To address the unprecedented community spread of mpox (formerly known as monkeypox) during the 2022 global outbreak, some affected countries, mostly in Europe and north America, deployed large scale mpox vaccination programmes targeting high-risk groups such as gay, bisexual and men who have sex with men (GBMSM). These vaccination programmes used Modified Vaccinia Ankara-Bavarian Nordic (MVA-BN), a third-generation smallpox vaccine licensed for prevention of mpox based on animal efficacy studies, and human safety and immunogenicity studies.1, 2 Although previous studies from Africa have suggested that first and second-generation smallpox vaccines provide cross-protective immunity against mpox,3 with an estimated 85% protective effectiveness in one study,4 there have been no previous studies assessing clinical effectiveness of the third generation MVA-BN before the 2022 outbreak.
In The Lancet Infectious Diseases, Marta Bertran5 and colleagues retrospectively investigated real-world effectiveness of vaccination with a single subcutaneous dose of MVA-BN against symptomatic mpox among GBMSM at higher risk of exposure to mpox in England. The authors assessed vaccine effectiveness using the case-coverage or screening method, which compared vaccine coverage among mpox cases to coverage in the estimated population of 89 240 at-risk GBMSM in England. A total of 1545 laboratory confirmed mpox cases in England diagnosed between July 4 and Oct 9, 2022, were invited to complete an electronic questionnaire on demographics, vaccination history, and symptoms. Of the 1545 cases, 508 (33%) returned the questionnaire and the final analysis included 363 GBMSM mpox cases aged 15–60 years or older who provided the required information.
Of the 363 mpox infections, 322 (89·0%) were unvaccinated, eight (2·2%) occurred at least 14 days after vaccination, and 32 (8·8%) occurred within 0–13 days after vaccination (one case with missing vaccination date was excluded). At the end of the study period, the population vaccine coverage was 50% and the estimated vaccine effectiveness at least 14 days after a single dose of MVA-BN was 78% (95% CI 54 to 89) and within 0–13 days was –4% (–50 to 29). Following a sensitivity analysis, the authors estimated vaccine effectiveness of 85% (95% CI 69 to 93) for high-coverage (63% vaccine coverage) and 71% (40 to 86) for low-coverage (42% vaccine coverage) scenarios. Four of the eight breakthrough infections after 14 days were people living with HIV and only one breakthrough infection occurred in those aged 50 years and older, who were people presumed to have received previous childhood smallpox vaccine. When people older than age 50 years were excluded, the estimated vaccine effectiveness was 74% (95% CI 43 to 88).
The 78% vaccine effectiveness reported by Marta Bertran and colleagues suggests that a single dose of MVA-BN is considerably protective against symptomatic mpox only after 13 days post-vaccination. Because people living with HIV have been shown to have a higher risk of breakthrough COVID-19 infections post-vaccination,6 the identification of four of eight breakthrough mpox infections among people living with HIV by Marta Bertran and colleagues is noteworthy. However, the MVA-BN vaccines have previously been shown to be immunogenic among adults with a history of AIDS7 and larger cohorts of people living with HIV will be required to ascertain if HIV is a risk factor for MVA-BN vaccine failure. The major limitations of their study were the low questionnaire return rate and the inability to systematically adjust for potential confounders of vaccine effectiveness, including age, underlying clinical conditions (such as HIV), previous childhood smallpox vaccination, and behavioral practices related to mpox exposure. Additionally, their study did not estimate the duration of protection. It is likely that the limitations did not significantly affect the estimated vaccine effectiveness since those vaccinated within 0–13 days consistently had a vaccine effectiveness which was close to zero.
Their findings compare with two other similar studies done during the 2022 mpox outbreak. Sagy and colleagues8 estimated a vaccine effectiveness of 86% (95% CI 59 to 95) at least 21 days after a single subcutaneous dose of MVA-BN vaccination among high-risk male individuals in Israel. In another study of vaccination with a single dose of MVA-BN vaccine among GBMSM in the USA, Payne and colleagues9 reported a 14·3 times higher incidence of mpox among unvaccinated people compared with those vaccinated 14 days previously or longer. These two studies excluded individuals who were likely to have received previous childhood smallpox vaccination (those aged 50 years and older) and enrolled more study participants (more than 2000). However, the authors did not adjust for relevant confounders of vaccine effectiveness and did not assess duration of protection beyond 147 days.
Overall, these studies suggest that the use of a single dose of MVA-BN as PreP is preferable to post-exposure prophylaxis to guarantee protection against symptomatic mpox. Knowledge gaps related to effectiveness against other clades (more prevalent in Africa); protection against asymptomatic infection; duration of protection following first and second dose; immunological correlates of protection; and the roles of other confounders such as intradermal vaccination, HIV, previous smallpox vaccination, gender, age group, and degree of exposure (including route and type) in the estimation of vaccine effectiveness warrant future studies.
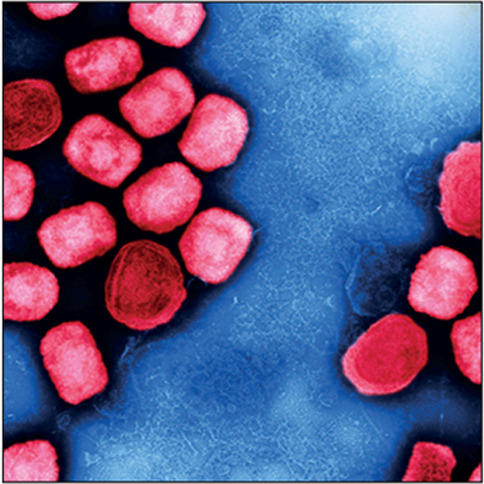
© 2023 Flickr - NIAID
DO is the President of the Nigerian Infectious Diseases Society. NSW declares no competing interests.
References
- 1.Turner Overton E, Schmidt D, Vidojkovic S, et al. A randomized phase 3 trial to assess the immunogenicity and safety of 3 consecutively produced lots of freeze-dried MVA-BN® vaccine in healthy adults. Vaccine. 2023;41:397–406. doi: 10.1016/j.vaccine.2022.10.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sudarmaji N, Kifli N, Hermansyah A, Yeoh SF, Goh B-H, Ming LC. Prevention and treatment of monkeypox: a systematic review of preclinical studies. Viruses. 2022;14 doi: 10.3390/v14112496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Poland GA, Kennedy RB, Tosh PK. Prevention of monkeypox with vaccines: a rapid review. Lancet Infect Dis. 2022 doi: 10.1016/S1473-3099(22)00574-6. published online Sept 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fine PEM, Jezek Z, Grab B, Dixon H. The transmission potential of monkeypox virus in human populations. Int J Epidemiol. 1988;17:643–650. doi: 10.1093/ije/17.3.643. [DOI] [PubMed] [Google Scholar]
- 5.Bertran M, Andrews N, Davison C, et al. Effectiveness of one dose of MVA-BN smallpox vaccine against mpox in England using the case-coverage method: an observational study. Lancet Infect Dis. 2023 doi: 10.1016/S1473-3099(23)00057-9. published online March 13. [DOI] [PubMed] [Google Scholar]
- 6.Coburn SB, Humes E, Lang R, et al. Analysis of postvaccination breakthrough COVID-19 infections among adults with HIV in the United States. JAMA Netw Open. 2022;5 doi: 10.1001/jamanetworkopen.2022.15934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Overton ET, Lawrence SJ, Stapleton JT, et al. A randomized phase II trial to compare safety and immunogenicity of the MVA-BN smallpox vaccine at various doses in adults with a history of AIDS. Vaccine. 2020;38:2600–2607. doi: 10.1016/j.vaccine.2020.01.058. [DOI] [PubMed] [Google Scholar]
- 8.Sagy YW, Zucker R, Hammerman A, et al. Real-world effectiveness of a single dose of mpox vaccine in males. Nature Med. 2023 doi: 10.1038/s41591-023-02229-3. published online Jan 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Payne AB, Ray LC, Kugeler KJ, et al. Incidence of monkeypox among unvaccinated persons compared with persons receiving ≥1 JYNNEOS vaccine dose—32 US Jurisdictions, July 31–September 3, 2022. MMWR Morb Mortal Wkly Rep. 2022;71:1278–1282. doi: 10.15585/mmwr.mm7140e3. [DOI] [PMC free article] [PubMed] [Google Scholar]


