Abstract
Since the summer of 2020, the rate of coronavirus cases in the United States has been higher in rural areas than in urban areas, raising concerns that patients with coronavirus disease 2019 (COVID-19) will overwhelm under-resourced rural hospitals. Using data from the University of Minnesota COVID-19 Hospitalization Tracking Project and the U.S. Department of Health and Human Services, we document disparities in COVID-19 hospitalization rates between rural and urban areas. We show that rural-urban differences in COVID-19 admission rates were minimal in the summer of 2020 but began to diverge in fall 2020. Rural areas had statistically higher hospitalization rates from September 2020 through early 2021, after which rural-urban admission rates re-converged. The insights in this article are relevant to policymakers as they consider the adequacy of hospital resources across rural and urban areas during the COVID-19 pandemic.
Keywords: COVID-19, hospitalizations, rural health, rural and urban disparities, hospital resources
Introduction
Since the novel 2019 coronavirus (COVID-19) was first detected in the United States in January 2020 (Holshue et al., 2020), total hospitalizations from COVID-19 infections have surpassed 1.8 million (University of Minnesota Carlson School of Management, 2020). Hospitalization surges during the pandemic have strained local health care systems, with hospitals reporting critical shortages of necessary infrastructure and supplies, including inpatient beds, intensive care unit (ICU) beds, medical devices, and clinical staff (Grimm, 2021; U.S. Food and Drug Administration, 2021; Wu et al., 2020). By October 2020, the majority of states had reported high occupancy for inpatient beds and ICU beds (Centers for Disease Control and Prevention, 2020; Karaca-Mandic et al., 2020; Trout & Chen, 2021), raising concerns that COVID-19 patients would not be able to access critical treatments due to capacity constraints. With the emergence of the Delta and Omicron variants, the issue of strained hospital capacity has continued prominence in the second and third years of the pandemic (Muller, 2022; Ungar & Meldrum, 2021).
The challenges of treating COVID-19 have been particularly acute in rural areas, which have faced high rates of COVID-19 cases (Linke, 2020; Paul et al., 2020). Rural areas have fewer health care resources than urban areas, including fewer ICU beds (Miller et al., 2020; Orgera et al., 2020) and a shortage of health care workers (Kaufman et al., 2020; Melvin et al., 2020). Moreover, rural areas have older and sicker populations that are at greater risk of hospitalization (Lakhani et al., 2020; Peters, 2020). These trends have raised concerns that rural health care systems will struggle to manage increased care burdens during the pandemic. However, rural hospitals entered the pandemic with more available beds per capita (Orgera et al., 2020) and lower occupancy rates (Hatten & Connerton, 1986) than urban hospitals, suggesting that rural areas may have more capacity to accommodate surges in COVID-19 hospitalizations.
Disparities in COVID-19 hospitalizations across rural and urban areas are not well understood. One barrier to research has been a lack of data on COVID-19 hospitalizations in rural and urban areas. The federal government did not begin reporting hospital-level hospitalization data until August 2020 (U.S. Department of Health & Human Services, 2022), seven months into the pandemic. Existing work on COVID-19 hospitalizations is generally based on state-level data (Gupta et al., 2021; Karaca-Mandic et al., 2021; Sen et al., 2020), which is too broad for analyzing rural versus urban disparities. To the best of our knowledge, there has been no analysis of rural versus urban trends in COVID-19 hospitalizations.
New Contributions
In this article, we provided the first evidence on disparities in COVID-19 hospitalization rates across rural and urban areas in the United States. We leveraged two unique datasets, quantifying the differential impacts of COVID-19 on rural and urban health care systems. Understanding rural-urban differences in COVID-19 burden is important because rural areas have fewer resources available to address the pandemic, including a limited health care workforce and financially strained hospitals (Lakhani et al., 2020; Peters, 2020). The results of our analyses are informative for policymakers as they consider the allocation of scarce hospital resources across rural and urban areas during the COVID-19 pandemic, as well as other public health events.
Method
Data
Our main analyses used two primary datasets. The first dataset came from the University of Minnesota (UMN) COVID-19 Hospitalization Tracking Project (University of Minnesota Carlson School of Management, 2020), which has collected COVID-19 hospitalization data from official state reporting agencies on a daily basis since the beginning of the pandemic. To the best of our knowledge, the UMN data is the only source of information about rural-urban hospitalization patterns at the beginning of the pandemic, during spring 2020. We focused on six states that have reported county-level COVID-19 hospitalizations since the pandemic’s early stage (spring 2020), allowing us to distinguish between rural and urban counties in each state. These states included Arizona, Florida, Georgia, Ohio, Utah, and Virginia. We used data on adult hospitalizations for COVID-19 from May 1, 2020, to July 1, 2021, aggregating the daily data to create a weekly panel of COVID-19 admissions.
The second dataset came from the Department of Health and Human Services (HHS) (U.S. Department of Health & Human Services, 2022), which has reported COVID-19 hospitalizations for every U.S. hospital on a weekly basis since August 7, 2020. We used data on confirmed, adult COVID-19 admissions through July 1, 2021, focusing on Short Term Hospitals and Critical Access Hospitals. We aggregated hospital-level data to the county level using Federal Information Processing System (FIPS) codes. Additional details of the data cleaning process and summary statistics of these two datasets are provided in the Supplementary Material.
We used designations from the Office of Management and Budget to categorize counties as urban or rural: Urban counties are in metropolitan areas (containing an urban core with at least 50,000 residents); rural counties are in micropolitan areas (containing an urban core with 10,000–50,000 residents) and noncore areas (Office of Management and Budget, 2021). In addition, we incorporated data on 2019 county-level demographics from the U.S. Census Bureau (2019), adult COVID-19 vaccination rates from the Centers for Disease Control and Prevention (2022), and the number of confirmed COVID-19 cases from the New York Times [NYT] (2022). Finally, we measured state-level policy responses to the pandemic compiled by Raifman et al. (2022), including stay-at-home orders, mask mandates, and restaurant closures. Data on county-level policy responses were not available.
Outcome Variables
We measured COVID-19 hospitalizations in each county by week. We calculated (a) the number of new COVID-19 admissions per week and (b) cumulative COVID-19 hospitalizations over time. The UMN data reported cumulative hospitalizations over time; we calculated new admissions in week t as cumulative hospitalizations in week t minus cumulative hospitalizations in week t−1. The HHS data reported weekly new admissions; we calculated cumulative hospitalizations in week t as the sum of the weekly new admissions between week 1 and week t.
To understand how the volume of COVID-19 hospitalizations was related to available hospital capacity, we normalized each hospitalization variable by the number of hospital beds in the county. As hospitals may add or reduce beds in response to surges in demand, we measured hospital beds using the time-varying number of staffed, adult inpatient beds reported weekly in the HHS data. Because the HHS data began August 7, 2020 (after the start of the UMN data), we used beds as of August 7, 2020 (the earliest available data) for all earlier time periods.
We also use local population in 2019 as a secondary normalization variable, modeling changes in per-capita hospitalizations (rather than hospitalizations per bed). A key difference between the two normalization variables is that hospital capacity could change over time, while local population was fixed at 2019 levels due to data availability.
Main Analysis
We used a multivariate linear regression model to assess the differential changes in COVID-19 hospitalization rates across rural and urban counties. We used the following estimating equation:
where measures hospitalization rates in county c in week t; is a binary variable that equals 1 if county c is rural and 0 otherwise; Weekt is an indicator of each week in the study period. Thus, measures the differential changes in hospitalization rates across rural and urban areas over time. is an error term. The regressions were weighted by county population, and the standard errors were clustered at the county level. We ran separate models using UMN data and HHS data and separate models that normalized hospitalizations by bed capacity and local population.
In addition to our county-level analyses, we studied differences in total occupancy rates across rural versus urban hospitals. The advantage of this analysis, relative to the county-level analysis, was that it compared hospital bed capacity to demand from all patients: COVID-19 and non-COVID-19 patients. That is, the county-level analysis assessed the COVID-19 hospitalization burden by rural/urban status, while the hospital-level analysis showed whether those COVID-19 hospitalization burdens pushed overall hospital occupancy to dangerous levels. Using hospital-level data from HHS, we computed weekly occupancy rates for each hospital as the number of occupied adult inpatient beds divided by the total number of staffed adult inpatient beds. We then measured differential occupancy rates across rural and urban hospitals, estimating a multivariate model analogous to the one above. In addition, we calculated the percent of rural and urban hospitals that reached 70% capacity, following Centers for Disease Control and Prevention (CDC) thresholds for high occupancy rates. All analyses were conducted using Stata version 16.0.
Supplementary Analyses
We conducted two types of sensitivity checks to assess the robustness of our results. First, we tested whether our results were sensitive to our choice of normalization variable. In our main analysis, we normalized COVID-19 hospitalizations by hospital bed capacity in each week—that is, time-varying bed capacity—as well as local population in 2019. In sensitivity checks, we re-ran our analyses using two alternative normalization variables. First, we normalized by time-invariant hospital bed capacity as of 2019 (Area Health Resources Files, 2020), immediately before the onset of the pandemic. Second, we normalized hospitalizations by confirmed COVID-19 cases in each week (NYT, 2022) to understand whether rural COVID-19 cases were more likely to result in hospitalization, on average.
Second, we assessed whether our results were sensitive to inclusion of controls in the regression model. In our main analysis, we did not include control variables so that the model would capture the absolute difference in hospitalization trends across rural and urban areas. In sensitivity analysis, we included control variables based on risk factors that have been identified in previous literature (Gomez et al., 2021; Karaca-Mandic et al., 2021): percent female, percent Hispanic, percent non-Hispanic Black, percent non-Hispanic white, percent 65 and older, percent of fully vaccinated adults, confirmed COVID-19 cases per 100,000 adults, and whether each state had implemented policy responses to the pandemic (including stay-at-home order, mask mandate, restaurant closure).
Results
Main Analyses
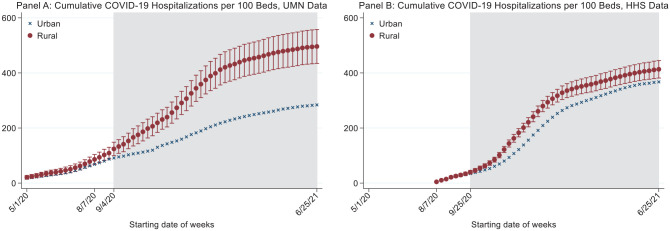
Our sample included 401 counties (44.4% rural) in the UMN data and 2,204 counties (59.8% rural) in the HHS data. Over the course of our study period, we observed approximately 230,000 COVID-19 hospitalizations in the UMN data (14.1% rural) and 1.9 million COVID-19 hospitalizations (11.4% rural) in the HHS data (Table A1). Figure 1 presents trends in new COVID-19 admissions per 100 beds in rural and urban areas, based on estimates from our regression model. Red circles show regression-adjusted hospitalization rates in rural areas. Blue x’s show regression-adjusted hospitalization rates in urban areas. Error bars report 95% confidence intervals on the difference in rural-urban rates (based on confidence intervals around alpha-hat from the estimating equation above). Full regression estimates are presented in Model 1 and Model 2 in Table A2.
Figure 1.
Trends in New COVID-19 Admissions Per 100 Beds in Rural Versus Urban Areas.
1. This figure shows regression-adjusted rates of new COVID-19 hospitalizations per 100 beds in rural and urban areas.
2. Red circles show adjusted hospitalization rates in rural areas. Blue x’s represent adjusted hospitalization rates for urban areas. Error bars report 95% confidence intervals on the difference between rural and urban hospitalization rates. Standard errors are clustered at the county level.
3. The shaded areas highlight the period during which the new admissions rates in rural areas were significantly higher than those in urban areas.
4. UMN data: data from University of Minnesota COVID-19 Hospitalization Tracking Project; HHS data: data from the Department of Health and Human Services.
In the UMN data (Figure 1, Panel A), new admissions were similar in rural and urban areas during the first wave of the pandemic (May to August 2020). In May 2020, there were two to three new COVID-19 admissions per 100 beds in both rural and urban areas, growing to 8.6 admissions per 100 beds in rural areas and 6.2 admissions per 100 beds in urban areas by mid-August 2020 (difference = 2.4, p-value = 0.36). Beginning in September 2020, however, rural and urban admission rates began to diverge. By late December 2020, rural areas had 19.3 new admissions per 100 beds; that is, COVID-19 new admissions accounted for nearly 20% of all hospital beds. Urban areas, in contrast, had 8.5 new admissions per 100 beds (rural-urban difference = 10.8; p-value < 0.01). Hospital admissions in rural areas slowed in late December 2020 and were statistically equivalent to urban hospitalization rates by early 2021.
The HHS data showed similar hospitalization patterns as the UMN data, although we could not observe the first wave in this sample (Figure 1, Panel B). Hospitalization patterns diverged in rural versus urban areas beginning in September 2020. Rural hospitalization rates peaked at approximately 20 new admissions per 100 beds in November and December 2020, similar to the pattern in the UMN data. Urban hospitalization rates, however, were higher in the HHS data than the UMN data, reaching 18.9 new admissions per 100 beds in late December. The high urban hospitalization rates in the HHS data (relative to the UMN data) were partially driven by states with large cities (including California, Illinois, New York, Pennsylvania, and Texas), which were not available in the UMN data. As shown in Figure A1, by the end of December 2020, the urban sample of these six states had a hospitalization rate of 23.8 per 100 beds, compared with 14.7 in the remaining urban sample excluding these six states (difference = 9.1; p-value < 0.01). Nevertheless, the HHS data showed a similar rural-urban hospitalization pattern to the UMN data: Rural hospitalization rates were significantly higher than urban hospitalization rates between September 2020 and January 2021. Rural-urban hospitalization rates then converged beginning in early 2021.
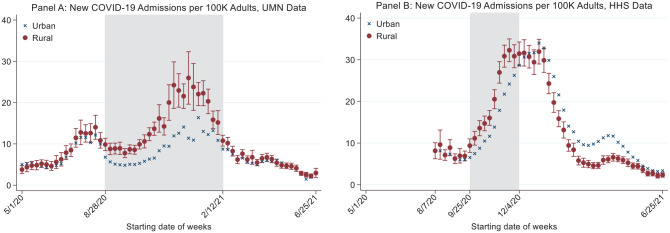
Figure 2 plots cumulative COVID-19 hospitalization rates over time. In Panel A, analysis of the UMN data showed that cumulative hospitalizations were largely similar in rural and urban areas during the first wave of the pandemic but began to diverge in fall 2020. The divergence began in early September, corresponding to the rural-urban divergence among new admissions (Figure 1). Cumulative hospitalizations in rural areas remained higher than in urban areas for the remainder of the study period, when rural areas had 496.2 cumulative hospitalizations per 100 beds, compared with 284.1 in their urban counterparts (difference = 212.1; p-value < 0.01). Thus, the UMN data showed that the total hospitalization burden from COVID-19 has been significantly higher in rural areas for the majority of the pandemic. Similar results were reached in our analysis of the HHS data (Figure 2, Panel B), though the rural-urban difference was smaller in magnitude (similar to Figure 1); cumulative hospitalizations in rural and urban areas diverged in the fall of 2020 and remained higher in rural areas for the remainder of the study period.
Figure 2.
Trends in Cumulative COVID-19 Hospitalizations in Rural Versus Urban Areas.
1. This figure shows regression-adjusted rates of cumulative COVID-19 hospitalizations per 100 beds in rural and urban areas.
2. Red circles show adjusted hospitalization rates in rural areas. Blue x’s represent adjusted hospitalization rates for urban areas. Error bars report 95% confidence intervals on the difference between rural and urban hospitalization rates. Standard errors are clustered at the county level.
3. The shaded areas highlight the period when the rural-urban differences in the cumulative admission rate are statistically significant.
4. UMN data: data from University of Minnesota COVID-19 Hospitalization Tracking Project; HHS data: data from the Department of Health and Human Services.
Figure 3 presents our results when we normalized COVID-19 hospitalizations by time-invariant adult population in 2019. In the UMN data, there were significantly higher hospitalization rates in rural areas relative to urban areas from fall 2020 to early 2021, followed by an equalization of hospitalization rates, as in our main results. In the HHS data, we found higher rural hospitalization rates in fall 2020, as in the main results, but estimated higher urban hospitalization rates in early 2021 (in contrast to the equal rural-urban rates in our main results). Since we normalized by time-varying bed capacity in the main analysis, these results suggest that urban hospitals were able to keep occupancy rates down by adding bed capacity during hospitalization surges. Indeed, we found that urban hospitals increased bed capacity by around 35% during the pandemic, while rural hospitals increased bed capacity by 15% (Figure A2).
Figure 3.
New COVID-19 Admissions Per 100k Adults in Rural Versus Urban Areas.
1. This figure shows regression-adjusted COVID-19 hospitalization rates per 100,000 adults in rural and urban areas.
2. Red circles represent adjusted hospitalization rates in rural areas. Blue x’s represent adjusted hospitalization rates in urban areas. Error bars report 95% confidence intervals on the difference in rural-urban hospitalization rates, with standard errors are clustered at the county level.
3. The shaded areas highlight the period during which the new admissions rates in rural areas were significantly higher than those in urban areas.
4. UMN data: data from University of Minnesota COVID-19 Hospitalization Tracking Project; HHS data: data from the Department of Health and Human Services.
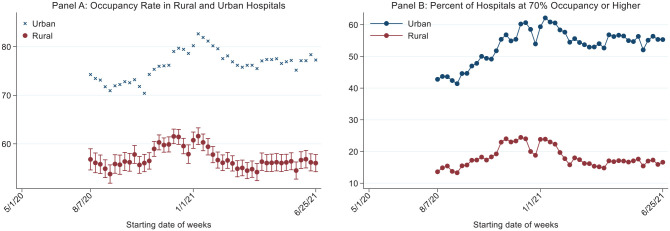
Next, we examined the overall occupancy rates (COVID-19 plus non-COVID-19) of rural versus urban hospitals during the COVID-19 pandemic (Figure 4). As discussed above, this analysis is distinct from the county-level analysis above because it assessed the total volume of hospitalizations, not only the volume of COVID-19 hospitalizations. We found that rural hospitals’ occupancy rates were consistently lower than those in urban hospitals (Figure 4, Panel A), despite having a higher relative burden of COVID-19 patients. In other words, rural hospitals had more COVID-19 patients per bed compared with urban hospitals but had fewer non–COVID-19 patients relative to the number of beds available. This finding is consistent with pre-pandemic hospital capacity: Rural hospitals tended to have large bed capacities relative to the demand for care, and therefore had lower occupancy rates going into the pandemic than urban hospitals (Hatten & Connerton, 1986; Orgera et al., 2020). The higher COVID-19 hospitalization burden in rural areas decreased this occupancy advantage in 2020 but did not offset it completely. Panel A of Figure 4 shows that occupancy rates were about 55% prior to fall 2020, rising to over 60% at the peak of the hospitalization surge. Urban hospitals, in contrast, began with an average occupancy rate of nearly 75%, which rose to over 80% during peak hospitalizations. Rural and urban hospital occupancy rates were closest in late October 2020. We find analogous results in Panel B of Figure 4, which plots the share of rural and urban hospitals at 70%+ occupancy, rather than the average occupancy rate.
Figure 4.
Trends in Occupancy Rates at Rural and Urban Hospitals.
1. Panel A shows the regression-adjusted occupancy rates at rural and urban hospitals. Occupancy is defined as the percent of beds occupied by COVID and non-COVID patients.
2. Panel B shows the unadjusted percent of rural and urban hospitals with at least 70% of beds occupied in each week.
3. Red circles show hospitalization rates in rural areas. Blue x’s represent hospitalization rates for urban areas. Error bars report 95% confidence intervals on the difference between rural and urban hospitalization rates. Standard errors are clustered at the county level.
4. This figure uses data from the Department of Health and Human Services.
Supplementary Analyses
In sensitivity checks, we assessed whether our results were sensitive to our choice of normalization variables: time-varying bed capacity in each week and local population in 2019. We assess two alternate normalization variables: time-invariant hospital bed capacity (based on pre-pandemic, 2019 levels) and confirmed COVID-19 cases in each county in each week. In Models 3 and 4 in Table A2, we present the results of normalizing hospitalizations using time-invariant hospital bed capacity. In the UMN data, there were significantly higher hospitalization rates in rural areas relative to urban areas from fall 2020 to early 2021, followed by an equalization of hospitalization rates, as in our main results. In the HHS data, we found higher rural hospitalization rates in fall 2020, as in the main results, but estimated higher urban hospitalization rates in early 2020 (similar to our results that normalized by time-invariant total population).
Figure A3 presents our results when we normalized hospitalizations by weekly confirmed COVID-19 cases. Analyses of the UMN data showed higher hospitalization rates per case in rural areas for the majority of the study period, consistent with rural residents having more risk factors for hospitalization on average. However, the HHS data showed little difference in hospitalizations per case across rural and urban areas.
In further sensitivity checks, we assessed whether our results were sensitive to including control variables (Table A2, Model 5 and Model 6). Overall, these models show similar results to our main model. We found higher rural hospitalization rates in the fall of 2020 in both datasets, with smaller rural-urban differences in other time periods.
Discussion
In this article, we used two unique datasets to assess COVID-19 hospitalization rates across rural and urban areas in the United States. Each dataset had its own advantage. The UMN data was the only source of information about rural-urban hospitalization patterns at the beginning of the pandemic, but it included only six states. The HHS data covered all hospitalizations nationally but did not contain information before August 2020. Analysis of both datasets led to similar conclusions: rural-urban differences in new COVID-19 admissions were minimal prior to fall 2020, at which point hospitalizations began to grow more quickly in rural areas. Both datasets showed statistically higher volumes of hospitalizations per bed in rural areas compared with urban areas between September 2020 and early 2021, after which the hospitalization rates in the two areas converged again. Our results were robust to a number of sensitivity checks that varied how we defined hospitalization rates (measuring hospitalizations per bed, per capita, and per confirmed case). Our conclusions were also robust to which variables we controlled for in the analysis.
Our results have several implications for policymakers as they respond to future COVID-19 variants and other public health emergencies that increase demands on the health care system. First, although COVID-19 hospitalization rates increased faster in rural areas than urban areas during the Delta variant wave, total occupancy rates at rural hospitals were consistently lower than those in urban areas; that is, rural hospitals had fewer non-COVID-19 hospitalizations relative to available beds, enabling them to accommodate surges in hospitalizations from a bed-capacity perspective. Separate from the COVID-19 pandemic, low occupancy rates at rural hospitals are typically considered a financial liability—empty hospital beds drive up the average cost of care. Policymakers have begun to emphasize downsizing rural hospitals, in part to help eliminate largely empty inpatient beds (Colyer et al., 2022). As rural hospital markets evolve, policymakers might consider how to promote pandemic/emergency readiness in rural areas that have reduced their health care infrastructure.
Importantly, while we found that rural hospitals had adequate bed capacity to accommodate COVID-19 hospitalizations, there are other reasons to be concerned about hospital resource shortages in rural areas during hospitalization surges. Rural areas have fewer clinicians per capita than urban areas, making it difficult to find replacement staff should a doctor or a nurse become ill. As such, increases in COVID-19 hospitalizations in rural areas may have strained clinician capacity, even when it did not strain overall bed capacity. A similar concern holds for the availability of ICU care, which requires specialized clinicians and is in short supply in rural areas (Charities Center for Rural Health, 2020). Moreover, rural hospitals tend to have fewer assets (Holmes et al., 2017), so it may have been difficult for rural hospitals to provide high-quality care for COVID-19 patients, which can require costly investments in protective equipment and other new medical supplies.
Second, we found evidence that urban hospitals were able to control occupancy rates by adding significant bed capacity during COVID-19 hospitalization surges, while rural hospitals had smaller increases in capacity. This pattern is consistent with lower resource levels at rural hospitals, which may impede efforts to respond to the increasing demand for COVID-19 care. However, our finding that the total occupancy rates for rural hospitals were lower than for urban hospitals suggests the possibility that additional capacity was not added at rural hospitals because it was not needed. Future work could provide more evidence on what types of hospitals added bed capacity during COVID-19 hospitalization surges, beyond the rural-urban distinction.
Third, we found similar rates of COVID-19 hospitalizations per confirmed COVID-19 case across rural and urban areas, suggesting that the increased hospitalization burden in rural areas was due to the higher number of underlying cases. Policymakers might, therefore, emphasize policies that aim to lower case rates. One example is increasing COVID-19 vaccination rates, which were lower in rural areas compared with urban areas during the study period and can result in lower levels of immunity and increased cases. Relatedly, many states addressed COVID-19 surges with statewide policies, failing to take rural areas’ specific needs and preferences into account (Ajilore, 2020). Such one-size fits all policy responses could have contributed faster and broader spread of the disease in rural areas (Callaghan et al., 2021).
Our study has several limitations. First, the UMN data only included six states, limiting our ability to study patterns in COVID-19 hospitalizations early in the pandemic; however, to the best of our knowledge, the UMN data represent the most extensive coverage of hospitalizations prior to August 2020. Second, we compared rural versus urban hospitalizations overall, which may mask important heterogeneity within each group. In particular, there may be important differences in hospitalization patterns and available resources in micropolitan rural areas (which have some proximity to urban centers) versus isolated rural areas. Future work could usefully disentangle rural COVID-19 hospitalization patterns along this dimension. Third, there may be measurement error in our hospitalization variable. In the UMN data, states varied in their definition of COVID-19 hospitalizations, with some states reporting confirmed hospitalizations and others reporting suspected COVID-19 hospitalizations; thus, the UMN data may overestimate the number of true COVID-19 hospitalizations in some states. In the HHS data, hospital-week data were suppressed if it was based on fewer than four hospitalizations, and therefore not counted toward the county aggregation. As such, the analyses with the HHS data may represent an underestimate of COVID-19 hospitalizations relative to the UMN data.
To our knowledge, this study is the first to quantify the COVID-19 hospitalization burden across rural and urban areas. As policymakers debate how to address the COVID-19 pandemic, our analysis provides important insights into the allocation of hospital resources. A major risk of COVID-19 surges is that demand for care will exceed the capacity of the health care system. Our findings are relevant for understanding what resources are needed and where, and for ensuring adequate hospital capacity as state and local governments move to loosen COVID-19 restrictions.
Supplemental Material
Supplemental material, sj-docx-1-mcr-10.1177_10775587221111105 for COVID-19 Hospitalization Trends in Rural Versus Urban Areas in the United States by Yi Zhu, Caitlin Carroll, Khoa Vu, Soumya Sen, Archelle Georgiou and Pinar Karaca-Mandic in Medical Care Research and Review
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Karaca-Mandic reports funding from the University of Minnesota, Office of Academic Clinical Affairs, and grants from United Health Foundation during this project. In the past 36 months, she also reports personal fees from Tactile Medical, personal fees from Precision Health Economics, personal fees from Sempre Health, grants from the Agency for Healthcare Research and Quality, grants from the American Cancer Society, grants from National Institute for Health Care Management, grants from National Institute on Drug Abuse, and grants from National Institutes of Health, all outside of the context of this manuscript. Dr. Karaca Mandic also serves in an executive position and holds equity in XanthosHealth LLC, which is developing a health information technology in oncology. These interests have been reviewed and managed by the University of Minnesota in accordance with its Conflict of Interest policies. Dr. Georgiou reports personal fees from HealthGrades outside the submitted work.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Yi Zhu  https://orcid.org/0000-0002-5748-6940
https://orcid.org/0000-0002-5748-6940
Caitlin Carroll  https://orcid.org/0000-0002-3759-5920
https://orcid.org/0000-0002-3759-5920
Data Accessibility: This research uses data from the University of Minnesota COVID-19 Hospitalization Project, which is partially funded by the University of Minnesota Office of Academic Clinical Affairs and the United Health Foundation. These organizations had no role in data collection or the conduct of this study and have not reviewed or approved the manuscript. Data used in this research are available by contacting the project team. This research also uses publicly available data on COVID-19 hospitalizations from the U.S. Department of Health and Human Services (HHS), which is downloadable from the HHS website. The University of Minnesota Institutional Review Board reviewed the study data and exempted it from review because it did not constitute human subject research.
Supplemental Material: Supplemental material for this article is available online.
References
- Ajilore O. (2020). Rural America has been forgotten during the coronavirus crisis—Center for American Progress. https://www.americanprogress.org/article/rural-america-forgotten-coronavirus-crisis/
- Area Health Resources Files. (2020). Health resources & services administration. https://data.hrsa.gov/topics/health-workforce/ahrf
- Callaghan T., Lueck J. A., Trujillo K. L., Ferdinand A. O. (2021). Rural and urban differences in COVID-19 prevention behaviors. The Journal of Rural Health, 37(2), 287–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020). COVID-19 data dashboard —patient impact & hospital capacity. Centers for Disease Control and Prevention. https://www.cdc.gov/nhsn/covid19/report-patient-impact.html [Google Scholar]
- Centers for Disease Control and Prevention. (2022). COVID-19 vaccinations in the United States. https://data.cdc.gov/Vaccinations/COVID-19-Vaccinations-in-the-United-States-County/8xkx-amqh
- Charities Center for Rural Health. (2020). The rural health safety net under pressure: Rural hospital vulnerability. https://www.chartis.com/forum/insight/the-rural-health-safety-net-under-pressure-rural-hospital-vulnerability/
- Colyer J., Barnett S., Bruffett K. M., Deschambeau W. G., Dodge M., Grant-Nierman M., Holmes G. M., Lupica J., Mills M. A., Myers B., Phillips K. M., Schou P., Wergin R. L., Werth J., Wilson L. (2022). Rural emergency hospital policy brief. https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/rural/publications/2021-rural-emergency-hospital-policy-brief.pdf
- Gomez J. M. D., Du-Fay-de-Lavallaz J. M., Fugar S., Sarau A., Simmons J. A., Clark B., Sanghani R. M., Aggarwal N. T., Williams K. A., Doukky R., Volgman A. S. (2021). Sex differences in COVID-19 hospitalization and mortality. Journal of Women’s Health, 30(5), 646–653. [DOI] [PubMed] [Google Scholar]
- Grimm C. A. (2021). Hospitals reported that the COVID-19 pandemic has significantly strained health care delivery (p. 62). https://oig.hhs.gov/oei/reports/OEI-09-21-00140.pdf
- Gupta S., Georgiou A., Sen S., Simon K., Karaca-Mandic P. (2021). US trends in COVID-19–associated hospitalization and mortality rates before and after reopening economies. JAMA Health Forum, 2(6), e211262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatten J. M., Connerton R. E. (1986). Urban and rural hospitals: How do they differ? Health Care Financing Review, 8(2), 77–85. [PMC free article] [PubMed] [Google Scholar]
- Holmes G. M., Kaufman B. G., Pink G. H. (2017). Predicting financial distress and closure in rural hospitals. The Journal of Rural Health, 33(3), 239–249. [DOI] [PubMed] [Google Scholar]
- Holshue M. L., DeBolt C., Lindquist S., Lofy K. H., Wiesman J., Bruce H., Spitters C., Ericson K., Wilkerson S., Tural A., Diaz G., Cohn A., Fox L., Patel A., Gerber S. I., Kim L., Tong S., Lu X., Lindstrom S., Pallansch M. A., . . . Washington State 2019-nCoV Case Investigation Team. (2020). First case of 2019 novel coronavirus in the United States. New England Journal of Medicine, 382(10), 929–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karaca-Mandic P., Georgiou A., Sen S. (2021). Assessment of COVID-19 hospitalizations by race/ethnicity in 12 states. JAMA Internal Medicine, 181(1), 131–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karaca-Mandic P., Sen S., Georgiou A., Zhu Y., Basu A. (2020). Association of COVID-19-related hospital use and overall COVID-19 mortality in the USA. Journal of General Internal Medicine. Advance online publication. 10.1007/s11606-020-06084-7 [DOI] [PMC free article] [PubMed]
- Kaufman B. G., Whitaker R., Pink G., Holmes G. M. (2020). Half of rural residents at high risk of serious illness due to COVID-19, creating stress on rural hospitals. The Journal of Rural Health, 36(4), 584–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakhani H. V., Pillai S. S., Zehra M., Sharma I., Sodhi K. (2020). Systematic review of clinical insights into novel coronavirus (CoVID-19) pandemic: Persisting challenges in U.S. rural population. International Journal of Environmental Research and Public Health, 17(12), 4279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linke M. (2020). Coronavirus is spreading faster in rural communities with aging populations. The Wall Street Journal. https://www.wsj.com/articles/coronavirus-is-spreading-faster-in-rural-communities-with-aging-populations-11589601660
- Office of Management and Budget. (2021, July16). 2020 standards for delineating core based statistical areas. Federal Register. https://www.federalregister.gov/documents/2021/07/16/2021-15159/2020-standards-for-delineating-core-based-statistical-areas
- Melvin S. C., Wiggins C., Burse N., Thompson E., Monger M. (2020). The role of public health in COVID-19 emergency response efforts from a rural health perspective. Preventing Chronic Disease, 17, E70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller I. F., Becker A. D., Grenfell B. T., Metcalf C. J. E. (2020). Disease and healthcare burden of COVID-19 in the United States. Nature Medicine, 26(8), 1212–1217. [DOI] [PubMed] [Google Scholar]
- Muller M. (2022). BA.2 variant spreading in U.S., CDC says, especially in New York, Northeast. Bloomberg. https://www.bloomberg.com/news/articles/2022-03-22/omicron-subvariant-takes-hold-in-u-s-as-new-york-cases-tick-up
- The New York Times. (2022). Coronavirus (Covid-19) data in the United States. https://github.com/nytimes/covid-19-data
- Orgera K., McDermott D., Rae M., Claxton G., Koma W., Cox C. (2020). Urban and rural differences in coronavirus pandemic preparedness. Peterson-KFF Health System Tracker. https://www.healthsystemtracker.org/brief/urban-and-rural-differences-in-coronavirus-pandemic-preparedness/
- Paul R., Arif A. A., Adeyemi O., Ghosh S., Han D. (2020). Progression of COVID-19 from urban to rural areas in the United States: A spatiotemporal analysis of prevalence rates. The Journal of Rural Health, 36(4), 591–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters D. J. (2020). Community susceptibility and resiliency to COVID-19 across the rural-urban continuum in the United States. The Journal of Rural Health, 36(3), 446–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raifman J., Bor J., Dean L. T., Jay J., Jones D. K., Lipson S. K., Brahim M. C. (2022). COVID-19 US state policies. Data Library—CUSP. https://statepolicies.com/data/library/
- Sen S., Karaca-Mandic P., Georgiou A. (2020). Association of stay-at-home orders with COVID-19 hospitalizations in 4 states. Journal of the American Medical Association, 323(24), 2522–2524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trout K. E., Chen L.-W. (2021). Geographic distribution of bed occupancy during the COVID-19 epidemic in the United States: A nationwide study. Health Science Reports, 4(2), e315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ungar L., Meldrum A. (2021, December6). Omicron v. delta: Battle of coronavirus mutants is critical. AP NEWS. https://apnews.com/article/coronavirus-pandemic-science-health-southern-africa-pandemics-2a445501cff8d0354fabcf493418365e
- University of Minnesota Carlson School of Management. (2020). COVID-19 hospitalization tracking project. https://carlsonschool.umn.edu/mili-misrc-covid19-tracking-project
- U.S. Census Bureau. (2019). County population by characteristics: 2010-2019. Census.gov. https://www.census.gov/data/tables/time-series/demo/popest/2010s-counties-detail.html
- U.S. Department of Health & Human Services. (2022). COVID-19 reported patient impact and hospital capacity by facility. HealthData.gov. https://healthdata.gov/Hospital/COVID-19-Reported-Patient-Impact-and-Hospital-Capa/anag-cw7u
- U.S. Food and Drug Administration. (2021, September10). Medical device shortages during the COVID-19 public health emergency. fda.gov. https://www.fda.gov/medical-devices/coronavirus-covid-19-and-medical-devices/medical-device-shortages-during-covid-19-public-health-emergency
- Wu H., Soe M. M., Konnor R., Dantes R., Haass K., Dudeck M. A., Gross C., Leaptrot D., Sapiano M. R. P., Allen-Bridson K., Wattenmaker L., Peterson K., Lemoine K., Tejedor S. C., Edwards J. R., Pollock D., Benin A. L., & National Healthcare Safety Network. (2020). Hospital capacities and shortages of healthcare resources among US hospitals during the coronavirus disease 2019 (COVID-19) pandemic, National Healthcare Safety Network (NHSN), March 27–July 14, 2020. Infection Control & Hospital Epidemiology. Advance online publication. 10.1017/ice.2021.280 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-mcr-10.1177_10775587221111105 for COVID-19 Hospitalization Trends in Rural Versus Urban Areas in the United States by Yi Zhu, Caitlin Carroll, Khoa Vu, Soumya Sen, Archelle Georgiou and Pinar Karaca-Mandic in Medical Care Research and Review