Abstract
Killian-Jameson diverticulum:
An 82-year-old male presented with progressive dysphagia and simultaneous hoarseness of voice for the past 6 months. He had mitral valve repair and a permanent pacemaker for a heart block 5 years ago. A computed tomographic scan of the neck demonstrated a cervical esophageal diverticulum. Oral Gastrogrifin contrast study confirmed esophageal diverticulum in Killian–Jamieson space. Open surgical diverticulectomy was performed safely. Patient’s dysphagia resolved immediately, and he regained his normal voice after 6 weeks.
Introduction:
Killian–Jamieson’s esophageal diverticulum is a rare form of pulsion diverticulum which originate through a muscular gap in the anterolateral wall of the esophagus, inferior to the cricopharyngeus muscle and superior to the circular and longitudinal muscle of the esophagus. Killian–Jamieson defined this area where the recurrent laryngeal nerve enters the pharynx, called Killian–Jamieson triangle. Ekberg and Nylander, in 1983, described an esophageal diverticulum in Killian–Jamieson space. The most common clinical manifestations in such patients are dysphagia, cough, epigastric pain, recurrent respiratory tract infections, and rarely hoarseness of voice. In symptomatic patients, surgical or endoscopic resection of the diverticulum is mandatory. We report this case in line with SCARE (Surgical CAse REport) criteria.
Case Report:
An 82-year-old male presented to our outpatient clinic with a history of progressive dysphagia for solid food and hoarseness of voice for the last 6 months. He denied gastroesophageal reflux, cough, and shortness of breath. On examination of the neck, there was swelling on the left side but no tenderness or lymphadenopathy. Basic blood investigations, including complete blood count, liver, and renal panels, were normal. An echocardiogram showed mild impairment of left ventricle function and normally functioning mitral valve. Chest X-ray showed a pacemaker in position. Computed tomography scan of the neck showed esophageal diverticulum. Gastrogrifin contrast study showed esophageal Killian–Jamieson diverticulum (KJD).
Discussion:
The acquired esophageal diverticulum is categorized into three types based on its anatomical location. Zenker’s and Killian–Jamieson (pulsion diverticulum) in the proximal part, traction diverticulum in the middle part, due to pulling from fibrous adhesions following the lymph node infection and epiphanic pulsion type in the distal esophagus. Although the KJD and Zenker’s diverticulum (ZD) arise close to each other in the pharyngoesophageal area, they are anatomically distinct. Although ZD and KJD have the same demographic features, they are more commonly found in older men (60–80 years) and women, respectively. The incidence of ZD is 0.01–0.11%, and KJD is 0.025% of the population. Rubesin et al. reported radiographic findings in 16 KJD cases. They found the majority of them were on the left side (72%), followed by 20% on the right side and 8% bilateral.
Conclusion:
In conclusion, we report a rare case of dysphagia and simultaneous hoarseness of voice in an octogenarian due to KJD, who was treated with open diverticulectomy, and dysphagia resolved; he regained his voice back after 6 weeks. In our opinion, endoscopic surgery in such a patient with KJD can put recurrent laryngeal at risk of injury since an endoscopic approach operator cannot visualize and dissect away the recurrent laryngeal nerve, particularly when KJD already compresses it.
Keywords: diverticulum, esophagus, Killian–Jamieson, surgery
Highlights
We report a rare case of Killian–Jamieson diverticulum in octogenarian.
Computed tomography scan and contrast study confirmed the diagnosis.
An open diverticulectomy was performed.
The patient postoperative recovery was uneventful, and his symptoms resolved completely.
Introduction
Killian–Jamieson’s esophageal diverticulum is a rare form of pulsion diverticulum which originate through a muscular gap in the anterolateral wall of the esophagus, inferior to the cricopharyngeus muscle and superior to the circular and longitudinal muscle of the esophagus. Killian–Jamieson defined this area where the recurrent laryngeal nerve enters the pharynx, called Killian–Jamieson triangle1,2 (Fig. 1). Ekberg and Nylander3, in 1983, described an esophageal diverticulum in Killian–Jamieson space. The most common clinical manifestations in such patients are dysphagia, cough, epigastric pain, recurrent respiratory tract infections, and rarely hoarseness of voice. In symptomatic patients, surgical or endoscopic resection of the diverticulum is mandatory. We report this case in line with SCARE (Surgical CAse REport) criteria4.
Figure 1.

Drawing demonstrates the origin of Zenker’s diverticulum and Killian–Jamieson diverticulum and its relation with recurrent laryngeal nerve.
Case report
An 82-year-old male presented to our outpatient with a history of progressive dysphagia for solid food and hoarseness of voice for the last 6 months. He denied gastroesophageal reflux, cough, and shortness of breath. On examination of the neck, there was swelling on the left side but no tenderness or lymphadenopathy. Basic blood investigations, including complete blood count, liver, and renal panels, were normal. An echocardiogram showed mild impairment of left ventricle function and normally functioning mitral valve. Chest X-ray showed a pacemaker in position (Fig. 2). Computed tomography (CT) scan of the neck showed esophageal diverticulum (Fig. 3A, B). Gastrogrifin contrast study showed esophageal Killian–Jamieson diverticulum (KJD) (Fig. 4A, B).
Figure 2.

Chest X-ray showing pacemaker in position.
Figure 3.

Computed tomography scan neck (A, B) showing esophageal diverticulum (Killian–Jamieson diverticulum).
Figure 4.
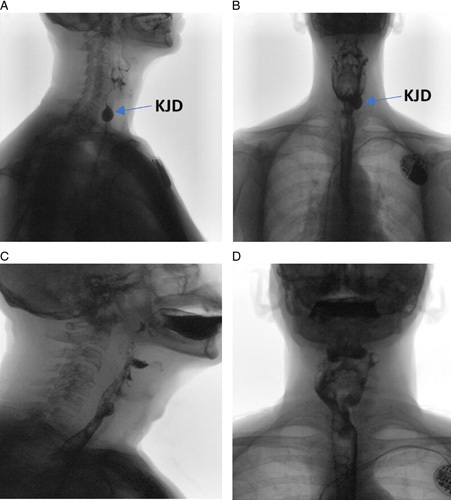
A,B preoperative Gastrografin swallow showing KJD. C,D postoperative Gastrografin swallow showing normal esophagus.
We contacted a Medtronic representative to reprogram the pacemaker from demand mode to fixed mode on the day of surgery. We approached the cervical esophagus through the neck incision along the anterior border of the sternocleidomastoid muscle; after identification, the diverticulum was carefully dissected free from surrounding structures to its origin (Fig 5A–D). d wide-bore nasogastric tube was inserted into the esophagus, and the diverticulum was stapled and removed (Fig. 2). The patient was extubated on the table, and the pacemaker was reprogrammed to demand mode. On the second postoperative recovery, the esophageal contrast study showed the free flow of contrast and no leak (Fig. 4C, D). The patient resumed a soft diet and subsequently continued with solids. Dysphagia resolved immediately and hoarseness 6 weeks after the surgery. The patient resumed back to his normal life.
Figure 5.

(A–C) Surgical exposure of Killian–Jamieson diverticulum and its origin from the esophagus. (D) Excised esophageal Killian–Jamieson diverticulum.
Discussion
The acquired esophageal diverticulum is categorized into three types based on its anatomical location. Zenker’s and Killian–Jamieson (pulsion diverticulum) in the proximal part, traction diverticulum in the middle part, due to pulling from fibrous adhesions following the lymph node infection and epiphanic pulsion type in the distal esophagus5,6. Although the KJD and ZD arise close to each other in the pharyngoesophageal area, they are anatomically distinct. Although ZD and KJD have the same demographic features, they are more commonly found in older men (60–80 years) and women, respectively. The incidence of ZD is 0.01–0.11%, and KJD is 0.025% of the population7,8. Rubesin et al. reported radiographic findings in 16 KJD cases. They found the majority of them were on the left side (72%), followed by 20% on the right side and 8% bilateral9. Pathogenies of KJD are based on the hypothesis that fictional outflow obstruction due to the inappropriate contraction of circular muscle leads to increased intraluminal pressure, which is transmitted to the weak. Another theory is that it can be due to inappropriate contraction of longitudinal and circular muscles of the esophagus associated with gastroesophageal reflux disease10,11. The KJD is often asymptomatic, but sometimes the patient can present with clinical manifestations similar to ZD patients, dysphagia, cough, respiratory tract infection due to aspiration regurgitation, chest pain, and rarely hoarseness of voice12.
Ultrasound of the neck is advised to differentiate between a thyroid nodule and KJD, as the cases have been reported as a KJD presenting synchronously with a thyroid nodule13.
Barium swallow (pharangoesophagogram) and cervical CT scan are the best diagnostic imaging modalities. The cervical CT scan can determine the origin of KJD and differentiate between ZD. There are three methods used for treating KJD conventional diverticulectomy (67%) followed by endoscopic diverticulectomy (28%), and diverticulopexy (5%)14.
Open surgical diverticulectomy is performed through a transverse or vertical neck incision with or without esophagostomy. Furthermore, Siow et al. reported that KJD is not associated with sphincter dysfunction and therefore did not require esophageal myotomy. The role of cricopharyngeal and proximal esophagostomy is controversial because KJD arises below the cricopharyngeal muscle15,16. The literature study showed that open diverticulectomy is performed in the majority of cases17–20 (Table 1). Endoscopic diverticulectomy for KJD is not a common practice because there is a high risk of recurrent laryngeal nerve injury as this nerve entry point corresponds to the base of KJD; there is a risk of the transaction and thermal damage. Few studies have been published regarding successful endoscopic treatment, including monopolar cautery and carbon dioxide laser to separate the intervening septum or an endoscopic stapler and needle knife to divide the septum21–23. Diverticulopexy should be done in high-risk patients with previous neck surgery. Conventional diverticulectomy is the standard treatment as this restores the pharyngoesophageal anatomy and eliminates the possibility of carcinogenesis in the diverticulum. Although there is no reported case of malignant changes, Herbella et al.24 reported a prevalence of malignant transformation in ZD from 0.3 to 7%. After diverticulectomy of ZD, suture or staple line leakage has been reported in 1.7–12.7% of patients25. Our case was very high risk because of old age, mitral valve repair, and permanent pacemaker dependency. The patient has hoarseness of voice, dysphagia for solids, and recent difficulty in breathing. Open diverticulectomy was performed safely, and the patient recovered fully.
Table 1.
To date reported cases of Killian–Jamieson diverticulum and treatment
| References | Age (years) | Gender | Site | Size (cm) | Management | Complication | Follow-up (months) |
|---|---|---|---|---|---|---|---|
| Roger et al.13 | 53 | F | Lt | NA | Open diverticulectomy myotomy | None | 24 |
| Present study17–20 | 55 | F | Lt | 1.6 | Endoscopic diverticulectomy | None | 3 |
| Tang et al.23 | 51 | F | Lt | 1.5 | Endoscopic diverticulectomy | None | 2 |
| Boisvert et al.18 | 69 | M | Bi | 4.5/3.5 | Diverticulectomy, esophageal open myotomy | None | 2 |
| Present study17–20 | 53 | F | Lt | 4.5 | Open diverticulectomy | None | 2 |
| Chea et al.11 | 52 | F | Rt | NA | Open diverticulectomy | None | 6 |
| Undavia et al.17 | 62 | F | Lt | 2.5 | Open diverticulectomy | None | NA |
| Kim et al.19 | 68 | M | Rt | 10 | Open diverticulectomy, esophageal myotomy | None | 6 |
| Mimatsu et al.15 | 74 | F | Bi | 1.5/4 | Open diverticulectomy | NA | 24 |
| Present study17–20 | 54 | F | Rt | NA | Open diverticulectomy, esophageal myotomy | NA | 24 |
| Present study17–20 | 18 | F | Rt | Open diverticulectomy | None | 12 | |
| Chang et al.22 | 46 | F | Lt | 5 | Endoscopic diverticulectomy | None | 6 |
| Present study17–20 | 49 | M | Rt | NA | Open diverticulectomy | None | 6 |
| Present study17–20 | 49 | F | Lt | NA | Open diverticulectomy | None | 3 |
| Present study17–20 | 2 | F | Rt | NA | Open diverticulectomy | NA | 5 |
| Present study17–20 | 88 | M | Lt | 2.5 | Endoscopic diverticulectomy | NA | 1 |
| Stewart et al.7 | 69 | M | Rt | Open diverticulectomy | None | 2 | |
| Present study17–20 | 71 | F | Lt | 2.5 | Endoscopic diverticulectomy | None | 2 |
| Saisho et al.14 | 77 | F | Lt | 2 | Open diverticulectomy | None | 24 |
| Present study17–20 | 52 | M | Lt | NA | Conservative | NA | NA |
| Present study17–20 | 54 | M | Lt | 1.1 | Conservative | NA | NA |
| Present study17–20 | 58 | F | Lt | NA | Conservative | NA | NA |
| Present study17–20 | 62 | F | Lt | 1 | Conservative | NA | NA |
| Present study17–20 | 56 | F | Lt | NA | Conservative | NA | NA |
| Huang et al. | 70 | F | Lt | 2.2 | Conservative | NA | NA |
| Yang and Draganov21 | 81 | M | Rt | 6.6 | Endoscopic diverticulectomy | None | NA |
| Present study17–20 | 76 | F | Lt | NA | Conservative | NA | NA |
| Orzell et al.12 | 78 | M | Rt | NA | Open diverticulectomy | None | NA |
| Our case | 82 | M | Lt | 5.5 | Open diverticulectomy | None | 7 |
Conclusion
In conclusion, we report a rare case of dysphagia and simultaneous hoarseness of voice in an octogenarian due to KJD, who was treated with open diverticulectomy, and dysphagia resolved; he regained his voice back after 6 weeks. In our opinion, endoscopic surgery in such a patient with KJD can put recurrent laryngeal at risk of injury since an endoscopic approach operator cannot visualize and dissect away the recurrent laryngeal nerve, particularly when KJD already compresses it.
Ethical approval
IRB approval.
Patient consent
Written informed consent was obtained from the patients for the publication of this and the accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
None.
Author contribution
I.U.H.C.: senior operating surgeon and wrote the discussion section; A.M.A.G.: wrote the abstract; M.A.A.A.: searched references; Y.A.Q.: wrote the introduction section; T.A.: searched references and helped in the revision; B.R.: searched references and wrote part of the discussion section; O.M.A.F.: assistant surgeon arranged the table and figures and wrote the highlights section.
Conflicts of interest disclosure
The authors declare that they have no financial conflicts of interest with regard to the content of this report.
Research registration unique identifying number (UIN)
Name of the registry: Research registry.
Unique identifying number or registration: 8609.
Hyperlink to your specific registration (must be publicly accessible and will be checked): http://www.researchregistry.com/browse-the-registry#home/
Guarantor
Ikram Ul H. Chaudhry.
Provenance and peer review
Not commissioned externally peer-reviewed.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 24 March 2023
Contributor Information
Ikram U. H. Chaudhry, Email: drihc007@gmail.com.
Abdullah M. Al Ghamdi, Email: Dr.surgeon@hotmail.com.
Yousif Al Qahtani, Email: yosif.qahtani@kfsh.med.sa.
Thabet Algazal, Email: thabetsurg@gmail.com.
Beenish Razzaq, Email: Beenishrazzaq7@gmail.com.
Meenal A. Al Abdulhai, Email: meenal.abulhai@gov.med.sa.
Othman M. Al Fraih, Email: Alfrah.othman@gmail.com.
References
- 1. Jamieson EB. Illustrations of Regional Anatomy (Section 2). E&S Livingstone Ltd; 1934:44. [Google Scholar]
- 2. Zanio C, Jacobson HG, Lepow H, et al. The pharyngoesophageal sphincter. Springfield’s Thomas 1950;29:144. [Google Scholar]
- 3. Ekberg O, Nylander G. Lateral diverticulum from the pharyngoesophageal junction area. Radiology 1983;146:117–22. [DOI] [PubMed] [Google Scholar]
- 4. Agha RA, Franchi T, Sohrabi C, et al. for the Scare group. The SCARE 2020 guidelines: updating consensus Surgical case report (SCARE) Guidelines. Int J Surg 2020;84:226–30. [DOI] [PubMed] [Google Scholar]
- 5. Khan N, Ismail F, Van de Werke IEA. Oesophageal pouches and diverticula: a pictorial review. S Afr J Surg 2012;50:71–5. [DOI] [PubMed] [Google Scholar]
- 6. Alnimer L, Zakaria A, Piper M. Killian Jamieson diverticulum: a rare cause of dysphagia. Cureus 2021;13:e13654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Stewart KE, Smith DRK, Woolley SL. Simultaneously occurring Zenker’s diverticulum and Killian–Jamieson diverticulum case report and literature review. J Laryngol Otol 2017;131:661–6. [DOI] [PubMed] [Google Scholar]
- 8. Boisvert RD, Bethune DCG, Acton D, et al. Bilateral Killian–Jamieson diverticula: a case report and literature review. Can J Gastroenterol 2010;24:173–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rubesin SE, Levine MS. Killian–Jamieson diverticula: radiographic findings in 16 patients. AJR Am J Roentgenol 2001;177:85–9. [DOI] [PubMed] [Google Scholar]
- 10. Resouly A, Braat J, Jackson A, et al. Pharyngeal pouch: link with reflux and esophageal dysmotility. Clin Otolarlaryngol Allied Sci 1994;19:241–2. [DOI] [PubMed] [Google Scholar]
- 11. Chea CH, Siow SL, Khor TW, et al. Killian–Jamieson diverticulum: the rare esophageal diverticulum. Med J Malaysia 2011;66:73–4. [PubMed] [Google Scholar]
- 12. Orzell S, Falcone T, Grillone G. Killian–Jamieson diverticulum: a case report and argument for transcervical diverticulectomy. J Otolaryngol Rhinol 2016;2:1–4. [Google Scholar]
- 13. Rogers PJ, Armstrong WB, Dana E. Killian–Jamieson diverticulum: a case report and review of the literature. Ann Otol Rhinol Laryngol 2000;109:1087–91. [DOI] [PubMed] [Google Scholar]
- 14. Saisho K, Matano S, Tanaka T, et al. Surgery for Killian–Jamieson diverticulum: a report of two cases. Surg Case Rep 2020;6:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mimatsu K, Odia T, Kano H, et al. Killian–Jamieson diverticula presenting synchronously with thyroid adenoma. Case Rep Gastroenterol 2013;7:188–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Siow SL, Mahendran HA, Hardin M. Transcervical diverticulectomy for Killian–Jamieson diverticulum. Asian J Surg 2017;40:324–8. [DOI] [PubMed] [Google Scholar]
- 17. Undavia S, Anand SM, Jacobson AS. Killian–Jamieson diverticulum: a case of open transcervical excision. Laryngoscope 2013;123:414–7. [DOI] [PubMed] [Google Scholar]
- 18. Boisvert RD, Bethune DCG, Acton D, et al. Bilateral Killian–Jamieson diverticula: case report and literature review. Can J Gastroenterol 2010;24:173–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kim DC, Hwang JJ, Lee WS, et al. Surgical treatment of Killian–Jamieson diverticulum. Korean J Thorac Cardiosvasc Surg 2012;45:272–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kim DC, Hawang JJ, Lee WS, et al. Surgical treatment of Killian–Jamieson diverticulum. Korean J Thorac Cardiovasc Surg 2012;45:272–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yang D, Draganov PV. Endoscopic Killian–Jamieson diverticulectomy using scissor type electrosurgical knife. Endoscopy 2018;50:E175–6. [DOI] [PubMed] [Google Scholar]
- 22. Chang Y-C, Chi C-Y, Lee C-J. Rigid endoscopic laser diverticulectomy for lateral pharyngoesophageal diverticula: case presentation and discussion. Eur Arch Otolayringol 2016;273:4637–42. [DOI] [PubMed] [Google Scholar]
- 23. Tang S-J, Tang L, Chen E, et al. Flexible endoscopic Killian–Jamiesin diverticulectomy and literature review. Gastrointest Endosc 2008;68:790–3. [DOI] [PubMed] [Google Scholar]
- 24. Herbella FAM, Dubecz A, Patti MG. Esophageal diverticula and cancer. Dis Esophagus 2012;25:153–8. [DOI] [PubMed] [Google Scholar]
- 25. Puma F, Vannucci J, Fioroni C, et al. Surgical treatment for Zenker’s diverticulum comparison between diverticulectomy and diverticulopexy. Esophagus 2014;11:64–71. [Google Scholar]


