One of the most significant effects of the pandemic globally has been the greatly diminished immunization coverage of children. The coronavirus disease 2019 (COVID-19) pandemic has harmed vaccination schedules by interrupting the vaccine trade, lowering vaccine accessibility and availability in healthcare facilities, discouraging people from attending vaccination programs, and reducing community vaccine sensitivities1. WHO data showed that up to November 2022, almost 40 million children worldwide had missed a measles vaccine dose in the past year. A historical high of 25 million children skipped their first dosage, and another 14.7 million missed their second. Because of it, there were approximately 9 million measles patients and more than 1 lakh deaths in 2021, while 22 nations experienced large disruptive outbreaks2. A total of 17,500 cases of measles were identified in African countries in early 2022, with Zimbabwe topping the list1. Furthermore, millions around the world, who were dislocated as a result of wars and catastrophes in countries with strained healthcare systems, such as Ukraine, Ethiopia, Somalia, Pakistan, and Afghanistan, faced disruptions in routine immunization services, a shortage of safe drinking water and sanitation, and poor living conditions, thereby increasing the risk of vaccine-preventable infectious diseases3,4.
The latest measles emergency in various regions of the world has highlighted how the COVID-19 pandemic has harmed the national immunization plans of various countries. The global rise of the increasing measles caseload is a worrisome indication of an increased danger of the emergence of vaccine-preventable illnesses, which might lead to more significant outbreaks.
A large number of cases in different countries can be credited to the COVID-19 pandemic, which imposed a prolonged nationwide lockdown. The pandemic overwhelmed the health systems and led to a revival and resurgence of fatal illnesses, including measles. This pandemic probably resulted in an immunization gap as people were hesitant to bring their kids for vaccinations. It was a gap in global immunization coverage that susceptible children could not afford. Measles can be averted by simply getting a vaccine. But the ensuing lockdown resulted in diminished hospital visits and missing vaccine doses. Measles, a highly contagious virion, thus spread like wildfire, with a manifold increase in the caseload. The hazard was further increased after the upliftment of the lockdown because many regions reduced social distancing policies put in place at the pandemic’s peak. This allowed the measles virus to spread akin a storm in unprotected communities5.
In partnership with other organizations, WHO and UNICEF assisted in attempting to improve immunization systems worldwide. They played a vital role in child welfare via vaccine development, dissemination, and delivery6. Numerous catch-up campaigns were launched in different countries to get the essential immunization services back on track and ensure everyone can access these life-savior vaccines. Many state officials judiciously organized many immunization camps and rapidly ramped up measles vaccination, employing door-to-door surveillance programs to vaccinate children under 5 years of age. However, the district health officials noted that regions with more significant home births, especially in the villages, had greater vaccine hesitancy or refusal7.
Measles is a highly contagious vaccine-preventable disease. The signs and symptoms include fever, rash, conjunctivitis or ‘red eye,’ runny nose, and cough. It also leads to meningoencephalitis, xerophthalmia, corneal ulcers (resulting in blindness), abnormal coagulation, and myocarditis8. It is the leading cause of blindness in children in low-income countries9. Moreover, it is one of the foremost reasons for diarrhea, pneumonia, and weakened immune systems or ‘immune amnesia’ in kids under 5years of age. Children can be protected from measles with two doses of the safe and effective measles vaccination and coverage of at least 95%. Evidence indicates that nonvaccinated children have a 70% higher risk of mortality than those vaccinated against the disease1
The way forward
Inadequate immunization and breakthrough illness are the critical reasons behind the spike in cases globally. Inequities in vaccine accessibility and a shift in funds away from routine immunization due to the COVID-19 pandemic kept too many children unprotected from measles and other vaccine-preventable infections. Though global agencies have made substantial efforts, a further commitment to the cause is essential. The authorities can consider lowering the age of primary vaccination for measles to 6 months. Moreover, malnourished children should be taken care of on a priority basis, as malnutrition correlates with augmented viral infection severity scores10. Two doses of vitamin A should be ensured alongside the measles vaccine to prevent ocular morbidity associated with the disease11. Speedy vaccination coverage should be promoted in vulnerable regions to decrease the number of unvaccinated children. The focus should primarily be on areas with more than 10% measles outbreaks. Attempts should also be put up to bust myths and misapprehensions regarding immunization in societies. Sensitization meetings should be conducted to educate the masses and raise awareness regarding the illness. Religious leaders should be involved in extending support for immunization. Meetings with vaccine-hesitant parents should be organized to alleviate their fears.
Measles outbreaks may potentially forewarn epidemics of other illnesses that may not spread as quickly. Robust surveillance practices are needed to recognize outbreaks immediately, treat them swiftly, and immunize all children who have not yet been immunized against vaccine-preventable illnesses2. So globally, nations stand at crossroads, requiring sustained efforts by public health experts, virologists, and pediatricians to mitigate this newfound crisis and provide equitable, affordable, and accessible vaccines to every child (Fig. 1).
Figure 1.
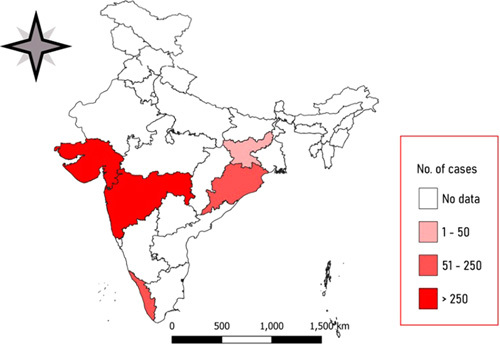
Choropleth map showing measles outbreaks in the states and union territories of India between 1 January 2022 and 28 November 2022, as reported in local media reports. The map was created using QGIS 3.28.0. The base layer map was used from the Survey of India.
Ethical approval
Not applicable.
Sources of funding
No funding was received.
Author contribution
P.C.G. and P.S.: designed and drew the original draft; A.G., R.S., and B.K.P.: reviewed the literature and critically edited the manuscript. All authors read and approved the final manuscript.
Conflicts of interest disclosure
There were no conflicts of interest.
Research registration unique identifying number (UIN)
1. Name of the registry: NA.
2. Unique identifying number or registration ID: NA.
3. Hyperlink to your specific registration (must be publicly accessible and will be checked): NA.
Guarantor
Ranjit Sah.
Footnotes
P.C.G. and P.S. contributed equally as first authors.
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article
Published online 17 February 2023
Contributor Information
Parul C. Gupta, Email: pcgpgi@gmail.com.
Prakasini Satapathy, Email: prakasini.satapathy@gmail.com.
Ankur Gupta, Email: ag_pgi@yahoo.com.
Ranjit Sah, Email: ranjitsah@iom.edu.np.
Bijaya K. Padhi, Email: bkpadhi@gmail.com.
References
- 1. Sah R, Dor VJ, Satapathy P, et al. A look at vaccine-preventable disease outbreaks amid crises in low-income countries through the lens of health equity. Travel Med Infect Dis 2023;51:102508. [DOI] [PubMed] [Google Scholar]
- 2. WHO. Nearly 40 million children are dangerously susceptible to growing measles threat. Accessed 10 January 2023. https://www.who.int/news/item/23-11-2022-nearly-40-million-children-are-dangerously-susceptible-to-growing-measles-threat
- 3. Iacobucci G. Measles is now “an imminent threat” globally, WHO and CDC warn. BMJ 2022;379. 10.1136/bmj.o2844 [DOI] [PubMed] [Google Scholar]
- 4. Tariq S, Niaz F, Afzal Y, et al. Pakistan at the precipice: the looming threat of measles amidst the COVID-19 pandemic. Front Public Health 2022;10:1000906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. UNICEF. Measles cases are spiking globally. Accessed 10 January 2023. https://www.unicef.org/stories/measles-cases-spiking-globally
- 6. WHO. UNICEF and WHO warn of perfect storm of conditions for measles outbreaks, affecting children. Accessed 10 January 2023. https://www.who.int/news/item/27-04-2022-unicef-and-who-warn-of--perfect-storm--of-conditions-for-measles-outbreaks--affecting-children
- 7. The Indian Express. 1.74 lakh children in Maharashtra missed measles shots till September. Published 23 November 2022. Accessed 27 November 2022. https://indianexpress.com/article/cities/mumbai/1-74-lakh-children-in-maharashtra-missed-measles-shots-till-september-8283905/
- 8. Kondamudi NP, Waymack JR. Measles. StatPearls Publishing; 2022. Accessed 11 January 2023. http://www.ncbi.nlm.nih.gov/books/NBK448068/ [PubMed] [Google Scholar]
- 9. Semba RD, Bloem MW. Measles blindness. Surv Ophthalmol 2004;49:243–55. [DOI] [PubMed] [Google Scholar]
- 10. Salman Y, Shaeen SK, Khan HA, et al. The effect of child malnourishment on measles spread amidst the COVID-19 pandemic in Afghanistan. Ann Med Surg 2022;78:103798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Imdad A, Mayo-Wilson E, Haykal MR, et al. Vitamin A supplementation for preventing morbidity and mortality in children from six months to five years of age. Cochrane Database Syst Rev 2022;3:CD008524. [DOI] [PMC free article] [PubMed] [Google Scholar]


