Highlights
-
•
Head and neck cancer radiotherapy lacks predictive tools due to its heterogeneity.
-
•
Deep learning models can successfully integrate clinical data and radiomics.
-
•
They promise to predict different outcomes to guide individualized decision.
-
•
Understanding, validating, expanding them is critical for clinical implementation.
Abbreviations: ADASYN, adaptive synthetic sampling; AI, artificial intelligence; ANN, artificial neural network; AUC, Area Under the ROC Curve; BMI, body mass index; CART, Classification and Regression Tree; CBCT, cone-beam computed tomography; C-Index, concordance index; CIFE, conditional informax feature extraction; CNN, convolutional neural network; CRT, chemoradiation; CT, computed tomography; DL, deep learning; DT, Decision Tree; DM, distant metastasis; DSC, Dice Similarity Coefficient; DSS, clinical decision support systems; DVH, Dose-volume histogram; GANs, Generative Adversarial Networks; GB, Gradient boosting; GPU, graphical process units; HNC, head and neck cancer; HPV, human papillomavirus; HR, hazard ratio; IAMB, incremental association Markov blanket; IBDM, image based data mining; IBMs, image biomarkers; IMRT, intensity-modulated RT; KNN, k nearest neighbor; LLR, Local linear forest; LR, logistic regression; LRR, loco-regional recurrence; ML, machine learning; MIFS, mutual information based feature selection; NPC, nasopharynx; MRMR, Minimum redundancy feature selection; MRI, Magnetic resonance imaging; N-MLTR, Neural Multi-Task Logistic Regression; NTCP, Normal Tissue Complication Probability; OPC, oropharyngeal cancer; ORN, osteoradionecrosis; OS, overall survival; PCA, Principal component analysis; PET, Positron emission tomography; PG, parotid glands; PLR, Positive likelihood ratio; PM, pharyngeal mucosa; PTV, Planning target volumes; PreSANet, deep preprocessor module and self-attention; QUANTEC, Quantitative Analyses of Normal Tissue Effects in the Clinic; RF, random forest; RFC, random forest classifier; RFS, recurrence free survival; RLR, Rigid logistic regression; RSF, random survival forest; RT, radiotherapy; RTLI, radiation-induced temporal lobe injury; RRF, Regularized random forest; SDM, shared decision making; SMG, submandibular glands; SMOTE, synthetic minority over-sampling technique; STIC, sticky saliva; SVC, support vector classifier; SVM, support vector machine; XGBoost, extreme gradient boosting
Keywords: Head and neck cancer, Artificial intelligence, Machine learning, Radiomic, Predictive modeling, Cancer outcomes
Abstract
Head and neck radiotherapy induces important toxicity, and its efficacy and tolerance vary widely across patients. Advancements in radiotherapy delivery techniques, along with the increased quality and frequency of image guidance, offer a unique opportunity to individualize radiotherapy based on imaging biomarkers, with the aim of improving radiation efficacy while reducing its toxicity. Various artificial intelligence models integrating clinical data and radiomics have shown encouraging results for toxicity and cancer control outcomes prediction in head and neck cancer radiotherapy. Clinical implementation of these models could lead to individualized risk-based therapeutic decision making, but the reliability of the current studies is limited. Understanding, validating and expanding these models to larger multi-institutional data sets and testing them in the context of clinical trials is needed to ensure safe clinical implementation. This review summarizes the current state of the art of machine learning models for prediction of head and neck cancer radiotherapy outcomes.
Introduction
Global approximate incidence of head and neck cancer (HNC) is 880 000 patients each year worldwide [1]. As a core therapeutic option, radiotherapy (RT) is being used in 75 % of cases, combined with other treatment modalities such as chemotherapy or surgery [2]. Current HNC RT is associated with high rates of toxicity as well as adverse impacts on patients’ quality of life [3]. HNC encompasses a heterogeneous group of cancers originating from various subsites that are associated with various risk factors including viral infections [4], tobacco and alcohol use [5]. In addition to known heterogeneity, RT efficacy and tolerance also vary across apparently similar patients presenting with the same cancer subtype, anatomical stage and apparent risk factors [6]. Patient-specific clinical, radiological and biological factors are thought to drive these individual cancer outcomes. To date, HPV-positive status is known to be a favorable predictor of response to treatment in oropharyngeal cancer and have led to the concept of de-escalation treatments, but which can not be used outside of clinical trials as studies have been inconclusive [18]. Currently, there are no other biomarkers used to guide decisions in HNC RT.
Over the last decades, the refinement of RT techniques, along with the parallel developments in image guidance for better delineation and tumor localization over the course of treatment [7], [8], have been associated with an increasing interest for individualized RT with the aim of increasing or maintaining tumor control and reducing radiation toxicity [7]. Machine learning (ML) consists in the analysis of large amounts of empirical data using computational algorithms and leading to automatic extraction of discriminative features and learning of complex patterns [9], [10]. Developments in artificial intelligence (AI), particularly ML and deep learning (DL), have led to significant enthusiasm for the concept of “rapid learning health system”, whereby decision-making would be individualized based on analysis of large patient cohorts [11]. AI offers a unique opportunity for the development of predictive models that can help stratify individual patient’s risk and guide therapeutic decisions for optimal patients’ outcomes and quality of life in HNC RT. Herein, we review the current stance of the role of AI in predicting toxicity and therapeutic outcomes in HNC patients treated with RT.
Radiation oncology and artificial intelligence
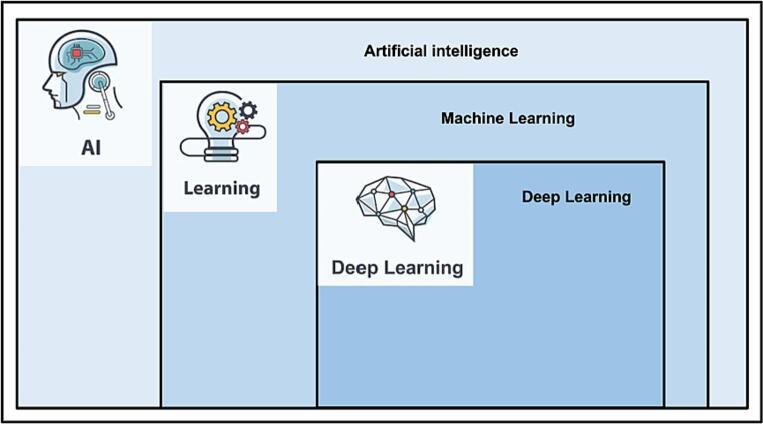
The term “Artificial intelligence” first appeared at the Dartmouth Scientific Conference in 1956 [12]. ML is a subfield of AI that uses an algorithm to find patterns within data. DL is a subcategory of ML based on the use of neural networks and representation learning (Fig. 1).
Fig. 1.
Various levels of Artificial intelligence, including machine learning and deep learning.
Since the success of computer vision based analysis due to the increase in access to graphical process units (GPU), the field of medical image analysis has seen rapid benefits from ML approaches, which contributed in advancing the fast growing field of adaptive RT. With the increasing digitization and standardization of image acquisition and storage processes, the primary drawback of ML methods - the large training data requirements - continues to diminish. More specifically, recent studies focused on opportunities to use big data as decision support by predicting tumor response and toxicity outcomes [19], [20]. ML-based risk stratification could support decisions such as RT or systemic therapy intensification (or de-intensification), or even guide prophylactic measures in prevention of expected toxicity.
Radiomics (Fig. 2) is a research field which consists in the extraction of a large number of quantitative, hand-crafted features from different medical images (CT; MRI; PET-CT) - that cannot be manually deciphered by clinicians [21], and which will be then integrated to data-characterization algorithms [22]. Although pathology can be gold standard, it is not feasible to biopsy every node or every area of the tumor and radiomics offers the promise of characterizing different areas of the cancer [23]. Radiomics offer a particular potential in HNC RT as an immense volume of different imaging modalities are gathered routinely. Most HNC patients begin with initial diagnostic and staging images including diagnostic and/or planning computed tomography (CT) and magnetic resonance imaging (MRI). Positron emission tomography (PET) is also frequently part of routine diagnostic (or planning) imaging in HNC [24], [25]. During RT, daily CBCT (cone-beam computed tomography) serves for patient positioning further contributing to the quantity of available anatomic imaging [26]. More recently, the MR-Linac, which is available in an increasing number of institutions, has allowed for daily online MRI, therefore further improving image guidance [27]. After RT completion, follow-up typically includes CT, MRI or PET, based on different factors and guidelines [28].
Fig. 2.
Schematic illustration of radiomic pipeline.
Classification models are used to cluster data into different groups by approximating a mapping from a different set of inputs to discrete a set of outputs, has been mainly used as a predictive ML algorithm for HNC. The main algorithms are logistic regression (LR), decision tree, random forest (RF), support vector machine (SVM), k nearest neighbor (KNN), naives Bayes and artificial neural network. These traditional models have allowed better understanding of medical images, but with the major disadvantage of the time consuming step involving extracting and selecting important image features [35]. To address this issue, convolution neural network (CNN), a DL model that automatically learns, extracts and selects important features have shown promise in imaging classification tasks [36]. For any AI models, including classifiers, overfitting is a common problem when an algorithm is too focused on the training data set that it can not be successfully applied to a new data set. In order to verify if the model is not overfitting, a k-fold cross validation could be done by randomly partitioning a data set into k mutually exclusive subsets. Different metrics can be used in order to evaluate a model’s performance. These include sensitivity, specificity, accuracy, precision and recall. Another measurement could be done with the Area Under the ROC Curve (AUC) ranging from 0 to 1 (0 for a model’s predictive performance is 100 % wrong and 1, as its performance is 100 % correct). The calculation of the concordance index (C-index) could also be measured for predictive performance, on a scale between zero and one with 0.5 indicating no prognostic value.
Table 1.
Summary list of potential use of AI algorithms in different steps in HNC RT.
| Steps | Clinical Use | Algorithms |
|---|---|---|
| 1) Diagnosis/Initial evaluation | Clinical/Pathological/radiological data processing | SVM, LR, RF, DT, KNN, Bayesian, Linear Discriminant Analysis, DL and combination of ML and DL |
| 2) Treatment Decision Making | Treatment Decision Aid | DSS, SDM |
| Outcome Prediction | SVM, LR, Bayesian, neural network, decision trees and combination | |
| Toxicities Prediction | Bayes, LR, KNN, SVM, SVC, RF, XGBoost PLR, RFC, IBDM, CART, CNN | |
| 3) Simulation | Synthetic Imaging Generation | Fuzzy c-means clustering, CNNs and GANs |
| 4) Treatment Planning | Auto-segmentation | DSC, CNN dd-Resnet |
| Dosimetric Optimization | Unet, DenseNet, GANs | |
| 5) Treatment delivery | Image Guidance and Motion Management | CNN, Bayesian, SVM, |
| CBCT quality improvement | CNN |
Abbreviations: CBCT, cone-beam computed tomography; CNN, convolutional neural network; CART, Classification and Regression Tree; DL, deep learning; DT, Decision Tree; DSC, Dice Similarity Coefficient; DSS, clinical decision support systems; KNN, k nearest neighbor; LR, logistic regression;ML, machine learning; GANs, Generative Adversarial Networks; IBDM, image based data mining; RF, random forest; RFC,random forest classifier; SDM, shared decision making; SVM, support vector machine; SVC, support vector classifier.
Prediction of toxicity
Different Normal Tissue Complication Probability (NTCP) models have been proposed in order to help understand and estimate the risk of different toxicities. The common traditional models are the Lyman-Kutcher-Burnman models based on simplified characterization of the radiation-dose response for each anatomy [37]. For different toxicities, some studies have shown good validation [38]. In clinical practice, radiation oncologists routinely use the Quantitative Analyses of Normal Tissue Effects in the Clinic (QUANTEC) dose–response guidelines to determine tolerance dose to organs at risk [39]. However, the predictive power of currently models is largely limited by the lack of integration of patient-specific risk factors [40], [41] and omission of the inclusion of radiomic features despite studies having shown their relevance [38]. In order to account for these issues and update the current NTCP models, different ML methods have been studied [43]. Table 2 summarizes the current literature on AI predictive models for toxicities.
Table 2.
AI predictive models for toxicities.
| Authors | Endpoints | Number of HNC cohort | Algorithms | Performance | Important features |
|---|---|---|---|---|---|
| Dean et al. (2016) [53] |
Mucositis | 351 | PLR, SVC, RFC | RFC with AUC 0.71 | Volumes of oral cavity receiving intermed - high dose |
| Dijk et al. (2016) [46] | Xerostomia and sticky saliva at 12 months | 249 | LASSO regularisation | AUC 0.77 | IBMs |
| Pota et al. (2017) [95] | PG shrinkage and Xerostomia at 12 months | 37 | fuzzy classification | AUC 0.86 and 0.79 | Final volume PG shrinkage |
| Dean et al. (2017) [49] | Dysphagia | 173 | PLR, SVC, RFC | RFC with AUC 0.71 | PM receiving >1 Gy/fraction |
| Cheng et al. (2017) [52] | WL during RT and EOT | 391 | CART | AUC 0.773 and 0.821 | Dose in OARs, oral intake, N stage, pain, nausea |
| Beasley et al. (2018) [47] | Trismus | 86 | Linear regression | Rs of −0.45 | IBDM clusters in ipsilateral masseter |
| Gabry s et al. (2018) [44] | Xerostomia at different timelines | 153 | 7 classifiers and 6 feature selectors | AUC 0.74–0.88 | Dose gradient in PGs, PG volume, PG eccentricity |
| Jiang et al. (2018) [45] | Xerostomia 3 months post RT | 427 | RLR, LLR, RF | AUC 0.70 | Dose pattern in PG/SMG |
| Reddy et al. (2019) [50] | Hospitalization Feeding tube WL | 2121 | RF, GB, LR | AUC 0.640-0.751 | – |
| Wojcieszynski et al (2019) [51] | Grade > 3 toxicity (90and180days) | 437 | PLR, RF, XGBoost | C-statistic 0.65 and 0.63 | PTV integral dose and integral dose out of PTV |
| Zhang et al. (2020) [54] | RTLI post RT in different timelines | 242 NPC | RF | AUCs 0.830, 0.773 and 0.716 | Features from medial temporal lobe |
| Humbert-Vidan et al. (2022) [55] | ORN | 140 | 3D CNN, DenseNet 21 | AUC 0.71 | Clinical dosimetric distribution |
Abbreviations: AUC, Area Under the ROC Curve; CART, Classification and Regression Tree; GB, Gradient boosting; IBMs, image biomarkers; LLR, Local linear forest; LR, logistic regression; PLR, Positive likelihood ratio; PG, parotid glands; PTV, Planning target volumes; RLR, Rigid logistic regression; RF, random forest; RFC, random forest classifier; SMG, Submandibular glands; SVC, support vector classifier; XGBoost, extreme gradient boosting; 3D, three dimensions.
As xerostomia is known to be a common major early- and long-term toxicity of HNC RT, different studies reported on radiomic features from salivary glands, namely the parotid glands (PGs) or submandibular glands (SMGs). Gabry et al [44] compared the predictive performance of seven classification algorithms, six feature selection methods, and ten data cleaning/class balancing techniques by integrating retrospective dosiomic, radiomic and demographic data from 153 HNC patients treated with definitive RT. Important features such as dosimetric shape and gradients, PG volume and eccentricity, and DVH spread were identified. Their MLs based models performed better compared to the traditional NTCP models based on mean dose to PG only. Jiang et al [45] tested three different algorithms applied to a data set including clinical and radiomic features such as voxels dose in the PGs and SMGs from 427 HNC patients treated with definitive RT. Similar to. Gabry et al, the authors were able to observe that specific dose patterns across the subvolumes in both organs were an important predictive feature and their ridge logistic regression model had the best performance with AUC of 0.70. Dijk et al [46] used the CT based image biomarkers (IBMs) of the PGs and SMGs from 249 HNC patients treated with definitive RT in order to improve the NTCP predictive models for sticky saliva (STIC) and moderate-severe xerostomia 12 months. For both toxicities, pre-selection through a lasso regularization identified different important radiomic features and the predictive performance of NTCP models were stronger when IBMs were added (AUC 0.74 vs 0.77). Beasley et al [47] also used ML applied to the image based data mining (IBDM) in order to identify clusters of dose distribution voxels involved in radiation induced trismus. From clinical and radiomic data set from 86 HNC patients focusing on the dose distributions within the anatomy of interest, different features investigated in a multivariable analysis and an internal/external validation demonstrated the importance of dose patterns within anatomy to predict trismus.
Dysphagia is also a common toxicity among patients treated with RT for HNC causing a major impact in patients’ quality of life [48]. In order to improve the current predictive NTCP model for dysphagia, Dean et al [49] incorporated spatial dose metrics in different ML models with a prospective data set of 173 HNC patients including clinical and dosimetric features focusing on pharyngeal mucosa (PM). Their RFC model with a highest AUC of 0.71 identified that the volume, length and circumference of PM receiving 1 Gy/fraction and higher were strongly associated with the risk of dysphagia. More recently, Reddy et al [50] used a different data set from 2,121 HNC patients in order to compare predictive performance of three different classifiers for unplanned hospitalizations, feeding tube placement and significant weight loss. This method identified over 700 treatment-related and clinical variables, and achieved AUC values of up to 0.64, 0.75, and 0.75 for RF, gradient boosting, and LR, respectively. Wojcieszynski et al [51] compared the predictive performance of three ML methods on a prospective data set of 437 HNC patients treated with definitive chemoradiation (CRT). Their RF model yielded moderate success for toxicity at 90 and 180 days with c-static of 0.65 and 0.63, respectively. From this study, higher integral doses outside of the target volume, target volume integral dose, body mass index (BMI) and age were important factors associated with increased grade 3 + toxicity. Cheng et al [52] used a Classification and Regression Tree model in HNC patients treated with definitive RT by using demographic, dosimetric and clinical data from 391 patients in order to predict weight loss ≥5 kg at 3 months post-RT. Two models were built, one during the RT planning and one at the end of the treatments. When additional treatment-related data was added to each model, the predictive performance was improved, with an AUC of 0.77 and 0.82, respectively.
Several other radiation-induced toxicities have been the focus of individual studies. Mucositis was the focus of a study by Dean et al [53], where clinical, dose-volume and spatial dose metrics data from 317 HNC patients were used to build predictive ML models for severe acute mucositis. Among different models tested, the discriminative performance was not improved with the additional spatial dose metrics. Important features were in the range V80-V220 and the most important feature was the V220. Interestingly, in contrast to the RTOG guidelines focusing on mean dose to the oral cavity, the authors therefore identified that the strongest feature associated with severe acute mucositis was the volume receiving intermediate and high doses. To predict radiation-induced temporal lobe injury, Zhang et al [54] used retrospective clinical and CT and MRI based radiomic data from 242 nasopharynx (NPC) patients treated with definitive RT. Different radiomic features were first extracted from the medial temporal lobe regions. RF predictive model showed strong predictive performance in three subsequent radiological follow-ups preceding the onset of radiation-induced temporal lobe injury with the mean AUCs of between 0.71 and 0.83. More recently, Humbert-Vidan et al [55] used retrospective demographic, clinical and dosimetric data (3D dose distribution map) of 140 HNC patients (70 patients with ORN and 70 patients as control group) in order to compare the predictive performance of a 3D densely-connected 121-layer convolutional neural network (CNN) model with a DVH based RF model. The 3D DenseNet121 CNN model had better performance with an average AUC of 0.71 (0.64–0.79), compared to 0.65 (0.57–0.73) for the RF model.
There was a general trend of increasing feature importance with increasing dose and feature importance was also high for RT dose metrics in the range V80 – V220.
Prediction of cancer control outcomes
Current predictive models for HNC are mainly based on the TNM (Primary tumor, regional lymph nodes and distant metastasis) staging [56], which guides oncologists in the selection of the appropriate therapeutic options for patients. In oropharyngeal cancer (OPC), other prognostic variables established in the context of clinical trials, namely human papillomavirus (HPV) status and tobacco smoking pack-years, have largely been integrated in the clinical practice. While patients with HPV-associated OPC generally have an improved prognosis, we now recognize that a subset of these patients present a highly aggressive behavior [57]. There is therefore a general concern that safe treatment de-escalation should not jeopardize the chance of cure of these patients, and that more reliable tools to predict tumor behavior are greatly needed. In recent years, several predictive AI models to better predict cancer control outcomes in HNC have been published and are presented in Table 3.
Table 3.
Different AI predictive models for outcomes.
| Authors | Patient population | Predicted outcomes | Number of patients | Algorithms | Performance | Important features |
|---|---|---|---|---|---|---|
| Parmar et al. (2015) [63] |
HNC SCC | 3Y OS | 206 | 13 feature selectors and 11 ML classifiers | 3 feature selectors (MRMR, MIFS and CIFE) with AUC 0.66–0.69 3 classifier (RF, NN and BY) with AUC 0.61–0.67 |
CT based radiomic features |
| Jiang et al. (2015) [62] |
NSC | OS | 347 | SVM | HR 3.45 | Combination of CRT |
| Li et al. (2018) [65] |
NSC | LR | 306 | PCA, ANN, KNN SVM |
ANN with accuracy of 0.812 | MRI based radiomic features |
| Zdilar et al. (2018) [64] |
OPC | OS RFC |
529 | MRMR, Wilcoxon, RF, RReliefF, RRF, IAMB, RSF, PCA | RF selectors AUC 0.75 and C-index 0.68 | CT based radiomic features |
| Fujima et al. (2019) [96] |
Sinonasal SCC | LF | 36 | SVM | Accuracy of 0.96 | MRI based radiomic features |
| Wu et al. (2019) [97] |
OPC | DMFS | 140 | RSF | C-index 0.73 | Max distance between nodes and tumor-nodes |
| Zhou et al. (2019) [67] |
NPC | DM | 176 | PyRadiomics features extraction, features selections (Mann-Whitney U test, mRMR, Lasso), LR | AUC 0.827 (training group) and 0.792 (validation group) | MRI based radiomic features |
| Tseng et al. (2020) [58] |
Oral cavity | Survival (Cancer specific and loco-regional recurrence free) | 334 | Elastic Net Penalized Cox Proportional Hazards regression | C index 0.689 and 0.693. Distant metastasis free survival not different |
Genetic data |
| Howard et al. (2020) [59] |
HNC SCC | OS | 33 527 | DeepSurv, RSF N-MTLR |
HR of 0.79, 0.83 and 0.90 | Stage T4, HPV status, tonsil subsite |
| De Felice et al. (2020) [32] |
OPC | OS | 273 | RF - Classification tree | Mean decrease accuracy of 4.29, 2.49 and 1.11 % | HPV status N status Early responders |
| Tran et al. (2020) [68] |
HNC SCC | Local nodal response | 32 | LR, KNN, naive-Bayes | Accuracy 87.5 % with three feature model | Quantitative US radiomic features |
| Tosado et al. (2020) [70] |
OPC | OS, RFS | 644 | RReliefF feature selector, Cox Model, RSF | AUC 0.6395 (OS) and 0.6483 (RFS) | Radiomic features combined with clinical features |
| Bogowicz et al. (2020) [71] |
OPC, hypo pharynx, larynx, oral cavity | 2YOS, HPV | 1174 | Feature selector (LR Z-Rad), Classification (hierarchical clustering, LR) | No significant differences in AUC between centralized and distributed. | 981 radomic features |
| Rich et al. (2021) [69] |
OPC HPV + | DM | 225 | Feature extractor (SMOTE, ADASYN, borderline SMOTE), SVM | AUC 0.84–0.95 | CT based radiomic |
| Le et al. (2022) [72] |
HNC SCC | 10Y DM, Lr, OS | 371 | Cox Model, RF, CNN, DenseNet, InceptionV3, ResNet, ResNeXt and PreSANet | PreSAnet - Accuracy of 74 % (Lr) and 79 % (OS) | Performance decrease with PET images |
Abbreviations: ADASYN, adaptive synthetic sampling; ANN, artificial neural network; BY, Bayesian; CT, Computed tomography; C-index, concordance index; CIFE, conditional informax feature extraction; CRT, chemo-radiotherapyDM, distant metastasis; DMFS, distant metastasis-free survival; HNC, head and neck cancer; HPV, human papillomavirus; HR, Hazard ratio; IAMB, incremental association Markov blanket; KNN, k nearest neighbor; LF, local failure; Lr, locoregional recurrence; LR, logistic regression; LRC, loco-regional control; NPC, nasopharyngeal cancer; MIFS, mutual information based feature selection; MRI, Magnetic resonance imaging; MRMR, Minimum redundancy feature selection; N, node; NN, nearest neighoor; N-MLTR, Neural Multi-Task Logistic Regression; OS, overall survival; PET, positron emission tomography; PCA, Principal component analysis; RF, random forest; RFC, relapse-free survival; RRF, Regularized random forest; RSF, random survival forest; SCC, squamous cell carcinoma; SMOTE, synthetic minority over-sampling technique; SVM, support vector machine; US, Ultrasounds; 2D CNN, two dimensions convolutional neural network; 3D CNN, three dimensions convolutional neural network.
To better stratify survival outcomes, Tseng et al [58] evaluated the elastic net penalized Cox proportional hazards regression-based risk stratification model in operated oral cavity cancers. The authors integrated clinicopathologic and genomic data from 334 patients with locally advanced HNC treated with curative intent surgery, combined with adjuvant RT or CRT. Compared to the baseline model using clinicopathologic data alone, the identification and integration of genetic features associated with prognostic led to a model with better classification performance, with mean C-indexes of 0.689 (vs 0.673) and 0.693 (vs 0.678) for cancer-specific survival and locoregional recurrence-free survival, respectively. Also in the post-operative setting, Howard et al [59] aimed to build an overall survival (OS) predictive model to better identify patients that may benefit from the addition of adjuvant concurrent chemotherapy. The authors evaluated different ML models integrating a large retrospective data from the National Cancer Database, including 33 527 patients with squamous cell carcinoma of the oral cavity, oropharynx, hypopharynx, or larynx treated with definitive surgery followed by an adjuvant RT or CRT. Three different models were trained, then validated using a subset of the same cohort. Compared to RTOG 95–01 and EORTC 22931 recommendations [60], [61], treatments guided by all three models had improved survival outcomes with hazard ratio (HR) of 0.79–0.90 and c index of 0.691–0.695 with similar accuracy and there was no survival benefit for CRT for patients recommended to receive RT alone. These models also identified important variables related to prognosis such as year of diagnosis, T4, HPV positivity and tonsillar subsite.
In order to evaluate the role of radiomics for risk stratification of DM, Rich et al [69] used CT based radiomic and clinical features from 225 locally advanced OPC HPV+ patients treated with curative intent RT or CRT. Nine different algorithms were built using different radiomic datasets derived using different algorithms integrated to SVM classifier. All classifiers achieved at least an excellent level in discriminating the two patient cohorts with DM or not. In order to build a predictive model for OS and RFS outcomes, Tosado et al [70] incorporated retrospective CT based radiomic data with clinical data from 644 OPC patients treated with RT or CRT. Distinctive radiomic and clinical features with the cluster labels were identified and different supervised models were built using these features. Compared to the baseline model based on clinical features only, these models had better predictive performance for both outcomes. In another study by Jiang et al [62], aiming to predict outcomes in metastatic NPC patients treated with chemotherapy alone, RT alone or the combination of both, the retrospective hematological, clinical and therapeutic parameters of 347 patients were used in a SVM model. The multivariate model had a strong performance with an AUC at 0.761 and the classifier was able to stratify the patients into low risk and high risk groups with significantly different 2 year OS of 71.4 % vs 18.8 %, respectively. This classifier also helped identify that combined CRT was associated with significantly better outcomes in the low risk groups, but not in the higher risk groups.
Other studies focused on integrating radiomic data into ML algorithms to optimize predictive models for HNC treatment outcomes. In order to identify the optimal ML methods for radiomic-based overall survival prediction, Parmar et al [63] compared the performance of 13 features selection methods and 11 ML classification methods integrating CT based 440 radiomic features from 196 HNC patients. Three feature selection methods had the best performance with AUC between 0.66 and 0.69 and stability between 0.66 and 0.70 compared to the median values of AUC = 0.61 and stability = 0.66. Three classifying methods had the best performance with AUC between 0.61 and 0.67. Zdilar et al [64] used retrospective CT based radiomic, clinical, demographic, toxicity and cancer control outcome data from 529 OPC patients treated with curative intent RT or CRT to compare the predictive performance of different selectors for OS and RFS. Among 3800 radiomic features extracted, selected features using 8 different methods resulted in better AUC compared to clinical features alone. Among the feature selectors, RF based selectors had the best overall scores. In order to build a model predicting a radioresistance, Li et al [65] used retrospective data from 306 NPC patients treated with definitive CRT. Clinicopathological and radiomic/dosimetric features from planning CT and from follow up imagings including CT, MRI or PET. Once detected, recurrent tumor volumes were delineated, then was categorized as “in field recurrence” if the recurrence was inside the high-dose target. Eight discriminative features were identified from pretreatment MRIs compared between the patients with and without the disease recurrence. Features were fed to three different MLs, which were trained, then validated and yield accuracies ranging between 0.732 and 0.812. These results could indicate possible differences in heterogeneity in LR tumors. For a predictive performance of loco-regional recurrence (LRR), Starke et al [66] used the retrospective data from 291 patients with locally advanced HNC treated with CRT. A baseline Cox proportional hazards model (CPHM) using clinical features alone was compared to different 3D-CNN and 2D-CNN models built from scratch combining clinical features and CT images. Among these, the ensemble of 3D-CNNs had the best performance and successful validation with a C-index of 0.31. Patient risk group defined by this model's predictions showed significant differences in LRR with p = 0.001. The C-index for 2D-CNN and for CPHM was 0.38 and 0.39, respectively. In order to satisfy risks for DM and 5Y OS, Zhou et al [67] used MRI based radiomic with dosiomic and clinical features from 176 NPC patients treated with curative intent RT or CRT. With the radiomic features extracted, an algorithm model was built in order to classify into high- and low risk groups for DM. With the clinical features, the radiomic based models show strong predictive performance for both in the training and validation cohorts with AUC of 0.827 and 0.792 respectively. Another study was done to predict therapeutic response in metastatic lymph nodes by Tran et al [68]. Their team used the quantitative ultrasound based radiomic markers from 32 HNC patients with positive lymph nodes treated with curative intent RT or CRT. Depending on their 3 months follow up MRI, patients were divided into two different categories: complete responders or partial responders. Different radiomic features were extracted, then applied in LR, KNN and a naive-Bayes. Multi Parametric models showed a strong predictive power with high accuracy of 87.5 %. Significant differences in radiomic parameters were found between the two groups.
In order to evaluate the role of radiomics for risk stratification of DM, Rich et al [69] used CT based radiomic and clinical features from 225 locally advanced OPC HPV+ patients treated with curative intent RT or CRT. Nine different algorithms were built using different radiomic datasets derived using different algorithms integrated to SVM classifier. All classifiers achieved at least an excellent level in discriminating the two patient cohorts with DM or not. In order to build a predictive model for OS and RFS outcomes, Tosado et al [70] incorporated retrospective CT based radiomic data with clinical data from 644 OPC patients treated with RT or CRT. Distinctive radiomic and clinical features with the cluster labels were identified and different supervised models were built using these features. Compared to the baseline model based on clinical features only, these models had better predictive performance for both outcomes. In another study by Jiang et al [62], aiming to predict outcomes in metastatic NPC patients treated with chemotherapy alone, RT alone or the combination of both, the retrospective hematological, clinical and therapeutic parameters of 347 patients were used in a SVM model. The multivariate model had a strong performance with an AUC at 0.761 and the classifier was able to stratify the patients into low risk and high risk groups with significantly different 2 year OS of 71.4 % vs 18.8 %, respectively. This classifier also helped identify that combined CRT was associated with significantly better outcomes in the low risk groups, but not in the higher risk groups.
The sufficient quantity of a radomic data set is a common problem for an AI algorithm development and multicenter approach can be a solution but implicating ethical issues. In order to address this issue, Bogowicz et al [71] tested the distributed learning technique enabling training models on multicenter data without data leaving the hospitals. Two different approaches, centralized and distributed, were compared for 2Y OS and HPV status predictive models built with CT based radiomic, dosiomic and clinical features from 1174 HNC patients treated with curative intent RT or CRT. For both feature selection and classification, there was no significant difference in terms of performance between these two approaches. Most recently, Le et al [72] used retrospective cross-institutional patho-clinical and PET-CT based radiomic data set from 298 HNC patients treated with curative intent RT or CRT in order to train a predictive model based on a pseudo-volumetric convolutional neural network with PreSANet. The model was internally validated, then an extensive set of ablation experiments on the public data set showed AUROC of DM, LR and OS between 80 and 82 %. External validation on a retrospective dataset showed an AUROC at 69 % and a validation of single site-holdout and cross-validation showed mean accuracy across four different institutions was between 70 and 72 %.
Discussion
Recent studies have shown promising results in the use of ML in the field of HNC RT in predicting therapeutic outcomes and toxicity. Different algorithms have shown good predictive performance and have helped identify features that provide insight into the heterogeneous nature of HNC. Those features have included demographic characteristics, molecular, dosimetric, radiomic and therapeutic factors. Their integration to the current clinical decision algorithms has the potential to improve risk stratification and selection of optimal therapeutic options.
Despite promising results, these models remain largely premature for clinical use at this stage. One major concern is the lack of standardization of the largely retrospective data used in a single center. In radiomics specifically, for each imaging modality, intra and inter-institutional variations in scanner, acquisition and reconstruction parameters have been shown to impact the robustness of the predictive models [73]. Pertaining to RT data, differences in tumor and organs at risk segmentations as well as dosimetric data further challenges reproducibility [42], [74]. In addition, variations in feature extraction techniques, choice of robustness metrics and outcome definitions used across studies complicate the interpretation of results. The small sample sizes and high heterogeneity of HNC and frequent lack of external validation lead lack of generalizability of the current studies. Increased use of open-access data sets and multicenter prospective cohorts, along with strict guidelines for data standardization would be critical for these models to reach clinical usability [71], [72], [75]. In addition, training clinical oncologists to the field of AI, as well as integrating them early in the development and validation of these models will be increasingly important. As clinicians are ultimately responsible for decision making, ensuring their adequate understanding and interpretation of these models will help overcome the ‘’black box’’ problem and facilitate clinical implementation of these tools [76], [77].
Beside the risk stratification and decision support in HNC RT, AI has substantial potential in other upstream tasks such as automatic detection and segmentation of anatomical structures [13], automatic registration of mono-modal or multimodal images [14], temporal motion compensation [15], tumor and lesion grade classification [16], and nomograms for risk stratification-prognostic modeling [17]. AI can independently be introduced at all stages of a patient’s treatment from diagnosis, to planning and re-planning, to long-term follow-up and prognosis, while allowing or benefiting from expert input along the way.
AI can reveal the radiomic signatures in HNC such as tumor characteristics including HPV status [29] or Programmed Death-Ligand 1 expression [30], identification of extranodal extension [31] as well as cancer control outcomes [32] and larynx/hypopharynx cancers [33]. Radiomics also has the potential to provide a quantitative assessment of tumor and normal tissue reaction to RT over the course of treatment (i.e. delta-radiomics) [34]. The emerging use of multi-omics ((Gen-omics, Epigen-omics, Transcipt-omics, prote-omics, metabol-omics and microbi-omics) [78], [79] in oncology, along with the increasing quantity and quality of imaging in radiation oncology, represent a clear opportunity to propule the role of AI in HNC. The integration of daily imaging used over the course of RT in order to capture dynamically tumor response or early signs of toxicity could guide therapeutic decision or early interventions more efficiently, as suggested in early work using CBCTs data in dynamic predictive algorithms [80], [81]. The increasing availability of the MR-Linac technology across institutions will lead to increased quality and both anatomic and functional information of daily RT imaging and will further increase the potential to unlock dynamic imaging-based biomarkers [82], [83], [84], [85]. Finally, as the field of liquid biopsy if expanding rapidly, non invasive biologic serum or salivary HNC biomarkers [86], [87], [88] could be further integrated to these algorithms to increase the precision of dynamic clinical outcomes predictions over the course of treatment and in post-treatment follow-ups [89], [90], [91], [92], [93], [94].
This review has several limitations. First, its non-systematic review method could cause potential risks of different bias with less transparency. However, this method seemed suitable to offer a general overview of the current stance of AI in HNC RT. Also, our study did not include a recently developed radiomics quality score, a tool built by Lambin et al. in order to determine the validity and completeness of radiomics studies [98]. For a more comprehensive understanding of the subject matter, future reviews could include use of this tool as well as an insight on the ongoing clinical trials evaluating AI and radiomics tools in HNC RT [99], [100], [101].
AI-models predicting cancel control and toxicity outcomes in HNC RT have shown promising performance and would be of high clinical utility for individualized risk-based decision making. These important challenges to the development and safe clinical implementation of these models could only be overcome with coordinated collaborative efforts to standardize, validate and expand these models to large enough datasets and test in the context of clinical trials.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Ferlay J., Sung H., Siegel R.L., et al. Globalcancerstatistics 2020: GLOBOCANestimatesof incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Atun R., et al. Expanding global access to radiotherapy. Lancet Oncol. 2015;16:1153–1186. doi: 10.1016/S1470-2045(15)00222-3. [DOI] [PubMed] [Google Scholar]
- 3.Trotti A. Toxicity in head and neck cancer: a review of trends and issues. Int J Radiat Oncol Biol Phys. 2000;47(1):1–12. doi: 10.1016/s0360-3016(99)00558-1. PMID: 10758302. [DOI] [PubMed] [Google Scholar]
- 4.Fernandes Q., Merhi M., Raza A., Inchakalody V.P., Abdelouahab N., Zar Gul A.R., et al. Role of Epstein-barr virus in the pathogenesis of head and neck cancers and its potential as an immunotherapeutic target. Front Oncol. 2018;6(8):257. doi: 10.3389/fonc.2018.00257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Di Credico G., Polesel J., Dal Maso L., et al. Alcohol drinking and head and neck cancer risk: the joint effect of intensity and duration. Br J Cancer. 2020;123:1456–1463. doi: 10.1038/s41416-020-01031-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caudell J.J., Torres-Roca J.F., Gillies R.J., Enderling H., Kim S., Rishi A., et al. The future of personalised radiotherapy for head and neck cancer. Lancet Oncol. 2017 May;18(5):e266–e273. doi: 10.1016/S1470-2045(17)30252-8. Epub 2017 Apr 26. PMID: 28456586; PMCID: PMC7771279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alterio D., Marvaso G., Ferrari A., Volpe S., Orecchia R., Jereczek-Fossa B.A. Modern radiotherapy for head and neck cancer. Semin Oncol. 2019 Jun;46(3):233–245. doi: 10.1053/j.seminoncol.2019.07.002. Epub 2019 Jul 26 PMID: 31378376. [DOI] [PubMed] [Google Scholar]
- 8.Grégoire V., Langendijk J.A., Nuyts S. Advances in Radiotherapy for Head and Neck Cancer. J Clin Oncol. 2015 Oct 10;33(29):3277–3284. doi: 10.1200/JCO.2015.61.2994. Epub 2015 Sep 8 PMID: 26351354. [DOI] [PubMed] [Google Scholar]
- 9.Giraud P., Giraud P., Gasnier A., et al. Radiomics and machine learning for radiotherapy in head and neck cancers. Front Oncol. 2019;9:174. doi: 10.3389/fonc.2019.00174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parmar C., Grossmann P., Bussink J., et al. Machine learning methods for quantitative radiomic biomarkers. Sci Rep. 2015;5:13087. doi: 10.1038/srep13087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lambin P., Roelofs E., Reymen B., Velazquez E.R., Buijsen J., Zegers C.M., et al. Rapid Learning health care in oncology' - an approach towards decision support systems enabling customised radiotherapy. Radiother Oncol. 2013 Oct;109(1):159–164. doi: 10.1016/j.radonc.2013.07.007. Epub 2013 Aug 28 PMID: 23993399. [DOI] [PubMed] [Google Scholar]
- 12.Moor J. The dartmouth college artificial intelligence conference: the next fifty years. AI Mag. 2006;27(4):87. [Google Scholar]
- 13.Nikolov, S. et al. Deep learning to achieve clinically applicable segmentation of head and neck anatomy for radiotherapy. Preprint at arXiv (2018). [DOI] [PMC free article] [PubMed]
- 14.Fan J, Cao X, Wang Q, Yap PT, Shen D. Adversarial learning for mono- or multi-modal registration. Med Image Anal. 2019 Dec;58:101545. 10.1016/j.media.2019.101545. Epub 2019 Aug 24. PMID: 31557633; PMCID: PMC7455790. [DOI] [PMC free article] [PubMed]
- 15.Shi L., Han S., Zhao J., Kuang Z., Jing W., Cui Y., et al. Respiratory prediction based on multi-scale temporal convolutional network for tracking thoracic tumor movement. Front Oncol. 2022 May;27(12) doi: 10.3389/fonc.2022.884523. PMID: 35692785; PMCID: PMC9184446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reimagining T. Staging through artificial intelligence and machine learning image processing approaches in digital pathology Kaustav Bera, Ian Katz, and Anant Madabhushi. JCO Clin Cancer Inf. 2020;4:1039–1050. doi: 10.1200/CCI.20.00110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Machine Learning and Nomogram Prognostic Modeling for 2-Year Head and Neck Cancer–Specific Survival Using Electronic Health Record Data: A Multisite Study Damian P. Kotevski, Robert I. Smee, Claire M. Vajdic, and Matthew Field JCO Clinical Cancer Informatics 2023:7. [DOI] [PubMed]
- 18.Belgioia L., Morbelli S.D., Corvò R. Prediction of response in head and neck tumor: focus on main hot topics in research. Front Oncol. 2021 Jan;8(10) doi: 10.3389/fonc.2020.604965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Niedzielski J.S., Yang J., Stingo F., Liao Z., Gomez D., Mohan R., et al. A novel methodology using CT imaging biomarkers to quantify radiation sensitivity in the esophagus with application to clinical trials. Sci Rep. 2017;7:6034. doi: 10.1038/s41598-017-05003-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carvalho S., Troost E.G.C., Bons J., Menheere P., Lambin P., Oberije C. Prognostic value of blood-biomarkers related to hypoxia, inflammation, immune response and tumour load in non-small cell lung cancer – a survival model with external validation. Radiother Oncol. 2016;119:487–494. doi: 10.1016/j.radonc.2016.04.024. [DOI] [PubMed] [Google Scholar]
- 21.Gonçalves M., Gsaxner C., Ferreira A., Li J., Puladi B., Kleesiek J., et al. Radiomics in head and neck cancer outcome predictions. Diagnostics. 2022;12:2733. doi: 10.3390/diagnostics12112733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koçak B., Durmaz E.Ş., Ateş E., Kılıçkesmez Ö. Radiomics with artificial intelligence: a practical guide for beginners. Diagn Interv Radiol. 2019 Nov;25(6):485–495. doi: 10.5152/dir.2019.19321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nardone V., Reginelli A., Grassi R., et al. Delta radiomics: a systematic review. Radiol med. 2021;126:1571–1583. doi: 10.1007/s11547-021-01436-7. [DOI] [PubMed] [Google Scholar]
- 24.Newbold K., Powell C. PET/CT in radiotherapy planning for head and neck cancer. Front Oncol. 2012 Dec;10(2):189. doi: 10.3389/fonc.2012.00189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eyassu E, Young M. Nuclear Medicine PET/CT Head and Neck Cancer Assessment, Protocols, And Interpretation. 2022 Nov 28. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 34424632. [PubMed]
- 26.Yan D., Lockman D., Martinez A., Wong J., Brabbins D., Vicini F., et al. Computed tomography guided management of interfractional patient variation. Semin Radiat Oncol. 2005;15:168–179. doi: 10.1016/j.semradonc.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 27.Mutic S., Dempsey J.F. The ViewRay system: magnetic resonance-guided and controlled radiotherapy. Semin Radiat Oncol. 2014;24:196–199. doi: 10.1016/j.semradonc.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 28.Simo R., Homer J., Clarke P., Mackenzie K., Paleri V., Pracy P., et al. Follow-up after treatment for head and neck cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol. 2016 May;130(S2):S208–S211. doi: 10.1017/S0022215116000645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sohn B., Choi Y.S., Ahn S.S., Kim H., Han K., Lee S.K., et al. Machine learning based radiomic HPV phenotyping of oropharyngeal SCC: A feasibility study using MRI. Laryngoscope. 2021 Mar;131(3):E851–E856. doi: 10.1002/lary.28889. Epub 2020 Jul 13 PMID: 33070337. [DOI] [PubMed] [Google Scholar]
- 30.Ren Q., Xiong F., Zhu P., Chang X., Wang G., He N., et al. Assessing the robustness of radiomics/deep learning approach in the identification of efficacy of anti-PD-1 treatment in advanced or metastatic non-small cell lung carcinoma patients. Front Oncol. 2022 Aug;5(12) doi: 10.3389/fonc.2022.952749. PMID: 35992867; PMCID: PMC9390967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kann B.H., Aneja S., Loganadane G.V., Kelly J.R., Smith S.M., Decker R.H., et al. Pretreatment identification of head and neck cancer nodal metastasis and extranodal extension using deep learning neural networks. Sci Rep. 2018;8:14036. doi: 10.1038/s41598-018-32441-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.De Felice F., Humbert-Vidan L., Lei M., King A., Guerrero U.T. Analyzing oropharyngeal cancer survival outcomes: a decision tree approach. Br J Radiol. 2020;93(1111):20190464. doi: 10.1259/bjr.20190464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhong J., Frood R., Brown P., Nelstrop H., Prestwich R., McDermott G., et al. Machine learning-based FDG PET-CT radiomics for outcome prediction in larynx and hypopharynx squamous cell carcinoma. Clin Radiol. 2021 Jan;76(1):78.e9–78.e17. doi: 10.1016/j.crad.2020.08.030. Epub 2020 Oct 6 PMID: 33036778. [DOI] [PubMed] [Google Scholar]
- 34.Fatima K., Dasgupta A., DiCenzo D., Kolios C., Quiaoit K., Saifuddin M., et al. Ultrasound delta-radiomics during radiotherapy to predict recurrence in patients with head and neck squamous cell carcinoma. Clin Transl Radiat Oncol. 2021 Mar;12(28):62–70. doi: 10.1016/j.ctro.2021.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kermany D.S., Goldbaum M., Cai W., Valentim C.C., Liang H., Baxter S.L., et al. Identifying medical diagnoses and treatable diseases by image-based deep learning. Cell. 2018;172(5):1122–1131. doi: 10.1016/j.cell.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 36.Yang R., Yu Y. Artificial convolutional neural network in object detection and semantic segmentation for medical imaging analysis. Front Oncol. 2021 Mar;9(11) doi: 10.3389/fonc.2021.638182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Deist T.M., Dankers F.J., Valdes G., Wijsman R., Hsu I., Oberije C., et al. Erratum: Machine learning algorithms for outcome prediction in (chemo)radiotherapy: An empirical comparison of classifiers. Med Phys. 2019;46:1080–1087. doi: 10.1002/mp.13329. [DOI] [PubMed] [Google Scholar]
- 38.Christianen M.E.M.C., van der Schaaf A., van der Laan H.P., Verdonck-de Leeuw I.M., Doornaert P., Chouvalova O., et al. Swallowing sparing intensity modulated radiotherapy (SW-IMRT) in head and neck cancer: clinical validation according to the model-based approach. Radiother Oncol. 2016;118:298–303. doi: 10.1016/j.radonc.2015.11.009. [DOI] [PubMed] [Google Scholar]
- 39.Houweling A.C., Philippens M.E.P., Dijkema T., Roesink J.M., Terhaard C.H.J., Schilstra C., et al. A comparison of dose-response models for the parotid gland in a large group of head-and-neck cancer patients. Int J Radiat Oncol Biol Phys. 2010;76(4):1259–1265. doi: 10.1016/j.ijrobp.2009.07.1685. [DOI] [PubMed] [Google Scholar]
- 40.Buettner F., Miah A.B., Gulliford S.L., Hall E., Harrington K.J., Webb S., et al. Novel approaches to improve the therapeutic index of head and neck radiotherapy: an analysis of data from the PARSPORT randomised phase III trial. Radiother Oncol. 2012;103(1):82–87. doi: 10.1016/j.radonc.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 41.Marks L.B., Yorke E.D., Jackson A., Ten Haken R.K., Constine L.S., Eisbruch A., et al. Use of normal tissue complication probability models in the clinic. Int J Radiat Oncol Biol Phys. 2010;76:10–19. doi: 10.1016/j.ijrobp.2009.07.1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Christianen M.E., Langendijk J.A., Westerlaan H.E., van de Water T.A., Bijl H.P. Delineation of organs at risk involved in swallowing for radiotherapy treatment planning. Radiother Oncol. 2011;101(3):394–402. doi: 10.1016/j.radonc.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 43.El Naqa I., Bradley J.D., Lindsay P.E., Hope A.J., Deasy J.O. Predicting radiotherapy outcomes using statistical learning techniques. Phys Med Biol. 2009;54(18):S9–S. doi: 10.1088/0031-9155/54/18/S02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gabrys H.S., Buettner F., Sterzing F., Hauswald H., Bangert M. Design and selection of machine learning methods using radiomics and dosiomics for normal tissue complication probability modeling of xerostomia. Front Oncol. 2018 doi: 10.3389/fonc.2018.00035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jiang W., Lakshminarayanan P., Hui X., Han P., Cheng Z., Bowers M., et al. Machine learning methods uncover radiomorphologic dose patterns in salivary glands that predict xerostomia in patients with head and neck cancer. Adv Radiat Oncol. 2019;4:401–412. doi: 10.1016/j.adro.2018.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dijk L., Brouwer C.L., Schaaf A.V., Burgerhof J.G., Beukinga R.J., Langendijk J.A., et al. CT image biomarkers to improve patient-specific prediction of radiation-induced xerostomia and sticky saliva. Radiother Oncol. 2017;122:185–191. doi: 10.1016/j.radonc.2016.07.007. [DOI] [PubMed] [Google Scholar]
- 47.Beasley W., Thor M., McWilliam A., Green A., Mackay R., Slevin N., et al. Image-based data mining to probe dosimetric correlates of radiation-induced trismus. Int J Radiat Oncol Biol Phys. 2018 November 15;102(4):1330–1338. doi: 10.1016/j.ijrobp.2018.05.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Terrell J.E., Ronis D.L., Fowler K.E., Bradford C.R., Chepeha D.B., Prince M.E., et al. Clinical predictors of quality of life in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg. 2004;130:401–408. doi: 10.1001/archotol.130.4.401. [DOI] [PubMed] [Google Scholar]
- 49.Dean J., Wong K., Gay H., Welsh L., Jones A.B., Schick U., et al. Incorporating spatial dose metrics in machine learning-based normal tissue complication probability (NTCP) models of severe acute dysphagia resulting from head and neck radiotherapy. Clin Transl Radiat Oncol. 2018;8:27–39. doi: 10.1016/j.ctro.2017.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Reddy J., Lindsay W., Berlind C., Ahern C., Holmes A., Smith B., et al. Applying a machine learning approach to predict acute radiation toxicities for head and neck cancer patients. Int J Radiat Oncol Biol Phys. 2019;105:S69. [Google Scholar]
- 51.Wojcieszynski A., Cava W.L., Baumann B., Lukens J., Ghiam A.F., Urbanowicz R., et al. Machine learning to predict toxicity in head and neck cancer patients treated with definitive chemoradiation. Int J Radiat Oncol Biol Phys. 2019;105:E139–E140. [Google Scholar]
- 52.Cheng Z., Nakatsugawa M., Hu C., Robertson S.P., Hui X., Moore J.A., et al. Evaluation of classification and regression tree (CART) model in weight loss prediction following head and neck cancer radiation therapy. Adv Radiat Oncol. 2017 Dec 7;3(3):346–355. doi: 10.1016/j.adro.2017.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dean J.A., Wong K.H., Welsh L.C., Jones A., Schick U., Newbold K.L., et al. Normal tissue complication probability (NTCP) modelling using spatial dose metrics and machine learning methods for severe acute oral mucositis resulting from head and neck radiotherapy. Radiother Oncol. 2016;120:21–27. doi: 10.1016/j.radonc.2016.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhang B., Lian Z., Zhong L., et al. Machine-learning based MRI radiomics models for early detection of radiation-induced brain injury in nasopharyngeal carcinoma. BMC Cancer. 2020;20:502. doi: 10.1186/s12885-020-06957-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Laia Humbert-Vidan, Vinod Patel, Robin Andlauer, Andrew P King, and Teresa Guerrero Urbano. 2022. Prediction of Mandibular ORN Incidence from 3D Radiation Dose Distribution Maps Using Deep Learning. In Applications of Medical Artificial Intelligence: First International Workshop, AMAI 2022, Held in Conjunction with MICCAI 2022, Singapore, September 18, 2022, Proceedings. Springer-Verlag, Berlin, Heidelberg, 49–58.
- 56.Brierley J., Gospodarowicz M., Wittekind C. eighth ed. Wiley; Chichester: 2017. UICC TNM classification of malignant tumours. [Google Scholar]
- 57.Kaka AS, Kumar B, Kumar P, Wakely PE Jr, Kirsch CM, Old MO, Ozer E, Agrawal A, Carrau RE, Schuller DE, Siddiqui F, Teknos TN. Highly aggressive human papillomavirus-related oropharyngeal cancer: clinical, radiologic, and pathologic characteristics. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013 Sep;116(3):327-35. 10.1016/j.oooo.2013.04.011. Epub 2013 Jun 14. PMID: 23770280; PMCID: PMC3748144. [DOI] [PMC free article] [PubMed]
- 58.Tseng Y.-J., Wang H.-Y., Lin T.-W., Lu J.-J., Hsieh C.-H., Liao C.-T. Development of a machine learning model for survival risk stratification of patients with advanced oral cancer. JAMA Netw Open. 2020;3(8):e2011768. doi: 10.1001/jamanetworkopen.2020.11768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Howard F.M., Kochanny S., Koshy M., Spiotto M., Pearson A.T. Machine learning-guided adjuvant treatment of head and neck cancer. JAMA Netw Open. 2020;3(11):e2025881. doi: 10.1001/jamanetworkopen.2020.25881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bernier J, Domenge C, Ozsahin M, etal; European Organization for Research and Treatment of Cancer Trial 22931. Postoperative irradiation with or without concomitant chemotherapy for locally advanced head and neck cancer. N Engl J Med. 2004;350(19):1945-1952. [DOI] [PubMed]
- 61.Cooper J.S., Pajak T.F., Forastiere A.A., et al. Radiation Therapy Oncology Group 9501/Intergroup. Postoperative concurrent radiotherapy and chemotherapy for high-risk squamous-cell carcinoma of the head and neck. N Engl J Med. 2004;350(19):1937–1944. doi: 10.1056/NEJMoa032646. [DOI] [PubMed] [Google Scholar]
- 62.Jiang R., You R., Pei X.Q., Zou X., Zhang M.X., Wang T.M., et al. Development of a ten-signature classifier using a support vector machine integrated approach to subdivide the M1 Stage Into M1a and M1b stages of nasopharyngeal carcinoma with synchronous metastases to better predict patients’ survival. Oncotarget. 2016;7(3):3645–3657. doi: 10.18632/oncotarget.6436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Parmar C., Grossmann P., Rietveld D., Rietbergen M.M., Lambin P., Aerts H.J.W.L. Radiomic machine-learning classifiers for prognostic biomarkers of head and neck cancer. Front Oncol. 2015;5:272. doi: 10.3389/fonc.2015.00272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zdilar L, Vock DM, Marai GE, Fuller CD, Mohamed ASR, Elhalawani H, et al. Evaluating the Effect of Right-Censored End Point Transformation for Radiomic Feature Selection of Data From Patients With Oropharyngeal Cancer. JCO Clin Cancer Inform (2018) 2):1–19. [DOI] [PMC free article] [PubMed]
- 65.Li S., Wang K., Hou Z., Yang J., Ren W., Gao Z., et al. Use of radiomics combined with machine learning method in the recurrence patterns after intensity-modulated radiotherapy for nasopharyngeal carcinoma: a preliminary study. Front Oncol. 2018;8:648. doi: 10.3389/fonc.2018.00648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Starke S., Leger S., Zwanenburg A., Leger K., Lohaus F., Linge A., et al. 2D and 3D convolutional neural networks for outcome modelling of locally advanced head and neck squamous cell carcinoma. Sci Rep. 2020;10(1):15625. doi: 10.1038/s41598-020-70542-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhou Z., Wang K., Folkert M., et al. Multifaceted radiomics for distant metastasis prediction in head & neck cancer. Phys Med Biol. 2020;65(15) doi: 10.1088/1361-6560/ab8956. [DOI] [PubMed] [Google Scholar]
- 68.Tran W.T., Suraweera H., Quaioit K., Cardenas D., Leong K.X., Karam I., et al. Predictive quantitative ultrasound radiomic markers associated with treatment response in head and neck cancer. Future Sci OA. 2020;6(1) doi: 10.2144/fsoa-2019-0048. FSO433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rich B., Huang J., Yang Y., Jin W., Johnson P., Wang L., et al. Radiomics predicts for distant metastasis in locally advanced human papillomavirus-positive oropharyngeal squamous cell carcinoma. Cancers (Basel) 2021;13(22):5689. doi: 10.3390/cancers13225689. PMID: 34830844; PMCID: PMC8616361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tosado J., Zdilar L., Elhalawani H., et al. Clustering of largely right-censored oropharyngeal head and neck cancer patients for discriminative groupings to improve outcome prediction. Sci Rep. 2020;10(1):3811. doi: 10.1038/s41598-020-60140-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bogowicz M., Jochems A., Deist T.M., et al. Privacy-preserving distributed learning of radiomics to predict overall survival and HpV status in head and neck cancer. Sci Rep. 2020;10(1):4542. doi: 10.1038/s41598-020-61297-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Le W.T., Vorontsov E., Romero F.P., et al. Cross-institutional outcome prediction for head and neck cancer patients using self-attention neural networks. Sci Rep. 2022;12:3183. doi: 10.1038/s41598-022-07034-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Reiazi R., Abbas E., Famiyeh P., Rezaie A., Kwan J.Y.Y., Patel T., et al. The impact of the variation of imaging parameters on the robustness of Computed Tomography radiomic features: A review. Comput Biol Med. 2021 Jun;133 doi: 10.1016/j.compbiomed.2021.104400. Epub 2021 Apr 16 PMID: 33930766. [DOI] [PubMed] [Google Scholar]
- 74.Larue R.T.H.M., van Timmeren J.E., de Jong E.E.C., Feliciani G., Leijenaar R.T.H., Schreurs W.M.J., et al. Influence of gray level discretization on radiomic feature stability for different CT scanners, tube currents and slice thicknesses: a comprehensive phantom study. Acta Oncol. 2017 Nov;56(11):1544–1553. doi: 10.1080/0284186X.2017.1351624. Epub 2017 Sep 8 PMID: 28885084. [DOI] [PubMed] [Google Scholar]
- 75.Zwanenburg A., et al. The Image Biomarker Standardization Initiative: standardized quantitative radiomics for high throughput image-based phenotyping. Radiology. 2020 doi: 10.1148/radiol.2020191145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gilpin, L. H. et al. in 2018 IEEE 5th International Conference on Data Science and Advanced Analytics (DSAA) 80–89 (2018).
- 77.Artificial Intelligence in Oncology: Current Capabilities, Future Opportunities, and Ethical Considerations Jacob T. Shreve, MD, Sadia A. Khanani, MD, and Tufia C. Haddad, MD American Society of Clinical Oncology Educational Book 2022 :42, 842-851. [DOI] [PubMed]
- 78.Hasin Y., Seldin M., Lusis A. Multi-omics approaches to disease. Genome Biol. 2017;18:83. doi: 10.1186/s13059-017-1215-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yan J., Risacher S.L., Shen L., Saykin A.J. Network approaches to systems biology analysis of complex disease: integrative methods for multi-omics data. Brief Bioinform. 2018;19:1370–1381. doi: 10.1093/bib/bbx066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sumner W., Kim S.S., Vitzthum L., et al. End of treatment cone-beam computed tomography (CBCT) is predictive of radiation response and overall survival in oropharyngeal squamous cell carcinoma. Radiat Oncol. 2021;16:147. doi: 10.1186/s13014-021-01871-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Muelas-Soria R., García-Mollá R., Morillo-Macías V., Bonaque-Alandí J., Sorribes-Carreras P., García-Piñón F., et al. The usefulness of adaptative radiotherapy in prostate cancer: how, when, and who? Biomedicines. 2022;10:1401. doi: 10.3390/biomedicines10061401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chin S., Eccles C.L., McWilliam A., Chuter R., Walker E., Whitehurst P., et al. Magnetic resonance-guided radiation therapy: A review. J Med Imaging Radiat Oncol. 2020;64:163–177. doi: 10.1111/1754-9485.12968. [DOI] [PubMed] [Google Scholar]
- 83.Jager E.A., Ligtenberg H., Caldas-Magalhaes J., Schakel T., Philippens M.E., Pameijer F.A., et al. Validated guidelines for tumor delineation on magnetic resonance imaging for laryngeal and hypopharyngeal cancer. Acta Oncol Stockh Swed. 2016;55:1305–1312. doi: 10.1080/0284186X.2016.1219048. [DOI] [PubMed] [Google Scholar]
- 84.King A.D., Thoeny H.C. Functional MRI for the prediction of treatment response in head and neck squamous cell carcinoma: potential and limitations. Cancer Imaging. 2016;16:23. doi: 10.1186/s40644-016-0080-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Watson G.A., Taylor K., Siu L.L. Innovation and advances in precision medicine in head and neck cancer. Crit Issues Head Neck Oncol. 2021;24:355–373. doi: 10.1007/978-3-030-63234-2_24. [DOI] [Google Scholar]
- 86.Shanmugam A., Hariharan A.K., Hasina R., Nair J.R., Katragadda S., Irusappan S., et al. Ultrasensitive detection of tumor-specific mutations in saliva of patients with oral cavity squamous cell carcinoma. Cancer. 2021 doi: 10.1002/cncr.33393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Arantes L.M.R.B., De Carvalho A.C., Melendez M.E., Carvalho A.L. Serum, plasma and saliva biomarkers for head and neck cancer. Expert Rev Mol Diagn. 2018;18:85–112. doi: 10.1080/14737159.2017.1404906. [DOI] [PubMed] [Google Scholar]
- 88.Kong L., Birkeland A.C. Liquid biopsies in head and neck cancer: current state and future challenges. Cancers. 1874;2021:13. doi: 10.3390/cancers13081874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jatana K.R., Balasubramanian P., Lang J.C., Yang L., Jatana C.A., White E., et al. Significance of circulating tumor cells in patients with squamous cell carcinoma of the head and neck: Initial results. Arch Otolaryngol Head Neck Surg. 2010;136:1274–1279. doi: 10.1001/archoto.2010.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Inhestern J., Oertel K., Stemmann V., Schmalenberg H., Dietz A., Rotter N., et al. Prognostic role of circulating tumor cells during induction chemotherapy followed by curative surgery combined with postoperative radiotherapy in patients with locally advanced oral and oropharyngeal squamous cell cancer. PLoS One. 2015;10:e0132901. doi: 10.1371/journal.pone.0132901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Strati A., Koutsodontis G., Papaxoinis G., Angelidis I., Zavridou M., Economopoulou P., et al. Prognostic significance of PD-L1 expression on circulating tumor cells in patients with head and neck squamous cell carcinoma. Ann Oncol Off J Eur Soc Med Oncol. 2017;28:1923–1933. doi: 10.1093/annonc/mdx206. [DOI] [PubMed] [Google Scholar]
- 92.Chera B.S., Kumar S., Shen C., Amdur R., Dagan R., Green R., et al. Plasma circulating tumor HPV DNA for the surveillance of cancer recurrence in HPV-associated oropharyngeal cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2020;38:1050–1058. doi: 10.1200/JCO.19.02444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rutkowski T.W., Mazurek A.M., Snietura M., Hejduk B., Jedrzejewska M., Bobek-Billewicz B., D’Amico A., Pigłowski W., Wygoda A., Składowski K., et al. Circulating HPV16 DNA may complement imaging assessment of early treatment efficacy in patients with HPV-positive oropharyngeal cancer. J Transl Med. 2020;18:1–10. doi: 10.1186/s12967-020-02330-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Theodoraki M.-N., Yerneni S.S., Brunner C., Theodorakis J., Hoffmann T.K., Whiteside T.L. Plasma-derived exosomes reverse epithelial-to-mesenchymal transition after photodynamic therapy of patients with head and neck cancer. Oncoscience. 2018;5:75–87. doi: 10.18632/oncoscience.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Pota M., Scalco E., Sanguineti G., Farneti A., Cattaneo G.M., Rizzo G., et al. Early prediction of radiotherapy-induced parotid shrinkage and toxicity based on CT radiomics and fuzzy classification. Artif Intell Med. 2017;81:41–53. doi: 10.1016/j.artmed.2017.03.004. [DOI] [PubMed] [Google Scholar]
- 96.Fujima N., Shimizu Y., Yoshida D., Kano S., Mizumachi T., Homma A., et al. Machine-learning-based prediction of treatment outcomes using MR imaging-derived quantitative tumor information in patients with sinonasal squamous cell carcinomas: a preliminary study. Cancers. 2019;11(6):800. doi: 10.3390/cancers11060800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wu J., Gensheimer M.F., Zhang N., Han F., Liang R., Qian Y., et al. Integrating tumor and nodal imaging characteristics at baseline and mid-treatment computed tomography scans to predict distant metastasis in oropharyngeal cancer treated with concurrent chemoradiotherapy. Int J Radiat Oncol. 2019;104(4):942–952. doi: 10.1016/j.ijrobp.2019.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lambin P., Leijenaar R., Deist T., et al. Radiomics: the bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol. 2017;14:749–762. doi: 10.1038/nrclinonc.2017.141. [DOI] [PubMed] [Google Scholar]
- 99.Ciro Franzese, Federico Fornasier. AI for Head Neck Cancer Treated With Adaptive RadioTherapy (RadiomicART) (RadiomicArt). NCT05081531.
- 100.Ye Zhang, Li Ma. Deep Learning-based Classification and Prediction of Radiation Dermatitis in Head and Neck Patients. NCT05607225.
- 101.Panagiotis Balermpas. MRI – Guided Adaptive RadioTHerapy for Reducing XerostomiA in Head and Neck Cancer (MARTHA-trial) (MARTHA). NCT03972072.