Abstract
Objectives
Post-acute sequalae of SARS-CoV-2 infection (PASC) is not well defined in pediatrics given its heterogeneity of presentation and severity in this population. The aim of this study is to use novel methods that rely on data mining approaches rather than clinical experience to detect conditions and symptoms associated with pediatric PASC.
Materials and Methods
We used a propensity-matched cohort design comparing children identified using the new PASC ICD10CM diagnosis code (U09.9) (N = 1309) to children with (N = 6545) and without (N = 6545) SARS-CoV-2 infection. We used a tree-based scan statistic to identify potential condition clusters co-occurring more frequently in cases than controls.
Results
We found significant enrichment among children with PASC in cardiac, respiratory, neurologic, psychological, endocrine, gastrointestinal, and musculoskeletal systems, the most significant related to circulatory and respiratory such as dyspnea, difficulty breathing, and fatigue and malaise.
Discussion
Our study addresses methodological limitations of prior studies that rely on prespecified clusters of potential PASC-associated diagnoses driven by clinician experience. Future studies are needed to identify patterns of diagnoses and their associations to derive clinical phenotypes.
Conclusion
We identified multiple conditions and body systems associated with pediatric PASC. Because we rely on a data-driven approach, several new or under-reported conditions and symptoms were detected that warrant further investigation.
Keywords: long COVID, post-acute sequelae of SARS-CoV-2 infection, COVID-19
BACKGROUND AND SIGNIFICANCE
The National Institutions of Health (NIH) launched the new RECOVER initiative in 20211 to leverage electronic health record (EHR) data to better identify and characterize patients with post-acute sequelae of SARS-CoV-2 infection (PASC), defined by the NIH as failure to recover from COVID-19, or those persistently symptomatic for >30 days.2 In the adult literature, advances have been made to predict PASC among COVID-19 affected patients3 and to describe etiology, risk factors, and outcomes.4–7 In contrast, there is currently a paucity of rigorous studies that accurately describe PASC in children.8 Research attempting to better elucidate PASC in children has been limited by small sample sizes,9–11 lack of a control group,12–14 or restrictions in source population15 that limit generalizability to a broader cohort.16
Access to EHR data in a large population of children offers an opportunity to better understand the spectrum of PASC across a wide range of demographics and clinical trajectories. A recent exploratory analysis using EHR data to characterize pediatric PASC examined symptoms, diagnoses, and medications occurring more frequently in a large cohort of SARS-CoV-2 viral test-positive patients when compared with SARS-CoV-2-negative controls. Similar studies have also been carried out in adult populations.7 However, these studies are limited in 2 important ways. First, SARS-CoV-2 positive patients are heterogeneous and therefore analyses are at risk for spurious associations attributable to residual confounding rather than significant clinical findings. Second and relatedly, studies of PASC-associated features employ outcomes defined by clusters of clinically similar diagnosis codes. Clustering clinical codes in this way may bias findings that confirm clinical experience. The rapidly evolving nature of the pandemic and the lack of consensus of specific symptoms that define PASC in children necessitate a more data-driven approach for knowledge discovery.17
In this study, we explored syndromic and systemic features associated with a clinical diagnosis of PASC compared to children with and without SARS-CoV-2 infection. The diagnosis code for PASC was established in October 2021—U09.9, post COVID-19 condition, unspecified. Prior to this, the nonspecific code, B94.8, Sequelae of other specified infectious and parasitic diseases, was proposed as a temporary alternative.18 While these codes reflect clinician judgment in diagnosing patients who may suffer from PASC, they are likely to have a higher positive predictive value than identifying cases using COVID-19 alone. To identify clusters of PASC-associated diagnoses from tens of thousands of diagnosis codes, we used a tree-based scan statistic, a data mining tool which detects signals from hierarchical structures without relying on prespecifying the clusters of codes of interest. This data-driven technique is especially advantageous in EHR research where mining a large corpus of data is feasible.
MATERIALS AND METHODS
Study population and design
The RECOVER PEDSnet EHR population includes EHR data from 9 children’s hospitals: Children’s Hospital of Philadelphia, Cincinnati Children’s Hospital Medical Center, Children’s Hospital of Colorado, Ann & Robert H. Lurie Children’s Hospital of Chicago, Nationwide Children’s Hospital, Nemours Children’s Health System (in Delaware and Florida), Seattle Children’s Hospital, and Stanford Children’s Health. The Children’s Hospital of Philadelphia’s institutional review board designated this study as not human subjects’ research and the need for consent was waived. The PEDSnet COVID-19 Database Version week 141 was used, which includes clinical histories through December 1, 2022 of patients who have been tested for SARS-CoV-2, diagnosed with COVID-19, or received a COVID-19 vaccine.1 This study is part of the NIH Researching COVID to Enhance Recovery (RECOVER) Initiative, which seeks to understand, treat, and prevent the post-acute sequelae of SARS-CoV-2 infection (PASC). For more information on RECOVER, visit https://recovercovid.org/.
Our primary analyses focused on 2 comparisons of interest. Cases consisted of patients with evidence of PASC; the 2 comparator cohorts were patients with and without SARS-CoV-2 infection. Evidence for PASC comprised a U09.9 diagnosis code or an interface terminology (IMO) term in the EHR with the following strings: (“post” and “acute” and “covid”) or (“complication” and “covid”). As evidence for PASC, we also admitted a B94.8 (Sequelae of other specified infectious and parasitic diseases) diagnosis code; because the B94.8 code is more general, we did not include such diagnoses where the IMO term indicated something other than PASC. We excluded patients who had a MIS-C diagnosis at any point in time based on the presence of the M35.81, U10, and U10.9 ICD10CM diagnostic codes; therefore, we use “PASC” to refer specifically to non-MIS-C variants. Patients were considered SARS-COV-2 infected if they had a diagnostic test that was positive for infection (polymerase chain reaction [PCR], antigen, or serology). Serology tests included IgM, IgG anti-N antibodies, IgG anti-S or receptor binding domain (RBD) antibodies, and IgG and IgA undifferentiated antibodies based on criteria from Mejias et al19 for positivity due to infection. Patients were also considered SARS-COV-2 infected if they had a diagnosis code for COVID-19 in the inpatient or emergency department (ED) setting. We excluded diagnosis codes for COVID-19 in the outpatient setting because of the possibility that the code was assigned as a rule-out diagnosis during a patient evaluation. Further, the observation period in the study aligned with the phase of the pandemic when viral testing was still widely performed in the healthcare setting. Patients were considered SARS-COV-2 uninfected if: (1) all available diagnostic tests (PCR, Ag, serology) during the study period were negative and (2) the patient did not have any diagnosis codes indicating SARS-COV-2 infection, MIS-C, or PASC in any setting.
Cohort entry date for incident PASC cases was defined as: (1) the date of the first positive PCR or antigen test, or (2) 4 weeks before the date of the first positive serology test, or (3) 4 weeks before the first occurrence of a diagnosis of PASC if no preceding confirmatory test was available. We recognize that imposing a date of infection may misclassify the risk window between initial infection and PASC diagnosis if no testing data is available but chose to be overly inclusive of patients rather than exclude patients with the diagnosis based on unavailability of testing data (only 533 of 1309 patients with PASC [40.7%] had evidence of SARS-CoV-2 infection prior to their earliest PASC diagnosis). The cohort entry date for non-PASC SARS-CoV-2 infected patients was defined based on the date of the earliest SARS-CoV-2 diagnostic test (unless serology positive, then 4 weeks earlier) or earliest COVID-19 diagnosis/encounter. For SARS-CoV-2 uninfected patients, cohort entry dates were chosen as the date of a random negative test. All patients across case and control definitions were <21 years of age at the date of cohort entry. Further, to ensure that patients had a history of care at their institution, we required that all patients had at least 2 encounters in the health system in the 18 months prior to cohort entry.
Additionally, we conducted a sensitivity analysis in which we compared SARS-CoV-2 positive to SARS-CoV-2 negative patients during the post-acute period—a description of the methods and results of this analysis are included in the Supplementary Appendix.
Matching
We extracted data for our study from the RECOVER pediatric database by identifying any patient who met study inclusion criteria between March 1, 2020, and December 1, 2022. We used a propensity score matched approach to balance covariates between cases and each of the comparison groups to minimize potential confounding.20 Propensity scores were estimated using logistic regression as the probability of a PASC diagnosis conditional on the following covariates: institution, age group (<1, 1–4, 5–11, 12–15, 16–20 years), sex, race/ethnicity (White non-Hispanic [NH], Black NH, Hispanic, Asian NH, multiracial NH, other NH), and clinical setting of testing. Additionally, we used the Pediatric Medical Complexity Algorithm (PMCA)21 to define for each body system an index indicating presence and complexity of chronic condition in that body system grouping and used these PMCA indices in our propensity score model. We then matched PASC patients to comparison patients (SARS-CoV-2 infected patients in the first cohort, SARS-COV-2 uninfected patients in the second cohort) using 5:1 nearest neighbor matching, additionally requiring exact matching on both cohort entry month and age group.22 We assessed the balance between the SARS-CoV-2 infected and uninfected patients via absolute standardized mean differences.
Tree-based scan statistic
The tree-based scan statistic is a data mining tool that is well established in vaccine safety23 and disease surveillance and characterization,23,24 making it salient for applications to understand pediatric PASC in its early stages of characterization. This approach simultaneously evaluates outcomes at different levels of granularity in a hierarchical structure, adjusting for multiple testing using a likelihood ratio statistic. In this study, we employed the unconditional analysis based on a Bernoulli probability model at each node of the tree, as described in the TreeScan User’s Guide.25 This approach identifies branches of the tree at which outcomes belonged most disproportionately to cases as compared to controls.
As inputs, we used the ICD10CM vocabulary following the ICD10CM Tabular List of Diseases and Injuries26 as developed by the National Center for Health Statistics (NCHS). For example, a path down the hierarchy might proceed as follows: C00-D49->C00-C97->C44->C44.1->C44.10->C44.102->C44.1021. In all, the hierarchy has 7 levels, with the following counts of nodes per level starting from the top down: 22, 262, 2274, 9502, 14 400, 22 236, 48 450.
We will alternately refer to the hierarchy as a tree, and the cluster consisting of a node together with all of its descendants will be referred to as a branch of the tree, or equivalently, as a cut. For each branch of the tree, we started with the observed count of cases who had an incident diagnosis in that branch during the outcome period. We also calculated the expected number of cases for each branch by multiplying the proportion of cases in the cohort (1/6 due to 5:1 matching) by the number of controls who had an incident diagnosis in the branch. The null hypothesis, for each cut, is that the number of observed cases equals the number of expected cases. This method adjusts for multiple testing in the sense that under the null hypothesis that the number of observed cases equals the number of expected cases at each cut, there is a 95% probability that there is no cut in the tree with a P value <.05. For each cut demonstrating significance at the P < .05 threshold, we calculated percent excess cases as the difference between number of observed cases and the number of expected cases divided by the number of expected cases. Analyses were carried out using R (4.1.0) and Treescan (2.0) software. Subclassification matching was implemented using the MatchIt R package and tree visualizations were built using the collapsibleTree R package.
Outcomes
For each patient and each diagnosis code, we calculated a binary indicator for whether the patient had an incident occurrence of that diagnosis code during the 28–179 days following cohort entry. We then used these to compute for each diagnosis code, and consequently each cluster of diagnosis codes defined by a branch of the tree, the number of cases and controls who had an incident diagnosis in that branch.
To define incident outcomes, we employed a washout period spanning from 18 months prior to cohort entry to 7 days prior to cohort entry for conditions grouped at the 3rd level of the ICD hierarchy (ie, the part of the ICD code before the decimal place) to ensure new incident diagnoses. In other words, conditions which occurred during the study period were not counted if a code in the same group occurred during the washout period.
RESULTS
Study population and matching
Between March 1, 2020, and June 22, 2022, there was a total of 14 399 patients identified for inclusion into the 3 cohorts, with PASC cases accounting for 1309 patients (Table 1). Older children and females were more likely to be included in the PASC cohort than younger children and males (overall: 54.9% vs 45.1%). The most common cohort entry months were in the fall of 2021. A majority of children in the PASC cohort (55.8%) had a chronic condition. Following 5:1 nearest neighbor matching, both comparison cohorts had excellent balance (|SMD|<0.1 for all variables) (Supplementary Appendix Figure 1a and b). After matching, the demographic distributions of both COVID-positive and COVID-negative cohorts reflect those of the PASC cohort.
Table 1.
Study population characteristics after matching
| Level | Overall | SARS CoV-2-negative | SARS CoV-2-positive | PASC | |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | ||
| n | 14 399 | 6545 | 6545 | 1309 | |
| Age at cohort entrance (%) | <1 | 363 (2.5) | 165 (2.5) | 165 (2.5) | 33 (2.5) |
| 1–4 | 1309 (9.1) | 595 (9.1) | 595 (9.1) | 119 (9.1) | |
| 5–11 | 4708 (32.7) | 2140 (32.7) | 2140 (32.7) | 428 (32.7) | |
| 12–15 | 4213 (29.3) | 1915 (29.3) | 1915 (29.3) | 383 (29.3) | |
| 16–20 | 3806 (26.4) | 1730 (26.4) | 1730 (26.4) | 346 (26.4) | |
| Sex (%) | Female | 7903 (54.9) | 3544 (54.1) | 3640 (55.6) | 719 (54.9) |
| Male | 6496 (45.1) | 3001 (45.9) | 2905 (44.4) | 590 (45.1) | |
| Race/ethnicity (%) | Non-Hispanic Asian/PI | 519 (3.6) | 245 (3.7) | 228 (3.5) | 46 (3.5) |
| Non-Hispanic Black/AA | 1425 (9.9) | 623 (9.5) | 674 (10.3) | 128 (9.8) | |
| Hispanic | 1698 (11.8) | 748 (11.4) | 793 (12.1) | 157 (12.0) | |
| Multiple | 593 (4.1) | 258 (3.9) | 282 (4.3) | 53 (4.0) | |
| Other/Unknown | 1275 (8.9) | 540 (8.3) | 607 (9.3) | 128 (9.8) | |
| Non-Hispanic White | 8889 (61.7) | 4131 (63.1) | 3961 (60.5) | 797 (60.9) | |
| Cohort entry month (%) | March 2020 | 77 (0.5) | 35 (0.5) | 35 (0.5) | 7 (0.5) |
| April 2020 | 132 (0.9) | 60 (0.9) | 60 (0.9) | 12 (0.9) | |
| May 2020 | 66 (0.5) | 30 (0.5) | 30 (0.5) | 6 (0.5) | |
| June 2020 | 110 (0.8) | 50 (0.8) | 50 (0.8) | 10 (0.8) | |
| July 2020 | 121 (0.8) | 55 (0.8) | 55 (0.8) | 11 (0.8) | |
| August 2020 | 110 (0.8) | 50 (0.8) | 50 (0.8) | 10 (0.8) | |
| September 2020 | 165 (1.1) | 75 (1.1) | 75 (1.1) | 15 (1.1) | |
| October 2020 | 198 (1.4) | 90 (1.4) | 90 (1.4) | 18 (1.4) | |
| November 2020 | 341 (2.4) | 155 (2.4) | 155 (2.4) | 31 (2.4) | |
| December 2020 | 341 (2.4) | 155 (2.4) | 155 (2.4) | 31 (2.4) | |
| January 2021 | 429 (3.0) | 195 (3.0) | 195 (3.0) | 39 (3.0) | |
| February 2021 | 242 (1.7) | 110 (1.7) | 110 (1.7) | 22 (1.7) | |
| March 2021 | 352 (2.4) | 160 (2.4) | 160 (2.4) | 32 (2.4) | |
| April 2021 | 385 (2.7) | 175 (2.7) | 175 (2.7) | 35 (2.7) | |
| May 2021 | 286 (2.0) | 130 (2.0) | 130 (2.0) | 26 (2.0) | |
| June 2021 | 385 (2.7) | 175 (2.7) | 175 (2.7) | 35 (2.7) | |
| July 2021 | 418 (2.9) | 190 (2.9) | 190 (2.9) | 38 (2.9) | |
| August 2021 | 671 (4.7) | 305 (4.7) | 305 (4.7) | 61 (4.7) | |
| September 2021 | 1111 (7.7) | 505 (7.7) | 505 (7.7) | 101 (7.7) | |
| October 2021 | 770 (5.3) | 350 (5.3) | 350 (5.3) | 70 (5.3) | |
| November 2021 | 957 (6.6) | 435 (6.6) | 435 (6.6) | 87 (6.6) | |
| December 2021 | 1584 (11.0) | 720 (11.0) | 720 (11.0) | 144 (11.0) | |
| January 2022 | 1837 (12.8) | 835 (12.8) | 835 (12.8) | 167 (12.8) | |
| February 2022 | 1023 (7.1) | 465 (7.1) | 465 (7.1) | 93 (7.1) | |
| March 2022 | 858 (6.0) | 390 (6.0) | 390 (6.0) | 78 (6.0) | |
| April 2022 | 693 (4.8) | 315 (4.8) | 315 (4.8) | 63 (4.8) | |
| May 2022 | 737 (5.1) | 335 (5.1) | 335 (5.1) | 67 (5.1) | |
| Institution (%) | A | 1116 (7.8) | 562 (8.6) | 453 (6.9) | 101 (7.7) |
| B | 1507 (10.5) | 664 (10.1) | 686 (10.5) | 157 (12.0) | |
| C | 2724 (18.9) | 1275 (19.5) | 1187 (18.1) | 262 (20.0) | |
| D | 469 (3.3) | 212 (3.2) | 218 (3.3) | 39 (3.0) | |
| E | 1058 (7.3) | 429 (6.6) | 541 (8.3) | 88 (6.7) | |
| F | 801 (5.6) | 333 (5.1) | 391 (6.0) | 77 (5.9) | |
| G | 1130 (7.8) | 525 (8.0) | 495 (7.6) | 110 (8.4) | |
| H | 2670 (18.5) | 1235 (18.9) | 1201 (18.3) | 234 (17.9) | |
| I | 2924 (20.3) | 1310 (20.0) | 1373 (21.0) | 241 (18.4) | |
| Test location (%) | ED | 2087 (14.5) | 863 (13.2) | 1055 (16.1) | 169 (12.9) |
| Inpatient | 1446 (10.0) | 627 (9.6) | 695 (10.6) | 124 (9.5) | |
| Other/unknown | 372 (2.6) | 139 (2.1) | 189 (2.9) | 44 (3.4) | |
| Outpatient office | 6702 (46.5) | 3130 (47.8) | 2940 (44.9) | 632 (48.3) | |
| Outpatient: test only | 3792 (26.3) | 1786 (27.3) | 1666 (25.5) | 340 (26.0) | |
| PMCA index (%) | Nonchronic | 6297 (43.7) | 2802 (42.8) | 2917 (44.6) | 578 (44.2) |
| Chronic noncomplex | 5605 (38.9) | 2572 (39.3) | 2535 (38.7) | 498 (38.0) | |
| Complex chronic | 2497 (17.3) | 1171 (17.9) | 1093 (16.7) | 233 (17.8) |
Tree-based scan statistic
When comparing patients with PASC to patients who were SARS-CoV-2 infected, we identified multiple statistical signals. At the highest level of the tree, significant cuts included R00–R99 Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified, M00–M99 Diseases of the musculoskeletal system and connective tissue, G00–G99 Diseases of the nervous system, J00–J99 Diseases of the respiratory system, F00–F99 Mental and behavioral disorders, E00–E90 Endocrine, nutritional, and metabolic diseases, I00–I99 Diseases of the circulatory system, Z00–Z99 Factors influencing health status and contact with health services, L00–L99 Diseases of the skin and subcutaneous tissue, and K00–K93 Diseases of the digestive system.
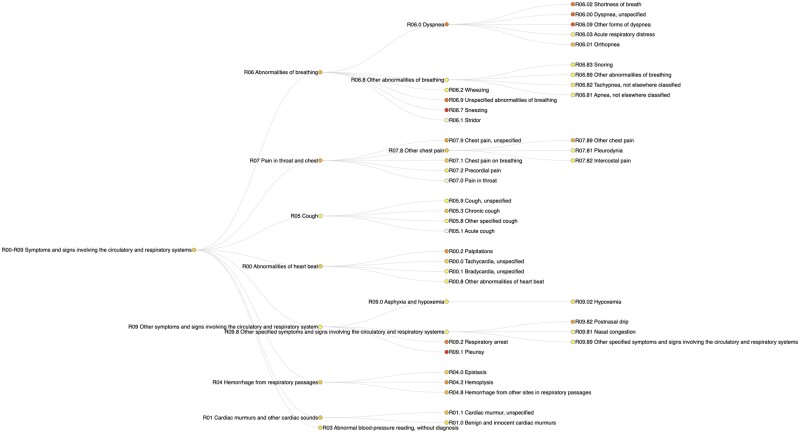
Within the R00–R99 branch, the top 3 cuts were R00–R09 Symptoms and signs involving the circulatory and respiratory systems, R50–R69 General symptoms and signs and R40–R46 Symptoms and signs involving cognition, perception, emotional state and behavior. Within the R00–R09 branch, the 3 most significant cuts included R06.0 Dyspnea, R07 Pain in throat and chest, R09.9 Chest pain, unspecified. This subbranch of the R00–R99 branch is visualized in Figure 1.
Figure 1.
Significant branches of the R00–R09 block of the ICD hierarchy with nodes colored by percent excess cases.
The PASC vs SARS-CoV-2 negative comparison showed significance for 304 cuts, and largely overlapped with the PASC vs SARS-CoV-2 negative comparison at the top of the tree, with the addition of H00–H59 Diseases of the eye and adnexa.
We refer the reader to Table 2 for a summary of systemic and syndromic findings collected from the 2 comparisons and Tables 3 and 4 for a full list of significant cuts, the likelihood ratio statistics, P values, and percent excess cases.
Table 2.
Summary of significant features in the 2 comparison cohorts
| Major systemic findings, or conditions (general and specific) | |
|---|---|
| Diseases of the nervous system | Migraines, headache syndromes, sleep disorders, insomnia, chronic pain, dysautonomia, post-viral fatigue syndrome, encephalitis, encephalopathya, disorders of autonomic nervous system, sleep apnea, transverse myelitisa |
| Mental and behavioral disorders | Anxiety disorders, severe stress and adjustment disorders, organic including symptomatic mental disorders, obsessive-compulsive disordera, dissociative and conversion disorders, mood disorders |
| Diseases of the respiratory system | Asthma, ARDS/respiratory failure, diseases of vocal cords and larynx, tonsilitis, exercise induced bronchospasma, pulmonary edemaa |
| Diseases of the circulatory system | Arrhythmias, cerebrovascular disease, thromboembolic disease, hypotension, tachycardiaa, cardiac murmursa |
| Disease of the musculoskeletal system and connective tissue | Pain in joints, pain in limbs, dorsalgia, myalgias, hypermobility syndrome, soft tissue disorders, muscle disorders, arthropathies, osteopathies, disorders of bone, reactive arthritis, physeal arrest, osteomyelitisa |
| Diseases of the digestive system | Diseases of oesophagus, stomach, and duodenum, aphagia and dysphagia, diseases of livera |
| Diseases of blood | Anemiasa, sickle cell disordersa |
| Endocrine, nutritional, and metabolic diseases | Nutritional deficienciesa, obesity and overweight, disorders of mineral metabolisma, volume depletion or fluid overload, obesity, hyperkalemiaa |
| Renal/Urinary | Acute kidney failurea, signs and symptoms involving the urinary system, hematuria |
| Diseases of the eye | Disorders of refraction and accommodationa |
| Immunologic findings | Other disorders involving the immune mechanism not elsewhere classified, cytomegaloviral diseasea |
| Major syndromic findings, or symptoms | |
| Circulatory and respiratory signs and symptoms | Palpitations, cough, dyspnea, shortness of breath, chest pain, viral and bacterial pneumonia, snoring, asphyxia and hypoxemia, hyperglycemiaa |
| GI signs/symptoms | Abdominal pain, nausea/vomiting, diarrheaa, constipationa, gastroenteritisa, pressure ulcera |
| CNS/musculoskeletal signs/symptoms | Lack of coordination, abnormalities of gait and mobility |
| Cognition, perception, emotional state | Dizziness, smell/taste disturbances, restlessness and agitationa, disorientationa, depressive episode |
| General signs and symptoms | Fatigue/malaise, muscle weakness, headache, weakness, syncope and collapse, pain not elsewhere classified, fevera, enlarged lymph nodesa, nasal congestiona, epistaxis, noninflammatory disorders of female genital tracta, other inflammation of vagina and vulvaa, visual disturbances |
| Skin | Symptoms and signs involving the skin and subcutaneous tissue, eczema,a urticariaa and erythemaa, paresthesia of skina |
Findings significant in PASC vs COVID-negative comparison but not PASC vs COVID-positive comparison.
Table 3.
PASC vs COVID positive comparison TreeScan results
| Cut | Node | Tree level | Log likelihood ratio | P value | N cases observed | N cases expected | Percent excess cases |
|---|---|---|---|---|---|---|---|
| A00–B99 Certain infections and parasitic diseases | |||||||
| 7 | B94 Sequelae of other and unspecified infectious and parasitic diseases | 3 | 281.31 | .001 | 157 | 26.17 | 499.92 |
| 8 | B90–B94 Sequelae of infectious and parasitic diseases | 2 | 281.31 | .001 | 157 | 26.17 | 499.92 |
| 9 | B94.8 Sequelae of other specified infectious and parasitic diseases | 4 | 275.93 | .001 | 154 | 25.67 | 499.92 |
| 17 | A00–B99 Certain infections and parasitic diseases | 1 | 120.32 | .001 | 1119 | 186.50 | 115.55 |
| 152 | A65–A69 Other spirochaetal diseases | 2 | 11.74 | .002 | 15 | 2.50 | 340.00 |
| 182 | B95–B98 Bacterial, viral, and other infectious agents | 2 | 9.95 | .024 | 301 | 50.17 | 61.45 |
| D50–D89 Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism | |||||||
| 44 | D89.89 Other specified disorders involving the immune mechanism, not elsewhere classified | 5 | 48.29 | .001 | 46 | 7.67 | 395.44 |
| 62 | D89 Other disorders involving the immune mechanism, not elsewhere classified | 3 | 27.93 | .001 | 116 | 19.33 | 179.36 |
| 65 | D50–D89 Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism | 1 | 26.84 | .001 | 941 | 156.83 | 56.86 |
| 69 | D89.8 Other specified disorders involving the immune mechanism, not elsewhere classified | 4 | 24.44 | .001 | 104 | 17.33 | 176.98 |
| 116 | D80–D89 Certain disorders involving the immune mechanism | 2 | 14.83 | .001 | 331 | 55.17 | 72.20 |
| E00–E90 Endocrine, nutritional, and metabolic diseases | |||||||
| 39 | E00–E90 Endocrine, nutritional, and metabolic diseases | 1 | 52.09 | .001 | 1571 | 261.83 | 61.56 |
| 59 | E70–E88 Metabolic disorders | 2 | 31.77 | .001 | 671 | 111.83 | 74.37 |
| 88 | E65–E68 Obesity and other hyperalimentation | 2 | 19.65 | .001 | 192 | 32.00 | 112.50 |
| 91 | E66 Overweight and obesity | 3 | 18.66 | .001 | 188 | 31.33 | 110.66 |
| 136 | E66.9 Obesity, unspecified | 4 | 12.92 | .001 | 78 | 13.00 | 146.15 |
| 147 | E87 Other disorders of fluid, electrolyte, and acid-base balance | 3 | 12.03 | .002 | 185 | 30.83 | 88.13 |
| 171 | E86.0 Dehydration | 4 | 10.57 | .019 | 101 | 16.83 | 113.90 |
| 174 | E86 Volume depletion | 3 | 10.31 | .020 | 106 | 17.67 | 109.39 |
| F00–F99 Mental and behavioral disorders | |||||||
| 21 | F00–F99 Mental and behavioral disorders | 1 | 97.90 | .001 | 2037 | 339.50 | 74.96 |
| 49 | F40–F48 Neurotic, stress-related, and somatoform disorders | 2 | 45.19 | .001 | 632 | 105.33 | 92.73 |
| 70 | F41 Other anxiety disorders | 3 | 24.34 | .001 | 277 | 46.17 | 103.60 |
| 74 | F80–F89 Disorders of psychological development | 2 | 22.51 | .001 | 506 | 84.33 | 71.94 |
| 89 | F41.9 Anxiety disorder, unspecified | 4 | 19.64 | .001 | 196 | 32.67 | 111.20 |
| 101 | F44 Dissociative and conversion disorders | 3 | 16.71 | .001 | 27 | 4.50 | 300.00 |
| 129 | F30–F39 Mood [affective] disorders | 2 | 13.88 | .001 | 279 | 46.50 | 76.34 |
| 143 | F00–F09 Organic, including symptomatic, mental disorders | 2 | 12.30 | .002 | 30 | 5.00 | 240.00 |
| 179 | F90–F98 Behavioral and emotional disorders with onset usually occurring in childhood and adolescence | 2 | 10.11 | .022 | 200 | 33.33 | 77.02 |
| 180 | F32 Depressive episode | 3 | 10.01 | .022 | 183 | 30.50 | 80.33 |
| 203 | F41.1 Generalized anxiety disorder | 4 | 9.03 | .042 | 36 | 6.00 | 183.33 |
| G00–G99 Diseases of the nervous system | |||||||
| 12 | G00–G99 Diseases of the nervous system | 1 | 199.49 | .001 | 2560 | 426.67 | 97.11 |
| 23 | G40–G47 Episodic and paroxysmal disorders | 2 | 89.80 | .001 | 1640 | 273.33 | 80.37 |
| 28 | G89–G99 Other disorders of the nervous system | 2 | 83.68 | .001 | 570 | 95.00 | 136.84 |
| 37 | G89 Pain, not elsewhere classified | 3 | 57.51 | .001 | 296 | 49.33 | 159.48 |
| 41 | G43 Migraine | 3 | 50.63 | .001 | 337 | 56.17 | 138.56 |
| 43 | G89.2 Chronic pain, not elsewhere classified | 4 | 48.80 | .001 | 225 | 37.50 | 169.33 |
| 45 | G89.29 Other chronic pain | 5 | 48.22 | .001 | 223 | 37.17 | 169.03 |
| 55 | G47 Sleep disorders | 3 | 36.02 | .001 | 581 | 96.83 | 85.89 |
| 57 | G90 Disorders of autonomic nervous system | 3 | 32.80 | .001 | 38 | 6.33 | 358.14 |
| 58 | G44 Other headache syndromes | 3 | 32.26 | .001 | 107 | 17.83 | 202.86 |
| 63 | G43.0 Migraine without aura | 4 | 27.64 | .001 | 137 | 22.83 | 162.81 |
| 68 | G90.9 Disorder of the autonomic nervous system, unspecified | 4 | 25.05 | .001 | 17 | 2.83 | 465.37 |
| 71 | G00–G09 Inflammatory diseases of the central nervous system | 2 | 23.34 | .001 | 62 | 10.33 | 229.14 |
| 73 | G44.5 Complicated headache syndromes | 4 | 22.88 | .001 | 26 | 4.33 | 361.89 |
| 90 | G04 Encephalitis, myelitis, and encephalomyelitis | 3 | 19.22 | .001 | 37 | 6.17 | 272.77 |
| 98 | G43.01 Migraine without aura, intractable | 5 | 16.91 | .001 | 49 | 8.17 | 218.24 |
| 99 | G44.52 New daily persistent headache (NDPH) | 5 | 16.87 | .001 | 22 | 3.67 | 335.97 |
| 115 | G04.8 Other encephalitis, myelitis, and encephalomyelitis | 4 | 14.85 | .001 | 24 | 4.00 | 300.00 |
| 119 | G90.1 Familial dysautonomia [Riley-Day] | 4 | 14.75 | .001 | 11 | 1.83 | 446.45 |
| 125 | G93 Other disorders of brain | 3 | 14.10 | .001 | 175 | 29.17 | 98.83 |
| 127 | G43.019 Migraine without aura, intractable, without status migrainosus | 6 | 13.99 | .001 | 39 | 6.50 | 223.08 |
| 132 | G47.3 Sleep apnea | 4 | 13.60 | .001 | 321 | 53.50 | 70.09 |
| 141 | G43.009 Migraine without aura, not intractable, without status migrainosus | 6 | 12.71 | .001 | 75 | 12.50 | 148.00 |
| 146 | G43.00 Migraine without aura, not intractable | 5 | 12.06 | .002 | 88 | 14.67 | 131.77 |
| 160 | G93.3 Postviral fatigue syndrome | 4 | 11.27 | .007 | 11 | 1.83 | 391.80 |
| 167 | G44.8 Other specified headache syndromes | 4 | 10.80 | .007 | 21 | 3.50 | 271.43 |
| 183 | G43.80 Other migraine, not intractable | 5 | 9.92 | .026 | 12 | 2.00 | 350.00 |
| 188 | G44.89 Other headache syndrome | 5 | 9.77 | .026 | 17 | 2.83 | 288.69 |
| I00–I99 Diseases of the circulatory system | |||||||
| 47 | I00–I99 Diseases of the circulatory system | 1 | 46.29 | .001 | 893 | 148.83 | 78.06 |
| 87 | I49 Other cardiac arrhythmias | 3 | 19.75 | .001 | 39 | 6.50 | 269.23 |
| 97 | I30–I52 Other forms of heart disease | 2 | 17.11 | .001 | 261 | 43.50 | 88.51 |
| 128 | I95.1 Orthostatic hypotension | 4 | 13.96 | .001 | 20 | 3.33 | 320.42 |
| 135 | I49.8 Other specified cardiac arrhythmias | 4 | 13.17 | .001 | 26 | 4.33 | 269.52 |
| 178 | I95–I99 Other and unspecified disorders of the circulatory system | 2 | 10.17 | .022 | 68 | 11.33 | 138.31 |
| 198 | I51 Complications and ill-defined descriptions of heart disease | 3 | 9.16 | .041 | 39 | 6.50 | 176.92 |
| J00–J99 Diseases of the respiratory system | |||||||
| 25 | J00–J99 Diseases of the respiratory system | 1 | 86.96 | .001 | 3044 | 507.33 | 56.90 |
| 53 | J40–J47 Chronic lower respiratory diseases | 2 | 41.76 | .001 | 885 | 147.50 | 74.24 |
| 54 | J45 Asthma | 3 | 41.35 | .001 | 852 | 142.00 | 75.35 |
| 75 | J45.9 Other and unspecified asthma | 4 | 22.14 | .001 | 254 | 42.33 | 103.17 |
| 86 | J30–J39 Other diseases of upper respiratory tract | 2 | 19.77 | .001 | 603 | 100.50 | 61.19 |
| 92 | J12.8 Other viral pneumonia | 4 | 18.35 | .001 | 23 | 3.83 | 343.86 |
| 94 | J96–J99 Other diseases of the respiratory system | 2 | 18.06 | .001 | 391 | 65.17 | 73.39 |
| 95 | J45.909 Unspecified asthma, uncomplicated | 6 | 17.67 | .001 | 180 | 30.00 | 110.00 |
| 111 | J12 Viral pneumonia, not elsewhere classified | 3 | 15.81 | .001 | 39 | 6.50 | 238.46 |
| 113 | J45.90 Unspecified asthma | 5 | 15.08 | .001 | 212 | 35.33 | 92.47 |
| 122 | J12.82 Pneumonia due to coronavirus disease 2019 | 5 | 14.49 | .001 | 13 | 2.17 | 406.91 |
| 139 | J38 Diseases of vocal cords and larynx, not elsewhere classified | 3 | 12.80 | .001 | 54 | 9.00 | 177.78 |
| 144 | J03 Acute tonsillitis | 3 | 12.30 | .002 | 30 | 5.00 | 240.00 |
| 150 | J98 Other respiratory disorders | 3 | 11.90 | .002 | 152 | 25.33 | 97.39 |
| 153 | J96.0 Acute respiratory failure | 4 | 11.61 | .003 | 82 | 13.67 | 134.09 |
| 156 | J03.91 Acute recurrent tonsillitis, unspecified | 5 | 11.38 | .006 | 9 | 1.50 | 433.33 |
| 175 | J45.4 Moderate persistent asthma | 4 | 10.22 | .021 | 156 | 26.00 | 88.46 |
| 184 | J09–J18 Influenza and pneumonia | 2 | 9.92 | .026 | 210 | 35.00 | 74.29 |
| 194 | J15 Bacterial pneumonia, not elsewhere classified | 3 | 9.33 | .038 | 26 | 4.33 | 223.33 |
| 199 | J45.40 Moderate persistent asthma, uncomplicated | 5 | 9.10 | .042 | 132 | 22.00 | 90.91 |
| K00–K93 Diseases of the digestive system | |||||||
| 165 | K20–K31 Diseases of oesophagus, stomach, and duodenum | 2 | 10.94 | .007 | 387 | 64.50 | 56.59 |
| 181 | K00–K93 Diseases of the digestive system | 1 | 10.00 | .022 | 2054 | 342.33 | 22.69 |
| L00–L99 Diseases of the skin and subcutaneous tissue | |||||||
| 96 | L00–L99 Diseases of the skin and subcutaneous tissue | 1 | 17.45 | .001 | 966 | 161.00 | 44.72 |
| M00–M99 Diseases of the musculoskeletal system and connective tissue | |||||||
| 15 | M00–M99 Diseases of the musculoskeletal system and connective tissue | 1 | 183.48 | .001 | 3258 | 543.00 | 81.58 |
| 22 | M20–M25 Other joint disorders | 2 | 93.84 | .001 | 1038 | 173.00 | 105.20 |
| 31 | M25 Other joint disorder, not elsewhere classified | 3 | 67.30 | .001 | 658 | 109.67 | 112.46 |
| 36 | M25.5 Pain in joint | 4 | 59.36 | .001 | 462 | 77.00 | 127.27 |
| 46 | M79 Other and unspecified soft tissue disorders, not elsewhere classified | 3 | 47.13 | .001 | 476 | 79.33 | 110.51 |
| 50 | M79.1 Myalgia | 4 | 43.85 | .001 | 111 | 18.50 | 235.14 |
| 52 | M70–M79 Other soft tissue disorders | 2 | 42.76 | .001 | 527 | 87.83 | 99.25 |
| 72 | M25.50 Pain in unspecified joint | 5 | 23.03 | .001 | 51 | 8.50 | 252.94 |
| 77 | M79.18 Myalgia, other site | 5 | 21.61 | .001 | 56 | 9.33 | 232.26 |
| 78 | M60–M63 Disorders of muscles | 2 | 21.37 | .001 | 402 | 67.00 | 79.10 |
| 82 | M79.10 Myalgia, unspecified site | 5 | 20.46 | .001 | 52 | 8.67 | 234.49 |
| 83 | M62 Other disorders of muscle | 3 | 20.15 | .001 | 396 | 66.00 | 77.27 |
| 84 | M25.56 Pain in knee | 5 | 20.03 | .001 | 171 | 28.50 | 121.05 |
| 93 | M02.3 Reiter’s disease | 4 | 18.16 | .001 | 13 | 2.17 | 453.00 |
| 102 | M50–M54 Other dorsopathies | 2 | 16.59 | .001 | 268 | 44.67 | 85.81 |
| 103 | M35 Other systemic involvement of connective tissue | 3 | 16.47 | .001 | 38 | 6.33 | 247.55 |
| 104 | M02.30 Reiter’s disease, unspecified site | 5 | 16.45 | .001 | 12 | 2.00 | 450.00 |
| 105 | M30–M36 Systemic connective tissue disorders | 2 | 16.32 | .001 | 97 | 16.17 | 147.37 |
| 107 | M02 Postinfective and reactive arthropathies | 3 | 16.12 | .001 | 14 | 2.33 | 415.02 |
| 110 | M54 Dorsalgia | 3 | 15.84 | .001 | 242 | 40.33 | 88.45 |
| 112 | M62.8 Other specified disorders of muscle | 4 | 15.76 | .001 | 343 | 57.17 | 73.17 |
| 114 | M00–M02 Infectious arthropathies | 2 | 15.05 | .001 | 19 | 3.17 | 341.64 |
| 121 | M21 Other acquired deformities of limbs | 3 | 14.56 | .001 | 177 | 29.50 | 100.00 |
| 126 | M79.6 Pain in limb, hand, foot, fingers, and toes | 4 | 14.06 | .001 | 318 | 53.00 | 71.70 |
| 130 | M24 Other specific joint derangements | 3 | 13.77 | .001 | 156 | 26.00 | 103.85 |
| 133 | M24.9 Joint derangement, unspecified | 4 | 13.23 | .001 | 16 | 2.67 | 349.44 |
| 137 | M25.55 Pain in hip | 5 | 12.87 | .001 | 71 | 11.83 | 153.59 |
| 140 | M86–M90 Other osteopathies | 2 | 12.78 | .001 | 144 | 24.00 | 104.17 |
| 151 | M35.7 Hypermobility syndrome | 4 | 11.87 | .002 | 25 | 4.17 | 259.71 |
| 154 | M79.60 Pain in limb, unspecified | 5 | 11.55 | .003 | 129 | 21.50 | 104.65 |
| 161 | M25.551 Pain in right hip | 6 | 11.09 | .007 | 29 | 4.83 | 231.26 |
| 172 | M25.561 Pain in right knee | 6 | 10.42 | .020 | 86 | 14.33 | 123.31 |
| 186 | M62.81 Muscle weakness (generalized) | 5 | 9.77 | .026 | 180 | 30.00 | 80.00 |
| 189 | M89.1 Physeal arrest | 4 | 9.69 | .034 | 10 | 1.67 | 379.04 |
| 192 | M79.66 Pain in lower leg | 5 | 9.40 | .037 | 32 | 5.33 | 200.19 |
| 193 | M21.8 Other specified acquired deformities of limbs | 4 | 9.37 | .037 | 23 | 3.83 | 239.43 |
| 196 | M89 Other disorders of bone | 3 | 9.27 | .040 | 49 | 8.17 | 157.04 |
| Q00–Q99 Congenital malformations, deformations, and chromosomal abnormalities | |||||||
| 191 | Q79 Congenital malformations of musculoskeletal system, not elsewhere classified | 3 | 9.52 | .036 | 59 | 9.83 | 144.15 |
| 197 | Q00–Q99 Congenital malformations, deformations, and chromosomal abnormalities | 1 | 9.23 | .041 | 746 | 124.33 | 36.73 |
| R00–R99 Symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified | |||||||
| 1 | R00–R99 Symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified | 1 | 816.06 | .001 | 8383 | 1397.17 | 109.49 |
| 6 | R00–R09 Symptoms and signs involving the circulatory and respiratory systems | 2 | 365.38 | .001 | 2038 | 339.67 | 152.60 |
| 10 | R06.0 Dyspnea | 4 | 242.71 | .001 | 381 | 63.50 | 304.72 |
| 11 | R06 Abnormalities of breathing | 3 | 207.49 | .001 | 706 | 117.67 | 199.99 |
| 13 | R50–R69 General symptoms and signs | 2 | 195.76 | .001 | 2236 | 372.67 | 103.40 |
| 14 | R53 Malaise and fatigue | 3 | 185.81 | .001 | 403 | 67.17 | 255.81 |
| 16 | R53.8 Other malaise and fatigue | 4 | 179.60 | .001 | 338 | 56.33 | 276.35 |
| 18 | R40–R46 Symptoms and signs involving cognition, perception, emotional state, and behavior | 2 | 106.54 | .001 | 724 | 120.67 | 137.01 |
| 19 | R53.83 Other fatigue | 5 | 105.25 | .001 | 230 | 38.33 | 254.81 |
| 20 | R06.02 Shortness of breath | 5 | 99.42 | .001 | 148 | 24.67 | 313.46 |
| 24 | R10–R19 Symptoms and signs involving the digestive system and abdomen | 2 | 88.31 | .001 | 1710 | 285.00 | 77.89 |
| 26 | R07 Pain in throat and chest | 3 | 86.65 | .001 | 281 | 46.83 | 205.36 |
| 27 | R06.00 Dyspnea, unspecified | 5 | 86.01 | .001 | 104 | 17.33 | 350.09 |
| 29 | R06.09 Other forms of dyspnea | 5 | 79.13 | .001 | 81 | 13.50 | 381.48 |
| 30 | R42 Dizziness and giddiness | 3 | 67.75 | .001 | 175 | 29.17 | 232.53 |
| 32 | R07.9 Chest pain, unspecified | 4 | 62.74 | .001 | 151 | 25.17 | 241.68 |
| 35 | R25–R29 Symptoms and signs involving the nervous and musculoskeletal systems | 2 | 60.00 | .001 | 300 | 50.00 | 162.00 |
| 38 | R51 Headache | 3 | 53.53 | .001 | 234 | 39.00 | 174.36 |
| 40 | R53.82 Chronic fatigue, unspecified | 5 | 51.50 | .001 | 48 | 8.00 | 400.00 |
| 42 | R51.9 Headache, unspecified | 4 | 48.87 | .001 | 208 | 34.67 | 176.90 |
| 48 | R00 Abnormalities of heart beat | 3 | 45.42 | .001 | 206 | 34.33 | 170.90 |
| 51 | R10 Abdominal and pelvic pain | 3 | 42.83 | .001 | 648 | 108.00 | 88.89 |
| 56 | R00.2 Palpitations | 4 | 34.35 | .001 | 74 | 12.33 | 256.85 |
| 60 | R29 Other symptoms and signs involving the nervous and musculoskeletal systems | 3 | 28.87 | .001 | 187 | 31.17 | 140.62 |
| 61 | R53.81 Other malaise | 5 | 28.50 | .001 | 60 | 10.00 | 260.00 |
| 64 | R07.89 Other chest pain | 5 | 27.49 | .001 | 88 | 14.67 | 206.75 |
| 66 | R07.8 Other chest pain | 4 | 25.91 | .001 | 104 | 17.33 | 182.75 |
| 67 | R05 Cough | 3 | 25.83 | .001 | 412 | 68.67 | 86.40 |
| 76 | R43 Disturbances of smell and taste | 3 | 21.89 | .001 | 39 | 6.50 | 284.62 |
| 79 | R55 Syncope and collapse | 3 | 21.24 | .001 | 88 | 14.67 | 179.48 |
| 80 | R11 Nausea and vomiting | 3 | 20.83 | .001 | 454 | 75.67 | 73.12 |
| 81 | R41 Other symptoms and signs involving cognitive functions and awareness | 3 | 20.57 | .001 | 128 | 21.33 | 143.79 |
| 100 | R00.0 Tachycardia, unspecified | 4 | 16.84 | .001 | 92 | 15.33 | 154.40 |
| 106 | R09 Other symptoms and signs involving the circulatory and respiratory system | 3 | 16.24 | .001 | 340 | 56.67 | 74.70 |
| 108 | R29.9 Unspecified symptoms and signs involving the nervous and musculoskeletal systems | 4 | 16.12 | .001 | 16 | 2.67 | 386.89 |
| 109 | R10.1 Pain localized to upper abdomen | 4 | 15.91 | .001 | 128 | 21.33 | 125.04 |
| 117 | R10.84 Generalized abdominal pain | 5 | 14.81 | .001 | 180 | 30.00 | 100.00 |
| 118 | R90–R96 Abnormal findings on diagnostic imaging and in function studies, without diagnosis | 2 | 14.79 | .001 | 278 | 46.33 | 79.15 |
| 120 | R10.8 Other abdominal pain | 4 | 14.65 | .001 | 189 | 31.50 | 96.83 |
| 123 | R29.90 Unspecified symptoms and signs involving the nervous system | 5 | 14.49 | .001 | 13 | 2.17 | 406.91 |
| 131 | R70–R79 Abnormal findings on examination of blood, without diagnosis | 2 | 13.68 | .001 | 298 | 49.67 | 73.14 |
| 134 | R26 | 3 | 13.17 | .001 | 26 | 4.33 | 269.52 |
| 138 | R27 Other lack of coordination | 3 | 12.83 | .001 | 38 | 6.33 | 215.96 |
| 142 | R06.8 Other abnormalities of breathing | 4 | 12.46 | .002 | 261 | 43.50 | 74.71 |
| 145 | R68 Other general symptoms and signs | 3 | 12.27 | .002 | 130 | 21.67 | 107.66 |
| 148 | R30–R39 Symptoms and signs involving the urinary system | 2 | 11.96 | .002 | 314 | 52.33 | 66.25 |
| 149 | R04 Hemorrhage from respiratory passages | 3 | 11.95 | .002 | 56 | 9.33 | 167.95 |
| 155 | R53.1 Weakness | 4 | 11.55 | .003 | 64 | 10.67 | 153.05 |
| 158 | R09.0 Asphyxia and hypoxemia | 4 | 11.31 | .006 | 106 | 17.67 | 115.05 |
| 159 | R09.02 Hypoxemia | 5 | 11.31 | .006 | 106 | 17.67 | 115.05 |
| 162 | R05.9 Cough, unspecified | 4 | 11.06 | .007 | 212 | 35.33 | 78.32 |
| 163 | R31 Hematuria | 3 | 11.05 | .007 | 48 | 8.00 | 175.00 |
| 164 | R19 Other symptoms and signs involving the digestive system and abdomen | 3 | 10.97 | .007 | 195 | 32.50 | 81.54 |
| 166 | R29.898 Other symptoms and signs involving the musculoskeletal system | 6 | 10.86 | .007 | 96 | 16.00 | 118.75 |
| 168 | R10.13 Epigastric pain | 5 | 10.76 | .007 | 81 | 13.50 | 129.63 |
| 169 | R11.0 Nausea | 4 | 10.59 | .019 | 97 | 16.17 | 116.45 |
| 170 | R29.89 Other symptoms and signs involving the musculoskeletal system | 5 | 10.59 | .019 | 97 | 16.17 | 116.45 |
| 173 | R29.8 Other symptoms and signs involving the nervous and musculoskeletal systems | 4 | 10.37 | .020 | 126 | 21.00 | 100.00 |
| 176 | R13 Aphagia and dysphagia | 3 | 10.22 | .021 | 299 | 49.83 | 62.55 |
| 177 | R13.1 Dysphagia | 4 | 10.22 | .021 | 299 | 49.83 | 62.55 |
| 185 | R68.89 Other general symptoms and signs | 5 | 9.82 | .026 | 96 | 16.00 | 112.50 |
| 187 | R26.2 Difficulty in walking, not elsewhere classified | 4 | 9.77 | .026 | 17 | 2.83 | 288.69 |
| 190 | R06.83 Snoring | 5 | 9.61 | .035 | 113 | 18.83 | 101.81 |
| 195 | R04.0 Epistaxis | 4 | 9.27 | .040 | 49 | 8.17 | 157.04 |
| 200 | R46 Symptoms and signs involving appearance and behavior | 3 | 9.10 | .042 | 132 | 22.00 | 90.91 |
| 201 | R41.8 Other symptoms and signs involving cognitive functions and awareness | 4 | 9.08 | .042 | 95 | 15.83 | 108.46 |
| 202 | R05.3 Chronic cough | 4 | 9.03 | .042 | 36 | 6.00 | 183.33 |
| S00–T98 Injury, poisoning, and certain other consequences of external causes | |||||||
| 157 | S72.3 Fracture of shaft of femur | 4 | 11.38 | .006 | 9 | 1.50 | 433.33 |
| U00–U95 Codes for special purposes | |||||||
| 2 | U09 Post COVID-19 condition | 3 | 614.57 | .001 | 343 | 57.17 | 499.97 |
| 3 | U09.9 Post COVID-19 condition, unspecified | 4 | 614.57 | .001 | 343 | 57.17 | 499.97 |
| 4 | U00–U95 Codes for special purposes | 1 | 509.50 | .001 | 657 | 109.50 | 338.36 |
| 5 | U00–U49 Provisional assignment of new diseases of uncertain etiology or emergency use | 2 | 509.50 | .001 | 657 | 109.50 | 338.36 |
| 33 | U07.1 Emergency use of U07.1 | COVID-19 | 4 | 62.65 | .001 | 314 | 52.33 | 161.80 |
| 34 | U07 | 3 | 62.65 | .001 | 314 | 52.33 | 161.80 |
| Z00–Z99 Factors influencing health status and contact with health services | |||||||
| 85 | Z69–Z76 Persons encountering health services in other circumstances | 2 | 19.96 | .001 | 268 | 44.67 | 94.76 |
| 124 | Z00–Z99 Factors influencing health status and contact with health services | 1 | 14.19 | .001 | 2063 | 343.83 | 27.10 |
Table 4.
PASC vs COVID negative comparison TreeScan results
| Cut | Node | Tree level | Log likelihood ratio | P value | N cases observed | N cases expected | Percent excess cases |
|---|---|---|---|---|---|---|---|
| A00–B99 Certain infections and parasitic diseases | |||||||
| 10 | B90–B94 Sequelae of infectious and parasitic diseases | 2 | 281.31 | .001 | 157 | 26.17 | 499.92 |
| 11 | B94 Sequelae of other and unspecified infectious and parasitic diseases | 3 | 281.31 | .001 | 157 | 26.17 | 499.92 |
| 12 | B94.8 Sequelae of other specified infectious and parasitic diseases | 4 | 275.93 | .001 | 154 | 25.67 | 499.92 |
| 15 | A00–B99 Certain infections and parasitic diseases | 1 | 239.90 | .001 | 797 | 132.83 | 202.64 |
| 76 | B95–B98 Bacterial, viral, and other infectious agents | 2 | 35.38 | .001 | 190 | 31.67 | 155.76 |
| 96 | B25–B34 Other viral diseases | 2 | 27.51 | .001 | 162 | 27.00 | 148.15 |
| 116 | B97 Viral agents as the cause of diseases classified elsewhere | 3 | 23.01 | .001 | 81 | 13.50 | 196.30 |
| 128 | B34 Viral infection of unspecified site | 3 | 20.49 | .001 | 121 | 20.17 | 147.89 |
| 214 | B97.2 Coronavirus as the cause of diseases classified elsewhere | 4 | 12.54 | .002 | 7 | 1.17 | 498.29 |
| 215 | B97.29 Other coronavirus as the cause of diseases classified elsewhere | 5 | 12.54 | .002 | 7 | 1.17 | 498.29 |
| 217 | A30–A49 Other bacterial diseases | 2 | 12.54 | .002 | 48 | 8.00 | 187.50 |
| 240 | B97.89 Other viral agents as the cause of diseases classified elsewhere | 5 | 11.38 | .003 | 54 | 9.00 | 166.67 |
| 246 | B34.8 Other viral infections of unspecified site | 4 | 11.14 | .006 | 18 | 3.00 | 300.00 |
| 252 | B97.8 Other viral agents as the cause of diseases classified elsewhere | 4 | 10.98 | .006 | 55 | 9.17 | 161.72 |
| 286 | B25 Cytomegaloviral disease | 3 | 9.69 | .020 | 10 | 1.67 | 379.04 |
| D50–D89 Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism | |||||||
| 33 | D50–D89 Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism | 1 | 91.55 | .001 | 623 | 103.83 | 136.93 |
| 50 | D89.89 Other specified disorders involving the immune mechanism, not elsewhere classified | 5 | 55.61 | .001 | 42 | 7.00 | 442.86 |
| 55 | D89 Other disorders involving the immune mechanism, not elsewhere classified | 3 | 48.34 | .001 | 83 | 13.83 | 290.46 |
| 63 | D89.8 Other specified disorders involving the immune mechanism, not elsewhere classified | 4 | 43.65 | .001 | 73 | 12.17 | 294.41 |
| 65 | D80–D89 Certain disorders involving the immune mechanism | 2 | 42.19 | .001 | 221 | 36.83 | 157.94 |
| 158 | D64.9 Anemia, unspecified | 4 | 16.91 | .001 | 49 | 8.17 | 218.24 |
| 161 | D60–D64 Aplastic and other anemias | 2 | 16.73 | .001 | 129 | 21.50 | 127.91 |
| 185 | D64 Other anemias | 3 | 14.59 | .001 | 70 | 11.67 | 165.64 |
| 200 | D55–D59 Hemolytic anemias | 2 | 13.41 | .001 | 37 | 6.17 | 224.15 |
| 210 | D65–D69 Coagulation defects, purpura, and other hemorrhagic conditions | 2 | 12.71 | .001 | 75 | 12.50 | 148.00 |
| 211 | D57 Sickle-cell disorders | 3 | 12.64 | .001 | 24 | 4.00 | 275.00 |
| E00–E90 Endocrine, nutritional, and metabolic diseases | |||||||
| 30 | E00–E90 Endocrine, nutritional, and metabolic diseases | 1 | 98.96 | .001 | 1294 | 215.67 | 96.13 |
| 42 | E70–E88 Metabolic disorders | 2 | 73.49 | .001 | 491 | 81.83 | 138.30 |
| 71 | E87 Other disorders of fluid, electrolyte, and acid-base balance | 3 | 40.29 | .001 | 105 | 17.50 | 231.43 |
| 119 | E86 Volume depletion | 3 | 22.80 | .001 | 72 | 12.00 | 208.33 |
| 123 | E86.0 Dehydration | 4 | 22.21 | .001 | 70 | 11.67 | 208.48 |
| 129 | E65–E68 Obesity and other hyperalimentation | 2 | 20.43 | .001 | 189 | 31.50 | 115.87 |
| 133 | E66 Overweight and obesity | 3 | 19.94 | .001 | 183 | 30.50 | 116.39 |
| 203 | E87.7 Fluid overload | 4 | 13.17 | .001 | 26 | 4.33 | 269.52 |
| 208 | E66.9 Obesity, unspecified | 4 | 12.92 | .001 | 78 | 13.00 | 146.15 |
| 212 | E87.70 Fluid overload, unspecified | 5 | 12.64 | .001 | 24 | 4.00 | 275.00 |
| 239 | E87.5 Hyperkalemia | 4 | 11.38 | .003 | 9 | 1.50 | 433.33 |
| 261 | E83 Disorders of mineral metabolism | 3 | 10.61 | .012 | 129 | 21.50 | 100.00 |
| 270 | E50–E64 Other nutritional deficiencies | 2 | 10.33 | .013 | 147 | 24.50 | 91.84 |
| F00–F99 Mental and behavioral disorders | |||||||
| 27 | F00–F99 Mental and behavioral disorders | 1 | 108.72 | .001 | 1973 | 328.83 | 80.64 |
| 51 | F40–F48 Neurotic, stress-related, and somatoform disorders | 2 | 54.50 | .001 | 590 | 98.33 | 106.45 |
| 81 | F41 Other anxiety disorders | 3 | 30.21 | .001 | 254 | 42.33 | 122.06 |
| 94 | F80–F89 Disorders of psychological development | 2 | 27.72 | .001 | 475 | 79.17 | 83.15 |
| 111 | F41.9 Anxiety disorder, unspecified | 4 | 24.05 | .001 | 180 | 30.00 | 130.00 |
| 171 | F44 Dissociative and conversion disorders | 3 | 15.83 | .001 | 28 | 4.67 | 285.44 |
| 189 | F00–F09 Organic, including symptomatic, mental disorders | 2 | 14.49 | .001 | 27 | 4.50 | 277.78 |
| 242 | F80 Specific developmental disorders of speech and language | 3 | 11.29 | .003 | 114 | 19.00 | 110.53 |
| 253 | F69 Unspecified disorder of adult personality and behavior | 3 | 10.75 | .011 | 6 | 1.00 | 500.00 |
| 267 | F90–F98 Behavioral and emotional disorders with onset usually occurring in childhood and adolescence | 2 | 10.45 | .013 | 198 | 33.00 | 78.79 |
| 275 | F32 Depressive episode | 3 | 10.19 | .013 | 182 | 30.33 | 81.34 |
| 294 | F43 Reaction to severe stress, and adjustment disorders | 3 | 9.45 | .022 | 222 | 37.00 | 70.27 |
| G00–G99 Diseases of the nervous system | |||||||
| 13 | G00–G99 Diseases of the nervous system | 1 | 259.71 | .001 | 2311 | 385.17 | 118.35 |
| 25 | G40–G47 Episodic and paroxysmal disorders | 2 | 122.60 | .001 | 1475 | 245.83 | 100.55 |
| 29 | G89–G99 Other disorders of the nervous system | 2 | 101.22 | .001 | 520 | 86.67 | 159.61 |
| 48 | G43 Migraine | 3 | 57.17 | .001 | 318 | 53.00 | 152.83 |
| 52 | G47 Sleep disorders | 3 | 53.89 | .001 | 501 | 83.50 | 115.57 |
| 53 | G89 Pain, not elsewhere classified | 3 | 52.73 | .001 | 309 | 51.50 | 148.54 |
| 57 | G89.2 Chronic pain, not elsewhere classified | 4 | 47.17 | .001 | 229 | 38.17 | 164.61 |
| 59 | G89.29 Other chronic pain | 5 | 46.20 | .001 | 228 | 38.00 | 163.16 |
| 73 | G44 Other headache syndromes | 3 | 39.27 | .001 | 95 | 15.83 | 241.12 |
| 78 | G00–G09 Inflammatory diseases of the central nervous system | 2 | 31.56 | .001 | 51 | 8.50 | 300.00 |
| 82 | G43.0 Migraine without aura | 4 | 30.11 | .001 | 131 | 21.83 | 174.85 |
| 99 | G90 Disorders of autonomic nervous system | 3 | 26.46 | .001 | 44 | 7.33 | 295.63 |
| 101 | G44.5 Complicated headache syndromes | 4 | 25.75 | .001 | 24 | 4.00 | 400.00 |
| 106 | G93 Other disorders of brain | 3 | 24.61 | .001 | 138 | 23.00 | 152.17 |
| 112 | G04 Encephalitis, myelitis, and encephalomyelitis | 3 | 23.84 | .001 | 32 | 5.33 | 331.52 |
| 131 | G47.3 Sleep apnea | 4 | 20.12 | .001 | 284 | 47.33 | 92.27 |
| 135 | G44.52 New daily persistent headache (NDPH) | 5 | 19.39 | .001 | 20 | 3.33 | 380.48 |
| 144 | G43.01 Migraine without aura, intractable | 5 | 18.74 | .001 | 46 | 7.67 | 238.98 |
| 148 | G47.9 Sleep disorder, unspecified | 4 | 18.19 | .001 | 75 | 12.50 | 180.00 |
| 149 | G04.8 Other encephalitis, myelitis, and encephalomyelitis | 4 | 18.05 | .001 | 21 | 3.50 | 357.14 |
| 159 | G90.9 Disorder of the autonomic nervous system, unspecified | 4 | 16.87 | .001 | 22 | 3.67 | 335.97 |
| 168 | G93.3 Postviral fatigue syndrome | 4 | 16.13 | .001 | 9 | 1.50 | 500.00 |
| 176 | G43.019 Migraine without aura, intractable, without status migrainosus | 6 | 15.24 | .001 | 37 | 6.17 | 240.36 |
| 207 | G43.00 Migraine without aura, not intractable | 5 | 13.01 | .001 | 85 | 14.17 | 139.94 |
| 209 | G93.4 Other and unspecified encephalopathy | 4 | 12.87 | .001 | 64 | 10.67 | 162.42 |
| 223 | G43.009 Migraine without aura, not intractable, without status migrainosus | 6 | 12.37 | .002 | 76 | 12.67 | 144.67 |
| 231 | G44.89 Other headache syndrome | 5 | 11.74 | .002 | 15 | 2.50 | 340.00 |
| 235 | G44.8 Other specified headache syndromes | 4 | 11.62 | .002 | 20 | 3.33 | 290.39 |
| 241 | G47.30 Sleep apnea, unspecified | 5 | 11.38 | .003 | 54 | 9.00 | 166.67 |
| 258 | G04.81 Other encephalitis and encephalomyelitis | 5 | 10.68 | .012 | 16 | 2.67 | 311.99 |
| 272 | G90.1 Familial dysautonomia [Riley-Day] | 4 | 10.27 | .013 | 14 | 2.33 | 329.18 |
| 292 | G93.40 Encephalopathy, unspecified | 5 | 9.50 | .022 | 20 | 3.33 | 260.36 |
| 297 | G25 Other extrapyramidal and movement disorders | 3 | 9.40 | .023 | 32 | 5.33 | 200.19 |
| H00–H59 Diseases of the eye and adnexa | |||||||
| 238 | H53.1 Subjective visual disturbances | 4 | 11.44 | .002 | 13 | 2.17 | 360.83 |
| 256 | H53.14 Visual discomfort | 5 | 10.75 | .011 | 6 | 1.00 | 500.00 |
| 291 | H53–H54 Visual disturbances and blindness | 2 | 9.59 | .020 | 138 | 23.00 | 91.30 |
| 298 | H53 Visual disturbances | 3 | 9.38 | .023 | 114 | 19.00 | 100.00 |
| I00–I99 Diseases of the circulatory system | |||||||
| 32 | I00–I99 Diseases of the circulatory system | 1 | 95.20 | .001 | 682 | 113.67 | 133.13 |
| 75 | I30–I52 Other forms of heart disease | 2 | 35.57 | .001 | 193 | 32.17 | 154.90 |
| 151 | I95.1 Orthostatic hypotension | 4 | 17.71 | .001 | 17 | 2.83 | 394.70 |
| 157 | I95–I99 Other and unspecified disorders of the circulatory system | 2 | 16.93 | .001 | 52 | 8.67 | 211.42 |
| 163 | I95 Hypotension | 3 | 16.47 | .001 | 38 | 6.33 | 247.55 |
| 194 | I49 Other cardiac arrhythmias | 3 | 14.11 | .001 | 48 | 8.00 | 200.00 |
| 213 | I60–I69 Cerebrovascular diseases | 2 | 12.58 | .001 | 79 | 13.17 | 142.98 |
| 226 | I10–I19 Hypertensive diseases | 2 | 12.03 | .002 | 131 | 21.83 | 106.14 |
| 228 | I26–I28 Pulmonary heart disease and diseases of pulmonary circulation | 2 | 11.95 | .002 | 46 | 7.67 | 186.83 |
| 247 | I49.8 Other specified cardiac arrhythmias | 4 | 11.09 | .006 | 29 | 4.83 | 231.26 |
| 290 | I51 Complications and ill-defined descriptions of heart disease | 3 | 9.61 | .020 | 38 | 6.33 | 184.36 |
| J00–J99 Diseases of the respiratory system | |||||||
| 14 | J00–J99 Diseases of the respiratory system | 1 | 246.45 | .001 | 2185 | 364.17 | 118.58 |
| 35 | J40–J47 Chronic lower respiratory diseases | 2 | 86.15 | .001 | 682 | 113.67 | 126.09 |
| 36 | J45 Asthma | 3 | 83.40 | .001 | 661 | 110.17 | 126.01 |
| 64 | J96–J99 Other diseases of the respiratory system | 2 | 43.41 | .001 | 282 | 47.00 | 140.43 |
| 67 | J30–J39 Other diseases of upper respiratory tract | 2 | 41.35 | .001 | 480 | 80.00 | 102.50 |
| 69 | J45.9 Other and unspecified asthma | 4 | 40.97 | .001 | 193 | 32.17 | 167.33 |
| 74 | J09–J18 Influenza and pneumonia | 2 | 35.85 | .001 | 122 | 20.33 | 200.05 |
| 79 | J45.909 Unspecified asthma, uncomplicated | 6 | 31.00 | .001 | 139 | 23.17 | 171.90 |
| 85 | J45.90 Unspecified asthma | 5 | 29.52 | .001 | 160 | 26.67 | 154.97 |
| 103 | J96 Respiratory failure, not elsewhere classified | 3 | 25.29 | .001 | 154 | 25.67 | 145.42 |
| 114 | J00–J06 Acute upper respiratory infections | 2 | 23.47 | .001 | 460 | 76.67 | 77.38 |
| 117 | J45.4 Moderate persistent asthma | 4 | 22.92 | .001 | 111 | 18.50 | 164.86 |
| 118 | J96.0 Acute respiratory failure | 4 | 22.82 | .001 | 57 | 9.50 | 236.84 |
| 121 | J12.8 Other viral pneumonia | 4 | 22.55 | .001 | 20 | 3.33 | 410.51 |
| 122 | J12 Viral pneumonia, not elsewhere classified | 3 | 22.38 | .001 | 31 | 5.17 | 325.53 |
| 126 | J45.40 Moderate persistent asthma, uncomplicated | 5 | 21.38 | .001 | 91 | 15.17 | 176.86 |
| 134 | J12.82 Pneumonia due to coronavirus disease 2019 | 5 | 19.71 | .001 | 11 | 1.83 | 501.09 |
| 139 | J98 Other respiratory disorders | 3 | 19.14 | .001 | 125 | 20.83 | 140.04 |
| 166 | J38 Diseases of vocal cords and larynx, not elsewhere classified | 3 | 16.32 | .001 | 47 | 7.83 | 219.28 |
| 174 | J45.30 Mild persistent asthma, uncomplicated | 5 | 15.34 | .001 | 130 | 21.67 | 121.50 |
| 188 | J03 Acute tonsillitis | 3 | 14.49 | .001 | 27 | 4.50 | 277.78 |
| 196 | J35 Chronic diseases of tonsils and adenoids | 3 | 13.85 | .001 | 65 | 10.83 | 167.77 |
| 199 | J96.01 Acute respiratory failure with hypoxia | 5 | 13.45 | .001 | 34 | 5.67 | 235.10 |
| 216 | J22 Unspecified acute lower respiratory infection | 3 | 12.54 | .002 | 7 | 1.17 | 498.29 |
| 224 | J45.99 Other asthma | 5 | 12.25 | .002 | 33 | 5.50 | 227.27 |
| 232 | J80–J84 Other respiratory diseases principally affecting the interstitium | 2 | 11.73 | .002 | 28 | 4.67 | 242.61 |
| 236 | J45.3 Mild persistent asthma | 4 | 11.60 | .002 | 166 | 27.67 | 91.54 |
| 244 | J20–J22 Other acute lower respiratory infections | 2 | 11.26 | .006 | 41 | 6.83 | 192.83 |
| 254 | J15.21 Pneumonia due to Staphylococcus aureus | 5 | 10.75 | .011 | 6 | 1.00 | 500.00 |
| 255 | J15.2 Pneumonia due to Staphylococcus | 4 | 10.75 | .011 | 6 | 1.00 | 500.00 |
| 257 | J38.3 Other diseases of vocal cords | 4 | 10.68 | .012 | 16 | 2.67 | 311.99 |
| 262 | J15 Bacterial pneumonia, not elsewhere classified | 3 | 10.61 | .013 | 24 | 4.00 | 250.00 |
| 264 | J45.2 Mild intermittent asthma | 4 | 10.55 | .013 | 180 | 30.00 | 83.33 |
| 284 | J03.0 Streptococcal tonsillitis | 4 | 9.71 | .017 | 8 | 1.33 | 426.32 |
| 285 | J03.01 Acute recurrent streptococcal tonsillitis | 5 | 9.71 | .017 | 8 | 1.33 | 426.32 |
| 288 | J03.91 Acute recurrent tonsillitis, unspecified | 5 | 9.69 | .020 | 10 | 1.67 | 379.04 |
| 295 | J45.20 Mild intermittent asthma, uncomplicated | 5 | 9.44 | .022 | 143 | 23.83 | 88.84 |
| K00–K93 Diseases of the digestive system | |||||||
| 77 | K00–K93 Diseases of the digestive system | 1 | 35.37 | .001 | 1701 | 283.50 | 48.15 |
| 155 | K20–K31 Diseases of oesophagus, stomach, and duodenum | 2 | 17.20 | .001 | 343 | 57.17 | 76.67 |
| 179 | K55–K64 Other diseases of intestines | 2 | 14.87 | .001 | 625 | 104.17 | 51.68 |
| 225 | K59.0 Constipation | 4 | 12.19 | .002 | 505 | 84.17 | 52.07 |
| 249 | K59 Other functional intestinal disorders | 3 | 11.01 | .006 | 521 | 86.83 | 48.57 |
| 250 | K70–K77 Diseases of liver | 2 | 10.98 | .006 | 62 | 10.33 | 151.69 |
| 274 | K31.8 Other specified diseases of stomach and duodenum | 4 | 10.23 | .013 | 50 | 8.33 | 164.11 |
| 304 | K31 Other diseases of stomach and duodenum | 3 | 8.97 | .031 | 57 | 9.50 | 142.11 |
| L00–L99 Diseases of the skin and subcutaneous tissue | |||||||
| 62 | L00–L99 Diseases of the skin and subcutaneous tissue | 1 | 44.06 | .001 | 766 | 127.67 | 82.50 |
| 138 | L80–L99 Other disorders of the skin and subcutaneous tissue | 2 | 19.14 | .001 | 198 | 33.00 | 109.09 |
| 222 | L89 Pressure ulcer | 3 | 12.42 | .002 | 27 | 4.50 | 255.56 |
| 233 | L20–L30 Dermatitis and eczema | 2 | 11.69 | .002 | 248 | 41.33 | 74.21 |
| 268 | L49–L54 Urticaria and erythema | 2 | 10.41 | .013 | 53 | 8.83 | 160.48 |
| M00–M99 Diseases of the musculoskeletal system and connective tissue | |||||||
| 18 | M00–M99 Diseases of the musculoskeletal system and connective tissue | 1 | 215.57 | .001 | 3089 | 514.83 | 91.52 |
| 38 | M79 Other and unspecified soft tissue disorders, not elsewhere classified | 3 | 81.52 | .001 | 370 | 61.67 | 170.80 |
| 39 | M70–M79 Other soft tissue disorders | 2 | 79.67 | .001 | 402 | 67.00 | 161.19 |
| 41 | M20–M25 Other joint disorders | 2 | 77.45 | .001 | 1113 | 185.50 | 91.37 |
| 46 | M25.5 Pain in joint | 4 | 58.78 | .001 | 464 | 77.33 | 126.30 |
| 49 | M25 Other joint disorder, not elsewhere classified | 3 | 57.07 | .001 | 701 | 116.83 | 99.44 |
| 60 | M79.1 Myalgia | 4 | 45.14 | .001 | 109 | 18.17 | 241.22 |
| 70 | M79.6 Pain in limb, hand, foot, fingers, and toes | 4 | 40.67 | .001 | 211 | 35.17 | 158.74 |
| 80 | M86–M90 Other osteopathies | 2 | 30.38 | .001 | 95 | 15.83 | 209.54 |
| 90 | M79.10 Myalgia, unspecified site | 5 | 28.35 | .001 | 42 | 7.00 | 314.29 |
| 93 | M50–M54 Other dorsopathies | 2 | 27.90 | .001 | 220 | 36.67 | 126.34 |
| 97 | M54 Dorsalgia | 3 | 26.87 | .001 | 197 | 32.83 | 131.50 |
| 100 | M60–M63 Disorders of muscles | 2 | 26.43 | .001 | 375 | 62.50 | 92.00 |
| 102 | M62 Other disorders of muscle | 3 | 25.69 | .001 | 366 | 61.00 | 91.80 |
| 107 | M25.50 Pain in unspecified joint | 5 | 24.50 | .001 | 49 | 8.17 | 267.20 |
| 125 | M79.60 Pain in limb, unspecified | 5 | 22.11 | .001 | 96 | 16.00 | 175.00 |
| 137 | M25.56 Pain in knee | 5 | 19.22 | .001 | 174 | 29.00 | 117.24 |
| 142 | M30–M36 Systemic connective tissue disorders | 2 | 18.96 | .001 | 90 | 15.00 | 166.67 |
| 143 | M62.8 Other specified disorders of muscle | 4 | 18.80 | .001 | 325 | 54.17 | 82.76 |
| 153 | M79.18 Myalgia, other site | 5 | 17.23 | .001 | 64 | 10.67 | 190.53 |
| 162 | M35 Other systemic involvement of connective tissue | 3 | 16.47 | .001 | 38 | 6.33 | 247.55 |
| 164 | M02.30 Reiter’s disease, unspecified site | 5 | 16.45 | .001 | 12 | 2.00 | 450.00 |
| 167 | M00–M02 Infectious arthropathies | 2 | 16.28 | .001 | 18 | 3.00 | 366.67 |
| 169 | M24 Other specific joint derangements | 3 | 16.00 | .001 | 147 | 24.50 | 116.33 |
| 183 | M89 Other disorders of bone | 3 | 14.60 | .001 | 38 | 6.33 | 231.75 |
| 186 | M02.3 Reiter’s disease | 4 | 14.54 | .001 | 15 | 2.50 | 380.00 |
| 187 | M02 Postinfective and reactive arthropathies | 3 | 14.54 | .001 | 15 | 2.50 | 380.00 |
| 190 | M99 Biomechanical lesions, not elsewhere classified | 3 | 14.33 | .001 | 8 | 1.33 | 501.50 |
| 191 | M99–M99 Biomechanical lesions, not elsewhere classified | 2 | 14.33 | .001 | 8 | 1.33 | 501.50 |
| 192 | M99.0 Segmental and somatic dysfunction | 4 | 14.33 | .001 | 8 | 1.33 | 501.50 |
| 204 | M62.81 Muscle weakness (generalized) | 5 | 13.11 | .001 | 163 | 27.17 | 98.75 |
| 221 | M79.66 Pain in lower leg | 5 | 12.42 | .002 | 27 | 4.50 | 255.56 |
| 245 | M35.7 Hypermobility syndrome | 4 | 11.17 | .006 | 26 | 4.33 | 246.42 |
| 263 | M86 Osteomyelitis | 3 | 10.58 | .013 | 36 | 6.00 | 200.00 |
| 271 | M24.9 Joint derangement, unspecified | 4 | 10.27 | .013 | 19 | 3.17 | 278.55 |
| 277 | M79.605 Pain in left leg | 6 | 10.08 | .013 | 37 | 6.17 | 191.73 |
| 281 | M79.662 Pain in left lower leg | 6 | 9.92 | .015 | 12 | 2.00 | 350.00 |
| 287 | M89.1 Physeal arrest | 4 | 9.69 | .020 | 10 | 1.67 | 379.04 |
| 300 | M25.561 Pain in right knee | 6 | 9.34 | .024 | 90 | 15.00 | 113.33 |
| 301 | M21 Other acquired deformities of limbs | 3 | 9.30 | .024 | 205 | 34.17 | 72.67 |
| N00–N99 Diseases of the genitourinary system | |||||||
| 130 | N00–N99 Diseases of the genitourinary system | 1 | 20.35 | .001 | 768 | 128.00 | 54.69 |
| 195 | N17 Acute kidney failure | 3 | 13.99 | .001 | 39 | 6.50 | 223.08 |
| 220 | N76 Other inflammation of vagina and vulva | 3 | 12.42 | .002 | 27 | 4.50 | 255.56 |
| 278 | N17.9 Acute kidney failure, unspecified | 4 | 9.99 | .013 | 34 | 5.67 | 199.82 |
| 293 | N80–N98 Noninflammatory disorders of female genital tract | 2 | 9.46 | .022 | 263 | 43.83 | 64.27 |
| 303 | N70–N77 Inflammatory diseases of female pelvic organs | 2 | 9.03 | .031 | 36 | 6.00 | 183.33 |
| Q00–Q99 Congenital malformations, deformations, and chromosomal abnormalities | |||||||
| 182 | Q79 Congenital malformations of musculoskeletal system, not elsewhere classified | 3 | 14.63 | .001 | 47 | 7.83 | 206.51 |
| 198 | Q79.6 Ehlers-Danlos syndromes | 4 | 13.45 | .001 | 43 | 7.17 | 206.83 |
| 202 | Q00–Q99 Congenital malformations, deformations, and chromosomal abnormalities | 1 | 13.18 | .001 | 700 | 116.67 | 45.71 |
| 260 | Q20–Q28 Congenital malformations of the circulatory system | 2 | 10.62 | .012 | 93 | 15.50 | 119.35 |
| R00–R99 Symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified | |||||||
| 1 | R00–R99 Symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified | 1 | 1327.81 | .001 | 6736 | 1122.67 | 160.72 |
| 6 | R00–R09 Symptoms and signs involving the circulatory and respiratory systems | 2 | 608.75 | .001 | 1533 | 255.50 | 235.81 |
| 7 | R06.0 Dyspnea | 4 | 334.81 | .001 | 306 | 51.00 | 403.92 |
| 8 | R50–R69 General symptoms and signs | 2 | 326.26 | .001 | 1791 | 298.50 | 153.94 |
| 9 | R06 Abnormalities of breathing | 3 | 313.01 | .001 | 546 | 91.00 | 287.91 |
| 19 | R53 Malaise and fatigue | 3 | 197.77 | .001 | 387 | 64.50 | 270.54 |
| 20 | R53.8 Other malaise and fatigue | 4 | 189.63 | .001 | 326 | 54.33 | 290.21 |
| 21 | R10–R19 Symptoms and signs involving the digestive system and abdomen | 2 | 154.74 | .001 | 1400 | 233.33 | 117.29 |
| 22 | R40–R46 Symptoms and signs involving cognition, perception, emotional state, and behavior | 2 | 142.00 | .001 | 628 | 104.67 | 173.24 |
| 23 | R07 Pain in throat and chest | 3 | 137.91 | .001 | 209 | 34.83 | 310.57 |
| 24 | R06.02 Shortness of breath | 5 | 137.06 | .001 | 119 | 19.83 | 414.37 |
| 26 | R53.83 Other fatigue | 5 | 121.77 | .001 | 209 | 34.83 | 290.47 |
| 28 | R06.00 Dyspnea, unspecified | 5 | 103.08 | .001 | 92 | 15.33 | 408.81 |
| 31 | R06.09 Other forms of dyspnea | 5 | 96.99 | .001 | 71 | 11.83 | 449.45 |
| 34 | R07.9 Chest pain, unspecified | 4 | 88.76 | .001 | 120 | 20.00 | 330.00 |
| 37 | R42 Dizziness and giddiness | 3 | 81.90 | .001 | 155 | 25.83 | 275.53 |
| 40 | R51 Headache | 3 | 77.98 | .001 | 188 | 31.33 | 241.53 |
| 43 | R51.9 Headache, unspecified | 4 | 71.08 | .001 | 167 | 27.83 | 244.95 |
| 44 | R00 Abnormalities of heart beat | 3 | 70.07 | .001 | 160 | 26.67 | 248.71 |
| 45 | R10 Abdominal and pelvic pain | 3 | 62.08 | .001 | 564 | 94.00 | 117.02 |
| 47 | R05 Cough | 3 | 57.90 | .001 | 295 | 49.17 | 160.32 |
| 54 | R25–R29 Symptoms and signs involving the nervous and musculoskeletal systems | 2 | 52.31 | .001 | 321 | 53.50 | 144.86 |
| 56 | R07.89 Other chest pain | 5 | 47.31 | .001 | 62 | 10.33 | 335.62 |
| 58 | R07.8 Other chest pain | 4 | 46.89 | .001 | 72 | 12.00 | 308.33 |
| 61 | R11 Nausea and vomiting | 3 | 44.98 | .001 | 344 | 57.33 | 128.50 |
| 66 | R00.2 Palpitations | 4 | 41.77 | .001 | 65 | 10.83 | 306.28 |
| 68 | R09 Other symptoms and signs involving the circulatory and respiratory system | 3 | 41.14 | .001 | 238 | 39.67 | 149.56 |
| 72 | R53.82 Chronic fatigue, unspecified | 5 | 40.04 | .001 | 57 | 9.50 | 321.05 |
| 84 | R06.8 Other abnormalities of breathing | 4 | 29.75 | .001 | 188 | 31.33 | 142.58 |
| 86 | R50 Fever of other and unknown origin | 3 | 29.25 | .001 | 175 | 29.17 | 146.83 |
| 87 | R90–R96 Abnormal findings on diagnostic imaging and in function studies, without diagnosis | 2 | 29.08 | .001 | 216 | 36.00 | 130.56 |
| 88 | R00.0 Tachycardia, unspecified | 4 | 28.77 | .001 | 68 | 11.33 | 244.22 |
| 89 | R53.81 Other malaise | 5 | 28.50 | .001 | 60 | 10.00 | 260.00 |
| 91 | R70–R79 Abnormal findings on examination of blood, without diagnosis | 2 | 28.31 | .001 | 230 | 38.33 | 124.37 |
| 92 | R20–R23 Symptoms and signs involving the skin and subcutaneous tissue | 2 | 28.25 | .001 | 200 | 33.33 | 134.02 |
| 95 | R29 Other symptoms and signs involving the nervous and musculoskeletal systems | 3 | 27.58 | .001 | 191 | 31.83 | 135.63 |
| 98 | R05.9 Cough, unspecified | 4 | 26.70 | .001 | 150 | 25.00 | 152.00 |
| 104 | R55 Syncope and collapse | 3 | 25.15 | .001 | 80 | 13.33 | 207.58 |
| 105 | R43 Disturbances of smell and taste | 3 | 24.64 | .001 | 36 | 6.00 | 316.67 |
| 108 | R09.0 Asphyxia and hypoxemia | 4 | 24.49 | .001 | 72 | 12.00 | 216.67 |
| 109 | R09.02 Hypoxemia | 5 | 24.49 | .001 | 72 | 12.00 | 216.67 |
| 110 | R50.9 Fever, unspecified | 4 | 24.46 | .001 | 142 | 23.67 | 149.26 |
| 113 | R19 Other symptoms and signs involving the digestive system and abdomen | 3 | 23.76 | .001 | 144 | 24.00 | 145.83 |
| 115 | R30–R39 Symptoms and signs involving the urinary system | 2 | 23.09 | .001 | 254 | 42.33 | 105.53 |
| 120 | R41 Other symptoms and signs involving cognitive functions and awareness | 3 | 22.70 | .001 | 122 | 20.33 | 155.78 |
| 127 | R68 Other general symptoms and signs | 3 | 20.63 | .001 | 103 | 17.17 | 162.09 |
| 132 | R10.8 Other abdominal pain | 4 | 20.08 | .001 | 167 | 27.83 | 122.78 |
| 136 | R11.10 Vomiting, unspecified | 5 | 19.32 | .001 | 162 | 27.00 | 122.22 |
| 140 | R10.9 Unspecified abdominal pain | 4 | 19.12 | .001 | 107 | 17.83 | 152.38 |
| 141 | R10.84 Generalized abdominal pain | 5 | 19.04 | .001 | 163 | 27.17 | 120.83 |
| 145 | R06.83 Snoring | 5 | 18.63 | .001 | 84 | 14.00 | 171.43 |
| 146 | R13 Aphagia and dysphagia | 3 | 18.48 | .001 | 250 | 41.67 | 94.38 |
| 147 | R13.1 Dysphagia | 4 | 18.48 | .001 | 250 | 41.67 | 94.38 |
| 150 | R09.8 Other specified symptoms and signs involving the circulatory and respiratory systems | 4 | 17.74 | .001 | 160 | 26.67 | 117.47 |
| 152 | R20 Disturbances of skin sensation | 3 | 17.38 | .001 | 34 | 5.67 | 270.37 |
| 154 | R11.1 Vomiting | 4 | 17.22 | .001 | 198 | 33.00 | 103.03 |
| 160 | R46 Symptoms and signs involving appearance and behavior | 3 | 16.74 | .001 | 103 | 17.17 | 144.61 |
| 165 | R29.90 Unspecified symptoms and signs involving the nervous system | 5 | 16.45 | .001 | 12 | 2.00 | 450.00 |
| 170 | R46.8 Other symptoms and signs involving appearance and behavior | 4 | 15.86 | .001 | 102 | 17.00 | 141.18 |
| 173 | R68.8 Other general symptoms and signs | 4 | 15.36 | .001 | 89 | 14.83 | 149.49 |
| 175 | R10.1 Pain localized to upper abdomen | 4 | 15.34 | .001 | 130 | 21.67 | 121.50 |
| 177 | R68.89 Other general symptoms and signs | 5 | 15.13 | .001 | 79 | 13.17 | 158.16 |
| 178 | R11.2 Nausea with vomiting, unspecified | 4 | 15.13 | .001 | 62 | 10.33 | 180.74 |
| 181 | R29.9 Unspecified symptoms and signs involving the nervous and musculoskeletal systems | 4 | 14.75 | .001 | 17 | 2.83 | 359.36 |
| 184 | R11.0 Nausea | 4 | 14.59 | .001 | 84 | 14.00 | 150.00 |
| 193 | R19.7 Diarrhea, unspecified | 4 | 14.33 | .001 | 92 | 15.33 | 141.36 |
| 197 | R52 Pain, unspecified | 3 | 13.61 | .001 | 49 | 8.17 | 193.76 |
| 201 | R63 Symptoms and signs concerning food and fluid intake | 3 | 13.24 | .001 | 274 | 45.67 | 75.17 |
| 205 | R53.1 Weakness | 4 | 13.11 | .001 | 60 | 10.00 | 170.00 |
| 206 | R20.2 Paresthesia of skin | 4 | 13.06 | .001 | 10 | 1.67 | 438.92 |
| 219 | R13.10 Dysphagia, unspecified | 5 | 12.46 | .002 | 98 | 16.33 | 126.58 |
| 227 | R10.13 Epigastric pain | 5 | 12.03 | .002 | 77 | 12.83 | 141.62 |
| 229 | R04 Hemorrhage from respiratory passages | 3 | 11.95 | .002 | 56 | 9.33 | 167.95 |
| 234 | R05.3 Chronic cough | 4 | 11.67 | .002 | 31 | 5.17 | 228.82 |
| 237 | R31 Hematuria | 3 | 11.49 | .002 | 47 | 7.83 | 180.97 |
| 243 | R09.81 Nasal congestion | 5 | 11.29 | .003 | 118 | 19.67 | 108.44 |
| 248 | R26 | 3 | 11.09 | .006 | 29 | 4.83 | 231.26 |
| 251 | R10.3 Pain localized to other parts of lower abdomen | 4 | 10.98 | .006 | 148 | 24.67 | 94.57 |
| 265 | R40 Somnolence, stupor, and coma | 3 | 10.52 | .013 | 33 | 5.50 | 209.09 |
| 266 | R01 Cardiac murmurs and other cardiac sounds | 3 | 10.52 | .013 | 27 | 4.50 | 233.33 |
| 269 | R46.89 Other symptoms and signs involving appearance and behavior | 5 | 10.35 | .013 | 94 | 15.67 | 116.98 |
| 273 | R79 Other abnormal findings of blood chemistry | 3 | 10.25 | .013 | 139 | 23.17 | 94.22 |
| 276 | R41.8 Other symptoms and signs involving cognitive functions and awareness | 4 | 10.10 | .013 | 91 | 15.17 | 117.53 |
| 279 | R59 Enlarged lymph nodes | 3 | 9.99 | .013 | 34 | 5.67 | 199.82 |
| 280 | R43.9 Unspecified disturbances of smell and taste | 4 | 9.92 | .015 | 12 | 2.00 | 350.00 |
| 282 | R93 Abnormal findings on diagnostic imaging of other body structures | 3 | 9.84 | .016 | 51 | 8.50 | 158.82 |
| 283 | R46.81 Obsessive-compulsive behavior | 5 | 9.71 | .017 | 8 | 1.33 | 426.32 |
| 289 | R04.0 Epistaxis | 4 | 9.65 | .020 | 48 | 8.00 | 162.50 |
| 299 | R01.1 Cardiac murmur, unspecified | 4 | 9.37 | .023 | 23 | 3.83 | 239.43 |
| S00–T98 Injury, poisoning, and certain other consequences of external causes | |||||||
| 302 | T86 Complications of transplanted organs and tissue | 3 | 9.19 | .027 | 60 | 10.00 | 140.00 |
| U00–U95 Codes for special purposes | |||||||
| 2 | U00–U49 Provisional assignment of new diseases of uncertain etiology or emergency use | 2 | 853.05 | .001 | 481 | 80.17 | 498.73 |
| 3 | U00–U95 Codes for special purposes | 1 | 853.05 | .001 | 481 | 80.17 | 498.73 |
| 4 | U09 Post COVID-19 condition | 3 | 614.57 | .001 | 343 | 57.17 | 499.97 |
| 5 | U09.9 Post COVID-19 condition, unspecified | 4 | 614.57 | .001 | 343 | 57.17 | 499.97 |
| 16 | U07 | 3 | 239.73 | .001 | 138 | 23.00 | 495.65 |
| 17 | U07.1 Emergency use of U07.1 | COVID-19 | 4 | 239.73 | .001 | 138 | 23.00 | 495.65 |
| V01–Y98 External causes of morbidity and mortality | |||||||
| 230 | V01–Y98 External causes of morbidity and mortality | 1 | 11.89 | .002 | 190 | 31.67 | 86.30 |
| 296 | V00–V99 Transport accidents | 2 | 9.41 | .022 | 156 | 26.00 | 84.62 |
| Z00–Z99 Factors influencing health status and contact with health services | |||||||
| 83 | Z00–Z99 Factors influencing health status and contact with health services | 1 | 29.88 | .001 | 1843 | 307.17 | 42.27 |
| 124 | Z69–Z76 Persons encountering health services in other circumstances | 2 | 22.15 | .001 | 258 | 43.00 | 102.33 |
| 156 | Z99.8 Dependence on other enabling machines and devices | 4 | 17.06 | .001 | 81 | 13.50 | 166.67 |
| 172 | Z99.81 Dependence on supplemental oxygen | 5 | 15.74 | .001 | 45 | 7.50 | 220.00 |
| 180 | Z89 Acquired absence of limb | 3 | 14.75 | .001 | 11 | 1.83 | 446.45 |
| 218 | Z99 Dependence on enabling machines and devices, not elsewhere classified | 3 | 12.52 | .002 | 133 | 22.17 | 107.49 |
| 259 | Z77–Z99 Persons with potential health hazards related to family and personal history and certain conditions influencing health status | 2 | 10.62 | .012 | 579 | 96.50 | 45.08 |
DISCUSSION
We have employed a tree-based data mining approach to detect new-onset conditions presenting in children with a PASC (U09.9 or B94.8) diagnosis. Our data-driven approach identified and ranked features in a large corpus of EHR data.
Comparison of PASC-diagnosed and non-PASC-diagnosed SARS-CoV-2 positive patients
In the first of our 2 primary analyses, we compared PASC-diagnosed patients with non-PASC-diagnosed SARS-CoV-2 positive patients. The signals identified indicate long-term sequelae of PASC that differentiate from having COVID-19.
Significant results from this comparison included both systemic and syndromic manifestations of PASC, with the former describing organ-level dysfunction and the latter focusing on signs and symptoms. Consistent with other studies and biologic mechanisms, we found significant enrichment among children with PASC in cardiac, respiratory, neurologic, psychological, endocrine, gastrointestinal, and musculoskeletal systems.27
We found the most significant point of difference between PASC and COVID-19 positive children was at the R00–R99 cluster of diagnostic codes (Symptoms, signs, and abnormal clinical and laboratory findings, not otherwise classified). These codes designate abnormal clinical findings not elsewhere described that encompass a range of organ systems. This finding is not surprising given the heterogeneity of previously reported manifestations of PASC and the difficulty in gaining clinical consensus to define PASC.28,29
Within the R00–R99 category, the codes with the greatest signal are symptoms related to circulatory and respiratory systems. These results align again with prior observations in smaller groups of patients or previous studies, and include dyspnea,12,16 shortness of breath,16,30 and other breathing abnormalities31; chest pain10,32,33; malaise and fatigue14,30,33,34; cough14; and abnormalities of heartbeat including palpitations and tachycardia.35,36 However, within this category we also detected novel signals such as hematuria as well as nonspecific symptoms and signs involving the urinary system.
Neurologic diagnoses such as headache and migraine were recurring, with several specific codes enriched in the cases. Sleep disturbances and, specifically, sleep apnea, were also present.12,31 Generalized pain was a key feature in our musculoskeletal system findings, which include nonlocalized myalgias, joint pain, knee and leg pain, hip pain, upper abdomen and epigastric pain, and generalized soft tissue pain. The recurring appearance of multiple and diverse pain symptoms in this study warrants further investigation to better characterize causal biologic pathways.
Respiratory conditions were also significantly featured in our analysis. Both vocal cord disorders and dysautonomia were present as PASC-related features in our study. Interestingly, new onset asthma was present in our results as a specific diagnosis rather than a constellation of nonspecific symptoms. Asthma is one of the few specific health conditions with a significant and strong signal in our study. Respiratory findings associated with PASC have been characterized in detail elsewhere.9
In contrast to previous work, our study did not identify new-onset diabetes as a persistent long-term complication of COVID-19.37 Endocrine findings in this study included nutritional deficiencies, volume depletion or fluid overload, and obesity. To our knowledge, these symptoms have not been described in detail elsewhere. It is unclear whether clinicians are recording obesity in the post-infection period as an indication that obesity complicated recovery of SARS-CoV-2 infection or that it points to a patient’s exacerbation of health conditions unrelated to COVID-19.
Gastrointestinal (eg, Diseases of esophagus, stomach, and duodenum) and psychological findings (eg, Reaction to severe stress, and adjustment disorders) followed a pattern of TreeScan cuts primarily at nonspecific levels. Future work should focus on characterizing co-occurrences of these nonspecific symptoms across body systems to detect clinically meaningful patterns. The branches of the ICD hierarchy that are a priori unlikely to be related to COVID-19, eg, injuries (S00–T98), external causes of morbidity and mortality (V01–Y98), and congenital malformations, deformations, and chromosomal abnormalities (Q00–Q99) serve as a negative control outcome; the relative dearth of diagnoses from these branches serves as a check on residual bias from unmeasured confounding.
Comparison of PASC-diagnosed and SARS-CoV-2 negative patients
We also compared children with a PASC diagnosis code to SARS-CoV-2 test-negative patients. Most cuts from this comparator cohort overlap with the findings where SARS-CoV-2 test-positive patients served as the control. These demonstrate consistency and increase the likelihood that these findings are truly associated with PASC. Additionally, several diagnoses unique to the test-negative cohort were identified, many of which include symptoms relating to acute respiratory infection. Some specific infection codes, such as B25, Cytomegaloviral Disease (CMV) were found significant, which may be a result of reactivation in patients infected with SARS-CoV-2.38 Other codes, such as D89, Other disorders involving the immune mechanism, not elsewhere classified, or skin conditions such as dermatitis and eczema (L20–L30), were also enriched in the PASC patients when compared to SARS-CoV-2 negative patients. Autoimmunity following an infection has been documented and warrants further investigation in the pediatric population.39 Alternate findings enriched in this analysis include features plausibly associated with COVID-19 infection including acute myocarditis, hypotension, fever, nasal congestion, epistaxis, tachycardia, and gastrointestinal symptoms such as diarrhea, constipation, and gastroenteritis. More serious conditions such as pulmonary embolism and pulmonary edema were also enriched in this population but may be due to follow up care from an acute COVID-19 infection, and not a new finding in the post-acute period. However, these findings warrant further investigation.
Compared to previous work identifying pediatric PASC features by comparing SARS-CoV-2 test-positive to test-negative patients in the PEDSnet EHR, we found several differences. Abnormal liver enzymes, allergies, disorders of teeth/gingiva, and bronchiolitis were all reported as potential PASC-associated features in Rao et al,17 but were not identified as significant cuts in this study when PASC patients were compared to COVID+ or COVID− cohorts, either at the specific code or macro level. Conversely, significant findings in our study which were not present in the results of Rao et al,17 and included sleep disorders, anemias, eye disorders, constipation, sepsis, nutritional deficiencies, hypotension, and various musculoskeletal conditions and soft tissue and muscle disorders.
Sensitivity analyses
Finally, we conducted 2 sensitivity analyses: the first comparing COVID positive to COVID negative patients, and the second comparing PASC-positive to COVID positive patients pre- and post-omicron. By identifying events that occur in the PASC risk window more frequently in COVID-positive patients, we can increase the sensitivity of capturing potential PASC features. This may come at the expense of precision, as we recognize that statistical signals identified in this analysis may correspond to features not truly associated with PASC, either due to confounding resulting from a more heterogeneous population than PASC-diagnosed patients or due to surveillance bias due to COVID-positivity. While there was significant overlap of the features identified in this and the primary analyses, there were also many additional features identified in the COVID-positive to COVID-negative analysis. In our analysis stratified by pre- and post-omicron variant, we found that the pre-omicron era was enriched for metabolic (eg, E70–E88: metabolic disorders), immunologic (eg, D80–D89: Certain disorders involving the immune mechanism), and circulatory system (eg, I95: hypotension) codes, as well as disturbances of smell and taste, while the post-omicron era was enriched for conditions affecting the urinary system (eg, R31: hematuria) and multiple migraine diagnoses. However, further analyses and additional methodologic rigor to ensure adequate power as well as balance of visit utilization and other potential confounders between the cohorts is warranted and beyond the scope of the current analysis. In our analysis stratified by pre-omicron and omicron variants, we found that the pre-omicron era was enriched for metabolic (eg, E70–E88: metabolic disorders), immunologic (eg, D80–D89: Certain disorders involving the immune mechanism), and circulatory system (eg, I95: hypotension) codes, as well as disturbances of smell and taste, while the omicron era was enriched for conditions affecting the urinary system (eg, R31: hematuria) and multiple migraine diagnoses. However, further analyses and additional methodologic rigor to ensure adequate power as well as balance of potential confounders between the cohorts is warranted and beyond the scope of the current analysis.
Study strengths and limitations
Strengths of our study include using a tree-based scan statistic approach in children to detect groups of clinical diagnoses specific to this population, as well as the use of the U09.9 and B94.8 diagnosis codes to do so. Our study is further strengthened by multiple comparison groups diagnoses of PASC rather than surveys or case series analyses. We have confirmed previous findings and provide new insights into how diagnosis clusters relate to each other in importance. Further, an advantage of EHR data is the ability to learn from previous clinical history of patients. In our analysis, we included an 18-month washout period to ensure that the signals we were observing were not due to baseline differences in disease prevalence.
Prior work identifying pediatric PASC-associated features17 relied on a set of diagnosis clusters developed by the study team to group similar diagnoses. Our study addresses this methodological limitation by a broader approach where diagnosis clusters are tested along all levels of the ICD-10-CM hierarchy. Importantly, among features of PASC found in previous work, our study contributes precise, diagnosis code-level results showing how PASC features are identified in clinical practice. This makes our findings ideally suited for development of rules-based phenotypes for identifying pediatric PASC in EHRs.
At the same time, there were several significant limitations to our study. First, we are at risk of misclassifying patients in our PASC-negative comparator cohort by relying solely on the U09.9 and B94.8 codes to identify cases. There are likely children and adolescents in our comparison cohort with complications of COVID-19 who never receive a formal PASC diagnosis and may either present to a health system with symptoms that the clinician did not distinguish as a complication of COVID-19 or may not receive care for their symptoms at all. However, this would likely bias toward the null. Further, the U09.9 code has only been formally implemented since October 2021, and while the B94.8 code likely served as a proxy for PASC prior to this, the likely lack of uniform code usage, particularly early in the pandemic, introduces potential bias with regards to the timing of cohort entry dates in our cohort during the pandemic. Additionally, for PASC-diagnosed and serology test positive patients in our cohort who had no prior COVID diagnoses or positive viral testing, our imputation of cohort entry dates may not accurately reflect timing of COVID infection, and in the case of PASC-diagnosed patients, PASC onset. Second, our ascertainment of other diagnosis codes is similarly subject to the biases of health care delivery. For example, our findings may disproportionately include diagnoses that are required for utilization (eg, to justify diagnostic testing) or symptoms that are uncommon and previously associated in clinical practice with COVID-19 and may under-detect changes following COVID-19 in relatively common childhood illness that escape coding practices. Third, we have analyzed the pandemic as a single cross-section and thus our results concern PASC-associated features in aggregate over the time period of the study; the course of PASC may differ by variant and further information may be gained by studying evolution of diagnoses across different portions of the pandemic or over time since infection. Finally, the cohort comprises patients followed in large pediatric health systems, and results may reflect the largely urban demographics of these systems or the practice patterns of pediatric specialists. Only about half of these hospitals offer robust primary care networks, and therefore children seen in tertiary care centers exclusively may not be representative of all children in the United States. This is complicated by the fact that children may only visit these health systems occasionally (eg, ED visits) and receive the majority of their care elsewhere. Nonetheless, despite these limitations, in previous studies, we have successfully replicated similar rates of health outcomes in our database as have been reported in data representative of the general pediatric population.40,41 In the COVID-19 context, we have reported that 76% of our patient population have no chronic conditions, 12% have chronic conditions, and 11% have complex-chronic conditions,42 which are similar to patients found in medicated populations.43 Further, the risk of this bias altering the findings of the current study relies on differential impact on cases and controls, and we have mitigated this risk by matching on medical complexity and demographic factors. Finally, we required at least 2 encounters with the health system 7 days to 18 months prior to cohort entry to ensure history of clinical care within the network.
CONCLUSION
This systematic evaluation of diagnoses in a large, multisystem national cohort of children with PASC provides a valuable addition to our understanding of this condition’s protean manifestations. Our results can inform the design of further prospective studies to more deeply investigate the patterns identified here to develop improved clinical practice and to direct the study of the biological basis of PASC.
Supplementary Material
ACKNOWLEDGMENTS
The authors gratefully acknowledge the contributions of Miranda Higginbotham.
Footnotes
More information on the PEDSnet RECOVER cohort is available at https://github.com/PEDSnet/Data_Models_Public/blob/master/PEDSnet/docs/RECOVER%20Cohort.md
Contributor Information
Vitaly Lorman, Applied Clinical Research Center, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania, USA.
Suchitra Rao, Department of Pediatrics, University of Colorado School of Medicine and Children’s Hospital of Colorado, Aurora, Colorado, USA.
Ravi Jhaveri, Division of Infectious Diseases, Ann & Robert H. Lurie Children’s Hospital of Chicago, Chicago, Illinois, USA.
Abigail Case, Division of Physical Medicine & Rehabilitation, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania, USA.
Asuncion Mejias, Division of Infectious Diseases, Department of Pediatrics, Nationwide Children’s Hospital and The Ohio State University, Columbus, Ohio, USA.
Nathan M Pajor, Division of Pulmonary Medicine, Cincinnati Children’s Hospital Medical Center, University of Cincinnati College of Medicine, Cincinnati, Ohio, USA.
Payal Patel, Department of Neurology, University of Washington, Seattle, Washington, USA.
Deepika Thacker, Nemours Cardiac Center, Nemours Children’s Health, Wilmington, Delaware, USA.
Seuli Bose-Brill, Internal Medicine and Pediatrics Section, Division of General Internal Medicine, Department of Internal Medicine, Ohio State University College of Medicine and Ohio State University Wexner Medical Center, Columbus, Ohio, USA.
Jason Block, Division of Chronic Disease Research Across the Lifecourse, Department of Population Medicine, Harvard Pilgrim Health Care Institute, Harvard Medical School, Boston, Massachusetts, USA.
Patrick C Hanley, Division of Endocrinology, Nemours Children’s Hospital, Wilmington, Delaware, USA.
Priya Prahalad, Division of Endocrinology, Department of Pediatrics, Stanford University, Stanford, California, USA.
Yong Chen, Department of Biostatistics, Epidemiology and Informatics, University of Pennsylvania, Philadelphia, Pennsylvania, USA.
Christopher B Forrest, Applied Clinical Research Center, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania, USA.
L Charles Bailey, Applied Clinical Research Center, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania, USA.
Grace M Lee, Division of Infectious Diseases, Department of Pediatrics, Stanford University School of Medicine, Stanford, California, USA.
Hanieh Razzaghi, Applied Clinical Research Center, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania, USA.
FUNDING
This research was funded by the National Institutes of Health (NIH) Agreement OT2HL161847-01 as part of the Researching COVID to Enhance Recovery (RECOVER) program of research.
AUTHOR CONTRIBUTIONS
LCB, VL, and HR had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. GML, VL, and HR were responsible for the study conceptualization and design. GML, VL, HR, and YC were involved in statistical analyses. GML, VL, and HR contributed to the drafting of the manuscript. All authors contributed to interpretation of the data and review of the manuscript. SR, GML, LCB, and CBF were involved in obtaining funding for the study. The content is solely the responsibility of the authors and does not necessarily represent the official views of the RECOVER Program, the NIH, or other funders.
SUPPLEMENTARY MATERIAL
Supplementary material is available at JAMIA Open online.
CONFLICT OF INTEREST STATEMENT
SR reports prior grant support from GSK and Biofire and is a consultant for Sequiris. RJ is a consultant for AstraZeneca, Seqirus, Dynavax, receives an editorial stipend from Elsevier and Pediatric Infectious Diseases Society and royalties from Up To Date/Wolters Kluwer. AM reports funding from Janssen and Merck for research support; Janssen, Merck and Sanofi-Pasteur for Advisory Board participation, and Sanofi-Pasteru and AstraZeneca for CME lectures. PP reports funding from the National Institute of Health and Bayer Pharmaceuticals. SB-B received support from Novartis and Regeneron Pharmaceuticals within in the last year. YC receives consulting support from GSK. LCB has received grants from Patient-Centered Outcomes Research Institute. All other authors have nothing to disclose.
DATA AVAILABILITY
The results reported here are based on detailed individual-level patient data compiled as part of the RECOVER Program. Due to the high risk of reidentification based on the number of unique patterns in the date, patient privacy regulations prohibit us from releasing the data publicly. The data are maintained in a secure enclave, with access managed by the program coordinating center to remain compliant with regulatory and program requirements. Please direct requests to access the data, either for reproduction of the work reported here or for other purposes, to recover@chop.edu.
REFERENCES
- 1. RECOVER: Researching COVID to Enhance Recovery. https://recovercovid.org. Accessed July 10, 2022.
- 2. Younger DS. Post-acute sequelae of SARS-CoV-2 infection (PASC): peripheral, autonomic, and central nervous system features in a child. Neurol Sci 2021; 42 (10): 3959–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pfaff ER, Girvin AT, Bennett TD, et al. ; N3C Consortium. Identifying who has long COVID in the USA: a machine learning approach using N3C data. Lancet Digit Health 2022; 4 (7): e532–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Munipalli B, Seim L, Dawson NL, Knight D, Dabrh AMA.. Post-acute sequelae of COVID-19 (PASC): a meta-narrative review of pathophysiology, prevalence, and management. SN Compr Clin Med 2022; 4 (1): 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Reese J, Blau H, Casiraghi E, et al. Generalizable long COVID subtypes: Findings from the NIH N3C and RECOVER. eBioMedicine2023; 87: 104413. doi: 10.1016/j.ebiom.2022.104413. [DOI] [PMC free article] [PubMed]
- 6. Yoo SM, Liu TC, Motwani Y, et al. Factors associated with post-acute sequelae of SARS-CoV-2 (PASC) after diagnosis of symptomatic COVID-19 in the inpatient and outpatient setting in a diverse cohort. J Gen Intern Med 2022; 37 (8): 1988–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zhang H, Zang C, Xu Z, et al. Data-driven identification of post-acute SARS-CoV-2 infection subphenotypes. Nat Med 2023; 29 (1): 226–35. doi: 10.1038/s41591-022-02116-3. [DOI] [PMC free article] [PubMed]
- 8. Behnood SA, Shafran R, Bennett SD, et al. Persistent symptoms following SARS-CoV-2 infection amongst children and young people: a meta-analysis of controlled and uncontrolled studies. J Infect 2022; 84 (2): 158–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Palacios S, Krivchenia K, Eisner M, et al. Long-term pulmonary sequelae in adolescents post-SARS-CoV-2 infection. Pediatr Pulmonol 2022; 57 (10): 2455–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ashkenazi-Hoffnung L, Shmueli E, Ehrlich S, et al. Long COVID in children: observations from a designated pediatric clinic. Pediatr Infect Dis J 2021; 40 (12): e509–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Asadi-Pooya AA, Nemati M, Nemati H.. ‘Long COVID’: symptom persistence in children hospitalised for COVID-19. J Paediatr Child Health 2022; 58 (10): 1836–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Buonsenso D, Munblit D, De Rose C, et al. Preliminary evidence on long COVID in children. Acta Paediatr 2021; 110 (7): 2208–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fainardi V, Meoli A, Chiopris G, et al. Long COVID in children and adolescents. Life 2022; 12 (2): 9950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Roge I, Smane L, Kivite-Urtane A, et al. Comparison of persistent symptoms after COVID-19 and other non-SARS-CoV-2 infections in children. Front Pediatr 2021; 9: 752385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Thallapureddy K, Thallapureddy K, Zerda E, et al. Long-term complications of COVID-19 infection in adolescents and children. Curr Pediatr Rep 2022; 10 (1): 11–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Brackel CLH, Lap CR, Buddingh EP, et al. Pediatric long-COVID: an overlooked phenomenon? Pediatr Pulmonol 2021; 56 (8): 2495–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rao S, Lee GM, Razzaghi H, et al. Clinical features and burden of post-acute sequelae of SARS-CoV-2 infection in children and adolescents. JAMA Pediatr 2022; 176 (10): 1000. doi: 10.1001/jamapediatrics.2022.2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. aapmr. CDC announces approval of ICD-10 code for post-acute sequelae of COVID-19. 2021. https://www.aapmr.org/members-publications/member-news/member-news-details/2021/07/20/cdc-announces-approval-of-icd-10-code-for-post-acute-sequelae-of-covid-19. Accessed July 8, 2022.
- 19. Mejias A, Schuchard J, Rao S, et al. Leveraging serologic testing to identify children at risk for post-acute sequelae of SARS-CoV-2 infection: an EHR-based cohort study from the RECOVER program [published online ahead of print February 21, 2023]. J Pediatr. doi: 10.1016/j.jpeds.2023.02.005. [DOI] [PMC free article] [PubMed]
- 20. Wang SV, Jin Y, Fireman B, et al. Relative performance of propensity score matching strategies for subgroup analyses. Am J Epidemiol 2018; 187 (8): 1799–807. [DOI] [PubMed] [Google Scholar]
- 21. Simon TD, Haaland W, Hawley K, Lambka K, Mangione-Smith R.. Development and validation of the pediatric medical complexity algorithm (PMCA) version 3.0. Acad Pediatr 2018; 18 (5): 577–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rassen JA, Shelat AA, Myers J, Glynn RJ, Rothman KJ, Schneeweiss S.. One-to-many propensity score matching in cohort studies. Pharmacoepidemiol Drug Saf 2012; 21(Suppl 2): 69–80. [DOI] [PubMed] [Google Scholar]
- 23. Sun YX, Wang M, Yang MF, Zhan SY. [Review on tree-based scan statistic in drug and vaccine safety monitoring]. Zhonghua Liu Xing Bing Xue Za Zhi 2021; 42 (7): 1286–91. [DOI] [PubMed] [Google Scholar]
- 24. Templeton AR, Maxwell T, Posada D, Stengård JH, Boerwinkle E, Sing CF.. Tree scanning: a method for using haplotype trees in phenotype/genotype association studies. Genetics 2005; 169 (1): 441–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kulldorff M. TreeScan User Guide, v2.0. 2020. [Google Scholar]
- 26. CDC. ICD-10-CM tabular list of diseases and injuries. 2022. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/Publications/ICD10CM/2022/icd10cm-tabular-2022-April-1.pdf. Accessed August 1, 2022.
- 27. Crook H, Raza S, Nowell J, Young M, Edison P.. Long covid-mechanisms, risk factors, and management. BMJ 2021; 374: n1648. [DOI] [PubMed] [Google Scholar]
- 28. Rando HM, Bennett TD, Byrd JB, et al. Challenges in defining long COVID: striking differences across literature, electronic health records, and patient-reported information. medRxiv. 2021. doi: 10.1101/2021.03.20.21253896. [DOI]
- 29. Estiri H, Strasser ZH, Brat GA, Semenov YR, Patel CJ, et al. ; Consortium for Characterization of C-bEHR. Evolving phenotypes of non-hospitalized patients that indicate long COVID. BMC Med 2021; 19 (1): 249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Asadi-Pooya AA, Nemati H, Shahisavandi M, et al. Long COVID in children and adolescents. World J Pediatr 2021; 17 (5): 495–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Osmanov IM, Spiridonova E, Bobkova P, et al. Risk factors for post-COVID-19 condition in previously hospitalised children using the ISARIC Global follow-up protocol: a prospective cohort study. Eur Respir J 2022; 59 (2): 2101341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Radtke T, Ulyte A, Puhan MA, Kriemler S.. Long-term symptoms after SARS-CoV-2 infection in children and adolescents. JAMA 2021; 326 (9): 869–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Borch L, Holm M, Knudsen M, Ellermann-Eriksen S, Hagstroem S.. Long COVID symptoms and duration in SARS-CoV-2 positive children—a nationwide cohort study. Eur J Pediatr 2022; 181 (4): 1597–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Molteni E, Sudre CH, Canas LS, et al. Illness duration and symptom profile in symptomatic UK school-aged children tested for SARS-CoV-2. Lancet Child Adolesc Health 2021; 5 (10): 708–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Erol N, Alpinar A, Erol C, Sari E, Alkan K.. Intriguing new faces of Covid-19: persisting clinical symptoms and cardiac effects in children. Cardiol Young 2022; 32 (7): 1085–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lopez-Leon S, Wegman-Ostrosky T, Ayuzo Del Valle NC, et al. Long-COVID in children and adolescents: a systematic review and meta-analyses. Sci Rep 2022; 12 (1): 9950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Barrett CK, Koyama AK, Alvarez P, et al. Risk for newly diagnosed diabetes >30 days after SARS-CoV-2 infection among persons aged <18 years—United States, March 1, 2020–June 28, 2021. MMWR Morb Mortal Wkly Rep 2022; 71 (2): 59–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Naendrup JH, Garcia Borrega J, Eichenauer DA, Shimabukuro-Vornhagen A, Kochanek M, Böll B.. Reactivation of EBV and CMV in severe COVID-19-epiphenomena or trigger of hyperinflammation in need of treatment? A large case series of critically ill patients. J Intensive Care Med 2022; 37 (9): 1152–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dotan A, Muller S, Kanduc D, David P, Halpert G, Shoenfeld Y.. The SARS-CoV-2 as an instrumental trigger of autoimmunity. Autoimmun Rev 2021; 20 (4): 102792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Goodwin Davies AJ, Xiao R, Razzaghi H, et al. Skeletal outcomes in children and young adults with glomerular disease. J Am Soc Nephrol 2022; 33 (12): 2233–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Cooper C, Dennison EM, Leufkens HG, Bishop N, van Staa TP.. Epidemiology of childhood fractures in Britain: a study using the general practice research database. J Bone Miner Res 2004; 19 (12): 1976–81. [DOI] [PubMed] [Google Scholar]
- 42. Forrest CB, Burrows EK, Mejias A, et al. Severity of acute COVID-19 in children <18 years old March 2020 to December 2021. Pediatrics 2022; 149 (4): e2021055765. [DOI] [PubMed] [Google Scholar]
- 43. Simon TD, Cawthon ML, Stanford S, et al. ; Center of Excellence on Quality of Care Measures for Children with Complex Needs (COE4CCN) Medical Complexity Working Group. Pediatric medical complexity algorithm: a new method to stratify children by medical complexity. Pediatrics 2014; 133 (6): e1647–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The results reported here are based on detailed individual-level patient data compiled as part of the RECOVER Program. Due to the high risk of reidentification based on the number of unique patterns in the date, patient privacy regulations prohibit us from releasing the data publicly. The data are maintained in a secure enclave, with access managed by the program coordinating center to remain compliant with regulatory and program requirements. Please direct requests to access the data, either for reproduction of the work reported here or for other purposes, to recover@chop.edu.