Abstract
Introduction
A systematic literature review and meta-analysis was conducted to identify and obtain a precise single summary estimate on complete spectacle independence after bilateral implantation of a trifocal intraocular lens (IOL) (AcrySof PanOptix, TFNTXX/TFATXX) for patients undergoing cataract surgery.
Methods
A search was conducted in PubMed from January 2017 to September 2021. Relevant congress presentations were also searched to include data from completed studies not yet published. Search terms included the intervention (TFNTXX, TFATXX, PanOptix) and outcomes of interest (patient-reported spectacle independence rates). A Bayesian random-effects meta-analysis was conducted, providing a pooled estimate (median and its 95% credible interval) of complete spectacle independence rates among cataract surgery patients. Subgroup analyses evaluated spectacle independence after cataract surgery across different working distances (near, intermediate, far).
Results
Nineteen unique clinical studies were identified. Based on a meta-analysis of 13 studies (N = 513 patients), the complete spectacle independence rate after cataract surgery with TFNTXX/TFATXX IOL was 91.6% (95% credible interval 86.8–95.9%). Additionally, the spectacle independence rates at each focal point (N = 13 studies, 603 patients) were 89.6% (near), 96.3% (intermediate), and 95.9% (far).
Conclusions
This meta-analysis demonstrated that at least nine out of ten patients receiving TFNTXX/TFATXX trifocal IOL during cataract surgery can expect to achieve complete spectacle independence. This study provides informative data for clinicians and patients to feel confident in the use of trifocal intraocular lenses as presbyopia-correcting IOLs that offer high rates of complete spectacle independence.
Keywords: Cataract surgery, Trifocal IOL, PanOptix IOL, Presbyopia, Spectacle independence
Key Summary Points
| With advancements in intraocular lens (IOL) technologies and increased patient expectations, spectacle independence after cataract surgery has become of greater interest in recent years. |
| Many studies have reported spectacle independence rates among patients implanted with PanOptix trifocal IOL, but pooled results were unclear. |
| This meta-analysis of 13 unique clinical studies demonstrated that at least nine out of ten patients receiving PanOptix trifocal IOL during cataract surgery can expect to achieve complete spectacle independence. |
| We believe that the findings from this review will help clinicians and patients make an informed decision in the selection of trifocal intraocular lens technology for presbyopia correction during cataract surgery. |
Introduction
Cataract surgery is one of the most frequently performed surgical procedures in the USA, with nearly 4.7 million surgeries carried out in 2021 [1]. Many of these patients undergoing cataract surgery also present with presbyopia, an age-related refractive disorder (common among individuals 40 years and older) that impairs near vision due to decrease in accommodation of the eye [2, 3].
In recent years, advancements in intraocular lens (IOL) technologies have provided patients with the opportunity to correct or mitigate presbyopia during cataract surgery and achieve a high degree of postoperative spectacle independence [2]. With new available technologies, the number of patients receiving presbyopia-correcting IOLs (PCIOLs) in the USA has increased to 8% in 2021, compared with 6.7% in 2019 [1].
In 2019, AcrySof IQ PanOptix (TFNTXX/TFATXX; Alcon Laboratories, Inc.) became the first trifocal IOL approved by the US Food and Drug Administration (FDA) [4]. Bilateral implantation of TFNTXX/TFATXX is clinically shown to reduce the effects of presbyopia by delivering 20/20 visual acuity at near (40 cm), intermediate (60 cm), and far (4 m) vision while significantly reducing the need for glasses after surgery, when compared with a standard monofocal IOL [4].
Complete spectacle independence, or never requiring glasses for any daily activities, after implantation of the TFNTXX/TFATXX IOL has been reported in several clinical studies across the world. However, reported rates of spectacle independence have considerable variation across studies, making it difficult for surgeons and patients to make an informed choice regarding expected postoperative spectacle independence outcomes. Therefore, we conducted this systematic literature review and meta-analysis to identify and pool published evidence on complete spectacle independence after bilateral implantation of the TFNTXX/TFATXX IOL for patients undergoing cataract surgery.
Methods
Literature Search
A systematic literature review was conducted to identify relevant studies. The review followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines [5]. A literature search was conducted in PubMed from January 2017 to September 2021. Abstracts from relevant 2021 cataract and ophthalmology congresses (American Society of Cataract and Refractive Surgery, ASCRS; European Society of Cataract and Refractive Surgeons, ESCRS; Asia Pacific Association of Cataract and Refractive Surgeons, APACRS; American Academy of Ophthalmology, AAO; Asia Pacific Academy of Ophthalmology, APAO) were also searched to include data from completed studies not yet published. Relevant search terms included the intervention (TFNTXX, TFATXX, PanOptix) and outcomes of interest (patient-reported spectacle independence rates). The target population was patients requiring cataract surgery who were implanted bilaterally with the TFNTXX/TFATXX trifocal IOL, without geographical restriction. Randomized and observational clinical studies that reported spectacle independence rates at a postsurgery follow-up of at least 1 month were included. For the studies that reported results with both bilateral and unilateral implantation of TFNTXX/TFATXX, only the results pertaining to those patients implanted bilaterally were included. The inclusion and exclusion criteria are detailed in Table 1.
Table 1.
Literature review inclusion and exclusion criteria
| Category | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Patient population |
Patients requiring cataract surgery No geographical restriction |
|
| Intervention | Bilateral implantation of TFNTXX/TFATXX IOL | Studies reporting unilateral implantation of TFNTXX/TFATXX and those reporting a combination of results (unilateral and bilateral) |
| Outcomes |
Complete spectacle independence (base-case analysis) Spectacle independence for far, intermediate, and near vision (subgroup analyses) |
|
| Study design | Randomized and observational clinical studies with at least 1 month follow-up |
IOL intraocular lens
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Extraction
The data from the studies included in the review were extracted by one reviewer using a predefined data extraction grid and quality checked by a second reviewer. Data collected included study citation, objective, location, methodology, follow-up duration, patient-reported outcome measure used, participants/observations, inclusion criteria, exclusion criteria, PanOptix IOL model, and spectacle independence rates (complete, far, intermediate, and near vision).
Quality Assessment
The quality assessment was performed using the RoB2 (a revised Cochrane risk-of-bias tool for randomized trials) [6] and ROBINS-I (Risk Of Bias In Non-randomised Studies-of Interventions) [7] tools to evaluate the risk of bias of each study. The possible risk-of-bias judgments included low,1 moderate/some concerns,2 and serious/critical/high [6, 7].3 However, an “a priori” decision was made to not exclude any studies on the basis of study quality in order to include all possible estimates related to spectacle independence in the meta-analysis.
Meta-Analyses
A Bayesian Markov Chain Monte Carlo (MCMC) approach was conducted using a random-effects model to pool published evidence on the spectacle independence rate in patients with bilateral implantation of TFNTXX/TFATXX IOL [8]. The random-effects model allows for heterogeneity in the effect of the trifocal IOL on overall spectacle independence across studies. The model assumed the log odds (i.e., log ratio of the probability of achieving spectacle independence and probability of not achieving spectacle independence) from each study to be of a normal distribution, where the pooled effect represents the overall population mean effect and standard deviation represents heterogeneity among the studies. Posterior distributions are summarized by the median and 95% credible intervals (95% probability that the true effect falls within the interval), which is analogous to 95% confidence intervals in classical statistics.
All analyses were conducted in the freely available software package WinBUGS and R, using the R2Winbugs interface package [9]. Convergence to the target posterior distributions was assessed using the Gelman–Rubin statistic [10]. The chains converged within 50,000 iterations, so a burn-in of 50,000 iterations was used. We retained a further 30,000 iterations of the Markov chain to estimate parameters using one chain and thinning every 5 iterations. The absolute goodness of fit was checked by comparing the number of data points with the total residual deviance. A model has a good fit when the estimated total residual deviance is close to the number of data points.
The base-case analysis was performed to estimate the pooled rate of complete spectacle independence in patients undergoing cataract surgery with bilateral implantation of the TFNTXX/TFATXX trifocal IOL. Further subgroup analyses were conducted to estimate the rate of spectacle independence for far, intermediate, and near vision in patients undergoing cataract surgery with bilateral implantation of TFNTXX/TFATXX.
Results
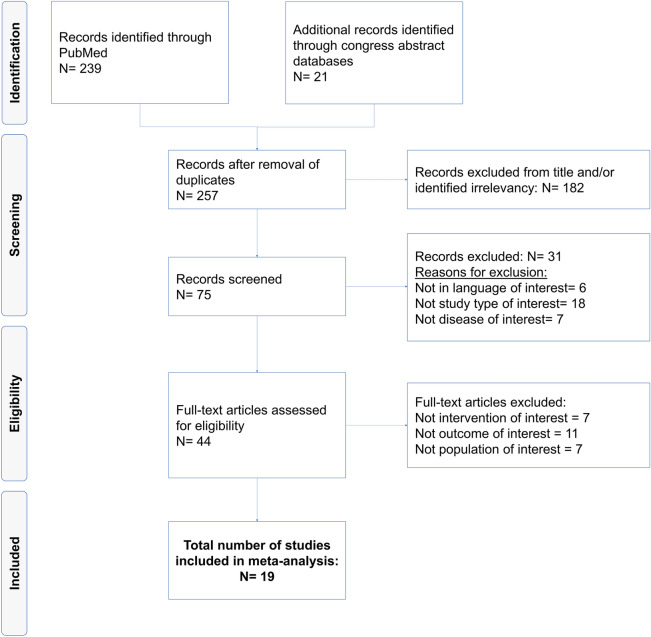
The PubMed and congress presentation search identified 257 studies. After title and abstract screening, 44 studies were included for full text reads, 19 of which were included in the review; 13 studies reported complete spectacle independence after cataract surgery, and 13 reported spectacle independence based on far, intermediate, and near vision. A PRISMA flow chart showing the screening process with reason of exclusion is provided in Fig. 1.
Fig. 1.
PRISMA flow chart
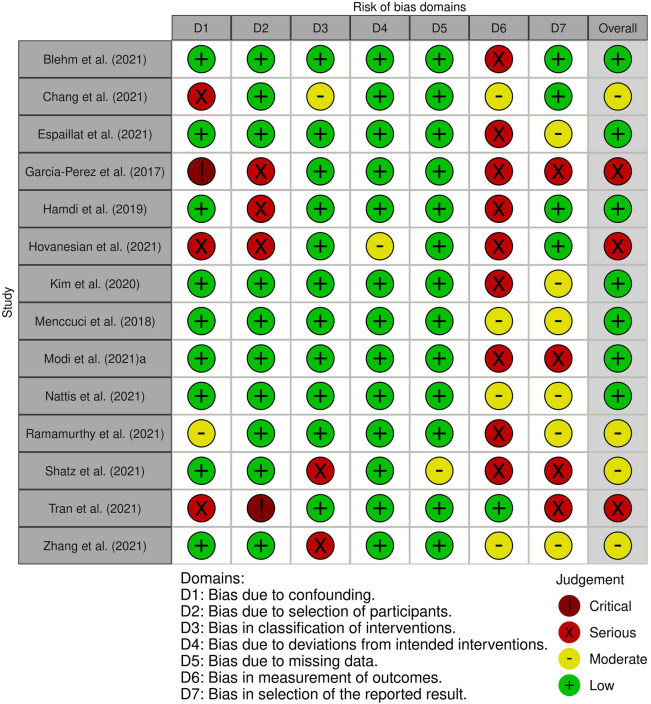
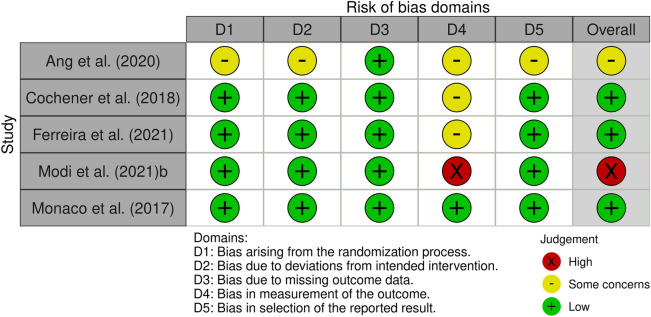
The studies included in the review were from 14 countries, the majority of which were from the USA (N = 7). Most studies were peer-reviewed publications (N = 13), while six were congress presentations. In terms of study design, 17 were prospective and 2 were retrospective, with a mix of randomized controlled trials, case series, and multicenter single-arm and double-arm nonrandomized case series. The characteristics and reported spectacle independence estimates of each study are detailed in Table 2 [11–29]. Of note, the patient demographics included individuals requiring bilateral cataract surgery with no pre-existing ocular pathology or systemic diseases that might affect postoperative visual acuity. The majority of patients also underwent their second eye surgery within 7–90 days, with one study (Shatz et al. [27]) noting patients were bilaterally implanted with the trifocal IOL on the same day. From the quality assessment, the overall judgment for risk of bias of the studies included in the review was low (N = 10), moderate/some concerns (N = 5), and serious/high (N = 4). The details of the quality assessment for each study are provided in the supplementary data (Figs. 2, 3).
Table 2.
Characteristics and reported spectacle independence (SI) of included studies
| References | Study country | N (pts) | Study design | Follow-up (months) | Method used to determine SI | SI (complete) | SI (far) | SI (intermediate) | SI (near) |
|---|---|---|---|---|---|---|---|---|---|
| Ang et al. [11] | Singapore, Philippines, Spain, New Zealand, Germany | 54 | Prospective multicenter randomized | 12 | PRSIQ | 91% | 93% | 93% | 83% |
| Blehm et al. [12] | USA | 30 | Prospective single arm | 3 | PRSIQ | 86.7% | 97% | 90% | 87% |
| Chang et al. [13] | China | 21 | Prospective | 3 | NR | 100% | NR | NR | NR |
| Cochener et al. [14] | France | 20 | Prospective randomized single-center comparative | 6 | A quality-of-life questionnaire | 89% | NR | NR | NR |
| Espaillat et al. [15] | Dominican Republic | 70 | Retrospective single center | 6 | Nonvalidated questionnaire | NR | 98.3% | 100% | 98.3% |
| Ferreira et al. [16] | Portugal | 30 | Randomized comparative clinical trial | 3 | NR | 96% | NR | NR | NR |
| Garcia-Perez et al. [17] | Spain | 58 | Prospective case series | 9–12 | Nonvalidated questionnaire | 94.8% | 94.8% | 98.3% | 96.6% |
| Hamdi et al. [18] | Saudi Arabia | 25 | Prospective case series | Average 2.5 (range 1–9) | Nonvalidated questionnaire | 96.8% | NR | NR | NR |
| Hovanesian et al. [19] | USA | 59 | Prospective open-label multicenter | > 1 | Validated PRO (MDBackline, Laguna Beach, CA, USA) | 83% | NR | NR | NR |
| Kim et al. [20] | South Korea | 44 | Prospective multicenter single arm | 3 | 12-Item questionnaire | NR | 96% | 91% | 84% |
| Menccuci et al. [21] | Italy | 20 | Prospective nonrandomized case series | 3 | Nonvalidated questionnaire | NR | 100% | 100% | 70% |
| Modi et al. [22] | USA | 127 | Prospective multicenter nonrandomized | 6 | IOLSAT | 80.5% | 95.9% | 94.3% | 83.6% |
| Modi et al. [23] | USA | 15 | Prospective randomized single center | 1 | NR | 100% | NR | NR | NR |
| Monaco et al. [24] | Italy | 20 | Prospective randomized case series | 3 | Spectacle dependence questionnaire asked patients to rate how often (always, sometimes, never) they used spectacles for any purpose and for far, intermediate, and near vision | 85% | 90% | 100% | 90% |
| Nattis et al. [25] | USA | 39 | Prospective nonrandomized | 1 | Nonvalidated questionnaire | NR | 95% | 97% | 92% |
| Ramamurthy et al. [26] | India | 67 | Prospective multicenter single arm | 3 | Derived from SILVER and APPLES | NR | 94% | 97% | 95.5% |
| Shatz et al. [27] | USA | 29 | Prospective single arm | 3 | PRSIQ | 90% | 97% | 97% | 86% |
| Tran et al. [28] | USA | 25 | Prospective single-center double-arm masked | Average 4.1 (range 2.6–8.2) | PRSIQ | 96% | 96% | 96% | 88% |
| Zhang et al. [29] | China | 18 | Prospective comparative | 3 | Chinese version validated QUVID | NR | 100% | 94.4% | 83.3% |
APPLES Assessment of Photic Phenomena and Lens EffectS, EU Europe, IOLSAT Intraocular Lens Satisfaction, NR not reported, pts patients, PRSIQ Patient Reported Spectacle Independence Questionnaire, QUVID Questionnaire for Visual Disturbance, SI spectacle independence, SILVER Spectacle Independence Lens Vision Evaluation and Repurchase
Fig. 2.
Quality assessment for nonrandomized studies using the ROBINS-I tool
Fig. 3.
Quality assessment of randomized studies using the RoB2 tool
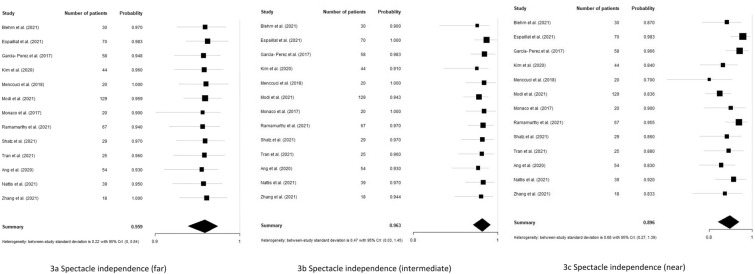
The base-case meta-analysis of 13 studies that reported complete spectacle independence in 513 patients who underwent cataract surgery with bilateral implantation of TFNTXX/TFATXX was 91.6%, with 95% credible interval (CrI) between 86.8 and 95.9%. The heterogeneity in the treatment effect was high, with a between study standard deviation of 0.65 (95% Crl 0.22–1.46) (See Fig. 4).
Fig. 4.
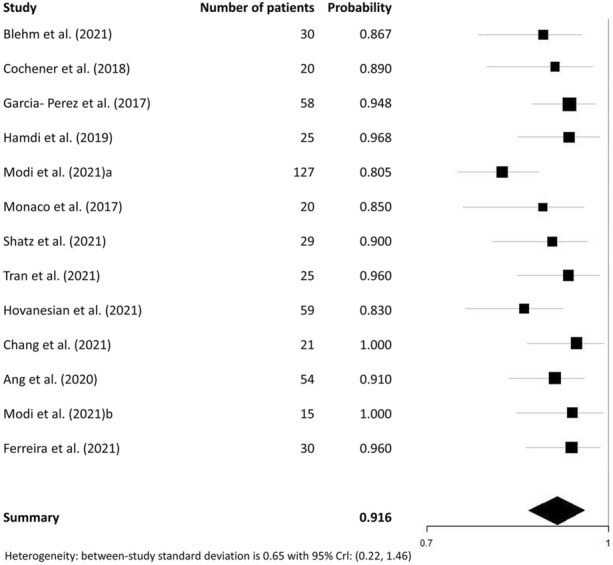
Forest plot for the base-case meta-analysis (complete spectacle independence after cataract surgery with bilateral implantation of TFNTXX/TFATXX trifocal IOL)
We performed a total of three subgroup analyses, namely for far, intermediate, and near vision after cataract surgery. Among 13 studies and 603 patients receiving cataract surgery with TFNTXX/TFATXX bilateral implantation, far vision spectacle independence was 95.9% (95% CrI 93.9–97.4%), intermediate vision spectacle independence was 96.3% (95% CrI 94.1–98.2%), and near vision spectacle independence was 89.6% (95% CrI 84.1–93.9%). The heterogeneity in the treatment effect for far, intermediate, and near spectacle independence was moderate (between-study standard deviation of 0.22, 95% CrI 0–0.84), moderate (0.47, 95% CrI 0.03 to 1.45), and high (0.68, 95% CrI 0.27 to 1.39), respectively (Fig. 5a–c). A summary of estimates generated through the meta-analyses as well as number of studies and patients that were included in each analysis are reported in Table 3.
Fig. 5.
a–c Forest plots for the subgroup meta-analyses (spectacle independence based on distance after cataract surgery with bilateral implantation of TFNTXX/TFATXX trifocal IOL)
Table 3.
Meta-analysis summary of spectacle independence estimates
| Model description | Studies (N) | Absolute model fit | Heterogeneity | Spectacle independence | |
|---|---|---|---|---|---|
| Number of patients | TRD | SD (95% CrI) | Probability (95% CrI) | ||
| Base-case analysis | |||||
| Complete spectacle independence | 13 | 513 | 13.3 | 0.65 (0.22, 1.46) | 0.916 (0.868, 0.959) |
| Subgroup analyses | |||||
| Far vision spectacle independence | 13 | 603 | 8.86 | 0.22 (0.00, 0.84) | 0.959 (0.939, 0.974) |
| Intermediate vision spectacle independence | 13 | 603 | 14.56 | 0.47 (0.03, 1.45) | 0.963 (0.941, 0.982) |
| Near vision spectacle independence | 13 | 603 | 13.07 | 0.68 (0.27, 1.39) | 0.896 (0.841, 0.939) |
CrI credible interval, SD standard deviation, TRD total residual deviance
Discussion
The present study is a systematic literature review and meta-analysis based on 13 clinical studies that yields novel important results, demonstrating that complete spectacle independence (not requiring glasses for any daily activities) is almost 92% in patients receiving TFNTXX/TFATXX IOL after cataract surgery. Furthermore, spectacle independence is highest for intermediate and far vision (about 96%), and lowest for near vision (90%). This information can help clinicians with preoperative counseling and in feeling confident in selecting IOLs for cataract surgery as per patients’ needs, and in turn offering improved overall vision-related quality of life for patients [30].
The high rate of spectacle independence can be attributed to the technology behind TFNTXX/TFATXX IOL, that is, a trifocal IOL model with proprietary ENLIGHTEN optical technology providing high light utilization that allows it to transmit 88% of the light to the retina to optimize visual acuity at each focal point as well as the diffractive optical zone of 4.5 mm non-apodized for pupil independence [22]. These attributes provide patients with a range of vision from intermediate to near, while preserving far vision. The nonsequential diffractive optics also provide further optimization for peak intermediate distance of 60 cm (range 40–80 cm), benefiting patients to perform tasks at an arm’s length [22].
To the best of the authors’ knowledge, this is the first meta-analysis study reporting pooled estimates for complete, far, intermediate, and near spectacle independence in patients undergoing cataract surgery with bilateral implantation of a trifocal IOL. While interpreting the results of this study, it is important to consider that this meta-analysis did not include any comparators, which is a limitation of this study. This was an “a priori” decision before commencing the meta-analysis as our systematic literature review revealed that the PanOptix IOL is the most studied trifocal IOL technology and the majority of evidence on comparator technologies was from single-arm studies, making it difficult to generate head-to-head (H2H) comparisons. With that in mind, there were only two clinical studies included in our meta-analysis that compared spectacle independence outcomes of trifocal IOLs H2H. Cochener and colleagues [14] conducted a comparative study among PanOptix and FineVision Micro F trifocal IOLs, with complete spectacle independence rates of 89% and 86%, respectively. The second study, by Ferreira et al. [16], provided complete spectacle independence rates among three different trifocal IOLs, including PanOptix, Synergy, and FineVision POD F, demonstrating that more than 96% of patients in all groups did not require the use of glasses after surgery. This study also highlights that no significant differences in the level of complete spectacle independence were detected among the different trifocal IOL groups [16]. With these limited data available, future clinical studies should focus on comparing spectacle independence outcomes between different trifocal IOL technologies and developing evidence for conducting a H2H meta-analysis.
Furthermore, outlier studies are important to consider while interpreting the pooled estimates. The study by Modi et al. [22] reported the lowest complete spectacle independence rate of 80.5%. This may be due to surgeon experience with the specific lens at the time of the study, given that this was a USFDA registration trial with a new IOL and surgeons were likely adapting to the new technology. A further study with low complete spectacle independence was conducted by Hovanesian et al. [19], a result that perhaps could be due to an inconsistent follow-up time of “at least 1 month,” which potentially may have led to some variability in the reported results.
Several factors contribute to the overall strength of the analysis. One of the major strengths of this review is the meta-analysis that includes 513 patients from across the world to estimate the pooled rate of complete spectacle independence. Though no single study can provide definitive estimates and understanding of an intervention, a systematic review and meta-analysis provides the best possible estimates for evidence-based medical practice. The ability of a meta-analysis to produce a single estimate based on several studies, accounting for heterogeneity and the quality of studies, places it on the top of the hierarchy of evidence [31].
Additionally, we used the Bayesian meta-analysis approach to generate pooled estimates. The Bayesian framework is an alternative framework to the frequentist approach for estimating parameters. The core concept of the Bayesian approach is to combine the likelihood (data) with our prior knowledge (prior distribution) using Bayes’ theorem, which results in an updated probability (posterior probability) to make the inference. Because of recent advanced computing methods, the Bayesian approach is becoming more common as it is intuitive and flexible.
This review also has some limitations. As previously mentioned, due to the paucity of comparative clinical evidence between PanOptix and other trifocal IOL technologies, we could not perform an H2H meta-analysis in this study. We propose that future analyses should focus on comparative outcomes once evidence from multiple prospective, controlled, good-quality clinical studies becomes available. Additionally, the statistical heterogeneity in this study across all meta-analyses is moderate to high (0.22–0.68), indicating diversity among the included studies. Firstly, there is variation in the participant characteristics (inclusion and exclusion criteria) and methods by which spectacle independence was measured across the studies. Some of the studies used validated questionnaires, while others reported use of nonvalidated questionnaires or did not report the method at all. Furthermore, the spectacle independence rates were derived from patient-reported outcome measures and were not objectively verified; however, we believe this approach is an appropriate method since patients themselves are best placed to report whether they are truly spectacle independent or not. Secondly, we included studies that reported spectacle independence rates at a post-cataract surgery follow-up of at least 1 month, which may be considered a short follow-up time; however, from clinical experience, patients’ visual outcomes are stable at 1 month post-surgery. Lastly, data from six studies included in this analysis were available only from congress presentations, making it difficult to fully evaluate the quality and bias of each study.
Conclusion
This meta-analysis of 13 unique clinical studies (513 patients) demonstrated that at least 9 out of 10 patients receiving TFNTXX/TFATXX trifocal IOL during cataract surgery can expect to achieve complete spectacle independence. Furthermore, spectacle independence among the subgroup analyses for far, intermediate, and near distances is at or above 90%; the highest spectacle independence is for intermediate vision (96.3%). The results from this review provide informative data for clinicians and patients to feel confident in selecting trifocal intraocular lens technology for presbyopia correction during cataract surgery as it offers high rates of complete spectacle independence.
Acknowledgements
Funding
Sponsorship for this study, and the journal’s Rapid Service Fee, were funded by Alcon Vision LLC, Fort Worth, Texas, USA.
Medical Writing and Editorial Assistance:
The authors would like to thank Radha Shukla, MBBS, PhD and Tushar Srivastava, MSc (ConnectHEOR) for managing and providing writing assistance towards the development of this manuscript. Support for this assistance was funded by Alcon.
Author Contributions
All authors contributed to the study conception and design. Material preparation and data collection were completed by Dagny Zhu, Kayla Mills, Jessie Hull, and Mukesh Dhariwal, and analysis was performed by Shijie Ren. The first draft of the manuscript was written by Radha Shukla and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Prior Presentation
This study was originally presented as a paper session at the 2022 American Society of Cataract and Refractive Surgery (ASCRS) congress, held April 2022 in Washington, D.C., USA.
Disclosures
Dagny Zhu has received consulting fees and honorarium for participation in advisory boards from Alcon and Johnson & Johnson, as well as a speaker honorarium from Alcon. ConnectHEOR received consulting fees from Alcon to conduct the study. Shijie Ren is an expert at ConnectHEOR. Kayla Mills (at the time of research), Jessie Hull and Mukesh Dhariwal are employees of Alcon. The authors report no other conflicts of interest related to this work.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Footnotes
Clear evidence that all reported results correspond to all intended outcomes, analyses, and subcohorts.
Evidence that shows some bias but not at high risk.
Evidence that clearly denotes bias and concerns within the study.
References
- 1.Freeman B. 2021 Premium Cataract Surgery Market Report. Market Scope. 2021.
- 2.Davidson RS, Dhaliwal D, Hamilton DR, et al. Surgical correction of presbyopia. J Cataract Refract Surg. 2016;42:920–930. doi: 10.1016/j.jcrs.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 3.Berdahl J, Bala C, Dhariwal M, et al. Patient and economic burden of presbyopia: a systematic literature review. Clin Ophthalmol. 2020;14:3439–3450. doi: 10.2147/OPTH.S269597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.U.S. Food and Drug Administration. Alcon Laboratories, Inc. AcrySof® IQ PanOptix® Trifocal Intraocular Lens (Model TFNT00) and AcrySof® IQ PanOptix® Toric Trifocal Intraocular Lens (Models TFNT30, TFNT40, TFNT50, TFNT60). https://public4.pagefreezer.com/content/FDA/28-01-2022T11:16/https://www.fda.gov/medical-devices/recently-approved-devices/alcon-laboratories-inc-acrysofr-iq-panoptixr-trifocal-intraocular-lens-model-tfnt00-and-acrysofr-iq. Accessed 29 May 2022.
- 5.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. doi: 10.1016/j.ijsu.2021.105906. [DOI] [PubMed] [Google Scholar]
- 6.Sterne JA, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. Bmj. 2019;366 :l4898. https://www.bmj.com/content/366/bmj.l4898 [DOI] [PubMed]
- 7.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. Bmj. 2016;355 :i4919. https://www.bmj.com/content/355/bmj.i4919 [DOI] [PMC free article] [PubMed]
- 8.Sutton AJ, Abrams KR. Bayesian methods in meta-analysis and evidence synthesis. Stat Methods Med Res. 2001;10(4):277–303. doi: 10.1177/096228020101000404. [DOI] [PubMed] [Google Scholar]
- 9.Sturtz S, Ligges U, Gelman A. R2WinBUGS: a package for running WinBUGS from R. J Stat Softw. 2005;12:1–16. doi: 10.18637/jss.v012.i03. [DOI] [Google Scholar]
- 10.Brooks SP, Gelman A. General methods for monitoring convergence of iterative simulations. J Comput Graph Stat. 1998;7(4):434–455. [Google Scholar]
- 11.Ang R, Villarrubia A, Palomino C, et al. Depth of focus, visual outcomes, and spectacle independence of a new diffractive presbyopia-correcting intraocular lens. Paper presented at: European Society of Cataract and Refractive Surgeons; October 2, 2020; Dublin, Ireland.
- 12.Blehm C, Potvin R. Reported patient satisfaction and spectacle independence following bilateral implantation of the PanOptix® trifocal intraocular lens. Clin Ophthalmol (Auckland, NZ) 2021;15:2907. doi: 10.2147/OPTH.S323337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chang J. Early clinical outcome of a trifocal intraocular lens in Asian eyes. Paper presented at: American Society of Cataract and Refractive Surgery; July 23, 2021; Las Vegas, Nevada, USA.
- 14.Cochener B, Boutillier G, Lamard M, et al. A comparative evaluation of a new generation of diffractive trifocal and extended depth of focus intraocular lenses. J Refract Surg. 2018;34(8):507–514. doi: 10.3928/1081597X-20180530-02. [DOI] [PubMed] [Google Scholar]
- 15.Espaillat A, Coelho C, Batista MJM, et al. Predictors of photic phenomena with a trifocal IOL. Clin Ophthalmol (Auckland, NZ) 2021;15:495. doi: 10.2147/OPTH.S282469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferreira T. Comparison of refractive and visual outcomes of three presbyopia-correcting intraocular lenses. Paper presented at: European Society of Cataract and Refractive Surgeons; October 8, 2021; Amsterdam, Netherlands.
- 17.García-Pérez JL, Gros-Otero J, Sánchez-Ramos C, et al. Short term visual outcomes of a new trifocal intraocular lens. BMC Ophthalmol. 2017;17(1):1–9. doi: 10.1186/s12886-017-0462-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hamdi IM. Subjective perception of trifocal IOL performance, including toric models. Clin Ophthalmol (Auckland, NZ) 2019;13:1955. doi: 10.2147/OPTH.S223062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hovanesian JA, Jones M, Allen Q. The PanOptix trifocal IOL vs the ReSTOR 2.5 active focus and ReSTOR 3.0-add multifocal lenses: a study of patient satisfaction, visual disturbances, and uncorrected visual performance. Clin Ophthalmol (Auckland, NZ) 2021;15:983. doi: 10.2147/OPTH.S285628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim MJ, Chung TY, Lee K, et al. Visual outcomes and safety after bilateral implantation of a trifocal presbyopia correcting intraocular lens in a Korean population: a prospective single-arm study. BMC Ophthalmol. 2020;20(1):1–11. doi: 10.1186/s12886-020-01549-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mencucci R, Favuzza E, Caporossi O, et al. Comparative analysis of visual outcomes, reading skills, contrast sensitivity, and patient satisfaction with two models of trifocal diffractive intraocular lenses and an extended range of vision intraocular lens. Graefes Arch Clin Exp Ophthalmol. 2018;256(10):1913–1922. doi: 10.1007/s00417-018-4052-3. [DOI] [PubMed] [Google Scholar]
- 22.Modi S, Lehmann R, Maxwell A, et al. Visual and patient-reported outcomes of a diffractive trifocal intraocular lens compared with those of a monofocal intraocular lens. Ophthalmology. 2021;128(2):197–207. doi: 10.1016/j.ophtha.2020.07.015. [DOI] [PubMed] [Google Scholar]
- 23.Modi S. A prospective, randomized comparison of bilaterally implanted extended depth of focus lenses and trifocal intraocular lenses. Paper presented at: American Society of Cataract and Refractive Surgery; July 23, 2021; Las Vegas, Nevada, USA.
- 24.Monaco G, Gari M, Di Censo F, et al. Visual performance after bilateral implantation of 2 new presbyopia-correcting intraocular lenses: trifocal versus extended range of vision. J Cataract Refract Surg. 2017;43(6):737–747. doi: 10.1016/j.jcrs.2017.03.037. [DOI] [PubMed] [Google Scholar]
- 25.Nattis A. Evaluation of visual outcomes and patient satisfaction with trifocal intraocular lens implantation. Presented at: American Society of Cataract and Refractive Surgery; July 23, 2021; Las Vegas, Nevada, USA.
- 26.Ramamurthy D, Vasavada A, Padmanabhan P, et al. Clinical outcomes after bilateral implantation of a trifocal presbyopia-correcting intraocular lens in an Indian population. Clin Ophthalmol (Auckland, NZ) 2021;15:213. doi: 10.2147/OPTH.S279001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shatz AC, Potvin R. Spectacle independence and quality of vision after bilateral implantation of a trifocal intraocular lens. Clin Ophthalmol (Auckland, NZ) 2021;15:2545. doi: 10.2147/OPTH.S318203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tran DB, Owyang A, Hwang J, et al. Visual acuity, quality of vision, and patient-reported outcomes after bilateral implantation with a trifocal or extended depth of focus intraocular lens. Clin Ophthalmol (Auckland, NZ) 2021;15:403. doi: 10.2147/OPTH.S295503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang G. A prospective, comparative study of the vison outcomes between a trifocal IOL and an extended depth of focus IOL among Chinese population. Presented at: Asia-Pacific Academy of Ophthalmology Congress; September 5, 2021; virtual congress.
- 30.Berdahl J, Bala C, Dhariwal M, et al. A cost-benefit analysis comparing trifocal intraocular lens (IOL) with monofocal IOL from patient perspective in the USA. Paper presented at: American Society of Cataract and Refractive Surgery; July 23, 2021; Las Vegas, Nevada, USA.
- 31.Haidich A-B. Meta-analysis in medical research. Hippokratia. 2010;14(Suppl 1):29. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.