Abstract
Acute pancreatitis (AP) and chronic pancreatitis are the third leading gastrointestinal causes for admissions and readmissions to hospitals in the United States. This review of articles published between 2019-2022 (December) from international sources identified four categories of crucial new findings: The report includes (1) New genetic pathogenic mutations (TRPV6); expected genetic outcomes in a Northern European population; (2) a new serum diagnostic marker for AP-fatty acid ethyl esters-distinguishing acute pancreatitis associated with alcohol; explanations of the impact of monocytes/macrophages on the inflammatory process that defines their future in diagnosis, staging, and treatment; (3) innovations in timing of per os low-fat, solid food intake immediately on admission; resolution of concepts of aggressive parenteral fluid intake; dramatic shifts to non-operative from operative treatment of infected pancreatic necrosis. Each modification reduced interventions, complications, and lengths-of-stay; and (4) authoritarian recommendations for medical treatment of chronic pain. These advances offer opportunities to initiate newly proven treatments to enhance outcomes, alter the natural history, and envision the future of two diseases that have no known cure.
Keywords: Genetics, New diagnostics, Macrophage regulation, New approaches to early feeding, Fluid management
Core Tip: Acute and chronic pancreatitis are leading causes for admissions to hospitals. This review identified four categories of crucial new findings including: (1) New genetic mutations (TRPV6); expected genetic outcomes; (2) new serum diagnostic markers-distinguishing pancreatitis associated with alcohol, and defining the impact of monocytes/macrophages on the inflammatory process; (3) critical innovations: In timing of PO low-fat, solid food intake immediately on admission; resolved concepts on fluid intake; non-operative treatment of infected necrosis; and (4) authoritarian recommendations for treatment of chronic pain. These advances offer opportunities to initiate newly-proven treatments to enhance outcomes and alter the natural history.
INTRODUCTION
Acute pancreatitis (AP) and chronic pancreatitis (CP) are two of the most common causes for gastrointestinal-related office visits and admissions to hospital[1-3]. AP and CP are multifactorial diseases in which the former may progress to the latter as chronic inflammation and autodigestion lead to fibrosis and atrophy. Information that improves understanding of the diseases is critical to advancing therapy. The objective of this review was to identify pivotal studies that directly impart usable information relative to pathophysiology, diagnosis, preventative and other treatments.
METHODS
The information in this review was obtained between 2019 through December 2022 from PubMed, Ovid, International Guidelines, expert opinion, and personal contact with experts. We looked specifically for well-designed, randomized, controlled original research, systematic reviews, meta-analyses, expert guidelines, and professional association guidelines addressing changes favorably affecting outcomes. Case reports, case series and others considered irrelevant to the study were excluded as were most articles outside the inclusive dates, although some were included for supporting information. Over 400 articles were reviewed for possible relevance, with primary selections based on new information considered important and usable for health care workers.
OBSERVATIONS AND DISCUSSION
Pathophysiology: Genetic risks and clinical characterization
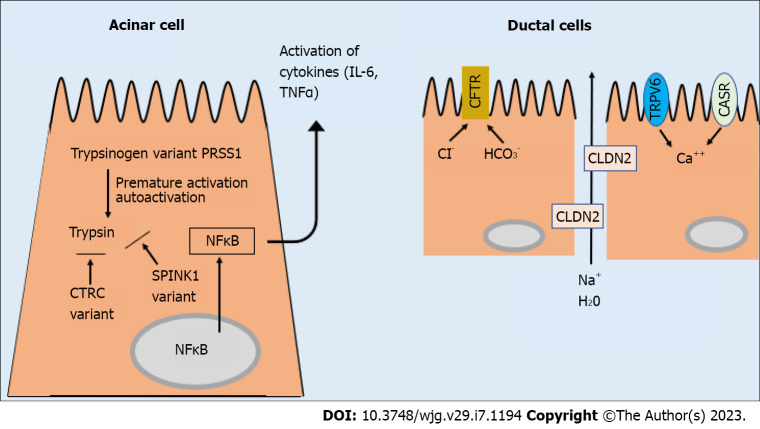
The landmark discovery of mutations in the pancreatic digestive genes coding for trypsinogen (PRSS1 and PRSS2[4] catalyzed a search for additional pathologic variants in pancreatic digestive genes. The search has been rewarded with the discovery of a sufficient number of genetic variants to permit a mechanistic classification suggesting their pathogenic effect[5-7]. These include genetic variants in: (1) The trypsin-dependent pathway, including PRSS1, PRSS2, SPINK1, and chymotrypsin C (CTRC) genes; (2) the ductal physiology pathway including the cystic fibrosis transmembrane conductance receptor (CFTR), claudin 2 (CLDN2), possibly the calcium sensing receptor (CASR); proposed, and offered on many testing panels, but still controversial), plus newly discovered variants in the calcium channel coding genes (TRPV6, not yet on most testing panels)[8]; and (3) the misfolding-dependent pathway including a distinct subset of PRSS1 variants, carboxypeptidase A1 (CPA1), and rare variants of carboxyl ester lipase (CEL) (Figure 1). The TRPV6 variants are important new additions to the ductal-pathway genes, which alter calcium concentration in ductal fluid. The TRPV6 variant is identified in 4.3% of nonalcoholic CP patients in Japan and 2.0% in Europe, indicating a substantial global risk gene for CP. Most of the carriers were heterozygous for the variant, implicating the potent pathogenic effect of certain TRVP6 variants (i.e., haploinsufficiency). Furthermore, 20% with defective TRPV6 variants were transheterozygous for SPINK1 variants, an unusually high association[8,9]. More than half of the TRPV6 variants cause subtle functional defects with loss-of-function for removing calcium from the ductal fluid, leading to increased ductal calcium concentrations. This discovery offers a possible novel target for therapeutic intervention since TRPV6 expression is regulated by 1-alpha,25-dihydroxyvitamin D3, and partial correction of TRPV6 dysfunction in heterozygous carriers might be feasible with vitamin D supplements[9]. Collateral laboratory studies demonstrate that much of the injury in acute and chronic pancreatitis evolves from alterations of acinar and ductal digestive function by these pancreatitis-susceptibility mutants, culminating in disruption of the protease-antiprotease interaction in the serine protease trypsinogen pathway within pancreatic acinar and ductal cells[5-9].
Figure 1.
Diagrammatic depiction of fundamental events contributing to the complex molecular pathways resulting in pancreatitis. Although a unifying concept is not available for all events, recent literature has provided a clearer description of the complexity of pathologic events which is briefly summarized. A proposed first step is injury to cytoplasmic organelles from external stressors, including prolonged, high intake of ethanol and smoking. These injuries result in endoplasmic reticulum stress, mitochondrial depolarization, inadequate ATP production, vacuole accumulation, protein misfolding, and disordered autophagy leading to activation of trypsinogen and inflammatory pathways. Disruption of the normal pathways may be augmented by genetic mutations at key functional sites responsible for trypsinogen activation, trypsin inhibition, Ca++ concentrations, and HCO3- and H2O movement[4-9,20,21]. CTRC: Chymotrypsin C; CFTR: Cystic fibrosis transmembrane conductance receptor; NF-Κb: Noncanonical nuclear factor-kappaB; TNF-α: Tumour necrosis factor alpha; IL: Interleukin.
Recent studies by Lewis et al[10] provide clinical characterization of genetic risks for CP in a North American population of European ancestry. Patients with early-onset (< 35 years) idiopathic CP and no alcohol exposure had significantly more pathogenic variants in 49% of cases compared to no more than 26% in those with late-onset idiopathic CP or CP associated with light-to-moderate or heavy-to-very heavy drinking. Likewise, the early-onset group was significantly more likely to have pathogenic variants in SPINK1 (24%) or CFTR (36%) than patients with late-onset idiopathic CP (9% and 15%) or CP associated with light-to-moderate drinking (7% and 19%) or heavy-to-very heavy drinking (9% and 13%). Evidence supporting pathogenicity of the mutants included a younger age of onset of symptoms in which the SPINK1 mutation decreased the age at onset to 12 years from 24 years in early-onset idiopathic CP (P = 0.004) and to 24 years from 50 years in the light-to-moderate drinkers (P < 0.001). The CFTR mutation dropped the age at onset to 41 years from 50 years in the light-to-moderate drinkers (P = 0.030). Sixty-one cases of early-onset ICP were characterized by persons with an average age of 20 years, incessant pain, pancreatic calcifications, and genetic variants in the SPINK1, CTRC, or CFTR genes in almost half the cases. These collective findings reclassified as many as 23%-49% of cases of ICP to those with potential genetic causes.
CFTR was the most common gene with pathogenic variants in 13%-36%. It is important to recognize that interactions between incompletely penetrant genetic variants-including several working synergistically (i.e., epistasis) and a pronounced exposure to alcohol, smoking, or other toxins are frequently involved in the final pathways leading to acute and chronic pancreatitis. More often than not, multiple factors are responsible. The pathologic progression then gradually leads to well-recognized complications of chronic inflammation with fibrosis, ductular calcifications, pain, steatorrhea, insulin insufficiency, fluid collections, disability, and premature death.
Along with appropriate counseling, testing for the six (or seven including the newly described TRPV6 variants) commercially evaluable genetic causes of acute and chronic pancreatitis is recommended in cases that have age of onset < 35 years, relapsing pancreatitis, or are idiopathic. The results offer valuable information regarding diagnostic probability of a genetic predisposition, a prediction as to probable cofactors, how to initiate available treatment as early in the process as possible, and do not require repetitive testing. Persons who have extensive comorbidities or are elderly may not benefit from genetic investigation.
Acute pancreatitis: New tools for diagnosis
AP, a disease with a variety of etiologies and risk factors is diagnosed by blood levels of amylase and lipase, abdominal pain, and imaging abnormalities of the pancreas[11-13]. A new diagnostic test has produced intriguing results. Vela and colleagues conducted a prospective, blinded trial comparing blood levels of fatty acid ethyl esters (FAEEs), nonesterified fatty acids, and ethanol in 175 patients at the time of hospitalization with alcoholic pancreatitis, alcoholic intoxication, nonalcoholic pancreatitis, and normal controls[14]. Distinguishing differences were that median FAEEs were similarly elevated in alcoholic pancreatitis (103 nmol/L) and alcoholic intoxication (205 nmol/L), whereas there was no significant elevation in nonalcoholic causes of AP (8 nmol/L) or controls (1.7 nmol/L). By its unique ability to demonstrate diagnostic elevations of FAEEs in association with alcohol intake, this test could become an efficient tool for identifying alcohol as the cause in alcohol-associated pancreatitis when present and eliminating alcohol as the culprit when caused by other factors. That alcohol intoxication without AP raises the level of FAEEs is explained by a well-known effect of excessive ethanol ingestion on cell membranes. The study did not distinguish between AP and alcohol-induced AP superimposed on CP, although the latter would be suspected in most of the latter cases.
In a similar vein, Manohar et al[15] have presented data defining the complex role of immune responses in monocytes and macrophages using single-cell mass Cytometry by Time Of Flight in two experimental models and in patients with acute, recurrent, and severe AP. As inflammatory cells determine disease severity and pancreatic damage is increased by tissue-derived neutrophils, macrophages are the predominant immune cell in the early phases of AP. Their report explains the role of the immune response in AP, provides insight toward the biological significance of novel Ly6Gc+/CD206+ monocytes and macrophages, and shows how these cellular components may be used to diagnose AP, define its severity, and target potential treatment[15,16].
Chronic pancreatitis: Alcohol and smoking
CP is diagnosed by imaging scans showing glandular atrophy, ductal distortion, and calcifications, or by biopsy demonstrating widespread fibrosis, and is, like AP, characterized by a variety of similar etiologies and risk factors, excepting gallstones and medications[2,3,13]. The relationship of ethanol and smoking to CP is indisputable. Both the amount and duration of exposure matter, and the exposures may vary with time and gender. A contemporary analysis of daily ethanol consumption in persons with alcoholic CP revealed a median of 5.1 drinks/d, in which 12.0 g/drink = 61.5 g/d of ethanol[17]. Consumption of up to 110-277 g/d over 5-25 years may transpire by the time of diagnosis of alcoholic CP[2,3,17-19]. A lower intake of < 50 g/d is implicated where the disease progresses more slowly, and persons are older at the time of diagnosis with less pain and fewer complications[10]. Evidence substantiating the role of ethanol and tobacco intake in perpetuating the fibro-inflammatory phase is exemplified by unabated progression even if ethanol and tobacco intake are discontinued, although at a slower pace when compared with continued usage of both[2,3,10], implicating ethanol and tobacco activating subclinical pancreatic stellate cell fibrosis for years before becoming clinically apparent[19-21].
Recently, models ranging from necroptosis to pyroptosis show how a pathogenic metabolic pathway can provoke inflammation, often initiated by premature intrapancreatic activation of trypsinogen, and be perpetuated by synergy between genetic, epigenetic, immune and environmental factors[5-9] as clinical and post-mortem studies of chronic alcoholics without a sentinel AP event show pathologically recognizable CP in the form of fibrosis and/or ductal calcifications in 47%-68%, indicating extensive damage present before diagnosis[19,22,23].
NEW TREATMENTS
Early feedings in acute pancreatitis
Initiating early feeding per os or via nasogastric/nasojejunal routes beginning after the onset of AP is supported by multiple randomized controlled trials and has replaced prior practices of resting the gastrointestinal tract until pain subsides. This approach increases bowel motility and reduces rates of organ failure, infection, length of stay and mortality, substantiating the suspicion that an idle intestine leads to bacterial overgrowth, increased permeability and bacterial translocation[2,3,11,24]. Questions regarding preferred timing had remained but new results from a randomized controlled trial of 131 patients with mild-moderate AP provide clarity. The study compared those fed a low-fat, solid diet immediately upon decision for admission, regardless of symptoms or laboratory parameters, to those receiving conventional feeding with progressive diet as clinical and laboratory parameters improved. The results indicate that immediate feeding is safe and feasible with significantly decreased complications (4.2% vs 18.3%) and shorter length of stay (3.4 d vs 8.8 d) at one-half the costs[25].
Fluid resuscitation in acute pancreatitis
A major question addressing the appropriateness of early, aggressive hydration was just answered in an important multicenter, randomized, controlled trial from India, Italy, Mexico, and Spain that assessed the efficacy and safety of aggressive fluid resuscitation as compared with moderate resuscitation using lactated Ringer’s solution in patients with AP; patients with moderate to severe disease or heart failure at baseline were excluded[26]. The primary outcome was the development of moderately severe or severe acute pancreatitis and secondary outcomes included organ failure and local complications occurring after randomization and during the hospitalization. The aggressive-group received a bolus of 20 mL/kg body weight over 2 h, followed by an infusion rate of 3 mL/kg/h, and the moderate-group a dose of 1.5 mL/kg/h, with a bolus of 10 mL/kg/h if hypovolemic. Oral feeding was started at 12 h if the intensity of abdominal pain permitted. The first interim analysis included 249 of the planned sample size of 744 patients and uncovered significant fluid overload in the aggressive-resuscitation group at 20.5% vs 6.3% (P = 0.004), and the trial was stopped[26]. Significant differences were not reached for the primary or secondary endpoints, although the results tended to favor the moderate resuscitation group. An editorial analysis concluded that the trial results were stunning and irrefutable and that clinicians should follow an infusion rate of the moderate group with careful monitoring of volemic status, adding fluid if underhydrated or diuresis if overhydrated[27].
Pancreatic fluid collections
New data have created a decisive shift in treatment of infected necrotizing pancreatitis, in which antibiotics without drainage are replacing the long-held concept of antibiotics and immediate drainage of infection developing after AP[28]. The crucial substantiation came from a randomized, superiority trial in the Netherlands that compared immediate drainage of infected necrotizing pancreatitis vs postponement of drainage in patients with infected tissue occurring within 35 d from onset of initial symptoms of AP. Infection was documented by gram stain, culture, or clinical deterioration and both groups received antibiotics. The Dutch study enrolled 104 qualifying patients; complications and mortality were similar for both groups. However, the mean number of interventions was 4.4 for the immediately drained group compared to only 2.6 (40% less) for the deferred group; 37% (19/52) of patients in the deferred group did not require drainage, and the number of hospital days was shorter by 15% (51 d vs 59 d). The rationale for the study had been supported by retrospective studies that showed apparent safety in postponing intervention with drainage, although none have demonstrated superiority[28-30].
Current concepts for pain management in chronic pancreatitis
Pain affects most persons with CP and is the most significant obstacle to successful treatment.
Pain is the major cause of morbidity, disability, and impaired quality of life. Pain syndromes are complex, widely variable and range from severe and chronic to absent[31,32]. An up-to-date study of pain patterns in 1131 persons in 30 Dutch hospitals revealed continuous pain in 52%, intermittent pain in 20%, and no pain in 28%[33]. Patients with continuous pattern had more severe pain, used more opioids and neuropathic medications, and had lower quality of life.
Current concepts emphasize that pain may arise from origins other than the pancreas. Persistent, severe pain can transfer centrally in association with cerebral cortical thinning, central sensitization, central pain processing, or other neuropathology, and becomes less likely to respond to conventional measures. Pancreatic quantitative sensory testing that interrogates nociception and sensory response could help unmask irreversible central neuropathic changes that make interventional treatment of pancreatic pain less likely to be successful. During the course of disease, pain severity may increase or decrease as disease progresses over 10-25 years[31-33]. The initial treatment of choice for those who drink and/or smoke is complete abstinence to reduce the pain, prevent further episodes of AP, forestall progressive damage to the pancreas and lessen cancer risk to the pancreas and other organs[2,3,18,19,28-32]. Early diagnosis of the cause represents the first chance to initiate treatment to retard the progress of a disease that no one can cure. In cases of mild or intermittent pain, non-narcotic oral analgesics including NSAIDS, acetaminophen, tricyclic antidepressants, mirtazapine, and cognitive behavioral therapy may be helpful. Treatment with antioxidants may produce a small improvement, but pancreatic enzyme supplementation does not. Opioids are not recommended, due to their frequent and rising association with addiction and hyperalgesia, but may be considered after other reasonable options are exhausted[2,3,31-34].
In recognition that the longer pain is present, the more difficult it is to treat, a recent randomized surgical study of 88 patients (ESCAPE trial) compared early pancreatic ductal drainage by surgery for those with strong to weak pain of less than 2-6 mo vs conventional medical and endoscopic treatment. The initial results indicated a lower pain score in the surgical group of 37 vs 49 (P = 0.02)[35], similar to data from Cahen[35]. Additional endoscopic and surgical approaches have been addressed[36-41] but are beyond the scope of this review.
CONCLUSION
This narrative review captures the highlights of a number of significant articles published between January 2019 and December 2022 bearing new concepts in pathophysiology, diagnosis, and treatment of AP and CP. The major findings include clinical identification and application of new genetic information, newly identified serum biomarkers-FAEEs, for diagnosis of alcohol-related AP, novel concepts regarding monocyte/macrophage participation in the immune reaction, important acceleration in timing of early per os feedings in AP, answers to major questions concerning the appropriateness of early, aggressive parenteral hydration, decisive shifts in non-operative management of infected pancreatic fluid, and updated, expert approaches to medical management of pain in CP. These advances are evaluated in the context of enhancing outcomes for these two acute and chronic inflammatory diseases.
ACKNOWLEDGMENT
We thank Ms. Dilan Clements for technical assistance with the graphics.
Footnotes
Conflict-of-interest statement: There are no conflicts of interest to report.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: November 15, 2022
First decision: January 2, 2023
Article in press: February 14, 2023
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gupta MK, Germany; Kirkik D, Turkey S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
Contributor Information
Williamson B Strum, Department of Gastroenterology, Scripps Clinic, La Jolla, CA 92037, United States. williamsonstrum@yahoo.com.
Clement Richard Boland, Department of Medicine, University of California San Diego, La Jolla, CA 92037, United States.
References
- 1.Peery AF, Crockett SD, Murphy CC, Jensen ET, Kim HP, Egberg MD, Lund JL, Moon AM, Pate V, Barnes EL, Schlusser CL, Baron TH, Shaheen NJ, Sandler RS. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2021. Gastroenterology. 2022;162:621–644. doi: 10.1053/j.gastro.2021.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vege SS, Chari ST. Chronic Pancreatitis. N Engl J Med. 2022;386:869–878. doi: 10.1056/NEJMcp1809396. [DOI] [PubMed] [Google Scholar]
- 3.Singh VK, Yadav D, Garg PK. Diagnosis and Management of Chronic Pancreatitis: A Review. JAMA. 2019;322:2422–2434. doi: 10.1001/jama.2019.19411. [DOI] [PubMed] [Google Scholar]
- 4.Whitcomb DC, Gorry MC, Preston RA, Furey W, Sossenheimer MJ, Ulrich CD, Martin SP, Gates LK Jr, Amann ST, Toskes PP, Liddle R, McGrath K, Uomo G, Post JC, Ehrlich GD. Hereditary pancreatitis is caused by a mutation in the cationic trypsinogen gene. Nat Genet. 1996;14:141–145. doi: 10.1038/ng1096-141. [DOI] [PubMed] [Google Scholar]
- 5.Mayerle J, Sendler M, Hegyi E, Beyer G, Lerch MM, Sahin-Tóth M. Genetics, Cell Biology, and Pathophysiology of Pancreatitis. Gastroenterology. 2019;156:1951–1968.e1. doi: 10.1053/j.gastro.2018.11.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Masamune A, Kotani H, Sörgel FL, Chen JM, Hamada S, Sakaguchi R, Masson E, Nakano E, Kakuta Y, Niihori T, Funayama R, Shirota M, Hirano T, Kawamoto T, Hosokoshi A, Kume K, Unger L, Ewers M, Laumen H, Bugert P, Mori MX, Tsvilovskyy V, Weißgerber P, Kriebs U, Fecher-Trost C, Freichel M, Diakopoulos KN, Berninger A, Lesina M, Ishii K, Itoi T, Ikeura T, Okazaki K, Kaune T, Rosendahl J, Nagasaki M, Uezono Y, Algül H, Nakayama K, Matsubara Y, Aoki Y, Férec C, Mori Y, Witt H, Shimosegawa T. Variants That Affect Function of Calcium Channel TRPV6 Are Associated With Early-Onset Chronic Pancreatitis. Gastroenterology. 2020;158:1626–1641.e8. doi: 10.1053/j.gastro.2020.01.005. [DOI] [PubMed] [Google Scholar]
- 7.Sahin-Tóth M. Channelopathy of the Pancreas Causes Chronic Pancreatitis. Gastroenterology. 2020;158:1538–1540. doi: 10.1053/j.gastro.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Habtezion A, Gukovskaya AS, Pandol SJ. Acute Pancreatitis: A Multifaceted Set of Organelle and Cellular Interactions. Gastroenterology. 2019;156:1941–1950. doi: 10.1053/j.gastro.2018.11.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saluja A, Dudeja V, Dawra R, Sah RP. Early Intra-Acinar Events in Pathogenesis of Pancreatitis. Gastroenterology. 2019;156:1979–1993. doi: 10.1053/j.gastro.2019.01.268. [DOI] [PubMed] [Google Scholar]
- 10.Lewis MD, Talluri J, Wilcox CM, Abberbock JN, Tang G, Conwell DL, Banks PA, Cote GA, Sherman S, Alkaade S, Gardner TB, Anderson MA, Sandhu BS, Muniraj T, Forsmark CE, Guda N, Gelrud A, Romagnuolo J, Brand R, LaRusch J, Amann ST, Slivka A, Whitcomb DC, Yadav D. Differences in Age at Onset of Symptoms, and Effects of Genetic Variants, in Patients With Early vs Late-Onset Idiopathic Chronic Pancreatitis in a North American Cohort. Clin Gastroenterol Hepatol. 2021;19:349–357. doi: 10.1016/j.cgh.2020.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mederos MA, Reber HA, Girgis MD. Acute Pancreatitis: A Review. JAMA. 2021;325:382–390. doi: 10.1001/jama.2020.20317. [DOI] [PubMed] [Google Scholar]
- 12.Gardner TB. Acute Pancreatitis. Ann Intern Med. 2021;174:ITC17–ITC32. doi: 10.7326/AITC202102160. [DOI] [PubMed] [Google Scholar]
- 13.Whitcomb DC North American Pancreatitis Study Group. Pancreatitis: TIGAR-O Version 2 Risk/Etiology Checklist With Topic Reviews, Updates, and Use Primers. Clin Transl Gastroenterol. 2019;10:e00027. doi: 10.14309/ctg.0000000000000027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vela S, Guerra A, Farrell G, Trivedi S, Chaffin H, Rood C, Singh R, Kostenko S, Chang YH, Snozek C, Patel K, Khatua B, Singh VP. Pathophysiology and Biomarker Potential of Fatty Acid Ethyl Ester Elevation During Alcoholic Pancreatitis. Gastroenterology. 2021;161:1513–1525. doi: 10.1053/j.gastro.2021.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Manohar M, Jones EK, Rubin SJS, Subrahmanyam PB, Swaminathan G, Mikhail D, Bai L, Singh G, Wei Y, Sharma V, Siebert JC, Maecker HT, Husain SZ, Park WG, Pandol SJ, Habtezion A. Novel Circulating and Tissue Monocytes as Well as Macrophages in Pancreatitis and Recovery. Gastroenterology. 2021;161:2014–2029.e14. doi: 10.1053/j.gastro.2021.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Allawadhi P, Beyer G, Mahajan UM, Mayerle J. Novel Insights Into Macrophage Diversity During the Course of Pancreatitis. Gastroenterology. 2021;161:1802–1805. doi: 10.1053/j.gastro.2021.09.049. [DOI] [PubMed] [Google Scholar]
- 17.Jeon CY, Whitcomb DC, Slivka A, Brand RE, Gelrud A, Tang G, Abberbock J, AlKaade S, Guda N, Mel Wilcox C, Sandhu BS, Yadav D. Lifetime Drinking History of Persons With Chronic Pancreatitis. Alcohol Alcohol. 2019;54:615–624. doi: 10.1093/alcalc/agz072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Strum WB. Abstinence in alcoholic chronic pancreatitis. Effect on pain and outcome. J Clin Gastroenterol. 1995;20:37–41. doi: 10.1097/00004836-199501000-00010. [DOI] [PubMed] [Google Scholar]
- 19.Strum WB, Spiro HM. Chronic pancreatitis. Ann Intern Med. 1971;74:264–277. doi: 10.7326/0003-4819-74-2-264. [DOI] [PubMed] [Google Scholar]
- 20.Lugea A, Gerloff A, Su HY, Xu Z, Go A, Hu C, French SW, Wilson JS, Apte MV, Waldron RT, Pandol SJ. The Combination of Alcohol and Cigarette Smoke Induces Endoplasmic Reticulum Stress and Cell Death in Pancreatic Acinar Cells. Gastroenterology. 2017;153:1674–1686. doi: 10.1053/j.gastro.2017.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sahin-Tóth M, Hegyi P. Smoking and Drinking Synergize in Pancreatitis: Multiple Hits on Multiple Targets. Gastroenterology. 2017;153:1479–1481. doi: 10.1053/j.gastro.2017.10.031. [DOI] [PubMed] [Google Scholar]
- 22.Pitchumoni CS, Glasser M, Saran RM, Panchacharam P, Thelmo W. Pancreatic fibrosis in chronic alcoholics and nonalcoholics without clinical pancreatitis. Am J Gastroenterol. 1984;79:382–388. [PubMed] [Google Scholar]
- 23.Hori Y, Vege SS, Chari ST, Gleeson FC, Levy MJ, Pearson RK, Petersen BT, Kendrick ML, Takahashi N, Truty MJ, Smoot RL, Topazian MD. Classic chronic pancreatitis is associated with prior acute pancreatitis in only 50% of patients in a large single-institution study. Pancreatology. 2019;19:224–229. doi: 10.1016/j.pan.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 24.Crockett SD, Wani S, Gardner TB, Falck-Ytter Y, Barkun AN American Gastroenterological Association Institute Clinical Guidelines Committee. American Gastroenterological Association Institute Guideline on Initial Management of Acute Pancreatitis. Gastroenterology. 2018;154:1096–1101. doi: 10.1053/j.gastro.2018.01.032. [DOI] [PubMed] [Google Scholar]
- 25.Ramírez-Maldonado E, López Gordo S, Pueyo EM, Sánchez-García A, Mayol S, González S, Elvira J, Memba R, Fondevila C, Jorba R. Immediate Oral Refeeding in Patients With Mild and Moderate Acute Pancreatitis: A Multicenter, Randomized Controlled Trial (PADI trial) Ann Surg. 2021;274:255–263. doi: 10.1097/SLA.0000000000004596. [DOI] [PubMed] [Google Scholar]
- 26.Buxbaum JL, Bolado F, de-Madaria E. Aggressive or Moderate Fluids in Acute Pancreatitis. Reply. N Engl J Med. 2022;387:2199–2200. doi: 10.1056/NEJMc2213440. [DOI] [PubMed] [Google Scholar]
- 27.Gardner TB. Fluid Resuscitation in Acute Pancreatitis - Going over the WATERFALL. N Engl J Med. 2022;387:1038–1039. doi: 10.1056/NEJMe2209132. [DOI] [PubMed] [Google Scholar]
- 28.Boxhoorn L, van Dijk SM, van Grinsven J, Verdonk RC, Boermeester MA, Bollen TL, Bouwense SAW, Bruno MJ, Cappendijk VC, Dejong CHC, van Duijvendijk P, van Eijck CHJ, Fockens P, Francken MFG, van Goor H, Hadithi M, Hallensleben NDL, Haveman JW, Jacobs MAJM, Jansen JM, Kop MPM, van Lienden KP, Manusama ER, Mieog JSD, Molenaar IQ, Nieuwenhuijs VB, Poen AC, Poley JW, van de Poll M, Quispel R, Römkens TEH, Schwartz MP, Seerden TC, Stommel MWJ, Straathof JWA, Timmerhuis HC, Venneman NG, Voermans RP, van de Vrie W, Witteman BJ, Dijkgraaf MGW, van Santvoort HC, Besselink MG Dutch Pancreatitis Study Group. Immediate versus Postponed Intervention for Infected Necrotizing Pancreatitis. N Engl J Med. 2021;385:1372–1381. doi: 10.1056/NEJMoa2100826. [DOI] [PubMed] [Google Scholar]
- 29.Baron TH. Drainage for Infected Pancreatic Necrosis - Is the Waiting the Hardest Part? N Engl J Med. 2021;385:1433–1435. doi: 10.1056/NEJMe2110313. [DOI] [PubMed] [Google Scholar]
- 30.Trikudanathan G, Rana SS. Current Controversies and Challenges in Endoscopic Management of Necrotizing Pancreatitis. Clin Gastroenterol Hepatol. 2022;20:2717–2721. doi: 10.1016/j.cgh.2022.06.016. [DOI] [PubMed] [Google Scholar]
- 31.Yadav D, Palermo TM, Phillips AE, Bellin MD, Conwell DL. Painful chronic pancreatitis - new approaches for evaluation and management. Curr Opin Gastroenterol. 2021;37:504–511. doi: 10.1097/MOG.0000000000000769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beyer G, Habtezion A, Werner J, Lerch MM, Mayerle J. Chronic pancreatitis. Lancet. 2020;396:499–512. doi: 10.1016/S0140-6736(20)31318-0. [DOI] [PubMed] [Google Scholar]
- 33.Kempeneers MA, Issa Y, Verdonk RC, Bruno M, Fockens P, van Goor H, Alofs E, Bollen TL, Bouwense S, van Dalen ASHM, van Dieren S, van Dullemen HM, van Geenen EJ, Hoge C, van Hooft JE, Kager LM, Keulemans Y, Nooijen LE, Poley JW, Seerden TCJ, Tan A, Thijs W, Timmer R, Vleggaar F, Witteman B, Ahmed Ali U, Besselink MG, Boermeester MA, van Santvoort HC Dutch Pancreatitis Study Group. Pain patterns in chronic pancreatitis: a nationwide longitudinal cohort study. Gut. 2021;70:1724–1733. doi: 10.1136/gutjnl-2020-322117. [DOI] [PubMed] [Google Scholar]
- 34.Gardner TB, Adler DG, Forsmark CE, Sauer BG, Taylor JR, Whitcomb DC. ACG Clinical Guideline: Chronic Pancreatitis. Am J Gastroenterol. 2020;115:322–339. doi: 10.14309/ajg.0000000000000535. [DOI] [PubMed] [Google Scholar]
- 35.Issa Y, Kempeneers MA, Bruno MJ, Fockens P, Poley JW, Ahmed Ali U, Bollen TL, Busch OR, Dejong CH, van Duijvendijk P, van Dullemen HM, van Eijck CH, van Goor H, Hadithi M, Haveman JW, Keulemans Y, Nieuwenhuijs VB, Poen AC, Rauws EA, Tan AC, Thijs W, Timmer R, Witteman BJ, Besselink MG, van Hooft JE, van Santvoort HC, Dijkgraaf MG, Boermeester MA Dutch Pancreatitis Study Group. Effect of Early Surgery vs Endoscopy-First Approach on Pain in Patients With Chronic Pancreatitis: The ESCAPE Randomized Clinical Trial. JAMA. 2020;323:237–247. doi: 10.1001/jama.2019.20967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cahen DL, Gouma DJ, Laramée P, Nio Y, Rauws EA, Boermeester MA, Busch OR, Fockens P, Kuipers EJ, Pereira SP, Wonderling D, Dijkgraaf MG, Bruno MJ. Long-term outcomes of endoscopic vs surgical drainage of the pancreatic duct in patients with chronic pancreatitis. Gastroenterology. 2011;141:1690–1695. doi: 10.1053/j.gastro.2011.07.049. [DOI] [PubMed] [Google Scholar]
- 37.Drewes AM, Kempeneers MA, Andersen DK, Arendt-Nielsen L, Besselink MG, Boermeester MA, Bouwense S, Bruno M, Freeman M, Gress TM, van Hooft JE, Morlion B, Olesen SS, van Santvoort H, Singh V, Windsor J. Controversies on the endoscopic and surgical management of pain in patients with chronic pancreatitis: pros and cons! Gut. 2019;68:1343–1351. doi: 10.1136/gutjnl-2019-318742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kitano M, Gress TM, Garg PK, Itoi T, Irisawa A, Isayama H, Kanno A, Takase K, Levy M, Yasuda I, Lévy P, Isaji S, Fernandez-Del Castillo C, Drewes AM, Sheel ARG, Neoptolemos JP, Shimosegawa T, Boermeester M, Wilcox CM, Whitcomb DC. International consensus guidelines on interventional endoscopy in chronic pancreatitis. Recommendations from the working group for the international consensus guidelines for chronic pancreatitis in collaboration with the International Association of Pancreatology, the American Pancreatic Association, the Japan Pancreas Society, and European Pancreatic Club. Pancreatology. 2020;20:1045–1055. doi: 10.1016/j.pan.2020.05.022. [DOI] [PubMed] [Google Scholar]
- 39.Kempeneers MA, Issa Y, Ali UA, Baron RD, Besselink MG, Büchler M, Erkan M, Fernandez-Del Castillo C, Isaji S, Izbicki J, Kleeff J, Laukkarinen J, Sheel ARG, Shimosegawa T, Whitcomb DC, Windsor J, Miao Y, Neoptolemos J, Boermeester MA Working group for the International (IAP-APA-JPS-EPC) Consensus Guidelines for Chronic Pancreatitis. International consensus guidelines for surgery and the timing of intervention in chronic pancreatitis. Pancreatology. 2020;20:149–157. doi: 10.1016/j.pan.2019.12.005. [DOI] [PubMed] [Google Scholar]
- 40.Abu-El-Haija M, Anazawa T, Beilman GJ, Besselink MG, Del Chiaro M, Demir IE, Dennison AR, Dudeja V, Freeman ML, Friess H, Hackert T, Kleeff J, Laukkarinen J, Levy MF, Nathan JD, Werner J, Windsor JA, Neoptolemos JP, Sheel ARG, Shimosegawa T, Whitcomb DC, Bellin MD. The role of total pancreatectomy with islet autotransplantation in the treatment of chronic pancreatitis: A report from the International Consensus Guidelines in chronic pancreatitis. Pancreatology. 2020;20:762–771. doi: 10.1016/j.pan.2020.04.005. [DOI] [PubMed] [Google Scholar]
- 41.Strand DS, Law RJ, Yang D, Elmunzer BJ. AGA Clinical Practice Update on the Endoscopic Approach to Recurrent Acute and Chronic Pancreatitis: Expert Review. Gastroenterology. 2022;163:1107–1114. doi: 10.1053/j.gastro.2022.07.079. [DOI] [PubMed] [Google Scholar]