Abstract
Background:
The purpose of this study was to evaluate the association between pre-injury Katz Index of Independence in Activities of Daily Living (Katz ADL) functional status and discharge to a facility in non-neurologically injured older trauma patients.
Methods:
Data were obtained from 207 patients in the Trauma Medical Home study cohort. Multivariable logistic regression was performed to identify factors associated with non-home discharge.
Results:
Average patient age was 67.9 (SD 11.1). Patients were predominantly white (89.4%) and female (52.2%) with a median ISS of 11 (IQR 9–14). The most common mechanism of injury was fall (48.3%), followed by motor vehicle crash (41.1%). Nearly all patients (94.7%) reported independence in activities of daily living prior to hospitalization for injury. Discharge disposition varied, 51.7% of patients were discharged home, 37.7% to subacute rehabilitation, 10.1% to acute rehabilitation and 0.5% to long-term acute care. There was no relationship between pre-injury independence and likelihood of discharge home (p=0.1331). Age (p<0.0001), BMI (p=0.0002), Charlson comorbidity score of 3 or greater (p=0.0187), being single (p=0.0077), ISS ≥ 16 (p=0.0075) and being female with self-reported symptoms of anxiety and/or depression over the past two weeks (p=0.0092) were associated with significantly greater odds of non-home discharge.
Conclusions:
Pre-injury Katz ADL is not associated with discharge disposition, though other significantly associated factors were identified. It is imperative that discussions regarding discharge disposition are initiated early during acute hospitalization. Trauma programs could potentially benefit from implementing an inpatient intervention focused on building coping skills for older patients exhibiting symptoms of anxiety or depression.
Keywords: Activities of daily living, Katz score, trauma, older adults, discharge location
BACKGROUND
As the United States undergoes a demographic shift, the average age of the population is increasing, resulting in an increase in older patient admissions at trauma centers. Clinical decision making is often more complex in this population, as older trauma patients often require more multidisciplinary care and experience worse outcomes than equally-injured younger patients. This is due to a variety of factors, including decreased physiologic reserve, polypharmacy, and medical comorbidities, complicating both inpatient and outpatient management. Older trauma patients are also discharged to a location other than home nearly twice as often as their younger counterparts.1–4 Non-home discharge has unique and serious implications for older adults; Lancaster et al. (2017) found that a quarter of patients who were discharged to inpatient rehabilitation never returned home, despite nearly all patients reporting living at home prior to injury.2
Several studies have investigated factors associated with discharge disposition in the trauma population. Overall injury severity score (ISS), head abbreviated injury scale (AIS) score, and Glasgow Coma Scale (GCS) at admission were found to be predictors of adverse discharge disposition in trauma patients presenting after a fall.5 In older patients admitted with rib fractures, age, sex, race, mechanism of injury, number of rib fractures, and certain comorbidities were independently associated with non-home discharge.1 Additionally, studies in patients with hip fractures have shown a relationship between prehospital dependence in activities of daily living and the need for post-acute care.6, 7 However, data on the use of a validated measure of functional independence to predict discharge disposition in the older injured patient is limited. Factors associated with non-home discharge in non-neurologically injured patients are of particular interest, as these patients typically have the capacity to return to full function after injury.
The Katz Index of Independence in Activities of Daily Living (Katz ADL) is a validated, six item questionnaire that measures ability to bathe, dress, toilet, remain continent, transfer, and eat that was originally developed to assess patients who experience hip fracture.8 It has since been used extensively to evaluate patients who had significant injury and is one of the most popular measures of pre-hospital functional status.4, 8, 9 One study found that Katz ADL score, along with various other factors, independently predicted discharge to LTAC/skilled nursing facility versus home/rehabilitation in elderly trauma patients, but no other studies have attempted to replicate these findings to date.4 While the use of Katz ADL as a tool to assess ability to complete basic activities of daily living is well established, its relationship with discharge disposition in older trauma patients remains relatively unexplored and unvalidated.
Given the paucity of data regarding functional independence and discharge disposition, the primary objective of this study was to ascertain whether independence as measured by the Katz Index of Activities of Daily Living is associated with discharge disposition in non-neurologically injured older trauma patients. Our secondary objective was to identify any potentially modifiable targets for intervention. We hypothesized that pre-injury dependent functional status is associated with discharge to a facility.
METHODS
Study Cohort
Data were obtained from baseline surveys completed by 207 non-neurologically injured patients in the Trauma Medical Home (TMH) study cohort, a prospective, randomized controlled trial, enrolled from October 2017 to February 2020 at three level 1 trauma centers in Indiana. The TMH study was approved by the Indiana University Institutional Review Board and informed consent was obtained from all participants. Patients were eligible for the TMH study if they were at least 50 years old, had an Injury Severity Score (ISS) of 9 or higher, were able to consent, spoke English, and had access to a telephone. Exclusion criteria were: history of dementing illness or other neurodegenerative disease, life expectancy <1 year, significant traumatic brain injury, spinal cord injury with persistent neurologic deficit, pregnancy, having a primary residence outside the state of Indiana, incarceration at time of study enrollment, presence of acute stroke upon admission or developing a stroke as a new event during hospitalization, inability to complete study questionnaires due to severe hearing loss, recent history of substance or alcohol abuse, and admission with a burn affecting >10% total body surface area. Details of the TMH study are described elsewhere.10
Study Variables
Demographic and clinical variables including age, sex, race, insurance status, comorbidities, mechanism of injury, injury severity, and discharge disposition were abstracted from electronic medical records. Patient-reported measures of depression, anxiety, health-related quality of life, and pre-injury functional status, in addition to other demographic information, were obtained via a baseline survey conducted during or shortly after the patient’s hospital stay. Symptoms of anxiety and/or depression were defined as scoring 5 or higher on the GAD-7 or PHQ-9 questionnaires, which both assess for the presence of depressive or anxious symptoms over the past two weeks. The cutoff value of 5 was selected as previous literature identified that score as the cutoff for mild depression and/or anxiety.11, 12 The main exposure variable was preinjury Katz ADL functional status. Independent functional status was defined as reporting independence in all six basic activities of daily living prior to injury on the Katz ADL, whereas dependent functional status was defined as reporting dependence in at least one of the six basic activities of daily living (i.e., a score of 5 or lower). The primary outcome of interest was discharge disposition and discharging to a facility was defined as discharging anywhere besides home, i.e., subacute rehabilitation, acute rehabilitation, or a long-term acute care hospital.
Statistical Analysis
Descriptive statistics were expressed as means and standard deviations for normally-distributed continuous variables, medians and interquartile ranges for non-normally distributed continuous variables, and frequencies and percentages for categorical variables. Patients with incomplete or missing functional status data were excluded from analysis. Demographic information, injury and hospitalization characteristics were compared between patients who discharged home and those who discharged to a facility using chi2 and Kruskal-Wallis tests. Covariates found to be associated with discharge disposition with a p value of 0.20 or less in the univariate analysis were eligible for inclusion in the initial multivariable logistic regression model, along with several pre-selected covariates of interest based on the literature. Of note, Katz ADL score was analyzed in a binary fashion (i.e., independent or dependent) due to the fact that the vast majority of patients reported preinjury independence in all six categories. Control variables in the initial regression model included age, sex, Body Mass Index (BMI), Charlson Comorbidity Index, marital status, education level, caregiver status, mechanism of injury, injury severity score (ISS), functional status, income, type of insurance, and symptoms of anxiety or depression. First order interaction terms were included to assess for the presence of effect modification between age and BMI, age and ISS, BMI and ISS, gender and symptoms of anxiety/depression, and gender and caregiver status. Backwards elimination was used with variables requiring significance of p≤0.20 in order to be retained in the model. Candidate models were then pared down by eliminating non-significant variables and the final model was chosen using the Akaike Information Criterion (AIC). This method of analysis was performed on both the full cohort and also an a. priori subgroup of patients without significant lower extremity injury (lower extremity abbreviated injury score <2). This subgroup was selected because it represents patients without lower extremity fracture who, generally speaking, would be expected to be able to return home. An alpha level of 0.05 or lower was considered statistically significant and all analyses were completed using SAS 9.4.
RESULTS
Of the 217 patients enrolled in the TMH study, 10 patients were excluded due to missing or incomplete functional status data. The remaining 207 patients with complete baseline data were analyzed. The average patient age was 67.9 (SD 11.1). Patients were predominantly white (89.4%) and female (52.2%) with a median ISS of 11 (IQR 9–14). The most common mechanism of injury was fall (48.3%), followed by motor vehicle crash (41.1%). Nearly all patients (94.7%) reported independence in basic activities of daily living prior to hospitalization for injury and approximately half (49.8%) had an in-home caregiver. The majority of patients had some kind of government insurance (Medicare or Medicaid; 65.2%). Over half of patients reported having symptoms of depression and/or anxiety (53.3%). Overall discharge disposition varied; 51.7% (n=107) of patients were discharged home, 37.7% to subacute rehabilitation (n=78), 10.1% to acute rehabilitation (n=21), and 0.5% to long-term acute care (n=1).
Upon multivariable logistic regression analysis of the full cohort, there was no relationship between reported pre-injury independence and likelihood of discharge home (p=0.1331). However, age, BMI, Charlson comorbidity score ≥ 3, relationship status, ISS ≥ 16, and symptoms of anxiety and/or depression were associated with significantly greater odds of discharging to a facility. After adjusting for other variables, we identified a significant interaction between sex and symptoms of anxiety and/or depression. Specifically, patients exhibiting symptoms of anxiety or depression who were female had significantly higher odds of discharging to a facility (OR=4.02, 95% CI 1.41–11.43) than male patients exhibiting symptoms (OR=0.59, 95% CI 0.20–1.73), see Figure 1. Because 34.3% (n=71) of patients completed the GAD-7 and PHQ-9 on or after the day of discharge and therefore may have known their discharge location, a sensitivity analysis was performed including only patients who completed the questionnaires at least two days prior to discharge (n=91). The odds ratio for females with symptoms of anxiety or depression increased significantly (OR=19.95, 95% CI 2.05–194.18) and the odds ratio for males remained small and nonsignificant (OR=0.14, 95% CI 0.02–1.17).
Figure 1.
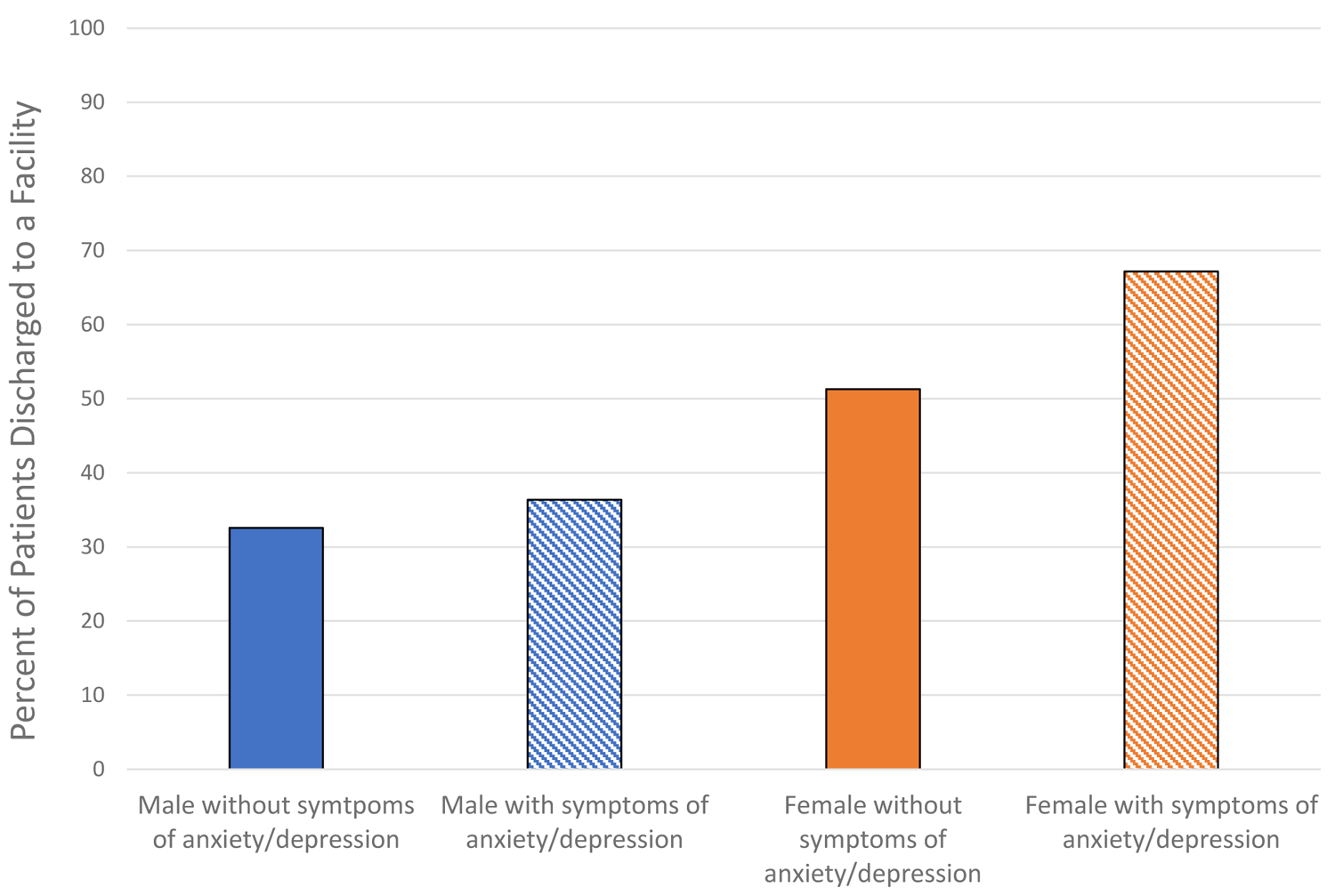
Effect Modification: Gender and Symptoms of Anxiety and/or Depression Over the Past Two Weeks
Multivariable analysis of the subgroup of patients without significant lower extremity injury (n=114) also demonstrated no relationship between reported pre-injury independence and likelihood of discharge home. Age, BMI, sex, and ISS ≥ 16 remained significantly associated with discharge disposition in the final model after adjusting for other variables.
DISCUSSION
The purpose of this investigation was to determine if pre-injury functional status as measured by the Katz ADL is associated with discharge disposition in non-neurologically injured older adults. In this prospective study of 207 older injured patients, we found that functional independence was not associated with discharge to a facility in both the full cohort and the group of patients without significant lower extremity injury, which is inconsistent with our initial hypothesis. These findings differ from the results of a study by Dunham et al., who found that Katz score did predict discharge to a nursing home/LTAC.4 However, there are several notable differences between the two study populations that could explain this discrepancy. First, the patient group analyzed by Dunham et al. was significantly older than this cohort (average ages were 80 and 67.9, respectively).4 Dementia and permanent neurologic deficit were exclusion criteria in the present study and our population was younger. While over 95% of patients were functionally independent based on the Katz ADL in the current study, nearly half the patients were unable to go directly home from the hospital. It is important to note that Dunham et al.’s outcome of interest was discharge to a nursing home or LTAC versus a rehabilitation facility or home. This differs from our primary outcome, which was any non-home discharge. It is possible that pre-injury Katz ADL is associated with discharge disposition in a less healthy older population but the association weakens when used for a non-neurologically injured older trauma population that had high pre-injury functional status.
The current literature identifies age as an important factor in the determination of discharge disposition and our results support this conclusion. Injury severity score, and gender are also well-supported by the literature as factors associated with discharge disposition in trauma patients. A study by Beaulieu et al. (2014) found that age, female sex, admission to the intensive care unit, hospital length of stay, and comorbidities all predicted discharge location in a sample of nearly 3,000 trauma patients.13 In an investigation of non-home discharge in older trauma patients presenting with rib fractures, Halevi et al. (2017) reported age, female sex, Caucasian race, number of rib fractures, and comorbidities as factors significantly associated with adverse discharge disposition.1 Similar to Halevi’s results and the results of other studies, we found that a Charlson comorbidity score of 3 or greater was associated with greater odds of discharge to a facility in the full cohort.4, 14 This highlights the fact that patients with multiple comorbidities may need extra assistance when trying to manage comorbid health conditions and a concomitant acute injury. However, when we focused on the sub-group without significant lower extremity injuries, comorbidities were not associated with discharge disposition. This indicates that patients with lower extremity injury and high levels of comorbidities could potentially benefit from early discharge planning and from coordinated care in an outpatient setting in order to avoid a discharge to a place other than home.
While we found female sex to be associated with greater odds of discharge to a facility in both the full cohort and the subgroup of patients without significant lower extremity injury and the literature is generally supportive, there are a few studies that present contradictory evidence. For example, James et al. (2018) found female sex to be non-significant in an analysis of 1,121 trauma patients presenting after a fall, and a study by Deakin et al. (2008) found males to have 2.5 times the odds of non-home discharge compared to females after hospitalization for hip fracture.5, 6 It is important to note that living alone was not a significant factor in either study. The mechanism behind these differences is not readily apparent.
The association between relationship status and discharge disposition in trauma patients is supported by the literature. Konda et al. (2020) found that single, divorced, or widowed patients had significantly greater odds of discharging to a facility than married patients, even after controlling for age, gender, medical characteristics, and insurance type.15 Relationship status can be considered a proxy for social support, which has been shown to predict discharge disposition in several populations.16, 17 Patients who perceive themselves as having substantial social support may feel better equipped to handle going home, as they know they will have help available even if they live alone.
Insurance status was not a significant factor in our analysis, contradicting the findings of several other studies. One possible explanation for this discrepancy is the older age of this study’s cohort; patients under the age of 50 were excluded and the vast majority of patients were insured either publicly or privately. Uninsured patients are more likely to discharge home even if rehabilitation is recommended, often due to a lack of financial resources.18
Perhaps one of the most interesting findings of this study was the significant association between self-reported symptoms of anxiety or depression over the past two weeks and discharge disposition. While it appears that this study may be the first investigating prospectively ascertained symptoms of anxiety and depression in relation to discharge location in non-neurologically injured older adults, these results do generally align with the findings of studies in other populations. In one study of 608 patients undergoing surgery for spondylolisthesis, patients with depression had nearly four times the odds of non-routine discharge (OR 4.28, 95% CI 1.96–9.35, p<0.001).19 However, anxiety was not significant in their analysis. Another study by Rondon et al. found that depression was significantly associated with discharge to inpatient rehabilitation facilities after total knee arthroplasty (OR 1.73, p=0.006).20 Of note, the interaction we observed between sex and symptoms of anxiety or depression is supported by the literature as studies show that women are more likely than men to have one of these conditions.21, 22
While the vast majority of the variables discussed are non-modifiable, symptoms of anxiety and/or depression are a potential target for intervention. There is a wealth of literature linking psychological comorbidities like depression and anxiety to worse outcomes in trauma patients, though the mechanism behind this association is unknown.23–26 Trauma programs could potentially benefit from implementing a depression and anxiety screening protocol for patients and following up with a brief psychosocial intervention as part of a collaborative care model, or providing patients with self-education materials to enhance coping skills. Inpatient interventions for smoking cessation have been shown to be both beneficial to patients and cost-effective, and could be used to guide development of similar programs for trauma patients.27, 28 Improving patient coping skills via an inpatient intervention could potentially help patients feel better equipped to handle discharging home, leading to increased patient quality of life, satisfaction, and lower healthcare costs.
While it may be a complex process, early discharge disposition planning in older adults has substantial benefits. A meta-analysis by Fox et al. (2013) found that early discharge planning in acutely ill and injured geriatric patients reduced the number of hospital readmissions, readmission length of stay, and improved both health-related and overall patient quality of life.29 Early initiation of the discharge disposition conversation also has the added benefit of mentally-preparing patients for the possibility of non-home discharge, even though they may have been functionally independent prior to injury. Discharge disposition planning should be initiated with at-risk patients as soon as possible to establish clear discharge expectations and help prepare them for the possibility of going to a facility.
Strengths and Limitations
This study has several strengths. To the best of the authors’ knowledge, this is the second and largest study investigating the association between pre-injury Katz ADL and non-home discharge in older trauma patients. A merit of this study is the subgroup analysis of patients without significant lower extremity injury, which provides insight into factors associated with discharge to a facility in patients whom physicians might expect to be able to go home. In addition, prospectively gathered self-report data on depression and anxiety symptoms is significantly more reliable than relying on ICD-9/10 codes from the EMR, as is common practice in retrospective studies. This study does have important limitations. First, we assumed in this study that discharging home is a good thing and it is unclear if that is actually the case. It’s possible that discharging to a facility is actually more beneficial to patients and is a desirable outcome in certain circumstances. Second, this was a relatively small study limited to three level I trauma centers in Indiana so the results may not be generalizable to the overall non-neurologically injured older trauma population. Since the TMH study only enrolled patients who had the potential to make a full recovery (i.e., neurologically injured patients were excluded), the study cohort does not represent all trauma patients ages 50 and older. Approximately one third of the patients knew their discharge disposition at the time of the baseline survey and that could have contributed to self-reported anxiety and/or depression. However, the results of the sensitivity analysis including only patients who completed the GAD-7 and PHQ-9 at least two days prior to discharge support our initial findings and suggest that symptoms of anxiety and depression is an important factor for women. As with any prospective study, it is possible that there are inherent differences between the patients who agreed to enroll in the study and those who declined participation. Finally, there is also the potential for unmeasured confounders or residual confounding distorting the estimates, despite our best efforts to minimize this.
Future Directions
Currently, there is little research available on the relationship between pre-injury functional status and non-home discharge. Future studies investigating other measurements of pre-injury functional status, such as the Lawton Instrumental Activities of Daily Living Scale, would contribute to the body of knowledge and help further characterize the relationship between functional independence and discharge disposition. The authors also suggest pilot studies evaluating the effectiveness of a brief intervention in promoting discharge home in older non-neurologically injured trauma patients reporting symptoms of anxiety or depression.
Conclusion
Our results suggest that pre-injury functional status is not associated with discharge disposition in non-neurologically injured older trauma patients. While patient injuries and ability to participate in therapy play a large role in decision making, there are also various non-modifiable and modifiable factors that can be used to identify patients at greater risk of discharging to a facility. Discharge disposition conversations should be initiated as early as possible to prepare patients for the possibility of not going home. Self-reported symptoms of anxiety and depression are a potential target for an inpatient intervention, and teaching patients coping skills could potentially help them to discharge home. Additional research is needed to investigate the effectiveness of such interventions in older trauma patients.
Table 1.
Study Cohort Characteristics
| Variable | Total (n=207) | Discharged home (n=107) | Discharged to facility (n=100) | P-value |
|---|---|---|---|---|
| Age, mean (SD) | 67.9 (11.1) | 64.3 (10.3) | 71.8 (10.8) | 0.0001 * |
| BMI, median (IQR) | 29.7 (26.0–35.2) | 29.5 (25.2–33.6) | 30.1 (26.9–36.4) | 0.0358 * |
| Charlson comorbidity score, N (%) | 0.0004 | |||
| 0 | 114 (55.1) | 72 (67.3) | 42 (42.0) | |
| 1–2 | 69 (33.3) | 29 (27.1) | 40 (40.0) | |
| 3+ | 24 (11.6) | 6 (5.6) | 18 (18.0) | |
| Male, N (%) | 99 (47.8) | 65 (60.8) | 34 (34.0) | 0.0001 |
| Race, minority, N (%) | 22 (10.6) | 10 (9.4) | 12 (12.0) | 0.5358 |
| Relationship status, N (%) | 0.0009 | |||
| Married or part of unmarried couple | 108 (52.2) | 69 (64.5) | 39 (39.0) | |
| Single | 99 (47.8) | 38 (35.5) | 61 (61.0) | |
| Insurance status, N (%) | <0.0001 | |||
| Commercial | 61 (29.5) | 43 (40.2) | 18 (18.0) | |
| Government | 135 (65.2) | 55 (51.4) | 80 (80.0) | |
| Other | 11 (5.3) | 9 (8.4) | 2 (2.0) | |
| Individual annual income, N (%) | 0.0200 | |||
| Less than $25,000 | 35 (16.9) | 13 (12.2) | 22 (22.0) | |
| $25,000 – less than $50,000 | 38 (18.4) | 22 (20.6) | 16 (16.0) | |
| $50,000 or more | 54 (26.1) | 36 (33.6) | 18 (18.0) | |
| Did not wish to disclose | 80 (38.7) | 36 (33.6) | 44 (44.0) | |
| Education, N (%) | 0.0855 | |||
| Up to high school/GED | 75 (38.1) | 32 (31.1) | 43 (45.8) | |
| Some college/Associates/Bachelors | 87 (44.2) | 49 (47.6) | 38 (40.4) | |
| Masters or Doctorate degree | 35 (17.8) | 22 (21.3) | 13 (13.8) | |
| Caregiver (in-home), N (%) | 0.0301 | |||
| Yes | 120 (58.3) | 70 (65.4) | 50 (50.5) | |
| No | 86 (41.7) | 37 (34.6) | 49 (49.5) | |
| Functional status, N (%) | 0.2958 | |||
| Independent | 196 (94.7) | 103 (96.3) | 93 (93.0) | |
| Dependent | 11 (5.3) | 4 (3.7) | 7 (7.0) | |
| Injury severity score, N (%) | 0.0348 | |||
| 9–15 | 162 (78.3) | 90 (84.1) | 72 (72.0) | |
| 16+ | 45 (21.7) | 17 (15.9) | 28 (28.0) | |
| Mechanism of injury, N (%) | 0.0075 | |||
| Fall | 100 (48.3) | 45 (24.1) | 55 (55.0) | |
| Motor vehicle crash | 85 (41.1) | 44 (41.1) | 41 (41.0) | |
| Other | 22 (10.6) | 18 (16.8) | 4 (4.0) | |
| Hospital length of stay, median (IQR) | 6 (3–9) | 4 (2–6) | 7.5 (5.5–11.5) | <0.0001 * |
| Symptoms of depression/anxiety, N (%) | 0.0978 | |||
| Yes | 122 (59.8) | 57 (53.3) | 65 (65.0) | |
| No | 82 (40.2) | 48 (44.9) | 34 (34.0) |
Bolded values indicate statistical significance.
Kruskal-Wallis test; Insurance: other = self-pay or worker’s comp. Breakdown of discharge disposition: Home n=107, 51%; Acute Rehabilitation n=21, 10.1%; Subacute rehabilitation n=78, 37.7%; LTAC n=1, 0.5%; Numbers may not equal total due to nondisclosure by patients; statistical analysis was performed on non-missing data.
Table 2.
Multivariable Logistic Regression, Discharge to Facility vs Discharge Home – Full Cohort
| Variable | Adjusted Odds Ratio (95% CI) | P-value |
|---|---|---|
| Age | 1.09 (1.05–1.13) | <0.0001 |
| BMI | 1.12 (1.05–1.18) | 0.0002 |
| Charlson comorbidity score | ||
| 0 | Referent | |
| 1–2 | 1.67 (0.75–3.74) | 0.2093 |
| 3+ | 4.14 (1.27–13.55) | 0.0187 |
| Relationship status | ||
| Married or in a relationship | Referent | |
| Single | 2.78 (1.31–5.91) | 0.0077 |
| ISS≥16 | 3.09 (1.37–7.23) | 0.0075 |
| Independent | 3.36 (0.73–18.16) | 0.1331 |
| Symptoms of anxiety or depression | ||
| Female | 4.02 (1.41–11.43) | 0.0092 |
| Male | 0.59 (0.20–1.73) | 0.3381 |
Bolded values indicate statistical significance.
Table 3.
Multivariable Logistic Regression, Discharge to Facility vs Discharge Home – Patients without significant lower extremity injury (lower extremity AIS <2)
| Variable | Adjusted Odds Ratio (95% CI) | P-value |
|---|---|---|
| Age | 1.12 (1.06–1.18) | <0.0001 |
| BMI | 1.11 (1.01–1.21) | 0.0285 |
| Female | 3.01 (1.14–8.39) | 0.0293 |
| ISS≥16 | 3.61 (1.19–11.86) | 0.0271 |
Bolded values indicate statistical significance.
Table 4.
Study Cohort by Age Group and Discharge Location
| Age Group, n (%) | Total (n=207) | Discharged Home (n=107) | Discharged to Facility (n=100) |
|---|---|---|---|
| 50–59 | 61 (29.5) | 44 (72.1) | 17 (27.9) |
| 60–69 | 59 (28.5) | 34 (57.6) | 25 (42.4) |
| 70–79 | 47 (22.7) | 16 (34.0) | 31 (66.0) |
| 80–89 | 34 (16.4) | 11 (32.4) | 23 (67.6) |
| 90+ | 6 (2.9) | 2 (33.3) | 4 (66.7) |
Percentages displayed in the ‘Discharged Home’ and ‘Discharged to Facility’ columns represent the percentage of the age group.
Funding Sources:
The Trauma Medical Home randomized controlled trial is funded by NIH Grant 1R01AG052493-01A1. The funding sources had no role in the design, execution, analysis, interpretation of data, or decision to submit results for this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: none.
Contributor Information
Emma Holler, Department of Trauma and Acute Care Surgery, Eskenazi Health, Indianapolis, IN, USA.
Ashley D Meagher, Department of Surgery, Indiana University School of Medicine, Indianapolis, IN, USA.
Damaris Ortiz, Department of Surgery, Indiana University School of Medicine, Indianapolis, IN, USA.
Sanjay Mohanty, Department of Surgery, Indiana University School of Medicine, Indianapolis, IN, USA.
America Newnum, Department of Surgery, Indiana University School of Medicine, Indianapolis, IN, USA.
Anthony Perkins, Department of Biostatistics, Indiana University School of Medicine, Indianapolis, IN, USA.
Sujuan Gao, Department of Biostatistics, Indiana University School of Medicine, Indianapolis, IN, USA.
Gabriel Kinnaman, Department of Surgery, Indiana University School of Medicine, Indianapolis, IN, USA.
Malaz Boustani, Department of Medicine, Indiana University School of Medicine, Indianapolis, IN, USA.
Ben Zarzaur, Department of Surgery, University of Wisconsin School of Medicine, Madison, WI, USA.
References
- 1.Halevi AE, et al. , Predictors of Dependency in Geriatric Trauma Patients with Rib Fractures: A Population Study. Am Surg, 2018. 84(12): p. 1856–1860. [PubMed] [Google Scholar]
- 2.Lancaster CW, et al. , Functional outcomes after inpatient rehabilitation for trauma-improved but unable to return home. J Surg Res, 2018. 222: p. 187–194 e3. [DOI] [PubMed] [Google Scholar]
- 3.Criddle LM, 5-year survival of geriatric patients following trauma center discharge. Adv Emerg Nurs J, 2009. 31(4): p. 323–36. [DOI] [PubMed] [Google Scholar]
- 4.Dunham CM, et al. , Geriatric preinjury activities of daily living function is associated with glasgow coma score and discharge disposition: a retrospective, consecutive cohort study. J Trauma Nurs, 2015. 22(1): p. 6–13. [DOI] [PubMed] [Google Scholar]
- 5.James MK, et al. , Clinical and non-clinical factors that predict discharge disposition after a fall. Injury, 2018. 49(5): p. 975–982. [DOI] [PubMed] [Google Scholar]
- 6.Deakin DE, Wenn RT, and Moran CG, Factors influencing discharge location following hip fracture. Injury, 2008. 39(2): p. 213–8. [DOI] [PubMed] [Google Scholar]
- 7.Hagino T, et al. , Prognostic prediction in patients with hip fracture: risk factors predicting difficulties with discharge to own home. J Orthop Traumatol, 2011. 12(2): p. 77–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Katz S, et al. , STUDIES OF ILLNESS IN THE AGED. THE INDEX OF ADL: A STANDARDIZED MEASURE OF BIOLOGICAL AND PSYCHOSOCIAL FUNCTION. Jama, 1963. 185: p. 914–9. [DOI] [PubMed] [Google Scholar]
- 9.Hartigan I, A comparative review of the Katz ADL and the Barthel Index in assessing the activities of daily living of older people. Int J Older People Nurs, 2007. 2(3): p. 204–12. [DOI] [PubMed] [Google Scholar]
- 10.Ortiz D, et al. , A trauma medical home, evaluating collaborative care for the older injured patient: study protocol for a randomized controlled trial. Trials, 2020. 21(1): p. 655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kroenke K, Spitzer RL, and Williams JB, The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med, 2001. 16(9): p. 606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spitzer RL, et al. , A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med, 2006. 166(10): p. 1092–7. [DOI] [PubMed] [Google Scholar]
- 13.Beaulieu RA, et al. , Predictive factors and models for trauma patient disposition. J Surg Res, 2014. 190(1): p. 264–9. [DOI] [PubMed] [Google Scholar]
- 14.Khorgami Z, et al. , Predictors of discharge destination in patients with major traumatic injury: Analysis of Oklahoma Trauma Registry. Am J Surg, 2019. 218(3): p. 496–500. [DOI] [PubMed] [Google Scholar]
- 15.Konda SR, et al. , Marriage Status Predicts Hospital Outcomes Following Orthopedic Trauma. Geriatr Orthop Surg Rehabil, 2020. 11: p. 2151459319898648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brosseau L, et al. , Post-stroke inpatient rehabilitation. II. Predicting discharge disposition. Am J Phys Med Rehabil, 1996. 75(6): p. 431–6. [DOI] [PubMed] [Google Scholar]
- 17.Farrell RT, Bennett BK, and Gamelli RL, An analysis of social support and insurance on discharge disposition and functional outcomes in patients with acute burns. J Burn Care Res, 2010. 31(3): p. 385–92. [DOI] [PubMed] [Google Scholar]
- 18.Englum BR, et al. , Association Between Insurance Status and Hospital Length of Stay Following Trauma. Am Surg, 2016. 82(3): p. 281–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mummaneni PV, et al. , Predictors of nonroutine discharge among patients undergoing surgery for grade I spondylolisthesis: insights from the Quality Outcomes Database. J Neurosurg Spine, 2019: p. 1–10. [DOI] [PubMed]
- 20.Rondon AJ, et al. , Who Goes to Inpatient Rehabilitation or Skilled Nursing Facilities Unexpectedly Following Total Knee Arthroplasty? J Arthroplasty, 2018. 33(5): p. 1348–1351.e1. [DOI] [PubMed] [Google Scholar]
- 21.Altemus M, Sarvaiya N, and Neill Epperson C, Sex differences in anxiety and depression clinical perspectives. Front Neuroendocrinol, 2014. 35(3): p. 320–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Simonds VM and Whiffen VE, Are gender differences in depression explained by gender differences in co-morbid anxiety? J Affect Disord, 2003. 77(3): p. 197–202. [DOI] [PubMed] [Google Scholar]
- 23.Balentine CJ, et al. , Depression is associated with prolonged and complicated recovery following colorectal surgery. J Gastrointest Surg, 2011. 15(10): p. 1712–7. [DOI] [PubMed] [Google Scholar]
- 24.Brandel MG, et al. , The Association between Psychiatric Comorbidities and Outcomes for Inpatients with Traumatic Brain Injury. J Neurotrauma, 2017. 34(5): p. 1005–1016. [DOI] [PubMed] [Google Scholar]
- 25.Haupt E, et al. , Pre-injury depression and anxiety in patients with orthopedic trauma and their treatment. Injury, 2018. 49(6): p. 1079–1084. [DOI] [PubMed] [Google Scholar]
- 26.Lewis FD and Horn GJ, Depression following traumatic brain injury: Impact on post-hospital residential rehabilitation outcomes. NeuroRehabilitation, 2017. 40(3): p. 401–410. [DOI] [PubMed] [Google Scholar]
- 27.Gadomski AM, et al. , Effectiveness of an inpatient smoking cessation program. J Hosp Med, 2011. 6(1): p. E1–8. [DOI] [PubMed] [Google Scholar]
- 28.Lee D, Lee YR, and Oh IH, Cost-effectiveness of smoking cessation programs for hospitalized patients: a systematic review. Eur J Health Econ, 2019. 20(9): p. 1409–1424. [DOI] [PubMed] [Google Scholar]
- 29.Fox MT, et al. , Effectiveness of early discharge planning in acutely ill or injured hospitalized older adults: a systematic review and meta-analysis. BMC Geriatr, 2013. 13: p. 70. [DOI] [PMC free article] [PubMed] [Google Scholar]


