Objective
The aim of the study is to quantify the effects of virtual reality–based exercise on balance after stroke.
Design
The PubMed, Embase, Cochrane Library, Cumulative Index of Nursing and Allied Health Literature, and Web of Science databases were searched until December 31, 2021. Independent investigators abstracted data, assessed the quality of the evidence, and rated the certainty of the evidence. The intergroup differences were determined by calculating mean difference and 95% confidence interval by RevMan 5.3 software.
Results
Fourteen randomized controlled trials involving 423 stroke patients were included. Patients who received virtual reality–based exercise illustrated marked improvements in the Berg Balance Scale (mean difference, 1.35; 95% confidence interval, 0.58 to 1.86; P < 0.00001; I2 = 44%), Timed Up and Go test (mean difference, −0.81; 95% confidence interval, −1.18 to −0.44; P < 0.0001; I2 = 0%), Functional Reach Test (mean difference, 3.06; 95% confidence interval, 1.31–4.80; P = 0.0006; I2 = 0%), 10-Meters Walking Test (mean difference, −1.53; 95% confidence interval, −2.92 to −0.13; P = 0.03; I2 = 33%), and Modified Barthel Index (mean difference, 5.26; 95% confidence interval, 1.70 to 8.82; P = 0.004; I2 = 0%) compared with the control group.
Conclusions
Existing low-evidence analyses showed that virtual reality–based exercise could effectively and safely improve balance in chronic stroke. Longer-term virtual reality–based exercise was more effective on functional ability of stroke.
Key Words: Virtual Reality, Balance, Stroke, Systematic Review, Meta-analysis
What Is Known
Virtual reality–based exercise has significant effects on balance in patients with chronic stroke.
What Is New
Significant effects of virtual reality–based exercise on balance and functional ability, gait, and activities of daily living ability for chronic stroke and statistically more effective functional ability for acute/subacute stroke were detected in this study. Longer-term virtual reality–based interventions are more effective than shorter-term interventions, especially regarding the functional ability of stroke. The current evidence is insufficient to draw conclusions on the effects of virtual reality–based exercise combined with other physiotherapy for stroke. Virtual reality–based exercise can be a part of the treatment programs for stroke.
Stroke is the most common neurological disease caused by cerebral ischemia or hemorrhage, resulting in physical impairments, such as decreased muscle strength, abnormal muscle tone, impaired proprioception, and cognitive dysfunction.1 Balance and postural control, essential for keeping the body upright and maintaining stability, are further adversely affected by sensorimotor impairment in stroke.2 It has been reported that insufficient balance and poor postural control are the cardinal abnormal motor features of 80% of chronic stroke patients who exhibit weight-bearing asymmetry, postural swing, and gait disturbance.3,4
Several different classification systems have been used to describe the stage of stroke. One of the most strongly recommended frameworks to stage stroke is based on the time from stroke onset. Thus, 6 mos after stroke is the cutoff between acute and chronic stroke.5 Among survivors, dependence in activities of daily living 3 mos after the event varies from 16.2%6 to 19.2%.7 Previous studies have found that 38% of chronic stroke victims cannot ambulate after stroke onset, and their risk of falling increases.8,9 Therefore, the maintenance of balance is the most essential step to improving functional status and quality of life after stroke.
Over the last couple of decades, some promising approaches have emerged to improve balance and to promote active exercise in patients after stroke. To treat stroke, conventional rehabilitation comprehends the physical therapy and occupational therapy, which focus on repetitive and task-specific practice.10 The issues of cost-effectiveness, compliance, and generalizability remain controversial in conventional stroke rehabilitation. In recent years, previous reviews have indicated the potential of virtual reality (VR) to solve some of the challenges due to low motivation and adherence to therapy after stroke. Its immersive interactivity is believed to provide a particularly engaging approach, as well as a cost-effective and engaging procedural preparation medium. Virtual reality–based training through its computer-generated and interactive environment and experiences has begun to gain widespread application as an augmented exercise for stroke rehabilitation.11 Virtual reality balance training, simulating a virtual rehabilitation scene, can be systematically manipulated to improve neural connectivity and enjoyable patient-specific motor retraining by repetition of practice and sensory and visual feedback input.12–14
A previous review of the literature reported significant methodological issues and the need for further research but found that the evidence still shows that VR has considerable potential in a variety of clinical settings.15 Another challenge in this field of VR rehabilitation is identifying the best time to implement recovery and repair-focused interventions. The first week to first month after stroke is a critical period for neuroplasticity, but there is some uncertainty about how early and intensively to start training.16 However, only a few studies have compared the effects of VR-based exercise with conventional balance therapy among adults with acute, subacute, and chronic stroke.
Although there is increasing evidence that VR can be effective for people with stroke, quantitative meta-analysis has not been performed to investigate the effects of different duration time of VR-based exercise on stroke patients taking into account the wide variation in the time since stroke and whether it has significant differences in outcomes compared with general balance training and conventional physiotherapy. The present systematic review with meta-analysis, therefore, aimed to examine the evidence for the effects of duration time of VR-based programs on improving balance in patients with acute/subacute and chronic stroke.
METHODS
Data Sources and Search Strategy
Following the Preferred Reporting Items for Systematic Reviews and Meta-analysis guidelines and PICOs principle (population, intervention/exposure, comparison, outcomes and study designs). For a completed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist, see Supplementary Checklist (Appendix S1, Supplemental Digital Content 1, http://links.lww.com/PHM/B830). This review was registered with the number CRD42021266012 on the PROSPERO Website. A comprehensive search was conducted in the PubMed, Embase, Cochrane Library, Cumulative Index of Nursing and Allied Health Literature, and Web of Science databases until December 31, 2021. Key terms were used including “stroke” and “virtual reality,” to identify articles on the effects of VR for balance training on stroke (Appendix S2, Supplemental Digital Content 2, http://links.lww.com/PHM/B831).
Literature Selection
Studies were considered to be eligible if they met the following criteria: (1) randomized controlled trial; (2) patients who were diagnosed with stroke; (3) intervention: VR-based exercise by using some devices to generate realistic images, sounds, and other sensations that simulate a patient’s physical presence in a virtual environment and interact with virtual features or items; (4) comparisons: conventional therapies; (5) outcomes concentrating on the effects for balance, functional performance, and activities of daily living; and (6) peer-reviewed English journals. Two reviewers (JS and XG) independently assessed the eligibility of the articles. The preliminary screening was based on the title and abstract. The selected articles were then evaluated in their entirety. If there was a disagreement, the full text of the article was checked and discussed, if necessary, with third-party adjudication (MS).
Data Extraction
Reviewers independently extracted data from the included studies (HL and YS). If their results were inconsistent, a third reviewer re-evaluated the articles and discussed them with the two reviewers to reach an agreement (HB). They abstracted the following data using a data extraction form: number of men and women, age, mean weight/height/body mass index, number of etiologies, lesion side, onset period of stroke, outcome assessed, interventions, relevant statistical data, and adverse events. Virtual reality–based exercise and control group interventions in parallel group trials were extracted. The schedule of the VR-based training was defined by its intensity (number of sets and repetitions), frequency (number of training sessions per week), and duration (in weeks).
The Risk of Bias
Reviewers independently assessed the risk of bias using the revised Cochrane risk of bias assessment tool for randomized controlled trial studies (YY and LL).17 There are five domains in the revised Cochrane risk of bias assessment tool: randomization process, deviations from the intended intervention, missing outcome data, measurement of the outcome, and selection of the reported data. For missing outcome data in individual studies, we stipulated a low risk of bias for loss to follow-up of less than 10% and a difference of less than 5% in missing data between intervention/exposure and control groups. Publication bias was assessed through visual inspection of funnel plots for each outcome in which 10 or more eligible studies were identified.
Statistical Analysis
RevMan 5.3 software (Cochrane Collaboration, Oxford, United Kingdom) was used to analyze the data in this meta-analysis (YL). The effects of VR-based exercise were expressed as the mean difference (MD) with 95% confidence interval (CI). The heterogeneity was estimated by using the I2 test. If the I2 value was smaller than 50%, a fixed-effects model was used; otherwise, a random-effects model was used. Publication bias was assessed with a funnel plot. A statistically significant P value was set to 0.05.
The evidence and its certainty separately for bodies of evidence from randomized controlled trials were summarized (JF). The evidence for each outcome was divided into four levels (high, moderate, low, or very low) by the Grading of Recommendations Assessment, Development and Evaluation system. The overall risk of bias, imprecision, inconsistency, indirectness, and publication bias five parts were used to summarize the quality of the results.18
RESULTS
Fourteen randomized control trials were finally selected with a total of 423 stroke patients, as shown in Figure 1. The baseline demographic and clinical characteristics of the included studies are shown in Appendix S3 (Supplemental Digital Content 3, http://links.lww.com/PHM/B832). The mean age of the participants ranged from 45.91 to 65.26 yrs in the VR-based exercise group19,20 and 49.16 to 63.50 yrs in the control group.19,21 Three studies included patients with acute/subacute stroke (<3 mos)22–24 and 11 targeted patients with chronic stroke (≥6 mos).19–21,25–32 Comparison were made before and after interventions in 11 studies, and comparisons were conducted before, after interventions, and at follow-up of patients by Morone et al.,23 de Rooij et al.,24 and Yatar and Yildirim.29 Patients had the ability to walk 10 meters independently with or without assistive devices in two studies19,20 and the ability to stand for 30 mins in another two studies.31,32 The level of patients was more than two grades of FAC (Functional Ambulation Category) in two studies, and Brunnstrom reported that patients were grade 3 or higher.21,26 Only the state of consciousness, which was K-MMSE (Korean Mini-Mental Status Examination) scores greater than 24, was mentioned in three studies.19,25,30
FIGURE 1.
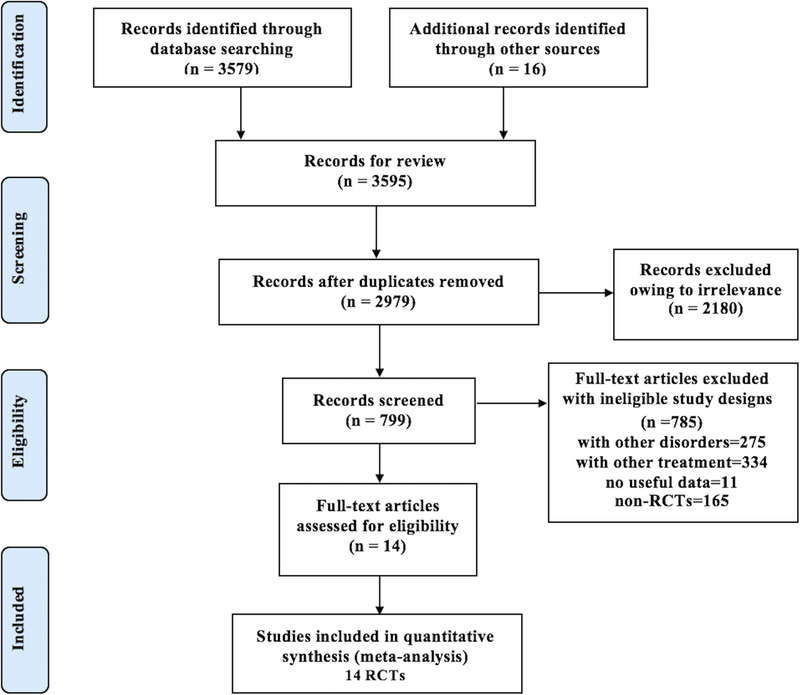
The flowchart of selection process.
According to the inclusion criteria, all studies were balance-interventions oriented. The intervention was only VR balance training in two studies and combined VR exercise with conventional therapy in 12 studies. There was a wide variety in the frequency, intervention time, type, and duration of the VR intervention. The frequency of VR training varied between 2 and 5 times a week. The VR took 30 mins per session in most studies and was 20 mins in only one study.23 The duration of intervention was ranged from 4 to 8 wks in hospitals. To project the virtual environment, a Wii balance board system was used in five studies, and the game setting of lower extremity balance was suitable for seniors. All subjects in this study were older stroke patients, and most games consisted of performing activities of daily living, such as washing, cooking, and bathing. The difficulty degree of training in all courses was divided into different levels based on the previous level. The therapist explained the VR training method to the subjects and provided adequate rest to avoid fatigue during the training. Participants selected specific VR activities (Appendix S4, Supplemental Digital Content 4, http://links.lww.com/PHM/B833).
The risk of bias measured by the revised Cochrane risk of bias assessment tool in the included studies is presented in Table 1. Seven studies generated an adequately randomized sequence, and the overall methodological assessment of the studies was high for two studies, low for six studies, and unclear for five studies. The Grading of Recommendations Assessment, Development and Evaluation for all outcome measurements was inconsistent and ranged from moderate to very low quality; thus, most studies were classified as fair thereby (Appendix S5, Supplemental Digital Content 5, http://links.lww.com/PHM/B834).
TABLE 1.
The Cochrane tool of assessing risk of bias for methodological assessment (RoB 2.0 tool)
| Article, Year | Randomization Process | Deviations From Intended Interventions | Missing Outcome Data | Measurement of the Outcome | Selection of the Reported | Overall |
|---|---|---|---|---|---|---|
| Jeon et al.,22 2019 | High | Low | Low | Low | Low | High |
| Barcala et al.,21 2013 | Low | Low | Low | Low | Low | Low |
| Cho et al.,20 2012 | Low | Low | Low | Unclear | Low | Unclear |
| Yu and Cho,25 2016 | Unclear | Low | Low | Unclear | Low | Unclear |
| Lee et al.,19 2015 | Unclear | Low | Low | Unclear | Low | Unclear |
| Lee et al.,26 2017 | Low | Low | Low | Low | Low | Low |
| Lloréns et al.,27 2015 | Low | Low | Low | Low | Low | Low |
| Marques-Sule et al.,28 2021 | Low | Low | Low | Low | Low | Low |
| Yatar and Yildirim,29 2015 | High | Low | Low | Unclear | Low | High |
| Song and Park,30 2015 | Unclear | Low | Low | Unclear | Low | Unclear |
| Choi et al.,31 2018 | Low | Low | Low | Low | Low | Low |
| Morone et al.,23 2014 | Low | Low | Low | Low | Low | Low |
| Kim et al.,32 2009 | Unclear | Low | Low | Low | Low | Unclear |
| de Rooij et al.,24 2021 | Low | Low | Low | Low | Low | Low |
The Berg Balance Scale (BBS) was designed to rate the ability of balance. The BBS consists of 14 items, each scored on a scale of 0–4 and a total of 56 points, with higher scores indicating better balance. When data from 11 randomized controlled studies were pooled (Fig. 2), a significant improvement in balance was found after VR-based balance intervention (MD, 1.35; 95% CI, 0.85 to 1.86; P < 0.00001; I2 = 44%). Nine studies reported a significant improvement in chronic stroke patients in the VR-based balance group (MD, 1.35; 95% CI, 0.84 to 1.86; P < 0.0001, I2 = 55%). However, we failed to find any differences between the two groups for acute/subacute stroke patients (MD, 1.43; 95% CI, −1.70 to 4.55; P = 0.61; I2 = 0%; Fig. 2). In addition, the funnel plot showed an asymmetrical distribution regarding balance, which suggested that there would be a high risk of publication bias (Fig. S1, Supplemental Digital Content 6, http://links.lww.com/PHM/B835). According to the different intervention durations, significantly better improvement on the BBS was observed in the VR-based balance group than in the control group (MD, 2.70; 95% CI, 0.69 to 4.71; P = 0.008), and heterogeneity was low (P = 0.35, I2 = 11%) at 4 wks. The meta-analysis showed that the VR-based balance group exhibited significant improvement compared with the control group after 5–8 wks of treatment (MD, 1.26; 95% CI, 0.74 to 1.78, P < 0.00001), and heterogeneity was high (P = 0.03, I2 = 62%; Fig. S2, Supplemental Digital Content 7, http://links.lww.com/PHM/B836).
FIGURE 2.
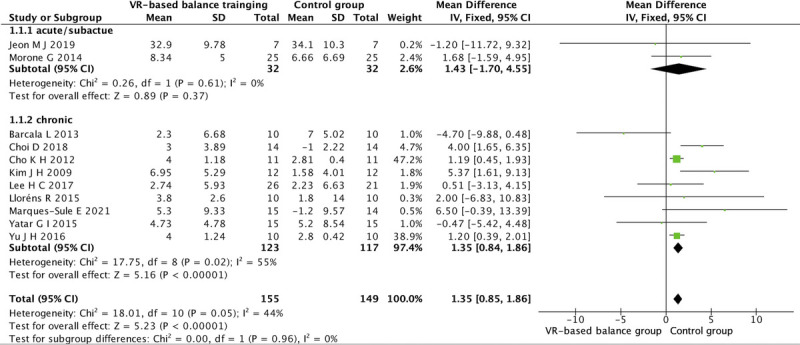
Forest plots of VR-based exercise on the BBS.
The Timed Up and Go (TUG) test was used to evaluate functional performance. The patient was asked to sit on a height-adjusted chair with an armrest and was instructed to get up at the cue of “start,” walk forward to a 3-meter point, and then return to the chair. The height of the chair seat was adjusted so that the knee joint of the patient was at 90 degrees. The average time for three trials recorded using a stopwatch was the TUG. The pooled results for the TUG showed a significant MD of −0.81 (95% CI, −1.18 to −0.44; P < 0.0001; I2 = 0%) in favor of the VR-based balance group (Fig. 3). Seven studies reported a significant improvement in chronic stroke in the VR-based balance group (MD, −0.85; 95% CI, −1.38 to −0.32; P = 0.002; I2 = 0%). The pooled MD for VR-based balance in addition to conventional therapy was also significantly different between the two groups for acute/subacute stroke patients (MD, −0.78; 95% CI, −1.29 to −0.26, P = 0.003, I2 = 0%). Improvements were observed in patients (MD, −0.81; 95% CI, −1.18 to −0.44, P < 0.0001, I2 = 0%) after 5–8 wks of intervention. However, no significant difference was observed in the subgroup analysis of 4 wks of intervention, along with high heterogeneity (MD, −1.69; 95% CI, −6.59 to 3.20; P = 0.5; I2 = 58%; Fig. S3, Supplemental Digital Content 8, http://links.lww.com/PHM/B837).
FIGURE 3.
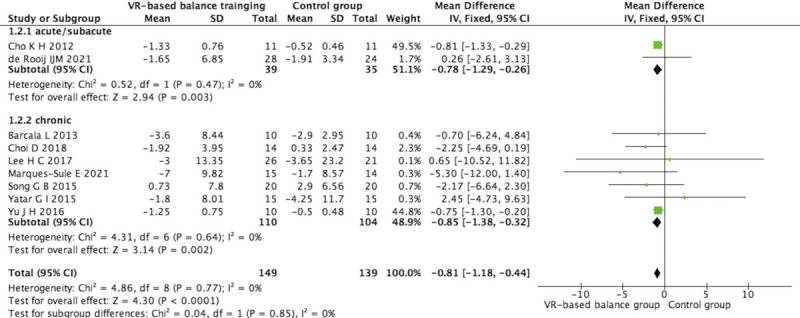
Forest plots of VR-based exercise on the TUG.
Functional performance was also evaluated using the Functional Reach Test (FRT) and the 10-Meter Walking Test.3 The patients moved their upper limbs and trunk to the front, if possible, and the distances were measured to the end of the middle finger by a standard ruler. The tests were repeated 3 times, and the average value was recorded for the FRT. Overall, the VR-based balance group had a higher score than the control group (MD, 3.06; 95% CI, 1.31 to 4.80; P = 0.0006; I2 = 0%; Fig. 4). The 10-Meters Walking Test is a performance measure used to assess walking speed in meters per second over a short distance. The subject was instructed to walk for 14 meters, and the average walking speed for 10 meters was measured by excluding 4 meters corresponding to the acceleration and deceleration distances. When data from four randomized controlled studies were pooled (Fig. S4, Supplemental Digital Content 9, http://links.lww.com/PHM/B838), statistically significantly difference was found associated with VR-based exercise in stroke (MD, −1.53; 95% CI, −2.92 to −0.13; P = 0.03). There was moderate evidence of heterogeneity (I2 = 33%).
FIGURE 4.
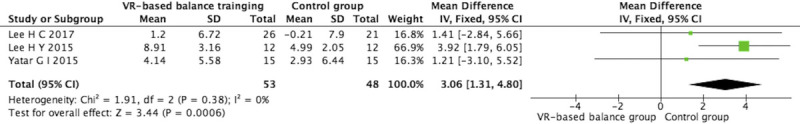
Forest plots of VR-based exercise on the FRT.
The Modified Barthel Index was used to assess the activities of daily living. The Modified Barthel Index contains 10 parts, and the total score is summed as a minimum of 0 and a maximum of 100 points. A score of 60 on the Modified Barthel Index means that daily activities are self-supporting by the patient. The higher the score, the more independent the patient is in completing activities of daily livings. The meta-analysis showed that VR-based exercise produced a significant and sustained improvement (MD, 5.26; 95% CI, 1.70 to 8.82; P = 0.004; I2 = 0%; Fig. S5, Supplemental Digital Content 10, http://links.lww.com/PHM/B839). Adverse events reported in only one study were soreness (6), hypertonicity (5), dizziness (6), and leg pain (2) in the intervention group and soreness (15), hypertonicity (7), dizziness (2), and shoulder pain (4), and low back pain (2) in the control group (Appendix S3, Supplemental Digital Content 3, http://links.lww.com/PHM/B832).26
DISCUSSION
This systematic review was conducted to identify the effects of VR-based exercise on stroke survivors. The results of this study indicated that VR-based exercise was valuable in producing significantly greater improvements in balance, functional ability, gait, and activities of daily living ability than physical therapy, including conventional balance training, although the changes in VR-based exercise did not indicate an active trend in balance with a mean time since stroke of less than 6 mos. The positive motor function improvement of VR-based exercise was in line with previous reviews on the effects of VR on the lower limbs in patients with stroke.33 Some studies focused on upper extremity function with no balance measures.34,35 Taking sports rehabilitation as an example, the advantages of immersive properties of VR include how it induces the illusion of virtual body ownership and agency through multisensory feedback. To characterize and ultimately predict those most likely to respond to a given intervention, efforts to understand the recovery of different types of stroke will help target efficacious treatments toward responders and focus on developing better treatments for nonresponders. This review is the first to analyze the changes in balance function of acute/subacute and chronic stroke, and different duration intervention time after VR training. Virtual reality training has a better balance improving effect on stroke in the chronic stage than in the acute/subacute stage. As its most distinguishing mechanism, a VR-based balance program inducing cortical reorganization from aberrant ipsilateral to contralateral sensory-motor cortex activation has been explored.36 Based on the enhanced cortical reorganization, the restoration of motor function could be facilitated in patients with chronic stroke by VR training.
Concerning the primary outcomes, a statistically significance change of 1.62 points on the BBS in favor of VR-based exercise was observed in this review (P = 0.002). It was revealed that the effects of VR-based exercise were higher in chronic patients. During upright standing posture, the individual integrates sensory inputs to execute of the movement to get equilibrium body.37 Because of an alteration in somatosensory and vestibular systems, patients with stroke frequently present a high reliance upon environmental visual information to control body posture.38 Virtual reality not only senses the weight distribution but also reflects it onto a television screen using an avatar, thus allowing patients to observe movements and providing positive feedback, and fun resources may produce greater motivation during physical therapy sessions. When patients perform immersion motion and visualization, the use-dependent plasticity changes in the higher sensor motor areas belonging to the mirror neuron system are stimulated and improved.39
We found that the time of TUG was decreased by VR-based exercise. Most VR programs are based on game-based tasks, using the Nintendo Wii, meaning that patients show more interest in training.40 In addition, task-oriented training in the included VR studies is considered to facilitate the reorganization of the brain to allow functional improvement. We observed significant results in the functional reach test. However, Lee et al.26 have reported negative effects of VR in the FRT. The execution of the FRT requires shifting the center of gravity forward, but the lower limbs cannot be moved, which is similar to the requirement of the Wii balance board training. The VR game–based tasks encourage the load-unloading sway strategy at the hip by increasing speed and precision to carry out different actions. Balance function is closely related to activities of daily living performance. Virtual reality is thought to be an evidence-based intervention for chronic stroke that can enhance high intensity, repetition, and task-oriented training.
The equipment required for such rehabilitation is often complex and expensive and can only be used in specialized centers. Not only does the Nintendo Wii offer relatively simple and inexpensive opportunities for VR treatments, but it also shows good results in the progression of chronic stroke survivors. Most treatments, including those in studies, are short-lived, and many studies have increased the frequency of treatments per week. This suggests that patients with chronic stroke need rest to learn the exercises. However, the number of studies included in this study was limited, and the quality of the results was not statistically high. Therefore, it was felt that there was a limit to the interpretation and that more research needs to be conducted and reanalyzed in the future.
This review acknowledges several limitations that should be taken into account in explaining the impact of VR-based exercise on stroke rehabilitation patients. As shown in the funnel plot, there was some chance of publication bias. Furthermore, we cannot exclude the possibility of bias in our meta-analysis because of the small sample size and short intervention period of the included studies. Follow-up was conducted in only three randomized controlled trial studies, and it is unknown whether the changes would persist beyond this time point. Given the outcome metrics of this study, participants need to achieve the ability to maintain a stride-standing position for some seconds or to walk a distance of 10 meters before participating in VR. Further exploration requires stricter evaluation standards and a high-quality randomized controlled trial design to determine the effects of VR-based exercise on patients with wide variations in the time since stroke.
CONCLUSIONS
This meta-analysis suggests that VR-based exercise can improve the balance, functional ability, gait, and activities of daily living compared with the conventional therapy, including balance training, although the changes in VR-based exercise did not indicate an active trend in balance with a mean time since stroke of less than 6 mos. In particular, VR-based therapy for patients with acute or subacute stroke was statistically more effective as reflected in the TUG test than conventional therapy. However, the effectiveness of VR-based exercise on balance remains unclear in acute or subacute stroke patients. Longer-term (5–8 wks) VR-based interventions are more effective than shorter-term interventions (4 wks), especially regarding functional ability after stroke. Therefore, additional high-quality large randomized controlled trials and/or patients in the acute or subacute stroke phase will be needed to provide better evidence supporting its use.
Supplementary Material
Footnotes
JS and XG contributed equally to this work.
This work was supported by the Science and Technology Plan Project of Jiaxing (2022AD30004), the Key Research and Development Project of Science and Technology Commission of Zhejiang Province, China (2022C03177), the Science and Technology Common Wealth Foundation of Zhejiang Province, China (LGF21H170004), and the Medical and Health Science and Technology Plan of Zhejiang Province, China (2020KY956).
Financial disclosure statements have been obtained, and no conflicts of interest have been reported by the authors or by any individuals in control of the content of this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.ajpmr.com).
Contributor Information
Jie Shen, Email: shenjie066@gmail.com.
Xudong Gu, Email: jxgxd@hotmail.com.
Yunhai Yao, Email: yzy168110@163.com.
Liang Li, Email: liliang0573@163.com.
Meifang Shi, Email: jxmeifang402@163.com.
Hui Li, Email: kfyx12jx@163.com.
Ya Sun, Email: sysr0427@163.com.
Hefeng Bai, Email: 1049385390@qq.com.
Yan Li, Email: liyan6101@126.com.
Jianming Fu, Email: fjm_7758@163.com.
REFERENCES
- 1.Benjamin EJ Blaha MJ Chiuve SE, et al.: Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation 2017;135:e146–603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guzik A Drużbicki M Maistrello L, et al.: Relationship between observational Wisconsin gait scale, gait deviation index, and gait variability index in individuals poststroke. Arch Phys Med Rehabil 2019;100:1680–7 [DOI] [PubMed] [Google Scholar]
- 3.Tyson SF Hanley M Chillala J, et al.: Balance disability after stroke. Phys Ther 2006;86:30–8 [DOI] [PubMed] [Google Scholar]
- 4.Roelofs JMB van Heugten K de Kam D, et al.: Relationships between affected-leg motor impairment, postural asymmetry, and impaired body sway control after unilateral supratentorial stroke. Neurorehabil Neural Repair 2018;32:953–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bernhardt J Hayward KS Kwakkel G, et al.: Agreed definitions and a shared vision for new standards in stroke recovery research: the Stroke Recovery and Rehabilitation Roundtable Taskforce. Int J Stroke 2017;12:444–50 [DOI] [PubMed] [Google Scholar]
- 6.Ullberg T Zia E Petersson J, et al.: Changes in functional outcome over the first year after stroke: an observational study from the Swedish stroke register. Stroke 2015;46:389–94 [DOI] [PubMed] [Google Scholar]
- 7.Magalhães R Abreu P Correia M, et al.: Functional status three months after the first ischemic stroke is associated with long-term outcome: data from a community-based cohort. Cerebrovasc Dis 2014;38:46–54 [DOI] [PubMed] [Google Scholar]
- 8.Kollen B, Kwakkel G, Lindeman E: Longitudinal robustness of variables predicting independent gait following severe middle cerebral artery stroke: a prospective cohort study. Clin Rehabil 2006;20:262–8 [DOI] [PubMed] [Google Scholar]
- 9.Yang C Ghaedi B Campbell TM, et al.: Predicting falls using the stroke assessment of fall risk tool. PM R 2021;13:274–81 [DOI] [PubMed] [Google Scholar]
- 10.Stinear CM Lang CE Zeiler S, et al.: Advances and challenges in stroke rehabilitation. Lancet Neurol 2020;19:348–60 [DOI] [PubMed] [Google Scholar]
- 11.Laver KE Lange B George S, et al.: Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev 2017;11:Cd008349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Riva G Mancuso V Cavedoni S, et al.: Virtual reality in neurorehabilitation: a review of its effects on multiple cognitive domains. Expert Rev Med Devices 2020;17:1035–61 [DOI] [PubMed] [Google Scholar]
- 13.Sokolov AA, Collignon A, Bieler-Aeschlimann M: Serious video games and virtual reality for prevention and neurorehabilitation of cognitive decline because of aging and neurodegeneration. Curr Opin Neurol 2020;33:239–48 [DOI] [PubMed] [Google Scholar]
- 14.Kiper P Luque-Moreno C Pernice S, et al.: Functional changes in the lower extremity after non-immersive virtual reality and physiotherapy following stroke. J Rehabil Med 2020;52:jrm00122. [DOI] [PubMed] [Google Scholar]
- 15.Zhang B Li D Liu Y, et al.: Virtual reality for limb motor function, balance, gait, cognition and daily function of stroke patients: a systematic review and meta-analysis. J Adv Nurs 2021;77:3255–73 [DOI] [PubMed] [Google Scholar]
- 16.Biernaskie J, Chernenko G, Corbett D: Efficacy of rehabilitative experience declines with time after focal ischemic brain injury. J Neurosci 2004;24:1245–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sterne JAC Savović J Page MJ, et al.: RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- 18.Atkins D Best D Briss PA, et al.: Grading quality of evidence and strength of recommendations. BMJ 2004;328:1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee HY, Kim YL, Lee SM: Effects of virtual reality–based training and task-oriented training on balance performance in stroke patients. J Phys Ther Sci 2015;27:1883–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cho KH, Lee KJ, Song CH: Virtual-reality balance training with a video-game system improves dynamic balance in chronic stroke patients. Tohoku J Exp Med 2012;228:69–74 [DOI] [PubMed] [Google Scholar]
- 21.Barcala L Grecco LA Colella F, et al.: Visual biofeedback balance training using Wii fit after stroke: a randomized controlled trial. J Phys Ther Sci 2013;25:1027–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jeon MJ, Moon JH, Cho HY: Effects of virtual reality combined with balance training on upper limb function, balance, and activities of daily living in persons with acute stroke: a preliminary study. Phys Ther Rehabil Sci 2019;8:187–93 [Google Scholar]
- 23.Morone G Tramontano M Iosa M, et al.: The efficacy of balance training with video game–based therapy in subacute stroke patients: a randomized controlled trial. Biomed Res Int 2014;2014:580861–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Rooij IJM van de Port IGL Punt M, et al.: Effect of virtual reality gait training on participation in survivors of subacute stroke: a randomized controlled trial. Phys Ther 2021;101:pzab051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yu JH, Cho KH: Effectiveness of virtual reality game on functional movement and activities of daily living in hemiparetic stroke patients. J Nanoelectronics Optoelectronics 2016;11:98–102 [Google Scholar]
- 26.Lee HC Huang CL Ho SH, et al.: The effect of a virtual reality game intervention on balance for patients with stroke: a randomized controlled trial. Games Health J 2017;6:303–11 [DOI] [PubMed] [Google Scholar]
- 27.Lloréns R Gil-Gómez JA Alcañiz M, et al.: Improvement in balance using a virtual reality–based stepping exercise: a randomized controlled trial involving individuals with chronic stroke. Journal article; randomized controlled trial. Clin Rehabil 2015;29:261–8 [DOI] [PubMed] [Google Scholar]
- 28.Marques-Sule E Arnal-Gómez A Buitrago-Jiménez G, et al.: Effectiveness of Nintendo Wii and physical therapy in functionality, balance, and daily activities in chronic stroke patients. J Am Med Dir Assoc 2021;22:1073–80 [DOI] [PubMed] [Google Scholar]
- 29.Yatar GI, Yildirim SA: Wii Fit balance training or progressive balance training in patients with chronic stroke: a randomised controlled trial. J Phys Ther Sci 2015;27:1145–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Song GB, Park EC: Effect of virtual reality games on stroke patients' balance, gait, depression, and interpersonal relationships. J Phys Ther Sci 2015;27:2057–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Choi D, Choi W, Lee S: Influence of Nintendo Wii Fit balance game on visual perception, postural balance, and walking in stroke survivors: a pilot randomized clinical trial. Games Health J 2018;7:377–84 [Google Scholar]
- 32.Kim JH Jang SH Kim CS, et al.: Use of virtual reality to enhance balance and ambulation in chronic stroke: a double-blind, randomized controlled study. Am J Phys Med Rehabil 2009;88:693–701 [DOI] [PubMed] [Google Scholar]
- 33.Lee HS, Park YJ, Park SW: The effects of virtual reality training on function in chronic stroke patients: a systematic review and meta-analysis. Biomed Res Int 2019;2019:7595639–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang SH Chung EJ Lee J, et al.: The effect of trunk stability training based on visual feedback on trunk stability, balance, and upper limb function in stroke patients: a randomized control trial. Healthcare (Basel) 2021;9:532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Long Y, Ouyang RG, Zhang JQ: Effects of virtual reality training on occupational performance and self-efficacy of patients with stroke: a randomized controlled trial. J Neuroeng Rehabil 2020;17:150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.You SH Jang SH Kim YH, et al.: Virtual reality-induced cortical reorganization and associated locomotor recovery in chronic stroke: an experimenter-blind randomized study. Stroke 2005;36:1166–71 [DOI] [PubMed] [Google Scholar]
- 37.Embrechts E Van Criekinge T Schröder J, et al.: The association between visuospatial neglect and balance and mobility post-stroke onset: a systematic review. Ann Phys Rehabil Med 2021;64:101449. [DOI] [PubMed] [Google Scholar]
- 38.Yang F Lees J Simpkins C, et al.: Interventions for preventing falls in people post-stroke: a meta-analysis of randomized controlled trials. Gait Posture 2021;84:377–88 [DOI] [PubMed] [Google Scholar]
- 39.Buccino G, Solodkin A, Small SL: Functions of the mirror neuron system: implications for neurorehabilitation. Cogn Behav Neurol 2006;19:55–63 [DOI] [PubMed] [Google Scholar]
- 40.Prosperini L Tomassini V Castelli L, et al.: Exergames for balance dysfunction in neurological disability: a meta-analysis with meta-regression. J Neurol 2021;268:3223–37 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


