ABSTRACT
Mental health stigma has been identified as a barrier to help-seeking in the United States. This may be particularly salient for military personnel who tend to report higher mental health stigma than the general population. Evidence suggests that both supportive and destructive military leadership are related to service members’ attitudes toward seeking help. In the current study, a sample of military service members and Veterans (N = 232) completed an online survey regarding mental health stigma, previous experiences with military leaders, and mental health help-seeking behaviors. Findings indicated that destructive and supportive leadership experiences were significantly related to self stigma, public stigma, and help-seeking. Military members and Veterans who experienced destructive leadership were more likely to report internalized mental health stigma, which decreased the likelihood of seeking help. Supportive leadership, on the other hand, was associated with greater likelihood of seeking help for mental health concerns, and was indirectly related to help-seeking through lower self-stigma. Findings suggest that the military leadership style plays a significant role in service members’ and Veterans’ willingness to seek assistance for mental health concerns.
KEYWORDS: Military, Veteran, help-seeking, stigma, leadership
What is the public significance of this article?---Mental health stigma is a significant barrier to help-seeking in the United States, and is particularly salient in military settings. Findings suggest that both destructive and supportive military leadership styles contribute to how service members’ and Veterans’ view mental health/illness and psychological treatment, and these associations differed by military branch. Military leaders and decision makers must understand the significant power leaders have on their troops’ psychological adjustment and closely examine how they train their leadership force in order to ensure the safety and well-being of all military personnel.
Mental health stigma is one of the strongest predictors of help-seeking behavior (Clement et al., 2015). In Western cultures, an estimated 52–74% of the individuals with a mental disorder do not seek help (Alonso et al., 2004; Kessler et al., 2001; Wittchen & Jacobi, 2005). Yet delaying treatment for mental health concerns is related to worse outcomes for major depressive disorders, anxiety disorders, bipolar disorder, and psychosis (Boonstra et al., 2012; Dell’Osso, Glick, Baldwin, & Altamura, 2012). The National Comorbidity Survey found that “concern about what others might think” was a key barrier to seeking mental health treatment (Kessler et al., 2001, p. 996). In a systematic review, Clement and colleagues concluded that stigma was a moderate barrier to help-seeking, ranking behind confidentiality concerns and access to treatment. However, military personnel ranked mental health stigma as a much greater barrier to care than civilian populations. Military leadership seems to play a crucial role in how service members cope with stress (Bliese & Castro, 2000; Bliese, Ritzer, Thomas, & Jex, 2001; McGurk et al., 2014), and their likelihood to seek help (Britt, Wright, & Moore, 2012). The current study examined relationships between mental health stigma, perceptions of military leadership, and mental health help-seeking behaviors in a sample of military service members and Veterans (SMV).
Mental health stigma
Mental health stigma can be parsed into two components: public stigma and self-stigma (Vogt, 2011). Public stigma is the concern that mental health problems will be viewed unfavorably by others, while self-stigma is one’s own detrimental personal beliefs about people with mental illness, including oneself. Previous research on public stigma identified three themes regarding societal beliefs about mental illness: “authoritarianism” (i.e., people with mental illness are irresponsible/unreliable), “fear and exclusion” (i.e., people with mental illness are dangerous and should be isolated), and “benevolence” (i.e., people with mental illness are naïve and incompetent) (Corrigan & Penn, 1999; Couture & Penn, 2003). If these attitudes and beliefs about mental illness are internalized by individuals with psychological problems, self-stigma can develop. Self-stigma presumably lowers self-esteem, which can decrease the motivation to seek treatment (Mechanic, McAlpine, Rosenfield, & Davis, 1994). Furthermore, people are less likely to seek help if they believe that they are the cause of their own problems (Cooper, Corrigan, & Watson, 2003).
Although public and self-stigma occurs in the general population (Clement et al., 2015; Kessler et al., 2001), mental health stigma is a highly salient cultural interdiction in the United States (US) military (Greene-Shortridge, Britt, & Castro, 2007; Hoge, Auchterlonie, & Milliken, 2006; Tanielian et al., 2016). SMVs who encountered dangerous environments, suffered injury, and/or were at risk of serious injury or death have an increased probability of developing depression and post-traumatic stress disorder (PTSD; Schwarzbold et al., 2008; Thomas et al., 2010). However, evidence suggests that many SMVs in need of care are unlikely to seek help (Gould et al., 2010; Kim, Thomas, Wilk, Castro, & Hoge, 2010) or follow up with a psychological referral compared to a medical referral (Britt, 2000). Some of the stigma surrounding mental health and treatment is fueled by the military culture’s judgment of a mental disorder as a personal weakness and/or something service members should have control over (Nash, Silva, & Litz, 2009).
Greene-Shortridge et al. (2007) proposed a model to explain how public stigma, self-stigma, and other barriers to care may affect military personnel’s ability to access mental health care. Specifically, SMVs who develop psychological symptoms may perceive distancing or blame from other unit members. The behaviors of others along with previously held beliefs about society’s perception of mental illness contribute to the development of public stigma. When these messages and previously held beliefs about mental illness are internalized, SMVs experience self-stigma, which contributes to efforts to hide and/or suppress emotional distress.
As part of the VA initiative to improve service utilization, a comprehensive review identified public stigma as one of the most salient concerns for SMVs, noting few studies at the time examining self-stigma in military and Veteran populations (Vogt, 2011). In a large qualitative study conducted across six different military installations, active duty personnel reported that public stigma regarding the attitudes and perceptions of their leaders and whether their careers would be negatively affected were some of their main concerns about seeking treatment (Tanielian et al., 2016). As researchers turned their attention to self-stigma, findings indicated that soldiers who received mental health treatment had lower self-stigma than soldiers who had not received treatment (Skopp et al., 2012). Similarly, in a study examining different stigma perceptions in a military sample (i.e., career consequences, differential treatment of others, self-stigma, and stigmatizing others who seek treatment), self-stigma was the only unique predictor of premature treatment termination (Britt, Jennings, Cheung, Pury, & Zinzow, 2015). Importantly, Wade et al. (2015) reported that self-stigma fully mediated the relationship between public stigma and attitudes/intent to seek help.
Leadership
Military leaders are responsible for the physical and psychological well-being of their troops (Castro & Adler, 2011; Castro, Thomas, & Adler, 2006; Greenberg & Jones, 2011), and their behaviors are associated with how service members cope with stress in dangerous environments (Bliese & Castro, 2000; Britt, Davison, Bliese, & Castro, 2004; McGurk et al., 2014). Researchers examining management styles across different work contexts have identified two leadership styles: supportive and destructive leadership (Aasland, Skogstad, Notelaers, Nielson, & Einarsen, 2010; Mitchell & Ambrose, 2007; Tepper, 2000). Generally, supportive leader behaviors include frequent contact with subordinates, praise for employee’s work, and an emphasis on workplace safety. Conversely, destructive leader behaviors include publicly embarrassing subordinates, favoritism, and delegating extraneous tasks to “look good” to their superiors. In other words, supportive leaders are concerned with the professional and personal development of their subordinates, while destructive leaders are more likely to use their subordinates as tools to further promote their own careers. These leadership behaviors are differentially associated with subordinates’ overall performance, motivation, and health (Aasland et al., 2010; Duffy, Ganster, & Pagon, 2002; Tepper, 2000; Tepper, Moss, Lockhart, & Carr, 2007).
Although the majority of research on destructive and supportive leadership behaviors has utilized civilian samples, researchers have also looked at leadership styles in a military setting. Leadership behaviors appear to be associated with the development of psychological symptoms among troops following combat, particularly PTSD. Among the 960 junior enlisted soldiers in 74 platoons on duty in Iraq or Afghanistan, soldiers in units exposed to high levels of direct combat and low supportive leadership by noncommissioned officers were over twice as likely to meet the criteria for PTSD (23%) than those with high combat and high supportive leadership (9%) (McGurk et al., 2014). Military leader behaviors are not only associated with the development of mental illness in their troops, but they may also be linked to their subordinates’ likelihood to seek help for mental health concerns. After finding that supportive leadership behaviors reduced the number of perceived barriers to care and destructive leadership was associated with increased stigma, Britt et al. (2012) suggested that embarrassing unit members in front of others could create a work environment where troops feel anxious about seeking help due to fear of public humiliation for having a mental illness. Additionally, evidence suggests that the leaders themselves experience self-stigma, which reduces the likelihood of seeking mental health care (Hamilton, Coleman, & Davis, 2017) and possibly influences their subordinates’ beliefs.
Current study
Leadership seems to play a crucial role in how service members cope with stress (Bliese et al., 2001; Bliese & Castro, 2000; McGurk et al., 2014), their level of mental health stigma (Greene-Shortridge et al., 2007; Skopp et al., 2012; Tanielian et al., 2016; Vogt, 2011), and their likelihood to seek help (Britt et al., 2012). As one of the first investigations examining leadership, stigma, and help-seeking among SMVs, the current study extended the literature by exploring interrelations among perceptions military leadership and mental health public and self-stigma to help us better understand service members’ help-seeking behaviors. We hypothesized that: (H1a) high destructive leadership is significantly associated with high public and self-stigma, and (H1b) is indirectly related to low help-seeking intentions via paths through high public and self-stigma, and (H2a) supportive leadership is significantly associated with low public and self-stigma, and (H2b) is indirectly related to high help-seeking intentions via paths through low public and self-stigma.
Method
Participants and procedure
The current study was part of a larger project that examined the psychological and relational functioning of an SMV sample. After receiving approval from the university’s Institutional Review Board to ensure confidentiality and protection of human subjects, participants (N = 232) were recruited via online social media sites (i.e, Facebook, Twitter, etc.) and in-person at local Veterans of Foreign Wars and American Legion posts. Participants provided consent before completing an anonymous Qualtrics survey, and received a debrief notice at the end including mental health referral sources. As an incentive, one dollar per participant was donated to the Fisher House Foundation, a nonprofit organization supporting SMV families.
The sample included both active duty (n= 73; 31.5%) and Veteran (n= 159; 68.5%) service members with an average of 9.5 years served (SD = 7.49 years; Range = 1–36.6 years). Approximately 70% (n = 163) of the sample reported at least one foreign deployment, almost two-thirds of which were to a war zone (n= 145; 62.5%), with the rest having never been deployed (n= 70; 30%). Participants were predominantly male (n= 166; 71.6%) with a mean age of 37.72 (SD = 11.17). Table 1 presents sample characteristics, including race/ethnicity, military branch and rank, and number of deployments.
Table 1.
Demographic characteristics
| Characteristic | Total Sample N = 232 |
|
|---|---|---|
| n | % | |
| Military Service | ||
| Veteran | 159 | 68.5 |
| Active Duty | 73 | 31.5 |
| Gender | ||
| Male | 166 | 71.6 |
| Female | 66 | 28.4 |
| Deployment Experience | ||
| Deployed at least once to foreign soil | 163 | 70.0 |
| Deployed at least once to war zone | 145 | 62.5 |
| One deployment (any) | 63 | 27.0 |
| Two deployments (any) | 52 | 22.3 |
| Three deployments (any) | 22 | 9.4 |
| Four deployments (any) | 7 | 3.0 |
| Five deployments (any) | 19 | 8.2 |
| Never deployed | 70 | 30.0 |
| Ethnicity | ||
| African American | 6 | 2.6 |
| Asian/Pacific Islander | 5 | 2.1 |
| Hispanic | 19 | 8.2 |
| White/ European American | 184 | 79 |
| Bi/multi-racial/Other | 12 | 5.2 |
| Native American | 7 | 3 |
| Branch | ||
| Air Force | 52 | 22.3 |
| Army | 87 | 37.3 |
| Marines | 37 | 15.9 |
| Navy | 56 | 24 |
| Did not answer | 1 | .4 |
| Rank | ||
| Junior Enlisted (E1-E3) | 15 | 6.6 |
| Noncommissioned Officers (E4-E6) | 151 | 64.8 |
| Senior Noncommissioned Officers (E7-E9) | 26 | 11.2 |
| Commissioned Officers (O1-O6) | 37 | 15.9 |
| Did not answer | 4 | 1.7 |
Measures
The Background Information Questionnaire-Military Version (BGI-M; Campbell & Riggs, 2015) gathers demographic data and information regarding military background (e.g., branch, rank, deployment information, etc.), as well as relationship and mental health history.
Help-seeking
To assess participants’ help-seeking behaviors, we used the General Help-Seeking Questionnaire (GHSQ; Wilson, Deane, Ciarrochi, & Rickwood, 2005). Participants indicated the likelihood that they would seek help from 10 different sources (e.g., intimate partner, friend, family, mental health professional, doctor, minister, no one, etc.) on a 7-point response scale ranging from Extremely Unlikely (1) to Extremely Likely (7). Scale score was computed by averaging across items with higher scores indicating greater likelihood to seek help for personal or emotional problems (M = 33.33; SD = 10.22). The GHSQ demonstrated reliability and validity in a broad range of contexts (Wilson et al., 2005). In this study, Cronbach’s alpha for the GHSQ was .89.
Stigma
We used 26-items taken from the Military Stigma Scale (MSS; Skopp et al., 2012) to measure Public Stigma (e.g., “A person seeking mental health treatment is seen as weak”) and Self-Stigma (e.g., “My self-confidence would be harmed if I got help from a mental health provider”). Items were presented to respondents with a 4-point response scale ranging from Definitely Disagree (1) to Definitely Agree (4). Some items were reverse coded to help identify inconsistent responding (e.g., “My self-esteem would increase if I talked to a therapist”). Scale scores were computed by averaging across items with higher scores indicating greater levels of Public (M = 23.32; SD = 7.84) or Self-Stigma (M = 9.36; SD = 3.41). Both the public and self-stigma subscales demonstrated good reliability and validity in military populations (Skopp et al., 2012). The Cronbach's alpha coefficient for both scales was .99.
Leadership
We used the 6-item Noncommissioned Officer Leadership Scale – Short (NCOLS-S; McGurk et al., 2014) to assess participants’ perceptions of their military superiors’ Supportive Leadership (e.g., “Are concerned about the safety of their troops”) and Destructive Leadership (e.g., “Embarrass troops in front of other unit members”). Participants rated the items on a 5-point response scale ranging from Strongly Disagree (1) to Strongly Agree (5). Scale scores for each variable were computed by averaging across items with higher scores indicating greater levels of Supportive (M = 10.70; SD = 2.88) or Destructive Leadership (M = 9.36; SD = 3.41). Using three items each to measure supportive (α = .77) and destructive (α = .76) leadership, McGurk et al. reported that the short version of the measure performed similarly to the original measure in terms of reliability and validity. In this study, Cronbach’s alpha was .73 for the Supportive Leadership scale and .77 for the Destructive Leadership scale.
Results
Data were analyzed using SPSS Version 25.0. Missing data were examined (<5% for each measure), and missing values were imputed using mean substitution. Skewness and kurtosis for key variables were within acceptable limits. Table 2 provides means, standard deviations, and correlations. Preliminary analyses indicate that most demographic variables were unrelated to key variables. However, ANOVA results showed significant group differences between military branch and help-seeking (F[3, 228] = 2.76, p= .04), self-stigma (F[3, 228] = 2.94, p= .03), supportive leadership (F[3, 228] = 3.12, p= .03), and destructive leadership (F[3, 228] = 2.64, p= .05). Post-hoc findings indicated that Marines were less likely to seek help and perceived more destructive leadership than Soldiers, Airmen, and Sailors; they also reported significantly more self-stigma than Airmen and Soldiers, as well as less supportive leadership than Soldiers. As a result, the military branch (Marines vs other branches) was controlled for in primary analyses.
Table 2.
Correlations, means, and standard deviations
| Correlation Matrix | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| (1)Supportive Leadership | 1 | ||||
| (2)Destructive Leadership | −.60*** | 1 | |||
| (3)Self-Stigma | −.22*** | .08** | 1 | ||
| (4)Public Stigma | −.39*** | .40*** | .58*** | 1 | |
| (5)Help-Seeking | .15* | −.06 | −.48*** | −.32*** | 1 |
| Mean SD |
10.70 2.88 |
9.36 3.41 |
23.32 7.84 |
40.82 11.83 |
33.33 10.22 |
*p < .05, **p < .01, ***p < .001
For primary hypothesis testing, each variable was converted to standardized z-scores. Path analyses using PROCESS Model 6 in the PROCESS 3.0 macros for SPSS, tested study hypotheses. As predicted and shown in Figure 1, we found direct effects between destructive leadership and both self (t[227] = 2.33, p= .02) and public stigma (t[226] = 6.19, p < .001). Also, there was a significant indirect effect between destructive leadership and help-seeking through self-stigma, with a bootstrapped partial indirect effect of −.06 (95% C.I. β [−.14- −.01]) but no indirect effect emerged for public stigma. Thus, perceptions of more destructive leadership are associated with higher self and public stigma, and through the exacerbation of self-stigma, participants reporting higher destructive leadership are less likely to seek help for mental health concerns. Overall, this model explained 24% of the variance in help-seeking (R2 = .24).
Figure 1.
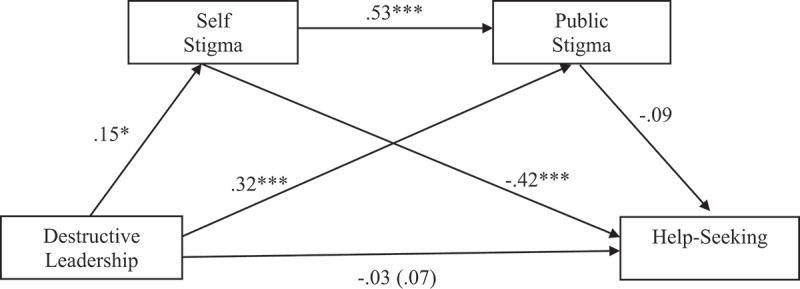
Standardized regression coefficients for the relationship between destructive leadership and help-seeking as mediated by self and public stigma. The standardized regression coefficient between destructive leadership and help-seeking, controlling for stigma, is in parentheses
In support of hypotheses (H2a, H2b), the second path model (see Figure 2) also showed significant direct effects from supportive leadership to lower self-stigma (t[227] = −3.07, p= .002) and public stigma (t[226] = −5.29, p < .001), and greater help-seeking (t[227] = 1.92, p= .05). After controlling for stigma in the model, the relationship between supportive leadership and help-seeking was non-significant (95% C.I. β [.02-.18]). A significant indirect effect emerged in the path between supportive leadership and help-seeking through self-stigma, with a bootstrapped standardized indirect effect of .08 (95% C.I. β [.02-.15]). In other words, perceptions of supportive leadership were significantly associated with low self and public stigma, and through the reduction of self-stigma, participants reporting more supportive leadership were more likely to seek help for mental health concerns. Overall, this model explained 24% of the variance in help-seeking (R2 = .24).
Figure 2.
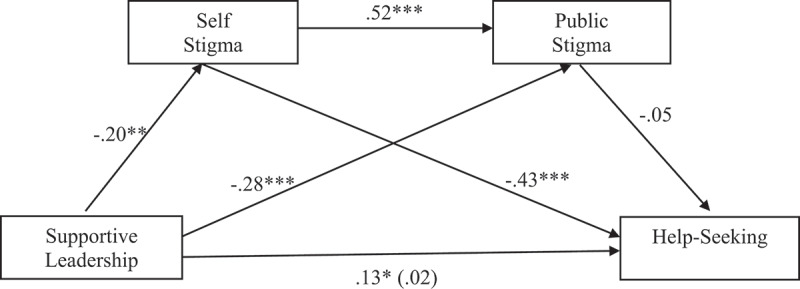
Standardized regression coefficients for the relationship between supportive leadership and help-seeking as mediated by self and public stigma. The standardized regression coefficient between supportive leadership and help-seeking, controlling for stigma, is in parentheses
Discussion
The current study contributes to our knowledge of military leadership styles in relation to public and self-stigma, and SMVs’ likelihood to seek help for mental health concerns. Overall, the results supported hypotheses that military leadership styles are associated with public stigma and self-stigma, and partially supported predicted indirect effects on help-seeking behavior. The present findings lend weight to previous research (Britt et al., 2012; McGurk et al., 2014), building further evidence that military leadership styles are worthy considerations in the mental health and well-being of SMVs. Current findings and their implications are discussed below.
As predicted, destructive leadership was associated with higher self and public stigma, and was indirectly related to low help-seeking through high self-stigma. In this sample, SMVs who perceived destructive leadership were more likely to endorse internalized stigma that decreased their likelihood of seeking mental health assistance. Conversely, perceptions of supportive leadership were associated with greater likelihood of seeking help for mental health concerns, and were indirectly related to help-seeking through lower self-stigma. Current findings suggest that different leadership styles among officers and senior enlisted personnel could promote or conversely counter mental health self-stigma and indirectly influence the likelihood of service members and Veterans seeking help. Longitudinal research with a more robust sample is needed to substantiate mediation by self-stigma over time.
The findings are consistent with the only other study to date exploring leadership and mental health stigma in a military context, which found that destructive leadership was associated with increased stigma and supportive leadership was related to less perceived barriers to treatment (Britt et al., 2012). However, the results did not support a hypothesized indirect effect of public stigma in either path model despite a significant direct correlation with help-seeking intentions in preliminary analyses, implying that other variables in the model accounted for the effects of public stigma. Wade et al. (2015) found that self-stigma fully mediated the relationship between public stigma and attitudes/intent to seek help in a sample of active-duty service members referred for neuropsychological assessment. Current findings similarly suggest that self-stigma may be a more powerful or more proximal predictor of service members’ help-seeking behaviors than public stigma. These results shed light on the potential influence of military leaders with respect to perceived stigma among their subordinates and whether troops seek the mental health care they need. In particular, SMVs who encountered more destructive leadership may experience shame and self-blame for their distress, which can make them less likely to seek help. Conversely, troops who received more supportive leadership may be less likely to have negative self-attributions when experiencing distressing psychological symptoms, which could increase the likelihood they will seek psychological services when needed.
Notably, preliminary analyses documented intriguing differences between Marines and other military branches. Specifically, Marines reported they were less likely to seek services for mental health and had more destructive leadership than members of all other military branches. Marines also reported significantly more self-stigma than Airmen and Soldiers, and less supportive leadership experiences than Soldiers. Although Marines represented 15.9% of current sample, which exceeds the 12.1% proportion of Marines in the total 2018 US military force (Department of Defense [DoD], 2018), the actual number of Marines in this sample was minimal (n= 37) and thus these findings may not generalize to the larger population of Marines. There is a dearth of empirical studies examining the unique subcultural differences between branches of the US military, with a recent comprehensive review of stigma as a barrier to care in the military finding no studies that analyzed branch differences (Sharp et al., 2015). With little to draw from, an explanation for this finding must wait for future research that includes a cross-branch examination of these psychological constructs. In particular, considering that Marines have the highest ratio of enlisted members to officers (7.7:1) among the four main US military branches, which together averaged 4.1 enlisted personnel for every officer on Active Duty (DoD, 2018), researchers may want to explore whether this discrepancy is relevant to various leadership styles or possibly overburdened officer leadership in different branches, which may contribute to a delegative versus transformational (i.e., by example) style of leadership.
The current study is limited by a cross-sectional design, which cannot identify directionality nor yield causal conclusions. Furthermore, the sample was mostly comprised of Veterans (68.5%), and despite no significant differences between Veterans and active-duty troops in preliminary analyses, the sampling method and sample size should give pause before generalizing broadly to both service members and Veterans. For example, the use of self-report measures in an online survey introduced the possibility of biased reporting; in particular, retrospective self-reports of military experiences for Veterans who have been out of the service for an extended time may not accurately assess their experiences. In addition, a report of hypothetical help-seeking from any source may not reflect actual help-seeking behaviors and does not tell us specifically about seeking therapeutic treatment. Due to high rates of stigma in SMV populations (Greene-Shortridge et al., 2007; Hoge et al., 2004; Tanielian et al., 2016), there is also the possibility that potential participants high in mental health stigma opted not to participate in a research study about mental health. Future studies may benefit from longitudinal designs that follow military personnel across time to more accurately assess their ongoing experiences of leadership behaviors, changes in public and self-stigma as a result of these experiences, and tangible help-seeking behaviors (e.g., receiving psychological treatment). For instance, a cross-sequential design with a larger stratified sample of SMVs across the major military branches will allow sophisticated statistical modeling approaches and closer examination of differences related to demographic diversity (e.g., sex, race, age) and military characteristics (e.g., active-duty vs Veteran, branch, rank, deployment), as well as within-leader variation in levels of destructive and supportive leadership behavior.
In conclusion, findings from this study underscore the potential systemic influence of leadership behaviors on military and Veteran troops’ mental health stigma and likelihood of seeking psychological treatment and suggest areas for future investigation with larger representative SMV samples. Importantly, research on destructive and supportive leadership styles can inform military leadership training and policy in ways that might prevent or ameliorate psychological distress among SMVs, and reduce the mental health stigma of seeking help for that distress if it develops. Military leaders and decision makers in each of the service branches may benefit from examining how they train their leadership force and the potential effects different types of leaders have on their troops’ psychological well-being, self-stigma, and help-seeking behavior. As a step in the right direction, the Defender’s Edge (DEFED) program was designed to reduce mental health stigma utilizing a strength-based philosophy. After embedding a psychologist within a US Air Force Security Forces unit, Bryan and Morrow (2011) found that the DEFED program promoted increased trustworthiness and utilization of both formal and informal services with the psychologist. Similar programs to train leaders on the mental health needs of their troops may be highly beneficial in reducing unit stigma and increasing access to and use of psychological treatment. Future studies should also further examine subcultural differences in leadership and mental health stigma, which may provide important information about differential experiences between military branches that can inform prevention and treatment planning.
Acknowledgment
This study was based on the dissertation research of the first author, utilizing data from a larger research project. At the time of the research, all authors were affiliated with the University of North Texas. Currently, James McGuffin, Ph.D., is a U.S.A.F. Veteran currently working in private practice; Shelley Riggs, Ph.D., is a professor at Sam Houston State University; Emily M. Raiche, Ph.D., is a Postdoctoral Fellow at the Counseling Center of New England, Lifestance Health and Cpt Daniel H. Romero, Ph.D., is serving in the US Army. Please address all correspondence to Shelley A. Riggs, Ph.D., at sxr142@shsu.edu.
Funding Statement
This work was supported by the University of North Texas.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Aasland, M. S., Skogstad, A., Notelaers, G., Nielson, M. B., & Einarsen, S. (2010). The prevalence of destructive leadership behaviour. British Journal of Management, 21, 438–452. [Google Scholar]
- Alonso, J., Angermeyer, M. C., Bernert, S., Bruffaerts, R., Brugha, T. S., Bryson, H., … Haro, J. M. (2004). Use of mental health services in Europe: Results from the European study of the epidemiology of mental disorders (ESEMeD) project. Acta Psychiatrica Scandinavica, 109(s420), 47–54. doi: 10.1111/j.1600-0047.2004.00325.x [DOI] [PubMed] [Google Scholar]
- Bliese, P. D., & Castro, C. A. (2000). Role clarity, work overload and organizational support: Multilevel evidence of the importance of support. Work and Stress, 14(1), 65–73. doi: 10.1080/026783700417230 [DOI] [Google Scholar]
- Bliese, P. D., Ritzer, P., Thomas, J. L., & Jex, S. M. (2001, August). Supervisory support and stressor–commitment relations: A multi-level investigation. Paper presented at the annual conference of the Society for Industrial and Organizational Psychology, San Diego, CA. [Google Scholar]
- Boonstra, N., Klaassen, R., Sytema, S., Marshall, M., De Haan, L., Wunderink, L., & Wiersma, D. (2012). Duration of untreated psychosis and negative symptoms—a systematic review and meta-analysis of individual patient data. Schizophrenia Research, 142(1), 12–19. doi: 10.1016/j.schres.2012.08.017 [DOI] [PubMed] [Google Scholar]
- Britt, T. W. (2000). The stigma of psychological problems in a work environment: Evidence from the screening of service members returning from Bosnia. Journal of Applied Social Psychology, 30(8), 1599–1618. doi: 10.1111/j.1559-1816.2000.tb02457.x [DOI] [Google Scholar]
- Britt, T. W., Davison, J., Bliese, P. D., & Castro, C. A. (2004). How leaders can influence the impact that stressors have on soldiers. Military Medicine, 169(7), 541. doi: 10.7205/MILMED.169.7.541 [DOI] [PubMed] [Google Scholar]
- Britt, T. W., Jennings, K. S., Cheung, J. H., Pury, C. L., & Zinzow, H. M. (2015). The role of different stigma perceptions in treatment seeking and dropout among active duty military personnel. Psychiatric Rehabilitation Journal, 38(2), 142. doi: 10.1037/prj0000120 [DOI] [PubMed] [Google Scholar]
- Britt, T. W., Wright, K. M., & Moore, D. (2012). Leadership as a predictor of stigma and practical barriers toward receiving mental health treatment: A multilevel approach. Psychological Services, 9(1), 26. doi: 10.1037/a0026412 [DOI] [PubMed] [Google Scholar]
- Bryan, C. J., & Morrow, C. E. (2011). Circumventing mental health stigma by embracing the warrior culture: Lessons learned from the defender’s edge program. Professional Psychology, Research and Practice, 42(1), 16. doi: 10.1037/a0022290 [DOI] [Google Scholar]
- Campbell, R., & Riggs, S. A. (2015). The role of psychological symptomatology and social support in the academic adjustment of previously deployed student veterans. Journal of American College Health, 63(7), 473–481. doi: 10.1080/07448481.2015.1040408 [DOI] [PubMed] [Google Scholar]
- Castro, C. A., Thomas, J. L., & Adler, A. B. (2006). Toward a liberal theory of military leadership. In Adler A. B., Castro C. A., & Britt T. W. (Eds.), Military life: The psychology of serving in peace and combat (Vol. 2, pp. 192–212). Westport, CT: Praeger Security International. [Google Scholar]
- Castro, C. A., & Adler, A. B. (2011). Reconceptualizing combat-related posttraumatic stress disorder as an occupational hazard. In Adler A. B., Bliese P. B., & Castro C. A. (Eds.), Deployment psychology: Evidence-based strategies to promote mental health in the military (pp. 217–241). Washington, DC: American Psychological Association. [Google Scholar]
- Clement, S., Schauman, O., Graham, T., Maggioni, F., Evans-Lacko, S., Bezborodovs, N., … Thornicroft, G. (2015). What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychological Medicine, 45(1), 11–27. doi: 10.1017/S0033291714000129 [DOI] [PubMed] [Google Scholar]
- Cooper, A. E., Corrigan, P. W., & Watson, A. C. (2003). Mental illness stigma and care seeking. The Journal of Nervous and Mental Disease, 191(5), 339–341. doi: 10.1097/01.NMD.0000066157.47101.22 [DOI] [PubMed] [Google Scholar]
- Corrigan, P. W., & Penn, D. L. (1999). Lessons from social psychology on discrediting psychiatric stigma. American Psychologist, 54(9), 765. doi: 10.1037/0003-066X.54.9.765 [DOI] [PubMed] [Google Scholar]
- Couture, S., & Penn, D. (2003). Interpersonal contact and the stigma of mental illness: A review of the literature. Journal of Mental Health, 12(3), 291–305. doi: 10.1080/09638231000118276 [DOI] [Google Scholar]
- Dell’Osso, B., Glick, I. D., Baldwin, D. S., & Altamura, A. C. (2012). Can long-term outcomes be improved by shortening the duration of untreated illness in psychiatric disorders? A conceptual framework. Psychopathology, 46(1), 14–21. doi: 10.1159/000338608 [DOI] [PubMed] [Google Scholar]
- Department of Defense . (2018). 2018 demographics: Profile of the military community. Retrieved from https://download.militaryonesource.mil/12038/MOS/Reports/2018-demographics-report.pdf
- Duffy, M. K., Ganster, D. C., & Pagon, M. (2002). Social undermining in the workplace. Academy of Management Journal, 45(2), 331–351. [Google Scholar]
- Gould, M., Adler, A., Zamorski, M., Castro, C., Hanily, N., Steele, N., … Greenberg, N. (2010). Do stigma and other perceived barriers to mental health care differ across Armed Forces? Journal of the Royal Society of Medicine, 103(4), 148–156. doi: 10.1258/jrsm.2010.090426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg, N., & Jones, N. (2011). Optimizing mental health support in the military: The role of peers and leaders. In Adler A. B., Bliese P. B., & Castro C. A. (Eds.), Deployment psychology: Evidence based strategies to promote mental health in the military (pp. 69–101). Washington, DC: American Psychological Association. [Google Scholar]
- Greene-Shortridge, T. M., Britt, T. W., & Castro, C. A. (2007). The stigma of mental health problems in the military. Military Medicine, 172(2), 157–161. doi: 10.7205/MILMED.172.2.157 [DOI] [PubMed] [Google Scholar]
- Hamilton, J. A., Coleman, J. A., & Davis, W. J. (2017). Leadership perspectives of stigma-related barriers to mental health care in the military. Military Behavioral Health, 5(1), 81–90. doi: 10.1080/21635781.2016.1257964 [DOI] [Google Scholar]
- Hoge, C. W., Auchterlonie, J. L., & Milliken, C. S. (2006). Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA, 295(9), 1023–1032. doi: 10.1001/jama.295.9.1023 [DOI] [PubMed] [Google Scholar]
- Hoge, C. W., Castro, C. A., Messer, S. C., McGurk, D., Cotting, D. I., & Koffman, R. L. (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine, 351(1), 13–22. doi: 10.1056/NEJMoa040603 [DOI] [PubMed] [Google Scholar]
- Kessler, R. C., Berglund, P. A., Bruce, M. L., Koch, J. R., Laska, E. M., Leaf, P. J., … Wang, P. S. (2001). The prevalence and correlates of untreated serious mental illness. Health Services Research, 36(6 Pt 1), 987. [PMC free article] [PubMed] [Google Scholar]
- Kim, P. Y., Thomas, J. L., Wilk, J. E., Castro, C. A., & Hoge, C. W. (2010). Stigma, barriers to care, and use of mental health services among active duty and National Guard soldiers after combat. Psychiatric Services, 61(6), 582–588. doi: 10.1176/ps.2010.61.6.582 [DOI] [PubMed] [Google Scholar]
- McGurk, D., Sinclair, R. R., Thomas, J. L., Merrill, J. C., Bliese, P. D., & Castro, C. A. (2014). Destructive and supportive leadership in extremis: Relationships with post-traumatic stress during combat deployments. Military Behavioral Health, 2(3), 240–256. doi: 10.1080/21635781.2014.963765 [DOI] [Google Scholar]
- Mechanic, D., McAlpine, D., Rosenfield, S., & Davis, D. (1994). Effects of illness attribution and depression on the quality of life among persons with serious mental illness. Social Science &Medicine, 39(2), 155–164. [DOI] [PubMed] [Google Scholar]
- Mitchell, M. S., & Ambrose, M. L. (2007). Abusive supervision and workplace deviance and the moderating effects of negative reciprocity beliefs. Journal of Applied Psychology, 92(4), 1159–1168. doi: 10.1037/0021-9010.92.4.1159 [DOI] [PubMed] [Google Scholar]
- Nash, W. P., Silva, C., & Litz, B. (2009). The historic origins of military and veteran mental health stigma and the stress injury model as a means to reduce it. Psychiatric Annals, 39(8), 789. doi: 10.3928/00485713-20090728-05 [DOI] [Google Scholar]
- Schwarzbold, M., Diaz, A., Martins, E. T., Rufino, A., Amante, L. N., Thais, M. E., … Walz, R. (2008). Psychiatric disorders and traumatic brain injury. Neuropsychiatric Disease and Treatment, 4(4), 797–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp, M. L., Fear, N. T., Rona, R. J., Wessely, S., Greenberg, N., Jones, N., & Goodwin, L. (2015). Stigma as a barrier to seeking health care among military personnel with mental health problems. Epidemiologic Reviews, 37(1), 144–162. doi: 10.1093/epirev/mxu012 [DOI] [PubMed] [Google Scholar]
- Skopp, N. A., Bush, N. E., Vogel, D. L., Wade, N. G., Sirotin, A. P., McCann, R. A., & MetzgerAbamukong, M. J. (2012). Development and initial testing of a measure of public and self‐stigma in the military. Journal of Clinical Psychology, 68(9), 1036–1047. doi: 10.1002/jclp.21889 [DOI] [PubMed] [Google Scholar]
- Tanielian, T., Woldetsadik, M. A., Jaycox, L. H., Batka, C., Moen, S., Farmer, C., & Engel, C. C. (2016). Barriers to engaging service members in mental health care within the USmilitary health system. Psychiatric Services, 67(7), 718–727. doi: 10.1176/appi.ps.201500237 [DOI] [PubMed] [Google Scholar]
- Tepper, B. J. (2000). Consequences of abusive supervision. Academy of Management Journal, 43, 178–190. [Google Scholar]
- Tepper, B. J., Moss, S. E., Lockhart, D. E., & Carr, J. C. (2007). Abusive supervision, upward maintenance communication, and subordinates’ psychological distress. Academy of Management Journal, 50, 1169–1180. [Google Scholar]
- Thomas, J. L., Wilk, J. E., Riviere, L. A., McGurk, D., Castro, C. A., & Hoge, C. W. (2010). Prevalence of mental health problems and functional impairment among active component and National Guard soldiers 3 and 12 months following combat in Iraq. Archives of General Psychiatry, 67(6), 614–623. doi: 10.1001/archgenpsychiatry.2010.54 [DOI] [PubMed] [Google Scholar]
- Vogt, D. (2011). Mental health-related beliefs as a barrier to service use for military personnel and veterans: A review. Psychiatric Services, 62(2), 135–142. doi: 10.1176/ps.62.2.pss6202_0135 [DOI] [PubMed] [Google Scholar]
- Wade, N. G., Vogel, D. L., Armistead-Jehle, P., Meit, S. S., Heath, P. J., & Strass, H. A. (2015). Modeling stigma, help-seeking attitudes, and intentions to seek behavioral healthcare in a clinical military sample. Psychiatric Rehabilitation Journal, 38(2), 135. doi: 10.1037/prj0000131 [DOI] [PubMed] [Google Scholar]
- Wilson, C. J., Deane, F. P., Ciarrochi, J., & Rickwood, D. (2005). Measuring help-seeking intentions: Properties of the general help-seeking questionnaire. Canadian Journal of Counselling, 39(1), 15. [Google Scholar]
- Wittchen, H. U., & Jacobi, F. (2005). Size and burden of mental disorders in Europe—a critical review and appraisal of 27 studies. European Neuropsychopharmacology, 15(4), 357–376. doi: 10.1016/j.euroneuro.2005.04.012 [DOI] [PubMed] [Google Scholar]