Abstract
Introduction
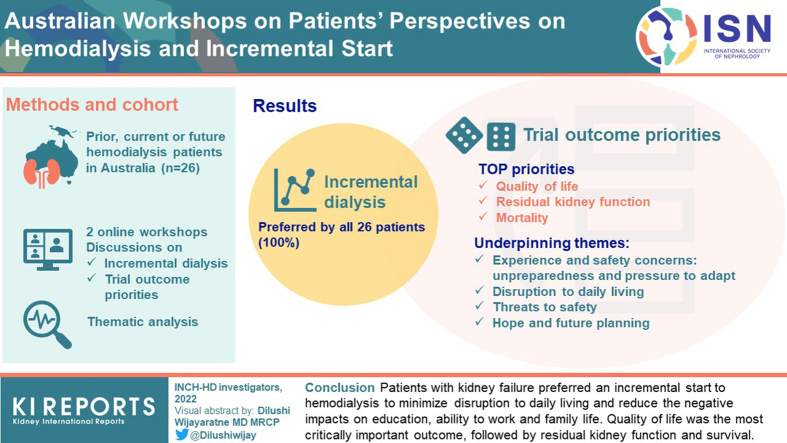
Most patients with kidney failure commence and continue hemodialysis (HD) thrice weekly. Incremental initiation (defined as HD less than thrice weekly) is increasingly considered to be safe and less burdensome, but little is known about patients’ perspectives. We aimed to describe patients’ priorities and concerns regarding incremental HD.
Methods
Patients currently, previously, or soon to be receiving HD in Australia participated in two 90-minute online workshops to discuss views about HD focusing on incremental start and priorities for trial outcomes. Transcripts were analyzed using thematic analysis. Outcomes were ranked on the basis of the sum of participants’ priority scores (i.e., single allocation of 3 points for most important, 2 for second, and 1 for third most important outcome).
Results
All 26 participants (1 caregiver and 25 patients) preferred an incremental HD approach. The top prioritized outcomes were quality of life (QOL) (56 points), residual kidney function (RKF) (27 points), and mortality (16 points). The following 4 themes underpinning outcome priorities, experience, and safety concerns were identified: (i) unpreparedness and pressure to adapt, (ii) disruption to daily living, (iii) threats to safety, and (iv) hope and future planning.
Conclusion
Patients with kidney failure preferred an incremental start to HD to minimize disruption to daily living and reduce the negative impacts on their education, ability to work, and family life. QOL was the most critically important outcome, followed by RKF and survival.
Keywords: hemodialysis, incremental dialysis, patient-centered care, patient perspectives, quality of life, residual kidney function
Graphical abstract
Chronic kidney disease is a global health issue with an estimated global prevalence of 13.4% (95% confidence interval: 11.7–15.1). A systematic review found that most of these cases were in stage 3 chronic kidney disease.1 HD is the most common treatment for kidney failure and is typically initiated and continued thrice weekly at fixed times. However, many patients starting HD have sufficient RKF to safely initiate HD at a lower frequency with a gradual increase in dose and frequency as their RKF decreases. The Global Kidney Health Atlas Project summarized data from 118 countries and showed that 100% offered HD, 80% offered peritoneal dialysis (PD), and 79% offered kidney transplantation to treat people with kidney failure.2 In Australia, all 3 kidney replacement therapy modality options are offered, 83% of all dialysis patients receive HD, and 3% of HD patients start HD twice weekly.3,4 Whilst high-income countries perform twice-weekly HD in <5% of patients; dosing varies internationally with up to 26% of Chinese patients and 75% of Thai patients dialyzing twice-weekly.5,6 Observational studies suggest that an incremental start to HD (defined as less than thrice-weekly HD) may offer therapeutic advantages over thrice-weekly HD including better preservation of RKF and reduced risks of mortality, cardiovascular events, and vascular access complications.7, 8, 9, 10, 11 However, these findings are limited by inherent selection bias and have not been replicated in 2 small pilot randomized controlled trials (RCTs).12, 13, 14, 15, 16
Patients undergoing HD have a high symptom burden and report their QOL to be <60% of QOL in full health because of reduced physical function, loss of role, increased physical pain, and impaired emotional and mental wellbeing.17 There is growing interest in whether an incremental start to HD might allow patients greater ability to cope and participate in life while providing safe and effective HD.4 The literature on QOL in patients starting incremental HD is sparse and limited by selection bias, residual confounding, inadequate sample size, and inconsistency.15,18 Although 1 observational cohort study reported better patient satisfaction with health-related QOL on incremental HD,18 other studies did not show any clear difference in QOL outcomes compared with conventional HD.6,15
Incremental HD requires an individualized approach with adjustment of HD dose as RKF diminishes to prevent medical complications such as uremia, hyperkalemia, and fluid overload. Patient involvement in the design and conduct of an incremental HD trial will ensure that outcomes of interest to patients are adequately addressed, that the trial is conducted in a safe and patient-centered manner and that participant recruitment and retention are optimized.19,20
Methods
Consumer Workshops
We conducted 2 national online workshops for patients currently, previously, or soon to be receiving HD and caregivers in Australia on September 24 and 25, 2020. The aim of the workshops were to establish patients’ and caregivers’ perspectives, priorities, and safety concerns regarding incremental HD. The workshops also informed the design and conduct of an RCT entitled INCremental dialysis to improve Health outcomes in people initiating hemodialysis (INCH-HD) that compares twice weekly (incremental) HD to 3 times weekly (conventional) HD (NCT04932148). INCH-HD is an investigator-initiated, multinational RCT led by an international group of HD experts including HD nurses and nephrologists, clinical trialists, statisticians, and patients coordinated through the Australasian Kidney Trials Network. The patient workshops received ethics approval from The University of Sydney (2020/567).
Participants
The workshops were advertized using a standardized invitation flyer (Supplementary Figure S1) through consumer networks, social media, and professional societies/organizations (Australian and New Zealand Society of Nephrology, Kidney Health Australia, Better Evidence and Translation for Chronic Kidney Disease, and the Standardized Outcomes in Nephrology [SONG] database). Participants registered their email on the Better Evidence and Translation for Chronic Kidney Disease website to receive an email invitation with a unique link to an online consent form and a survey for participant characteristics. The workshop was attended by 25 patients and 1 caregiver from 2 states in Australia (Queensland and New South Wales). An additional 5 patients registered for the workshop but were unable to attend. These 5 patients provided feedback after the workshop to add their perspectives to this report. The characteristics of all participants and contributors are shown in Table 1. The full list of INCH-HD workshop participants, facilitators, cofacilitators and contributors is provided in the Appendix section.
Table 1.
Participant characteristics (N = 31)
| Characteristics | n | % |
|---|---|---|
| Participant role | ||
| Patients | 30 | 96 |
| Family/Caregivers | 1 | 4 |
| Sex | ||
| Male | 12 | 39 |
| Female | 19 | 61 |
| Age group (yr) | ||
| 18–30 | 2 | 7 |
| 31–40 | 7 | 23 |
| 41–50 | 10 | 31 |
| 51–60 | 4 | 13 |
| 61–70 | 6 | 19 |
| >70 | 2 | 7 |
| Median age in yr (Range) | 24 (20–73) | |
| Highest level of education | ||
| Primary school (< yr 10 level) | 0 | 0 |
| School certificate (yr 10 level) | 2 | 7 |
| High school certificate (yr 12 level) | 3 | 10 |
| Technical and further education | 12 | 39 |
| University (Bachelor degree or higher) | 14 | 44 |
| Employment | ||
| Full time | 9 | 30 |
| Part time or casual | 5 | 16 |
| Unemployed | 7 | 23 |
| Retired | 10 | 31 |
| Current kidney replacement therapy | ||
| Nondialysis chronic kidney disease | 5 | 16 |
| Peritoneal dialysis | 1 | 5 |
| Hemodialysis | 15 | 48 |
| Kidney transplant | 10 | 31 |
| Previous kidney replacement therapy (if differs from current therapy) |
||
| Peritoneal dialysis | 6 | 19 |
| Hemodialysis | 7 | 23 |
| Kidney transplant | 4 | 13 |
Workshop Program and Materials
The workshop program and facilitators’ guide are included in Supplementary Figure S2. The 90-minute online workshops were hosted via the Zoom platform. Background materials (Supplementary Figure S3) were sent to all registered participants before the workshop. The workshop started with a presentation summarizing the current literature on incremental dialysis and a preliminary INCH-HD trial proposal. Participants were then allocated to 5 facilitated breakout discussion groups. Each group had 1 trained facilitator (AKV, AJ, or NSR) and 1 cofacilitator (MW, DR, KHe, JC, or JIS). Each facilitator used a standard run sheet to guide the breakout discussion. The questions were developed based on a literature review on incremental dialysis and discussion among the multidisciplinary investigator team. The breakout discussions addressed 3 objectives:
-
1.
To explore the participants’ experiences and challenges with starting HD in general, and the perceived risks and benefits of starting HD incrementally.
-
2.
To identify, prioritize, and discuss potential outcomes for a trial of incremental HD. Participants were provided with a list of proposed outcomes identified through review of the literature21 and discussions among the multidisciplinary investigator team. They were also invited to suggest additional outcomes of interest. Each participant was asked to rank the top 3 outcomes of interest by allocating 3 points to the most important outcome, 2 points to the second most important outcome, and 1 point to the third most important outcome. They were also encouraged to explain their reasons for prioritization. Participants were also asked to review proposed “trigger criteria” that should prompt an increase in HD frequency from twice to thrice weekly treatments and to propose additional triggers.
-
3.
To identify potential facilitators and barriers to patient study recruitment and retention.
The workshop concluded with a plenary session where a spokesperson from each breakout group provided a summary of the discussion.
Data Collection and Analysis
The workshop discussions were audiotaped and transcribed verbatim. The transcripts were entered into Hyper RESEARCH (ResearchWare Inc., United States; Version 4.5.2.) to facilitate coding and analysis of the data. KHe, AJ, and AV read the transcripts line-by-line, and inductively identified and coded concepts into themes reflecting stakeholder perspectives. Themes were presented and discussed among the facilitators and investigators to ensure the range and depth of discussions was captured. All participants and contributors received a draft workshop report and were asked to provide feedback. Additional comments were integrated into the final report.
Consumer Authorship and Involvement
Third author NS-R has lived experience of both dialysis and kidney transplantation. NS-R participated in the workshops as a consumer and contributed to the manuscript.
Results
Rankings of Outcomes
The top 3 outcome priorities to be addressed in the INCH-HD trial as ranked by the participants were QOL (56 points), RKF (27 points) and mortality (16 points). Table 2 shows all outcomes and priority scores established during the workshop and Table 3 highlights the top priority outcomes.
Table 2.
Prioritized list of outcomes for a trial in incremental hemodialysis
| Outcomes | Group A1 (n = 7) | Group A2 (n = 5) | Group B1 (n = 4) | Group B2 (n = 5) | Group B3 (n = 4) | Total Score |
|---|---|---|---|---|---|---|
| Quality of life | 12 | 11 | 9 | 13 | 11 | 56 |
| Residual kidney function | 16 | 3 | 8 | - | - | 27 |
| Mortality | 2 | 2 | 1 | 8 | 3 | 16 |
| Fluid overload | - | 5.5a | 1 | 4 | 2 | 12.5a |
| Ability to work | - | 7 | 3 | - | - | 10 |
| Vascular access function | 6 | - | - | - | 2 | 8 |
| Symptom burden | 2 | 3 | - | - | 3 | 8 |
| Hospitalizations (or avoidance thereof) | 2 | - | - | 3 | - | 5 |
| Major CVE | - | 2 | - | - | 1 | 3 |
| Nutritional status | - | 0.5a | 2 | - | - | 2.5a |
| High potassium | - | - | - | 2 | - | 2 |
| Impact on familyb | - | - | - | - | 2 | 2 |
| Suitability for kidney transplantationb | 1 | - | - | - | - | 1 |
| Duration of incremental HDb | 1 | - | - | - | - | 1 |
| Complete loss of urine output | - | - | - | - | - | 0 |
| Health care-related costs | - | - | - | - | - | 0 |
| Impact on fertilityb | - | - | - | - | - | 0 |
CVE, cardiovascular events; HD, hemodialysis.
Points calculated by adding individual participants’ outcome priority scores: most important outcome = 3 points, second = 2 points and third = 1 point.
Two participants had no third outcomes hence 2 scoring points missing from final table.
Two participants preferred to split their single point across 2 items resulting in half point allocations.
New outcomes identified.
Table 3.
First outcome priority selected by participants for a trial in incremental hemodialysis
| Outcomes | Group A1 (n = 7) | Group A2 (n = 5) | Group B1 (n = 4) | Group B2 (n = 5) | Group B3 (n = 4) |
|---|---|---|---|---|---|
| Quality of life | 4 | 3 | 4 | 3 | 3 |
| Residual kidney function | 3 | 1 | - | - | - |
| Mortality | - | - | - | 2 | 1 |
| Fluid overload | - | 1 | - | - | - |
Workshop Discussions
Four themes were identified from the discussion: unpreparedness, shock, and pressure to adapt; disruption to daily living; threats to safety; and hope and future planning. The themes and respective subthemes are described below, and illustrative participant quotations are presented in Table 4.
Unpreparedness, Shock, and Pressure to Adapt
The Great Unknown
Patients with HD experience described dialysis initiation as being, “thrown in the deep end.” They felt the effectiveness of communication with patients varied among clinicians and many did not feel adequately prepared. “When you first start… you don’t know what to expect and the doctors don’t really explain to you what’s going to happen. They just basically say, ‘come in at this time and you’re going to start dialysis.’” Some turned to online forums and social media groups to ask questions of other patients as they were “learning a new way of life” (Table 4).
Table 4.
Illustrative quotations for themes identified in the workshop discussions
| Unpreparedness, shock, and pressure to adapt | |
|---|---|
| The great unknown | It was just very, very overwhelming because we hadn’t had any time to prepare. It was just, “Here you go. You’re starting dialysis tomorrow”–patient (W2B3) When you first start, if it’s your first time ever, you don’t know what to expect and the doctors don’t really explain to you what’s going to happen. They just basically say, “Oh, come in at this time, and you’re going to start dialysis.” If you’ve never experienced it… you don’t know what to expect”–patient (W2B1) People felt thrown in the deep end, and a lack of education or schooling of what was going to happen. A lack of information–patient (W2B1) |
| The thing that I found hardest about dialysis was not so much the physical stuff… but the notion of what’s going to happen to me, who’s going to do it, how’s it going to work. I got quite anxious–patient (W1B2) | |
| Shocked by the harsh reality | Dialysis is my hardest thing–patient (W1B1) Dialysis itself as a treatment is a tiring one–patient (W1B1) … [the] burden of being on dialysis 3 times a wk and spending the next day recovering–patient (W1B2) I found it exhausting…I know I was benefiting, but I didn’t feel it–patient (W2B2) Yeah, I find my only really good day is Monday–patient (W2B3) The dialysis machine started and my blood pressure fell through the floor–patient (W2B2) |
| …realizing that without those machines you’re going to die–patient (W1B2) | |
| No choice and no control | It was just so much pressure. Learning a new way of life, learning new restrictions on your life. Losing that control over your life. What you can do. It sort of strips you as a person, as well–patient (W1B2) |
| Everything fits around my dialysis–patient (W1B1) What you can and can’t eat and what you can and can’t do–patient (W1B2) Yep, you don’t have much of a choice–patient (W2B3) It was a big toll on my family as well, because I am the only child. My dad worked full time, my mum worked full time. She had to go and get a job [at] night… because we weren’t given a choice of what time you can come into dialysis, you were just given that time–patient (W2B1) |
|
| They start moving you to and from different centers, and different times. You might do a morning 1 day, then an afternoon, then a twilight. And you can’t get into a proper routine doing that–patient (W2B1) You’re expected, by the doctors, to drop everything–patient (W2B1) |
|
| Disruption to daily living | |
|---|---|
| Loss of lifestyle and livelihood | I’m quite active myself, and have lots of other hobbies that I don’t want to give up on or stopping that way. I want to be able to do everything that I do now–patient (W1B1) I had to quit my job because I wasn’t able to work 2 days and work wasn’t able to take me on for those 2 days–patient (W2B2) I didn’t fully understand how this redefined my whole life–patient (W1B2) If I could do it 2 times a week, that’d be great. I work full-time and that’s my biggest concern in starting dialysis. Will I have time to work?–patient (W1B1) I ended up leaving school, because I just found it too hard to do school and to do dialysis–patient (W2B1) I’ve had to retire from work, I’ve had to stop doing some stuff, lifestyle wise–patient (W2B2) |
| Time stolen by dialysis days | .. you’ll miss out on things because the only days off that other people would have are your dialysis days. You’ve got to work your social life around dialysis–patient (W2B3) .. 85% of the time, if I’m not at the renal unit here or at home, I’m in hospital getting checked up and seen–patient (W2B2) We had so many appointments. If we weren’t at the hospital dialyzing, we were at appointments the other 2 days because Mum does it Monday, Wednesday, Friday. The other Tuesday and Thursday, we were at appointments. We had absolutely no days free. It was just really exhausting, so only doing it 2 days, I think would have given us an extra day to just do our thing…–caregiver (W2B3) |
| Struggling to protect quality of life | Mortality, I’m not worried about that. I’ve been dealing with this for too long to worry about it, but it’s what I live with daily that I’m more concerned about–patient (W2B3) Quality of life is very important to me. In fact, I don’t think I’d go on dialysis again if I had to–patient (W2B2) In terms of quality of life, my hemodialysis most certainly has eaten into that big time. It would be wonderful to only have 2 days a week of hemo and therefore have 3 days during the week when you’ve got more life to consider as being quality.–patient (W1B2) I think 99% of the people would choose the 2 days a week knowing the fact that having an extra day of dialysis would take away from their living, from their quality of life.–patient (W2B2) But day by day, quality of life is very low because I have to go to in-center.–patient (W1B1) It’s very difficult to maintain a good quality of life with your 2 days off per week–patient (W1B2) If you don’t have quality of life, you really don’t have anything–patient (W2B1) |
| Threats to safety | |
|---|---|
| Fear of life-threatening complications and concern for treatment adequacy | I’ve heard this saying before, that when you have that 2 days break on the weekend, whether it’s Saturday, Sunday, or Monday, it’s called "the death break"–patient (W2B1) And then the mortality. Well, with kidney failure, that’s one of the major things that you always think about. Like all the, “It’s not good for your heart. It’s not good for this. It’s not good for that. The fluid overload as well.” There’s so many things–patient (W2B1) If you have a high potassium, that can cause the pressure on the heart, fluid overload can put pressure on the heart so that comes back to the mortality–patient (W2B2) |
| Worried about vascular access complications The trauma of hemodialysis |
There were a few of us who had issues around vascular access and we thought the less amount of times people have to access fistulas was good–patient (W1B1) Are they going to hit it today or not? How many times is it going to take? Am I going to have 2, 4, or 6 attempts today?” If you have a blow or all the other things that go along with it, it just can be a little bit of a pain, literally–patient (W2B3) Number one was looking after your fistula, that was my concern. For it to be needled correctly, and to be looked after, and not be infiltrated, which has happened–patient (W2B1) I think the most traumatic thing for me was it happened really suddenly and getting the catheter put in, it was very painful and it was just a horrible experience–patient (W2B2) One of the key things I was worried about was infection because the thought of being needled, 2 needles in your arm 2–3 times a week and just maintaining that and not having issues with an infection–patient (W2B3) There was a time when the dressings popped when I was driving and blood went everywhere–patient (W1B2) The thing I think is the biggest risk here, for me anyways, what I’ve seen [from] a lot of research around kidney disease and kidney health is a lack of acknowledgment of the psychological concerns–patient (W1B2) I went through a massive grief process when my transplant failed–patient (W2B1) I think one thing that hasn’t been mentioned... is the emotional and psychological issues that you obviously have when starting dialysis–patient (W2B2) …a lot of anxiety and stress. It can bring on a lot of depression if you concentrate on it too much–patient (W2B1) We’ve lost 3 of our people; and particularly our last person who passed away, that hit us very, very hard–patient (W1B2) …that grieving process again, of, “Oh, no, I’m...” And the depression would set in, of, “Now, this is... How long now do I have to... How much longer is this going to go on?”– patient (W2B1) [Incremental HD] It would make it not so daunting and help people ease into it so they’re not thinking, “Oh, this is going to take up this many days in my life,” and mentally help them prepare for it, if they ease into it–patient (W2B3) |
| Hope and future planning | |
|---|---|
| Preserving kidney function for overall wellbeing | But the rationale behind the incremental dialysis in India is, no matter what stage you are in, they always start on 2 times a week to prevent or to protect the residual kidney function. Because I never lost my residual kidney function but I was still producing urine, half a liter a day even after or closer to my transplant–patient (W1B1) …residual kidney function and just with the capabilities of having less dialysis so I can fit in work and the activities, and symptoms–patient (W1B1) But if you can approach it more gently with less sessions and that is sufficient for you, then that preserves kidney function. That prevents complications coming in the future so I think that’s quite important–patient (W1B1) If you’re extending the life of your kidney for as long as possible, then that’s going to affect how well-nourished you are, and how ready you are feeling to participate in life events–patient (W2B1) I think incremental dialysis plays a crucial role in preserving the residual kidney function–patient (W1B1) |
| Being part of the family | And for me, pregnancy, and fertility. I’m 30, don’t have children, want to have children and how my kidney function will affect that in the future and all that is really important–patient (W1B1) When you’ve got people who are reliant on you…you want to let them know that things are going to be okay, for a least a little while–patient (W2B3) She comes into my room at 6 o’clock in the morning on the days I’m not doing hemodialysis. So that’s why it’s a bit of a priority because when I’m off dialysis, she wants to go on a bike ride and go to the beach–patient (W1B1) I had to go to Perth for a funeral for my mother-in-law, and the closest dialysis center they could get me in was 60 kms away from my dad's place and obviously the travel... I hired a car so I had to do dialysis and I had to travel back–patient (W2B2) I still have a little bit of anxiety thinking about that, what does the future hold for my son and I… I think that the incremental dialysis for a new patient, I think it’d be very beneficial for anyone starting–patient (W1B2) I missed a whole season of my son’s basketball because I was dialyzing on a Friday night when his games were. I’d finish just as his games were over. I missed an entire season–patient (W2B3) |
Shocked by the Harsh Reality
Patients felt shocked by the “harshness” of HD and felt that an incremental start may have improved their ability to adjust physically and mentally. For some, blood pressure issues with treatment made them feel unwell without warning: “The dialysis machine started and my blood pressure fell through the floor.” Many commented on how treatments felt “exhausting,” and that symptoms persisted to the point that they would need to “spend the next day recovering” (Table 4).
No Choice and No Control
Workshop participants believed the demanding, uncompromising nature of dialysis treatment undermined their sense of control. They felt a lack of control from the HD schedule to daily restrictions on what they were able to eat and drink, “it was just so much pressure… Losing that control over your life [and] what you can do.” They experienced a sudden change in flexibility: “you’re expected, by the doctors, to drop everything.” The dialysis schedule dominated work and life for the entire family, “It was a big toll on my family as well...My mum had to go and get a job [at] night… because we weren’t given a choice of what time you can come into dialysis; you were just given that time” (Table 4).
Disruption to Daily Living
Loss of Lifestyle and Livelihood
Patients grieved the loss of lifestyle when commencing HD, “[I] have lots of other hobbies that I don’t want to give up on. I want to be able to do everything that I do now.” Other patients faced loss of education or employment: “I ended up leaving school…I just found it too hard to do school and do dialysis,” and “I had to quit my job because I wasn’t able to work 2 days and work wasn’t able to [accommodate].” Workshop participants acknowledged financial concerns with loss of income and travel costs. Incremental HD was favored for its potential to allow patients to keep working or maintain their lifestyle, “If I could do it 2 times a week, that’d be great. I work full time and that’s my biggest concern in starting dialysis” (Table 4).
Time Stolen by Dialysis Days
Dialysis-free days allowed patients time for recovery or self-care, and days on dialysis robbed them of social interactions and personal space: “If we weren’t at the hospital dialyzing, we were at appointments ... We had absolutely no days free.” Another patient noted “you’ll miss out on things because the only days off that other people would have are your dialysis days.” Patients agreed that an increased number of dialysis-free days with incremental initiation of HD was appealing and would increase time away from dialysis to be spent instead with family and friends or in recovery mode (Table 4).
Struggling to Protect QOL
Patients gave highest priority to QOL as an outcome of interest. QOL was even ranked above death because, “Mortality, I’m not worried about that...it’s what I live with daily that I’m more concerned about.” One patient summarized the sentiments of the group: “If you don’t have quality of life, you really don’t have anything.” Patients felt the standard HD schedule reduced their QOL and were confident that others on HD would also favor incremental HD, “I think 99% …would choose the 2 days a week knowing…that having an extra day of dialysis would take away from their living, from their quality of life” (Table 4).
Threats to Safety
Fear of Life-Threatening Complications and Concern for Treatment Adequacy
Patients feared the unknown threats to safety in HD initiation: “We actually don’t get a lot of the negative stuff given to us around the safety. Until you start delving [for more information] you do not actually realize how dangerous it is.” Patients were concerned about inadequate treatment leading to biochemical abnormalities and potentially life-threatening fluid-related complications: “When you have that 2 days break on the weekend…it’s called the 'death break'.” Patients were in favor of incremental HD but were clear that they expected careful safety monitoring with any reduced frequency treatment: “I know some patients who do [less dialysis] and their… potassium’s high…it’s not good for the heart.” Participants suggested that individual concerns that dialysis was not adequate should be a safety trigger to review HD frequency. Patients supported regular 24-hour urine volume collection to monitor RKF if it would inform safety assessment and individualized care while on twice weekly HD (Tables 4 and 5).
Table 5.
Workshop-led changes made to the INCH-HD trial design
|
|
|
|
|
|
|
INCH, INCremental dialysis to improve Health; HD, hemodialysis.
Worried About Vascular Access Complications
Patients reported that vascular access complications compounded the stress and anxiety of commencing HD: “Are they going to hit it today or not? How many times is it going to take? Am I going to have 2, 4, or 6 attempts today?” Others had central line-related pain and trauma: “It happened really suddenly and getting the catheter put in…was very painful, and it was just a horrible experience.” In discussion, participants hypothesized that incremental HD initiation might reduce access complications owing to less frequent use of a new fistula (Table 4).
The Emotional Trauma of HD
Patients commented on the significant “emotional and psychological issues that you obviously have when starting dialysis.” Patients felt the mental health impact was underestimated, not adequately addressed, and subsequently relived when returning to HD after transplantation: “I went through a massive grief process when my transplant failed.” Some felt that an incremental HD start could ease some of the psychological strain: “It would make it not so daunting and help people ease into it.” The group acknowledged that patients on twice weekly HD might have difficulty transitioning to thrice weekly HD and would require proactive communication and support from the health care team (Table 4).
Hope and Future Planning
Preserving Kidney Function for Overall Wellbeing
Patients prioritized preservation of RKF against other outcome measures when evaluating incremental initiation of dialysis. Patients felt that incremental HD “plays a crucial role in preserving residual kidney function.” They felt optimized urine output could improve safety and lead to an increased sense of wellness, support, and QOL. “If you're extending the life of your kidney for as long as possible, then that's going to affect how well-nourished you are, and how ready you are feeling to participate in life events” (Table 4).
Being Part of the Family
Many participants wanted to engage more fully with family and were frustrated by the barriers presented by standard HD. Standard HD made being available to their family during daytime activities or special events more difficult: “I missed a whole season of my son's basketball because I was dialyzing on a Friday night when his games were.” Finally, there was a general concern for the future and how each patient’s kidney failure and intensive thrice-weekly treatment could impact loved ones: “When you've got people who are reliant on you…you want to let them know that things are going to be okay for a least a little while” (Table 4).
Discussion
Workshop participants favored an incremental approach to HD to minimize disruption to daily living and reduce the negative impacts on their education, ability to work, and family life. Patients felt they were inadequately prepared for the sudden transition and experienced loss of control over their lives when commencing HD. They emphasized the underappreciated toll HD initiation had on their emotional and psychological health. An incremental start to HD could ease the transition and was viewed as less traumatic for physical, social, and mental health. For these reasons, participants considered QOL the most critically important outcome to be addressed in a clinical trial. They did not propose a strict definition for QOL but framed the discussion in terms of improved life participation and a greater sense of wellbeing (see illustrative quotations in Table 4). Preservation of RKF was viewed as the second most important outcome because it was felt to better support general wellbeing and safety. Patients were concerned about serious complications associated with HD and considered mortality to be the third most important outcome. They emphasized the need for close safety monitoring of patients undergoing incremental HD to ensure prompt escalation of dialysis frequency to prevent life-threatening complications such as hyperkalemia and fluid overload. They also suggested adding a safety trigger to increase HD frequency on the basis of patients’ own concerns in addition to biochemical and clinical triggers.
Outcome priorities identified for inclusion before the workshops were informed by the outcome priorities established through the global Standardized Outcomes Nephrology-Hemodialysis initiative. The Standardized Outcomes Nephrology-Hemodialysis core outcomes were fatigue; vascular access complications; mortality and cardiovascular disease; and other critically important outcomes included impact on family/friends, dialysis-free time, ability to work, and drop in blood pressure.21, 22, 23 Incremental HD may be a promising strategy to address these outcomes and warrants further study in adequately powered RCTs.
Patients with kidney failure have previously described feeling unprepared for and overwhelmed by the transition to HD.24,25 The life-changing impact and the sense of loss of lifestyle, control, freedom, and family have also been highlighted.26 In this workshop, participants were hopeful that incremental HD could reduce the challenge of maintaining QOL by minimizing the time spent on HD and ease the abrupt transition to HD by starting with a twice weekly schedule. The reduced HD frequency could allow people on HD to retain employment or create space for educational, exercise, social, or family commitments.
Currently, there is insufficient evidence to suggest a QOL advantage with an incremental HD approach. Vilar et al.15 conducted a randomized controlled feasibility trial with 55 patients initiating incremental HD versus standard initiation of HD including QOL as a secondary outcome measure. They found no significant difference in QOL between groups at baseline, at 6 months, and at 12 months, but the trial was not powered for this outcome. Observational studies examining QOL in incremental HD are limited6,18 and a systematic review and meta-analyses comparing incremental to standard-dose dialysis has not addressed QOL as an outcome.12 However, better preservation of RKF has been shown to improve health-related-quality-of-life in the HD population,27 and an incremental approach may support greater RKF. Broader consumer involvement in trial design to enrich key outcomes of interest will further improve HD treatment. In this study, patients prioritized QOL as an outcome of interest and therefore adequately powered RCTs examining QOL in incremental HD should be conducted to better inform patient-centered-care.
Workshop participants ranked preservation of RKF as the second most important outcome of interest when considering a trial of initiation of HD. Previous work has demonstrated accelerated loss of RKF and urine output with standard initiation of HD when compared to PD or incremental HD.8,15,28 Systematic reviews by Liu et al.,12 Garofalo et al.,14 and multiple observational trials have suggested that incremental HD better preserves RKF.7,10,12,29, 30, 31 Two small pilot RCTs of incremental HD did not show a significant difference in RKF between incremental and thrice-weekly HD, although they were not sufficiently powered to address this issue.15,16 With regard to other dialysis modalities, incremental initiation of PD is felt to better preserve RKF.14,32 The purported reduction in RKF decline with incremental dialysis modalities may relate to a reduction in repeated hemodynamic stress and ischemic insults causing less end organ injury8,15; however, there remains uncertainty because of the inherent risk of bias and residual confounding of observational data.33
Demonstrating safety with incremental HD is a key concern for both clinicians and patients. Patients wanted to be reassured that trial participants randomized to incremental HD would be regularly assessed to ensure individuals received a safe and adequate dose of HD. They were concerned that incremental HD could increase the risk of complications associated with inadequate HD such as fluid overload, hyperkalemia, and cardiac events. In the discussion on safety monitoring, there was clear patient support for regular urine volume monitoring to assess RKF. Patients also acknowledged the potential for psychological or emotional challenges when considering transition from twice-weekly to thrice-weekly HD. Previous work has suggested that the mortality risk of incremental HD is comparable to that of standard HD,15,16,34 except in highly comorbid patients or those with very minimal RKF.8,35 One cohort study found that incremental HD was associated with improved survival when compared to thrice-weekly HD (HR = 0.49, 95% confidence interval 0.26–0.93, P = 0.29).36 Concern for worse outcomes in patients with insufficient RKF informed the INCH-HD RCT to exclude this group from incremental HD treatment.
Our study has several strengths, including the broad representation of patient experiences across different stages of kidney disease and HD experiences (84% prior or current HD/PD and 16% not yet experienced HD/PD), 61% female and 39% male participants, and varied education and employment status. However, there were important limitations. This study was small and conducted in a single high-income country with English-speaking participants, such that the participants’ views may not align with those of other consumer populations in the international community. In addition, 44% of participants were university-educated and capable of participating in an online meeting which may have led to selection bias. This group appeared younger than the general HD population with 93% of participants <70 years old and a median age of 24 years old. Selected outcomes varied between the groups, likely reflecting the small numbers and different experiences of members in each group. These factors limit transferability and generalizability of findings. An important limitation was that only one participant had lived experience with incremental HD. However, this is consistent with the low prevalence (3%) of incremental HD in Australia.4
This report adds novel insights into how patients view and experience dialysis initiation and how they would design a clinical trial comparing incremental to conventional HD initiation. Previous research has highlighted that consumer engagement in research improves the quality and relevance of research19,20 and that patient involvement in planning for research has been lacking.37 Findings from this workshop have informed the design of the INCH-HD trial, a multinational RCT comparing incremental initiation of HD with full dose initiation of HD. Consumer feedback from these workshops was directly incorporated into the trial design, including taking QOL in place of RKF as the primary outcome; the addition of a patient-identified concern trigger criterion for increasing HD frequency, which could be raised at any time during treatment or review; patient endorsement of planned trial procedures such as frequent 24-hour urine collection to assess urine output and RKF; recording out-of-pocket HD-related expenses (e.g. taxis, food purchased away from home) to assess financial burden; recording employment status to assess ability to work; addition of a life participation measure; and consumer support for routine assessment of the psychological impact of HD as part of the trial procedure (see Table 5).
Conclusion
Incremental HD offers a patient-centered, individualized approach to dialysis initiation with potential to improve important patient priorities including dialysis-free time, ability to work, and participation in social and family life. Patients favored incremental HD and advocated for QOL as the most critically important outcome for clinical trials in incremental HD, followed by RKF, and mortality. These workshops have informed the design of INCH-HD, a multinational, multicenter RCT which will assess the safety, efficacy (especially with respect to QOL), and cost-effectiveness of incremental versus conventional HD commencement.
Disclosure
DWJ has received consultancy fees, research grants, speaker’s honoraria, and travel sponsorships from Baxter Healthcare and Fresenius Medical Care, consultancy fees from Astra Zeneca, Bayer, and AWAK, speaker’s honoraria from ONO and BI and Lilly, and travel sponsorships from ONO and Amgen. JIS has received consultancy fees from Outset Medical and Dialco Medical. AKV receives grant support from a Jacquot Research Establishment Fellowship, a Queensland Advancing Clinical Research Fellowship and an National Health and Medical Research Council Emerging Leader Grant (1196033). DWJ is a current recipient of an Australian National Health and Medical Research Council Leadership Investigator Grant. JIS receives grant support from the CIHR. The remaining authors have no relevant conflicts of interest to disclose.
Acknowledgments
Funding
This project is supported by a National Health and Medical Research Council (NHMRC) program grant (1092597).
Author Contributions
Research idea and study design was by AKV, MH, KHe, AJ, and NSR; data acquisition was done by AKV, AJ, AB, KHe, DR, JS, MW, and NSR; data analysis/interpretation was performed by KHe, AKV, and AJ; supervision or mentorship was done by AKV, AJ, MH, DW, and CH. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved. KHe prepared the first draft of the manuscript. All other authors contributed to redrafting and approved the final version.
Footnotes
Supplementary FigureS1. Patient invitation to participate in workshops.
Supplementary FigureS2. Workshop program and run sheet.
Supplementary Figure S3. Patient perspectives and involvement in co-design of a trial of incremental hemodialysis.
Appendix
List of the INCH-HD Trial Investigators
Workshop Investigators
Workshop participants who gave permission to be listed as investigators and facilitators/cofacilitators:
| Name | Role |
|---|---|
| Adam Martin | Patient Partner |
| Allison Jaure | Facilitator |
| Amanda Baumgart | Co-Facilitator |
| Andrea K Viecelli | Facilitator |
| Annette Davey | Patient Partner |
| Annie Lionnet | Patient Partner |
| Anthony Tobia | Patient Partner |
| Brendan Foley | Patient Partner |
| Cheryl Harrington | Patient Partner |
| Cheryl Palmer | Patient Partner |
| Danny Kupa | Patient Partner |
| Deb Batty | Patient Partner |
| Donna Reidlinger | Co-Facilitator |
| Frederick Feige | Patient Partner |
| Leyesha Roberts | Patient Partner |
| Jane Morrey | Patient Partner |
| Janelle Watson | Patient Partner |
| Jenny Shen | Co-Facilitator |
| Jim Walsh | Patient Partner |
| Jo Cottrell | Patient Partner |
| Jonna MacFadyen | Patient Partner |
| Karlee Wall | Caregiver |
| Katharine Hegerty | Co-Facilitator |
| Katherine Widders | Patient Partner |
| Kimberley Gardner | Patient Partner |
| Laura Heffernan | Patient Partner |
| Lina Yaghoubpour | Patient Partner |
| Lisa Richardson | Patient Partner |
| Martin Wolley | Co-facilitator |
| Melissa Kiely | Patient Partner |
| Nicole Scholes-Robertson | Facilitator |
| Paul Cruice | Patient Partner |
| Peter Murko | Patient Partner |
| Phillip Carswell | Patient Partner |
| Shelley Dawns | Patient Partner |
| Shyam Muthuramalingam | Patient Partner |
| Tamara Clements | Patient Partner |
| Vincent Houlihan | Patient Partner |
INCH-HD Trial Principal Investigators
| Name | Affiliation |
|---|---|
| Professor Peter Kerr | Monash Medical Center and Monash University |
| Professor David W Johnson | Queensland Health and The University of Queensland |
| Assoc Prof Matthew Roberts | Eastern Health Clinical School and Monash University |
| Dr Martin Wolley | Queensland Health and The University of Queensland |
| Assoc Prof Andrea K Viecelli | Queensland Health and The University of Queensland |
| Prof Kirsten Howard | University of Sydney |
| Prof Allison Jaure | University of Sydney |
| Prof Stephen McDonald | South Australian Health and Medical Research Institute Ltd |
| Prof Robert Walker | University of Otago, New Zealand |
| Prof Charmaine Lok | University Health Network, Canada |
INCH-HD Trial Associate Investigators
| Name | Affiliation |
|---|---|
| Prof Carmel Hawley | The University of Queensland |
| Dr Brendan Smyth | NHMRC Clinical Trials Center, University of Sydney |
| Assoc Prof Nigel Toussaint | Melbourne Health |
| Dr Ginger Chu | John Hunter Hospital |
| Dr Nicole Scholes-Robertson | University of Sydney |
| Prof Carol Pollock | University of Sydney |
| Dr Shyam Muthuramalingam | South Australian Health and Medical Research Institute Ltd |
| Dr Doris Chan | Western Australia Health |
| Assoc Prof Rathika Krishnasamy | The University of Queensland |
| Mrs Veronica Oliver | Princess Alexandra Hospital, Queensland Health |
| Assoc. Prof David Mudge | Redlands Hospital, Queensland Health |
| Dr Ken-Soon Tan | Logan Hospital, Queensland Health |
| Mrs Sharon Cottingham | Redlands Hospital, Queensland Health |
| Dr Janak de Zoysa | University of Auckland |
| Assoc Prof Emma Wyeth | University of Otago |
| Dr Luke Wilson | University of Otago |
Supplementary Materials
Supplementary FigureS1. Patient invitation to participate in workshops.
Supplementary FigureS2. Workshop program and run sheet.
Supplementary Figure S3. Patient perspectives and involvement in co-design of a trial of incremental hemodialysis.
References
- 1.Hill N.R., Fatoba S.T., Oke J.L., et al. Global prevalence of chronic kidney disease-a systematic review and meta-analysis. PLoS One. 2016;11 doi: 10.1371/journal.pone.0158765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Htay H., Alrukhaimi M., Ashuntantang G.E., et al. Global access of patients with kidney disease to health technologies and medications: findings from the Global Kidney Health Atlas project. Kidney Int Suppl (2011) 2018;8:64–73. doi: 10.1016/j.kisu.2017.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.ANZDATA Registry (44th Report). Chapter 2: prevalence of kidney failure with replacement therapy. Published 2021. Accessed October 21, 2022. https://www.anzdata.org.au/wp-content/uploads/2021/09/c02_prevalence_2020_ar_2021_chapter_v1.0_20211112_Final.pdf
- 4.Wolley M.J., Hawley C.M., Johnson D.W., et al. Incremental and twice weekly haemodialysis in Australia and New Zealand. Nephrol (Carlton) 2019;24:1172–1178. doi: 10.1111/nep.13556. [DOI] [PubMed] [Google Scholar]
- 5.Panaput T., Thinkhamrop B., Domrongkitchaiporn S., et al. Dialysis dose and risk factors for death among ESRD patients treated with twice-weekly hemodialysis: a prospective cohort study. Blood Purif. 2014;38:253–262. doi: 10.1159/000368885. [DOI] [PubMed] [Google Scholar]
- 6.Bieber B., Qian J., Anand S., et al. Two-times weekly hemodialysis in China: frequency, associated patient and treatment characteristics and Quality of Life in the China Dialysis Outcomes and Practice Patterns study. Nephrol Dial Transplant. 2014;29:1770–1777. doi: 10.1093/ndt/gft472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vilar E., Wellsted D., Chandna S.M., et al. Residual renal function improves outcome in incremental haemodialysis despite reduced dialysis dose. Nephrol Dial Transplant. 2009;24:2502–2510. doi: 10.1093/ndt/gfp071. [DOI] [PubMed] [Google Scholar]
- 8.Obi Y., Streja E., Rhee C.M., et al. Incremental hemodialysis, residual kidney function, and mortality risk in incident dialysis patients: a cohort study. Am J Kidney Dis. 2016;68:256–265. doi: 10.1053/j.ajkd.2016.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaja Kamal R.M., Farrington K., Busby A.D., et al. Initiating haemodialysis twice-weekly as part of an incremental programme may protect residual kidney function. Nephrol Dial Transplant. 2019;34:1017–1025. doi: 10.1093/ndt/gfy321. [DOI] [PubMed] [Google Scholar]
- 10.Wong J., Vilar E., Davenport A., Farrington K. Incremental haemodialysis. Nephrol Dial Transplant. 2015;30:1639–1648. doi: 10.1093/ndt/gfv231. [DOI] [PubMed] [Google Scholar]
- 11.Murea M., Moossavi S., Garneata L., Kalantar-Zadeh K. Narrative review of incremental hemodialysis. Kidney Int Rep. 2020;5:135–148. doi: 10.1016/j.ekir.2019.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu Y., Zou W., Wu J., et al. Comparison between incremental and thrice-weekly haemodialysis: systematic review and meta-analysis. Nephrol (Carlton) 2019;24:438–444. doi: 10.1111/nep.13252. [DOI] [PubMed] [Google Scholar]
- 13.Hanson J.A., Hulbert-Shearon T.E., Ojo A.O., et al. Prescription of twice-weekly hemodialysis in the USA. Am J Nephrol. 1999;19:625–633. doi: 10.1159/000013533. [DOI] [PubMed] [Google Scholar]
- 14.Garofalo C., Borrelli S., De Stefano T., et al. Incremental dialysis in ESRD: systematic review and meta-analysis. J Nephrol. 2019;32:823–836. doi: 10.1007/s40620-018-00577-9. [DOI] [PubMed] [Google Scholar]
- 15.Vilar E., Kaja Kamal R.M., Fotheringham J., et al. A multicenter feasibility randomized controlled trial to assess the impact of incremental versus conventional initiation of hemodialysis on residual kidney function. Kidney Int. 2022;101:615–625. doi: 10.1016/j.kint.2021.07.025. [DOI] [PubMed] [Google Scholar]
- 16.Murea M., Patel A., Highland B.R., et al. Twice-weekly hemodialysis with adjuvant pharmacotherapy and transition to thrice-weekly hemodialysis: a pilot study. Am J Kidney Dis. 2022;80:227–240.e1. doi: 10.1053/j.ajkd.2021.12.001. [DOI] [PubMed] [Google Scholar]
- 17.Merkus M.P., Jager K.J., Dekker F.W., et al. Quality of life in patients on chronic dialysis: self-assessment 3 months after the start of treatment. The Necosad study group. Am J Kidney Dis. 1997;29:584–592. doi: 10.1016/s0272-6386(97)90342-5. [DOI] [PubMed] [Google Scholar]
- 18.Park J.I., Park J.T., Kim Y.L., et al. Comparison of outcomes between the incremental and thrice-weekly initiation of hemodialysis: a propensity-matched study of a prospective cohort in Korea. Nephrol Dial Transplant. 2017;32:355–363. doi: 10.1093/ndt/gfw332. [DOI] [PubMed] [Google Scholar]
- 19.Chalmers I., Bracken M.B., Djulbegovic B., et al. How to increase value and reduce waste when research priorities are set. Lancet. 2014;383:156–165. doi: 10.1016/S0140-6736(13)62229-1. [DOI] [PubMed] [Google Scholar]
- 20.Mea J., Manns B., Laupacis A., et al. Assessing the extent to which current clinical research is consistent with patient priorities: a scoping review using a case study in patients on or nearing dialysis. Can J Kidney Health Dis. 2015;2:35. doi: 10.1186/s40697-015-0070-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tong A., Manns B., Hemmelgarn B., et al. Establishing core outcome domains in hemodialysis: report of the standardized outcomes in nephrology-hemodialysis (SONG-HD) consensus workshop. Am J Kidney Dis. 2017;69:97–107. doi: 10.1053/j.ajkd.2016.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Evangelidis N., Tong A., Manns B., et al. Developing a set of core outcomes for trials in hemodialysis: an international Delphi survey. Am J Kidney Dis. 2017;70:464–475. doi: 10.1053/j.ajkd.2016.11.029. [DOI] [PubMed] [Google Scholar]
- 23.Urquhart-Secord R., Craig J.C., Hemmelgarn B., et al. Patient and caregiver priorities for outcomes in hemodialysis: an international nominal group technique study. Am J Kidney Dis. 2016;68:444–454. doi: 10.1053/j.ajkd.2016.02.037. [DOI] [PubMed] [Google Scholar]
- 24.Song M.K., Lin F.C., Gilet C.A., et al. Patient perspectives on informed decision-making surrounding dialysis initiation. Nephrol Dial Transplant. 2013;28:2815–2823. doi: 10.1093/ndt/gft238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walker R.C., Howard K., Morton R.L., et al. Patient and caregiver values, beliefs and experiences when considering home dialysis as a treatment option: a semi-structured interview study. Nephrol Dial Transplant. 2015;31:133–141. doi: 10.1093/ndt/gfv330. [DOI] [PubMed] [Google Scholar]
- 26.Montalescot L., Rascle N., Combe C., Untas A. Patients’ experience one year after dialysis initiation: a lexicometric analysis. Health Psychol Behav Med. 2021;9:380–397. doi: 10.1080/21642850.2021.1918552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elgendy A., Abdelsalam A.I., Mansour M., Nassar M.K. Can residual kidney function affect quality of life and cognitive function in hemodialysis patients? BMC Nephrol. 2022;23:263. doi: 10.1186/s12882-022-02892-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Teruel-Briones J.L., Fernández-Lucas M., Rivera-Gorrin M., et al. Progression of residual renal function with an increase in dialysis: haemodialysis versus peritoneal dialysis. Nefrologia. 2013;33:640–649. doi: 10.3265/Nefrologia.pre2013.May.12038. [DOI] [PubMed] [Google Scholar]
- 29.Kalantar-Zadeh K., Unruh M., Zager P.G., et al. Twice-weekly and incremental hemodialysis treatment for initiation of kidney replacement therapy. Am J Kidney Dis. 2014;64:181–186. doi: 10.1053/j.ajkd.2014.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang M., Wang M., Li H., et al. Association of initial twice-weekly hemodialysis treatment with preservation of residual kidney function in ESRD patients. Am J Nephrol. 2014;40:140–150. doi: 10.1159/000365819. [DOI] [PubMed] [Google Scholar]
- 31.Lin Y.F., Huang J.W., Wu M.S., et al. Comparison of residual renal function in patients undergoing twice-weekly versus three-times-weekly haemodialysis. Nephrology (Carlton) 2009;14:59–64. doi: 10.1111/j.1440-1797.2008.01016.x. [DOI] [PubMed] [Google Scholar]
- 32.Blake P.G., Dong J., Davies S.J. Incremental peritoneal dialysis. Perit Dial Int. 2020;40:320–326. doi: 10.1177/0896860819895362. [DOI] [PubMed] [Google Scholar]
- 33.Basile C., Casino F.G., EUDIAL Working Group of ERA-EDTA Incremental haemodialysis and residual kidney function: more and more observations but no trials. Nephrol Dial Transplant. 2019;34:1806–1811. doi: 10.1093/ndt/gfz035. [DOI] [PubMed] [Google Scholar]
- 34.Torreggiani M., Fois A., Chatrenet A., et al. Incremental and personalized hemodialysis start: a new standard of care. Kidney Int Rep. 2022;7:1049–1061. doi: 10.1016/j.ekir.2022.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mathew A., Obi Y., Rhee C.M., et al. Treatment frequency and mortality among incident hemodialysis patients in the United States comparing incremental with standard and more frequent dialysis. Kidney Int. 2016;90:1071–1079. doi: 10.1016/j.kint.2016.05.028. [DOI] [PubMed] [Google Scholar]
- 36.Jaques DA, Ponte B, Haidar F, et al. Outcomes of incident patients treated with incremental haemodialysis as compared to standard haemodialysis and peritoneal dialysis. Nephrol Dial Transplant. 10.1093/ndt/gfac205 [DOI] [PMC free article] [PubMed]
- 37.Tong A., Chando S., Crowe S., et al. Research priority setting in kidney disease: a systematic review. Am J Kidney Dis. 2015;65:674–683. doi: 10.1053/j.ajkd.2014.11.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.