Abstract
Objective
To evaluate whether the expansion of Federally Qualified Health Centers (FQHCs) improved late prenatal care initiation, low birth weight, and preterm birth among Medicaid‐covered or uninsured individuals.
Data Sources and Study Setting
We identified all FQHCs in California using the Health Resources and Services Administration's Uniform Data System from 2000 to 2019. We used data from the U.S. Census American Community Survey to describe area characteristics. We measured outcomes in California birth certificate data from 2007 to 2019.
Study Design
We compared areas that received their first FQHC between 2011 and 2016 to areas that received it later or that had never had an FQHC. Specifically, we used a synthetic control with a staggered adoption approach to calculate non‐parametric estimates of the average treatment effects on the treated areas. The key outcome variables were the rate of Medicaid or uninsured births with late prenatal care initiation (>3 months' gestation), with low birth weight (<2500 grams), or with preterm birth (<37 weeks' gestation).
Data Collection/Extraction Methods
The analysis was limited to births covered by Medicaid or that were uninsured, as indicated on the birth certificate.
Principal Findings
The 55 areas in California that received their first FQHC in 2011–2016 were more populous; their residents were more likely to be covered by Medicaid, to be low‐income, or to be Hispanic than residents of the 48 areas that did not have an FQHC by the end of the study period. We found no statistically significant impact of the first FQHC on rates of late prenatal care initiation (ATT: −10.4 [95% CI −38.1, 15.0]), low birth weight (ATT: 0.2 [95% CI −7.1, 5.4]), or preterm birth (ATT: −7.0 [95% CI −15.5, 2.3]).
Conclusions
Our results from California suggest that access to primary and prenatal care may not be enough to improve these outcomes. Future work should evaluate the impact of ongoing initiatives to increase access to maternal health care at FQHCs through targeted workforce investments.
Keywords: maternal and perinatal care and outcomes, Medicaid, observational data/quasi‐experiments, obstetrics/gynecology, uninsured/safety net providers
What is known on this topic
Federally Qualified Health Centers (FQHCs) improve access to care in the areas they serve.
Many low‐income and minoritized people of reproductive age use FQHCs for contraception and prenatal care.
New federal funding has driven rapid growth in the number of FQHC clinic sites since 2010.
What this study adds
We examine whether the opening of the first FQHC in a Primary Care Service Area improves the timing of prenatal care initiation and birth outcomes.
We did not detect statistically significant changes in rates of late prenatal care initiation, low birth weight, or preterm birth after an area received its first FQHC.
Our results suggest that access to primary and prenatal care may not be sufficient for improving these outcomes.
1. INTRODUCTION
The United States lags peer countries and national targets in maternal and child health outcomes. 1 , 2 Infants born preterm or with low birth weight face elevated risk of infant death, developmental, cognitive, and behavioral challenges, and worse educational and economic outcomes later in life. 3 Centuries of structural racism drive disparities in these outcomes. 4 In the United States in 2019, 14.4% of non‐Hispanic Black births and 10.0% of Hispanic births were preterm, compared to 9.3% of non‐Hispanic White births. 5
Access to prenatal care anchors approaches to improving these outcomes. 6 Receiving prenatal care early in pregnancy helps to identify and manage complications, provides pregnant people with resources for support, and improves neonatal outcomes. 7 , 8 Nearly all pregnant people in the United States receive some prenatal care. 9 However, in 2016, late (beginning in the third trimester) or no prenatal care preceded 6% of all births, 9% of Medicaid‐covered births, and 20% of births to uninsured individuals. 9 Ten percent of non‐Hispanic Black pregnant people and 8% of Hispanic pregnant people had late or no prenatal care, compared to 5% of non‐Hispanic White pregnant people. 5
More evidence is needed on whether expanding the availability of outpatient care improves late initiation of prenatal care and birth outcomes. Prior work has shown that receiving pre‐conception health care is associated with early prenatal care initiation. 10 , 11 People living in areas with a higher density of obstetrician‐gynecologists or primary care physicians experience better prenatal care access and birth outcomes. 11 , 12 A recent study using historical data found reductions in low birth weight and improved access to prenatal care following the rollout of community health centers in the mid‐1960s to late‐1980s. 13 However, this analysis largely predates major increases in Medicaid eligibility for pregnant individuals, as well as changes in the demographic and health profiles of health center patients. 14 , 15
Understanding how the continued expansion of health centers might affect access to prenatal care and birth outcomes can inform national policy on improving maternal and child health. Such expansions are part of state and federal strategies targeting these outcomes, alongside investments in the social determinants of health. 16 Experts recommend targeted investments in community‐based organizations and clinics that are positioned to meet the diverse needs of local communities. 17 , 18
Federally Qualified Health Centers (FQHCs) can be key partners. These health centers are non‐profit clinics with a majority‐patient governing board that provide free or low‐cost, culturally tailored care to low‐income patients. The federal government supports FQHCs with financial and programmatic resources. In addition to a wide range of health care services, FQHCs provide non‐clinical services, such as language interpretation, transportation, and health education. 19 In 2020, over 12,000 FQHC sites across the country cared for more than 28.6 million patients. 20 FQHCs serve nearly one‐third of all low‐income women of reproductive age. 21 They also serve 8% of all pregnant people nationwide and a higher proportion from minoritized groups: 18% of Hispanic and 10% of Black non‐Hispanic pregnant people. 20 About two‐thirds of FQHC clinic networks include a site that provides prenatal care directly, and the rest refer patients to other clinics. 20 Racial disparities in access to care and birth outcomes are diminished among patients served by FQHCs relative to the general population. 22
New or existing clinics can apply to the Health Resources and Services Administration (HRSA) for FQHC certification. Eligible clinics are non‐profit, serve patients in a medically underserved area regardless of their ability to pay, and have a governing board of mostly patients, among other requirements. Due to limited funding, not all eligible clinics become FQHCs. HRSA prioritizes applicants based on the needs of their communities and their demonstrated ability to meet those needs. The Affordable Care Act increased funding for FQHCs with the establishment of the Community Health Center Fund. This fund, which has been twice reauthorized and has grown from $1 billion in 2010 to $4 billion in 2019, has supported the operation and expansion of FQHCs nationwide. 23 This led to a 33% increase in the number of FQHC sites and patients served between 2010 and 2016, consistent with growth seen during prior increases in funding for this program. 24 , 25
FQHCs may impact access to prenatal care and birth outcomes via several mechanisms (Figure 1). Patients in areas served by FQHCs are more likely to report having a usual source of primary care than patients in areas without FQHCs. 26 , 27 , 28 One study found that this translated into mortality reductions following the expansion of community health centers from 1965 to 1974. 29 Having a usual source of primary care enables better management of chronic health conditions, like hypertension or diabetes, and, in turn, reduces the risk of pregnancy complications and adverse birth outcomes. 10 Patients connected to a clinic may obtain a pregnancy test there, leading to earlier identification of their pregnancy and the initiation of prenatal care. 7 , 10 , 30 , 31 FQHCs improve access to highly effective contraception, which can decrease rates of unintended pregnancy. 32 , 33 Unintended pregnancy is associated with later initiation of prenatal care and worse birth outcomes. 7 FQHCs could therefore also impact the demographic composition of the birthing population by changing birth rates among their patients.
FIGURE 1.
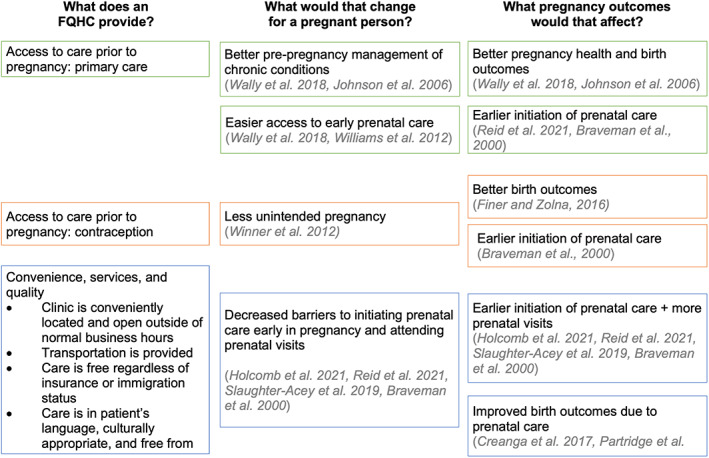
Mechanisms of FQHC impact on prenatal care and birth outcomes [Color figure can be viewed at wileyonlinelibrary.com]
Features of the care provided at FQHCs may reduce obstacles to initiating prenatal care, which include inflexible work or school schedules, inconvenient locations, inaccessible transportation, cost, language barriers, and racism or discrimination by clinic staff or providers. 7 , 31 , 34 , 35 FQHCs are located near their patient populations, often provide transportation services, and have more convenient hours. 19 Care at FQHCs is free or low‐cost. The clinics provide language translation services and benefit from programs that create a diverse workforce to match their patient population's demographic profile. 36
We study whether FQHCs impact late initiation of prenatal care, low birth weight, and preterm birth among births covered by Medicaid or to uninsured individuals. We leverage the recent growth in FQHC sites to study whether the geographic expansion of pre‐conception and prenatal care improves these outcomes.
2. METHODS
We conducted a synthetic control study to estimate the impact of the first FQHC presence in an area on prenatal care and birth outcomes in California between 2007 and 2019. We analyzed Primary Care Service Areas (PCSAs), a geographic market definition for primary care based on Medicare claims data. 37 Primary Care Service Areas comprise neighboring ZIP codes in which most Medicare beneficiaries receive their primary care from the same providers. Our analysis is limited to California due to the availability of outcome data at the ZIP code level.
2.1. Data, sample, and outcomes
We measured outcomes in vital records and birth certificate data from the California Department of Public Health. These data included demographic and clinical characteristics of every birth in the state from 2007 to 2019. We used the birthing person's ZIP code of residence and the PCSA Data Crosswalk Files from the Dartmouth Atlas Project to attribute each birth to a PCSA. 38 We restricted the analysis to births covered by Medicaid and to uninsured individuals since privately insured pregnant people are less likely to receive care at an FQHC. We limited the sample to PCSAs that had at least 10 births in every year from 2007 to 2019 to maintain data deidentification.
We defined PCSAs' treatment status using the Uniform Data System (UDS). The UDS compiles information that FQHCs submit annually to HRSA. It includes the addresses of all clinic sites, which we used to identify the location of all FQHC sites in California. In UDS data from 2000 to 2019, we identified the year in which an FQHC first appeared in each PCSA (its treatment year). To observe outcome data for at least four pre‐treatment years and three post‐treatment years, we defined the treatment group as all PCSAs that received their first FQHC between 2011 and 2016 (see Appendix A for additional detail). Though many PCSAs treated prior to 2011 received additional FQHC sites over this time period, we did not include them in the analysis because the evolving impacts of earlier treatments could have contaminated our estimates. 39 , 40 PCSAs treated between 2017 and 2019 were excluded due to an insufficient post‐period. PCSAs without an FQHC by 2019 were considered never‐treated and may have been included in the synthetic control (discussed below).
We used data from the American Community Survey (ACS) to describe the PCSAs' total population size and the percent enrolled in Medicaid, with less than a high school education, under 200% of the Federal Poverty Level, and that were identified as White. We aggregated the ZIP code‐level 5‐year estimates covering 2007–2019 to the PCSA‐year level by applying the ZIP‐to‐PCSA crosswalk and creating sums or population‐weighted averages (see Appendix A for additional detail on the years of data used). We used additional demographic variables from the birth certificate data to describe the rates of births to individuals with less than a high school education and who were White.
We examined three primary outcomes: the population rate of births preceded by late prenatal care initiation (after 3 months of gestation), of infants born with low birth weight (< 2500 grams), and of infants born preterm (at <37 weeks' completed gestation). We chose these outcomes because they are all important to maternal and child health and are plausibly affected by an FQHC within its first few years (Figure 1).
We estimated population rates for these outcomes in each PCSA from 2007 to 2019. The outcomes are reported as rates per 10,000 reproductive‐age females with Medicaid or who were uninsured. The numerators were the number of births covered by Medicaid or to uninsured individuals with late prenatal care initiation, low birth weight, or preterm birth, respectively. The denominators were the approximate numbers of reproductive‐age females (ages 15–44) who were uninsured or had Medicaid coverage. Since ZIP‐code level data on insurance coverage were not available prior to 2013, we approximated this quantity. Specifically, we obtained the number of females ages 15–44 from the ACS and multiplied it by the percent of births covered by Medicaid or that were uninsured, as observed in the birth certificate data. We conducted a sensitivity analysis to assess any potential bias from this approximation by replacing the percent of births covered by Medicaid or that were uninsured with the percent of females ages 19–64 with Medicaid or who were uninsured.
To evaluate whether our results could be explained by a shift in the demographic composition of the birthing population due to changes in family planning, we measured whether the first FQHC in a PCSA led to changes in three secondary outcomes among the population of females ages 15–44 with Medicaid or who were uninsured: the overall birth rate, rates of births to Hispanic individuals, and rates of births to individuals less than 20 years old (teens). Finally, because our study period overlaps with California's county‐level Medicaid expansion, we assess whether county expansion decisions differed by treatment status and its potential effects on our results (Appendix B).
2.2. Statistical analysis
To estimate the impacts of the first FQHC presence, we compared outcomes in treated and untreated PCSAs. Because we expected untreated areas to have different outcome levels and trends, we did not naively compare the two groups. Instead, we assumed that outcomes in the two groups were comparable only after conditioning on their past outcome trajectories. We used a synthetic control method, which enabled more flexible conditioning on past outcomes than matching or including lagged outcomes in a regression (see Appendix C for a detailed description of this approach). 41 PCSAs were treated at different times, so we indexed time in years relative to the treatment year ().
A PCSA's synthetic control could include two types of PCSAs: never‐treated PCSAs (no FQHC by 2019) and later‐treated PCSAs. Later‐treated PCSAs were those that had their first FQHC presence at least 3 years (the length of the post‐period) after the treated PCSA was treated. All the never‐treated and later‐treated PCSAs for a given treated PCSA were considered potential “donors” to its synthetic control. Each donor's PCSA made a weighted contribution to the synthetic control. The weights were proportional to the similarity of pre‐treatment outcome trends between the treated and donor PCSA.
The estimates were the average treatment effect on the treated years after treatment for each and for the entire post‐period . The estimator was the average difference between the weighted combination of the treated PCSAs' outcomes in year and the synthetic control's outcome in year . The estimator denotes the average across the post‐period We allowed for an intercept difference between the treated units and the synthetic control. We used a wild bootstrap procedure to construct 95% confidence intervals around the treatment effect estimates. 42
This procedure, described in Ben‐Michael et al. (2021), was a “partially pooled” synthetic control as it combined two types of synthetic controls: the pooled approach and the separate approach. The pooled approach created one synthetic control based on the average pre‐period outcomes across all treated units. The separate approach created a distinct synthetic control for each treated unit (see Appendix D). The partially pooled synthetic control created a weighted combination of these two synthetic controls to minimize the bias from each. The synthetic control was constructed based on pre‐period outcomes, and there was therefore a unique synthetic control for each outcome examined in this study (see Appendix E for additional detail on variation in the composition of the synthetic control across PCSAs and outcomes). To succinctly describe the evolution of covariates in the treated group and synthetic control group, we created an average synthetic control group by normalizing the weights across the never‐treated and later‐treated PCSAs for the low birth weight outcome.
The key assumption is that the synthetic control's outcomes in the post period approximate the treated group's post period outcomes if they had not been treated. Though this assumption is not empirically testable, Ben‐Michael et al. suggest that it can be supported if the pre‐treatment difference in outcomes between the treated group and the synthetic control ( for ) is close to zero. While characteristics of treated and untreated PCSAs are likely to differ, any differences that are stable over time will not bias our results. In addition, the synthetic control uses untreated PCSAs with similar outcome trends to the treated PCSAs, which is the basis for comparability of their post‐period outcomes. Thus, even time‐varying differences are not biased so long as our synthetic control is well‐matched. We believe this is the case, based on the observed similarity in pre‐period trends between the treated and synthetic control groups. We conducted all analyses in R version 4.0.2 using the augsynth package. 43
3. RESULTS
3.1. Characteristics of treatment and synthetic control groups
Between 2011 and 2016, 55 PCSAs received their first FQHC (Figure 2). Forty‐eight PCSAs had not received their first FQHC by the end of 2019 (never‐treated). Over the study period, residents of treated PCSAs were more likely to have Medicaid, to have low income, and to be non‐White or Hispanic (Figure 3). The two groups experienced similar trends in these characteristics over the study period: the income and racial/ethnic makeup were relatively unchanged, and the percent with Medicaid rose. Compared to their synthetic controls, treated PCSAs had larger total and birthing populations (Appendix F). They had a similar rate of Medicaid or uninsured births among the reproductive age population and a higher percent of births that were covered by Medicaid or were uninsured. These measures were stable over the study period in both groups.
FIGURE 2.
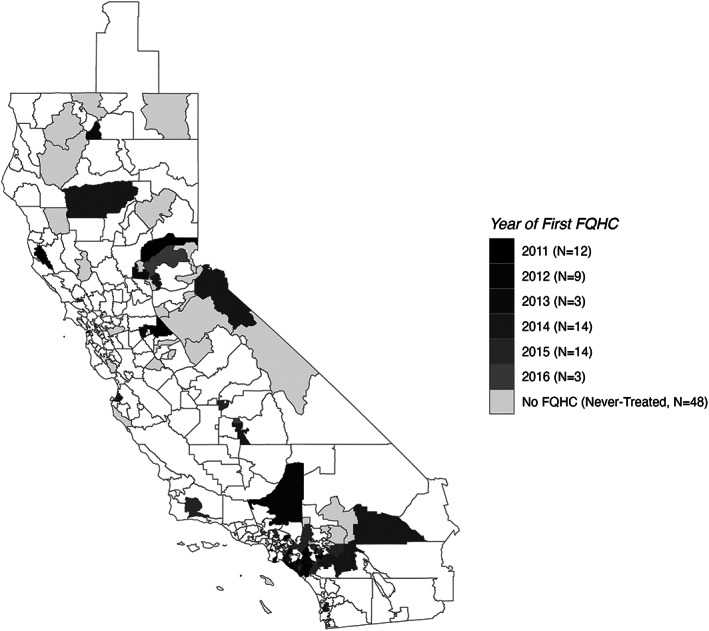
California primary care service areas that received their first FQHC (treatment) in 2011–2016, by year. The boundaries in the map represent the Primary Care Service Areas (PCSAs) that are at least partially within California (N = 348). The PCSAs shown in white are excluded from the analysis because they received their first FQHC prior to 2011 (N = 199), or after 2016 (N = 10), or because they had fewer than 10 uninsured or Medicaid‐covered births in any year between 2007 and 2019 (N = 36).
FIGURE 3.
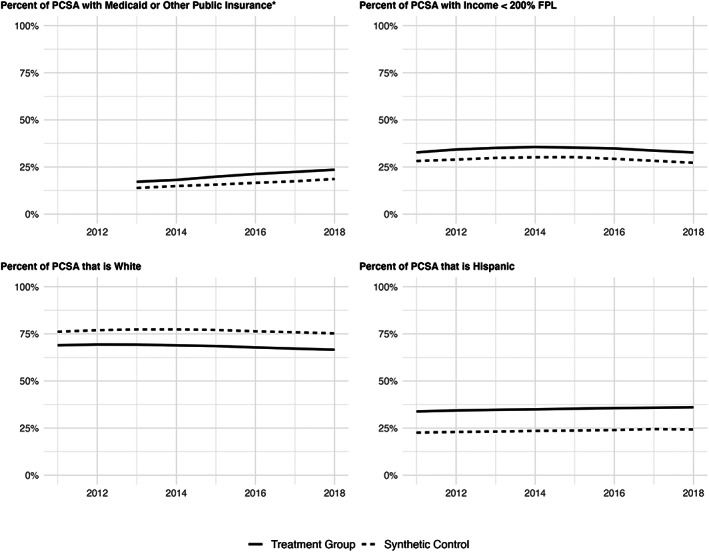
Primary Care Service Area (PCSA) population characteristics by treatment group and year. Each solid line represents the average across treated PCSAs. Each dotted line represents the average synthetic control based on the low birth weight outcome. Data on all measures were obtained from the American Community Survey. *ZIP‐Code level insurance coverage information was only collected by the United States Census American Community Survey beginning in 2013. Other public insurance does not include Medicare or TRICARE.
The rate of births to teens with Medicaid or who were uninsured was similar in the treated and synthetic control PCSAs and declined over the study period (Appendix F). The rate of births among individuals with low educational attainment in this population was higher in the treatment group and declined over the study period. The decline appears steeper in the treated PCSAs. Treated areas had a lower rate of Medicaid or uninsured births among White individuals and a higher rate among Hispanic individuals. The population rate of Medicaid or uninsured births to Hispanic individuals declined in both groups over the study period.
3.2. Estimating the impact of FQHCs on outcomes
Prior to treatment, the average of the outcomes in the treated group were (in rates per 10,000 reproductive‐age females with Medicaid or who were uninsured): 75 births with late prenatal care initiation (S.D. 61), 20 births with low birth weight (S.D. 13), and 36 preterm births (S.D. 23). The synthetic control group achieved good balance on pre‐period outcomes compared to the treatment group. This is shown in Figure 4, where the black line representing the difference between the two groups is approximately zero through the whole pre‐period for each outcome.
FIGURE 4.
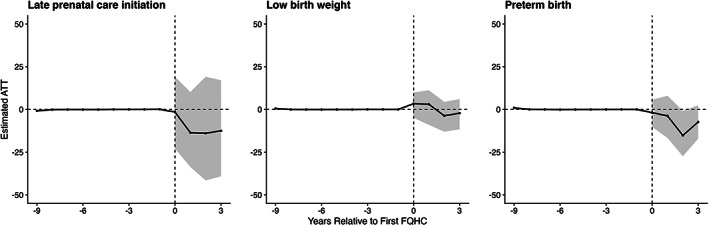
The Impact of the first FQHC in a primary care service area on late prenatal care initiation and birth outcomes. The black dots show the , or difference between the treatment group and synthetic control, for each k years relative to the year of treatment (k = 0). The gray bands are 95% confidence intervals from the wild bootstrap procedure.
We found no statistically significant impact of the first FQHC in a PCSA on the average post‐period treatment effect () for late prenatal care initiation, low birth weight, or preterm birth (Figure 4 & Appendix G). The year‐specific point estimates () for late prenatal care initiation were negative (lower rates of late prenatal care initiation in the treated group), and those for low birth weight changed from positive (higher rates of low birth weight births) to negative over the 3‐year post period. The year‐specific point estimates for preterm birth were consistently negative (lower rates of preterm births in the treated group), and there was a statistically significant treatment effect in the second year following treatment ( = −15.2 [95% CI −27.3, −0.9]). However, the treatment effect over the whole post‐period had a wide 95% confidence interval ( = −7.0 [95% CI −15.5, 2.3]) that precluded us from rejecting the null hypothesis of no effect.
We also found no statistically significant average post‐period treatment effect () for the overall rate of Medicaid or uninsured births or the rates of births to Hispanic individuals or to teens (Appendix H). However, our results suggest a pattern of declining birth rates among Hispanic and teenage individuals following the first FQHC in a PCSA. The sensitivity analysis using an alternative denominator (the percent of females ages 19–64 with Medicaid or who were uninsured) for the outcomes yielded qualitatively similar results (not shown). Finally, we find no evidence that our results are driven by differences in county adoption of Medicaid expansion by treatment status (Appendix B).
4. DISCUSSION
We did not find any consistent, statistically significant changes in maternal and child health outcomes in the years following the introduction of the first Federally Qualified Health Center in a Primary Care Service Area. This suggests that increasing access to outpatient care and enabling services may not improve the late initiation of prenatal care or birth outcomes. This may be because access to these services is insufficient to overcome the structural determinants of these outcomes, which include racism, environmental health, and stable housing. 4 , 44 , 45 , 46
Although we observed a small and statistically significant effect on preterm birth in the second post‐period year, the effect was smaller and non‐significant in both the first and third years. One potential explanation for the “dip” is noise in the estimates comprising the synthetic control estimator. Appendix D shows the variation in the PCSA‐specific treatment effects that are combined to form the partially pooled estimator. The PCSAs with the largest variation in treatment effects tended to have fewer births per year. Treatment assignment was at the PCSA‐level, so variation in our estimates was primarily driven by the number of PCSAs. Although our sample of births was very large, we had a modest number of treated and effective comparison units; only 55 PCSAs were treated, and many comparison PCSAs received weights close to zero in the synthetic control algorithm (Appendix E).
We offer a few explanations for our results. FQHCs may change the composition of the birthing population by providing family planning and contraceptive care. If so, our treatment effects would combine impacts on who gives birth with impacts on outcomes for individuals. We found no statistically significant changes in the average post‐period demographic composition of the birthing population following the first FQHC, consistent with prior work. 13 However, following the first FQHC, treated areas experienced a gradual differential decrease in birth rates among individuals in our study population, as well as among Hispanic and teenage individuals in the population. These monotonic decreases suggest that FQHCs' provision of family planning services may lead to decreased birth rates in the populations they serve. In addition to the wide uncertainty around these estimates, we cannot assign a normative interpretation to declining birth rates. These may be desirable or not, depending on patient preferences. 47 Future studies might address FQHC effects on access to patient‐centered family planning services.
Decreasing birth rates in these populations are unlikely to have driven the null treatment effect estimates for our primary outcomes. Hispanic and teenage individuals tend to have higher rates of late prenatal care initiation and low birth weight, and similar rates of preterm birth compared to the overall birthing population. 48 Therefore, the shifts we observed were toward a birthing population with better outcomes, which would amplify rather than offset any true positive treatment effects of a new FQHC. However, the possibility remains that the composition of the birthing population changed in unmeasured ways that counteracted the positive impacts of FQHCs on individuals.
It is also possible that the current FQHC program, which is not primarily aimed at impacting maternal health, could be better targeted to improve these outcomes. Indeed, HRSA has planned workforce investments in areas with limited maternity care professionals. 49 HRSA will dispatch obstetrician/gynecologists and certified nurse midwives from the National Health Service Corp to clinics in newly identified maternity care health professional target areas. These more targeted programmatic goals may improve the impact of FQHCs on these outcomes.
There are important limitations to our data and analytic approach. First, there are limitations to the Uniform Data System. The UDS does not include detail on the FQHCs' operational history. As a result, our treatment definition of the first FQHC in an area includes both the establishment of new physical clinic sites and the conversion of existing clinic sites to FQHC status. We also cannot observe changes in the presence of FQHC Look‐Alike clinics or other community health centers that are not part of the FQHC program. The UDS does not include information on services provided at the FQHC site level, so we cannot observe whether the sites in our sample provide prenatal care directly or only by referral. However, the direct provision of prenatal care is only one mechanism by which FQHCs could impact these outcomes. We are also not able to observe whether the FQHCs in our sample are, as per their mission, providing high‐quality, culturally sensitive care that is tailored to their communities.
Second, we only estimate treatment effects for the 3 years following the first FQHC in an area. The clinics may become more effective at impacting these outcomes over time as they become more known and trusted and learn how to best reach and help their patient population. Over a longer post‐period, FQHCs could also impact other outcomes, including birth spacing and pre‐conception health.
Third, the key assumption of the synthetic control approach—that the synthetic control based on lagged outcomes is a suitable counterfactual for the treated group in the post‐period—is not empirically verifiable. The balance achieved between the lagged outcomes in the treated group and the synthetic control group lends confidence in this assumption.
Finally, detailed outcome data at the PCSA level were not available for a nationwide analysis, which may have been more generalizable and better powered to detect any true treatment effects. California's rates of late prenatal care initiation, low birth weight, and preterm birth are lower than the national averages; it is possible that we would have been able to detect an impact of FQHCs in states with worse outcomes at baseline. 50 Still, these outcomes had room for improvement in California over the study period.
Despite these limitations, our study provides evidence on an important and timely research question using novel, rigorous statistical methods. We use data from a large and diverse state, use a validated geographic level of analysis that reflects care‐seeking behaviors, and employ a clearly defined treatment (i.e., the first FQHC). The FQHC program continues to receive significant federal investment, including $6 billion in the 2021 American Rescue Plan. 51 Though we found no statistically significant impact of the first FQHC in a PCSA on prenatal care initiation and birth outcomes, future investments in the program that more specifically target maternal and infant health may yield different results.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
Supporting information
Appendix S1. Supporting Information.
ACKNOWLEDGMENTS
The authors acknowledge funding from the Harvard Graduate School of Arts and Sciences and material support from the California Department of Public Health.
Gourevitch RA, Hatfield LA. Changes in prenatal care and birth outcomes after federally qualified health center expansion. Health Serv Res. 2023;58(2):489‐497. doi: 10.1111/1475-6773.14099
Funding information Harvard Graduate School of Arts and Sciences
REFERENCES
- 1. Tikkanen R, Gunja MZ, FitzGerald M, Zephyrin L. Maternal mortality and maternity Care in the United States Compared to 10 other developed countries. The Commonwealth Fund. 10.26099/411v-9255 [DOI]
- 2. MacDorman MF, Mathews TJ, Mohangoo AD, Zeitlin J. International comparisons of infant mortality and related factors: United States and Europe, 2010; 2014:7. [PubMed]
- 3. Institute of Medicine (US) Committee on Understanding Premature Birth and Assuring Healthy Outcomes . In: Behrman RE, Butler AS, eds. Preterm Birth: Causes, Consequences, and Prevention. National Academies Press (US); 2007. Accessed January 20, 2022. http://www.ncbi.nlm.nih.gov/books/NBK11362/ [PubMed] [Google Scholar]
- 4. Crear‐Perry J, Correa‐de‐Araujo R, Lewis Johnson T, McLemore MR, Neilson E, Wallace M. Social and structural determinants of health inequities in maternal health. J Women's Health. 2021;30(2):230‐235. doi: 10.1089/jwh.2020.8882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Osterman M, Hamilton B, Martin J, Driscoll A, Valenzuela C. Births: Final Data for 2019. National Center for Health Statistics (U.S.); 2021. doi: 10.15620/cdc:112078 [DOI] [PubMed] [Google Scholar]
- 6. Peahl AF, Howell JD. The evolution of prenatal care delivery guidelines in the United States. Am J Obstet Gynecol. 2021;224(4):339‐347. doi: 10.1016/j.ajog.2020.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Braveman P. Barriers to timely prenatal care among women with insurance: the importance of prepregnancy factors. Obstet Gynecol. 2000;95(6):874‐880. doi: 10.1016/S0029-7844(00)00780-8 [DOI] [PubMed] [Google Scholar]
- 8. Cygan‐Rehm K, Karbownik K. The effects of incentivizing early prenatal care on infant health. National Bureau of Economic Research Working Paper Series. 2020;28816:54. [DOI] [PubMed]
- 9. Osterman MJK, Martin JA. Timing and Adequacy of Prenatal Care in the United States, 2016. National Center for Health Statistics (U.S.); 2018. [PubMed] [Google Scholar]
- 10. Wally MK, Huber LRB, Issel LM, Thompson ME. The association between preconception care receipt and the timeliness and adequacy of prenatal care: an examination of multistate data from pregnancy risk assessment monitoring system (PRAMS) 2009–2011. Matern Child Health J. 2018;22(1):41‐50. doi: 10.1007/s10995-017-2352-6 [DOI] [PubMed] [Google Scholar]
- 11. Kozhimannil KB, Hung P, Henning‐Smith C, Casey MM, Prasad S. Association between loss of hospital‐based obstetric services and birth outcomes in rural counties in the United States. JAMA. 2018;319:1239‐1247. doi: 10.1001/jama.2018.1830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shi L, Macinko J, Starfield B, et al. Primary care, infant mortality, and low birth weight in the states of the USA. J Epidemiol Community Health. 2004;58(5):374‐380. doi: 10.1136/jech.2003.013078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kose E, O'Keefe S, Rosales‐Rueda M. Does the Delivery of Primary Health Care Improve Birth Outcomes? Evidence from the Rollout of Community Health Centers. 2022. https://www.nber.org/papers/w30047 [Google Scholar]
- 14. Nath JB, Costigan S, Hsia RY. Changes in demographics of patients seen at federally qualified health centers, 2005‐2014. JAMA Intern Med. 2016;176(5):712‐714. doi: 10.1001/jamainternmed.2016.0705 [DOI] [PubMed] [Google Scholar]
- 15. Currie J, Gruber J. Saving babies: the efficacy and cost of recent changes in the Medicaid eligibility of pregnant women. J Polit Econ. 1996;104(6):1263‐1296. doi: 10.1086/262059 [DOI] [Google Scholar]
- 16. Katon JG, Enquobahrie DA, Jacobson K, Zephyrin L. Policies for reducing maternal morbidity and mortality and enhancing equity in maternal health. The Commonwealth Fund. 2021. doi: 10.26099/ecxf-a664 [DOI]
- 17. Godbolt D, Glover S, Sakala C. Tackling maternal health disparities: a look at four local organizations with innovative approaches. National Partnership for Women & Families; 2019. Accessed January 20, 2022. https://www.nationalpartnership.org/our-work/resources/health-care/maternity/tackling-maternal-health-disparities-a-look-at-four-local-organizations-with-innovative-approaches.pdf
- 18. Scott KA, Bray S, McLemore MR. First, do No harm: why philanthropy needs to Re‐examine its role in reproductive equity and racial justice. Health Equity. 2020;4(1):17‐22. doi: 10.1089/heq.2019.0094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yue D, Pourat N, Chen X, et al. Enabling services improve access to care, preventive services, and satisfaction among health center patients. Health Aff. 2019;38(9):1468‐1474. doi: 10.1377/hlthaff.2018.05228 [DOI] [PubMed] [Google Scholar]
- 20. Health Resources & Services Administration . Author's analysis of Uniform Data System (UDS) Awardee Data. 2020. Accessed January 13, 2022. https://data.hrsa.gov/tools/data-reporting/program-data/national
- 21. Wood SF, Strasser J, Sharac J, Wylie J, Tran TC, Rosenbaum S. Community health centers and family planning in an era of policy uncertainty. Kaiser Family Foundation; 2018:24.
- 22. Shi L, Stevens GD, Wulu JT, Politzer RM, Xu J. America's health centers: reducing racial and ethnic disparities in perinatal care and birth outcomes. Health Serv Res. 2004;39(6p1):1881‐1902. doi: 10.1111/j.1475-6773.2004.00323.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kaiser Family Foundation . Community Health Centers Prepare for Funding Uncertainty ; 2019. Accessed September 7, 2022. https://www.kff.org/medicaid/issue‐brief/community‐health‐centers‐prepare‐for‐funding‐uncertainty/.
- 24. Shi L, Lebrun LA, Tsai J. Assessing the impact of the health center growth initiative on health center patients. Public Health Rep. 2010;125(2):258‐266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. National Association of Community Health Centers . Federal Grant Funding. NACHC. Accessed October 6, 2020. https://www.nachc.org/focus-areas/policy-matters/health-center-funding/federal-grant-funding/
- 26. Hadley J, Cunningham P. Availability of safety net providers and access to Care of Uninsured Persons. Health Serv Res. 2004;39(5):1527‐1546. doi: 10.1111/j.1475-6773.2004.00302.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. McMorrow S, Zuckerman S. Expanding Federal Funding to community health centers slows decline in access for low‐income adults. Health Serv Res. 2014;49(3):992‐1010. doi: 10.1111/1475-6773.12141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Saloner B, Wilk AS, Levin J. Community health centers and access to care among underserved populations: a synthesis review. Med Care Res Rev. 2020;77(1):3‐18. doi: 10.1177/1077558719848283 [DOI] [PubMed] [Google Scholar]
- 29. Bailey MJ, Goodman‐Bacon A. The war on Poverty's experiment in public medicine: community health centers and the mortality of older Americans. Am Econ Rev. 2015;105(3):1067‐1104. doi: 10.1257/aer.20120070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Williams L, Zapata LB, D'Angelo DV, Harrison L, Morrow B. Associations between preconception counseling and maternal behaviors before and during pregnancy. Matern Child Health J. 2012;16(9):1854‐1861. doi: 10.1007/s10995-011-0932-4 [DOI] [PubMed] [Google Scholar]
- 31. Reid CN, Fryer K, Cabral N, Marshall J. Health care system barriers and facilitators to early prenatal care among diverse women in Florida. Birth. 2021;48(3):416‐427. doi: 10.1111/birt.12551 [DOI] [PubMed] [Google Scholar]
- 32. Farid M. The impact of federally qualified health centers on youth outcomes. Working Paper. Vol 40; 2020. https://scholar.harvard.edu/files/mfarid/files/farid_jmp.pdf [Google Scholar]
- 33. Ranji U, 2019. Financing family planning Services for low‐income Women: the role of public programs. KFF. Accessed October 9, 2020. https://www.kff.org/womens‐health‐policy/issue‐brief/financing‐family‐planning‐services‐for‐low‐income‐women‐the‐role‐of‐public‐programs/
- 34. Slaughter‐Acey JC, Sneed D, Parker L, Keith VM, Lee NL, Misra DP. Skin tone matters: racial microaggressions and delayed prenatal care. Am J Prev Med. 2019;57:321‐329. doi: 10.1016/j.amepre.2019.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bellerose M, Rodriguez M, Vivier PM. A systematic review of the qualitative literature on barriers to high‐quality prenatal and postpartum care among low‐income women. Health Serv Res. 2022;18:1475‐6773.14008. doi: 10.1111/1475-6773.14008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Health resources and service administration. Health Careers Pipeline and Diversity Programs; 2017. https://bhw.hrsa.gov/sites/default/files/bureau‐health‐workforce/data‐research/health‐careers‐pipeline‐and‐diversity‐2017.pdf
- 37. Goodman DC, Mick SS, Bott D, et al. Primary care service areas: a new tool for the evaluation of primary care services. Health Serv Res. 2003;38(1 Pt 1):287‐309. doi: 10.1111/1475-6773.00116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. PCSA Data Crosswalk ‐ dataset by dartmouthatlas. data.world. Accessed January 20, 2022. https://data.world/dartmouthatlas/pcsa-data-crosswalk
- 39. Chang CH, Bynum JP, Lurie JD. Geographic expansion of federally qualified health centers 2007‐2014. J Rural Health. 2019;35(3):385‐394. doi: 10.1111/jrh.12330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Callaway B. Sant'Anna PHC. Difference‐in‐differences with multiple time periods. J Econ. 2021;225(2):S0304407620303948. doi: 10.1016/j.jeconom.2020.12.001 [DOI] [Google Scholar]
- 41. Ben‐Michael E, Feller A, Rothstein J. Synthetic controls with staggered adoption. J R Stat Soc Ser B. 2021;00:1‐31. doi: 10.1111/rssb.12448 [DOI] [Google Scholar]
- 42. Otsu T, Rai Y. Bootstrap inference of matching estimators for average treatment effects. J Am Stat Assoc. 2017;112(520):1720‐1732. doi: 10.1080/01621459.2016.1231613 [DOI] [Google Scholar]
- 43. Ben‐Michael E. Augsynth: Augmented Synthetic Control Method. 2022. Accessed January 21, 2022. https://github.com/ebenmichael/augsynth
- 44. Wallace M, Crear‐Perry J, Richardson L, Tarver M, Theall K. Separate and unequal: structural racism and infant mortality in the US. Health Place. 2017;45:140‐144. doi: 10.1016/j.healthplace.2017.03.012 [DOI] [PubMed] [Google Scholar]
- 45. Bekkar B, Pacheco S, Basu R, DeNicola N. Association of air Pollution and Heat Exposure with Preterm Birth, low birth weight, and stillbirth in the US: a systematic review. JAMA Netw Open. 2020;3(6):e208243. doi: 10.1001/jamanetworkopen.2020.8243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Khadka A, Fink G, Gromis A, McConnell M. In utero exposure to threat of evictions and preterm birth: evidence from the United States. Health Serv Res. 2020;55(S2):823‐832. doi: 10.1111/1475-6773.13551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Roberts D. Reproductive justice, not just rights. Dissent. 2015;62(4):79‐82. doi: 10.1353/dss.2015.0073 [DOI] [Google Scholar]
- 48.Osterman M, Hamilton B, Martin JA, Driscoll A, Valenzuela C. Births: Final Data for 2020. National Center for Health Statistics (U.S.); 2021. doi: 10.15620/cdc:112078 [DOI] [PubMed] [Google Scholar]
- 49. Federal Register . Criteria for determining maternity care health professional target areas. Federal Register. 2021. Accessed January 27, 2022. https://www.federalregister.gov/documents/2021/09/27/2021‐20855/criteria‐for‐determining‐maternity‐care‐health‐professional‐target‐areas
- 50. March of Dimes . Peristats: State Summary for California. March of Dimes|PeriStats. 2022. Accessed September 21, 2022. https://www.marchofdimes.org/peristats/state-summaries/california?lev=1&obj=3®=99&slev=4&sreg=06&stop=55&top=3
- 51. Biden Administration Invests More Than $6 Billion from the American Rescue Plan into Community Health Centers Nationwide|HRSA. Accessed September 28, 2022. https://www.hrsa.gov/about/news/press-releases/health-center-program-american-rescue-plan
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supporting Information.


