Abstract
Background:
Nonsurgical interventions such as bracing with ankle foot orthoses (AFOs) aim to assist, restore, and redirect weightbearing forces to address difficulty with mobilization. We identified a custom carbon fiber passive dynamic ankle foot orthosis (PDAFO) that was designed to meet the needs of military combat veterans. We sought to evaluate the off-loading properties of one model of PDAFO (ExoSym) in a civilian population.
Methods:
Civilian patients 18 years or older were prescribed a PDAFO by a single surgeon. Pedobarographic data were obtained using the Tekscan F-Scan system. With the insole, participants were instructed to walk at a self-selected pace along a 20 m walkway under 3 conditions: (1) insole placed in between the brace and foot (over); (2) insole placed between the brace and insole of the shoe (under); (3) without the brace, the insole was placed in between the foot and insole of the shoe in both limbs (without).
For assessment, forefoot and heel areas were evaluated with respect to maximal force, force*time integral (FTI), maximal contact area, maximal contact pressure, pressure*time integral (PTI), center of force (COF) excursion.
Results:
Six patients with arthritic foot and ankle conditions completed pedobarographic assessment for analysis. The brace reduced forefoot maximal force and contact pressures by 66% and 49%, respectively (538 ± 236 to 185 ± 130 N [P < .001], and 99 ± 38 to 50 ± 24 P < .002). Additionally, participants were observed to load the forefoot portion of the brace with double the maximum contact pressures compared to the unbraced foot (204 ± 57 to 99 ± 38 kPa, P < .001).
Conclusion:
The results of this study showed that the PDAFO unloaded substantial force and pressure experienced by the forefoot. Participants loaded the brace to a greater extent than when going unbraced. ADAFO can provide measurable pressure relief for patients with arthritic conditions.
Level of Evidence:
Level IV, case series.
Keywords: arthritis, gait studies, PDAFO, brace
Introduction
Injuries to the midfoot and ankle can have a profoundly debilitating effect on health-related quality of life.2,8,9,12,13,17,18,27 Bracing provides support to the foot and ankle by limiting motion through painful or unstable motion segments.11,14 A rigid ankle foot orthosis (AFO) reduces joint reactive forces experienced by the ankle but can interfere with gait kinematics.16
Bracing for arthritic foot and ankle conditions faces resistance for a variety of reasons. Patients often face challenges finding suitable footwear and may dislike the inconvenience of donning and doffing an AFO. Patients may also view braces as less effective than surgery for ankle arthritis. Overall patient satisfaction with ankle bracing has been questioned.12,29 Bracing rationale is often incompletely explained to patients; furthermore, custom braces are expensive, and cost may present a barrier.25 Therefore, demonstrating measurable effects of bracing would help clarify indications for brace treatment.
Newer brace materials and design principles enable alleviating forces experienced by the foot and ankle in addition to providing stability. Passive dynamic AFOs (PDAFOs) were initially designed to compensate for insufficient plantarflexion strength.1 PDAFOs function as a torsion spring (Figure 1) whereby forces are transmitted from the footplate across the ankle via flexible struts connected to a cuff on the calf. This type of brace design can serve multiple purposes: (1) provide push-off power in cases of insufficient gastroc-soleus complex, (2) stabilize the entire foot and ankle, and (3) provide forefoot offloading.21
Figure 1.

Left: PDAFO (ExoSym); right: torsion spring. Thick lines show sensor placement (over and under the brace).
The United States Department of Defense supported development of the earliest iteration of PDAFO named the Intrepid Design Exoskeletal Orthosis (IDEO).10 It has been rebranded for commercial civilian use as ExoSym (used in the present study) but is not widely available. PDAFO is an umbrella term used to describe the type of brace while not identifying a specific product. Other versions of PDAFOs exist, but currently none has gained wide acceptance in the medical community for treating arthritic conditions involving the foot and ankle.
In a military population, PDAFOs have been demonstrated to address weakness, open tibia fracture sequela, and other high-energy injuries.19,20,22,23 In many cases, patients have returned to vigorous activity with the assistance of PDAFOs and a comprehensive rehabilitation program.6 Bracing with PDAFOs has also been shown to improve measures in functional performance and patient-reported outcomes in a military population.23
Less is known about the performance of PDAFOs in a nonmilitary population. Furthermore, access to this type of custom brace is often restricted because of cost and insurance claim denial. We believe that PDAFOs can provide significant benefit to civilian patients. The distinction of PDAFOs from most traditional bracing is that PDAFOs utilize a full-length customized foot plate, a posterior strut, and a proximal ground reaction cuff to create a dynamic AFO. This feature allows storage and release of energy during the gait cycle. Traditional bracing rarely employs a full-length, custom molded foot plate and is primarily designed to control painful sagittal and coronal motion via immobilization.16,17 Because PDAFOs are designed to function differently from traditional braces, they may offer some advantages.
Our purpose is to demonstrate the benefits of PDAFO bracing in civilian patients with foot and ankle arthritic conditions; we aim to show these benefits by quantifying pressures and forces experienced by both the brace and the foot during walking.
Materials and Methods
Participants
All participants provided informed consent, and this study protocol was approved by the Institutional Review Board. The participants were recruited from ≥18-year-old patients who were prescribed a PDAFO by the same orthopaedic surgeon at the same institution between 2014 and 2018, and the PDAFO of all participants were made by the same orthotist. Participants with neurologic or musculoskeletal disease in the contralateral leg, spinal cord injury, or central nervous system pathology were excluded from the study. Six civilian participants (5 male and 1 female) were included in the study. Indications for bracing treatment included arthritic foot or ankle conditions amenable to dynamic bracing. See Table 1 for the patient characteristics.
Table 1.
Patient Characteristics and Pain Scores.a
| Participant | Age (y) | Gender | Body Mass Index | Musculoskeletal Injury | Involved Side | Pain Scale Without PDAFO | Pain Scale With PDAFO |
|---|---|---|---|---|---|---|---|
| 1 | 40 | M | 24.4 | Midfoot arthrosis | R | 2 | 0 |
| 2 | 47 | M | 27.5 | Symptomatic ankle fusion | R | 4 | 1 |
| 3 | 26 | M | 25.6 | Arthrosis following navicular fracture | R | 1 | 0 |
| 4 | 54 | M | 23.8 | Ankle arthritis | L | 3 | 1 |
| 5 | 49 | M | 30.5 | Symptomatic ankle fusion | L | 3 | 1 |
| 6 | 31 | F | 20.0 | Arthrosis following talar fracture | L | 5 | 0 |
Abbreviation: F, female; M, male; PDAFO, passive dynamic ankle foot orthosis.
Pain was rated on a scale from 1 to 10, with 0 representing “no pain” and 10 “very much pain.”
Foot Pressure Data Collection During 20-m Walk
Foot pressure was measured using the Tekscan F-Scan system (Tekscan Inc, Norwood, MA) with a resolution of 4 sensels/cm2 and a sampling rate of 50 Hz. The ultrathin, in-shoe sensors were trimmed to the size of the participant’s feet and provided dynamic force, pressure, and timing information.
Three experimental conditions were tested with the F-Scan sensor: (1) Without—the participant walked without the PDAFO; the sensor was placed between the foot and the shoe insole. (2) Under—the participant walked with the PDAFO; the sensor was placed between the PDAFO and the shoe insole. (3) Over—the participant walked with the PDAFO; the sensor was placed between the foot and the PDAFO (Figure 1). In all 3 conditions, the sensor was placed between the foot and shoe insole on the unaffected side. Patients selected their own footwear.
Prior to data collection in each condition, real-time data were collected to inspect for crinkles of the insole, which would be represented as high-pressure areas near the edge of the insole. If any high-pressure areas were found, the sensors were repositioned or retrimmed. Before data collection of each condition of each participant, the insoles were calibrated according to the Tekscan user manual.
After the insole was calibrated, the participant was instructed to walk at a self-selected comfortable speed along a 20-m leveled walkway. Three successful trials were collected for each condition. The participants had several minutes to rest between trials.
Patient-Reported Outcome
Patients were asked to rate their pain on a 0 to 10 pain scale with or without the PDAFO.
Data Analysis
The foot pressure data were analyzed using F-Scan Research software version 7.55 (Tekscan Inc). Each trial of 20 m walking contained 10 to 20 stances, with an average of 13.3 ± 2.0 stances per trial among all trials of all conditions of all participants. The software identified the stances, excluded the first and the last stances, and averaged the rest of the stances. Then, the forefoot and heel areas were identified automatically by the software and manually adjusted by the user if necessary. Next, the maximal force, force*time integral (FTI), maximal contact area, maximal contact pressure, pressure*time integral (PTI) were calculated for the forefoot and the heel, respectively. In addition, the center of force (COF) excursion of the entire foot was calculated. Finally, the values of the 3 trials in each condition were averaged for each variable listed above. The above analyses were performed for each participant before the statistical analysis.
Statistical Analysis
Paired samples Student t test with two tails were used to compare the pain scores with and without the PDAFO for all participants. One-way analysis of variance with repeated measures was performed to detect effects of the condition (3 levels: Without, Under, and Over). Effects were statistically significant at the .05 significance level. Pairwise comparison with least significant difference (equivalent to no adjustments) was performed to detect difference among the conditions.
Differences were statistically significant at the .05 significance level.
Results
Differences among the 3 conditions can be seen by a visual examination of the foot pressure data of each condition of each participant displayed in Figures 2 and 3. Compared to the Without condition, the Under condition showed higher pressure in both the heel and the forefoot areas (especially in the forefoot) in most participants; COF excursion was increased in some participants. Compared to the Without condition, the Over condition showed reduced pressure in both the heel and the forefoot areas (especially in the forefoot) in most participants.
Figure 2.
Foot pressure data of the 3 conditions (Without, Under, Over) of participants 1 to 4. Foot pressure data are presented as 2-dimensional contours using a color scale that indicates pressure. Rectangles define the heel and the forefoot areas. The black trajectory is the center of force trajectory as the weight shifts from the heel to the toes during walking.
Figure 3.
Foot pressure data of the 3 conditions (Without, Under, Over) of participants 5 and 6.
The statistical results below only included the involved side of the 6 participants. Table 2 and Figure 4 show the results of 1-way analysis of variance with repeated measures of the participants. The participants were drawn from a cohort of 30 patients who were prescribed the brace between 2014 and 2018 (Figure 5).
Table 2.
One-Way ANOVA With Repeated Measures That Detect Effects of the Condition (3 Levels: Without, Under, and Over) for the Affected Side.a
| Mean ± SD | ANOVA | Pairwise Comparison P | ||||||
|---|---|---|---|---|---|---|---|---|
| Without | Under | Over | F(2, 10) | P | Without vs Under | Without vs Over | Under vs Over | |
| Max force (N) | ||||||||
| Heel | 536 ± 96 | 685 ± 243 | 604 ± 87 | 2.46 | NS | NS | NS | NS |
| Forefoot | 538 ± 236 | 792 ± 131 | 185 ± 130 | 56.39 | <.001 | .013 | .001 | <.001 |
| FTI (N × sec) | ||||||||
| Heel | 157 ± 44 | 179 ± 65 | 262 ± 73 | 4.86 | .033 | NS | .038 | NS |
| Forefoot | 149 ± 71 | 200 ± 59 | 71 ± 48 | 21.24 | <.001 | NS | .001 | .002 |
| Maximum contact area (cm2) | ||||||||
| Heel | 45.4 ± 10.4 | 36.6 ± 8.6 | 52.8 ± 8.8 | 8.00 | .008 | NS | .023 | .025 |
| Forefoot | 58.2 ± 23.7 | 48.7 ± 14.0 | 43.0 ± 24.0 | 3.98 | .053 | NS | .041 | NS |
| Maximum contact pressure (kPa) | ||||||||
| Heel | 127 ± 42 | 186 ± 48 | 120 ± 28 | 7.93 | .009 | .04 | NS | .016 |
| Forefoot | 99 ± 38 | 204 ± 57 | 50 ± 24 | 46.97 | <.001 | .003 | .002 | <.001 |
| PTI (kPa × s) | ||||||||
| Heel | 40.5 ± 23.9 | 50.7 ± 10.7 | 51.4 ± 14.5 | 0.89 | NS | NS | NS | NS |
| Forefoot | 30.1 ± 9.9 | 43.6 ± 5.9 | 21.8 ± 9.2 | 15.98 | .001 | .03 | .002 | .006 |
| COF excursion (cm) | ||||||||
| Foot | 18.1 ± 1.1 | 21.4 ± 2.7 | 6.9 ± 3.3 | 68.56 | <.001 | .044 | <.001 | <.001 |
Abbreviations: ANOVA, analysis of variance; COF, center of force; FTI, force*time integral; NS, nonsignificant; PTI, pressure*time integral.
Significance was set at the .05 Level.
Figure 4.
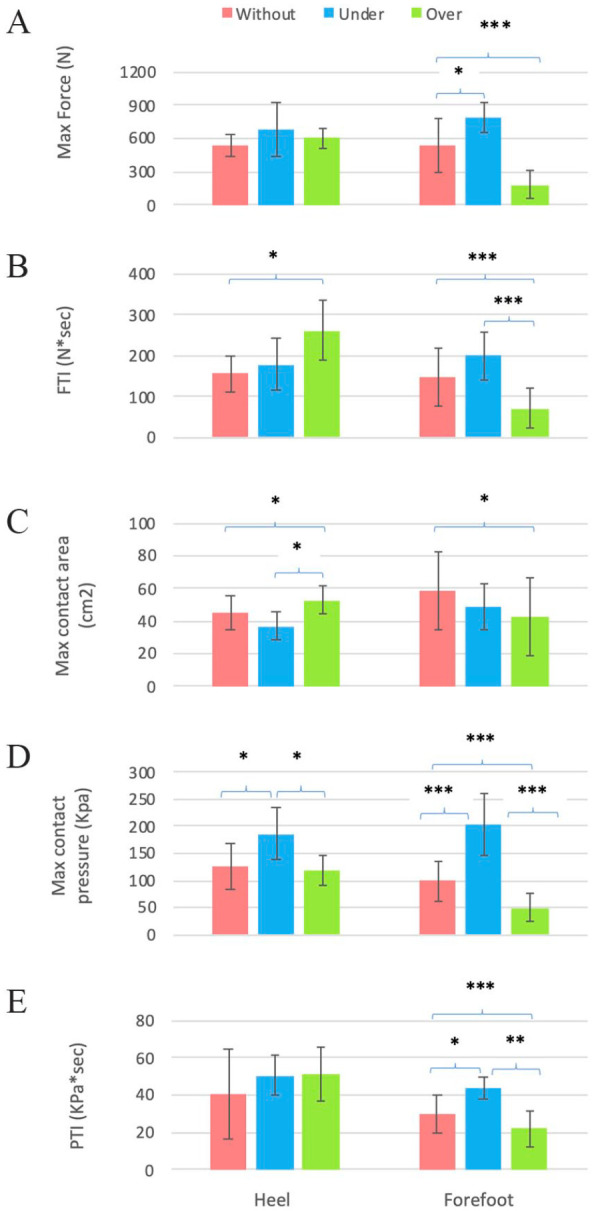
Foot pressure variables of the heel (left) and forefoot (Right) areas in the 3 experimental conditions. A = MaxForce, B = FTI, C = Max Contact Area, D = Max contact pressure, E = PTI.
Pairwise comparison p value: *P < .05. **P < .01. ***P < .005.
Figure 5.
Passive dynamic ankle foot orthosis (PDAFO) flow diagram.
For maximal force (Table 2 and Figure 4A), there was a significant effect noted in the forefoot area, but not the heel. Maximal force in the forefoot area in the Over condition was lower than in the Without condition by 66% in the forefoot area (185 ± 130 and 538 ± 236 N, respectively; P = .001). Notably, the forefoot Over position experienced 77% reduction of the force compared to the Under position (792 ± 131 vs 185 ± 130 N, P < .001). This indicated the PDAFO appeared to increase push-off power as ground reaction forces were applied.
For FTI (Table 2 and Figure 4B), sensor position had a greater effect in the forefoot than heel, but was significant in both. FTI in the Over condition was lower than that in the Without condition and lower than that in the Under condition. FTI is the integral of force over time. The above results showed through the FTI how the PDAFO relieves forces in the forefoot area.
The maximal contact area (Table 2 and Figure 4C) in the heel was larger in the Over condition than in the Without condition, which showed the heel cup of PDAFO increased the contact area. Sensor location in the forefoot area did not reach significance, but there was a trend of reduced contact area in the forefoot area in the Over condition than in the Without condition.
Maximal heel contact pressure (Table 2 and Figure 4D) in the Under condition was higher than in the Without and Over conditions. Maximal forefoot contact pressure in the Under condition was higher than in the Without condition. The maximal contact pressure in the Over condition was 49% lower than that in the Without condition. The reduction of forefoot pressure by the PDAFO from the Under to Over position was 75% (204 ± 57 vs 50 ± 24 kPa, P < .001). The PDAFO also generated higher pressures in forefoot push-off than Without the brace (99 ± 38 vs 204 ± 57 kPa, P = .003). These results showed that although the maximal contact pressure was increased in both the heel and forefoot areas Under PDAFO, the maximal contact pressure on the foot inside the PDAFO was not increased in the heel area and was substantially decreased in the forefoot area.
PTI (Table 2 and Figure 4E) in the Under condition was higher than that in the Without condition, and PTI in the Over condition was lower than that in the Without condition. These PTI results in the forefoot area showed that although the PTI was decreased in the Over position as compared to Under and Without.
COF excursion (Table 2) in the Under condition was longer than in the Without condition, and COF excursion in the Over condition was shorter than that in the Without condition. COF excursion shows transfer of weight from the heel to the toes and is an indicator of roll-over and push-off. Longer COF excursion indicates more complete roll-over of the foot and stronger push-off. Although COF excursion under the PDAFO was increased, it was decreased under the foot inside the PDAFO because the force in the forefoot area was reduced.
All participants reported reduced pain when walking with the PDAFO compared to walking without the PDAFO (Table 1). Paired Student t test showed the pain scores are significantly lower (P < .005) with the PDAFO than without the PDAFO.
Discussion
The results show that PDAFOs reduce forefoot forces and peak pressures in a civilian population with arthritic conditions of the foot and ankle. Existing literature has only evaluated this brace in military personnel. Our study supports the use of PDAFO bracing by showing how it can offload arthritic joints, store energy, and then return energy to assist forward propulsion.
The results of this study also showed that PDAFO relieved contact pressures experienced by the foot while generating force. Moreover, COF excursion under the PDAFO increased (which indicated more complete roll-over of the foot and stronger push-off), but it decreased under the foot inside the PDAFO because the force in the forefoot area was reduced. The change in the COF excursion and the maximal contact pressure indicated that the greatest offloading occurs from midstance through terminal stance, which is consistent with the findings of Stewart et al.26 Their study looked at pressure relief between the foot and the brace, but did not evaluate the forces exerted on the ground by the brace. The results of the present study demonstrated that the PDAFO generated forefoot force (and thus power: Table 2, Without 538 ± 236 vs Under 792 ± 131 N, P = .013). The present study showed that the maximal force in the forefoot area Under the brace is 47% higher than that without the brace; correspondingly, brace use resulted in 49% reduction in forefoot (Over) peak pressures, a finding that is similar to the 60% reduction reported by Stewart et al.26 These results provide insight into the mechanism by which PDAFOs reduce forces experienced by the foot, and corresponds to improved function shown in other studies.19 ,20,22,23 Using customized design, the PDAFO can unload or reduce pressure in specific areas of the foot and therefore reduce painful forces during weightbearing (present study and Bedigrew et al5).
Bracing is often advocated along with weight loss when deploying first-line conservative treatment for arthritic foot and ankle conditions. Other studies have evaluated the effect of body weight in relation to foot pressures.3,15,24,28 Our study suggests PDAFO bracing might be more effective in alleviating forefoot pressures than considerable weight loss. One study7 observed that a 19-kg weight loss resulted in 14% reductions in plantar forefoot pressure. Another study3 of adults wearing 15-kg vests experienced peak pressure increase of 30% in the forefoot while using similar equipment to our study. For comparison, our study demonstrated PDAFO reduced maximal contact pressure by 49% in the forefoot. This suggests that PDAFO offers equal or greater effect to therapeutic weight loss on forefoot pressures. PDAFO use has been shown independently to improve patients’ ability to return to desired levels of activity6; this may make desired weight loss more achievable, creating a virtuous circle for pain relief.
Regarding brace indications, there lacks uniformity in recommendation for arthritic conditions of the foot and ankle. A review article has suggested a role for dynamic AFOs, highlighting their shock-absorptive properties.11 Another commended rigid AFOs for their static properties of immobilization.14 There is no consensus on what constitutes optimal bracing for arthritic foot and ankle conditions; realistically, each patient should receive individual consideration for what constitutes optimal bracing. PDAFO should be considered as an alternative to traditional gauntlet AFOs. What a PDAFO offers beyond traditional bracing is the pressure relief via absorption and release of ground reactive forces in addition to joint stabilization. For patients wishing to remain active, a PDAFO may hold an advantage over traditional bracing.
Strengths of this study included the use of plantar force and pressure measurements that are straightforward to perform, require minimal equipment, and provide quantitative and objective evaluations. This study evaluated the effect of PDAFO bracing on walking by comparing foot pressure in 3 conditions—without, under, and over the brace. Also, this study offers affirmative and complementary information to the work performed by Stewart et al;26 our study analyzed additional variables such as the maximal force, maximal contact area, FTI, and PTI. The additional variables provide greater insight into the accumulated effect of changes in force, pressure and contact area, because pain is relevant not only to increased peak pressure but also to the accumulation of increased peak pressure over time. Finally, although most published studies were performed on military service members, our study was on civilians. Stewart et al’s26 study involved a population treated at the Naval Medical Center in San Diego whose average age was 29 years; the average age of our civilian population was over a decade higher. Service members were usually fit physically before injury and were motivated in physical therapy after injury.26 The severity of injuries may have been different between the service members and civilian patients.26 The participants in the published studies on military personel had access to very specialized health care and specialized rehabilitation,19 which may be quite different from the resources of the civilian patients. The ability to translate the PDAFO and rehabilitation program into the civilian population was unknown and worth investigating.5 The present study begins to fill this gap.
This study is limited by small sample size. The primary reason for low numbers is low availability of the ExoSym PDAFO brace in a civilian population. Its cost represents a barrier, and it is not covered by commercial insurance, Medicare or Medicaid. We did not assess dorsal foot pressures against shoe upper; these may be elevated in “overstuffed” shoes.
PDAFOs represent a technologic advance in bracing. Individual patient assessment and customization is routine in the fabrication of amputation sockets.4 Similarly, fabrication of ankle braces can include a more sophisticated attention to patient-specific variables.
In conclusion, our work quantifies pressure relief and power generation of PDAFO braces in a civilian population. In this context, PDAFO braces hold promise for expanded usage beyond a military population to groups with lower functional demands. The analogy of how the brace functions as a torsional spring explains our findings of forefoot offloading. Our findings merit further study in larger patient populations.
Acknowledgments
The authors would like to acknowledge the invaluable help of Michael Hahn, PhD, in data collection and Todd DeWees, MHA, CPO, in editing the manuscript.
Footnotes
Ethical Approval: Ethical approval for this study was obtained from the Oregon Health and Sciences University Institutional Review Board (STUDY00018222: Patient-Reported Outcomes after Use of ExoSym Braces).
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Austin Thompson, BS,  https://orcid.org/0000-0003-3194-6184
https://orcid.org/0000-0003-3194-6184
James E. Meeker, MD,  https://orcid.org/0000-0002-8346-7938
https://orcid.org/0000-0002-8346-7938
References
- 1. Arch ES, Stanhope SJ. Passive-dynamic ankle–foot orthoses substitute for ankle strength while causing adaptive gait strategies: a feasibility study. Ann Biomed Eng. 2015;43(2):442-450. doi: 10.1007/s10439-014-1067-8 [DOI] [PubMed] [Google Scholar]
- 2. International Foot and Ankle Osteoarthritis Consortium; Arnold JB, Bowen CJ, Chapman LS, et al. International Foot and Ankle Osteoarthritis Consortium review and research agenda for diagnosis, epidemiology, burden, outcome assessment and treatment. Osteoarthritis Cartilage. 2022;30(7):945-955. doi: 10.1016/j.joca.2022.02.603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Arnold JB, Causby R, Pod GD, Jones S. The impact of increasing body mass on peak and mean plantar pressure in asymptomatic adult subjects during walking. Diabet Foot Ankle. 2010;1(1):5518. doi: 10.3402/dfa.v1i0.5518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ballit A, Mougharbel I, Ghaziri H, Dao TT. Computer-aided parametric prosthetic socket design based on real-time soft tissue deformation and an inverse approach. Vis Comput. 2022;38(3):919-937. doi: 10.1007/s00371-021-02059-9 [DOI] [Google Scholar]
- 5. Bedigrew KM, Patzkowski JC, Wilken JM, et al. ; Skeletal Trauma Research Consortium (STReC). Can an integrated orthotic and rehabilitation program decrease pain and improve function after lower extremity trauma? Clin Orthop Relat Res. 2014;472(10):3017-3025. doi: 10.1007/s11999-014-3609-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Blair JA, Patzkowski JC, Blanck RV, Owens JG, Hsu JR. Return to duty after integrated orthotic and rehabilitation initiative. J Orthop Trauma. 2014;28(4):e70-e74. doi: 10.1097/BOT.0000000000000006 [DOI] [PubMed] [Google Scholar]
- 7. Bolte K. Pressure changes under the feet of obese adults after a weight reduction program. Arch Physiol Biochem. 2000;108:70. [Google Scholar]
- 8. Coester LM, Saltzman CL, Leupold J, Pontarelli W. Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg Am. 2001;83(2):219-228. doi: 10.2106/00004623-200102000-00009 [DOI] [PubMed] [Google Scholar]
- 9. Daniels TR, Younger ASE, Penner M, et al. Intermediate-term results of total ankle replacement and ankle arthrodesis: a COFAS multicenter study. J Bone Joint Surg Am. 2014;96(2):135-142. doi: 10.2106/JBJS.L.01597 [DOI] [PubMed] [Google Scholar]
- 10. Devore DI, Walters TJ, Christy RJ, et al. For Combat wounded: extremity trauma therapies from the USAISR. Mil Med. 2011;176(6):660-663. doi: 10.7205/MILMED-D-10-00362 [DOI] [PubMed] [Google Scholar]
- 11. Elattar O, Smith T, Ferguson A, Farber D, Wapner K. Uses of braces and orthotics for conservative management of foot and ankle disorders. Foot Ankle Orthop. 2018;3(3):247301141878070. doi: 10.1177/2473011418780700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fisher LR, McLellan DL. Questionnaire assessment of patient satisfaction with lower limb orthoses from a district hospital. Prosthet Orthot Int. 1989;13(1):29-35. doi: 10.3109/03093648909079407 [DOI] [PubMed] [Google Scholar]
- 13. Fuchs S, Sandmann C, Skwara A, Chylarecki C. Quality of life 20 years after arthrodesis of the ankle: a study of adjacent joints. J Bone Joint Surg Br. 2003;85-B(7):994-998. doi: 10.1302/0301-620X.85B7.13984 [DOI] [PubMed] [Google Scholar]
- 14. Hayes BJ, Gonzalez T, Smith JT, Chiodo CP, Bluman EM. Ankle arthritis: you can’t always replace it. J Am Acad Orthop Surg. 2016;24(2):e29-e38. doi: 10.5435/JAAOS-D-15-00354 [DOI] [PubMed] [Google Scholar]
- 15. Hills AP, Hennig EM, Byrne NM, Steele JR. The biomechanics of adiposity – structural and functional limitations of obesity and implications for movement. Obes Rev. 2002;3(1):35-43. doi: 10.1046/j.1467-789X.2002.00054.x [DOI] [PubMed] [Google Scholar]
- 16. Kitaoka HB, Crevoisier XM, Harbst K, Hansen D, Kotajarvi B, Kaufman K. The effect of custom-made braces for the ankle and hindfoot on ankle and foot kinematics and ground reaction forces. Arch Phys Med Rehabil. 2006;87(1):130-135. doi: 10.1016/j.apmr.2005.08.120 [DOI] [PubMed] [Google Scholar]
- 17. Mayich DJ, Novak A, Vena D, Daniels TR, Brodsky JW. Gait analysis in orthopedic foot and ankle surgery—topical review, part 1: principles and uses of gait analysis. Foot Ankle Int. 2014;35(1):80-90. doi: 10.1177/1071100713508394 [DOI] [PubMed] [Google Scholar]
- 18. Norvell DC, Ledoux WR, Shofer JB, et al. Effectiveness and safety of ankle arthrodesis versus arthroplasty: a prospective multicenter study. J Bone Joint Surg Am. 2019;101(16):1485-1494. doi: 10.2106/JBJS.18.01257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Owens JG, Blair JA, Patzkowski JC, Blanck RV, Hsu JR. Return to running and sports participation after limb salvage. J Trauma Inj Infect Crit Care. 2011;71(1):S120-S124. doi: 10.1097/TA.0b013e3182219225 [DOI] [PubMed] [Google Scholar]
- 20. Patzkowski JC, Blanck RV, Owens JG, et al. ; Skeletal Trauma Research Consortium. Comparative effect of orthosis design on functional performance. J Bone Joint Surg Am. 2012;94(6):507-515. doi: 10.2106/JBJS.K.00254 [DOI] [PubMed] [Google Scholar]
- 21. Patzkowski JC, Blanck RV, Owens JG, Wilken JM, Blair JA, Hsu JR. Can an ankle-foot orthosis change hearts and minds? J Surg Orthop Adv. 2011;20(1):8-18. [PubMed] [Google Scholar]
- 22. Peterson SL, Kingsbury TD, Djafar T, Stewart J, Kuhn KM. Military service members with major lower extremity fractures return to running with a passive-dynamic ankle-foot orthosis: comparison with a normative population. Clin Orthop. 2021;479(11):2375-2384. doi: 10.1097/CORR.0000000000001873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Potter BK, Sheu RG, Stinner D, et al. Multisite evaluation of a custom energy-storing carbon fiber orthosis for patients with residual disability after lower-limb trauma. J Bone Joint Surg Am. 2018;100(20):1781-1789. doi: 10.2106/JBJS.18.00213 [DOI] [PubMed] [Google Scholar]
- 24. Song J, Kane R, Tango DN, et al. Effects of weight loss on foot structure and function in obese adults: a pilot randomized controlled trial. Gait Posture. 2015;41(1):86-92. doi: 10.1016/j.gaitpost.2014.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stevens TT, Hartline JT, Ojo O, et al. Race and insurance status association with receiving orthopedic surgeon-prescribed foot orthoses. Foot Ankle Int. 2021;42(7):894-901. doi: 10.1177/1071100721990343 [DOI] [PubMed] [Google Scholar]
- 26. Stewart J, Djafar T, Miltenberger R, Kingsbury T, Wyatt M. Plantar pressure changes with use of an intrepid dynamic exoskeletal orthosis. J Prosthet Orthot. 2020;32(1):59-64. doi: 10.1097/JPO.0000000000000281 [DOI] [Google Scholar]
- 27. Thomas RH, Daniels TR. Ankle arthritis. J Bone Joint Surg Am. 2003;85(5):923-936. doi: 10.2106/00004623-200305000-00026 [DOI] [PubMed] [Google Scholar]
- 28. Vela SA, Lavery LA, Armstrong DG, Anaim AA. The effect of increased weight on peak pressures: implications for obesity and diabetic foot pathology. J Foot Ankle Surg. 1998;37(5):416-420. doi: 10.1016/S1067-2516(98)80051-3 [DOI] [PubMed] [Google Scholar]
- 29. Zuccarino R, Anderson KM, Shy ME, Wilken JM. Satisfaction with ankle foot orthoses in individuals with Charcot-Marie-Tooth disease. Muscle Nerve. 2021;63(1):40-45. doi: 10.1002/mus.27027 [DOI] [PMC free article] [PubMed] [Google Scholar]





