Acute kidney injury (AKI) increases the risks of hospitalization and long-term mortality,1 and is a challenging task in Sub-Saharan Africa, in which delayed presentation to health care centers and a shortage of resources to support patients with established AKI are key issues.2 The etiology and presentation of AKI vary between high-income and low-income countries.3 In Africa, the most reported causes are infections, such as malaria, dengue, HIV, diarrheal diseases, viral and parasitic infections, nephrotoxins, and obstetric and surgical complications.4 AKI during pregnancy can be caused by the same disorders that lead to AKI in the general population, or it can occur as a direct consequence of obstetric complications. Pregnancy-related AKI (PRAKI) is underreported in Africa. The prevalence rate of PRAKI has significantly reduced in developed countries as a result of better overall health care delivery.5 Somalia has one of the highest rates of maternal mortality in the world. According to the 2020 Somalia Health Demographic Survey, the maternal mortality rate is 692 per 100,000 live births, with the majority of these deaths being preventable.6 PRAKI is a major public health problem in Somaliland regions. Because of the lack of accessibility to maternal health care services in Somaliland, many women experience major complications during pregnancy or postdelivery. We studied the prevalence, etiology, presentation, and the fetal and maternal outcomes of PRAKI in the only tertiary care center of Somaliland.
Of the 9457 deliveries that were performed in the department of obstetrics and gynecology at Hargeisa Group Hospital during the study's time frame, 31 women had PRAKI (prevalence of 0.33%, 95% confidence interval [CI], 25.11–28.57). The demographic details of the patients are shown in Table 1. The patients’ age ranged from 18 to 36 years, and 58.06% were from rural regions. Only 54.84% were institutional deliveries, and most of them (64.52%) did not receive any antenatal care. Most cases occurred during the third trimester and the postpartum periods. Anemia was reported in 14 (45.20%) patients with a mean hemoglobin level of 7.29 gm/dl.
Table 1.
Demographic details of the patients
| Variables | Frequency(n) | Mean ± SD |
|---|---|---|
| Age (yr) | 31 | 26.84 ± 4.3 |
| Percentage | ||
| 18–20 | 4 | 12.90% |
| 21–25 | 9 | 29.03% |
| 26–36 | 18 | 58.07% |
| Residency | Frequency (n) | Percentage |
|---|---|---|
| Rural | 18 | 58.07% |
| Urban | 13 | 41.93% |
| Pregnancy stage | ||
| Second trimester | 6 | 19.35% |
| Third trimester | 10 | 32.26% |
| Postpartum period | 15 | 48.39% |
| Parity | ||
| Primigravida | 13 | 41.94% |
| Multigravida | 18 | 58.06% |
| Antenatal care | ||
| Received | 11 | 35.48% |
| Not received | 20 | 64.52% |
| Delivery | ||
| Institutional delivery | 17 | 54.84% |
| Noninstitutional delivery | 14 | 45.16% |
| Mode of delivery | ||
| Vaginal delivery | 24 | 77.42% |
| LSCS | 7 | 22.58% |
| Anemia | N | Mean | Std Deviation |
|---|---|---|---|
| Hemoglobin | 14 | 7.29 mg/dl | 0.98 |
LSCS, lower segment cesarean section.
The most common clinical presentations are shown in Supplementary Table S1.
From our findings, the leading causes of PRAKI were postpartum hemorrhage (29.03%), puerperal sepsis (25.81%), pre-eclampsia (19.35%), eclampsia (9.68%), placental previa (6.45%), hemolysis, elevated liver enzymes, and low platelets syndrome (6.45%), and acute fatty liver of pregnancy (3.23%) (Table 2).
Table 2.
Etiology of patients with pregnancy-related acute kidney injury
| Etiology | Frequency (n) | Percent (%) |
|---|---|---|
| Obstetric Complications | ||
| Postpartum hemorrhage | 9 | 29.03% |
| Placental Previa | 2 | 6.45% |
| Puerperal sepsis | 8 | 25.81% |
| Pregnancy specific disorders | ||
| Pre-eclampsia | 6 | 19.35% |
| Eclampsia | 3 | 9.68% |
| HELLP syndrome | 2 | 6.45% |
| AFLP | 1 | 3.23% |
| Total | 31 | 100.0% |
AFLP, acute fatty liver of pregnancy; HELLP, hemolysis, elevated liver enzymes, and low platelets.
Outcome of patients with PRAKI are shown in Supplementary Table S2. Only 48.39% of the patients recovered fully, and the maternal and fetal mortality were high ([9.68%; 95% CI, 22.49–27.51] and [58.6%; 95% CI, 1.45–1.99], respectively).
In Sub-Saharan Africa, approximately 4.4 million children, including 1.2 million newborns, and 265,000 mothers die every year because of pregnancy and childbirth complications. The fact that approximately 9 deaths occur every minute is indeed frightening.7 PRAKI continues to remain common in low-income countries with an incidence of 4.2% to 15%.8
To the best of our knowledge, no previous studies have reported the prevalence of PRAKI from Somaliland, which is deprived of the essential basic obstetric care. A recent large study conducted in Somaliland found that women with medical complications had the highest mortality rate (63%), followed by obstetric hemorrhage (13%), infection (10%), and hypertensive disorders (7.9%).9 Another report in a nearby region identified that antepartum or/and postpartum hemorrhage, eclampsia, sepsis, and obstructed labor were major causes of direct obstetric mortalities.S2 From our findings, the most common cause of PRAKI was obstetric complications (61.30%). It is not surprising that AKI was common, with 29.03% of women experiencing postpartum hemorrhage, 6.45% experiencing placental previa, and 25.81% experiencing puerperal sepsis. A World Health Organization analysis of causes of maternal death reported that the most frequent direct cause of maternal mortality in Africa was hemorrhage, which accounted for 34% of all maternal deaths; in addition, 10% were caused by sepsis/infections, and 4% were related to anemia.S3 Pregnancy specific disorders were the second leading cause in the current study; pre-eclampsia in 19.35%, eclampsia in 9.68%, hemolysis, elevated liver enzymes, and low platelets syndrome in 6.45%, and fatty liver of pregnancy in up to 3.23% of the patients. Pre-eclampsia and other hypertensive disorders of pregnancy are the most common causes of PRAKI, according to previous research.S4–S7
Patients from rural areas predominantly (64.52%) received no antenatal care and noninstitutional delivery counted up to 45.16% (they were brought to our center postpartum). That further contributed to excessive blood loss, presumably contributing to their initial low hemoglobin and high fetal mortality. Home delivery is prevalent in major towns in Somalia. As per a community-based health survey, women who were less aware of the importance of health facility delivery, along with those who did not receive antenatal care, were more prone to giving birth at home. In Somaliland, only a small proportion of deliveries occur in institutions with trained medical staff; the overwhelming majority of deliveries takes place at home with assistance from traditional birth attendants who lack formal training.S8 Similarly, in a community-based cross-sectional study conducted in Ethiopia in which 657 eligible women were enrolled, 71% of respondents reported having had noninstitutional childbirths.S9 Of the 31 patients in the current study, 11 (35.52%) had AKI Stage 1, 6 (19.32%) had AKI Stage 2, and 14 (45.16%) had AKI Stage 3.
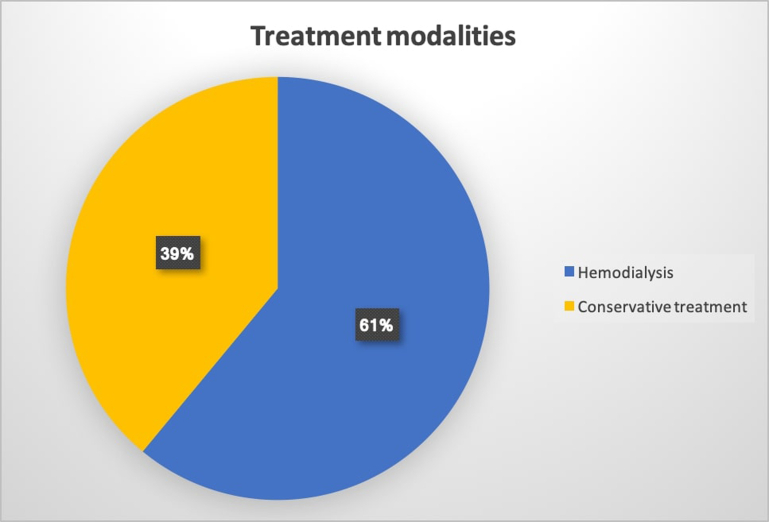
With respect to maternal outcome, hemodialysis was needed in 19 (61.0 %) whereas the remaining 12 (39.0 %) were managed conservatively (Figure 1). Intensive care unit admission was required in 8 patients 26.0 % (Figure 2). We noted complete recovery in 48.39% of cases, 6.45% were dialysis dependent, whereas 19.35% had recovered partially. Three maternal deaths occurred as a result of postpartum hemorrhage and puerperal sepsis. The pattern of maternal deaths in our study area is vastly different from that in more industrialized nations. It is important to prioritize and ensure health care access to all women during pregnancy to reduce preventable infant and maternal fatalities. However, many pregnant African girls, adolescent mothers, and their babies are susceptible to PRAKI because of the lack of accessibility to antenatal and postnatal care. Similar to our current result, direct obstetric complications are the leading cause of maternal deaths in Africa and are heavily influenced by hemorrhage, maternal sepsis, and hypertensive diseases that are entirely preventable.7
Figure 1.
Treatment modalities
Figure 2.
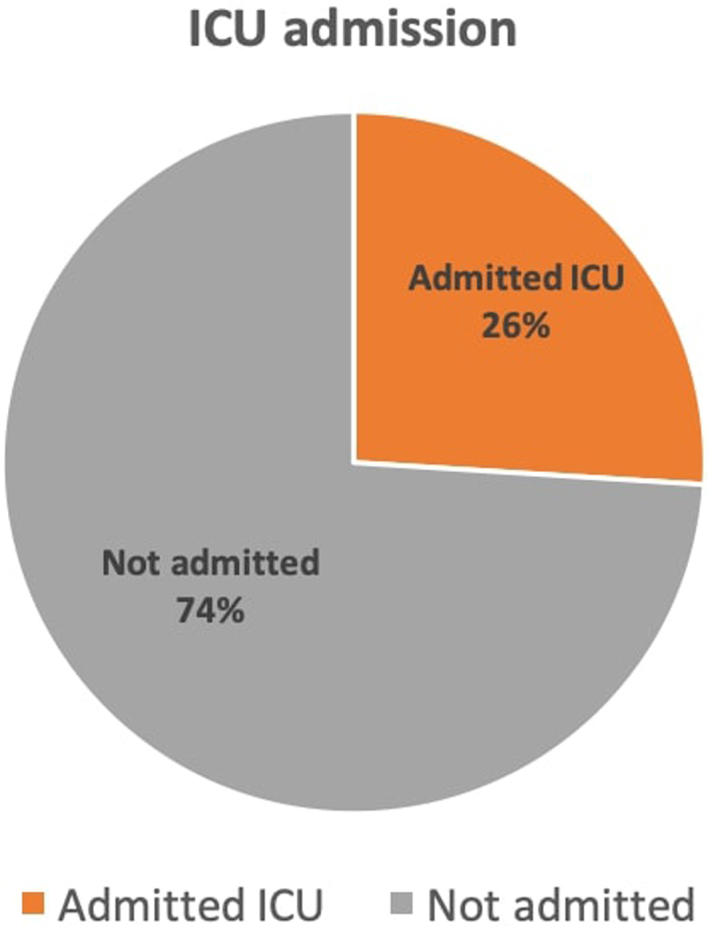
PRAKI related ICU admission. ICU, intensive care unit; PRAKI, pregnancy-related AKI.
During the times of disaster, the maternal and fetal outcomes have been shown to be poor with increased risk of gestational hypertension, pre-eclampsia and eclampsia, low birthweight, miscarriages, and premature deliveries.S10–S12 Destruction and disruptions of health care services are common. Access to basic services like water and electricity is hampered, adding to the psychological and physiological stress. This can compromise the antenatal and postnatal care and lead to reduction in monitored institutional deliveries, which ultimately impact the pregnancy outcomes negatively. Such calamities can have disastrous consequences and can adversely affect maternal and infant mortality in Africa—a region that is already grappling with the effects of inadequate health care and many additional underreported barriers. Strengthening of emergency preparedness and response both financially and by optimum manpower is therefore required to tackle such situations. This becomes very important because according to World Risk Report 2021, Africa is the continent with the highest overall societal vulnerability; 12 of the 15 most vulnerable countries in the world are in Africa.S13 Strengthening basic primary health care is important in preparing for safe deliveries during such disasters. A strong social support system is also similarly important and should not be ignored.
In conclusion, AKI during pregnancy and postpartum period is challenging to treat in low-resource settings. Fortunately, it is preventable if proper precautions are taken. A poor prognosis may be indicated by severity at presentation. To reduce mortality among women with PRAKI, antenatal care for all pregnant women and appropriate interventions for the postnatal period should be considered. The management of this during natural calamities and disaster will need extra preparedness to avert the worsening of already poor outcome.
Disclosure
All the authors declared no competing interests.
Acknowledgments
This work has been made possible through the ISN mentorship program.
Footnotes
Supplementary Method.
Supplementary Reference.
Table S1. The most common clinical presentation.
Table S2. Outcome of patients with PRAKI.
Supplementary Material
Supplementary Method.
Supplementary Reference.
Table S1. The most common clinical presentation.
Table S2. Outcome of patients with PRAKI.
References
- 1.Hou S.H., Bushinsky D.A., Wish J.B., Cohen J.J., Harrington J.T. Hospital-acquired renal insufficiency: a prospective study. Am J Med. 1983;74:243–248. doi: 10.1016/0002-9343(83)90618-6. [DOI] [PubMed] [Google Scholar]
- 2.Naicker S., Aboud O., Gharbi M.B. Epidemiology of acute kidney injury in Africa. Semin Nephrol. 2008;28:348–353. doi: 10.1016/j.semnephrol.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 3.Lameire N.H., Bagga A., Cruz D., et al. Acute kidney injury: an increasing global concern. Lancet. 2013;382:170–179. doi: 10.1016/S0140-6736(13)60647-9. [DOI] [PubMed] [Google Scholar]
- 4.Kahindo C.K., Mukuku O., Wembonyama S.O., Tsongo Z.K. Prevalence and factors associated with acute kidney injury in sub-Saharan African adults: a review of the current literature. Int J Nephrol. 2022;2022 doi: 10.1155/2022/5621665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stratta P., Besso L., Canavese C., et al. Is pregnancy-related acute renal failure a disappearing clinical entity? Ren Fail. 1996;18:575–584. doi: 10.3109/08860229609047680. [DOI] [PubMed] [Google Scholar]
- 6.The Somali health and demographic survey 2020. reliefweb. Accessed 2022.
- 7.Kinney M.V., Kerber K.J., Black R.E., et al. Sub-Saharan Africa’s mothers, newborns, and children: where and why do they die? PLoS Med. 2010;7 doi: 10.1371/journal.pmed.1000294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gumber M.R., Jain S.H., Kute V.B., et al. Outcome of second kidney transplant: a single center experience. Saudi J Kidney Dis Transpl. 2013;24:696–701. doi: 10.4103/1319-2442.113857. [DOI] [PubMed] [Google Scholar]
- 9.Egal J.A., Kiruja J., Litorp H., Osman F., Erlandsson K., Klingberg-Allvin M. Incidence and causes of severe maternal outcomes in Somaliland using the sub-Saharan Africa maternal near-miss criteria: a prospective cross-sectional study in a national referral hospital. Int J Gynecol Obstet. 2022;159:856–864. doi: 10.1002/ijgo.14236. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.