BACKGROUND
Delirium, an acute disorder of attention and cognition, is a frequent and often preventable clinical syndrome that commonly occurs after surgery. Currently, older adults ≥65 years of age account for greater than 40% of all inpatient operations.1 Postoperative delirium is associated with longer hospital length of stay, functional and cognitive decline and higher mortality, and at the systems level, the associated costs are estimated at nearly $33 billion a year.2 Importantly, delirium is preventable, making it a prime candidate for preventive interventions targeted to improve surgical outcomes. Despite this, most surgical training programs still have little delirium training incorporated explicitly into the curricula.
Promising initiatives specifically focused on training surgery residents in geriatric principles have been developed in the past; but unfortunately, there continues to be a gap in standardized teaching curriculum on perioperative delirium for surgical trainees. In addition, to the best of our knowledge, there have not been any studies that have reported on longitudinal follow-up or the retention of knowledge and understanding of key concepts surrounding delirium for surgery residents. As such, our team has developed a formalized curriculum on perioperative delirium for surgery residents with foundations in prevention, assessment, and management of delirium.
METHODS
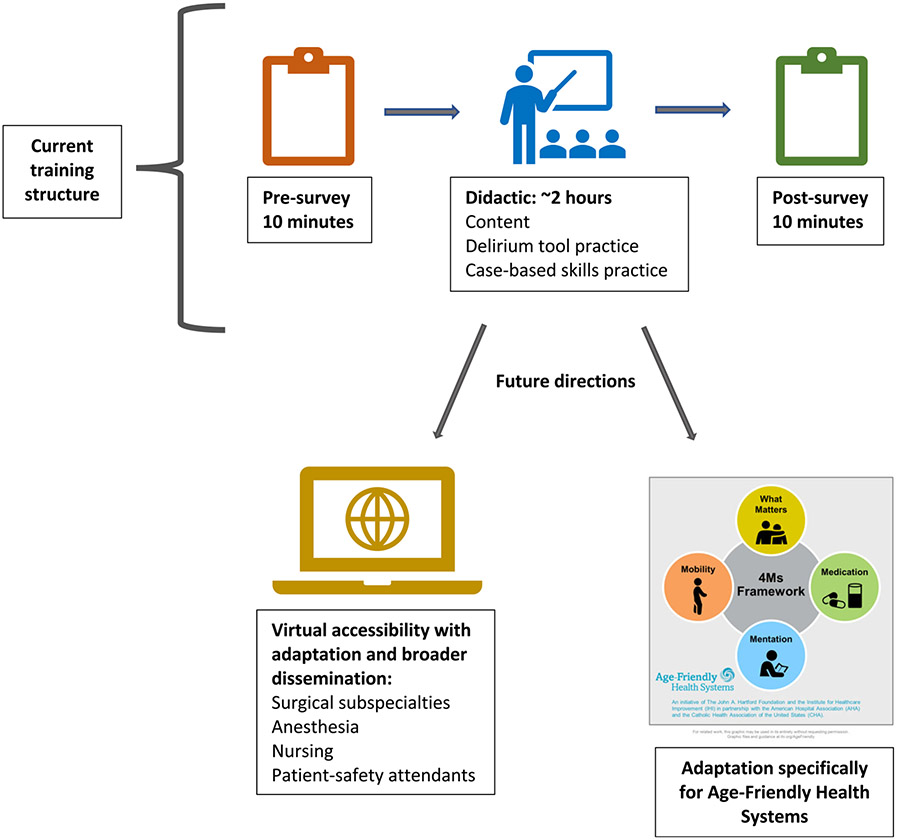
The delirium curriculum was delivered to 64 first-year surgery residents at the John Hopkins University between 2015 and 2018 (available on POGOe, ID: 21896 and as Supplementary Material S1). A follow-up survey was sent 3 years after the initiation of the curriculum to assess retention of knowledge and understanding of delirium. The curriculum was delivered in approximately 2.5 h and included a small group learning experience with a short didactic developed and delivered by a board-certified Geriatrician with expertise in perioperative delirium followed by opportunities to practice skills through watching video-based scenarios and assessing for delirium using a validated delirium assessment tools including 3D-CAM (3 minute-diagnostic assessment) and 4A's Test (4AT) (Figure 1).3 The session closed out with a case-based small group discussion focused on identifying risk factors, calculating delirium risk, listing preventive measures, assessing delirium, and discussing options for non-pharmacologic and pharmacologic treatment.
FIGURE 1.
Structure and future directions for delirium training
The 3-year follow-up assessment was developed and disseminated to former participants using an anonymous, voluntary Qualtrics survey. The assessment included 12 questions that gathered basic demographic data as well as assessed recall and application of the concepts reviewed in the course. This study was conducted in accordance with the Johns Hopkins School of Medicine Institutional Review Board.
RESULTS
Between 2015 and 2018, 64 first-year residents completed our perioperative delirium training with 47 residents remaining in the Johns Hopkins health system at the 3-year follow-up point. Fifty-five percent of these remaining residents (26 residents) responded to our follow-up survey. Seventy-five percent of the respondents were general surgery residents and the other 25% a mix of preliminary residents. Eighty-one percent of residents recalled taking the delirium training course during their intern year. One-third of residents had a standardized approach to assessing perioperative delirium, most commonly identifying the 3D-CAM or 4AT as the tool utilized. Ninety-six percent identified strategies to treat delirium, with every resident identifying non-pharmacological treatment options as their first-line approach to delirium. This included changing times of laboratory draws, minimizing vital sign checks and ensuring day-night orientation. Ninety-nine percent of participants felt the training should be a required component of their surgical training education with nearly a third noting that there should be a longitudinal component added throughout their surgical training to help refresh their knowledge throughout residency.
DISCUSSION
The larger purpose of this work is to create a curriculum with a long-lasting impact on delirium education. This specific evaluation helped us understand the long-term recall and impact of our delirium training for surgery residents at Johns Hopkins. The results from our survey suggest residents who took our training recall our training and important take-home points including non-pharmacologic means for managing post-operative delirium as well as evidence-based screening tools for assessing delirium such as the 3D-CAM and 4-AT. Additionally, we have been able to create a sustainable model for training these residents with our 7th year of the training occurring this year.
The past 2 years of the training have occurred during the global pandemic and have provided opportunities for us to reflect upon innovative ways that we can deliver this important content in a more concise manner and through an online means. We have successfully adapted the training to be delivered virtually and have delivered variations of it to trainees internationally relatively seamlessly. We recognize this as an opportunity to continue to adapt the model of delivery to be more innovative with the changing times and the needs of the busy surgery resident.
We recognize there are limitations to this study including the fact that the retention of knowledge we measured was over variable time periods ranging from 1 to 3 years. Moreover, the course is only delivered at a single training site and during a single year of training. An online version of the course could allow dissemination to other health systems and could be potentially used as part of the Age-Friendly Health Systems initiative.4 We also recognize that we are missing a key component of delirium management, which is the clear multidisciplinary approach that it requires. We plan to expand the reach of our curriculum to include training for our colleagues within nursing and our patient safety attendants, both of whom who are important to the preoperative assessment and prevention of delirium (Figure 1).
Geriatricians, as experts in delirium, play a key role as systems leaders in training other disciplines around delirium and empowering them to care for this condition, which will ultimately improve the care of older adults. For surgeons, training programs that start early in residency and give practical skills for assessment, management, and prevention of delirium are key with an emphasis on a longitudinal component to the training to reinforce concepts and electronic and online versions that make dissemination more possible. With the changing learning environment fostered by the pandemic, we see many avenues to provide the course virtually and will partner with interdisciplinary colleagues to broaden the impact of this work.
Supplementary Material
Supplementary Material S1. Original facilitator's guide and learners guide (published on POGOe) and training guide adapted for virtual teaching.
Acknowledgments
Dr. Gabbard was supported by the National Institute On Aging of the National Institutes of Health under Award Number K23AG070234. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
CONFLICT OF INTEREST
None.
SUPPORTING INFORMATION
Additional supporting information can be found online in the Supporting Information section at the end of this article.
Presented as a Presidential Poster at American Geriatrics Society Annual Meeting 2019.
REFERENCES
- 1.Centers for Disease Control. National Hospital Discharge Survey: Number of All-Listed Procedures for Discharges from Short-Stay Hospitals, by Procedure Category and Age: United States, 2010. 2010. Accessed November 2021. www.cdc.gov/nchs/data/nhds/4procedures/2010pro4_numberprocedureage.pdf
- 2.Gou RY, Hshieh TT, Marcantonio ER, et al. One-year Medicare costs associated with delirium in older patients undergoing major elective surgery. JAMA Surg. e207260. Published online February 24, 2021. doi: 10.1001/jamasurg.2020.7260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shenkin SD, Fox C, Godfrey M, et al. Delirium detection in older acute medical inpatients: a multicentre prospective comparative diagnostic test accuracy study of the 4AT and the confusion assessment method. BMC Med. 2019; 17(1):138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mate K, Fulmer T, Pelton L, et al. Evidence for the 4Ms: interactions and outcomes across the care continuum. J Aging Health. 2021;33(7-8):469–481. doi: 10.1177/0898264321991658 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material S1. Original facilitator's guide and learners guide (published on POGOe) and training guide adapted for virtual teaching.