Abstract
Background
The aim of the study was to evaluate the clinical and diagnostic findings, treatment, and follow-up of cases of anomalous origin of coronary arteries from the pulmonary artery.
Methods
Between January 1998 and June 2021, a total of 14 patients (5 males, 9 females; median age: 15 months; range, 3 to 156 months) diagnosed with anomalous origin of coronary arteries from the pulmonary artery were retrospectively analyzed. Demographic and clinical data of the patients, electrocardiographic, echocardiographic, angiographic, surgical, and follow-up findings were evaluated.
Results
The most common symptoms were respiratory distress (n=6) and murmur (n=3). With the exception of three cases, all other patients were diagnosed by echocardiography in the first examination. Severe mitral valve insufficiency was detected in four patients and four other patients had moderate mitral insufficiency on echocardiography. Ejection fraction values ranged between 38 and 79%. Eleven patients underwent direct implantation of the coronary artery into the aorta, and three underwent a Takeuchi procedure. Mortality occurred in only one case. After surgery, mitral insufficiency and ejection fraction values improved. Median follow-up was 62 (range, 5 to 170) months and all patients were asymptomatic, except one who required redo surgery.
Conclusion
Anomalous origin of the coronary arteries from the pulmonary artery is an uncommon congenital anomaly. Echocardiography is the main diagnostic tool. If all echocardiographic findings of the coronary anomaly are not investigated thoroughly, the diagnosis may be overlooked.
Keywords: Anomalous origin of the coronary arteries from the pulmonary artery, congenital coronary abnormality, echocardiography, surgery
Introduction
Anomalous origin of coronary arteries from the pulmonary artery (ACAPA) accounts for approximately 0.01% of the cases in a large series of patients undergoing coronary angiography. The majority of cases are of anomalous left coronary artery origin from the pulmonary artery (ALCAPA), while cases of anomalous right coronary artery origin from the pulmonary artery (ARCAPA) are rarely seen.[1,2] The time of onset and severity of symptoms depends on the type of anomaly, the direction of blood flow in the anomalous vessel, and the extent of collateralization. Although some patients may be completely asymptomatic and survive to adulthood, approximately 90% of them die suddenly at a mean age of 35 years. Others may develop early mortality due to heart failure, valvular insufficiencies, or myocardial infarction.
Neonatal ALCAPA patients are largely asymptomatic due to the high pulmonary arterial pressure during this period. During the first months of life when the pulmonary vascular resistance declines, the left coronary artery (LCA) changes to a retrograde flow with collaterals from the right coronary artery (RCA). Coronary steal from the LCA to the pulmonary artery leads to myocardial ischemia and, consequently, symptoms may develop. Early diagnosis and surgical intervention are critical, as the mortality rate in children who are symptomatic in infancy with late diagnosis and treatment can exceed 90%, particularly in the first year of life.[3] Transthoracic echocardiography serves as a non-invasive method for the diagnosis of ACAPA. Therefore, clinicians, particularly echocardiographers, should have a comprehensive understanding of the echocardiographic manifestations of this abnormality to reduce misdiagnoses and missed diagnoses.[4]
In the present study, we aimed to discuss the management of children with ACAPA based on our single-center experience.
Patients and Methods
This single-center, retrospective study was conducted at Çukurova University Faculty of Medicine, Department of Pediatric Cardiology between January 1998 and June 2021. The hospital database was searched to identify all patients diagnosed with ALCAPA and ARCAPA. A total of 14 patients (5 males, 9 females; median age: 15 months; range, 3 to 156 months) were included. Exclusion criteria were as follows: Patients whose full clinical and surgical data could not be obtained. Demographic data of the patients, including age, sex, presentation type, initial diagnosis, and electrocardiography (ECG), echocardiography, cardiac catheterization, and angiographic finding were evaluated. The surgical findings, outpatient clinic follow-up, and echocardiography results were assessed. Two-dimensional, M-mode, and Doppler echocardiography were performed using standard imaging techniques in accordance with the recommendations of the American Society of Echocardiography (ASE). All ECGs were evaluated for the presence of pathological Q wave, ST elevation, and ST depression.
Other data from the coronary angiography study were also recorded. Coronary artery angiography was performed in all patients, if a diagnosis of ACAPA was suspected on transthoracic echocardiography.
Statistical analysis
Statistical analysis was performed using the SPSS for Windows version 15.0 software (SPSS Inc., Chicago, IL, USA). Continuous data were presented in mean ± standard deviation (SD) or median (min-max), while categorical variables were presented in number and frequency.
Results
Clinical presentation
Of a total of 14 patients, 12 had ALCAPA and two had ARCAPA. The median weight was 9 (range, 3 to 32) kg. The most common complaint in the patients with ALCAPA was respiratory distress (n=6). Three patients were presented with a murmur, one with palpitation, one with chest pain, and one with fatigue. One patient with ALCAPA underwent mitral valve surgery at an external center at the age of 3 years, but anomalous LCA was not noticed. This patient was admitted at the age of 13 years with the complaint of fatigue related to severe mitral insufficiency and was diagnosed with ALCAPA. Two patients with ARCAPA were diagnosed at the age of 5 and 5.5 years, respectively. One of these patients was previously hospitalized due to ventricular septal defect (VSD)-related heart failure, but was subsequently diagnosed with ARCAPA with the identification of septal collaterals. The other patient had an atrial septal defect (ASD) which was closed with a transcatheter device. Meanwhile, ARCAPA was not noticed. In subsequent echocardiographic follow-ups, an abnormality was suspected, as septal collaterals were identified. The diagnosis was confirmed by angiography in both patients. The demographic, clinical, and imaging data are presented in Table 1.
Table 1. Demographic, clinical, and imaging characteristics of ACAPA patients.
| Patient no | Sex/age (months/years) |
Symptoms | Electrocardiography | Echocardiography |
| 1 | M/8 years | Chest pain | ST depression in V6 | EF: 70%, LVEDd Z score: 0.35 RCA/AA >1.4, ICC: +, MR: No, PMH: -, RDF+ |
| 2 | F/9.5 years | Murmur | ALMI | EF: 67%, LVEDd Z score: 1.7 RCA/AA >1.4, ICC: +, PMH: - MR: moderate, RDF: + |
| 3t | M/13 years | Fatigue | T negativity in aVL, V1-V3 Left anterior hemiblock |
EF: 66%, LVEDd Z score: 2.7 ICC: +, PMH: - MR: Severe, RDF: + |
| 4 | F/5 months | Respiratory distress | ALMI | EF: 54%, LVEDd Z score: 7.3 MR: Mild, PMH: +, ICC: + |
| 5* | F/5 years | No symptoms (during diagnosis; VSD, follow-up) |
Normal | EF: 75% LVEDd Z score: -0.6 LCA/AA >1.3, ICC: +, VSD |
| 6 | F/3 months | Respiratory distress, diaphoresis, failure to thrive | ALMI | EF: 40% LVEDd Z score: 4.2 MR: Severe, ICC: + PMH: +, RDF: +, RCA/AA >1.4 |
| 7 | F/6 months | Respiratory distress, decreased oral intake, diaphoresis, failure to thrive | ALMI | EF: 56% LVDDd Z score: 1.1 MR: Severe, ICC: +, PMH: + |
| 8 | F/7 months | Shortness of breath, diaphoresis, failure to thrive | ALMI | EF: 38% LVEDd Z score: 4.5 PMH: +, MR:severe, RDF |
| 9* | M/5.5 years | No symptoms (during diagnosis ASD follow-up) |
Incomplete RBBB, T negativity in V1-4 | EF: 79% LVEDd Z score: -0.5 ICC: +, RDF: +, ASD |
| 10 | M/2.5 years | Respiratory distress, | ALMI | EF: 60%, LVEDd Z score: 3.3 MR: Mild RCA/AA >1.4, PMH: +, ICC: + |
| 11 | F/9 months | Respiratory distress, diaphoresis, failure to thrive | ALMI | EF: 64% LVEDd Z score: 2.8 MR: Moderate, PMH: + ICC: +, RDF: + RCA/AA >1.4 |
| 12 | F/3 months | Respiratory distress, diaphoresis, failure to thrive | ALMI | EF: 44% LVEDd Z score: 5 MR: Moderate, PMH: + ICC: -, RDF: + RCA/AA >1.4 |
| 13 | F/15 months | Murmur | ALMI | EF: 64% LVEDd Z score: 3.3 MR: Mild, ICC: + RCA/AA >1.4, PMH: - |
| 14 | M/2 years | Palpitation | ALMI | EF: 59% LVDD Z score: 5.3 MR: Moderate, PMH: + ICC: +, RCA/AA >1.4 |
| ACAPA: Anomalous origin of coronary artery from the pulmonary artery; EF: Ejection fraction; LVEDd: Left Ventricular End Diastolic Diameter; RCA: Right coronary artery; AA: Aorta artery; ICC: Intercoronary septal collaterals; MR: Mitral regurgitation; PMH: Papillary muscle hyperechogenicity; RDF: Reverse Doppler flow; ALMI: Anterolateral myocardial infarction; LCA: Left coronary artery; VSD: Ventricular septal defect; ASD: Atrial septal defect; RBBB: Right bundle branch block; ARCAPA: Anomalous right coronary artery origin from the pulmonary artery; † This patient had mitral valve surgery at the age of 3 years; * ARCAPA patients. | ||||
Electrocardiography and echocardiographic findings
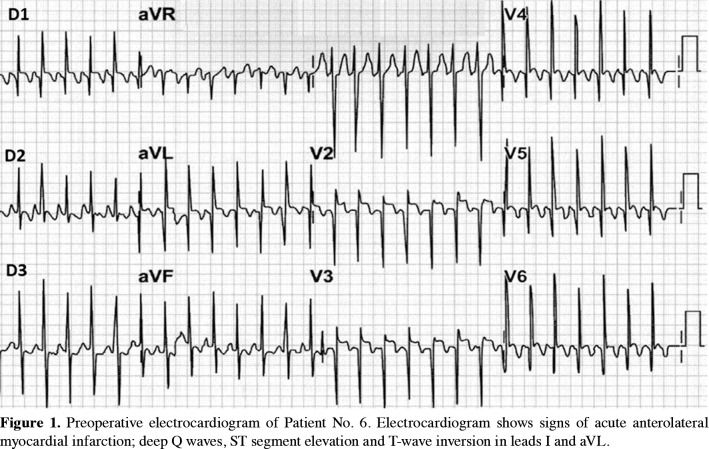
The ECGs of 10 ALCAPA patients showed a deep Q wave in the DI, aVL, and V6 leads (anterolateral myocardial infarction) (Figure 1). One patient had T negativity in aVL and left anterior hemiblock, which was probably related to previous mitral valve surgery. One ALCAPA patient had normal ECG findings. One of the patients with ARCAPA who also had ASD had an incomplete right bundle branch block, and one had normal ECG findings during diagnosis.
Figure 1. Preoperative electrocardiogram of Patient No. 6. Electrocardiogram shows signs of acute anterolateral myocardial infarction; deep Q waves, ST segment elevation and T-wave inversion in leads I and aVL.
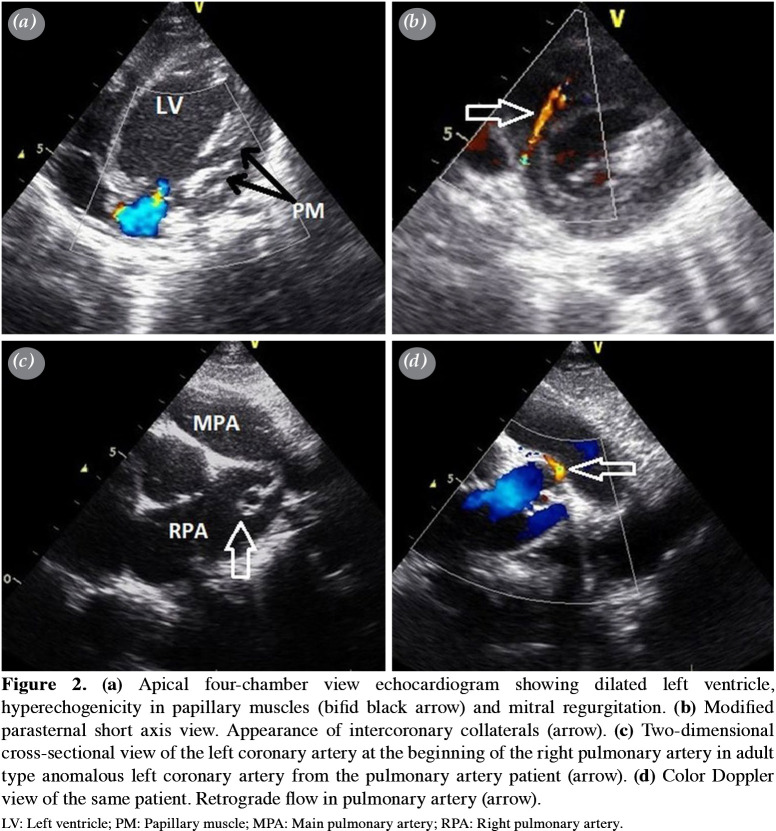
The echocardiographic features of the ALCAPA patients (n=12) showed abnormal left coronary ostium arising from the pulmonary trunk with retrograde coronary artery flow in seven patients, enlargement of the RCA in seven patients, intercoronary septal collaterals in 10 patients, papillary muscle hyperechogenicity in eight patients, moderateto- severe mitral regurgitation in eight patients, left ventricle dilatation in nine patients, and left ventricle systolic dysfunction in six patients (Figure 2). In the initial echocardiographic examination, one patient was misdiagnosed with myocarditis. This patient had mild mitral regurgitation and mild left ventricle systolic dysfunction. Coronary anomaly was not detected in the first examinations in both patients with ARCAPA. The diagnosis of ARCAPA was established during control echocardiographic studies by the detection of septal collaterals in both patients, as well as the LCA enlargement in one patient and the retrograde flow into the pulmonary artery in the other.
Figure 2. (a) Apical four-chamber view echocardiogram showing dilated left ventricle, hyperechogenicity in papillary muscles (bifid black arrow) and mitral regurgitation. (b) Modified parasternal short axis view. Appearance of intercoronary collaterals (arrow). (c) Two-dimensional cross-sectional view of the left coronary artery at the beginning of the right pulmonary artery in adult type anomalous left coronary artery from the pulmonary artery patient (arrow). (d) Color Doppler view of the same patient. Retrograde flow in pulmonary artery (arrow). LV: Left ventricle; PM: Papillary muscle; MPA: Main pulmonary artery; RPA: Right pulmonary artery.
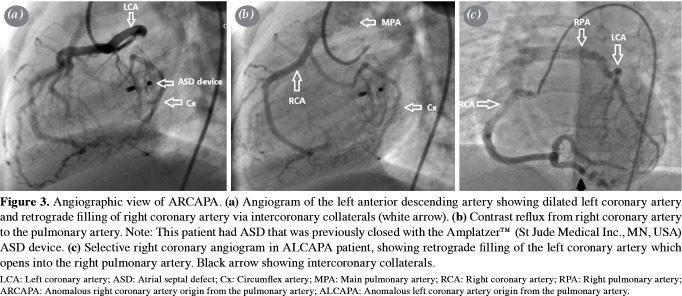
All patients were evaluated with cardiac catheterization and angiography. Catheter angiography was previously performed in one patient with ALCAPA, but was incorrectly considered to be a single coronary root. Selective coronary angiography was not performed on angiography. In this patient, angiography was performed again one month later due to continuing suspicion of anomalous LCA, and the diagnosis was confirmed (Patient No. 7). In the ARCAPA patient with previous ASD closure, the circumflex artery (Cx) also emerged from the RCA. Left ventricular systolic functions were normal in this patient (Figures 3a, b).
Figure 3. Angiographic view of ARCAPA. (a) Angiogram of the left anterior descending artery showing dilated left coronary artery and retrograde filling of right coronary artery via intercoronary collaterals (white arrow). (b) Contrast reflux from right coronary artery to the pulmonary artery. Note: This patient had ASD that was previously closed with the AmplatzerTM (St Jude Medical Inc., MN, USA) ASD device. (c) Selective right coronary angiogram in ALCAPA patient, showing retrograde filling of the left coronary artery which opens into the right pulmonary artery. Black arrow showing intercoronary collaterals. LCA: Left coronary artery; ASD: Atrial septal defect; Cx: Circumflex artery; MPA: Main pulmonary artery; RCA: Right coronary artery; RPA: Right pulmonary artery; ARCAPA: Anomalous right coronary artery origin from the pulmonary artery; ALCAPA: Anomalous left coronary artery origin from the pulmonary artery.LV: Left ventricle; PM: Papillary muscle; MPA: Main pulmonary artery; RPA: Right pulmonary artery.
All ACAPA patients underwent surgery. Of the ALCAPA patients, 10 had LCA arising from Sinus 1, from the non-facing sinus in one, and from the right pulmonary artery in one (Figure 3c). Two ARCAPA patients had RCA arising from Sinus 2. In nine cases with left and two with right anomalous coronary arteries origin from the pulmonary artery, direct implantation of the coronary artery into the aorta was performed. Three ALCAPA patients underwent tubular aortic anastomosis (Takeuchi technique). In five ALCAPA patients with moderate-to-severe mitral regurgitation, concomitant mitral valve plasty was performed. Mitral valve replacement was performed in the patient who previously had mitral valve repair in another center (Patient No. 3). One patient with moderate-to-severe left ventricular dysfunction and severe mitral regurgitation died in the early postoperative period. In this patient, there was postoperative low cardiac output that required extracorporeal membrane oxygenation, and the patient died two days later in the intensive care unit.
Follow-up
The median follow-up duration was 62 (range, 5 to 170) months for the entire cohort. At the end of the first month after coronary revascularization, the mean left ventricle ejection fraction (EF) in ALCAPA patients improved (60.7±6.2%, range 52 to 71%) compared to the preoperative EF values (56.8±10.8%, range 38 to 70%) (p<0.01). At six months, left ventricle EF was normal in all the ALCAPA patients (64.8±4.3%, range 58 to 72%). In four ALCAPA patients who underwent Holter ECG during follow-up, no arrhythmias were detected.
One ALCAPA patient developed severe pulmonary stenosis following the Takeuchi procedure and, therefore, pulmonary patch plasty was performed two years after the first operation. The most recent echocardiographic evaluations showed mild mitral valve regurgitation in six patients and moderate regurgitation in one. With the exception of the patient who died, 12 patients were categorized as New York Heart Association (NHYA) Class I at the postoperative follow-up examination. One ALCAPA patient who required reoperation due to pulmonary stenosis was categorized as NYHA Class II. The surgical and follow-up data are presented in Table 2.
Table 2. Surgical and follow-up characteristics of ACAPA patients (n=14).
| n | Mean±SD Median | Range | |
| Surgical method | |||
| Direct re-implantation | 11 | ||
| Takeuchi repair | 3 | ||
| Concomitant mitral repair/replacement | 5 | ||
| Mortality | 1 | ||
| Follow-up EF | |||
| At postoperative first month | 60.7+6.2% | 52-71 | |
| At postoperative sixth month | 64.8+4.3% | 58-72 | |
| Postoperative MR> moderate | 2 | ||
| Follow-up duration (month) | 62 | 5-170 | |
| Reoperation | 1 | ||
| NHYA classification | |||
| I | 12 | ||
| II | 1 | ||
| III | None | ||
| IV | None | ||
| ACAPA: Anomalous origin of coronary artery from the pulmonary artery; SD: Standard deviation; EF: Ejection fraction; MR: Mitral regurgitation; NYHA: New York Heart Association. | |||
Discussion
Anomalous origin coronary arteries from the pulmonary artery are life-threatening due to consequential conditions such as coronary ischemia, heart failure, and even sudden cardiac death.[5] Many infant patients present with symptoms of congestive heart failure. If not operated timely, the majority of these patients die within the first year of life.[6,7] In the present study, all patients diagnosed during infancy presented with heart failure symptoms. Approximately 10 to 15% of ALCAPA patients are diagnosed after infancy.[4] In our study, this rate was 25%. Thanks to recent advances in noninvasive cardiac imaging, there has been a substantial increase in the number of adults diagnosed with the syndrome. Their survival is due to a large dominant RCA with extensive intercoronary collaterals, as well as a restrictive opening between ALCAPA and the pulmonary artery. With subclinical myocardial ischemia, these patients may remain asymptomatic until adulthood. However, when coronary steal syndrome occurs or collaterals are narrowed, these patients may show symptoms or sudden death.[8,9] Yau et al.[10] reported that 66% of 151 adult ALCAPA cases presented with symptoms of angina, shortness of breath or fatigue, 17% with arrhythmia, syncope or sudden death. In the current study, three of six patients diagnosed after infancy were symptomatic and three were asymptomatic.
While most patients with ARCAPA are asymptomatic, a minority may be symptomatic with symptoms of murmur, angina, shortness of breath on exertion, and congestive heart failure.[11,12] Some authors have attributed this to the lower oxygen demand of the right ventricle.[2] The detection of this anomaly is usually incidental. In the literature, only one case has been reported in which both RCA and Cx originated from the pulmonary artery.[13] In that case, left ventricular EF was normal, as in the current case. In two patients, ARCAPA was not suspected in the initial evaluations in this study. Coronary anomalies may have been overlooked, probably due to the lack of careful examination with more focus on existing cardiac pathologies. Williams et al.[2] reported that, of 70 patients described in published literature, 34 presented with a murmur. Anomalous right coronary artery origin from the pulmonary artery is associated with other congenital heart anomalies in about 35 to 50% of cases.[2] One of t he current study cases had ASD and one had VSD.
Electrocardiogram in ALCAPA patients almost always shows evidence of anterolateral myocardial infarction in symptomatic patients. In patients with extensive collateral, there may be non-specific ECG changes. Rodriguez-Gonzalez et al.[14] conducted a study of 12 patients and reported that six had specific ECG changes compatible with lateral myocardial infarction. Electrocardiography in ARCAPA may be normal. In this study, the ECG examinations revealed anterolateral myocardial infarction in 10 ALCAPA patients.
Echocardiography is used as the first imaging modality in ACAPA patients. The anomalous exit origin of LCA from the pulmonary artery may not always be possible to demonstrate on echocardiography. Patel et al.[15] reported that the origins of the coronary arteries were clearly visualized in only 54% of cases. In this study, the origins of the abnormal coronary artery could be clearly demonstrated in 57% of the patients. Left ventricular systolic dysfunction and papillary muscle hyperechogenicity were identified as the most common echocardiographic findings in patients who were diagnosed during infancy, while in patients diagnosed after infancy, abundant intercoronary septal collaterals were the most prominent finding. The same findings have been shown in previous studies.[4,16] A nomalous l eft coronary artery origin from the pulmonary artery has a higher rate of false initial diagnosis.[17,18] There are few reports of cases in which ALCAPA was misdiagnosed as cardiomyopathy.[19] A false-negative finding of ALCAPA was also described by Patel et al.[15] In the present study, one patient with ALCAPA and two with ARCAPA were diagnosed with normal coronary artery patterns in the initial examination. One patient with ALCAPA was previously operated at an external center for severe mitral regurgitation, and the anomalous LCA was unable to be detected. Falsenegative misdiagnoses in the first examination were made at a rate of 21% in the current study. However, considering the subsequent follow-ups, a diagnosis could be made from echocardiography in all cases.
Most recent literature supports the accuracy of echocardiography, but usually, the diagnosis is confirmed by angiography and/or computed tomography (CT) and magnetic resonance imaging (MRI).[14,15,18-22] Of note, a poor acoustic image window may be a limitation for echocardiographic evaluation. Invasive coronary angiography remains the gold standard for ALCAPA diagnosis.[20] If selective coronary angiography is not performed, the diagnosis may be sometimes overlooked, as in Patient No. 7. Coronary angiography is not usually required currently; however, it is usually reserved for questionable cases. The CT or MRI imaging is usually preferred, particularly CT, as it is less invasive and highly accurate in coronary imaging.
Mitral regurgitation in ALCAPA can be functional, secondary to a dilated left ventricle or the result of papillary muscle ischemia and fibrosis. An intervention to the mitral valve during the first surgery in patients who are symptomatic during infancy is usually not recommended, as postoperative ventricular remodeling and mitral regurgitation are likely to improve with reperfusion.[23,24] Kanoh et al.[25] performed concomitant mitral annuloplasty in approximately 80% of ALCAPA patients with moderate-to-severe mitral insufficiency. In the present study, five ALCAPA patients needed mitral valve repair. A 13-year-old boy (Patient No. 3) with previous mitral valve repair underwent mitral valve replacement. During follow-up, four of these patients had mild mitral insufficiency, while one did not.
The prognosis of ACAPA depends on early diagnosis and successful cardiac surgery. Surgery is the only definitive treatment for ALCAPA, even in asymptomatic patients. Different surgical techniques have been employed including ligation of the LCA and coronary artery bypass grafting, re-implantation of the LCA to the aorta, and the Takeuchi procedure, which involves using an aortopulmonary window to create an intrapulmonary tunnel to connect the anomalous ostium to the aorta.[25-27] Ligation of RCA or LCA condemns the patient to a single coronary system, which can be considered inappropriate for the life expectancy for pediatric patients. The preferred method is direct re-implantation of the LCA to the aorta. If direct re-implantation is not possible, Takeuchi repair can be performed. In this study, two of the three patients who underwent Takeuchi repair were in the first 10 years of our experience. In the third patient in whom the Takeuchi procedure was performed, the LCA arose far from the aorta. Cardiac function improvements have been reported to be more prominent in patients diagnosed during infancy, as the reversibility of the constrictive myocardium after revascularization is higher than in adults.[24-26,29] It has b een reported t hat adult patients experience more frequent cardiovascular events after surgical correction due to preoperative long-term cardiac ischemia.[25]
Overall mortality after dual coronary system repair has been reported from several patient series, ranging from 0 to 17%.[30,31] In the present study, the mortality rate in the ALCAPA group was 8.3%. Different degrees of pulmonary stenosis can be found after Takeuchi repair. In the current study, one ALCAPA patient with Takeuchi repair required reoperation due to severe pulmonary stenosis. Regardless of the technique applied, during the follow-up period, all surviving patients had wellpreserved heart function.
As adverse outcomes including the increased risk for myocardial infarction and sudden cardiac death have been described in ARCAPA patients regardless of previous symptoms, surgical correction is recommended whenever this anomaly is diagnosed. In patients diagnosed incidentally, elective repair is mostly advocated to avoid development of cardiac dysfunction associated with the systemic to pulmonary shunt, as well as to establish a dusal coronary artery system. A review of published ARCAPA cases confirmed that this approach was adopted in almost 90% of asymptomatic patients.[32] Surgical correction of ARCAPA is associated with low operative mortality rates, ranging from 2 to 3%.[4,33]
Nonetheless, this study has certain limitations inherent to the retrospective design and small sample size. The fact that different surgeons performed these surgeries over a period of approximately 30 years, and the developments in different surgical techniques and perioperative care techniques at different times are among the limitations. Postoperative left ventricular systolic function was within a normal range almost in all ACAPA patients. However, there was no evaluation of the postoperative condition of myocardial damage as a consequence of long-term preoperative chronic ischemia, which causes cardiovascular events and cardiac dysfunction after revascularization.
In conclusion, different clinical conditions, postoperative course, long-term complications, difficulties in diagnosis are discussed in this study. Moreover, an unusual case is presented of isolated anomalous origin of both the right coronary artery and circumflex artery from the pulmonary artery. Our study results show that patients with anomalous origin of coronary arteries from the pulmonary artery who survive the perioperative period have a good prognosis. Although anomalous origin of coronary arteries from the pulmonary artery is a rare congenital abnormality, clinicians should pay attention to patients with coronary artery enlargement, interventricular coronary interaction, retrograde flow in the left or right coronary artery, and papillary muscle hyperechogenicity in anomalous left coronary artery origin from the pulmonary artery should raise suspicion of anomalous origin of coronary arteries from the pulmonary artery which can be confirmed by other diagnostic modalities. Anomalous left coronary artery origin from the pulmonary artery should be also excluded in patients with mitral regurgitation and dilated cardiomyopathy in infancy. Aortic implantation can be performed in almost all patients. If required, concomitant mitral valve repair can be also performed during surgery.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Author Contributions: Idea/concept: F.D, T.A.; Design: F.D., T.A., S.E.; Control/supervision: F.D., B.S., C.V., N.Ö.; Data collection and/or processing: F.D., T.A., N.Ö.; Analysis and/or interpretation: F.D., O.K.S., S.E., N.Ö.; Literature review: F.D., T.A., B.S.; Writing the article: F.D., T.A.; Critical review: O.K.S., N.Ö., C.V.; References and fundings: F.D., T.A., S.E.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1.Lange R, Vogt M, Hörer J, Cleuziou J, Menzel A, Holper K, et al. Long-term results of repair of anomalous origin of the left coronary artery from the pulmonary artery. Ann Thorac Surg. 2007;83:1463–1471. doi: 10.1016/j.athoracsur.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 2.Williams IA, Gersony WM, Hellenbrand WE. Anomalous right coronary artery arising from the pulmonary artery: A report of 7 cases and a review of the literature. Am Heart J. 2006;152:1004–1004. doi: 10.1016/j.ahj.2006.07.023. [DOI] [PubMed] [Google Scholar]
- 3.Hauser M. Congenital anomalies of the coronary arteries. Heart. 2005;91:1240–1245. doi: 10.1136/hrt.2004.057299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yuan XC, Hu J, Zeng X, Zhou AY, Chen L. Echocardiographic diagnosis of anomalous origin of the left coronary artery from the pulmonary artery. e18046Medicine (Baltimore) 2019;98 doi: 10.1097/MD.0000000000018046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Edwards JE. The direction of blood flow in coronary arteries arising from the pulmonary trunk. Circulation. 1964;29:163–166. doi: 10.1161/01.CIR.29.2.163. [DOI] [PubMed] [Google Scholar]
- 6.Schneider T, Rickli H, Gliech V, Maeder M. Bland-White- Garland syndrome and atrial septal defect - rare association and diagnostic challenge. Clin Res Cardiol. 2006;95:295–300. doi: 10.1007/s00392-006-0369-8. [DOI] [PubMed] [Google Scholar]
- 7.Koestenberger M, Nagel B, Gamillscheg A, Temmel W, Cvirn G, Beitzke A. Myocardial infarction in an adolescent: Anomalous origin of the left main coronary artery from the right coronary sinus in association with combined prothrombotic defects. e424-7Pediatrics. 2007;120 doi: 10.1542/peds.2006-3181. [DOI] [PubMed] [Google Scholar]
- 8.Wilson CL, Dlabal PW, Holeyfield RW, Akins CW, Knauf DG. Anomalous origin of left coronary artery from pulmonary artery. Case report and review of literature concerning teen-agers and adults. J Thorac Cardiovasc Surg. 1977;73:887–893. doi: 10.1016/S0022-5223(19)41448-7. [DOI] [PubMed] [Google Scholar]
- 9.Singh TP, Di Carli MF, Sullivan NM, Leonen MF, Morrow WR. Myocardial flow reserve in long-term survivors of repair of anomalous left coronary artery from pulmonary artery. J Am Coll Cardiol. 1998;31:437–443. doi: 10.1016/S0735-1097(97)00488-9. [DOI] [PubMed] [Google Scholar]
- 10.Yau JM, Singh R, Halpern EJ, Fischman D. Anomalous origin of the left coronary artery from the pulmonary artery in adults: A comprehensive review of 151 adult cases and a new diagnosis in a 53-year-old woman. Clin Cardiol. 2011;34:204–210. doi: 10.1002/clc.20848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burakovskiĭ VI, Sharykin AS, Garibian VA. Anomalous derivation of the right coronary artery from the pulmonary artery with an interventricular septal defect. Grudn Khir. 1981;(2):5–10. [PubMed] [Google Scholar]
- 12.Burroughs JT, Schmutzer KJ, Linder F, Neuhaus G. Anomalous origin of the right coronary artery with a orticopulmonary window and ventricular septal defect. Report of a case with complete operative correction. J Cardiovasc Surg (Torino) 1962;3:142–147. [PubMed] [Google Scholar]
- 13.Luciani GB, Vendrametto F, Barozzi L, Oberhollenzer R, Pitscheider W, Mazzucco A. Repair of anomalous right and circumflex coronary arteries arising from the pulmonary artery. J Thorac Cardiovasc Surg. 2006;132:970–972. doi: 10.1016/j.jtcvs.2006.05.053. [DOI] [PubMed] [Google Scholar]
- 14.Rodriguez-Gonzalez M, Tirado AM, Hosseinpour R, de Soto JS. Anomalous origin of the left coronary artery from the pulmonary artery: Diagnoses and surgical results in 12 pediatric patients. Tex Heart Inst J. 2015;42:350–356. doi: 10.14503/THIJ-13-3849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patel SG, Frommelt MA, Frommelt PC, Kutty S, Cramer JW. Echocardiographic diagnosis, surgical treatment, and outcomes of anomalous left coronary artery from the pulmonary artery. J Am Soc Echocardiogr. 2017;30:896–903. doi: 10.1016/j.echo.2017.05.005. [DOI] [PubMed] [Google Scholar]
- 16.Molaei A, Rastkar Hemmati B, Khosroshahi H, Malaki M, Zakeri R. Misdiagnosis of bland-white-garland syndrome: Report of two cases with different presentations. J Cardiovasc Thorac Res. 2014;6:65–67. doi: 10.5681/jcvtr.2014.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levitas A, Krymko H, Ioffe V, Zalzstein E, Broides A. Anomalous left coronary artery from the pulmonary artery in infants and toddlers misdiagnosed as myocarditis. Pediatr Emerg Care. 2016;32:232–234. doi: 10.1097/PEC.0000000000000511. [DOI] [PubMed] [Google Scholar]
- 18.Ma F, Zhou K, Shi X, Wang X, Zhang Y, Li Y, et al. Misdiagnosed anomalous left coronary artery from the pulmonary artery as endocardial fibroelastosis in infancy: A case series. e7199Medicine (Baltimore) 2017;96 doi: 10.1097/MD.0000000000007199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ben Ali W, Metton O, Roubertie F, Pouard P, Sidi D, Raisky O, et al. Anomalous origin of the left coronary artery from the pulmonary artery: Late results with special attention to the mitral valve. Eur J Cardiothorac Surg. 2009;36:244–248. doi: 10.1016/j.ejcts.2009.03.014. [DOI] [PubMed] [Google Scholar]
- 20.Sun Z, Lin C, Davidson R, Dong C, Liao Y. Diagnostic value of 64-slice CT angiography in coronary artery disease: A systematic review. Eur J Radiol. 2008;67:78–84. doi: 10.1016/j.ejrad.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 21.Peña E, Nguyen ET, Merchant N, Dennie C. ALCAPA syndrome: Not just a pediatric disease. Radiographics. 2009;29:553–565. doi: 10.1148/rg.292085059. [DOI] [PubMed] [Google Scholar]
- 22.Li RJ, Sun Z, Yang J, Yang Y, Li YJ, Leng ZT, et al. Diagnostic value of transthoracic echocardiography in patients with anomalous origin of the left coronary artery from the pulmonary artery. e3401Medicine (Baltimore) 2016;95 doi: 10.1097/MD.0000000000003401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang Y, Wang Z, Fang M, Jin Y, Liu Y, Han J, et al. Aortic implantation for anomalous connection of the coronary artery to the pulmonary artery in older children and adults. Thorac Cardiovasc Surg. 2017;65:18–25. doi: 10.1055/s-0036-1571812. [DOI] [PubMed] [Google Scholar]
- 24.Sarıoğlu T, Yalçınbaş YK, Erek E, Arnaz A, Türkekul Y, Avşar MK, et al. Pulmoner arterden çıkan sol koroner arter anomalisi: İkili koroner sistemin restorasyonundan sonra sol ventrikül fonksiyonu ve klinik sonuçlar. Turk Gogus Kalp Dama. 2013;21:1–6. doi: 10.5606/tgkdc.dergisi.2013.5920. [DOI] [Google Scholar]
- 25.Kanoh M, Inai K, Shinohara T, Tomimatsu H, Nakanishi T. Outcomes from anomalous origin of the left coronary artery from the pulmonary artery repair: Long-term complications in relation to residual myocardial abnormalities. J Cardiol. 2017;70:498–503. doi: 10.1016/j.jjcc.2017.03.008. [DOI] [PubMed] [Google Scholar]
- 26.Takeuchi S, Imamura H, Katsumoto K, Hayashi I, Katohgi T, Yozu R, et al. New surgical method for repair of anomalous left coronary artery from pulmonary artery. J Thorac Cardiovasc Surg. 1979;78:7–11. doi: 10.1016/S0022-5223(19)38154-1. [DOI] [PubMed] [Google Scholar]
- 27.Dodge-Khatami A, Mavroudis C, Backer CL. Anomalous origin of the left coronary artery from the pulmonary artery: Collective review of surgical therapy. Ann Thorac Surg. 2002;74:946–955. doi: 10.1016/S0003-4975(02)03633-0. [DOI] [PubMed] [Google Scholar]
- 28.Jin Z, Berger F, Uhlemann F, Schröder C, Hetzer R, Alexi-Meskhishvili V, et al. Improvement in left ventricular dysfunction after aortic reimplantation in 11 consecutive paediatric patients with anomalous origin of the left coronary artery from the pulmonary artery. Early results of a serial echocardiographic follow-up. Eur Heart J. 1994;15:1044–1049. doi: 10.1093/oxfordjournals.eurheartj.a060626. [DOI] [PubMed] [Google Scholar]
- 29.Ojala T, Salminen J, Happonen JM, Pihkala J, Jokinen E, Sairanen H. Excellent functional result in children after correction of anomalous origin of left coronary artery from the pulmonary artery--a population-based complete follow- up study. Interact Cardiovasc Thorac Surg. 2010;10:70–75. doi: 10.1510/icvts.2009.209627. [DOI] [PubMed] [Google Scholar]
- 30.Isomatsu Y, Imai Y, Shin'oka T, Aoki M, Iwata Y. Surgical intervention for anomalous origin of the left coronary artery from the pulmonary artery: The Tokyo experience. J Thorac Cardiovasc Surg. 2001;121:792–797. doi: 10.1067/mtc.2001.112834. [DOI] [PubMed] [Google Scholar]
- 31.Kühn A, Kasnar-Samprec J, Schreiber C, Vogt M. Anomalous origin of the right coronary artery from the pulmonary artery (ARCAPA) e27-8Int J Cardiol. 2010;139 doi: 10.1016/j.ijcard.2008.10.036. [DOI] [PubMed] [Google Scholar]
- 32.Guenther TM, Sherazee EA, Wisneski AD, Gustafson JD, Wozniak CJ, Raff GW. Anomalous origin of the right coronary artery from the pulmonary artery: A systematic review. Ann Thorac Surg. 2020;110:1063–1071. doi: 10.1016/j.athoracsur.2020.01.082. [DOI] [PubMed] [Google Scholar]
- 33.Hekmat V, Rao SM, Chhabra M, Chiavarelli M, Anderson JE, Nudel DB. Anomalous origin of the right coronary artery from the main pulmonary artery: Diagnosis and management. Clin Cardiol. 1998;21:773–776. doi: 10.1002/clc.4960211016. [DOI] [PMC free article] [PubMed] [Google Scholar]