing risk hazards models of the association between paid care and transitioning out of the community by adjusting for predisposing, enabling, and need factors in order. Based on the theoretical framework, we chose a stepwise approach to test the statistical significance of each group of predictors. We used multiple imputation to account for missing data on marital status, education, home ownership, and insurance coverage. We could not apply analytic weights provided by NHATS to our models due to the limitation of our statistical program while declaring a complex survey design and implementing the competing risk model in a subpopulation (i.e., NHATS participants with dementia; StataCorp, 2021). All statistical analyses were completed using Stata version 16.0 (StataCorp, 2019).
Results
Sample Characteristics
Table 1 illustrates the baseline data for the whole sample. Of the 303 community-dwelling older adults with dementia, 54.8% of them received paid care due to activity limitations in self-care, housework, and mobility, while the average number of limited activities was 5.3 (SD 4.7). The majority had two or more chronic conditions (n = 227; 74.9%), and 124 individuals (40.9%) had fallen on the floor or ground in the last 12 months. Of the whole sample, 99 individuals (32.7%) required proxy respondents due to having dementia or cognitive impairment, speech impairment, hearing impairment, or being ill. More than half of the participants identified themselves as White (56.7%), followed by Black (29.7%) and Hispanic (9.7%).
Table 1.
Sample Characteristics
| Variable | M | SD | n | % |
|---|---|---|---|---|
| Paid care services | 166 | 54.8 | ||
| Predisposing factors | ||||
| Age | 82.5 | 7.3 | ||
| Female | 196 | 64.7 | ||
| White | 170 | 56.7 | ||
| Black | 89 | 29.7 | ||
| Hispanic | 29 | 9.7 | ||
| Other | 12 | 4 | ||
| Enabling factors | ||||
| HS graduate and above | 157 | 53.4 | ||
| Married/partnered | 101 | 33.4 | ||
| Number of children | 3.1 | 2.4 | ||
| Rent and other arrangement | 110 | 42.2 | ||
| Income | 9.6 | 1.8 | ||
| Medicaid | 89 | 31.3 | ||
| TriCare | 13 | 4.5 | ||
| Private long-term care insurance | 27 | 8.9 | ||
| Need factors | ||||
| Number of helpers | 9.1 | 3.7 | ||
| Recent fall | 124 | 40.9 | ||
| Activity limitations | 5.3 | 4.7 | ||
| Multimorbidity | 227 | 74.9 | ||
| Proxy respondent | 99 | 32.7 |
Notes: N = 303. HS = high school. Income was log-transformed.
Hypothesis 1: Racial Differences in Paid Care
As seen in Table 2, there were no racial differences in paid care. Among predisposing factors, there were no racial differences in age and sex. As to enabling factors, Black older adults with dementia were less likely to be married or with partners, had more adult children, had lower income, had fewer individuals who graduated high school and above, and were more likely to receive Medicaid and TriCare compared to their White counterparts. A small number of both White and Black older adults had private LTC insurance with no statistically significant racial difference. Lastly, among need factors, Black older adults with dementia had a larger number of helpers and were more likely to have had a proxy respondent due to a medical reason. There were no racial differences in activity limitations, fall injuries, or multimorbidity. The finding of no Black–White difference in the receipt of paid care despite evidence that Black older adults with dementia had greater care needs than Whites provides some support for the hypothesis that Black older adults with dementia are less likely to use paid care than their White counterparts.
Table 2.
Racial Differences on Predisposing, Enabling, and Needs for Service Factors
| White (n = 170) | Black (n = 89) | ||||
|---|---|---|---|---|---|
| Variable | M/n | SD/% | M/n | SD/% | Effect size |
| Paid care services | 86 | 50.6 | 56 | 62.9 | phi = 0.12 |
| Predisposing factors | |||||
| Agea | 83.4 | 7.2 | 81.4 | 7.2 | d = 0.25 |
| Female | 111 | 65.3 | 61 | 68.5 | phi = 0.04 |
| Enabling factors | |||||
| HS graduate and above | 111 | 66.5 | 37 | 42.5 | phi = 0.21** |
| Married/partnered | 66 | 38.8 | 21 | 23.9 | phi = 0.14* |
| Number of childrena | 2.8 | 1.8 | 3.6 | 2.9 | d = −0.38* |
| Rent and other arrangement | 46 | 32.9 | 34 | 42 | phi = 0.05 |
| Incomea | 9.9 | 1.6 | 9.2 | 2 | d = 0.26* |
| Medicaid | 28 | 17.7 | 36 | 42.4 | phi = 0.22** |
| TriCare | 12 | 7.4 | 1 | 1.2 | phi = 0.12* |
| Private long-term care insurance | 18 | 10.6 | 7 | 7.9 | phi = 0.04 |
| Need factors | |||||
| Number of helpersa | 8.5 | 3.7 | 10.4 | 3.6 | d = −0.53* |
| Recent fall | 75 | 44.1 | 29 | 32.6 | phi = 0.11 |
| Activity limitationa | 5 | 4.6 | 5.8 | 4.2 | d = −0.22 |
| Multimorbidity | 124 | 72.9 | 66 | 74.2 | phi = 0.01 |
| Proxy respondent | 49 | 28.8 | 38 | 42.7 | phi = 0.15* |
Notes: HS = high school. Income was log-transformed.
aVariables were measured as continuous.
*p < .05.
** p < .01.
Hypothesis 2: Paid Care and Transitioning out of the Community
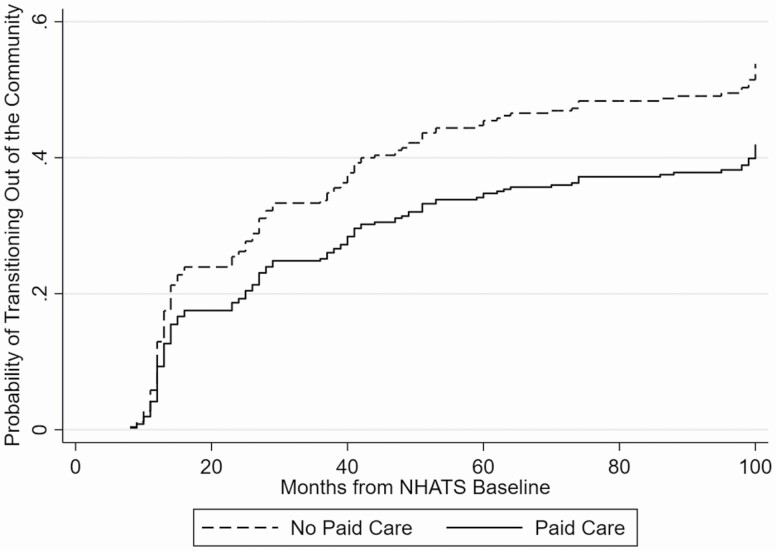
As given in Table 3, the results of the hierarchical competing risk regression analyses revealed that receiving paid care was significantly associated with reduced risk for institutionalization when the model was not adjusted for other covariates (Model 1). When we accounted for predisposing factors (Model 2), enabling factors (Model 3), and needs for service factors (Model 4), the effect of paid care on institutionalization risk remained statistically significant. In the raw model, the presence of paid care was significantly associated with lowered risk for institutionalization by 30% (see Figure 1). After adjusting for all covariates, receiving paid care had a statistically significant association with the reduced risk of institutionalization by 35%. This association was similar in a sensitivity analysis that added the harmonized cognitive variable as an additional covariate (paid help: SHR = 0.64, 95% CI [0.43, 0.94], p = .022). The effect of race was statistically significant throughout the models. As hypothesized, Black older adults were more likely to remain in the community longer than their White counterparts in all models.
Table 3.
Competing Risk Survival Analysis on Transitioning out of the Community
| Model 1 | Model 2 | Model 3 | Model 4 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 95% CI | 95% CI | 95% CI | 95% CI | |||||||||||||
| Variable | SHR | LL | UL | p | SHR | LL | UL | p | SHR | LL | UL | p | SHR | LL | UL | p |
| Paid care services | 0.70 | 0.50 | 0.98 | .039 | 0.69 | 0.48 | 0.98 | .037 | 0.66 | 0.46 | 0.95 | .026 | 0.65 | 0.44 | 0.95 | .028 |
| Agea | 1.02 | 1.00 | 1.05 | .088 | 1.01 | 0.98 | 1.04 | .504 | 1.01 | 0.99 | 1.04 | .389 | ||||
| Female | 1.51 | 1.03 | 2.21 | .034 | 1.17 | 0.78 | 1.77 | .45 | 1.24 | 0.81 | 1.90 | .318 | ||||
| Black | 0.50 | 0.33 | 0.77 | .002 | 0.49 | 0.31 | 0.76 | .002 | 0.50 | 0.31 | 0.78 | .003 | ||||
| Hispanic | 0.46 | 0.25 | 0.88 | .018 | 0.47 | 0.23 | 0.96 | .037 | 0.49 | 0.24 | 1.01 | .052 | ||||
| Other | 0.24 | 0.06 | 1.01 | .051 | 0.16 | 0.04 | 0.77 | .022 | 0.15 | 0.03 | 0.73 | .019 | ||||
| Number of childrena | 0.91 | 0.84 | 0.99 | .033 | 0.89 | 0.81 | 0.97 | .009 | ||||||||
| HS grad and above | 1.63 | 1.10 | 2.41 | .014 | 1.57 | 1.06 | 2.33 | .025 | ||||||||
| Married/partnered | 0.72 | 0.44 | 1.16 | .172 | 0.68 | 0.41 | 1.13 | .137 | ||||||||
| Rent and other arrangement | 1.55 | 1.00 | 2.41 | .048 | 1.46 | 0.93 | 2.28 | .101 | ||||||||
| Incomea | 0.95 | 0.86 | 1.05 | .297 | .97 | 0.87 | 1.07 | .536 | ||||||||
| Medicaid | 1.16 | 0.74 | 1.81 | .531 | 1.18 | 0.74 | 1.89 | .482 | ||||||||
| TriCare | 0.56 | 0.22 | 1.42 | .22 | 0.48 | 0.19 | 1.19 | .111 | ||||||||
| Private long-term care insurance | 1.27 | .65 | 2.48 | .491 | 1.17 | 0.56 | 2.43 | .677 | ||||||||
| Number of helpersa | 1.02 | 0.96 | 1.08 | .547 | ||||||||||||
| Fall | 1.51 | 1.03 | 2.20 | .035 | ||||||||||||
| Activity limitationa | 0.97 | 0.92 | 1.01 | .152 | ||||||||||||
| Multimorbidity | 0.82 | 0.54 | 1.25 | .359 | ||||||||||||
| Proxy respondent | 1.44 | 0.96 | 2.15 | .081 | ||||||||||||
Notes: CI = confidence interval; HS = high school; LL = lower limit; SHR = subhazard ratio; UL = upper limit. N = 303. Income was log-transformed.
aVariables were measured as continuous.
Figure 1.
Cumulative incidence of transitioning out of the community proportional with respect to receiving paid care. This plot was generated analyzing the crude model with no covariates. The crude model used unimputed data due to the restriction of the statistical package (i.e., Stata) not allowing the estimated cumulative incidence of outcome variable (i.e., stcurve) to be plotted while using imputed data (i.e., mi estimate) and competing risk model (i.e., stcrreg). NHATS = National Health and Aging Trends Study.
Discussion
This study attempted to document whether there was racial difference in paid care service use and to determine the relationship between receiving paid care and transitioning out of the community. The overall finding is that receiving paid care was significantly associated with reduced risk of transitioning out of the community, supporting the hypothesis that paid care represents an enabling factor. With regard to racial differences, Black and White individuals with dementia showed similar rates of paid care despite evidence of greater care needs among Black participants. Black older adults with dementia were less likely to transition out of the community.
Racial Differences in Paid Care
The finding of no Black–White difference in the receipt of paid care despite evidence that Black older adults with dementia had greater care needs than Whites indicates a potential disparity in paid care access or utilization. Specifically, Black participants used a larger number of helpers to meet their care needs and were more likely than White participants to require a proxy respondent for medical reasons. The disconnect between evidence of greater care needs among Blacks without a corresponding increase in paid care could be related to our finding that Black individuals with dementia evidenced lower socioeconomic status than Whites across all metrics. Previous research has suggested that racial differences in paid care were associated with affordability (Johnson & Wang, 2019). Thus, Black families may lack the financial resources needed to make out-of-pocket expenses, such as home health aide or personal care aide, accessible (Johnson & Wang, 2019; Park & Chen, 2020).
Support for Black older adults with dementia is often provided by family and friends, which can be fulfilling for the caregiver and more comfortable for the older adult. It is unclear if this could be attributable to preference associated with family-orientated care (Dilworth-Anderson, et al., 2020) or the availability of an informal caregiver network. It may be that a reliance on family, combined with paid help, could provide a stable ecosystem for care even with progressive cognitive and functional decline (Chi et al., 2019). Attention should focus on Black older adults with dementia who have unmet needs particularly due to lower financial resources. Economic challenges could lead to underutilization of paid care, placing significant strain on the family (Johnson & Wang, 2019). As mentioned, studies have indicated the association of high stress of caregivers of adults with dementia, thus neglecting the caregivers of this population can lead to compassion fatigue and burnout (Lynch et al., 2018). The implications indicate a risk for poor generational health outcomes related to stress and economic strain (Aranda et al., 2021). Attention should remain on the needs of Black older adults with dementia and their network of caregivers to develop plausible policies and programs that make paid care services accessible. The risk for continued structural violence persists if policies delineating the criteria for the eligibility and funding of social programs are left unattended (DeMaio & Ansell, 2018).
Transitioning out of the Community
Another finding supported by previous research was that Black older adults with dementia were less likely to transition out of the community (Young et al., 2020), which could reflect racial differences in estimation of health care needs (Black et al., 2019), resources, and/or preference for aging in place (Thomeer et al., 2015). Remaining in the community could be attributed to trepidation around racism on Black and other minority groups when seeking institutionalized care. These experiences include more frequent use of restraints, frequent development of pressure ulcers, and more frequent hospitalizations (Sloane et al., 2021). This evidence strengthens the theory that Black caregivers may feel a sense of cultural obligation and responsibility toward their loved ones (Xu et al., 2021).
Although it is beneficial for Black and White older adults with dementia to remain in the home, the research indicates a higher level of stress for the caregivers especially as the disease progresses (Black et al., 2019). This is concerning because higher levels of stress can lead to burnout, fatigue, and loss of income due to work loss, or decreased work productivity (Aranda et al., 2021; Chi et al., 2019). Policy makers must strive to find ways to support adults with dementia while simultaneously providing effective avenues for caregivers to secure the services best suited for their circumstances.
Limitations and Strengths
As with any study, some limitations exist. First, the inability to use sample weights and the small sample size limit the generalizability of our findings, particularly for Blacks. We also chose not to interpret Hispanic–White or Hispanic–Black differences due to a very small sample size of Hispanic participants. Second, NHATS uses a combination of algorithmically derived dementia classification, as well as self/proxy reports, rather than gold-standard dementia diagnosis. Third, we could not differentiate the types of paid care (e.g., home health aide or housekeeping) or sources of payment (e.g., private insurance or out-of-pocket spending). These limitations were taken into account while drawing our interpretations. Finally, although Andersen’s model includes attitudes/beliefs as predisposing factors, we were unable to incorporate information on family preferences for aging in place. Thus, a general preference for aging in place could have confounded the causal association between paid care and transitioning of the community. However, the finding that Whites were both more likely to have paid care (after accounting for care needs) and more likely to transition out of the community suggests that preferences for aging in place are unlikely to fully explain the current pattern of results.
Nevertheless, several strengths were noted in this study. Using the NHATS data set, a racially diverse national sample contributes to the external validity of Black–White comparisons. Also by using the Andersen model, we applied a cohesive theoretical framework to incorporate a comprehensive set of covariates for this study. Lastly, we selected high-quality measures of our exposures and outcomes, which strengthens the possibility of replicating this study in the future.
Conclusion
Our study found that paid care is significantly associated with reduced transitions into LTC settings. The findings also indicate a need for further research to determine the underlying cause of racial disparities, especially contextual factors such as insurance coverage and out of pocket costs. The essential recommendation based on this study is that future research should seek to explain racial disparities in access to and differences in preferences for home-based, community-based, and residential care. In-depth studies should be conducted to delineate structural violence associated with policies that could restrict access to services.
Contributor Information
Maria Roche-Dean, Bronson School of Nursing, Western Michigan University, 1903 West Michigan Avenue, Kalamazoo, MI 49008-5345, USA.
Sol Baik, University of Virginia Weldon Cooper Center for Public Service, University of Virginia, 2400 Old Ivy Rd, Charlottesville, VA 22903, USA.
Heehyul Moon, Kent School of Social Work and Family Science, University of Louisville, 2217 S. 3rd st., Louisville, KY 40292, USA.
Norma B Coe, Department of Medical Ethics and Health Policy, University of Pennsylvania, 423 Guardian Drive, Philadelphia, PA 19104, USA.
Anna Oh, San Francisco VA Health Care System, 4150 Clement Street, San Francisco, CA 94121, USA; Department of Social and Behavioral Sciences, University of California San Francisco, 490 Illinois St., Floor 12 San Francisco, CA 94143, USA.
Laura B Zahodne, Department of Psychology, University of Michigan, 530 Church Street, Ann Arbor, MI 48109, USA.
Funding
This work was supported by the Michigan Center for Contextual Factors in Alzheimer’s Disease (MCCFAD) [P30 AG059300], funded by the National Institute on Aging of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author Contributions
M. Roche-Dean contributed to study conception, planning, and writing the article. S. Baik performed all statistical analyses, created tables and figures, and contributed to data interpretation of the article. H. Moon, A. Oh, and N. Coe helped with study conception and design, data interpretation, and technical editing. L. Zahodne planned the study, supervised the data analysis, interpretation, and provided technical editing.
Conflict of Interest
None declared.
References
- Andersen, R., & Newman, J. F. (2005). Societal and individual determinants of medical care utilization in the United States. The Milbank Quarterly, 83(4), 95–124. doi: 10.1111/j.1468-0009.2005.00428.x [DOI] [PubMed] [Google Scholar]
- Aranda, M. P., Kremer, I. N., Hinton, L., Zissimopoulos, J., Whitmer, R. A., Hummel, C. H., & Fabius, C. (2021). Impact of dementia: Health disparities, population trends, care interventions, and economic costs. Journal of the American Geriatrics Society, 69(7), 1774–1783. doi: 10.1111/jgs.17345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babitsch, B., Gohl, D., & Von Lengerke, T. (2012). Re-revisiting Andersen’s behavioral model of health services use: A systematic review of studies from 1998–2011. GMS Psycho-Social-Medicine, 9, 1–15. doi:10.3205%2Fpsm000089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black, B. S., Johnston, D., Leoutsakos, J., Reuland, M., Kelly, J., Amjad, H., & Samus, Q. M. (2019). Unmet needs in community-living persons with dementia are common, often non-medical and related to patient and caregiver characteristics. International Psychogeriatrics, 31(11), 1643–1654. doi: 10.1017/S1041610218002296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewster, G. S., Bonds, K., McLennon, S., Moss, K. O., Epps, F., & Lopez, R. P. (2020). Missing the mark: The complexity of African American dementia family caregiving. Journal of Family Nursing, 26(4), 294–301. doi: 10.1177/1074840720945329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanova, M. (2021). Revisiting the role of gender and marital status as risk factors for nursing home entry. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 76(Suppl. 1), S86–S96. doi: 10.1093/geronb/gbab004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi, W., Graf, E., Hughes, L., Hastie, J., Khatutsky, G., Shuman, S., & Lamont, H. (2019). Community-dwelling older adults with dementia and their caregivers: Key indicators from the National Health and Aging Trends Study. U.S. Department of Health and Human Services.
- Cloutier, M., Gauthier-Loiselle, M., Gagnon-Sanschagrin, P., Guerin, A., Hartry, A., Baker, R. A.,... & Alzheimer’s Disease Neuroimaging Initiative. (2019). Institutionalization risk and costs associated with agitation in Alzheimer’s disease. Alzheimer’s & Dementia: Translational Research & Clinical Interventions, 5, 851–861. doi: 10.1016/j.trci.2019.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, A., & Bulanda, J. R. (2016). Social supports as enabling factors in nursing home admissions: Rural, suburban, and urban differences. Journal of Applied Gerontology, 35(7), 721–743. doi: 10.1177/0733464814566677 [DOI] [PubMed] [Google Scholar]
- DeMaio, F., & Ansell, D. (2018). “As natural as the air around us”: On the origin and development of the concept of structural violence in health research. International Journal of Health Services, 48(4), 749–759. doi: 10.1177/0020731418792825 [DOI] [PubMed] [Google Scholar]
- Dilts, A., Winter, Y., Biebricher, T., Johnson, E. V., Vázquez-Arroyo, A. Y., & Cocks, J. (2012). Revisiting Johan Galtung’s concept of structural violence. New Political Science, 34(2), e191–e227. doi: 10.1080/07393148.2012.714959 [DOI] [Google Scholar]
- Dilworth-Anderson, P., Moon, H., & Aranda, M. P. (2020). Dementia caregiving research: Expanding and reframing the lens of diversity, inclusivity, and intersectionality. The Gerontologist, 60(5), 797–805. doi: 10.1093/geront/gnaa050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabius, C. D., & Thomas, K. S. (2019). Examining black–white disparities among Medicare beneficiaries in assisted living settings in 2014. Journal of the American Medical Directors Association, 20(6), 703–709. doi:10.1016%2Fj.jamda.2018.09.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fine, J. P., & Gray, R. J. (1999). A proportional hazards model for the subdistribution of a competing risk. Journal of the American Statistical Association, 94(446), 496–509. doi: 10.1080/01621459.1999.10474144 [DOI] [Google Scholar]
- Gaugler, J. E., Yu, F., Krichbaum, K.,& Wyman, J. F. (2009). Predictors of nursing home admission for persons with Dementia. Medical Care, 47(2), 191–198. http://www.jstor.org/stable/40221859 [DOI] [PubMed] [Google Scholar]
- Gelberg, L., Andersen, R. M., & Leake, B. D. (2000). The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Services Research, 34(6), 1273–302. [PMC free article] [PubMed] [Google Scholar]
- Gilligan, A. M., Malone, D. C., Warholak, T. L., & Armstrong, E. P. (2013). Health disparities in cost of care in patients with Alzheimer’s disease: An analysis across 4 state Medicaid populations. American Journal of Alzheimer’s Disease & Other Dementias, 28(1), 84–92. doi: 10.1177/1533317512467679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammonds, E. M., & Reverby, S. M. (2019). Toward a historically informed analysis of racial health disparities since 1619. American Journal of Public Health, 109(10), 1348–1349. doi: 10.2105/AJPH.2019.305262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, R. W., & Wang, C. X. (2019). The financial burden of paid home care on older adults: Oldest and sickest are least likely to have enough income. Health Affairs, 38(6), 994–1002. doi: 10.1377/hlthaff.2019.00025 [DOI] [PubMed] [Google Scholar]
- Kasper, J. D. & Freedman, V. A. 2021. National Health and Aging Trends Study user guide: Rounds 1–10 final release. Johns Hopkins University School of Public Health.www.NHATS.org. [Google Scholar]
- Kasper, J. D., Freedman, V. A., Spillman, B. C., & Wolff, J. L. (2015). The disproportionate impact of dementia on family and unpaid caregiving to older adults. Health Affairs, 34(10), 1642–1649. doi: 10.1377/hlthaff.2015.0536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman, J. E., Gallo, W. T., & Fahs, M. C. (2020). The contribution of dementia to the disparity in family wealth between black and non-black Americans. Ageing & Society, 40(2), 306–327. doi: 10.1017/S0144686X18000934 [DOI] [Google Scholar]
- Kelley, A. S., McGarry, K., Gorges, R., & Skinner, J. S. (2015). The burden of health care costs for patients with dementia in the last 5 years of life. Annals of Internal Medicine, 163(10), 729–736. doi: 10.7326/M15-0381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luppa, M., Luck, T., Weyerer, S., König, H. H., Brähler, E., & Riedel-Heller, S. G. (2010). Prediction of institutionalization in the elderly. A systematic review. Age and Ageing, 39(1), 31–38. doi: 10.1093/ageing/afp202 [DOI] [PubMed] [Google Scholar]
- Lynch, S. H., Shuster, G., & Lobo, M. L. (2018). The family caregiver experience—Examining the positive and negative aspects of compassion satisfaction and compassion fatigue as caregiving outcomes. Aging & Mental Health, 22(11), 1424–1431. doi: 10.1080/13607863.2017.1364344 [DOI] [PubMed] [Google Scholar]
- Montaquila, J., Freedman, V. A., Edwards, B., & Kasper, J. D. (2012). National Health and Aging Trends Study round 1 sample design and selection. NHATS Technical Paper, 1, 1–8. [Google Scholar]
- Moon, H., Rote, S., & Haley, W. E. (2018). Factors that contribute to remaining in the community among older adults. Aging & Mental Health, 22(11), 1502–1509. doi: 10.1080/13607863.2017.1363869 [DOI] [PubMed] [Google Scholar]
- NHATS Data Collection Procedures: Round 1, 2011. Funded by the National Institute on Aging (U01AG032947 ). www.nhats.org. [Google Scholar]
- Park, S., & Chen, J. (2020). Racial and ethnic patterns and differences in health care expenditures among Medicare beneficiaries with and without cognitive deficits or Alzheimer’s disease and related dementias. BMC Geriatrics, 20(1), 1–11. doi: 10.1186/s12877-020-01888-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reckrey, J. M., Federman, A. D., Bollens-Lund, E., Morrison, R. S., & Ornstein, K. A. (2020). Homebound status and the critical role of caregiving support. Journal of Aging & Social Policy, 32(6), 590–603. doi: 10.1080/08959420.2019.1628625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reckrey, J. M., Morrison, R. S., Boerner, K., Szanton, S. L., Bollens-Lund, E., Leff, B., & Ornstein, K. A. (2020). Living in the community with dementia: Who receives paid care? Journal of the American Geriatrics Society, 68(1), 186–191. doi: 10.1111/jgs.16215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiekh, S. I., Cadogan, S. L., Lin, L. Y., Mathur, R., Smeeth, L., & Warren-Gash, C. (2021). Ethnic differences in dementia risk: A systematic review and meta-analysis. Journal of Alzheimer’s Disease, 80(1), 337–355. doi:10.3233%2FJAD-201209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloane, P. D., Yearby, R., Konetzka, R. T., Li, Y., Espinoza, R., & Zimmerman, S. (2021). Addressing systemic racism in nursing homes: A time for action. Journal of the American Medical Directors Association, 22(4), 886–892. doi: 10.1016/j.jamda.2021.02.023 [DOI] [PubMed] [Google Scholar]
- StataCorp. (2019). Stata statistical software (Version 16) (computer software). StataCorp LLC.https://www.stata.com/ [Google Scholar]
- StataCorp. (2021). Stata survey data reference manual: Release 17. Stata Press. [Google Scholar]
- Szanton, S. L., Walker, R. K., Roberts, L., Thorpe Jr, R. J., Wolff, J., Agree, E., & Seplaki, C. (2015). Older adults’ favorite activities are resoundingly active: Findings from the NHATS study. Geriatric Nursing, 36(2), 131–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomeer, M. B., Mudrazija, S., & Angel, J. L. (2015). How do race and Hispanic ethnicity affect nursing home admission? Evidence from the Health and Retirement Study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 70(4), 628–638. doi: 10.1093/geronb/gbu114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu, L., Lee, Y., Kim, B. J., & Chen, L. (2021). Determinants of discretionary and non-discretionary service utilization among caregivers of people with dementia: Focusing on the race/ethnic differences. Home Health Care Services Quarterly, 40(1), 75–92. doi: 10.1080/01621424.2020.1805083 [DOI] [PubMed] [Google Scholar]
- Yan, D., Wang, S., Temkin-Greener, H., & Cai, S. (2021). HCBS service spending and nursing home placement for patients with Alzheimer’s disease and related dementias: Does race matter? Journal of Applied Gerontology, 41(3), 638–649. doi: 10.1111/1475-6773.13353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young, Y., Papenkov, M., Hsu, W. H., Shahid, F., & Kuo, Y. H. (2020). Permanent transition of homecare recipients with dementia to nursing homes in New York State: Risk factors. Geriatric Nursing, 41(5), 553–558. doi: 10.1016/j.gerinurse.2020.02.006 [DOI] [PubMed] [Google Scholar]