Abstract
Cross-sectional analyses of 904 diverse men and women aged 50 years and older living with HIV in New York City were conducted to examine the unique experiences and needs of aging HIV-positive individuals. Using Minority Stress Theory and Syndemic Theory as guiding paradigms, the authors documented the mental health burdens of the sample with regard to depression, loneliness, and diminished psychological well-being and examined how multiple-minority status and HIV-related stigma explained these burdens. Mediation modeling demonstrated that the effects of minority stressors on mental health burden were mediated by HIV-related stigma. The mediation was significant for the overall sample and for the male subsample. Results suggest that to fully address the mental health burdens experienced by aging HIV-positive individuals, we must continue to address mental health burdens directly, and at the same time, look beyond the psychiatric symptoms to address the structural inequities faced by individuals based on their multiple-minority status.
Keywords: aging, AIDS, HIV, mental health, multiple-minority, stigma
INTRODUCTION
In the United States, the number of individuals living with HIV who are aged 50 and older continues to grow. As of 2009, in the 40 states with confidential HIV infection reporting, approximately 178,000 individuals living with HIV were aged 50 and older, and represented approximately 27% of all seropositive individuals, while those within that age group constituted 48% of all those diagnosed with AIDS (Centers for Disease Control and Prevention [CDC], 2009). This is in sharp contrast to the 17% who were infected with HIV and were aged 50 years and older in 2001 (CDC, 2008). Moreover, approximately 40% of those living with HIV are currently aged 40 to 49 (CDC, 2009), suggesting that, within a decade, seropositive individuals aged 50 and older will constitute the majority infected in the United States.
The “graying of AIDS” is due primarily to advances in antiretroviral treatment and partially to the increase in the number of new infections detected in individuals over age 50 (CDC, 2008). As is the case with the HIV/AIDS epidemic across all age ranges, the epidemic disproportionately affects ethnic and racial minorities, specifically blacks and Hispanics. Among these groups, the rates of HIV infection are, respectively, 12 and 5 times higher than that of whites aged 50 and over (CDC, 2008). Similar patterns are noted in urban epicenters such as New York City, where as of December 2009, approximately 40% were aged 50 and older, and another 35% were aged 40 to 49 (New York City Department of Health and Mental Hygiene [NYCDOHMH], 2010). By 2015, HIV-positive individuals aged 50 and older will constitute 50% of those infected nationally and locally (Kirk & Goetz, 2009). However, this vulnerable population remains understudied and underserved and must be considered in the design of HIV prevention programs (Halkitis, 2010), as well as services that address the realities of aging and HIV disease.
People living with HIV/AIDS often confront stigma related to their disease, which manifests itself in employment or housing discrimination, emotional or physical abuse, abandonment, rejection, loss of intimacy, and the inability to form and sustain relationships (Adimora & Auerbach, 2010). Many HIV-positive individuals internalize these societal burdens and manifest them as feelings of guilt and self-hatred (Lee, Kochman, & Sikkema, 2002). HIV-related stigma is also intricately linked with other forms of stigma related to minority status, including sexism, racism, homophobia, ableism, and ageism. However, as noted by Sandelowski, Barroso, and Voils (2009), HIV research often focuses on one stigmatized identity over others in an “either/or” assumption rather than a “both/and” paradigm. In effect, what is missing from the extant literature is an examination of how multiple-minority identities, in tandem, contribute to the experience of stigma among HIV-positive individuals, and whether those with a greater number of such identities experience higher levels of stigma due to their HIV status. This is to say that the experience of stigma may not be uniform for all HIV-positive people, but is likely affected by the other identities (i.e., gender, race, class, age, sexual orientation, etc.) that the person holds. This idea has been illuminated in the examination of the complex interactive effects of age and race on coping, stigma, and mental health among gay men (David & Knight, 2008).
Moreover, stigma and discrimination have often been studied separately, but social scientists recommend bridging these two related concepts (Stuber, Meyer, & Link, 2008). In the current literature, the “double jeopardy hypothesis” refers to the concept that possessing more than one socially marginalized identity will place individuals at increased risk for HIV and a spectrum of mental health problems (Pak, Dion, & Dion, 1991). However, among older, multiple-minority individuals currently living with HIV, the extent to which mental health problems result from the amount of HIV-related stigma they experience has yet to be studied within the broader contextual experience of discrimination.
Minority Stress Theory (Meyer, 1995, 2003) provides one paradigm from which to examine the cumulative effects of minority stressors on the well-being of HIV-positive individuals. From a conceptual perspective, minority stress theory maintains that individuals who have non-mainstream identities, such as gay men and/or racial/ethnic minorities, are at risk for increased levels of mental health problems, which, in turn, influence HIV risk-taking behaviors (Meyer, 1995). Minority Stress Theory asserts that stigma, prejudice, and discrimination create a hostile and stressful social milieu, and that these stressors are evidenced in multiple domains including but not limited to educational environment, political systems, employment, and health care settings, as well as housing. Meyer attributes the disparity in mental illness to the repeated occurrence of injustice among minority populations in these and other contexts. In essence, Minority Stress Theory posits that it is the unequal treatment of minority groups that is responsible for mental health problems. The Minority Stress model describes stress processes, including the experience of prejudice events, expectations of rejection, hiding and concealing, internalized homophobia, and ameliorative coping processes (Meyer, 2003). However, the paradigm has, to date, been limited to understandings of minority stress in gay, bisexual, and other men who have sex with men.
Finally, these findings also support the Syndemic Theory, which posits that multiple stressors, stigmas, and experiences of discrimination interact with issues of poverty, violence, sexual risk-taking, and drug use to produce greater difficulties in effectively navigating HIV transmission risk (Singer, 1994, 1996). In particular, Singer (1994, 1996) holds that HIV disproportionately affects those individuals in communities who are already disproportionately affected by issues of racism, poverty, mental health concerns, and poor access to health care. Stall, Friedman, and Catania (2008) extended this theory to explore the possibility of syndemic production developmentally among gay and bisexual men. Taken together, these theories underscore the importance of exploring other potentially marginalized identities to gain a better understanding of the unique experiences and needs of HIV-positive individuals as they age.
In the current analysis, the relation among multiple-minority status, perceived HIV-related stigma, and mental health burden, including depression, loneliness, and quality of life, is examined among a diverse group of aging HIV-positive individuals, both male and female, and of varied sexual orientations. Specifically, this analysis (a) examines the prevalence of multiple-minority statuses among men and women aged 50 years and older, living with HIV; (b) documents the mental health burdens in the sample; (c) delineates the association between multiple-minority status, HIV-related stigma, and mental health burden; and (d) assesses whether HIV-related stigma mediates the relation between multiple-minority status and mental health burden.
METHOD
Procedures
The Research on Older Adults with HIV (ROAH) study was conducted in 2005–2006 by the AIDS Community Research Initiative in America (ACRIA) to better understand the nuances and identify the needs of older HIV-positive people in New York City (Brennan, Karpiak, Shippy, & Cantor, 2009). The Copernicus Group Independent Review Board approved the methodology and protocols. Participants were sourced through local AIDS service organizations (ASOs), clinics, as well as the ACRIA database. The ACRIA database contains data on more than 1,500 older adults living with HIV/AIDS who have expressed interest in participating in clinical and behavioral research studies. Recruitment efforts included the use of flyers, mail, e-mail, and information sessions about the study.
Participants
To be eligible for the study, participants were required to (a) be HIV-positive, (b) be age 50 or older, (c) reside in or receive HIV-related health care in New York City, (d) not be cognitively impaired, (e) be fluent in English, and (f) be community-dwelling (i.e., not institutionalized). Those who were eligible and consented to be in the study completed a self-administered pen-and-paper survey. Survey administration occurred at ACRIA or other community-based organizations in the New York City area. At survey completion, participants received a $25 incentive for their time. Data were collected from 1000 participants. However, once data from unusable surveys were removed, information from a total of 914 eligible participants was included in the dataset.
Measures
Demographic characteristics
Participants self-reported age, gender, sexual orientation, disability status, race/ethnicity, immigration status, first language, and income. For analysis, we divided men and women and removed transgender individuals (n = 10) due to there being a small number in the study for a total of 904 individuals (264 women and 640 men) in the analysis.
HIV-related stigma
Participants’ experience of HIV-related stigma was assessed using the Berger’s Stigma Scale (Berger, Ferrans, & Lashley, 2001), which is a 40-item measure with four subscales used to measure personalized stigma, disclosure concerns, negative self-image, and concern with public attitudes about HIV. Participants rated their response to the HIV-related stigma questions on 4-point Likert-type scales with ratings ranging from 1 (strongly disagree) to 4 (strongly agree). A previous psychometric assessment found the extraction of one higher order factor revealing the presence of a single overall construct—HIV-related stigma, and thus we used a composite of all subscales. Construct validity was demonstrated by previous associations with related constructs. Berger’s stigma scale also was shown to have high internal-consistency reliability (Berger et al., 2001). In the current study, sum scores were calculated and the measure demonstrated high internal consistency (α = .87).
Depression
Study participants were assessed via the Center for Epidemiologic Studies–Depression Scale (CES-D; Radloff, 1977), which is a 20-item measure used to assess depressive symptomatology within the general population. Items assessed symptoms such as level of sadness, crying spells, depression, and poor appetite, and Likert-type responses ranged from 0 (Rarely or none of the time [less than 1 day]) through 3 (Most or all of the time [5–7 days]). The CES-D has been shown to have high internal consistency, adequate test-retest reliability, and evidence of construct validity, and the factor structure has been shown to remain stable across demographics (Radloff, 1977). In the current study, sum scores were calculated and the measure demonstrated high internal consistency (α = .87).
Loneliness
Participants were assessed using the UCLA Loneliness Scale (Version 3; Russell, 1996). This measure uses 20 items to assess level of loneliness. Examples include how often participants feel shy, outgoing, or alone. Answer options range from 1 (Never) through 4 (Always). This measure has been shown to have high internal consistency and test-retest reliability, as well as convergent and construct validity (Russell, 1996). In the current study, sum scores of the 20 items were calculated and the measure demonstrated high internal consistency (α = .90).
Psychological well-being
The Ryff Scales of Psychological Well-Being (Ryff & Keyes, 1995) were used to assess multiple facets of well-being. Six areas of well-being were measured, and items were measured on a 6-item scale ranging from 1 (Strongly disagree) to 6 (Strongly agree). Higher scores represent higher levels of mastery in the specified area. The developers report adequate internal consistency and test-retest reliability for the scales; the internal consistency for the current study was as follows: autonomy (α = .76), environmental mastery (α = .75), personal growth (α = .71), positive relations with others (α = .74), purpose in life (α = .71), and self-acceptance (α = .75).
Computed Measures
To assess for the additive effects of multiple-minority statuses, we dichotomized each demographic identity for both men and women with each of the following coded as a minority burden: (a) gay or bisexual orientation; (b) disabled status; (c) identifying as nonwhite; (d) being born in a country other than the United States; (e) speaking English as second language and not as primary language; and (f) with regard to poverty status, reporting having just enough money to get by or not having enough money to get by. The six minority statuses were then tallied for each participant to assign a total minority burden score (ranging from 0 to 6) to each of the participants.
Similarly, the eight mental health burden scales were each dichotomized using the published cut score of 50 for the UCLA Loneliness scale (Turkinaz, Magfiret, Gulay, & Behice, 2006) and 16 for the CES-D (Pandya, Metz, & Patten, 2005), and a median split was used for each of the six subscales of the Ryff to reduce the number of false positives as recommended by September, McCarrey, Baranowsky, Parent, and Schindler (2001). A lower than median score on each of the Ryff subscales indicated a lower quality of life rating in that domain, and was thus considered indicative of mental health burden. The eight dichotomous scores were then tallied for each participant to assign a total mental health burden score (ranging from 0 to 8) for each of the participants.
Analytic Plan
We first computed descriptive statistics of the sample and examined differences across each minority status variable in relation to gender using χ2 tests of independence. This was followed by nonparametric analyses examining gender in relation to each mental health burden. Independent-samples t tests were used to examine differences between women and men on mental health burden scores, minority burden scores, and stigma scores. Then, correlation analysis was used to examine the relation between minority burden score, mental health burden score, and perceived HIV-related stigma score. Finally, mediation analyses as outlined by Baron and Kenny (1986) were undertaken to examine whether HIV-related stigma mediates the relation between minority status burden and mental health burden for the entire sample and each gender separately.
RESULTS
Our sample consisted of 904 HIV-positive participants, of whom 640 were men and 264 were women. The average age for the entire sample was 55.53 years (SD = 4.88 years), with a median age of 54 years (range, 50 to 78 years). Among the men in our sample, the average age was 55.69 years (SD = 4.98 years), while among the women, the average age was 55.15 years (SD = 4.64 years). No difference in average age was detected across gender. The majority of our sample had a high school diploma or less (49.67%, n = 449), followed by those who had either attended some college or obtained a college degree (37.17%, n = 336). The remaining participants had either attended graduate school (8.85%, n = 80) or obtained some kind of vocational or other postsecondary education (3.65%, n = 33). Education was different by gender [χ2(3) = 21.87, p < .001], with more men reporting having a high school degree, some college, or a graduate school education than women.
Multiple-Minority Statuses
Table 1 presents the demographics of the current sample. In relation to race/ethnicity, 87.1% (n = 784) identified as nonwhite, with 94.7% (n = 248) of women identifying as nonwhite and 84.0% (n = 536) of men identifying as nonwhite. There was a statistically significant difference between the number of women identifying as nonwhite and the number of men identifying as nonwhite [χ2(1) = 18.74, p < .001]. Among the sample, 32.6% (n = 277) identified as gay, lesbian, or bisexual. There was a statistically significant difference between the number of men and the number of women identifying as non-heterosexual [χ2(1) = 46.50, p < .001], with 39.6% (n = 239) of men identifying as gay or bisexual and 15.4% (n = 38) of women identifying as lesbian or bisexual. In relation to national origin, there was a statistically significant difference between men and women [χ2(1) = 3.88, p = .05], with 18.5% (n = 117) of men noting they were born outside of the United States compared with 13% (n = 34) of women. Overall, 16.9% (n = 151) of our sample was non-U.S. born. No statistically significant differences were found among the sample in relation to primary language. Table 1 illustrates that a majority of the sample identified English as their primary or native language. Likewise, a majority of the sample participants did not believe they had an adequate income. There were no statistically significant differences observed between men and women in relation to either their primary language or the perceived adequacy of their income to cover their expenses.
TABLE 1.
Minority Status Burdens of HIV-Positive Men and Women Aged 50 Years and Over (N = 904)
| Female (n = 264) No. (%) |
Male (n = 640) No. (%) |
Total (N = 904) No. (%) |
|
|---|---|---|---|
| Race*** | |||
| Nonwhite | 248 (94.7) | 536 (84.0) | 784 (87.1) |
| Sexual orientation*** | |||
| Not straight | 38 (15.4) | 239 (39.6) | 277 (32.6) |
| Disability | |||
| Disabled | 136 (51.5) | 345 (53.9) | 481 (53.2) |
| National origin* | |||
| Born outside the United States | 34 (13.0) | 117 (18.5) | 151 (16.9) |
| Primary language | |||
| Non-native English speaker | 40 (16.6) | 108 (18.3) | 148 (17.8) |
| Perceived income | |||
| Inadequate income | 178 (71.8) | 468 (77.2) | 646 (75.6) |
p < .05,
p < .01,
p < .001.
Mental Health Burdens
Table 2 presents the χ2 analyses that were conducted on the dichotomized mental health burden variables to determine if there were differences between men and women. For loneliness, depression, personal growth, and autonomy, there were no significant differences found. However, men reported higher levels of burden than women with regard to lack of positive relations with others [χ2(1) = 10.23, p < .01], purpose in life [χ2(1) = 9.84, p < .01], self-acceptance [χ2(2) = 5.03, p < .05], and environmental mastery [χ2(1) = 17.15, p < .001].
TABLE 2.
Mental Health Burdens of HIV-Positive Men and Women Aged 50 Years and Older (N = 904)
| Female (n = 264) No. (%) |
Male (n = 640) No. (%) |
Total (N = 904) No. (%) |
|
|---|---|---|---|
| Experience of loneliness | 72 (28.1) | 205 (33.6) | 277 (32.0) |
| Experience of depression | 121 (61.1) | 305 (60.6) | 426 (60.5) |
| Lack of positive relations with others** | 102 (38.6) | 322 (50.3) | 424 (46.9) |
| Lack of purpose in life** | 103 (39.0) | 323 (50.5) | 426 (47.1) |
| Lack of self-acceptance* | 112 (42.4) | 324 (50.6) | 436 (48.2) |
| Lack of environmental mastery** | 92 (34.8) | 340 (53.1) | 432 (47.8) |
| Lack of personal growth | 119 (45.1) | 309 (48.3) | 428 (47.3) |
| Lack of autonomy | 115 (43.6) | 303 (47.3) | 418 (46.2) |
p < .05,
p < .001.
Relations Among Total Minority Burden, Total Mental Health Burden, and HIV-Related Stigma
Next we considered the relations between the computed variables of total minority burden and total mental health burden with HIV-related stigma in relation to gender. There was no significant difference found between men and women with respect to perceived HIV-related stigma. However, there was a significant difference found regarding the total minority burden score [t(902) = 2.61, p < .05], with the men (M = 2.90, SD = 1.07) reporting significantly more minority statuses than the women (M = 2.69, SD = 1.06). A significant difference was also found regarding total mental health burden [t(902) = 3.03, p < .01], with the men (M = 3.81, SD = 2.76) reporting significantly more mental health burden than the women (M = 3.12, SD = 2.62).
Mediation Analysis
We built mediation models to examine whether HIV-related stigma mediates the relation between minority status and mental health burden. As a preliminary step, we examined the relations between the variables and found a significant association between total mental health burden score and total minority burden score (r = .17, p < .001), total mental health burden score and total HIV-related stigma score (r = .49, p < .001), as well as total HIV-related stigma score and total minority burden score (r = .10, p < .01).
The first mediation model was tested for the entire sample. Simple linear regression established a significant relation between total minority burden score and total mental health burden score: F(1, 607) = 17.28, p < .001. A significant mediation was detected (Sobel test = 2.62, p < .001) where total HIV-related stigma score mediated the relation between total minority burden score and total mental health burden score (Figure 1).
FIGURE 1.
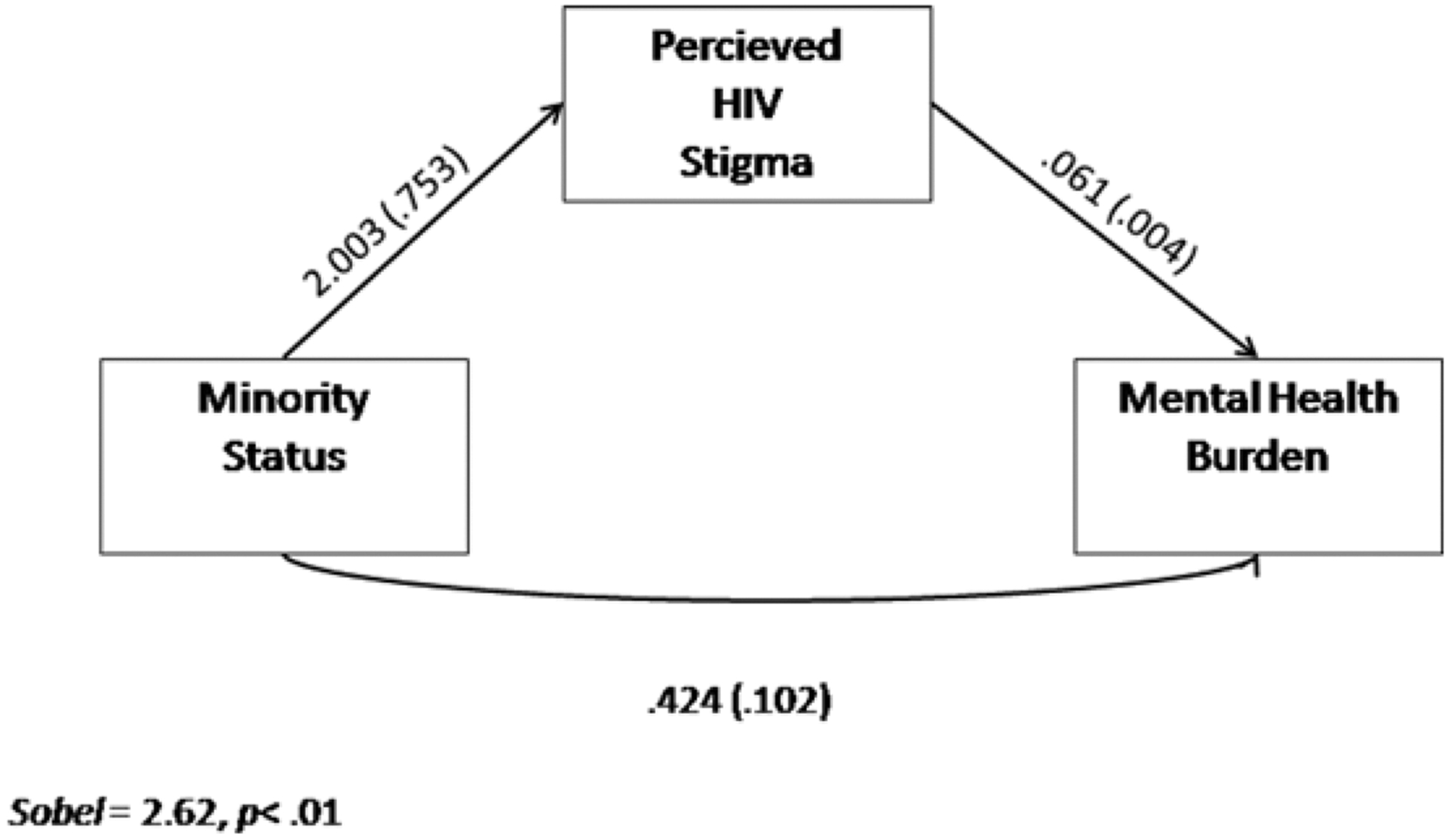
Mediation model (total sample).
Analyses were then conducted separately for the male and female sub-samples. For the male subsample, a relation was established between total minority burden score and total mental health burden score: F(1, 437) = 20.02, p < .001, and a significant mediation effect was again detected for total HIV-related stigma score (Sobel test = 2.36, p = .02; Figure 2). Simple regression of total minority status score on total mental health burden score failed to achieve significance for the female subsample, and thus mediation analysis was not undertaken.
FIGURE 2.
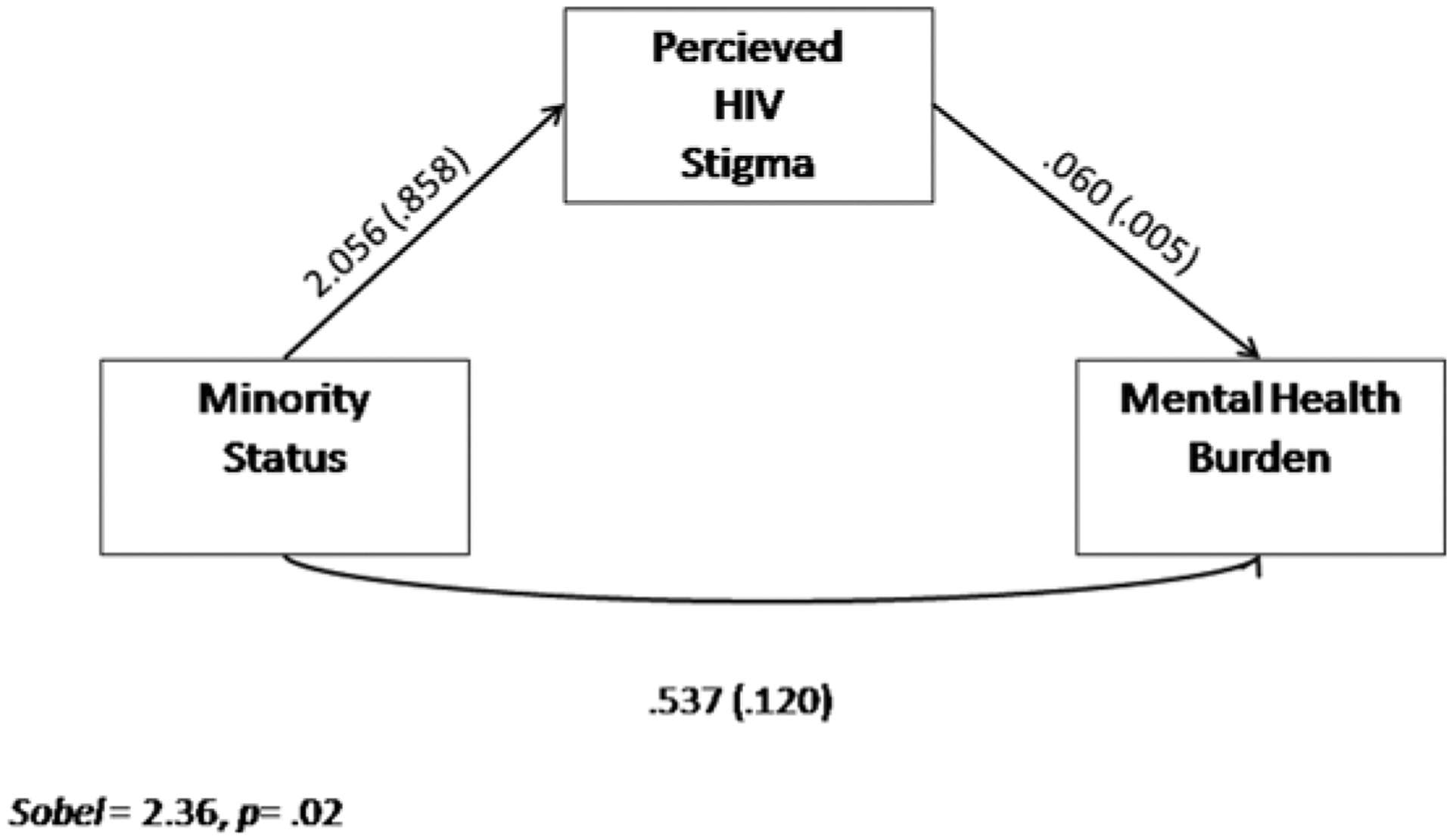
Mediation model (men only).
DISCUSSION
The current analyses establish a clear relation among multiple-minority status, perceived HIV-related stigma, and mental health burden. Results demonstrate that among this aging HIV-positive population, individuals with a greater number of minority burdens exhibit an increased experience of HIV-related stigma, which in turn is associated with increases in mental health burden. The current analyses also reveal that HIV-related stigma mediates the relation between minority status and mental health burden. That is, while minority status is significantly associated with mental health burden, those of minority demographic background experience an increase in mental health burden as a result of the increased level of HIV-related stigma they experience. These data suggest that it is the existent experience of discrimination, oppression, and marginalization related to one’s multiple-minority status that places older HIV-positive individuals at elevated risk for experiencing HIV-related stigma. Accordingly, these data indicate that HIV-positive multiple-minority individuals are experiencing more HIV-related stigma than are HIV-positive single or nonminority individuals. Finally, the current data indicate that the experience of HIV-related stigma is significantly associated with loneliness, depression, and lowered overall psychological well-being.
The current findings are consistent with those of Hatzenbuehler, O’Cleirigh, Mayer, Mimiaga, and Safren (2011) in that the experience of HIV-related stigma is shown to increase mental health burden and also extend the application of Minority Stress Theory to a diverse group of individuals living with HIV. It is not surprising given the complex manner in which economic and social factors, such as homophobia, racism, sexism, and poverty, fuel the HIV-epidemic (Adimora & Schoenbach, 2005) that identifying with multiple-minority backgrounds was found to be significantly associated with an increase in mental health burden among the aging HIV-positive population. What was less expected is that it was not merely the experience of belonging to multiple marginalized, discriminated, and oppressed minority statuses that explained the increase in depression, loneliness, and the decrease in overall quality of life among this sample. Rather, it was the totality of minority status burdens and their complex interaction with the experience of HIV-related stigma that explained the disparity in mental health burden. That is, for the entire sample, the effects of multiple-minority burdens imparted their effect on mental health burden through the experience of HIV-related stigma.
The current findings extend previous work that has shown that older individuals living with HIV often exhibit severe mental health burdens, which are tied to a variety of physical and psychosocial factors related to both aging and the HIV illness. Older HIV-positive individuals face multiple stigmas and often lack social support, which relates to many mental health burdens including suicidal ideation (Kalichman, Heckman, Kochman, Sikkema, & Bergholte, 2000; Shippy & Karpiak, 2005). Many older people living with HIV have experienced the loss of friends and loved ones to HIV/AIDS and suffer from AIDS-related bereavement, which also is linked with depression (Wight, 2000) and PTSD (Theuninck, Lake, & Gibson, 2010). Older people who have been living with HIV on a long-term basis may also feel isolated from HIV support because support groups and outreach often target newly positive individuals and younger people (Bhavan, Kampalath, & Overton, 2008). The current study demonstrated that it is likely the HIV-related stigma experienced by those of multiple-minority backgrounds that significantly increases their mental health burden and that the experience of mental health burden may not be monolithic in the population of older adults living with HIV. Said differently, those who navigate multiple-minority identities are likely to also experience heightened mental health problems because they also experience heightened levels of HIV-related stigma.
The limited amount of research that exists on older HIV-positive individuals in the United States often focuses solely on issues of ageism and/or HIV-stigma (Emlet, 2006). However, the current findings underscore the importance of understanding, not just the experiences of these two types of stigma in the lives of HIV-positive individuals, but also the impact that various other socially stigmatized identities may have in the lives of persons who are HIV-positive. From a clinical perspective, it is important to note the impact that the presence of multiple stigmatized identities may have on issues of mental health and how other possible experiences of discrimination may affect HIV-stigma (Rao, Pryor, Gaddist, & Mayer, 2008), which has been shown to be related to issues of mental health in both HIV-positive men and women (Logie & Gadalla, 2009; Vanable, Carey, Blair, & Littlewood, 2006).
Singer (1994; 1996) notes that illnesses like HIV are not democratic and often occur within communities that are already overly disadvantaged and/or stigmatized. It follows that these community disadvantages would continue into, and be further exacerbated by, older age. The current data support the reality that as HIV-positive individuals grow older, issues of race, ethnicity, culture, and socioeconomic status continue to play an important role in social interactions. In line with this, Emlet (2007) found that older, African American men who were HIV-positive endorsed higher levels of stigma than their white counterparts, with stigma being positively related to higher levels of depression within the entire sample. Furthermore, research supports that among Asian and Pacific Islander men, immigration status impacts one’s experience of HIV stigma (Kang, Rapkin, & DeAlmeida, 2006; Kang, Rapkin, Remien, Mellins, & Oh, 2005), with an undocumented status increasing such dimensions of HIV stigma as social rejection and perceived interpersonal insecurity. Given these results among HIV-positive men, it is important to extend our line of research exploring the impact of multiple, stigmatized identities among HIV-positive women in the literature (Sandelowski et al., 2009). Further study of the ways in which overlapping, socially stigmatized identities may impact such factors as HIV stigma and mental health among HIV-positive, older women is currently warranted. These understandings are critical since the HIV-epidemic disproportionately affects gay and bisexual men, especially men of color, as well as African American women (CDC, 2009). In effect, the disease appears to be nested in segments of the population already overburdened by social inequities. One might posit further that such social inequities are responsible for the heightened presence of HIV among those segments of the population (Doherty, Leone, & Aral, 2007).
Implications for Practice
Adimora and Auerbach (2010) suggest specific structural approaches that aim to shift harmful social norms, empower communities, and effect policy, social, and political change. These specific structural interventions aim to address the important environmental factors that influence the physical, mental, and behavioral health of those living with HIV. To improve the lives of those aging with HIV, it is not enough to simply treat the psychiatric symptoms of those presenting for treatment. Health care providers must consistently address and seek to change the overarching social, environmental, and contextual factors that place individuals at risk for HIV-related stigma and compromise their overall well-being. While the clinical needs of individuals must continue to be assessed and treated, health care providers also must seek to understand and address the specific environmental and contextual factors that contribute to overall mental health burden in the aging HIV-positive population.
Once the additional factors that contribute to the stigmatization of our aging HIV-positive clients have been delineated, clinicians may begin to address the psychological and social implications of living within a social structure that exacerbates overall mental health burden via additional discrimination and marginalization. By addressing the individual factors that contribute to the stigmatization of aging HIV-positive individuals, health care providers not only provide education and validation but also can empower their clients to take action and speak out against these additional sources of mental health burden. Amelioration of our HIV-positive clients’ well-being can be achieved through the empowerment of our clients, the social support they derive from one another, and our commitment to acting as agents of social change within the larger contexts in which we work and live.
Limitations
It is important to note that the current study was a secondary analysis of data collected in 2005–2006 and may not be inclusive of the most current experiences of HIV-related stigma among the HIV-aging population. The smaller sample size among women likely contributed to the nonsignificant mediation model among this subsample. Further, due to the small number of individuals who identified as transgender (n = 10), data from this understudied subsample were removed from the current analysis. A convenience sampling frame was used, recruiting many lower-income participants from the existing ACRIA database of individuals seeking services from New York City–based ASOs. That is, while highly diverse, the sample remains inherently limited in its generalizability to the greater population of the New York Metropolitan area. Finally, all HIV-positive people aged 50 and older are not the same; some are long-term survivors who seroconverted before the implementation of highly active antiretroviral therapy in 1996; and others who seroconverted in later adulthood (Emlet, Tozay, & Raveis, 2011). The experience of stigma and mental health burdens may also vary in this regard (CDC, 1998; Kirk & Goetz, 2009; Halkitis et al., in press). This provides a future avenue for exploration.
Conclusions
The findings of the current study suggest that aside from the standard discrimination that multiple-minority, HIV-positive individuals experience on the basis of their minority statuses, these individuals appear to be experiencing significantly more HIV-related stigma as well. The increase in HIV-related stigma has deleterious effects on overall mental health and ability to access care (Brems, Johnson, Warner, & Roberts, 2010). Consistent with Syndemic Theory (Singer, 1994, 1996), these findings suggest that there is a synergistic relationship between minority statuses where multiple points of discrimination feed one another, allowing for multiple access points from which an individual can experience HIV-related stigma. The current study underscores the need for structural interventions that address discrimination, marginalization, and oppression as well as HIV-related stigma for people living with HIV into late adulthood and aligns with an understanding of health and well-being informed by a biopsychosocial perspective.
Contributor Information
ERIK DAVID STORHOLM, Center for Health, Identity, Behavior & Prevention Studies, Steinhardt School of Culture, Education, and Human Development, New York University, New York, New York, USA.
PERRY N. HALKITIS, Center for Health, Identity, Behavior & Prevention Studies, Steinhardt School of Culture, Education, and Human Development, New York University, New York, New York, USA.
SANDRA A. KUPPRAT, Center for Health, Identity, Behavior & Prevention Studies, Steinhardt School of Culture, Education, and Human Development, New York University, New York, New York, USA.
MELVIN C. HAMPTON, Center for Health, Identity, Behavior & Prevention Studies, Steinhardt School of Culture, Education, and Human Development, New York University, New York, New York, USA.
JOSEPH J. PALAMAR, Center for Health, Identity, Behavior & Prevention Studies, Steinhardt School of Culture, Education, and Human Development, New York University, New York, New York, USA.
MARK BRENNAN-ING, AIDS Community Research Initiative of America, New York, New York, USA, and New York University College of Nursing, New York, New York, USA.
STEPHEN KARPIAK, AIDS Community Research Initiative of America, New York, New York, USA, and New York University College of Nursing, New York, New York, USA.
REFERENCES
- Adimora AA, & Auerbach JD (2010). Structural interventions for HIV prevention in the United States. Journal of Acquired Immune Deficiency Syndromes, 55(2), 132–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adimora AA, & Schoenbach VJ (2005). Social context, sexual networks, and racial disparities in rates of sexually transmitted infections, Journal of Infectious Diseases, 191(1), 115–122. [DOI] [PubMed] [Google Scholar]
- Baron RM, & Kenny DA (1986). Moderator-mediator variables distinction is social psychological research: Conceptual, strategic, and statistical considerations, Journal of Personality and Social Psychology, 51(6), 1173–1182. [DOI] [PubMed] [Google Scholar]
- Berger BE, Ferrans CE, & Lashley FR (2001). Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Research in Nursing & Health, 24, 518–529. [DOI] [PubMed] [Google Scholar]
- Bhavan KP, Kampalath VN, & Overton ET (2008). The aging of the HIV epidemic. Current HIV/AIDS Reports, 5(3), 150–158. [DOI] [PubMed] [Google Scholar]
- Brems C, Johnson ME, Warner TD, & Roberts LW (2010). Health care providers’ reports of perceived stigma associated with HIV and AIDS in rural and urban communities. Journal of HIV/AIDS & Social Services, 9, 356–370. [Google Scholar]
- Brennan M, Karpiak SE, Shippy RA, & Cantor MH (2009). Older adults with HIV: An in-depth examination of an emerging population. New York, NY: Nova Science Publishers. [Google Scholar]
- Centers for Disease Control and Prevention. (2009). HIV Surveillance Report, 2009; vol. 21. Retrieved from http://www.cdc.gov/hiv/topics/surveillance/resources/reports/
- Centers for Disease Control and Prevention. (2008). HIV/AIDS among persons aged 50 and older. Retrieved from http://www.cdc.gov/hiv/topics/over50/resources/factsheets/pdf/over50.pdf
- Centers for Disease Control and Prevention. (1998). AIDS among persons aged greater or equal to 50 years—United States, 1991–1996. Morbidity and Mortality Weekly Report, 47, 21–27. [PubMed] [Google Scholar]
- David S, & Knight BG (2008). Stress and coping among gay men: age and ethnic differences. Psychology and Aging, 23(1), 62–69. [DOI] [PubMed] [Google Scholar]
- Doherty IA, Leone PA, & Aral SO (2007). Social determinants of HIV infection in the deep south. American Journal of Public Health, 97(3), 391–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emlet C (2006). You’re awfully old to have this disease: Experiences of stigma and ageism in adults 50 years and older living with HIV/AIDS. The Gerontologist, 46(6), 781–790. [DOI] [PubMed] [Google Scholar]
- Emlet C (2007). Experiences of stigma in older adults living with HIV/AIDS: A mixed-methods analysis. AIDS Patient Care and STDs, 21(10), 740–752. [DOI] [PubMed] [Google Scholar]
- Emlet CA, Toxay S, & Raveis VH (2011). “I’m not going to die from the AIDS”: Resilience in aging with HIV disease. The Gerontologist, 51(1), 101–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Kupprat SA, Kingdon M, Perez-Figueroa R, Hampton ME, Eddy J, & Ompad DC (In press). Exploring a syndemic in HIV-positive gay, bisexual, and other MSM ages 50 and over. Annals of Applied Anthropology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN (2010). Reframing HIV prevention for gay men in the United States. American Psychologist, 65(8), 752–763. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, O’Cleirigh C, Mayer KH, Mimiaga MJ, & Safren SA (2011). Prospective associations between HIV-related stigma, transmission risk behaviors, and adverse mental health outcomes in men who have sex with men. Annals of Behavioral Medicine, 42(2), 227–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Heckman T, Kochman A, Sikkema K, & Bergholte J (2000). Depression and thoughts of suicide among middle-aged and older persons living with HIV-AIDS. Psychiatric Services, 51(7), 903–907. [DOI] [PubMed] [Google Scholar]
- Kang E, Rapkin BD, & DeAlmeida C (2006). Are psychological consequences of stigma enduring or transitory? A longitudinal study of HIV stigma and distress among Asians and Pacific Islanders living with HIV illness. AIDS Patient Care and STDs, 20(10), 712–723. [DOI] [PubMed] [Google Scholar]
- Kang E, Rapkin BD, Remien RH, Mellins CD, & Oh A (2005). Multiple dimensions of HIV stigma and psychological distress among Asians and Pacific Islanders living with HIV illness. AIDS and Behavior, 9(2), 145–154. [DOI] [PubMed] [Google Scholar]
- Kirk JB, & Goetz MB (2009). Human immunodeficiency virus in an aging population, a complication of success. Journal of the American Geriatrics Society, 57, 2129–2138. [DOI] [PubMed] [Google Scholar]
- Lee RS, Kochman A, & Sikkema K (2002). Internalized stigma among people living with HIV-AIDS. AIDS and Behavior, 6(4), 309–319. [Google Scholar]
- Logie C, & Gadalla TM (2009). Meta-analysis of health and demographic correlates of stigma towards people living with HIV. AIDS Care, 21(6), 742–753. [DOI] [PubMed] [Google Scholar]
- Meyer IH (1995). Minority stress and mental health in gay men, Journal of Health and Social Behavior, 36, 38–56. [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence, Psychological Bulletin, 129(5), 674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New York City Department of Health and Human Hygiene. (2010). New York City HIV/AIDS Annual Surveillance Statistics 2009. Retrieved from http://www.nyc.gov/html/doh/downloads/pdf/ah/surveillance2009_tables_all.pdf
- Pak AW, Dion KL, & Dion KK (1991). Social psychological correlates of experienced discrimination: Test of the double jeopardy hypothesis. International Journal of Intercultural Relations, 15, 243–254. [Google Scholar]
- Pandya R, Metz L, & Patten SB (2005). Predictive value of the CES-D in detecting depression among candidates for disease-modifying multiple sclerosis treatment. Psychosomatics, 46(2), 131–134. [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. [Google Scholar]
- Rao D, Pryor JB, Gaddist BW, & Mayer R (2008). Stigma, secrecy, and discrimination: Ethnic/racial differences in the concerns of people living with HIV/AIDS. AIDS and Behavior, 12, 265–271. [DOI] [PubMed] [Google Scholar]
- Russell DW (1996). UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of Personality Assessment, 66, 20–40. [DOI] [PubMed] [Google Scholar]
- Ryff C, & Keyes C (1995). The structure of psychological well-being revisited. Journal of Personality and Social Psychology, 69, 719–727. [DOI] [PubMed] [Google Scholar]
- Sandelowski M, Barroso J, & Voils C (2009). Gender, race/ethnicity, and social class in research reports on stigma in HIV-positive women. Health Care for Women.International, 30(4), 273–288. [DOI] [PubMed] [Google Scholar]
- September AN, McCarrey M, Baranowsky A, Parent C, & Schindler D (2001). The relation between well-being, impostor feelings, and gender role orientation among Canadian University students. Journal of Social Psychology, 141(2), 218–232. [DOI] [PubMed] [Google Scholar]
- Shippy RA, & Karpiak SE (2005). Perceptions of support among older adults with HIV. Research on Aging, 27(3), 290. [Google Scholar]
- Singer M (1994). AIDS and the health crisis of the U.S. urban poor: The perspective of critical medical anthropology. Social Science and Medicine, 39(7), 931–948. [DOI] [PubMed] [Google Scholar]
- Singer M (1996). A dose of drugs, a touch of violence, a case of AIDS: Conceptualizing the SAVA syndemic. Free Inquiry in Creative Sociology, 24, 99–110. [Google Scholar]
- Stall R, Friedman MS, & Catania J (2008). Interacting epidemics and gay men’s health: A theory of syndemic production among urban gay men. In Wolitski RJ, Stall R, & Valdiserri RO (Eds.), Unequal opportunities: Health disparities among gay and bisexual men in the United States (pp. 251–274). New York, NY: Oxford University Press. [Google Scholar]
- Stuber J, Meyer I, & Link B (2008). Stigma, prejudice, discrimination, & health. Social Science & Medicine, 67(3), 351–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theuninck AC, Lake N, & Gibson S (2010). HIV-related posttraumatic stress disorder: Investigating the traumatic events. AIDS Patient Care and STDs, 24(8), 499–524. [DOI] [PubMed] [Google Scholar]
- Turkinaz A, Magfiret K, Gulay I, & Behice E (2006). The experiences of loneliness, depression, and social support of Turkish patients with continuous ambulatory peritoneal dialysis and their caregivers. Journal of Clinical Nursing, 15(4), 490–497. [DOI] [PubMed] [Google Scholar]
- Vanable PA, Carey MC, Blair DC, & Littlewood RA (2006). Impact of HIV-related stigma on health behaviors and psychological adjustment among HIV-positive men and women. AIDS and Behavior, 10(5), 473–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wight RG (2000). Precursive depression among HIV infected AIDS caregivers over time. Social Science & Medicine, 51(5), 759–770. [DOI] [PubMed] [Google Scholar]


