ABSTRACT
Accumulating research suggests unique patterns of suicide risk, homelessness, and criminal-justice involvement in younger (age < 40) relative to older (aged 40+) cohorts of Veterans. However, potential explanations for these differences remain unclear. To address this gap, we analyzed data from a nationally representative sample of more than 4,000 US military Veterans to compare risk and protective correlations of prior suicidal behavior, homelessness, and justice-involvement in younger versus older Veterans. Results revealed that younger Veterans were significantly more likely than older Veterans to have a history of suicide attempt(s) (13.9% vs. 2.7%) and homelessness (22.5% vs. 8.7%). They also scored higher on measures of risk factors and lower on measures of protective factors. However, some factors – specifically, resilience, grit, impulsiveness, perceptions of the effect of the military on one’s life and social support – were less strongly associated with a history of adverse events in younger versus older Veterans. Findings highlight the need for preventative homelessness and mental health services for younger Veterans that are tailored to the unique characteristics and needs of this age cohort.
KEYWORDS: Veteran, age, suicide, homelessness, risk factors
What is the public significance of this article?—In a large, nationally representative sample, younger Veterans (age < 40) were more likely to have a history of suicide attempt(s) and homelessness, scored higher on measures of risk factors, and scored lower on measures of protective factors relative to older Veterans (age 40+). However, the strength of association between risk/protective factors and histories of suicide attempt(s) and homelessness was generally weaker among younger Veterans. Results highlight the need for preventative services that are tailored to the unique characteristics and needs of younger Veterans.
As recent combat operations end [i.e., Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND)] and increased attention is drawn to our nation’s youngest Veterans (i.e., those under the age of 40), a burgeoning literature has highlighted potential risks for suicide, homelessness, and criminal justice involvement in this population. For example, data from the US Department of Veterans Affairs (2020) suggest that suicide rates for Veterans aged 18–34 have almost doubled since 2006, now 37–68% greater than older Veterans, 149% greater than the general population, and 165% greater than their same-aged peers. The onset of homelessness (i.e., lack of a fixed, regular, and adequate residence) also occurs more quickly after discharge for OEF/OIF/OND Veterans than other cohorts (4.54 years versus 6.58–9.03 years; Tsai, Szymkowiak, & Pietrzak, 2020). Furthermore, data from the US Department of Justice (Bronson, Carson, Noonan, & Berzofsky, 2015) suggest that despite lower rates of justice-involvement compared to older Veterans and the general population, incarcerated younger Veterans are disproportionately convicted of violent crimes (71% versus 52% in the general population), suggesting additional, significant legal needs. While younger Veterans comprise a small proportion of the overall Veteran population (Department of Veterans Affairs, 2016), a considerable proportion of resources are allocated to addressing the impact of these adverse events on younger Veterans (Department of Veterans Affairs, 2021). Various regional and national initiatives aim to mitigate risk within this Veteran sub-population (e.g., Executive Order 13822, 116th Congress, 2020; Exec. Order No. 13822, 3 C.F.R., Supporting Our Veterans During Their Transition From Uniformed Service to Civilian Life, 2018), emphasizing the need to understand factors associated with such risk.
Two explanations may help to understand these adverse experiences of young Veterans. First, a generally “high-risk” profile appears similarly associated with histories of suicidal behavior, homelessness, and criminal justice involvement in Veterans. For example, Veterans with a history of one or more of these experiences (versus those without such history) tend to be more impulsive, less resilient, and more likely to have experienced low social support and psychosocial functioning following military discharge, adverse childhood experiences (ACEs; e.g., parental psychopathology, childhood abuse), military sexual trauma, and negative military experiences (Blonigen et al., 2016; Fogle et al., 2020; Holliday, Martin, Monteith, Clark, & LePage, 2021; Posey, 2009; Tsai & Rosenheck, 2015; Tsai, Trevisan, Huang, & Pietrzak, 2018). The occurrence of suicidal behavior, homelessness, and criminal justice involvement also tends to be significantly correlated in Veteran samples (Edwards, Barnes, Govindarajulu, Geraci, & Tsai, 2020; Edwards et al., 2020), thus suggesting that the experience of one is associated with increased risk for others. If younger Veterans are more likely to have a “high-risk” profile, it could explain, at least in part, their difficulties with suicidal behavior, homelessness, and criminal justice-involvement. Consistent with this, preliminary research suggests younger Veterans are more likely than older Veterans to have experienced certain risk factors, particularly military sexual trauma and adverse childhood experiences (Blosnich, Dichter, Cerulli, Batten, & Bossarte, 2014; Suris & Lind, 2008). However, these findings require replication, and implications on Veteran suicidal behavior, homelessness, and justice involvement remain unclear without further research.
It is also possible that risk/protective factors and age interact such that age moderates the strength of association between risk/protective factors and adverse events. Consistent with this, some factors appear differentially related to mental health across Veteran age cohorts. For example, research by Weiner, Monin, Mota, and Pietrzak (2016) revealed that mental health difficulties of younger Veterans are more closely associated with perceived social support than community integration, whereas the reverse is true of older Veterans. Similarly, because younger Veterans are often temporarily closer to military service than other-aged Veterans who might have discharged decades earlier, military-specific factors, such as unpleasant discharge experiences and/or military-to-civilian transitional stress, may be especially salient. Consistent with this, transitional stress is typically more severe for younger Veterans (Pew Research Center, 2011), and the degree of transitional stress is positively associated with suicide risk in Veterans (Kline, Ciccone, Falca-Dodson, Black, & Losonczy, 2011).
The current study
Distinctive patterns of suicidal behavior, homelessness, and criminal justice involvement have been routinely observed among younger Veterans. However, research investigating potential explanations for the comparatively elevated risk of this Veteran sub-population is lacking. To address this gap, we analyzed data from a nationally representative sample of US military Veterans to compare risk and protective correlations of suicidal behavior, homelessness, and justice involvement in younger versus older Veterans. In line with prior research, analyses focused on personality, ACEs, military-specific experiences, and post-military factors as potential correlates of these experiences (Blonigen et al., 2016; Fogle et al., 2020; Holliday et al., 2020; Posey, 2009; Tsai & Rosenheck, 2015; Tsai et al., 2018).
Three hypotheses were evaluated: (1) Younger Veterans would experience higher rates of prior suicide attempt and homelessness, and lower rates of prior arrest than older Veterans; (2) Adverse events would be associated with higher scores on measures of risk factors (i.e., impulsivity, hostility, military sexual trauma, moral injury, perceptions of military experience as having negative effects on life and psychosocial functioning difficulties) and lower scores on measures of protective factors (i.e., grit, mindfulness, resilience, community integration and social support); and (3) Age would moderate associations between adverse events and risk/protective correlates such that military-specific experiences and post-military difficulties will be more salient for younger Veterans than older Veterans.
Method
The data were analyzed from the 2019–2020 National Health and Resilience in Veterans Study (NHRVS), a nationally representative, population-based study of US military Veterans. Potential participants were drawn from a research panel of more than 50,000 households maintained by Ipsos, a survey research firm. Of the 7,860 Veterans invited to participate, 4,069 (51.7%) participated in the current study. All assessments were conducted using an anonymous, online survey. Post-stratification weights were computed using recent Census data from the 2019 Veterans Supplement of the Current Population Survey to permit generalizability of study results to the national population of US Veterans. Comprehensive methodological details of this study are available elsewhere (Tsai, Schick, Hernandez, & Pietrzak, 2020).
Participants
Participants included 4,069 Veterans divided into “Younger” (under the age of 40; n = 446) and “Older” (age 40+; n = 3,623) Veterans. Table 1 details demographic and military service information by age group.
Table 1.
Sample characteristics
| Younger Veterans (n = 446) Weighted M (SD) or n (Weighted %) |
Older Veterans (n = 3,623) Weighted M (SD) or n (Weighted %) |
Statistical Comparison | |
|---|---|---|---|
| Demographics | |||
| Age | 33.9 (4.2) | 65.7 (12.8) | t(4,067) = −51.94, p < .001, d = 3.33 |
| Male | 332 (74.4%) | 3,339 (92.2%) | χ2(1) = 141.33, p < .001 |
| Race (% White) | 295 (66.4%) | 2,881 (79.5%) | χ2(1) = 40.13, p < .001 |
| Marital Status (% Married) | 239 (71.6%) | 2,593 (53.7%) | χ2(1) = 51.05, p < .001 |
| Educational Attainment | 122 (27.4%) Highschool or less 123 (27.6%) Some College 66 (14.7%) Associates 98 (21.9%) Bachelors 24 (5.5%) Masters 12 (2.8%) Professional |
1,120 (30.9%) Highschool or less 868 (23.9%) Some College 441 (12.2%) Associates 654 (17.2%) Bachelors 443 (12.2%) Masters 127 (3.5%) Professional |
χ2(6) = 33.40, p < .001 |
| Currently Covered by VA Healthcare |
188 (42.2%) |
1,151 (31.8%) |
χ2(1) = 19.25, p < .001 |
| Military Service | |||
| Years of Service | 4.0 (1.3) | 4.4 (1.9) | t(4,067) = −5.04, p < .001, d = −0.29 |
| % Drafted | 3 (0.7%) | 442 (12.2%) | χ2(1) = 10.81, p = .001 |
| Deployment Frequency | 1.6 (0.9) | 4.6 (26.9) | t(1,398) = −1.65, p = .01, d = −0.16 |
| Combat Exposure | 230 (51.7%) | 1190 (32.9%) | χ2(1) = 61.36, p < .001 |
| Conflicts Serveda |
198 (86.8%) OEF/OIF/OND 20 (8.7%) Other Conflicts |
20 (1.7%) World War II 59 (5.0%) Korean War 592 (50.2%) Vietnam 248 (21.0%) Persian Gulf 277 (23.5%) OEF/OIF/OND 124 (10.5%) Other Conflicts |
– |
| Adverse Events | |||
| Suicide Attempt | 61 (13.9%) | 97 (2.7%) | χ2(1) = 130.07, p < .001 |
| Number of Attemptsb | 1.9 (0.9) | 2.1 (2.1) | t(147) = −0.73, p = .47, d = −0.13 |
| Age of Most Recent Attemptb | 24.9 (5.4) | 31.4 (14.2) | t(151) = −3.36, p = .001, d = −0.61 |
| Homelessness | 100 (22.5%) | 315 (8.7%) | χ2(1) = 81.76, p < .001 |
| Total Duration of Homelessnessc | 2.4 (2.0) | 3.1 (4.8) | t(215) = −1.01, p = .31, d = −0.20 |
| Years from Service to Homelessnessc | 3.2 (3.8) | 9.1 (11.1) | t(303) = −3.82, p < .001, d = −0.71 |
| Utilized VA Homelessness Servicesc | 30 (30.1%) | 65 (21.0%) | χ2(1) = 4.10, p = .04 |
| Arrest | 161 (36.3%) | 1134 (31.4%) | χ2(1) = 4.23, p = .04 |
| Number of Arrestsd |
1.8 (1.3) |
2.3 (5.2) |
t(1238) = −1.33, p = .18, d = −0.15 |
| Personality Characteristics | |||
| Grit | 3.5 (0.7) | 3.8 (0.6) | t(4,031) = −9.74, p < .001, d = −0.46 |
| Mindfulness | 4.3 (1.3) | 5.1 (1.1) | t(4,061) = −15.39, p < .001, d = −0.72 |
| Resilience | 37.0 (7.8) | 39.3 (6.7) | t(4,045) = −6.75, p < .001, d = −0.32 |
| Impulsiveness | 16.9 (4.2) | 14.44 (4.0) | t(4,049) = 11.97, p < .001, d = 0.59 |
| Hostility |
4.1 (5.1) |
1.5 (2.9) |
t(4,063) = 16.38, p < .001, d = 0.64 |
| Adverse Childhood Experiences |
2.3 (2.3) |
1.4 (1.9) |
t(4,056) = 9.36, p < .001, d = 0.44 |
| Military Specific Experiences | |||
| Perceived Effect of Military Experience | 1.3 (1.7) | 2.1 (1.3) | t(4,046) = −11.28, p < .001, d = −0.51 |
| Military Sexual Trauma | 0.2 (0.4) | 0.1 (0.2) | t(4,053) = 8.66, p < .001, d = 0.38 |
| Moral Injurya |
21.8 (10.0) |
17.5 (9.8) |
t(1,395) = 6.09, p = .21, d = 0.44 |
| Post-Military Experiences | |||
| Community Integration | 3.7 (1.9) | 4.4 (1.8) | t(4,054) = −4.67, p = .01, d = −0.39 |
| Social Support Received | 17.2 (5.3) | 18.7 (5.1) | t(4,051) = −5.85, p = .33, d = −0.29 |
| Psychosocial Functioning Difficulties | 1.4 (1.2) | 0.6 (0.9) | t(3,771) = −17.48, p < .001, d = 0.78 |
aFor Veterans reporting any combat exposure.
bFor Veterans reporting any prior suicide attempt.
cFor Veterans reporting any prior homelessness.
dFor Veterans reporting any prior arrest.
Measures
Adverse event history
Adverse event history was assessed through respondent’s self-report. History of suicidal behavior was assessed using the Suicide Behavior Questionnaire-Revised (Osman et al., 2001) and an additional item to assess frequency of prior suicide attempts, “How many times have you tried to kill yourself?” (coded dichotomously to indicate the presence of prior suicide attempt[s]). Histories of prior homelessness and justice involvement were assessed using items similar to those used in NESARC-III (Chen, Slater, Castle, & Grant, 2016), “In your entire adult life, have you ever been homeless (i.e., stayed in a shelter, transitional housing, outdoors, or some other unstable housing situation)?” and “In your lifetime, were you ever arrested?”
Risk and protective factors
In accordance with research suggesting histories of suicide, homelessness, and justice-involvement share common risk and protective factors (Blonigen et al., 2016; Fogle et al., 2020; Holliday et al., 2020; Posey, 2009; Tsai & Rosenheck, 2015; Tsai et al., 2018), a range of self-report measures were used to assess personality, adverse childhood experiences, military-specific experiences, and post-military factors commonly associated with history of adverse events. All included measures demonstrated strong psychometric properties across this (α = 0.63–0.90) and other samples (Bryan et al., 2016; Dube et al., 2003; Fields et al., 2015; Giangrasso & Casale, 2014; González, Sierra, Martínez, Martínez-Molina, & Ponce, 2015; Hoe & Brekke, 2009; Kleiman et al., 2020; Muenks, Wigfield, Yang, & O’Neal, 2017; Osman, Lamis, Bagge, Freedenthal, & Barnes, 2016; Ross, Waterhouse-Bradley, Contractor, & Armour, 2018). See Table 2 for a summary of these measures.
Table 2.
Measures of Veteran risk and protective factors
| Construct | Measure | Scoring | α |
|---|---|---|---|
| Personality | |||
| Grit | Short Grit Scale (Duckworth & Quinn, 2009) | 5-point Likert scale of “Very much like me” to “Not like me at all” | 0.78 |
| Mindfulness | 3 items from the Mindful Attention Awareness Scale (Brown & Ryan, 2003; Osman et al., 2016) | 6-point Likert scale of “Almost always” to “Almost never” | 0.90 |
| Resilience | 10-item Connor-Davidson Resilience Scale (Campbell‐Sills & Stein, 2007) | 5-point Likert scale of “Not at all true” to “Truly nearly all the time” | 0.90 |
| Impulsiveness | Barratt Impulsiveness Scale-Brief (Steinberg, Sharp, Stanford, & Tharp, 2013) | ||
| Hostility |
Brief Symptom Inventory-18, Hostility Subscale (Derogatis & Melisaratos, 1983) |
5-point Likert scale of “Not at all” to “Extremely” |
0.90 |
| Adverse Childhood Experiences |
Adverse Childhood Experiences Questionnaire (Felitti et al., 1998) |
Dichotomous items summed for total score |
0.76 |
| Military-Specific Experiences | |||
| Perceived Effect of Military Experience | “How has being in the military affected your life?” (Isaacs et al., 2017) | 7-point Likert scale of “Strong negative effect” to “Strong positive effect” | N/A |
| Military Sexual Assault | “When you were in the military, did you ever receive unwanted, threatening, or repeated sexual attention (for example, touching, cornering, pressure for sexual favors, or inappropriate verbal remarks, etc.)?” and “When you were in the military, did you have sexual contact against your will or when you were unable to say no (for example, after being forced or threatened or to avoid other consequences)?” (McIntyre et al., 1999) | Dichotomous responding; summed for total score | 0.63 |
| Moral Injurya |
Moral Injury Event Scale (MIES; Nash et al., 2013) |
7-point Likert scale of “Strongly disagree” to “Strongly agree” |
0.90 |
| Post-Military Experiences | |||
| Community Integration | “I feel well integrated in my community (e.g., regularly participate in community activities)” | 8-point Likert scale of “Strongly Disagree” to “Strongly Agree” | N/A |
| Social Support Received | Medical Outcomes Study Social Support Survey, “Social Support Received” subscale (Sherbourne & Stewart, 1991) | 5-point Likert scale of “None of the time” to “All of the time” | 0.89 |
| Psychosocial Functioning Difficulties | Brief Inventory of Psychosocial Functioning (Marx et al., 2019) | 7-point Likert scale of “Never” to “Always” | 0.85 |
aOnly administered to Veterans reporting combat exposure, n = 1,420.
Data analysis plan
Hypothesis 1. Pearson chi-square difference tests were conducted to compare the prevalence of prior suicide attempt, homelessness, and arrest in younger (aged <40) versus older (aged ≥40) Veterans.
Hypothesis 2. Correlation analyses were conducted to examine associations between the history of adverse events and identified risk and protective factors (i.e., personality traits, ACEs, military-specific experiences and post-military experiences).
Hypothesis 3. Multivariate analyses of variance were conducted to examine the potential moderating effect of age on associations between Veterans’ histories of each adverse event and risk/protective variables. Three analyses were conducted – one for each adverse event – with all risk/protective variables entered simultaneously. Because demographic composition of Veteran cohorts has changed considerably over time (VA, 2016b), gender, education, and military-service duration were included as covariates in multivariate analyses.
Given the large sample size and multiple analyses, a conservative alpha (.01) was used to determine statistical significance. Sampling weights were applied in inferential analyses to permit generalizability of results to the US Veteran population.
Results
Descriptive analyses
The prevalence of prior suicide attempt and homelessness was highest among Veterans aged 30–39 (Figure 1), and nearly all Veterans who reported prior suicide attempts described their most recent attempts as occurring before age 40 (including 77.5% of Veterans aged ≥40). In chi-square analyses, younger Veterans were significantly more likely than older Veterans to report a history of suicide attempt (13.9% versus 2.7%; χ2[1] = 130.07, p < .001) and homelessness (22.5% versus 8.7%; χ2[1] = 81.76, p < .001), but not arrest (36.3% versus 31.4%; χ2[1] = 4.23, p = .04). They also tended to score higher on measures of risk factors and lower on measures of protective factors (Table 1).
Figure 1.
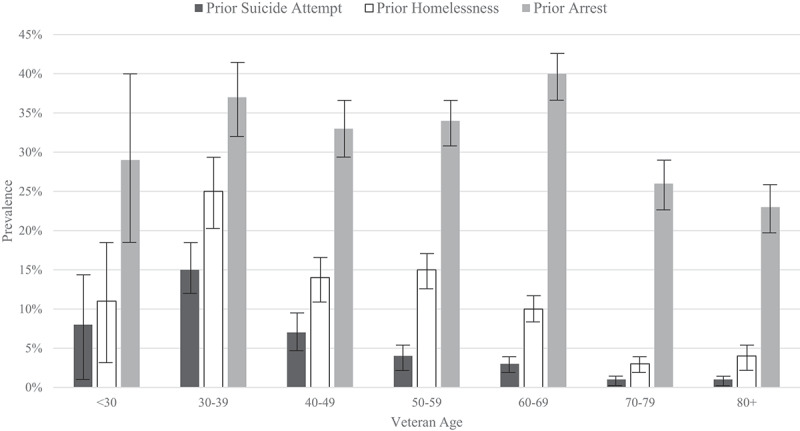
Adverse events by Veteran age.
Note: Error bars represent 95% confidence intervals.
Correlation analyses
Small, yet statistically significant correlations were observed between suicide attempt, homelessness, and arrest histories, suggesting that Veterans who experienced at least one prior adverse event were more likely to experience others. Adverse events generally showed hypothesized associations with risk and protective factors, with the strongest associations for homelessness and the weakest ones for arrest. Demographic comparisons suggested prior adverse events were most commonly reported by Veterans who were younger, unmarried, less educated, and members of a racial/ethnic minority. Prior suicidal behavior and homelessness were more common among Veterans who were women, had briefer duration of military service, and served in the OEF/OIF/OND conflict, whereas prior arrest was more common among Veteran men. However, the magnitude of associations of adverse events to demographic and service-related variables is generally small (Table 3).
Table 3.
Correlations of adverse events and risk and protective factors
| History of Suicide Attempt | History of Homelessness | History of Arrest | |
|---|---|---|---|
| Adverse Events | |||
| Suicide Attempt | – | ||
| Homelessness | .23** | – | |
| Arrest |
.05* |
.21** |
– |
| Demographics | |||
| Age | −.19** | −.20** | −.08** |
| Gendera | −.09** | −.08** | .06** |
| Race/ethnicityb | −.02 | −.12** | −.09** |
| Marital Statusc | −.08** | −.17** | −.11** |
| Educational Attainment |
−.02 |
−.09** |
−.12** |
| Military Service Characteristics | |||
| Years of Service | −.05* | −.08** | −.03 |
| Deployment Frequency | .02 | −.03 | .05 |
| Combat Exposure | .01 | .01 | .04 |
| OEF/OIF/OND Serviced |
.12** |
.10** |
.70 |
| Personality | |||
| Grit | −.08** | −.12** | .06** |
| Mindfulness | −.17** | −.18** | −.08** |
| Resilience | −.11** | −.12** | −.05* |
| Impulsiveness | .12** | .15** | .10** |
| Hostility |
.17** |
.23** |
.12** |
| Adverse Childhood Experiences |
.21** |
.35** |
.20** |
| Military Specific Experiences | |||
| Perceived Effect of Military Experience | −.11** | −.13** | −.04 |
| Military Sexual Trauma | .10** | .11** | .03 |
| Moral Injury |
.09* |
.18** |
.13** |
| Post-Military Experiences | |||
| Community Integration | −.11** | −.16** | −.13** |
| Social Support Received | −.12** | −.17** | −.10** |
| Psychosocial Functioning Difficulties | .17** | .24** | .09** |
*p < .01, **p < .001
aReference group male; bReference group White; cReference group married.
dOnly reported by Veterans with prior combat exposure.
Moderation analyses
After controlling for gender, educational attainment, and service duration, age cohort significantly moderated relations of prior suicide attempt (Wilks λ = 0.94, F[12, 1245] = 6.19, p < .001) and homelessness (Wilks λ = 0.95, F[12, 1249] = 5.12, p < .001), but not arrest (Wilks λ = 0.98, F[12, 1250] = 2.04, p = .02) to risk and protective factors in omnibus multivariate analyses of variance.
Follow-up univariate analyses suggested that after controlling for gender, educational attainment, and service duration, age cohort significantly moderated relations of prior suicide attempt to resilience (F[1, 1256] = 14.28, p < .001), grit (F[1, 1256] = 10.05, p < .01), perceived effect of military experience on one’s life (F[1, 1256] = 14.83, p < .001), MST (F[1, 1256] = 18.97, p < .001), and social support (F[1, 1256] = 9.17, p < .01). The patterns of these statistical interactions were remarkably consistent; strength of association between each factor and prior suicide attempt was weaker among younger Veterans than older Veterans (Figure 2). All other moderation effects were not statistically significant.
Figure 2.
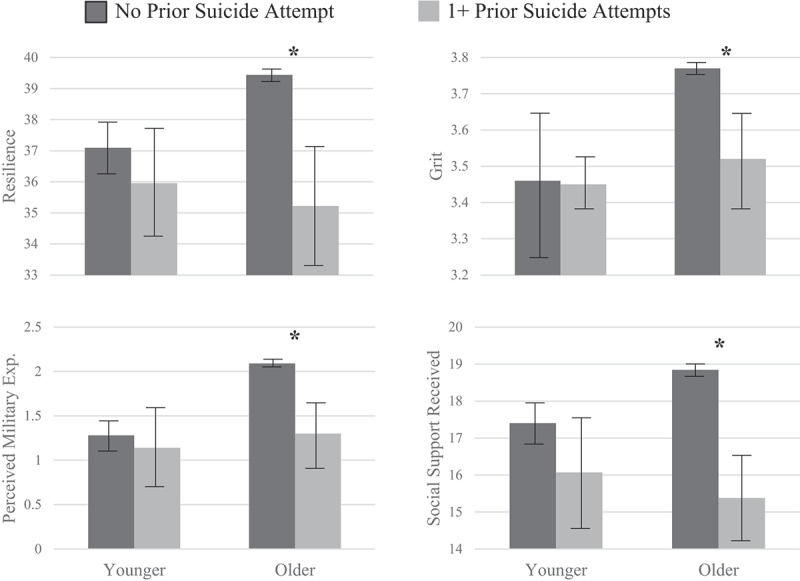
Moderating effect of age on relation of suicide attempt history to risk/protective factors.
Note: Error bars represent 95% confidence intervals. Statistically significant differences at p < .05 denoted by asterisks.
Similarly, age cohort significantly moderated relations of prior homelessness to resilience (F[1, 1260] = 11.72, p < .01), impulsiveness (F[1, 1260] = 14.50, p < .001), and social support (F[1, 1260] = 9.97, p < .01). Like suicide attempts, the strength of associations was notably weaker among younger Veterans than older Veterans (Figure 3). All other moderation effects were not statistically significant.
Figure 3.
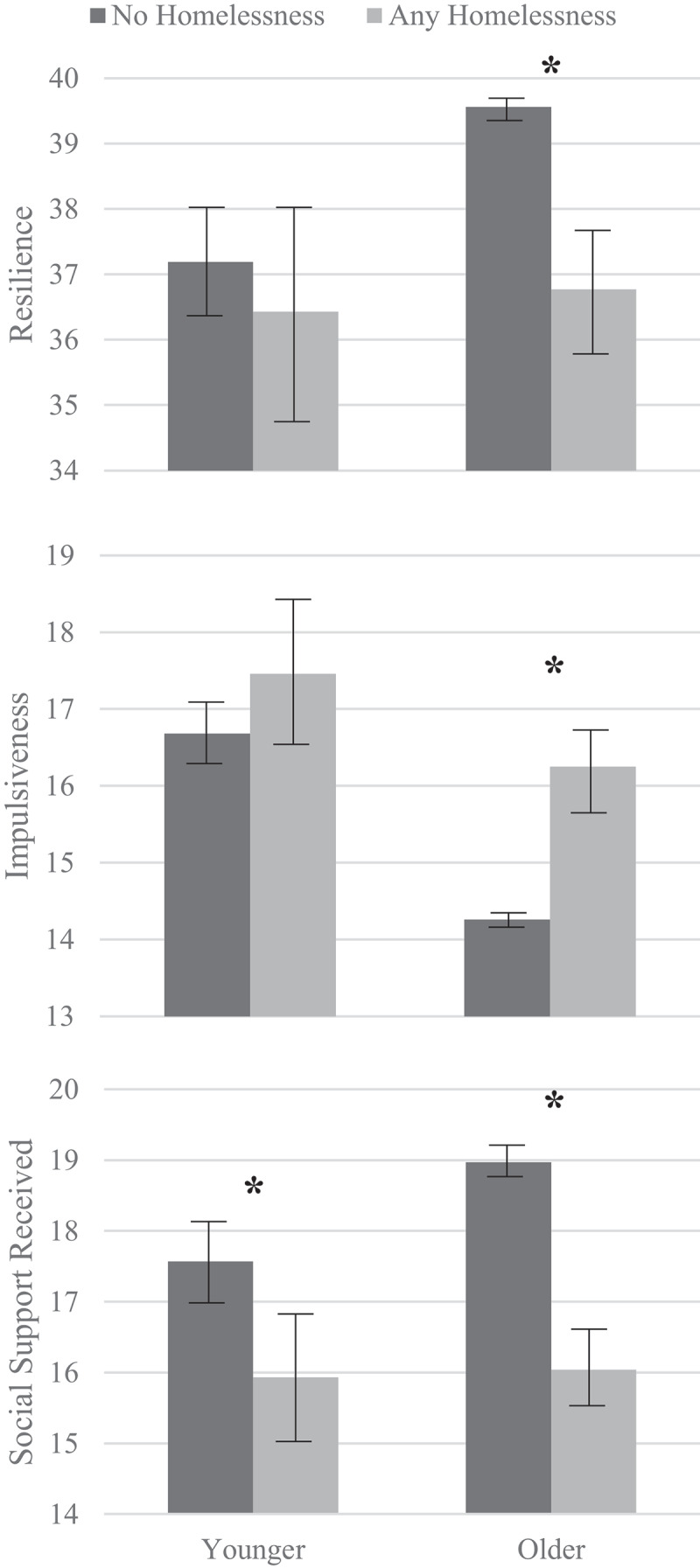
Moderating effect of age on relation of homelessness history to risk/protective factors.
Note: Error bars represent 95% confidence intervals. Statistically significant differences at p < .05 denoted by asterisks.
Post-hoc analysis
Post-hoc logistic regression analyses sought to explore whether associations between age cohorts and histories of suicidal behavior, homelessness, and arrest may be attributed, at least in part, to the relatively higher representation of OEF/OIF/OND Veterans and combat-exposed Veterans in the younger age cohort. Results revealed that even after adjusting for combat exposure, the younger age cohort had 83% greater odds of having a history of suicidal behavior (95% CI = 76–88%, p < .01) and 68% greater odds of having a history of homelessness (95% CI = 59–75%, p < .01) relative to the older age cohort. The association between age cohort and history of arrest was not significant after adjusting for combat exposure (p = .07). Similarly, after adjusting for involvement in the OEF/OIF/OND conflict, the younger age cohort had 65% greater odds of having a history of homelessness (95% CI = 44–78%, p < .01), though associations with histories of suicide (p = .05) and arrest (p = .02) were not significant.
In contrast, after adjusting for age cohort, combat exposure was not associated with histories of suicidal behavior (p = .55), homelessness (p = .14), or arrest (p = .04). Involvement in the OEF/OIF/OND conflict was associated with 2.5-fold greater odds of prior suicidal behavior (95% CI = 1.3–4.5, p < .01), though associations with homelessness (p = .47) and arrest (p = .42) were not significant.
Discussion
The results contribute to the growing literature on younger Veterans by highlighting differential associations of common risk and protective factors to suicidal behavior, homelessness, and criminal-justice involvement across Veteran age cohorts. In this nationally representative sample, younger Veterans were more likely to report prior suicide attempt(s) (13.9%) and homelessness (22.5%) than older Veterans (2.7% and 8.7%, respectively). These rates highlight the importance of preventative services for younger Veterans. Accordingly, recent efforts have expanded mental health services for Veterans transitioning from military to civilian life (e.g., Executive Order 13,822, 2018; Hannon Act, 2019), representing expansion of some VA-based services. However, only 20% of Veterans use the VA as their primary source of health care (Meffert et al., 2019), and some at-risk, younger Veterans are ineligible for VA-based care due to brief military service and/or less-than-honorable discharge (both associated with elevated risk for younger Veterans; Reger et al., 2015). Some exceptions aim to mitigate barriers for Veterans facing significant needs regardless of discharge status; for example, the Veteran HOUSE Act of 2020 allows Veterans with other-than-honorable discharges to receive housing support through the HUD-Veterans Affairs Supportive Housing program (H.R. 2398). However, the effectiveness of such exceptions in mitigating risk for young, at-risk Veterans remains undetermined. Community-based initiatives driven by various stakeholders (e.g., Department of Veterans Affairs, Veteran service organizations, employers, and higher education) are therefore needed to effectively engage this at-risk group (Geraci et al., 2020).
The findings are consistent with previous findings suggesting that younger Veterans experience higher rates of suicide (e.g., VA, 2020) and lower or similar rates of justice-involvement (e.g., Bronson et al., 2015) in comparison to other Veteran age cohorts. Our findings also reaffirm the notable risk for homelessness among younger Veterans (Spinola, Hoff, & Tsai, 2021; Tsai, Pietrzak, & Szymkowiak, 2021) and the importance of VA services for younger cohorts. Because data on younger Veterans unconnected to VA services are largely limited to epidemiological surveys like this study, further research on this potentially high-risk group is necessary. Importantly, such research should further clarify potential causes of observed elevations. Although post-hoc analyses appear to support a generational explanation rather than a service-related explanation, continued research is needed to further investigate the role of potential confounding variables, such as changes over time in mental health stigma, military recruitment practices, resource availability, accessibility and utilization of benefits, and larger cultural shifts. Given the common delays between data collection and analysis, such research should prioritize up-to-date datasets to ensure adequate representation of younger Veterans in study samples.
In line with elevated prevalence of prior suicide and homelessness in younger Veterans, this group also scored higher on measures of general risk factors and lower on measures of general protective factors relative to older Veterans. Such differences broadly suggest that younger Veterans are more trauma-exposed, less resilient, and less socially connected than earlier age cohorts. While results highlight implications for suicide and homelessness specifically, these data also have implications for Veterans’ mental health more broadly. Given their relatively high-risk profile, younger Veterans are likely to struggle to cope and problem solve effectively with life stressors; therefore, they will likely also endure higher rates of mental health disorders and require more support and resources than previous age cohorts. Continued research on this age cohort of Veterans is therefore warranted and necessary.
Observed differences in personality are consistent with research on the paradox of aging, which suggests that changes throughout the course of aging contribute to generally better psychological functioning among older Veterans despite declines in cognitive and physical health (Jeste et al., 2013; Pietrzak, Tsai, Kirwin, & Southwick, 2014; Thomas et al., 2016). Differences in post-military experiences and time from service to homelessness are also consistent with the growing literature on military-to-civilian transitional stress among younger Veterans (Pew Research Center, 2011; Sokol et al., 2021; Tsai et al., 2020), underscoring their difficulties navigating community reintegration after military service.
Despite the consistencies between prevalence of prior adverse events and scores of risk/protective correlates, however, moderation analyses suggested younger Veterans with distinctly different histories of suicidal behavior and/or homelessness scored similarly on measures of resilience, grit, impulsiveness, perceived effect of military experience on one’s life, and social support. While these findings are inconsistent with hypotheses and recent suicide prevention initiatives (e.g., Executive Order 13,822, 2018; 116th Congress, 2020), which generally assume factors associated with military service and transitional stress (e.g., deployment stress and general psychosocial functioning) have more salient effects for younger Veterans, they align with previous research suggesting the relevance of risk/protective factors may vary as a function of age in Veterans (Weiner et al., 2016).
In contrast, moderation analyses also suggested that ACEs, MST, moral injury, mindfulness, hostility, and community integration were similarly associated with suicide and homelessness across age cohorts. Initiatives to mitigate Veteran suicide and homelessness may therefore benefit from prioritizing interventions that target these factors. For example, many psychotherapies for suicide risk now integrate interventions for trauma, mindfulness, and interpersonal relationships, and show promising results in Veteran samples (e.g., Harned, Korslund, & Linehan, 2014; Meyers et al., 2017). Similarly, community-based, peer-to-peer programming often increases community integration, decreases trauma-related symptoms, and engages Veterans unconnected to VA-based services and/or otherwise hesitant of mental health services (e.g., ETS Sponsorship Program; Geraci et al., 2019). Descriptive statistics suggest that ACEs, MST, poor mindfulness, hostility, and poor community integration are particularly pronounced for younger Veterans; therefore, such interventions are likely especially relevant for this age cohort.
Limitations & future directions
Although the large, nationally representative sample maximizes generalizability of results to the broader Veteran population, the comparatively fewer number of younger Veterans and low base rates of adverse events limited statistical power to detect small yet potentially meaningful associations. Relatedly, the procedures did not sample from Veterans institutionalized or homeless at the time of data collection. Therefore, Veterans experiencing adverse events that resulted in more severe or prolonged consequences were under-represented in the current sample, limiting the scope of analysis. Future research would therefore benefit from replication in high-risk, institutionalized, and/or demographically matched samples.
Also, because assessments were cross-sectional, retrospective, and completed with Veterans of different ages, results cannot inform temporal/causal inferences. While risk/protective variables may be associated with a history of adverse events, analyses cannot ascertain whether factors occurred prior to or following adverse events nor can they inform inferences about temporal/causal associations between factors and adverse events. It is possible, for example, that a Veteran’s poor resilience contributed to their engagement in suicidal behavior. However, it is also possible that engagement in suicidal behavior impaired subsequent resilience or that an unassessed variable (e.g., generational trends or political climate) impacted both risk/protective correlations and adverse events for Veterans. Relatedly, whereas historical risk/protective factors (e.g., ACEs) are static across time, other factors (e.g., social support) may change considerably. It is therefore possible that relations of dynamic risk/protective variables to histories of adverse events are less stable than those of static risk/protective factors. Continued research using longitudinal study designs is needed to clarify temporal order and potential causal relationships among these variables.
Similarly, the life-history approach to the assessment of adverse events likely contributed to an underestimation of the full potential for adverse event(s) over the lifetime, particularly for younger Veterans. This underestimation is notable and suggests that observed elevations in suicidal behavior and homelessness may become more salient over time for Veterans currently in the youngest age cohort. Accordingly, among older Veterans, nearly 25% of most-recent suicide attempts occurred after age 40, and homelessness occurred, on average, nearly a decade after military service. Thus, while age was the primary independent variable in analyses, it could also be a notable confound. With age come many other factors not assessed by current analyses (e.g., changes in employment, family dynamics, etc.). Longitudinal research is needed to fully understand the long-term consequences of younger Veterans’ elevated risk characteristics.
Finally, many unassessed factors may account for the observed differences between younger and older Veteran cohorts. Although post-hoc analyses appear to suggest a generational explanation for results (rather than a service-era explanation), these analyses only included Veterans reporting combat exposure and did not include consideration of other service-era factors, such as military recruitment policies, introduction of the all-volunteer force, political climate, and wartime versus peacetime. Similarly, analyses did not account for larger cultural shifts, such as changes in mental health stigma or availability of social services, that likely had differential effects across age cohorts. Clarifying the role of these larger, systemic patterns through future research promises to aid in prospective predictions of risk for future Veteran cohorts.
The findings should also motivate research into potential mediators of the relation between Veteran age and adverse events. For example, younger Veterans experience higher rates of trauma and post-military difficulties than other-age Veterans, and these factors appear associated with higher rates of adverse events across ages. Future research may therefore investigate the degree to which trauma and/or post-military difficulties explain younger Veterans’ elevated rates of adverse events.
Conclusions
This study examined suicide attempt, homelessness, and arrest history across younger and older Veteran age cohorts. Younger Veterans reported higher rates of prior suicide attempt, homelessness, and risk factors and fewer protective factors than older Veterans. Additionally, some traditional factors associated with suicidal behavior and homelessness were found to be less salient for younger Veterans, which may inform targeted prevention efforts for this group. The findings highlight the need for preventative homelessness and mental health services for younger Veterans.
Disclosure statement
Work for this article was supported by the Department of Veterans Affairs, Office of Academic Affiliations, VA Special MIRECC Fellowship Program in Advanced Psychiatry and Psychology, the Veterans Affairs National Center on Homelessness among Veterans, and by the VISN-2 MIRECC. The National Health and Resilience for Veterans Study was funded by the US Department of Veterans Affairs, National Center for PTSD. The views expressed here are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Data availability statement
The data that support the findings of this study are available from Robert Pietrzak, PhD, MPH at robert.pietrzak@yale.edu upon reasonable request https://www.vacsp.research.va.gov/CSPEC/Studies/INVESTD-R/Ntl-Health-Resilience-Veterans-Study.asp.
References
- 116th Congress . (2020, October 17). Commander John Scott Hannon Veterans Mental Health Care Improvement Act of 2019. Public Law No: 116–171.
- Blonigen, D. M., Bui, L., Elbogen, E. B., Blodgett, J. C., Maisel, N. C., Midboe, A. M., & Timko, C. (2016). Risk of recidivism among justice-involved Veterans: A systematic review of the literature. Criminal Justice Policy Review, 27(8), 812–837. doi: 10.1177/0887403414562602 [DOI] [Google Scholar]
- Blosnich, J. R., Dichter, M. E., Cerulli, C., Batten, S. V., & Bossarte, R. M. (2014). Disparities in adverse childhood experiences among individuals with a history of military service. JAMA Psychiatry, 71(9), 1041–1048. doi: 10.1001/jamapsychiatry.2014.724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronson, J., Carson, E. A., Noonan, M., & Berzofsky, M. (2015). Veterans in prison and jail.U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics (NCJ 249144). Retrieved from https://www.bjs.gov/index.cfm?ty=pbdetail&id=5479
- Brown, K. W., & Ryan, R. M. (2003). The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84(4), 822848. doi: 10.1037/0022-3514.84.4.822 [DOI] [PubMed] [Google Scholar]
- Bryan, C. J., Bryan, A. O., Anestis, M. D., Anestis, J. C., Green, B. A., Etienne, N., … Ray-Sannerud, B. (2016). Measuring moral injury: Psychometric properties of the moral injury events scale in two military samples. Assessment, 23(5), 557–570. doi: 10.1177/1073191115590855 [DOI] [PubMed] [Google Scholar]
- Campbell‐Sills, L., & Stein, M. B. (2007). Psychometric analysis and refinement of the Connor– Davidson Resilience Scale (CD‐RISC): Validation of a 10‐item measure of resilience. Journal of Traumatic Stress, 20(6), 1019–1028. doi: 10.1002/jts.20271 [DOI] [PubMed] [Google Scholar]
- Center, P. R. (2011). Social & demographic trends, the military-civilian gap: War and sacrifice in the post-9/11 era. Retrived from https://www.pewresearch.org/social-trends/2011/10/05/war-and-sacrifice-in-the-post-911-era/.
- Chen, C. M., Slater, M. E., Castle, I.-J. P., & Grant, B. F. (2016). Alcohol use and alcohol use disorders in the United States: Main findings from the 2012–2013 national epidemiologic survey on alcohol and related conditions-III (NESARC-III). U.S. Alcohol Epidemiologic Data Reference Manual, Volume 10, NIH Publication No. 16-AA-8020. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism. [Google Scholar]
- Department of Housing and Urban Development . (2021). 2020 CoC homeless populations and subpopulations report: All states, territories, Puerto Rico, and Dc. US Department of Housing and Urban Development. Retrieved from: https://files.hudexchange.info/reports/published/CoC_PopSub_NatlTerrDC_2020.pdf [Google Scholar]
- Department of Veterans Affairs (2016). Veteran population projection model 2016: Executive summary. Retrieved from https://www.va.gov/vetdata/docs/Demographics/New_Vetpop_Model/Vetpop16_Executive_Summary.pdf
- Department of Veterans Affairs . (2020). 2020 national veteran suicide prevention annual report. Department of Veterans Affairs, Office of Mental Health and Suicide Prevention. Retrieved from: https://www.mentalhealth.va.gov/suicide_prevention/data.asp
- Department of Veterans Affairs . (2021). FY 2021 budget submission. Retrieved from: https://www.va.gov/budget/docs/summary/fy2021VAbudgetInBrief.pdf
- Derogatis, L. R., & Melisaratos, N. (1983). The brief symptom inventory: An introductory report. Psychological Medicine, 13(3), 595–605. doi: 10.1017/S0033291700048017 [DOI] [PubMed] [Google Scholar]
- Dube, S. R., Felitti, V. J., Dong, M., Chapman, D. P., Giles, W. H., & Anda, R. F. (2003). Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The adverse childhood experiences study. Pediatrics, 111(3), 564–572. doi: 10.1542/peds.111.3.564 [DOI] [PubMed] [Google Scholar]
- Duckworth, A. L., & Quinn, P. D. (2009). Development and validation of the Short Grit Scale (GRIT–S). Journal of Personality Assessment, 91(2), 166–174. doi: 10.1080/00223890802634290 [DOI] [PubMed] [Google Scholar]
- Edwards, E. R., Barnes, S., Govindarajulu, U., Geraci, J., & Tsai, J. (2020). Mental health and substance use patterns associated with lifetime suicide attempt, incarceration, and homelessness: A latent class analysis of a nationally representative sample of US Veterans. Psychological Services, Advance online publication doi: 10.1037/ser0000488 [DOI] [PubMed] [Google Scholar]
- Edwards, E. R., Gromatsky, M., Sissoko, D. R., Hazlett, E. A., Sullivan, S. R., Geraci, J., & Goodman, M. (2020). Arrest history and psychopathology among Veterans at risk for suicide. Psychological Services, Advance online publication doi: 10.1037/ser0000454 [DOI] [PubMed] [Google Scholar]
- Exec. Order No. 13822, 3 C.F.R., Supporting Our Veterans During Their Transition From Uniformed Service to Civilian Life . (2018, January 9)
- Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., … Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. doi: 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Fields, S., Edens, J. F., Smith, S. T., Rulseh, A., Donnellan, M. B., Ruiz, M. A., … Douglas, K. S. (2015). Examining the psychometric properties of the Barratt Impulsiveness Scale–Brief Form in justice-involved samples. Psychological Assessment, 27(4), 1211. doi: 10.1037/a0039109 [DOI] [PubMed] [Google Scholar]
- Fogle, B. M., Tsai, J., Mota, N., Harpaz-Rotem, I., Krystal, J. H., Southwick, S. M., & Pietrzak, R. H. (2020, December 9). The national health and resilience in Veterans study: A narrative review and future directions. Frontiers in Psychiatry, 11, 538218. doi: 10.3389/fpsyt.2020.538218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geraci, J., Goodman M., Seim R. (2019). ETS Sponsorship Program Helps Communities Fulfill Their Responsibility to Help Service Members Successfully Transition to Civilian Life. VAntage. Washington, DC: VA Office of Mental Health and Suicide Prevention. [Google Scholar]
- Geraci, J., Mobbs, M., Edwards, E. R., Doerries, B., Armstrong, N., Porcarelli, R., … Goodman, M. (2020). Expanded roles and recommendations for stakeholders to successfully reintegrate modern warriors and mitigate suicide risk. Frontiers in Psychology, 11, 1907. doi: 10.3389/fpsyg.2020.01907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giangrasso, B., & Casale, S. (2014). Psychometric properties of the medical outcome study social support survey with a general population sample of undergraduate students. Social Indicators Research, 116(1), 185–197. doi: 10.1007/s11205-013-0277-z [DOI] [Google Scholar]
- González, V. B. A., Sierra, M. T. C., Martínez, B. A., Martínez-Molina, A., & Ponce, F. P. (2015). An in-depth psychometric analysis of the Connor-Davidson resilience Scale: Calibration with rasch-andrich model. Health and Quality of Life Outcomes, 13(1), 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harned, M. S., Korslund, K. E., & Linehan, M. M. (2014). A pilot randomized controlled trial of dialectical behavior therapy with and without the dialectical behavior therapy prolonged exposure protocol for suicidal and self-injuring women with borderline personality disorder and PTSD. Behaviour Research and Therapy, 55, 7–17. doi: 10.1016/j.brat.2014.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoe, M., & Brekke, J. (2009). Testing the cross-ethnic construct validity of the Brief Symptom Inventory. Research on Social Work Practice, 19(1), 93–103. doi: 10.1177/1049731508317285 [DOI] [Google Scholar]
- Holliday, R., Martin, W. B., Monteith, L. L., Clark, S. C., & LePage, J. P. (2021). Suicide among justice-involved veterans: a brief overview of extant research, theoretical conceptualization, and recommendations for future research. Journal of Social Distress and Homelessness. 30(1), 41–49. [Google Scholar]
- Isaacs, K., Mota, N. P., Tsai, J., Harpaz-Rotem, I., Cook, J. M., Kirwin, P. D., … Pietrzak, R. H. (2017). Psychological resilience in U.S. military Veterans: A 2-year, nationally representative prospective cohort study. Journal of Psychiatric Research, 84, 301–309. doi: 10.1016/j.jpsychires.2016.10.017 [DOI] [PubMed] [Google Scholar]
- Jeste, D. V., Savla, G. N., Thompson, W. K., Vahia, I. V., Glorioso, D. K., Martin, A. S., … Depp, C. A. (2013). Association between older age and more successful aging: Critical role of resilience and depression. American Journal of Psychiatry, 170(2), 188–196. doi: 10.1176/appi.ajp.2012.12030386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiman, S. E., Bovin, M. J., Black, S. K., Rodriguez, P., Brown, L. G., Brown, M. E., … Marx, B. P. (2020). Psychometric properties of a brief measure of posttraumatic stress disorder–related impairment: The Brief Inventory of Psychosocial Functioning. Psychological Services, 17(2), 187–194. doi: 10.1037/ser0000306 [DOI] [PubMed] [Google Scholar]
- Kline, A., Ciccone, D. S., Falca-Dodson, M., Black, C. M., & Losonczy, M. (2011). Suicidal ideation among National Guard troops deployed to Iraq: The association with post-deployment readjustment problems. The Journal of Nervous and Mental Disease, 199(12), 914–920. doi: 10.1097/NMD.0b013e3182392917 [DOI] [PubMed] [Google Scholar]
- Marx, B. P., Schnurr, P. P., Lunney, C., Weathers, F. W., Bovin, M. J., & Keane, T. M. (2019). The brief inventory of psychosocial functioning (B-IPF). [Measurement instrument]. Retrived from: https://www.ptsd.va.gov/professional/assessment/documents/B-IPF.pdfs
- McIntyre, L. M., Butterfield, M. I., Nanda, K., Parsey, K., Stechuchak, K. M., McChesney, A. W., … Bastian, L. A. (1999). Validation of a trauma questionnaire in veteran women. Journal of General Internal Medicine, 14(3), 186–189. doi: 10.1046/j.1525-1497.1999.00311.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meffert, B. N., Morabito, D. M., Sawicki, D. A., Hausman, C., Southwick, S. M.Pietrzak, R. H., & Heinz, A. J. (2019). US Veterans who do and do not utilize Veterans affairs health care services. The Primary Care Companion for CNS Disorders, 21(1), 1. doi: 10.4088/PCC.18m02350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyers, L., Voller, E. K., McCallum, E. B., Thuras, P., Shallcross, S., Velasquez, T., & Meis, L. (2017). Treating Veterans with PTSD and borderline personality symptoms in a 12-week intensive outpatient setting: Findings from a pilot program. Journal of Traumatic Stress, 30(2), 178–181. doi: 10.1002/jts.22174 [DOI] [PubMed] [Google Scholar]
- Muenks, K., Wigfield, A., Yang, J. S., & O’Neal, C. R. (2017). How true is grit? Assessing its relations to high school and college students’ personality characteristics, self-regulation, engagement, and achievement. Journal of Educational Psychology, 109(5), 599–620. doi: 10.1037/edu0000153 [DOI] [Google Scholar]
- Nash, W. P., Marino Carper, T. L., Mills, M. A., Au, T., Goldsmith, A., & Litz, B. T. (2013). Psychometric evaluation of the moral injury events scale. Military Medicine, 178(6), 646–652. doi: 10.7205/MILMED-D-13-00017 [DOI] [PubMed] [Google Scholar]
- Osman, A., Bagge, C. L., Gutierrez, P. M., Konick, L. C., Kopper, B. A., & Barrios, F. X. (2001). The suicidal behaviors questionnaire-revised (SBQ-R): Validation with clinical and nonclinical samples. Assessment, 8(4), 443–454. doi: 10.1177/107319110100800409 [DOI] [PubMed] [Google Scholar]
- Osman, A., Lamis, D. A., Bagge, C. L., Freedenthal, S., & Barnes, S. M. (2016). The mindful attention awareness scale: Further examination of dimensionality, reliability, and concurrent validity estimates. Journal of Personality Assessment, 98(2), 189–199. doi: 10.1080/00223891.2015.1095761 [DOI] [PubMed] [Google Scholar]
- Pietrzak, R. H., Tsai, J., Kirwin, P. D., & Southwick, S. M. (2014). Successful aging among older Veterans in the United States. The American Journal of Geriatric Psychiatry, 22(6), 551–563. doi: 10.1016/j.jagp.2012.11.018 [DOI] [PubMed] [Google Scholar]
- Posey, S. (2009). Veterans and suicide: A review of potential increased risk. Smith College Studies in Social Work, 79(3–4), 368–374. doi: 10.1080/00377310903131447 [DOI] [Google Scholar]
- Reger, M. A., Smolenski, D. J., Skopp, N. A., Metzger-Abamukang, M. J., Kang, H. K., Bullman, T. A., … Gahm, G. A. (2015). Risk of suicide among US military service members following Operation Enduring Freedom or Operation Iraqi Freedom deployment and separation from the US military. JAMA Psychiatry, 72(6), 561–569. doi: 10.1001/jamapsychiatry.2014.3195 [DOI] [PubMed] [Google Scholar]
- Ross, J., Waterhouse-Bradley, B., Contractor, A. A., & Armour, C. (2018). Typologies of adverse childhood experiences and their relationship to incarceration in US military Veterans. Child Abuse & Neglect, 79, 74–84. doi: 10.1016/j.chiabu.2018.01.023 [DOI] [PubMed] [Google Scholar]
- Sherbourne, C. D., & Stewart, A. L. (1991). The MOS social support survey. Social Science & Medicine, 32(6), 705–714. doi: 10.1016/0277-9536(91)90150-B [DOI] [PubMed] [Google Scholar]
- Sokol, Y., Gromatsky, M., Edwards, E. R., Greene, A. L., Geraci, J. C., Harris, R. E., & Goodman, M. (2021). The deadly gap: Understanding suicide among Veterans transitioning out of the military. Psychiatry Research, 300, 113875. Advance online publication doi: 10.1016/j.psychres.2021.113875 [DOI] [PubMed] [Google Scholar]
- Spinola, S., Hoff, R. A., & Tsai, J. (2021). A psychosocial mediational model of homelessness among US male and female Veterans who served in Iraq and Afghanistan. Health & Social Care in the Community, 29(2), 453–463. doi: 10.1111/hsc.13106 [DOI] [PubMed] [Google Scholar]
- Steinberg, L., Sharp, C., Stanford, M. S., & Tharp, A. T. (2013). New tricks for an old measure: The development of the Barratt Impulsiveness Scale–Brief (BIS-Brief). Psychological Assessment, 25(1), 216. doi: 10.1037/a0030550 [DOI] [PubMed] [Google Scholar]
- Suris, A., & Lind, L. (2008). Military sexual trauma: A review of prevalence and associated health consequences in Veterans. Trauma, Violence & Abuse, 9(4), 250–269. doi: 10.1177/1524838008324419 [DOI] [PubMed] [Google Scholar]
- Thomas, M. L., Kaufmann, C. N., Palmer, B. W., Depp, C. A., Martin, A. S., Glorioso, D. K., … Jeste, D. V. (2016). Paradoxical trend for improvement in mental health with aging: A community-based study of 1,546 adults aged 21–100 years. The Journal of Clinical Psychiatry, 77(8), 1019–1025. doi: 10.4088/JCP.16m10671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai, J., Pietrzak, R. H., & Rosenheck, R. A. (2013). Homeless Veterans who served in Iraq and Afghanistan: Gender differences, combat exposure, and comparisons with previous cohorts of homeless Veterans. Administration and Policy in Mental Health and Mental Health Services Research, 40(5), 400–405. doi: 10.1007/s10488-012-0431-y [DOI] [PubMed] [Google Scholar]
- Tsai, J., Pietrzak, R. H., & Szymkowiak, D. (2021). The problem of veteran homelessness: An update for the new decade. Advance online publication American Journal of Preventive Medicine, 60(6), 774–780. doi: 10.1016/j.amepre.2020.12.012 [DOI] [PubMed] [Google Scholar]
- Tsai, J., & Rosenheck, R. A. (2015). Risk factors for homelessness among US Veterans. Epidemiologic Reviews, 37(1), 177–195. doi: 10.1093/epirev/mxu004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai, J., Schick, V., Hernandez, B., & Pietrzak, R. H. (2020). Is homelessness a traumatic event? Results from the 2019–2020 national health and resilience in Veterans study. Depression and Anxiety, 37(11), 1137–1145. doi: 10.1002/da.23098 [DOI] [PubMed] [Google Scholar]
- Tsai, J., Szymkowiak, D., & Pietrzak, R. H. (2020). Delayed homelessness after military discharge: Examination of a sleeper effect. American Journal of Preventive Medicine, 59(1), 109–117. doi: 10.1016/j.amepre.2020.03.001 [DOI] [PubMed] [Google Scholar]
- Tsai, J., Trevisan, L., Huang, M., & Pietrzak, R. H. (2018). Addressing veteran homelessness to prevent veteran suicides. Psychiatric Services, 69(8), 935–937. doi: 10.1176/appi.ps.201700482 [DOI] [PubMed] [Google Scholar]
- Weiner, M. R., Monin, J. K., Mota, N., & Pietrzak, R. H. (2016). Age differences in the association of social support and mental health in male US Veterans: Results from the national health and resilience in Veterans study. The American Journal of Geriatric Psychiatry, 24(4), 327–336. doi: 10.1016/j.jagp.2015.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from Robert Pietrzak, PhD, MPH at robert.pietrzak@yale.edu upon reasonable request https://www.vacsp.research.va.gov/CSPEC/Studies/INVESTD-R/Ntl-Health-Resilience-Veterans-Study.asp.