Abstract
Aim of the Study:
While out-of-hospital cardiac arrest (OHCA) is associated with poor survival, early bystander CPR (B-CPR) and telephone CPR (T-CPR) improves survival from OHCA. American Heart Association (AHA) Scientific Statements outline recommendations for T-CPR. We assessed these recommendations and hypothesized that meeting performance standards is associated with increased likelihood of survival. Additional variables were analyzed to identify future performance measurements.
Methods:
We conducted a retrospective cohort study of non-traumatic, adult, OHCA using the Singapore Pan-Asian Resuscitation Outcomes Study. The primary outcome was likelihood of survival; secondary outcomes were pre-hospital Return of Spontaneous Circulation (ROSC) and B-CPR.
Results:
From 2012–2016, 2,574 arrests met inclusion criteria. Mean age was 68±15; of 2,574, 1,125 (44%) received T-CPR with 5% (135/2574) survival. T-CPR cases that met the Lerner et al. performance metrics analyzed, demonstrated no statistically significant association with survival. Cases which met the Kurz et al. criteria, “Time for Dispatch to Recognize Need for CPR” and “Time to First Compression,” had adjusted odds ratios of survival of 1.01 (95% CI:1.00, 1.02; p=<0.01) and 0.99 (95% CI:0.99, 0.99; p=<0.01), respectively. Identified barriers to CPR decreased the odds of T-CPR and B-CPR being performed. Patients with prehospital ROSC had higher odds of B-CPR being performed. EMS response time < 8 minutes was associated with increased survival among patients receiving T-CPR.
Conclusion:
AHA scientific statements on T-CPR programs serve as ideal starting points for increasing the quality of T-CPR systems and patient outcomes. More work is needed to identify other system performance measures.
Introduction
Out-of-hospital cardiac arrest (OHCA) has an incidence of 55/100,000 person-years worldwide and 20.9 EMS-attended OHCAs per 100,000 person- years in Singapore1. Globally, survival is approximately 10% surviving to hospital discharge2, representing a significant public health problem.
Early cardiopulmonary resuscitation (CPR) is an important link in the chain of survival for OHCA. Performing CPR and decreasing time to first compression have positive effects on patient outcomes3,4. Dispatch-assisted CPR, also referred to as Telephone CPR (T-CPR), has demonstrated significant increases in performance of bystander CPR (B-CPR) and demonstrated 23–400% increases in odds of survival when compared to No-CPR3–5. EMS systems with T-CPR improve rates of B-CPR and patient outcomes in OHCA6,7. Two policy statements have been published from the AHA regarding T-CPR3,4. Lerner, et al. detailed metrics associated with high performing pre-hospital systems, while Kurz, et al. further detailed the impact of OHCA guidelines on development, maintenance, and minimal acceptable standards for T-CPR programs3,4. One other study investigated the Kurz, et al. T-CPR performance goals compared to OHCA data8. To our knowledge, there are no other international consensus statements or assessment of consensus statements for T-CPR using registry data. Considering the favorable patient outcomes associated with T-CPR programs, it is imperative to consider the impact of consensus guidance.
We examined the proposed T-CPR performance metrics and other process variables using registry data to describe associations with outcomes. Singapore has implemented a T-CPR as well as the Pan-Asian Resuscitation Outcome Study (PAROS) OHCA registry, allowing for appropriate T-CPR variable analysis9. We assessed the relationship of T-CPR process metrics with patient outcomes: survival to hospital discharge or 30-day survival (primary outcome), B-CPR (secondary outcome), and return of spontaneous circulation (ROSC) (secondary outcome).
Methods
Study Design
We performed a retrospective secondary analysis of non-traumatic, adult, OHCAs from the Singapore PAROS registry. We assessed the relationship between T-CPR process metrics and patient outcomes. This study was approved by SingHealth Centralized Institutional Review Board (CIRB ref: 2013/604/C and 2018/2937) and National Healthcare Group Domain Specific Review Boards (ref: 2013/00929) with waiver of informed consent.
Study Setting
Singapore is a multi-ethnic city-state in Southeast Asia, with a population of 5.7 million, and a total land area of 725.7 km210. Additionally, 9-9-5 is the national toll-free number for fire and medical emergencies run by Singapore’s national EMS agency, Singapore Civil Defence Force (SCDF). Calls are routed to a single dispatch center where EMS dispatchers use a computer-aided system for triaging and providing pre-arrival instructions11. SCDF has a fleet of 60 ambulances and responded to 191,468 EMS calls in 201912. SCDF implemented a comprehensive T-CPR package in mid-2012 as part of the international PAROS phase 2 trial13. The comprehensive package consisted of a standardized protocol, T-CPR training package, a data collection tool for T-CPR metrics, continuous quality improvement feedback for dispatchers and community CPR training programs13,14. There is a policy aim of 100% audited T-CPR voice recordings using a standardized audit template.
Study Population
The study population included individuals who suffered an OHCA and who were attended by SCDF from 2012–2016. We excluded arrests that involved individuals under 18 years of age, were non-cardiac in etiology, traumatic, witnessed by EMS, events that occurred in a healthcare center or residential institution, and those brought to the Emergency Department (ED) by non-EMS transport.
Sources of Data
To assess our question of interest, we used the PAROS registry. The registry is the result of a research network, established in 2010 to improve outcomes in prehospital emergency care access across the Asian Pacific region through quality research. To date, 13 countries and more than 30 participating sites contribute to the registry. The methodology has been previously described elsewhere15. Collected variables were categorized utilizing the Utstein definitions for OHCA16 including performance of T-CPR algorithms and B-CPR. De-identified data from seven tertiary hospitals in Singapore, collected prospectively, through an online data system managed by a research coordinator, was subject to data quality audits prior to submission to the larger PAROS dataset. The registry consists of 62 variables, 37 are pre-hospital, and 25 are related to ED or hospital outcomes. All audio recordings of OHCA data with T-CPR attempted or performed underwent a review process by medical audit specialists in SCDF for quality improvement using a standardized data collection tool consisting of T-CPR process metrics. Dispatch data included call transcriptions and audited data of all available T-CPR recordings. Resultant data were then entered in an online data system for matching with the PAROS database. This complete dataset was independently reviewed by study authors BSHL & NS.
Definition of outcome variables
The primary outcome was odds of survival at 30 days or survival to hospital discharge, whichever came first. Secondary outcomes were pre-hospital ROSC and performance of B-CPR.
T-CPR process variables
Identified independent variables were adapted to match metrics from the AHA policy statements from Lerner et al. and Kurz et al.3,4. The Lerner et al. metrics included: 1) Barriers to CPR, 2) Telecommunicator recognition of cardiac arrest and provision of CPR pre-arrival instructions, 3) The interval of time from call initiation to completion of the pre-arrival instruction algorithm by the dispatcher, 4) B-CPR performance, and 5) Dispatch of appropriate EMS resources4. Kurz et al. metrics included: 1) Percentage of total OHCA cases that were correctly identified by the public safety answering point (PSAP) (goal ≥75%), 2) The percentage of cases that were correctly identified that were recognizable (goal ≥95%), 3) Percentage of telecommunicator recognized OHCAs receiving T-CPR (goal ≥75%), 4) Median time between call connection and OHCA recognition (goal <90 seconds), and 5) Median time between call and the first T-CPR directed compression (goal <150 seconds)3.
The cases included in analysis were restricted to the 1,125 patients who received T-CPR and included the variables of interest. Cases that did not receive T-CPR recorded high levels of missingness in the variables of interest. However, among those cases that did receive T-CPR, very low levels of missingness were recorded. Considering the metrics described from Lerner et al., several were excluded from the analysis. Specifically, since patients in this restricted dataset received CPR and the appropriate EMS resources were dispatched for all calls, these two metrics were excluded from analysis given that the full dataset met the inclusion criteria. When considering metrics of “Recognition of arrest (by the dispatcher) and Provision of Pre-Arrival Instructions,” there was near total compliance, thus excluded given a reliable estimate of an odds ratio would not be possible. Two remaining criteria from Lerner et al. that could be reliably analyzed remained: 1) Any barriers to CPR and 2) Time for Dispatch to Recognize need for CPR.
From Kurz et al., several criteria were similarly excluded from the final analysis and the same 1,125 cases were analyzed. All cases included were correctly identified by the dispatcher and received T-CPR. The “Percentage of OHCA Cases correctly Identified by PSAP that were recognizable” was not documented. Two criteria were amenable to analysis: 1) Time for Dispatcher to Recognize Need for CPR and 2) Time to First Compression.
Secondary analyses were performed on other registry variables: Barriers to CPR (Y/N), Recognition of Arrest/Provision of CPR Pre-arrival Instructions, Time dispatch recognized need for CPR, B-CPR (Y/N), Identified correctly as cardiac arrest, and Time to first compression. The variable B-CPR indicates that a layperson performed CPR without the provision of instructions by a telecommunicator.
Statistical Analysis
Demographics and characteristics for the sample were stratified by receipt and type of CPR (No B-CPR, T-CPR, and Unassisted B-CPR (i.e., B-CPR without T-CPR)).
A univariable logistic regression was performed to characterize the relationship between survival and the criteria delineated prior (T-CPR process metrics). Multivariable logistic regression was performed to explore the association between type of CPR performed and clinical characteristics seen with cases of OHCA. Characteristics included: age, sex, residential location, arrest witnessed, response time, barrier to CPR present, and pre-hospital ROSC; cases with missing data were excluded. Among cases that received T-CPR, a univariable logistic regression was used to examine the association between arrest witnessed, response time, barrier to CPR present, and prehospital ROSC and the primary outcome. When applicable, analyses were restricted to complete cases due to low levels of missingness. All analysis was performed using R 3.6.317.
Results
Characteristics of the population
2,574 cases of OHCA during the study period met inclusion criteria, of which 37% (949) received no form of B-CPR, 44% (1,125) received T-CPR, and 19% (500) received Unassisted B-CPR (B-CPR only), (Figure 1). Overall survival was 5.2% (135/2,574). Most cases were male, mean age of 67.9±15.4 years. Prehospital-ROSC occurred in 9.3% (240/2,574) of cases with the highest subgroup prevalence of 15.4% (77/500) in the “Unassisted B-CPR” group. Cases that received “Unassisted B-CPR” tended to occur in public, were younger, and experienced higher rates of survival than those who belonged to the T-CPR or No-CPR Groups. Survival for the No-CPR group was 2.8% (27/949), T-CPR 4.5% (51/1,125), and 11.4% (57/500) for Unassisted B-CPR (Table 1). Overall, accounting for standards delineated by Kurz et al., all measure metrics besides time to first directed compression met prespecified goals (Supplemental Table 1).
Figure 1.
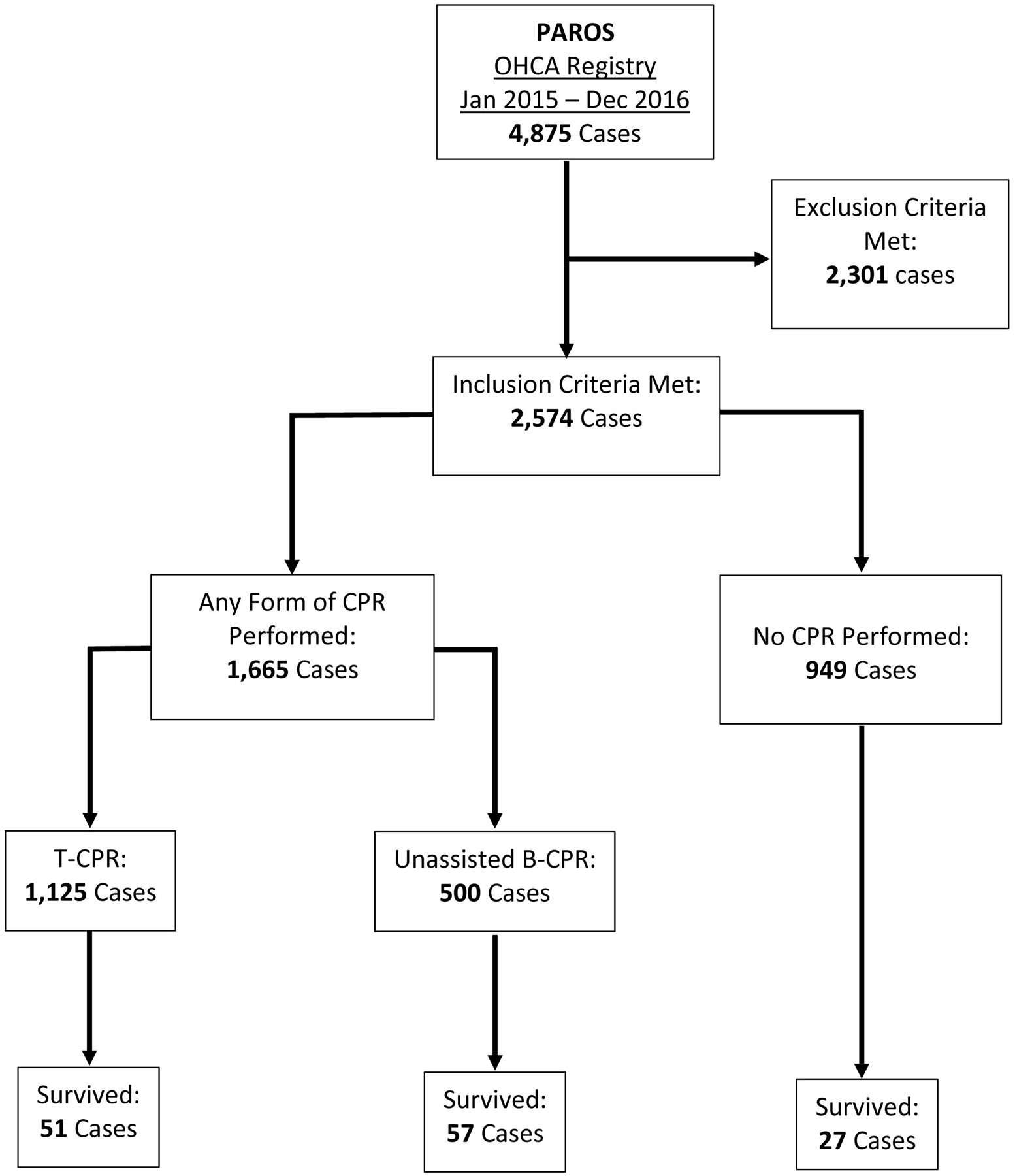
Flow chart of patients included in the study.
PAROS: Pan-Asian Resuscitation Outcomes Study; OHCA: Out of Hospital Cardiac Arrest; CPR: Cardiopulmonary Resuscitation; T-CPR: Telephone CPR; B-CPR: Bystander CPR
Table 1:
Demographics and Clinical Characteristics by Bystander CPR Status and Type
| No Bystander CPR | T-CPR | Non-Assisted-CPR | Total | |
|---|---|---|---|---|
| (N=949) | (N=1125) | (N=500) | (N=2574) | |
| Age | ||||
| Mean (SD) | 69.2 (14.6) | 69.0 (15.6) | 62.8 (15.4) | 67.9 (15.4) |
| Median [Min, Max] | 69.0 [25.0, 108] | 70.0 [19.0, 102] | 62.0 [20.0, 100] | 68.0 [19.0, 108] |
| Gender | ||||
| Female | 337 (35.5%) | 407 (36.2%) | 118 (23.6%) | 862 (33.5%) |
| Male | 612 (64.5%) | 718 (63.8%) | 382 (76.4%) | 1712 (66.5%) |
| Race | ||||
| Chinese | 610 (64.3%) | 767 (68.2%) | 303 (60.6%) | 1680 (65.3%) |
| Eurasian | 5 (0.5%) | 2 (0.2%) | 2 (0.4%) | 9 (0.3%) |
| Indian | 133 (14.0%) | 137 (12.2%) | 68 (13.6%) | 338 (13.1%) |
| Malay | 162 (17.1%) | 174 (15.5%) | 84 (16.8%) | 420 (16.3%) |
| Other | 39 (4.1%) | 45 (4.0%) | 43 (8.6%) | 127 (4.9%) |
| Location of Arrest | ||||
| Non-Residential | 178 (18.8%) | 119 (10.6%) | 235 (47.0%) | 532 (20.7%) |
| Residential | 771 (81.2%) | 1006 (89.4%) | 265 (53.0%) | 2042 (79.3%) |
| Site # | ||||
| 1 | 138 (14.5%) | 168 (14.9%) | 78 (15.6%) | 384 (14.9%) |
| 2 | 209 (22.0%) | 264 (23.5%) | 114 (22.8%) | 587 (22.8%) |
| 4 | 145 (15.3%) | 178 (15.8%) | 74 (14.8%) | 397 (15.4%) |
| 5 | 111 (11.7%) | 120 (10.7%) | 57 (11.4%) | 288 (11.2%) |
| 6 | 266 (28.0%) | 298 (26.5%) | 124 (24.8%) | 688 (26.7%) |
| 7 | 80 (8.4%) | 97 (8.6%) | 53 (10.6%) | 230 (8.9%) |
| Time of Arrest | ||||
| 06:00 – 15:59 | 449 (47.3%) | 534 (47.5%) | 262 (52.4%) | 1245 (48.4%) |
| 16:00 – 20:59 | 208 (21.9%) | 286 (25.4%) | 122 (24.4%) | 616 (23.9%) |
| 21:00 – 22:59 | 84 (8.9%) | 83 (7.4%) | 44 (8.8%) | 211 (8.2%) |
| 23:00 – 05:59 | 208 (21.9%) | 221 (19.6%) | 70 (14.0%) | 499 (19.4%) |
| Missing | 0 (0%) | 1 (0.1%) | 2 (0.4%) | 3 (0.1%) |
| Response Time (Minutes) | ||||
| Mean (SD) | 8.80 (3.26) | 8.74 (3.02) | 9.26 (3.68) | 8.86 (3.25) |
| Median [Min, Max] | 8.33 [1.28, 30.6] | 8.28 [1.85, 24.3] | 8.74 [2.10, 37.4] | 8.37 [1.28, 37.4] |
| Response Time | ||||
| Less Than 8 Minutes | 437 (46.0%) | 512 (45.5%) | 200 (40.0%) | 1149 (44.6%) |
| 8 or More Minutes | 512 (54.0%) | 613 (54.5%) | 300 (60.0%) | 1425 (55.4%) |
| First Arrest Rhythm | ||||
| Asystole | 436 (45.9%) | 566 (50.3%) | 180 (36.0%) | 1182 (45.9%) |
| PEA | 303 (31.9%) | 223 (19.8%) | 85 (17.0%) | 611 (23.7%) |
| Unknown | 0 (0%) | 3 (0.3%) | 5 (1.0%) | 8 (0.3%) |
| Unknown Shockable Rhythm | 10 (1.1%) | 38 (3.4%) | 49 (9.8%) | 97 (3.8%) |
| Unknown Unshockable Rhythm | 52 (5.5%) | 95 (8.4%) | 47 (9.4%) | 194 (7.5%) |
| VF or VT | 148 (15.6%) | 200 (17.8%) | 134 (26.8%) | 482 (18.7%) |
| Pre-Hospital ROSC | ||||
| No | 885 (93.3%) | 1026 (91.2%) | 423 (84.6%) | 2334 (90.7%) |
| Yes | 64 (6.7%) | 99 (8.8%) | 77 (15.4%) | 240 (9.3%) |
| Any ROSC | ||||
| No | 669 (70.5%) | 808 (71.8%) | 317 (63.4%) | 1794 (69.7%) |
| Yes | 280 (29.5%) | 317 (28.2%) | 183 (36.6%) | 780 (30.3%) |
| Prehospital Defibrillation | ||||
| No | 648 (68.3%) | 758 (67.4%) | 262 (52.4%) | 1668 (64.8%) |
| Yes | 301 (31.7%) | 367 (32.6%) | 238 (47.6%) | 906 (35.2%) |
| Survival | ||||
| No | 922 (97.2%) | 1074 (95.5%) | 443 (88.6%) | 2439 (94.8%) |
| Yes | 27 (2.8%) | 51 (4.5%) | 57 (11.4%) | 135 (5.2%) |
CPR: Cardiopulmonary Resuscitation; Site names not disclosed. PEA= Pulseless Electrical Activity; VF= Ventricular Fibrillation, VT= Ventricular Tachycardia; ROSC= Return of Spontaneous Circulation
Primary Outcomes
AHA Scientific Statement Criteria
Variables from the 2012 and 2020 AHA Statements3,4 are included in Table 2. Barriers to CPR, when documented, were present in 32.3% of cases, most common being inability to move the patient to an appropriate position. Recognition of arrest and provision of the CPR pre-arrival instructions was performed in 75.9% of cases, mean time to recognition of needing CPR was 96 seconds, 98.9% successfully identified. Any form of CPR occurred in 63.1% of cases, median time to first compression was 213 seconds.
Table 2:
Lerner and Kurz Criteria present in PAROS Dataset
| Overall | |
|---|---|
| (N=2574) | |
| Barriers to CPR (Y/N) [Lerner 2012] | |
| No | 1058 (41.1%) |
| Yes | 500 (19.4%) |
| Missing | 1016 (39.5%) |
| Recognition of Arrest/Provision of CPR Pre-arrival Instructions [Lerner 2012] | |
| No | 374 (14.5%) |
| Yes | 1176 (45.7%) |
| Missing | 1024 (39.8%) |
| Time dispatch recognized need for CPR (Seconds) [Kurz 2020] | |
| Mean (SD) | 96.4 (62.4) |
| Median [Min, Max] | 81.0 [2.00, 721] |
| Missing | 1088 (42.3%) |
| Bystander CPR (Assisted or Non-Assisted) [Lerner 2012] | |
| No | 949 (36.9%) |
| Yes | 1625 (63.1%) |
| Identified correctly as cardiac arrest [Kurz 2020] | |
| No | 28 (1.1%) |
| Yes | 2546 (98.9%) |
| Time to first compression (Seconds) [Kurz 2020] | |
| Mean (SD) | 230 (90.2) |
| Median [Min, Max] | 213 [0, 687] |
| Missing | 1512 (58.7%) |
Missing Variables: Barrier to CPR: 1016 (39.5%), Recognition of Arrest/Provision of CPR Pre-arrival instructions: 1024 (39.8%), Time dispatch recognized need for CPR: 1088 (42.3%), Time to first compression: 1512 (58.7%); [Lerner 2012] or [Kurz 2020] denote origin of associated AHA Statement metric and PAROS correlates
Univariable analysis
T-CPR cases that met the Lerner et al. performance metrics analyzed, “Any Barriers to CPR” and “Time for Dispatch to Recognize need for CPR” demonstrated no statistically significant association with survival (Table 3).
Table 3:
Odds ratios for Criteria and Survival (n=1,125)
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Criteria | Odds Ratio (95% Confidence Interval) | p-value | Odds Ratio (95% Confidence Interval) | p-value |
| Any Barriers to CPR [Lerner] | 1.17 (0.62, 2.19) | 0.632 | 1.12 (0.59, 2.11) | 0.727 |
| Time for Dispatch to Recognize Need for CPR (Seconds) [Lerner] | 1.003 (0.998, 1.007) | 0.215 | 1.003 (0.998, 1.007) | 0.224 |
| Time for Dispatch to Recognize Need for CPR (Seconds) [Kurz] | 1.003 (0.998, 1.007) | 0.215 | 1.011 (1.004, 1.018) | 0.002 |
| Time to First Compression (Seconds) [Kurz] | 0.997 (0.993, 1.001) | 0.112 | 0.992 (0.986, 0.997) | 0.003 |
CPR: Cardiopulmonary Resuscitation. Multivariable regression controlling for other criteria in this table; Adjusted OR are adjusted for the other criteria in the table
T-CPR cases that met the Kurz et al. criteria analyzed, the adjusted odds ratios for Time for Dispatch to Recognize Need for CPR was 1.01 (95% CI:1.00, 1.02; p=<0.01) and Time to First Compression was 0.99 (95% CI:0.99, 0.99; p=<0.01) (Table 3). Each additional second of delay to first compression was associated with a 0.8% decrease in the odds of survival.
Secondary Outcomes
Multivariate analysis
Using multinomial regression and controlling for age, sex, residential location, witnessed (yes/no), response time, barriers, and pre-hospital ROSC, we assessed the relationship between type of CPR with the secondary variables of interest. Several significant relationships were characterized (Table 4). The outcome being modeled was an unordered, three-level variable (No-CPR, Unassisted B-CPR, and T-CPR (B-CPR+T-CPR) with No-CPR as a reference group. In total 1,558 cases were analyzed using complete case analysis of which 1,125 received T-CPR and 253 received unassisted B-CPR, 180 received no CPR. For each additional year of age, there was a 2% decrease in the likelihood of receiving B-CPR compared to those that did not receive CPR (OR: 0.98 (95% CI: 0.97, 1.00); p=0.02). Patient sex did not have a significant effect on the receipt of CPR. Patients in residential locations were at much greater odds of receiving T-CPR and lower odds of receiving unassisted B-CPR when compared with no CPR (OR: 2.23 (95% CI: 1.24, 3.99); p<0.01 and OR: 0.39 (95% CI: 0.21, 0.72); p<0.01, respectively). Cases with increased response times greater than 8 minutes were not significantly associated with receipt of either form of CPR (unassisted B-CPR and T-CPR). A barrier to CPR significantly decreased the odds of any CPR being performed (unassisted B-CPR, OR: 0.04 (95% CI: 0.02, 0.07); p<0.01). Cases with prehospital ROSC were more likely to have received B-CPR than those that did not have CPR (OR: 2.67 (95% CI: 1.25, 5.72); p=0.01). No such significant relationship was observed with those that received T-CPR vs No-CPR.
Table 4:
Multinomial Regression for Bystander CPR and T-CPR (N = 1,378)
| Non-Assisted Bystander CPR (vs No Bystander CPR) N = 253 |
T-CPR (vs No Bystander CPR) N = 1,125 |
|||
|---|---|---|---|---|
| Variable | Odds Ratio (95% Confidence Interval) | p-value | Odds Ratio (95% Confidence Interval) | p-value |
| Age (Years) | 0.98 (0.97, 1.00) | 0.024 | 0.99 (0.98, 1.00) | 0.128 |
| Male Sex (Reference = Female) | 1.32 (0.81, 2.14) | 0.266 | 1.19 (0.81, 1.75) | 0.371 |
| Residential Location (Reference = Non-Residential) | 0.39 (0.21, 0.72) | 0.002 | 2.23 (1.24, 3.99) | 0.007 |
| Arrest Witnessed | 1.23 (0.80, 1.90) | 0.361 | 0.97 (0.68, 1.39) | 0.875 |
| Response Time > 8 minutes | 1.29 (0.84, 1.99) | 0.240 | 1.13 (0.79, 1.60) | 0.511 |
| Barrier to CPR, yes | 0.05 (0.03, 0.08) | <0.001 | 0.04 (0.02, 0.06) | <0.001 |
| Prehospital ROSC, yes | 2.67 (1.25, 5.72) | 0.011 | 1.80 (0.89, 3.62) | 0.101 |
CPR: Cardiopulmonary Resuscitation, T-CPR: Telephone CPR, ROSC: Return of Spontaneous Circulation; 3 level variable analysis with “no bystander CPR” as reference group
Among those that received T-CPR, prehospital ROSC was the strongest indicator (OR 26.78 (95% CI: 13.97, 51.35); p<0.01) (Table 5). Witnessed cases with a prompt EMS response (<8 minutes) were at greater odds of survival (OR 12.62 (95% CI: 4.01, 39.71); p<0.01). Cases in which pre-hospital ROSC occurred were also, expectedly, associated with survival (OR 27.23 (95% CI: 14.11, 52.53); p<0.01). A Response Time of less than 8 minutes was associated with a 162% increase in the odds of survival compared to those greater than 8 minutes (OR: 2.62 (95% CI: 1.33, 5.17); p=0.01).
Table 5:
Odds ratios for survival amongst patients receiving T-CPR (n=1,125)
| Variable | Odds Ratio (95% Confidence Interval) | p-value |
|---|---|---|
| Arrest Witnessed | 4.57 (1.94, 10.76) | 0.001 |
| EMS Response Time (Seconds) | 0.998 (0.996, 1.000) | 0.059 |
| Barriers to CPR | 1.09 (0.52, 2.26) | 0.826 |
| Prehospital ROSC | 26.78 (13.97, 51.35) | <0.001 |
EMS: Emergency Medical Services, CPR: Cardiopulmonary Resuscitation, ROSC: Return of Spontaneous Circulation
Discussion
In this study, we present a real-world application of the 2012 and 2020 AHA T-CPR performance measures and explore additional metrics to assess the association between T-CPR quality and survival. We evaluated the performance of these metrics with B-CPR, pre-hospital ROSC, and survival. In our cohort, identification of OHCA by the dispatcher met AHA specified standards but longer times to first compression were associated with poorer outcomes. Longer call to scene times for EMS were associated with increased rates of B-CPR performance, but shorter times were seen to be highly associated with survival. Unassisted B-CPR was associated with increased odds of pre-hospital ROSC.
Unassisted B-CPR was associated with a higher odds of survival than T-CPR. Prior literature supports this finding and demonstrates that good neurological outcomes were most strongly associated with unassisted B-CPR18. Several factors may contribute to this observation including generalizable factors and those that may be unique to our setting. Persons who are trained in CPR have demonstrated an understanding of the core principles behind the recognition and initial resuscitation of persons who are or may be in cardiac arrest; the quality of CPR by the trained is likely superior to a person given instructions over the phone (T-CPR)19–21. As observed in our study, short call to scene times were associated with survival and may be attributed to the performance of high-quality CPR compared to a possibly untrained person performing CPR for the first time with telephone instruction. There is likely a temporal component of delay associated with those having to rely on T-CPR to prompt the initiation of compressions/early defibrillation and automatic external defibrillator use. Our study re-enforces the known benefit of early CPR on survival; delays in CPR initiation or hesitancy in performance have been attributed to concern for hurting the patient and can be overcome with training22. In Singapore, CPR training is a requisite of physical education classes in the public education system, and outside of the education system the government offers free CPR and AED training, thus removing some barriers to knowing CPR23–25. The success of such public training programs and awareness campaigns on CPR and AEDs has been demonstrated globally22,26,27. Mandating CPR and AED training as part of national education systems and offering free, accessible training could lead to improved outcomes in OHCA.
The guidelines specified by the two AHA scientific statements provide goals that are supported by scientific evidence28,29, but real-world attainment of these metrics, even for high performing systems such as Singapore’s may not be realistic and is resource intensive. Although the PAROS dataset is rather extensive in what it sets out to capture, there is a high degree of missingness with the data recorded, highlighting the difficulty of T-CPR program monitoring. Though a similar study captured all of the 2020 criteria, a smaller sample size was included, and attainment of the pre-specified goals also proved to also be difficult8. As demonstrated prior, and again seen in our study, temporal measures of performance on the dispatch side of care are difficult to attain, but even so, not often associated with significant survival benefits30. Assessment of cases that were correctly identified that were “recognizable” is a labor and cost intensive measure of quality and may not contribute to better outcomes. In our study, it may be inferred that if 98.9% of the total OHCA cases were correctly identified by the PSAP, then the percentage of OHCA cases correctly identified by PSAP that were recognizable is likely higher.
Future research may determine what metrics of CPR performance are correlated with CPR quality and the interface of quality CPR and T-CPR. Prior studies showed the use of video assistance improved CPR quality but delayed initiation31,32. There is little evidence of proven methodology to assess the quality of CPR performed in the context of OHCA. CPR feedback devices exist, but as with other aspects related to studying OHCA, it is likely to also be too resource intensive to be an efficacious avenue of investigation or for large scale public distribution.
We propose that there should be consideration of increased consolidation and uniform application of T-CPR programs and EMS systems such that initiatives for case review and continuous quality improvement can be used. Centralized systems, such as in Singapore, and participation in a cardiac arrest registry such as PAROS demonstrate motivation to track and improve patient centered care initiatives such as T-CPR and have shown positive effects on patient outcomes33,34.
Aims for future study and development of T-CPR systems include public education campaigns and systems to improve rates of unassisted B-CPR and methods for improvement of EMS response times. Future research should focus on the measurement of B-CPR quality in OHCA and what alternative measures may be better suited to assess T-CPR programs effect on survival and outcomes.
Among the limitations of this study, assessment of the performance metrics for T-CPR systems as set out in the 2012 and 2020 scientific statements was incomplete due to inherent characteristics of the dataset.
Some limitations associated with EMS and hospital systems that may affect outcomes which can be considered confounders such as advances in EMS-care, post-ROSC care, and use of mechanical CPR devices cannot be assessed by our study. Singapore’s population and EMS structure may not be generalizable. Our sample was small and may not have accurately captured associations among variables and outcomes. The measurement and adequate performance of metrics is a small part of T-CPR programs.
Conclusions
Even with several longstanding T-CPR programs worldwide, little is known about the real-world implication of policy statement guidelines and their effect on patient outcomes in OHCA. In this study, the majority of cases were correctly and promptly identified by dispatchers, surpassing pre-specified standards. Delays to first compression was associated with reduced survival. One prior study has demonstrated greater anticipated lives saved with increased metric fulfillment8. Future work should assess what other process variables serve as targets for enhanced outcomes.
Supplementary Material
Acknowledgements:
The Duke Biostatistics, Epidemiology, and Research Design Core’s support was made possible by the CTSA Grant (UL1TR002553) from the National Center for Advancing Translational Sciences (NCATS) of the NIH and the NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not represent the official views of NCATS or NIH.
The authors would like to thank the late Ms. Susan Yap from Department of Emergency Medicine, Singapore General Hospital; Ms. Nurul Asyikin and Ms. Noor Azuin from Unit for Prehospital Emergency Care, Singapore General Hospital for their contributions and support to the Singapore OHCA registry. The authors would also like to acknowledge all the Medical Audit Specialists from UPEC, Singapore General Hospital for their support and efforts in implementing Dispatcher-Assisted CPR program and our colleagues at the Singapore Civil Defence Force: all EMS Dispatchers, AC Yazid Abdullah, COL Bob Tan, MAJ Joey Ai Meng Tay, WO2 Pey Yun Low and CPT Carl Ross De Souza for their fruitful collaboration throughout. We would also like to thank Ms. Patricia Tay from the Singapore Clinical Research Institute for her role as secretariat for the PAROS network.
Role of the funding source:
The PAROS study was supported by the National Medical Research Council, Clinician Scientist Award Singapore (NMRC/CSA/0049/2013) and Ministry of Health, Health Services Research Grant, Singapore (HSRG/0021/2012). The study sponsors were not involved in the study.
References
- 1.Kiguchi T, Okubo M, Nishiyama C, et al. Out-of-hospital cardiac arrest across the World: First report from the International Liaison Committee on Resuscitation (ILCOR). Resuscitation. 2020;152:39–49. doi: 10.1016/j.resuscitation.2020.02.044 [DOI] [PubMed] [Google Scholar]
- 2.Nichol G, Stiell IG, Laupacis A, Pham B, De Maio VJ, Wells GA. A cumulative meta-analysis of the effectiveness of defibrillator-capable emergency medical services for victims of out-of-hospital cardiac arrest. Ann Emerg Med. 1999;34(4 Pt 1):517–525. [PubMed] [Google Scholar]
- 3.Kurz Michael Christopher, Bobrow Bentley J., Buckingham Julie, et al. Telecommunicator Cardiopulmonary Resuscitation: A Policy Statement From the American Heart Association. Circulation. 2020;141(12):e686–e700. doi: 10.1161/CIR.0000000000000744 [DOI] [PubMed] [Google Scholar]
- 4.Brooke Lerner E., Rea Thomas D., Bobrow Bentley J., et al. Emergency Medical Service Dispatch Cardiopulmonary Resuscitation Prearrival Instructions to Improve Survival From Out-of-Hospital Cardiac Arrest. Circulation. 2012;125(4):648–655. doi: 10.1161/CIR.0b013e31823ee5fc [DOI] [PubMed] [Google Scholar]
- 5.Eberhard KE, Linderoth G, Gregers MCT, Lippert F, Folke F. Impact of dispatcher-assisted cardiopulmonary resuscitation on neurologically intact survival in out-of-hospital cardiac arrest: a systematic review. Scand J Trauma Resusc Emerg Med. 2021;29(1):70. doi: 10.1186/s13049-021-00875-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rea TD, Eisenberg MS, Culley LL, Becker L. Dispatcher-assisted cardiopulmonary resuscitation and survival in cardiac arrest. Circulation. 2001;104(21):2513–2516. doi: 10.1161/hc4601.099468 [DOI] [PubMed] [Google Scholar]
- 7.Vaillancourt C, Verma A, Trickett J, et al. Evaluating the effectiveness of dispatch-assisted cardiopulmonary resuscitation instructions. Acad Emerg Med Off J Soc Acad Emerg Med. 2007;14(10):877–883. doi: 10.1197/j.aem.2007.06.021 [DOI] [PubMed] [Google Scholar]
- 8.Byrsell F, Claesson A, Jonsson M, et al. Swedish dispatchers’ compliance with the American Heart Association performance goals for dispatch-assisted cardiopulmonary resuscitation and its association with survival in out-of-hospital cardiac arrest: A retrospective study. Resusc Plus. 2022;9:100190. doi: 10.1016/j.resplu.2021.100190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teo MHN, Wong WEJ, Daniel PCYN, et al. The use of dispatcher assistance in improving the quality of cardiopulmonary resuscitation: A randomised controlled trial. Resuscitation. 2019;138:153–159. doi: 10.1016/j.resuscitation.2019.03.003 [DOI] [PubMed] [Google Scholar]
- 10.Department of Statistics Singapore. Population Trends 2019. Accessed December 6, 2021. https://www.singstat.gov.sg/-/media/files/publications/population/population2019.pdf
- 11.Ho AFW, Chew D, Wong TH, et al. Prehospital Trauma Care in Singapore. Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. 2015;19(3):409–415. doi: 10.3109/10903127.2014.980477 [DOI] [PubMed] [Google Scholar]
- 12.Singapore Civil Defence Force. Fire, Ambulance and Enforcement Statistics 2019. Accessed December 6, 2021. https://www.scdf.gov.sg/docs/default-source/scdf-library/amb-fire-inspection-statistics/scdf-annual-statistics-2019.pdf
- 13.Ong MEH, Shin SD, Tanaka H, et al. Rationale, Methodology, and Implementation of a Dispatcher-assisted Cardiopulmonary Resuscitation Trial in the Asia-Pacific (Pan-Asian Resuscitation Outcomes Study Phase 2). Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. 2015;19(1):87–95. doi: 10.3109/10903127.2014.942482 [DOI] [PubMed] [Google Scholar]
- 14.Pek PP, Lim JYY, Leong BSH, et al. Improved Out-of-Hospital Cardiac Arrest Survival with a Comprehensive Dispatcher-Assisted CPR Program in a Developing Emergency Care System. Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. 2021;25(6):802–811. doi: 10.1080/10903127.2020.1846824 [DOI] [PubMed] [Google Scholar]
- 15.Ong MEH, Shin SD, Tanaka H, et al. Pan-Asian Resuscitation Outcomes Study (PAROS): rationale, methodology, and implementation. Acad Emerg Med Off J Soc Acad Emerg Med. 2011;18(8):890–897. doi: 10.1111/j.1553-2712.2011.01132.x [DOI] [PubMed] [Google Scholar]
- 16.Perkins GD, Jacobs IG, Nadkarni VM, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation. 2015;132(13):1286–1300. doi: 10.1161/CIR.0000000000000144 [DOI] [PubMed] [Google Scholar]
- 17.R: The R Project for Statistical Computing. Accessed July 5, 2021. https://www.r-project.org/
- 18.Kim MW, Kim TH, Song KJ, et al. Comparison between dispatcher-assisted bystander CPR and self-led bystander CPR in out-of-hospital cardiac arrest (OHCA). Resuscitation. 2021;158:64–70. doi: 10.1016/j.resuscitation.2020.11.010 [DOI] [PubMed] [Google Scholar]
- 19.Chocron R, Jobe J, Guan S, et al. Bystander Cardiopulmonary Resuscitation Quality: Potential for Improvements in Cardiac Arrest Resuscitation. J Am Heart Assoc. 2021;10(6). doi: 10.1161/JAHA.120.017930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Takei Y, Nishi T, Matsubara H, Hashimoto M, Inaba H. Factors associated with quality of bystander CPR: The presence of multiple rescuers and bystander-initiated CPR without instruction. Resuscitation. 2014;85(4):492–498. doi: 10.1016/j.resuscitation.2013.12.019 [DOI] [PubMed] [Google Scholar]
- 21.Hagihara A, Onozuka D, Shibuta H, Hasegawa M, Nagata T. Dispatcher-assisted bystander cardiopulmonary resuscitation and survival in out-of-hospital cardiac arrest. Int J Cardiol. 2018;265:240–245. doi: 10.1016/j.ijcard.2018.04.067 [DOI] [PubMed] [Google Scholar]
- 22.Kua PHJ, White AE, Ng WY, et al. Knowledge and attitudes of Singapore schoolchildren learning cardiopulmonary resuscitation and automated external defibrillator skills. Singapore Med J. 2018;59(9):487–499. doi: 10.11622/smedj.2018021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blewer AL, Ho AFW, Shahidah N, et al. Impact of bystander-focused public health interventions on cardiopulmonary resuscitation and survival: a cohort study. Lancet Public Health. 2020;5(8):e428–e436. doi: 10.1016/S2468-2667(20)30140-7 [DOI] [PubMed] [Google Scholar]
- 24.Workplace Safety and Health (First-Aid) Regulations - Singapore Statutes Online. Accessed March 2, 2022. https://sso.agc.gov.sg/SL/WSHA2006-RG4
- 25.DARE - Dispatcher-Assisted first REsponder. Accessed March 2, 2022. https://daretosave.sg/
- 26.Bradley S, Fahrenbruch C, Mesichke H, Allen J, Bloomingdale M, Rea T. Bystander CPR in out-of-hospital cardiac arrest: the role of limited English proficiency. Accessed April 1, 2020. https://www-ncbi-nlm-nih-gov.proxy.lib.duke.edu/pubmed/21388734 [DOI] [PubMed]
- 27.Lee MJ, Hwang SO, Cha KC, Cho GC, Yang HJ, Rho TH. Influence of nationwide policy on citizens’ awareness and willingness to perform bystander cardiopulmonary resuscitation. Resuscitation. 2013;84(7):889–894. doi: 10.1016/j.resuscitation.2013.01.009 [DOI] [PubMed] [Google Scholar]
- 28.Lewis M, Stubbs BA, Eisenberg MS. Dispatcher-assisted cardiopulmonary resuscitation: time to identify cardiac arrest and deliver chest compression instructions. Circulation. 2013;128(14):1522–1530. doi: 10.1161/CIRCULATIONAHA.113.002627 [DOI] [PubMed] [Google Scholar]
- 29.Sasson C, Rogers MAM, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3(1):63–81. doi: 10.1161/CIRCOUTCOMES.109.889576 [DOI] [PubMed] [Google Scholar]
- 30.Shah M, Bartram C, Irwin K, et al. Evaluating Dispatch-Assisted CPR Using the CARES Registry. Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. 2018;22(2):222–228. doi: 10.1080/10903127.2017.1376133 [DOI] [PubMed] [Google Scholar]
- 31.Ecker H, Lindacher F, Adams N, et al. Video-assisted cardiopulmonary resuscitation via smartphone improves quality of resuscitation: A randomised controlled simulation trial. Eur J Anaesthesiol. 2020;37(4):294–302. doi: 10.1097/EJA.0000000000001177 [DOI] [PubMed] [Google Scholar]
- 32.Lin YY, Chiang WC, Hsieh MJ, Sun JT, Chang YC, Ma MHM. Quality of audio-assisted versus video-assisted dispatcher-instructed bystander cardiopulmonary resuscitation: A systematic review and meta-analysis. Resuscitation. 2018;123:77–85. doi: 10.1016/j.resuscitation.2017.12.010 [DOI] [PubMed] [Google Scholar]
- 33.Bobrow BJ, Spaite DW, Vadeboncoeur TF, et al. Implementation of a Regional Telephone Cardiopulmonary Resuscitation Program and Outcomes After Out-of-Hospital Cardiac Arrest. JAMA Cardiol. 2016;1(3):294–302. doi: 10.1001/jamacardio.2016.0251 [DOI] [PubMed] [Google Scholar]
- 34.Meischke H, Painter IS, Stangenes SR, et al. Simulation training to improve 9-1-1 dispatcher identification of cardiac arrest: A randomized controlled trial. Resuscitation. 2017;119:21–26. doi: 10.1016/j.resuscitation.2017.07.025 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


