Abstract
Background
Pregnancy is a complex period that implies many biopsychosocial changes, and the way women adapt to these changes impacts their well-being and the chances of developing mental health problems. During the perinatal period, women have expressed a preference for support delivered on the web. In this regard, interventions such as behavioral activation (BA), which are brief and structured psychosocial interventions, seem particularly suited to be delivered through digital solutions.
Objective
This study aimed to map the literature investigating digital BA interventions deployed during the perinatal period. We paid particular attention to the methodological underpinnings of the studies, the potential impact of BA interventions on symptoms other than depression, and the existence of differences occurring when these interventions were administered during pregnancy versus the postpartum period.
Methods
A systematic search compliant with the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews) guidelines was conducted considering 5 bibliographic databases; reference lists and key journals were also screened by 2 independent authors following a double-blind approach.
Results
A total of 7 studies published between 2013 and 2022 were included. In total, 2 studies were protocols for randomized controlled trials, 5 were empirical studies, and 1 was a qualitative study. All studies focused on the postpartum period, except for 1 that focused on the broader perinatal period. Promising effects on depression symptoms were reported but not on other psychosocial symptoms. Low intervention adherence has emerged, whereas the usability associated with the digital means used to deploy interventions was scarcely addressed; moreover, information on the digital platforms used was poorly reported overall.
Conclusions
Our findings highlight the scarcity and preliminary nature of digital BA interventions deployed during the perinatal period, where the focus seems more on treatment rather than prevention. Moreover, future studies should also consider and address usability and user engagement, given their relevance to intervention efficacy.
Keywords: behavioral activation, eHealth, perinatal care, depression symptoms, scoping review, mobile phone
Introduction
Background
The transition to motherhood is a life-changing experience entailing a series of social, psychological, and hormonal changes, which may be challenging to adapt to and often cause exhaustion, a sense of overwhelm, and fatigue [1,2], thereby directly impacting pregnant and postpartum women’s quality of life and overall well-being. Taken together, these factors define the perinatal period as a high-risk period for women’s mental health [3,4]. The literature provides plenty of evidence on this matter, highlighting how pregnancy is often associated with mood instability [5] and common mental disorders (1%-37%) [6] as well as depression (approximately 25.3%) [6,7] and anxiety (1%-26%) [6]. Depression symptoms during pregnancy, in particular, are among the main predictors of postpartum depression [8]. From a clinical viewpoint, depression during the perinatal period is described as peripartum depression, which consists of an episode of major depression with peripartum onset, satisfying the criteria for either major depression or persistent depressive disorder [9]. The direct association of peripartum depression with the peculiar challenges and bodily changes intrinsic to the perinatal period makes the condition peculiar, thereby determining the need to consider it as a stand-alone disorder [10]. Accordingly, a recent review concluded that peripartum depression “may be distinct from major depressive disorder with respect to symptom severity, hormone contributions, heritability, epigenetic mechanisms, and response to standard and novel treatment interventions” [10].
Considering the detrimental effects that depression symptoms, together with the often associated anxiety and stress symptoms, have on the physical and psychological well-being of both mothers and children [4], it is paramount to take prompt action and minimize the incidence of adverse effects. In this regard, it is important to emphasize that in the present age, beside the abovementioned challenges, the perinatal period can be experienced very differently by women. Physiological pregnancies and artificially induced ones, that is, pregnancies reached through assisted reproductive techniques (ARTs; eg, in vitro fertilization and intracellular sperm injection), can particularly be distinguished between in this regard. As a matter of fact, ARTs are infertility treatment that determine a series of specific challenges that differentiate them from physiological pregnancies, such as increased psychological distress, loss of self-esteem, relationship problems, disruption in personal life, and even economic problems linked to the substantial expenses they entail [11-14]; this determines a greater psychological toll compared with physiological pregnancies. Moreover, ART are associated with an increased risk of miscarriage [15,16], which could further hinder women’s adaptation capacities; although having reached pregnancy, many women might still be mourning their previous interrupted ones [17]. For these reasons, physiological pregnancies, ART-induced pregnancies, and consequent postpartum periods must be deemed as very different experiences. Accordingly, it is paramount to account for their peculiarities in clinical practice by tailoring interventions specifically to their respective needs.
In this regard, contrary to women undergoing ART who are kept under greater clinical scrutiny by default, access to mental health care for women at large going through the perinatal period is severely limited by a series of logistic challenges; for instance, time constraints, lack of information about services, and social stigma are indicated by women themselves as the main obstacles hindering their ability and willingness to seek help [18-20]. However, such barriers can be overcome through the implementation of digital interventions; the literature not only highlights a clear preference for support delivered through a web-based format expressed by women experiencing mental health issues during the postpartum period [21-23] but also underscores how such treatments are effective in decreasing the severity of mood disorders, both during pregnancy and the postpartum period [24-26].
In this regard, behavioral activation (BA) interventions, which in their modern protocols can be counted among the so-called “third wave” cognitive and behavioral therapies [27], seem particularly suited to be implemented digitally. BA is a brief, structured, and empirically supported psychotherapeutic approach developed as a stand-alone treatment for depression [28]. Laying its foundation on the behavioral model, it is mainly aimed at increasing engagement in adaptive and pleasurable activities and decreasing engagement in maladaptive behaviors through the systematic targeting of patients’ escape and avoidance strategies [29,30]. The focus is exclusively on the promotion of behavioral change, stimulated by using a series of different strategies such as self-monitoring, activity scheduling, values and goals assessment, and skills training. The ultimate goal is to encourage patients to act in line with their values, allowing them to reconnect with sources of positive reinforcement and fostering a sense of well-being, agency, and mastery through the reconstruction of a routine [30]. Both the efficacy and effectiveness of in-person BA as a treatment specific for depression have been widely proven [31], and the literature also provides promising evidence regarding its efficacy in perinatal depression, both in terms of improved outcomes [29,32] and of engagement and satisfaction [33]. The distinctive features of BA render it a parsimonious, transportable, simple to implement, and cost-effective treatment, suitable to be administered by both specialists and generic mental health professionals [34] in a wide range of formats such as web-based interventions or self-guided smartphone apps [29]. Encouraging findings already exist on the feasibility of internet-based BA interventions for adults with symptoms of depression [35]; therefore, it seems appropriate to further investigate the topic within the context of perinatal care. Nonetheless, it is worth mentioning that evidence on the efficacy and specific features of BA interventions during the perinatal period is still scarce and inconspicuous. For instance, there is some initial evidence highlighting that the effect of in-person BA on depression symptoms might also generalize to other symptoms, thereby leading to the simultaneous reduction of the highly associated anxiety and stress [29,30,32]. However, studies investigating the efficacy of BA interventions have classically focused on the mere reduction of depression symptoms; thus, further research is needed to deepen our knowledge and provide solid evidence on its effects on other concurrent mental health conditions. Similarly, although as previously mentioned, existing studies regarding digital interventions show promising results, and it must be noted that it is a fairly new field and is still under development; therefore, further studies are needed in this area as well [35,36]. Accordingly, this scoping review aimed to map the available literature on digital BA interventions administered specifically during the perinatal period. Scoping reviews serve to bring together “literature in disciplines with emerging evidence, as they are suited to addressing questions beyond those related to the effectiveness or experience of an intervention” [37]. Indeed, this methodological approach to literature review allows us to map the range, nature, and extent of existing research evidence on a given topic regardless of the specific study design while also allowing the identification of gaps within the available literature [38]. Accordingly, this scoping review intended to investigate how BA interventions have been deployed through digital solutions, paying particular attention to their methodological underpinnings; a further aim was to assess if studies have considered the potential of digital BA interventions to influence symptoms and conditions other than depression (eg, anxiety and stress symptoms, overall quality of life, and well-being). This was expected to provide insights useful for refining the existing digital BA interventions. Moreover, it was also expected to support the further development of effective prevention and intervention programs divulged through digital solutions for women in the perinatal period, thereby supporting both their own and their children’s well-being.
Objectives
The specific research questions guiding this scoping review were as follows: (1) How have BA interventions been structured (eg, intervention length, number of modules, topics considered, and guided vs unguided interventions) to be administered through digital means? (2) Has a specific BA protocol been followed? If so, on what BA protocol were the interventions based? [39] (3) What were the main barriers, including both participants’ concerns and issues given by the digital tool itself, in implementing BA interventions through digital means? (4) Were digital BA interventions able to influence psychosocial symptoms other than depression? (5) Have they willingly been used to influence symptoms other than depression? and (6) Are there differences in the BA interventions administered during the antenatal period versus the postnatal period?
Methods
This scoping review was conducted in compliance with the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews) guidelines (refer to Table S1 in Multimedia Appendix 1 [40-47]).
Eligibility Criteria
The inclusion criteria for this study were as follows: (1) considering BA interventions administered through digital means (web-based, smartphone-based, telehealth, etc), (2) inclusion of women aged ≥18 years, (3) focusing on the peripartum period (both antenatal and post partum), (4) inclusion of women who were experiencing or had experienced a physiological pregnancy (up to 1 year post partum), and (5) being written in English.
The exclusion criteria were as follows: (1) being a review article, (2) focusing on or including women who were experiencing or had experienced artificially induced pregnancy, and (3) focusing on or including women with preexisting medical conditions.
In line with the intent of scoping reviews, that is, mapping the available literature regardless of its specific study design [38], no restrictions were imposed on the study design. Accordingly, any type of study satisfying the criteria mentioned above was included, as the intent was to provide an overview of existing literature that is informative of what has already been done (eg, already published studies), what is expected to be done in the near future (eg, study protocols), and what is still lacking entirely or needs further investigation (ie, literature gaps). For the same reason, studies relying on secondary data were also included if they provide information that adds up to the primary analysis, thereby allowing a more in-depth understanding of the intervention evaluated and, more broadly, of the state of the art.
Search Strategy
A total of 5 electronic bibliographic databases, namely, Web of Science, PubMed, PsycINFO, Embase, and CINAHL, were screened in April 2022 to identify studies that met the eligibility criteria. No search restrictions were applied. Reference lists were also scanned, and a handsearching of key journals (ie, Journal of Medical Internet Research and Telemedicine and e-Health) was performed to ensure a comprehensive literature search. Studies were identified using the following search strings: (behavioral activation OR behavioral activation OR activity scheduling OR pleasant events OR pleasant event) AND (digital interventions OR telehealth OR telemedicine) AND (perinatal depression OR antenatal depression OR postpartum depression OR perinatal mental health); (behavioral activation) AND (web-based interventions OR e-health OR internet-based interventions) AND (perinatal OR postnatal OR prenatal OR antenatal OR postpartum OR maternal OR pregnant OR pregnancy).
Study Screening and Data Charting Process
A double-blind screening of titles and abstracts was performed using the ASReview Lab software [48] by 2 authors (EM and DP), who also manually inspected the software results and then performed the subsequent full-text screening in a double-blind fashion. Any doubts or disagreements were resolved by consulting a third author (SS). Similarly, 2 independent authors (EM and DP) performed the data extraction in a double-blind fashion. Any disagreement was resolved by consulting a third author (SG). The extracted data, collected in an Excel (Microsoft Corporation) sheet, were as follows: study characteristics (digital object identifier; first author’s name; publication year; country of origin; study design; study aim; time points for data collection; outcomes considered by the included study; measurement tools used to evaluate the outcomes; main results; reason for dropout, if applicable; participants’ feedback on the intervention, if present; and type of comparator, if present), sample characteristics (sample size, age, ethnicity, occupation, marital status, educational level, income, clinical characteristics, gestational week or postpartum period, and inclusion and exclusion criteria for the participants), and BA intervention characteristics (description of the BA protocol, original BA protocol from which the new one was derived, if and how the protocol was modified, intervention length and structure, digital means used to administer the BA, and intervention delivery format).
Results
Search Results
The database search yielded 194 studies (Figure 1). Following duplicate removal, the titles and abstracts of 160 studies were screened; 141 studies were removed, resulting in 19 studies whose full text was screened in accordance with the inclusion and exclusion criteria. Of these 19 studies, 5 (26%) were eventually included. The database search was integrated with a manual search of key journals and the screening of reference lists, through which 7 more studies were identified for full-text screening; only 2 studies complied with the inclusion criteria. Taken together, 7 studies were ultimately included in this scoping review. Excluded studies with reasons for exclusion are reported in Tables S2, S3, and S4 in Multimedia Appendix 1.
Figure 1.
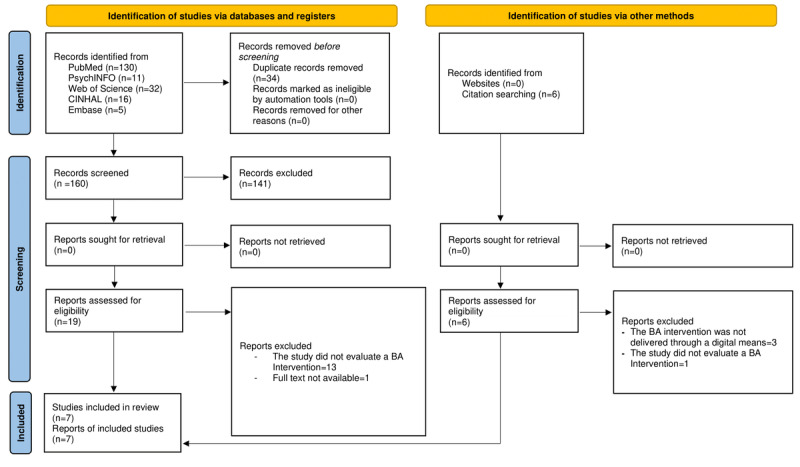
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 flow diagram, including searches of databases, registers, and other sources. BA: behavioral activation.
Studies’ Characteristics
The aims and design of the studies are reported in Table 1, and the studies’ main outcomes are summarized in Figure 2. The included studies were published between 2013 and 2022, of which 2 are randomized controlled trials (RCTs) [41,42] and 2 are protocols for RCTs [43,44]. Moreover, 2 studies are secondary analyses conducted on the RCT by O’Mahen et al [42], 1 is a secondary analysis focused on a subsample of the original sample [45], and 1 is a secondary analysis focused only on follow-up data of the total sample [46]. Finally, 1 is a qualitative study, which included participant-level analyses as well as 2 case studies [47]. Both the studies by Singla et al [44,47] relate to the same broad ongoing study. Only the 2 protocol studies [43,44] preregistered their clinical trials. All included studies were focused on evaluating the efficacy or effects of a digital BA intervention, except for 1 study [45], which investigated the processes underlying digital BA’s efficacy. The outcomes considered by the included studies are summarized in Figure 2. Although all interventions were developed to target depression symptoms, coherently with the intents of BA, studies have also marginally considered other maternal variables such as anxiety symptoms (n=3) [43,44,46], parental stress (n=1), quality of life (n=1) [43], social support (n=4) [42,44,46], work and social functioning (n=3) [42,45,46], and mother-child bonding (n=3) [42-44]. Moreover, only Obikane et al [43] and Singla et al [44] included child-related variables in their protocol study, such as maternal psychological and physical aggression toward the child (n=1) [43], the child’s physiological (n=1) [43] or mental development (n=1) [44], and the level of health care services used for the child (n=2) [43,44] (Figure 2; Table S5 in Multimedia Appendix 1). The included studies also marginally evaluated the intervention-related outcomes. Specifically, 1 study protocol [44] reported that they will evaluate therapy quality as well as homework completion and the frequency with which the intervention sessions are followed. Instead, 3 studies [44-46] evaluated intervention adherence, operationalized as the number of intervention modules opened and completed [45,46]. Only 2 studies specifically considered interventions’ feasibility (ie, if the intervention is feasible for further testing) and acceptability (ie, how well the intervention meets the needs of the target population) [41,43]. Finally, only 1 study [43], a study protocol, reported that the assessment of usability will be conducted through the System Usability Scale [49].
Table 1.
Aims and characteristics of the studies.
| Study | Study type | Study aim |
| Bagnall [46], 2014 | Long-term follow-up of RCTa (doctoral dissertation) |
|
| Obikane et al [43], 2021 | Protocol for RCT |
|
| O’Mahen et al [41], 2014 | RCT |
|
| O’Mahen et al [42], 2014 | RCT |
|
| O’Mahen et al [45], 2017 | Secondary analysis from the study by O’Mahen et al [42] |
|
| Singla et al [44], 2021 | Protocol for 4-arm RCT (noninferiority trial) |
|
| Singla et al [47], 2022 | Qualitative study |
|
aRCT: randomized controlled trial.
bBA: behavioral activation.
Figure 2.
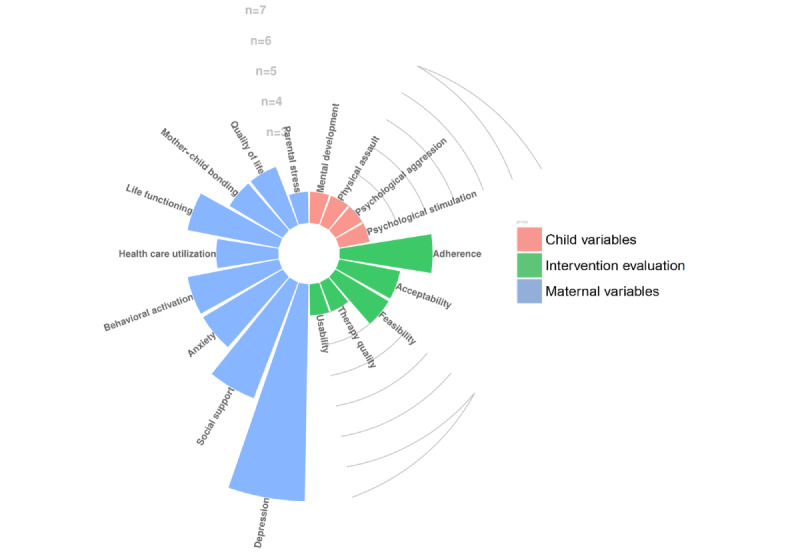
Circular bar plot of the main outcomes of the studies. n=frequency of the outcomes reported by the included studies.
Sample Characteristics
The sample characteristics and studies’ sample-related inclusion criteria are summarized in Table 2. All participants were postpartum women, except for those in the study by Singla et al [44,47], which focused on both antenatal and postnatal women. All studies used the Edinburgh Postnatal Depression Scale to include women in their study, albeit relying on different cutoff values. Moreover, in their 2014 study, O’Mahen et al [42,45,46] had supplemented the Edinburgh Postnatal Depression Scale with a telephone interview aimed at ensuring that women satisfied the criteria for major depressive disorder according to the International Classification of Diseases, Tenth Revision. With regard to demographic information (Table S6 in Multimedia Appendix 1), information on the sample’s age was reported by only 2 studies [42,47], the sample’s ethnicity by 3 studies [42,44,45], occupation by 4 studies [41,42,45,47], educational level by 3 studies [41,42,45], income by 2 studies [42,45], marital status by 4 studies [41,42,45,47], and the total number of children by 3 studies [41,42,45]. Finally, with regard to the studies’ sample sizes, the 2 protocol studies included [43,44] stated that they will include samples whose numerosity will be based on preliminary power analyses, and all the other included studies reported small sample sizes. Only 1 study [41] reported a larger sample size (<150); nonetheless, changes in the sample’s numerosity from baseline to intervention end point and follow-up are unclear.
Table 2.
Sample characteristics.
| Study | Sample, N | Perinatal period | Inclusion criteria | Exclusion criteria |
| Obikane et al [43], 2021 | Over 75 per group (4 groups: estimated) | Post partum |
|
|
| O’Mahen et al [41], 2013 | EGa: 164; CGb: 134 | Post partum |
|
|
| O’Mahen et al [42], 2014; Bagnall [46], 2014 | EG: 41; CG: 42 | Post partum |
|
|
| O’Mahen et al [45], 2017 | 32 (subsample of the study by O’Mahen et al [42]) | Post partum |
|
|
| Singla et al [44], 2021 | 342 per group (4 groups; estimated) | Perinatal |
|
|
| Singla et al [47], 2022 | 23 | Perinatal |
|
|
aEG: experimental group.
bCG: control group.
cEPDS: Edinburgh Postnatal Depression Scale.
dMDD: major depression disorder.
Digital Interventions’ Characteristics
The characteristics of the different interventions are reported in Table 3 and Table S7 in Multimedia Appendix 1. All interventions were based on validated BA protocols (ie, validated and manualized intervention protocols); however, none extensively explained the changes made to adapt the intervention to either the population or the digital setting. Studies’ intervention content structuring is quite consistent, with differences given mainly by the inclusion of optional modules [42,46] or the possibility to customize sessions [41]. Furthermore, in the qualitative study by Singla et al [47], the intervention protocol deployed during the COVID-19 lockdown was adapted to account for pandemic-related stressors and participants’ perceived racial injustice in a subsample of ethnic minority participants.
Table 3.
Characteristics of the interventions.
| Study | Intervention name | Length (weeks), total number of sessions | Guided versus unguided | Guided—description | Digital means | Intervention delivery format |
| Obikane et al [43], 2021 | SmartMama | 12, 12 | Guided (psychotherapists) |
|
Web-based app for smartphones |
|
| O’Mahen et al [41], 2013 | Postnatal iBAa | 15, 11 | Unguided |
|
Web based (Netmums site) |
|
| O’Mahen et al [42], 2013; O’Mahen et al [45], 2014; Bagnall [46], 2014 | NetmumsHWD | 17, 12 | Guided (mental health workers) |
|
Web based (Netmums site) |
|
| Singla et al [44], 2021 | Behavioral activation | 6-8, 6-8 | Guided (nonspecialists and specialists) |
|
Telemedicine |
|
| Singla et al [47], 2022 | Behavioral activation | Not reported, 8 | Guided (trained psychologists) |
|
Telemedicine |
|
aiBA: internet-based Behavioral Activation.
bN/A: not applicable.
All interventions were guided, except for an unguided one [41] that, nonetheless, included a sort of “technical” support, whereby psychologists or specialized health visitors gave advice for homework completion and answered participants’ questions on the program material; no further information was reported. With regard to guided interventions, only O’Mahen et al [42] and Singla et al [44,47] reported information on how supporters guiding them had been trained and monitored through supervision by expert clinicians. Moreover, in the studies by Singla et al [44,47] and O’Mahen et al [42], authors monitored and evaluated supporters through independent fidelity raters who listened to recordings of the sessions. All 3 studies by O’Mahen et al [41,42,45] and the related secondary analysis by Bagnall [46] considered the web-based Netmums BA program; both the studies by Singla et al [44,47] relied on telemedicine, whereas only Obikane et al [43] reported the development of a web-based BA intervention that can be deployed through smartphones. Obikane et al [43] further reported that they will ensure data confidentiality by temporarily storing data in the Amazon Elastic Compute Cloud system and will only later move them in a password-protected computer. No other study reported information referred to data privacy and storage.
Results of Individual Evidence and Overall Synthesis
The main results of the studies, referring to both clinical outcomes and intervention-related outcomes, are summarized in Table 4. Overall, these studies consistently showed a significant intervention effect on depression symptoms. However, following multiple imputation analyses, the results of the study by O’Mahen et al [42] showed that such differences were not significant between the intervention and control groups. The same authors reported a trend for reduced anxiety symptoms and improved work and social functioning compared with the control condition at the intervention end point; however, this trend was not statistically significant. Accordingly, in the secondary follow-up analysis by Bagnall [46], the intervention effect was not significantly different between groups at any time point. Notwithstanding, the 2 case studies reported by Singla et al [47] were useful in highlighting the subjective experience of participants and their perceived benefits of the interventions. In both case studies, participants reported an improvement in communication skills that favored the support between them and their husbands by sharing child-related responsibilities. Moreover, at the end of the intervention, participants reported better associating their mood with what was happening in their lives, thereby voluntarily redirecting their attention toward value-based activities that would improve their mood. At the intervention end point, one of the women self-reported remission in both depression and anxiety symptoms, whereas the other reported that she was then able to embrace her past traumas, triggered by postpartum-related stressors, and thereby requested a referral to a clinical professional. The secondary analysis performed by O’Mahen et al [45] was also useful in highlighting the relevant processes underlying the intervention that were associated with its efficacy. Specifically, the authors observed that slightly more than half of the sample (18/32, 51%) showed at least one sudden improvement or gain in depression symptoms, even though these were often followed by a depression spike; however, participants showing these sudden improvements reported much reduced depression symptoms at intervention end point and also reported having followed more web-based intervention modules compared with those who had not reported such improvements. The same participants had also talked about more specific and concrete topics during the telephone sessions preceding the sudden gains [45].
Table 4.
Main results of the studies.
| Study | Assessment time points | Clinical outputs | Intervention-related outputs |
| Bagnall [46], 2014 |
|
|
|
| Obikane et al [43], 2021 |
|
|
|
| O’Mahen et al [41], 2013 |
|
|
|
| O’Mahen et al [42], 2014 |
|
|
|
| O’Mahen et al [45], 2017 |
|
|
|
| Singla et al [44], 2021 |
|
|
|
| Singla et al [47], 2022 |
|
|
|
aT0: Time 0.
bT1: Time 1.
cT2: Time 2.
dT3: Time 3.
eBA: behavioral activation.
fN/A: not applicable.
gT4: Time 4.
Regarding the interventions’ feasibility, acceptability, and overall intervention adherence, the available information is limited. However, although studies explicitly evaluated these factors, their results on dropout rates and adherence seemingly suggest reduced acceptability. The studies by O’Mahen et al [41,42] provided information in this regard, reporting that dropouts were quite high and that there was limited participation in the real-time “online clinics” as well as in the chat rooms made available for mums to talk with each other. Moreover, limited intervention adherence was highlighted by the modest median completion rate of the intervention sessions. In this regard, it is noteworthy that reduced adherence was associated with women’s lower socioeconomic level, reduced social support as well as reduced work and social functioning, and with attending school or working [42]. Nonetheless, based on participants’ feedback, what had favored acceptability and adherence was the convenient delivery of the intervention’s content and the ease experienced in following the program; however, the latter is hindered when interventions include large number of sessions and activities that women are requested to follow [41]. Accordingly, O’Mahen et al [41,42] had simplified their intervention from their 2013 versus 2014 study. Moreover, contrary to what was reported by O’Mahen et al [42] regarding the predictors of intervention adherence, the study by Bagnall [46] did not identify any significant predictors (ie, depression symptoms level, level of BA, social support, and household income) of intervention adherence or the predictive role of assessments’ adherence to the intervention outcomes (eg, depression symptoms). The latter study was primarily focused on investigating participants’ adherence to follow-up assessments (which might thus better fit within the broader construct of “intervention feasibility” more than within that of “adherence”). In this regard, they reported that outreach helped improve participation in the follow-up assessments. No study investigated the programs’ usability; however, 1 of the included study protocols [43], as previously reported, is expected to provide further information in this regard.
Discussion
Principal Findings
This scoping review aimed to map the available literature on digital BA interventions administered during the perinatal period. The research questions guiding this work have focused on the interventions’ methodological underpinnings as well as on the interventions’ targets, referring to the specificities of the population considered as well as to the symptoms experienced by the latter.
Regarding research questions (4) Were digital BA interventions able to influence psychosocial symptoms other than depression? and (5) Have they willingly been used to influence symptoms other than depression? in line with expectations, they seem to be overall promising in reducing depression symptoms among postpartum women; however, owing to the limited literature available, it is not possible to draw definitive conclusions in this regard. Moreover, although an in-person BA intervention administered to pregnant women was effective in reducing anxiety symptoms [32], the sole concluded trial included in this review that had evaluated anxiety symptoms [42,46] reported no significant intervention effect. Accordingly, to date, it is not possible to draw complete conclusions on the generalizability of the efficacy of digital BA interventions on psychosocial variables (eg, anxiety and stress symptoms and quality of life) other than depression symptoms. This is mostly owing to the above-mentioned marginal investigation of these symptoms.
Referring, instead, to research question (6) Are there differences in the BA interventions administered during the antenatal period versus the postnatal period? it is noteworthy that of all the included studies, most [41-43,45,46] focused solely on the postnatal period by considering women who had recently given birth, whereas none specifically focused on pregnant women and, therefore, on the antenatal period. However, one of the included protocol studies [44] reported that it foresees the future inclusion of both antenatal and postnatal women to compare intervention efficacy as a function of the perinatal period during which it is deployed. Thus, overall, it is not possible to answer the research question focused on the efficacy of digital BA interventions deployed during the antenatal period versus the postnatal period. The lack of digital interventions administered during the antenatal period represents a limitation of the available literature in terms of both evidence-based treatments and prevention programs. This is relevant, especially considering the high prevalence of depressive symptoms during pregnancy (between 15% and 65% [50]) and of the interrelated [51,52] anxiety (between 18% and 24% [53]) and stress symptoms (low-moderate symptoms level 78% [54]). Altogether, these hinder women’s quality of life [55], with repercussions on the child’s development and well-being [56-58], while further significantly increasing the risk of postpartum depression [8,59]. These results might be particularly insightful if read through the lens of the Stepped Care model [60]. This specific approach to health care advocates for a highly collaborative approach among primary and secondary mental health services to choose and deliver the most appropriate treatment, ranging from primary low-burden care to more intensive and specialized care on the basis of patients’ specific level of need and distress, which should ultimately improve access to health care for patients on one hand and, on the other hand, the efficiency and cost-effectiveness of treatments themselves [60]. Within this theoretical framework, prevention programs can be regarded as primary health services; therefore, research on the feasibility and effectiveness of digital interventions within the perinatal period should be encouraged; such treatments are expected to be of great benefit for both women in the perinatal period and the health care system on the whole, as they should foster scalability and thereby reduce health care costs [61,62].
Similarly, with regard to overcoming the broader barriers already reported in the literature, limiting access to mental health care programs (eg, time constraints, lack of information about services, and social stigma [18-20]), the creation and implementation of acceptable and effective digital interventions would also be advantageous in terms of both time and expenses for both the patients and the health care specialists. Moreover, through the advent of social media platforms and the possibility to create ad hoc websites, digital interventions can be made known and spread with greater ease, thereby allowing the extension of care to patients living in hard-to-reach areas. These same premises might also be associated with a reduction in the social stigma surrounding health care seeking by, on the one hand, normalizing the reliance on psychological programs and, on the other hand, allowing the maintenance of privacy within one’s social environment. This review also attempted to identify the logistic, social, and pragmatic barriers specifically associated with digital BA interventions. Focusing, instead, on research question (3) What were the main barriers, including both participants’ concerns and issues given by the digital tool itself, in implementing BA interventions through digital means? the data reported here do not allow to gather insights or formulate suggestions regarding the existence and potential overcoming of barriers within the context of digital BA interventions during the perinatal period. In fact, only 1 study [47] specifically addressed the intervention’s barriers, raising some concerns about the maintenance of privacy during the intervention; however, this might be strictly linked to the use of telemedicine in general rather than on digital BA interventions specifically.
Regarding the remaining research questions, namely, (2) Has a specific BA protocol been followed? if so, on what BA protocol were the interventions based? [39] and (1) How have BA interventions been structured (eg, intervention length, number of modules, topics considered, and guided versus unguided interventions) to be administered through digital means? it is worth highlighting that all interventions were based on validated BA protocols [63], but no extensive explanation of the changes made to the original protocols were reported. Similarly, scarce information was reported on the role of the guidance in the guided interventions as well as on the specificities of the digital means used to administer the interventions. This limits the reproducibility of studies as well as the advancement of the matter, as it restricts the possibility of identifying the benefits and limitations of the different digital BA interventions. Likewise, all the included studies reported limited information on how the interventions’ content and home assignments were implemented and deployed. However, a thorough reporting of the choices made on the intervention content and structuring, of the specificities of the technological components used to implement the intervention, and of the potential drawbacks that might have emerged from the trials is needed to foster information exchange within the scientific community. This is particularly relevant, considering their value for the feasibility and efficacy of the intervention as well as for overall usability. Including such information in trial reports would ultimately contribute to the broader research field. In line with this thought, the work by O’Mahen et al [41,42] is noteworthy with regard to the investigation of the feasibility of interventions, as they reported refining their intervention structuring in line with participants’ feedback and then retesting its efficacy. In this regard, although none of the studies provided reasons for choosing a certain number of sessions composing the interventions, O’Mahen et al [41,42] reported reducing the number of core sessions while including some optional modules [42]—a decision based on participants’ feedback stating that they could not “keep up” with the intervention [41]. This particular mode of action is what seems to be lacking and should instead be promoted, as it provides information on the interventions’ specific structures, thereby favoring scientific exchange and, ultimately, the advancement of the matter. Future studies might benefit from including qualitative evaluations of the interventions’ experience and overall usability, for instance, by foreseeing the use of semistructured interviews at the end of the intervention [64]. In this regard, it should be stressed that usability was not evaluated by any of the concluded research studies included in this review, although the criticality of adherence to interventions was highlighted as it emerged in previous studies [65,66]. Usability is conceptualized as the output of the interaction between the user and the tools (eg, website) used [67] and includes 5 main concepts [68]: ease of use, intended as learnability, experienced by users learning how to use a digital tool; the efficiency with which users interact with the digital tool; the memorability of how to use a digital tool to which the user has been already exposed; the errors users make, intended as the number of trials needed to make a certain action correctly; and the perceived users’ satisfaction with the user experience. The latter further includes aspects relevant to user engagement, including the affective, cognitive, and behavioral response of the user to the digital tool [69]. In this regard, Bagnall [46], referring to the nonpredictive effect of intervention adherence on the intervention outcomes, discussed that beyond adherence, it might indeed be the level of engagement with the intervention, intended as behavioral participation, to be particularly relevant in influencing intervention efficacy. In line with this, O’Mahen et al [42] highlighted that intervention acceptability as well as adherence, as reported by women, was favored by the convenient delivery of the intervention’s content and the ease felt in following the program, which are all aspects relevant to usability. This further highlights the importance of accounting for usability facets when investigating the efficacy of digital interventions, which emerged in this review as a strong limitation of the literature on digital BA interventions deployed during the perinatal period. Future studies should, therefore, more carefully and consistently account for and thoroughly explain the results of the user experience while also accounting for user engagement [70].
Overall, the information retrieved through this scoping review does not allow to provide specific suggestions for the implementation of interventions. However, the gaps identified in the available literature can be useful for refining existing protocols and supporting the design of future interventions. Specifically, there has emerged a need to substantially investigate both the usability and user engagement associated with these digital interventions to better understand and refine them. The human-computer interaction aspects of these interventions, as of today, seem only marginally considered but should instead be central in future research, as they define the “setting” in which interventions take place. It should be noted that the existing literature does provide guidelines [70] or models [71] that should be followed in future trials to support adherence and engagement, as they are pivotal for the efficacy of interventions. Moreover, greater flexibility in the structuring of interventions (ie, the number of sessions and time required to complete each session) is recommended, as it would support acceptability. These aspects might be particularly valuable, considering the high attrition rate of these interventions, which had already been pointed out by existing literature and was coherently reported by the included studies as well [66].
Conclusions
Taken together, the available literature examined was useful in highlighting the potential, and also the immaturity, of the research field on digital BA interventions, while promptly stressing the need to develop interventions specifically targeting pregnant women. To address this gap, future research should focus on addressing such limitations, paying particular attention to the investigation of the feasibility, acceptability, and usability of interventions. Moreover, future studies should invest in the development and evaluation of digital prevention programs deployed during pregnancy.
Abbreviations
- ART
assisted reproductive technique
- BA
behavioral activation
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- PRISMA-ScR
Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews
- RCT
randomized controlled trial
Supplementary materials.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Cheng CY, Chou YH, Wang P, Tsai JM, Liou SR. Survey of trend and factors in perinatal maternal fatigue. Nurs Health Sci. 2015 Mar;17(1):64–70. doi: 10.1111/nhs.12149. https://pubmed.ncbi.nlm.nih.gov/24835296/ [DOI] [PubMed] [Google Scholar]
- 2.Nelson AM. Transition to motherhood. J Obstet Gynecol Neonatal Nurs. 2003 Jul;32(4):465–77. doi: 10.1177/0884217503255199. https://pubmed.ncbi.nlm.nih.gov/12903696/ S0884-2175(15)34101-0 [DOI] [PubMed] [Google Scholar]
- 3.Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, Holmes W. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Organ. 2012 Feb 01;90(2):139G–49G. doi: 10.2471/BLT.11.091850. https://europepmc.org/abstract/MED/22423165 .BLT.11.091850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Howard LM, Khalifeh H. Perinatal mental health: a review of progress and challenges. World Psychiatry. 2020 Oct;19(3):313–27. doi: 10.1002/wps.20769. https://europepmc.org/abstract/MED/32931106 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li H, Bowen A, Bowen R, Balbuena L, Feng C, Bally J, Muhajarine N. Mood instability during pregnancy and postpartum: a systematic review. Arch Womens Ment Health. 2020 Feb;23(1):29–41. doi: 10.1007/s00737-019-00956-6. https://pubmed.ncbi.nlm.nih.gov/30834475/ 10.1007/s00737-019-00956-6 [DOI] [PubMed] [Google Scholar]
- 6.Jha S, Salve HR, Goswami K, Sagar R, Kant S. Burden of common mental disorders among pregnant women: a systematic review. Asian J Psychiatr. 2018 Aug;36:46–53. doi: 10.1016/j.ajp.2018.06.020. https://pubmed.ncbi.nlm.nih.gov/29966886/ S1876-2018(18)30239-9 [DOI] [PubMed] [Google Scholar]
- 7.Gelaye B, Rondon MB, Araya R, Williams MA. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry. 2016 Oct;3(10):973–82. doi: 10.1016/S2215-0366(16)30284-X. https://europepmc.org/abstract/MED/27650773 .S2215-0366(16)30284-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hutchens BF, Kearney J. Risk factors for postpartum depression: an umbrella review. J Midwifery Womens Health. 2020 Jan;65(1):96–108. doi: 10.1111/jmwh.13067. https://pubmed.ncbi.nlm.nih.gov/31970924/ [DOI] [PubMed] [Google Scholar]
- 9.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 5th edition. Washington, DC, USA: American Psychiatric Association; 2013. [Google Scholar]
- 10.Batt MM, Duffy KA, Novick AM, Metcalf CA, Epperson CN. Is postpartum depression different from depression occurring outside of the perinatal period? A review of the evidence. Focus (Am Psychiatr Publ) 2020 Apr;18(2):106–19. doi: 10.1176/appi.focus.20190045. https://europepmc.org/abstract/MED/33162848 .FOC_20190045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Valoriani V, Lotti F, Lari D, Miccinesi G, Vaiani S, Vanni C, Coccia ME, Maggi M, Noci I. Differences in psychophysical well-being and signs of depression in couples undergoing their first consultation for assisted reproduction technology (ART): an Italian pilot study. Eur J Obstet Gynecol Reprod Biol. 2016 Feb;197:179–85. doi: 10.1016/j.ejogrb.2015.11.041. https://pubmed.ncbi.nlm.nih.gov/26773309/ S0301-2115(15)00440-6 [DOI] [PubMed] [Google Scholar]
- 12.Monga M, Alexandrescu B, Katz SE, Stein M, Ganiats T. Impact of infertility on quality of life, marital adjustment, and sexual function. Urology. 2004 Jan;63(1):126–30. doi: 10.1016/j.urology.2003.09.015. https://pubmed.ncbi.nlm.nih.gov/14751363/ S0090429503009993 [DOI] [PubMed] [Google Scholar]
- 13.Peterson BD, Pirritano M, Christensen U, Schmidt L. The impact of partner coping in couples experiencing infertility. Hum Reprod. 2008 May;23(5):1128–37. doi: 10.1093/humrep/den067. https://pubmed.ncbi.nlm.nih.gov/18325885/ den067 [DOI] [PubMed] [Google Scholar]
- 14.Schmidt L. Psychosocial burden of infertility and assisted reproduction. Lancet. 2006 Feb 04;367(9508):379–80. doi: 10.1016/S0140-6736(06)68117-8. https://pubmed.ncbi.nlm.nih.gov/16458748/ S0140-6736(06)68117-8 [DOI] [PubMed] [Google Scholar]
- 15.Wang L, Wang L, Yang X, Jin P, Zhang R, Jiang Y, Zhang X. Risk factors related to early pregnancy loss in fresh IVF/ICSI: an analysis of 954 embryo transfer cycles. Medicine (Baltimore) 2022 Aug 26;101(34):e30166. doi: 10.1097/MD.0000000000030166.00005792-202208260-00023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bu Z, Hu L, Su Y, Guo Y, Zhai J, Sun YP. Factors related to early spontaneous miscarriage during IVF/ICSI treatment: an analysis of 21,485 clinical pregnancies. Reprod Biomed Online. 2020 Feb;40(2):201–6. doi: 10.1016/j.rbmo.2019.11.001. https://pubmed.ncbi.nlm.nih.gov/31883882/ S1472-6483(19)30800-4 [DOI] [PubMed] [Google Scholar]
- 17.Malham S. The mental health effects of assisted reproductive technology. East Carolina University. 2022. [2022-10-31]. https://thescholarship.ecu.edu/handle/10342/10829 .
- 18.Hadfield H, Wittkowski A. Women's experiences of seeking and receiving psychological and psychosocial interventions for postpartum depression: a systematic review and thematic synthesis of the qualitative literature. J Midwifery Womens Health. 2017 Nov;62(6):723–36. doi: 10.1111/jmwh.12669. https://pubmed.ncbi.nlm.nih.gov/29210501/ [DOI] [PubMed] [Google Scholar]
- 19.Jones A. Help seeking in the perinatal period: a review of barriers and facilitators. Soc Work Public Health. 2019;34(7):596–605. doi: 10.1080/19371918.2019.1635947. https://pubmed.ncbi.nlm.nih.gov/31242074/ [DOI] [PubMed] [Google Scholar]
- 20.Megnin-Viggars O, Symington I, Howard LM, Pilling S. Experience of care for mental health problems in the antenatal or postnatal period for women in the UK: a systematic review and meta-synthesis of qualitative research. Arch Womens Ment Health. 2015 Dec;18(6):745–59. doi: 10.1007/s00737-015-0548-6. https://pubmed.ncbi.nlm.nih.gov/26184835/ 10.1007/s00737-015-0548-6 [DOI] [PubMed] [Google Scholar]
- 21.Ashford MT, Ayers S, Olander EK. Interest in web-based treatments for postpartum anxiety: an exploratory survey. J Reprod Infant Psychol. 2017 Sep;35(4):394–409. doi: 10.1080/02646838.2017.1320364. https://pubmed.ncbi.nlm.nih.gov/29517373/ [DOI] [PubMed] [Google Scholar]
- 22.Lackie ME, Parrilla JS, Lavery BM, Kennedy AL, Ryan D, Shulman B, Brotto LA. Digital health needs of women with postpartum depression: focus group study. J Med Internet Res. 2021 Jan 06;23(1):e18934. doi: 10.2196/18934. https://www.jmir.org/2021/1/e18934/ v23i1e18934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wenze SJ, Miers QA, Battle CL. Postpartum mental health care for mothers of multiples: a qualitative study of new mothers' treatment preferences. J Psychiatr Pract. 2020 May;26(3):201–14. doi: 10.1097/PRA.0000000000000469. https://pubmed.ncbi.nlm.nih.gov/32421291/ 00131746-202005000-00005 [DOI] [PubMed] [Google Scholar]
- 24.Chae J, Kim HK. Internet-based prenatal interventions for maternal health among pregnant women: a systematic review and meta-analysis. Child Youth Serv Rev. 2021 Aug 01;127:106079. doi: 10.1016/j.childyouth.2021.106079. https://psycnet.apa.org/record/2021-68229-001 . [DOI] [Google Scholar]
- 25.Dol J, Richardson B, Murphy GT, Aston M, McMillan D, Campbell-Yeo M. Impact of mobile health interventions during the perinatal period on maternal psychosocial outcomes: a systematic review. JBI Evid Synth. 2020 Jan;18(1):30–55. doi: 10.11124/JBISRIR-D-19-00191. https://pubmed.ncbi.nlm.nih.gov/31972680/ 01938924-202001000-00002 [DOI] [PubMed] [Google Scholar]
- 26.Lee EW, Denison FC, Hor K, Reynolds RM. Web-based interventions for prevention and treatment of perinatal mood disorders: a systematic review. BMC Pregnancy Childbirth. 2016 Feb 29;16:38. doi: 10.1186/s12884-016-0831-1. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-016-0831-1 .10.1186/s12884-016-0831-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hayes SC, Hofmann SG. "Third-wave" cognitive and behavioral therapies and the emergence of a process-based approach to intervention in psychiatry. World Psychiatry. 2021 Oct;20(3):363–75. doi: 10.1002/wps.20884. https://europepmc.org/abstract/MED/34505370 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jacobson NS, Martell CR, Dimidjian S. Behavioral activation treatment for depression: returning to contextual roots. Clin Psychol (New York) 2001;8(3):255–70. doi: 10.1093/clipsy.8.3.255. https://psycnet.apa.org/doiLanding?doi=10.1093%2Fclipsy.8.3.255 . [DOI] [Google Scholar]
- 29.Dimidjian S, Barrera Jr M, Martell C, Muñoz RF, Lewinsohn PM. The origins and current status of behavioral activation treatments for depression. Annu Rev Clin Psychol. 2011;7:1–38. doi: 10.1146/annurev-clinpsy-032210-104535. https://pubmed.ncbi.nlm.nih.gov/21275642/ [DOI] [PubMed] [Google Scholar]
- 30.Kanter JW, Manos RC, Bowe WM, Baruch DE, Busch AM, Rusch LC. What is behavioral activation? A review of the empirical literature. Clin Psychol Rev. 2010 Aug;30(6):608–20. doi: 10.1016/j.cpr.2010.04.001. https://pubmed.ncbi.nlm.nih.gov/20677369/ S0272-7358(10)00050-4 [DOI] [PubMed] [Google Scholar]
- 31.Soucy Chartier I, Provencher MD. Behavioural activation for depression: efficacy, effectiveness and dissemination. J Affect Disord. 2013 Mar 05;145(3):292–9. doi: 10.1016/j.jad.2012.07.023. https://pubmed.ncbi.nlm.nih.gov/22884236/ S0165-0327(12)00542-3 [DOI] [PubMed] [Google Scholar]
- 32.Dimidjian S, Goodman SH, Sherwood NE, Simon GE, Ludman E, Gallop R, Welch SS, Boggs JM, Metcalf CA, Hubley S, Powers JD, Beck A. A pragmatic randomized clinical trial of behavioral activation for depressed pregnant women. J Consult Clin Psychol. 2017 Jan;85(1):26–36. doi: 10.1037/ccp0000151. https://europepmc.org/abstract/MED/28045285 .2016-62045-002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.O'Mahen HA, Grieve H, Jones J, McGinley J, Woodford J, Wilkinson EL. Women's experiences of factors affecting treatment engagement and adherence in internet delivered behavioural activation for postnatal depression. Internet Interv. 2015 Mar;2(1):84–90. doi: 10.1016/j.invent.2014.11.003. https://www.sciencedirect.com/science/article/pii/S2214782914000335 . [DOI] [Google Scholar]
- 34.Ekers D, Richards D, McMillan D, Bland JM, Gilbody S. Behavioural activation delivered by the non-specialist: phase II randomised controlled trial. Br J Psychiatry. 2011 Jan;198(1):66–72. doi: 10.1192/bjp.bp.110.079111. https://pubmed.ncbi.nlm.nih.gov/21200079/ S000712500000903X [DOI] [PubMed] [Google Scholar]
- 35.Huguet A, Miller A, Kisely S, Rao S, Saadat N, McGrath PJ. A systematic review and meta-analysis on the efficacy of internet-delivered behavioral activation. J Affect Disord. 2018 Aug 01;235:27–38. doi: 10.1016/j.jad.2018.02.073. https://pubmed.ncbi.nlm.nih.gov/29649708/ S0165-0327(17)32154-7 [DOI] [PubMed] [Google Scholar]
- 36.Spates CR, Padalino R, Hale AC, Germain CS, Nimmo K, Kohler R. A review of web‐based technology in behavioural activation. Clin Psychol. 2016 Jan 21;20(1):27–35. doi: 10.1111/cp.12087. https://psycnet.apa.org/record/2016-19097-005 . [DOI] [Google Scholar]
- 37.Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015 Sep;13(3):141–6. doi: 10.1097/XEB.0000000000000050. https://pubmed.ncbi.nlm.nih.gov/26134548/ [DOI] [PubMed] [Google Scholar]
- 38.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2007 Feb 23;8(1):19–32. doi: 10.1080/1364557032000119616. https://www.tandfonline.com/doi/abs/10.1080/1364557032000119616 . [DOI] [Google Scholar]
- 39.Lejuez CW, Hopko DR, Acierno R, Daughters SB, Pagoto SL. Ten year revision of the brief behavioral activation treatment for depression: revised treatment manual. Behav Modif. 2011 Mar;35(2):111–61. doi: 10.1177/0145445510390929. https://pubmed.ncbi.nlm.nih.gov/21324944/ 35/2/111 [DOI] [PubMed] [Google Scholar]
- 40.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018 Oct 02;169(7):467–73. doi: 10.7326/M18-0850. https://www.acpjournals.org/doi/abs/10.7326/M18-0850?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .2700389 [DOI] [PubMed] [Google Scholar]
- 41.O'Mahen HA, Woodford J, McGinley J, Warren FC, Richards DA, Lynch TR, Taylor RS. Internet-based behavioral activation--treatment for postnatal depression (Netmums): a randomized controlled trial. J Affect Disord. 2013 Sep 25;150(3):814–22. doi: 10.1016/j.jad.2013.03.005. https://pubmed.ncbi.nlm.nih.gov/23602514/ S0165-0327(13)00230-9 [DOI] [PubMed] [Google Scholar]
- 42.O'Mahen HA, Richards DA, Woodford J, Wilkinson E, McGinley J, Taylor RS, Warren FC. Netmums: a phase II randomized controlled trial of a guided Internet behavioural activation treatment for postpartum depression. Psychol Med. 2014 Jun;44(8):1675–89. doi: 10.1017/S0033291713002092. https://europepmc.org/abstract/MED/24148703 .S0033291713002092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Obikane E, Baba T, Shinozaki T, Obata S, Nakanishi S, Murata C, Ushio E, Suzuki Y, Shirakawa N, Honda M, Sasaki N, Nishi D, O'Mahen H, Kawakami N. Internet-based behavioural activation to improve depressive symptoms and prevent child abuse in postnatal women (SmartMama): a protocol for a pragmatic randomized controlled trial. BMC Pregnancy Childbirth. 2021 Apr 20;21(1):314. doi: 10.1186/s12884-021-03767-9. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-021-03767-9 .10.1186/s12884-021-03767-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Singla DR, Meltzer-Brody SE, Silver RK, Vigod SN, Kim JJ, La Porte LM, Ravitz P, Schiller CE, Schoueri-Mychasiw N, Hollon SD, Kiss A, Clark D, Dalfen AK, Dimidjian S, Gaynes BN, Katz SR, Lawson A, Leszcz M, Maunder RG, Mulsant BH, Murphy KE, Naslund JA, Reyes-Rodríguez ML, Stuebe AM, Dennis CL, Patel V. Scaling up maternal mental healthcare by increasing access to treatment (SUMMIT) through non-specialist providers and telemedicine: a study protocol for a non-inferiority randomized controlled trial. Trials. 2021 Mar 05;22(1):186. doi: 10.1186/s13063-021-05075-1. https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-021-05075-1 .10.1186/s13063-021-05075-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.O'Mahen HA, Wilkinson E, Bagnall K, Richards DA, Swales A. Shape of change in internet based behavioral activation treatment for depression. Behav Res Ther. 2017 Aug;95:107–16. doi: 10.1016/j.brat.2017.05.011. https://pubmed.ncbi.nlm.nih.gov/28618298/ S0005-7967(17)30104-3 [DOI] [PubMed] [Google Scholar]
- 46.Bagnall KM. Long-term follow-up of netmumshwd: a feasibility randomised controlled trial of telephone supported online behavioural activation for postnatal depression at 16 months post-randomisation. University of Exeter. 2014. May 06, [2022-05-24]. https://ore.exeter.ac.uk/repository/handle/10871/15289 .
- 47.Singla DR, Hossain S, Ravitz P, Schiller CE, Andrejek N, Kim J, La Porte L, Meltzer-Brody SE, Silver R, Vigod SN, Jung JW, Dimidjian S. Adapting behavioral activation for perinatal depression and anxiety in response to the COVID-19 pandemic and racial injustice. J Affect Disord. 2022 Feb 15;299:180–7. doi: 10.1016/j.jad.2021.12.006. https://europepmc.org/abstract/MED/34875282 .S0165-0327(21)01321-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van de Schoot R, de Bruin J, Schram R, Zahedi P, de Boer J, Weijdema F, Kramer B, Huijts M, Hoogerwerf M, Ferdinands G, Harkema A, Willemsen J, Ma Y, Fang Q, Hindriks S, Tummers L, Oberski DL. An open source machine learning framework for efficient and transparent systematic reviews. Nat Mach Intell. 2021 Feb 01;3(2):125–33. doi: 10.1038/s42256-020-00287-7. https://www.nature.com/articles/s42256-020-00287-7 . [DOI] [Google Scholar]
- 49.Brooke J. SUS: a 'quick and dirty' usability scale. In: Jordan PW, Thomas B, McClelland IL, Weerdmeester B, editors. Usability Evaluation in Industry. Boca Raton, FL, USA: The CRC Press; 1996. pp. 189–94. [Google Scholar]
- 50.Dadi AF, Miller ER, Bisetegn TA, Mwanri L. Global burden of antenatal depression and its association with adverse birth outcomes: an umbrella review. BMC Public Health. 2020 Feb 04;20(1):173. doi: 10.1186/s12889-020-8293-9. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-8293-9 .10.1186/s12889-020-8293-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cena L, Gigantesco A, Mirabella F, Palumbo G, Camoni L, Trainini A, Stefana A. Prevalence of comorbid anxiety and depressive symptomatology in the third trimester of pregnancy: analysing its association with sociodemographic, obstetric, and mental health features. J Affect Disord. 2021 Dec 01;295:1398–406. doi: 10.1016/j.jad.2021.09.015. https://linkinghub.elsevier.com/retrieve/pii/S0165-0327(21)00974-5 .S0165-0327(21)00974-5 [DOI] [PubMed] [Google Scholar]
- 52.Cheng CY, Chou YH, Chang CH, Liou SR. Trends of perinatal stress, anxiety, and depression and their prediction on postpartum depression. Int J Environ Res Public Health. 2021 Sep 03;18(17):9307. doi: 10.3390/ijerph18179307. https://www.mdpi.com/resolver?pii=ijerph18179307 .ijerph18179307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dennis CL, Falah-Hassani K, Shiri R. Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br J Psychiatry. 2017 May;210(5):315–23. doi: 10.1192/bjp.bp.116.187179.S0007125000281361 [DOI] [PubMed] [Google Scholar]
- 54.Woods SM, Melville JL, Guo Y, Fan MY, Gavin A. Psychosocial stress during pregnancy. Am J Obstet Gynecol. 2010 Jan;202(1):61.e1–7. doi: 10.1016/j.ajog.2009.07.041. https://europepmc.org/abstract/MED/19766975 .S0002-9378(09)00826-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lagadec N, Steinecker M, Kapassi A, Magnier MA, Chastang J, Robert S, Gaouaou N, Ibanez G. Factors influencing the quality of life of pregnant women: a systematic review. BMC Pregnancy Childbirth. 2018 Nov 23;18(1):455. doi: 10.1186/s12884-018-2087-4. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-018-2087-4 .10.1186/s12884-018-2087-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Betts KS, Williams GM, Najman JM, Alati R. The relationship between maternal depressive, anxious, and stress symptoms during pregnancy and adult offspring behavioral and emotional problems. Depress Anxiety. 2015 Feb;32(2):82–90. doi: 10.1002/da.22272. https://pubmed.ncbi.nlm.nih.gov/24788841/ [DOI] [PubMed] [Google Scholar]
- 57.Field T, Diego M, Hernandez-Reif M, Figueiredo B, Deeds O, Ascencio A, Schanberg S, Kuhn C. Comorbid depression and anxiety effects on pregnancy and neonatal outcome. Infant Behav Dev. 2010 Feb;33(1):23–9. doi: 10.1016/j.infbeh.2009.10.004. https://europepmc.org/abstract/MED/19945170 .S0163-6383(09)00096-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Talge NM, Neal C, Glover V, Early Stress, Translational Research and Prevention Science Network: Fetal and Neonatal Experience on Child and Adolescent Mental Health Antenatal maternal stress and long-term effects on child neurodevelopment: how and why? J Child Psychol Psychiatry. 2007 Mar;48(3-4):245–61. doi: 10.1111/j.1469-7610.2006.01714.x.JCPP1714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Caparros-Gonzalez RA, Romero-Gonzalez B, Strivens-Vilchez H, Gonzalez-Perez R, Martinez-Augustin O, Peralta-Ramirez MI. Hair cortisol levels, psychological stress and psychopathological symptoms as predictors of postpartum depression. PLoS One. 2017 Aug 28;12(8):e0182817. doi: 10.1371/journal.pone.0182817. https://dx.plos.org/10.1371/journal.pone.0182817 .PONE-D-17-05812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Richards DA. Stepped care: a method to deliver increased access to psychological therapies. Can J Psychiatry. 2012 Apr;57(4):210–5. doi: 10.1177/070674371205700403. https://pubmed.ncbi.nlm.nih.gov/22480585/ [DOI] [PubMed] [Google Scholar]
- 61.Conejo-Cerón S, Lokkerbol J, Moreno-Peral P, Wijnen B, Fernández A, Mendive JM, Smit F, Bellón JÁ. Health-economic evaluation of psychological interventions for depression prevention: systematic review. Clin Psychol Rev. 2021 Aug;88:102064. doi: 10.1016/j.cpr.2021.102064.S0272-7358(21)00107-0 [DOI] [PubMed] [Google Scholar]
- 62.Wang Q, Su M, Zhang M, Li R. Integrating digital technologies and public health to fight Covid-19 pandemic: key technologies, applications, challenges and outlook of digital healthcare. Int J Environ Res Public Health. 2021 Jun 04;18(11):6053. doi: 10.3390/ijerph18116053. https://www.mdpi.com/resolver?pii=ijerph18116053 .ijerph18116053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Addis ME, Martell CR. Overcoming Depression One Step at a Time: The New Behavioral Activation Approach to Getting Your Life Back: New Harbinger Self-help Workbook. Oakland, CA, USA: New Harbinger; 2004. [Google Scholar]
- 64.Bassi G, Giuliano C, Perinelli A, Forti S, Gabrielli S, Salcuni S. A virtual coach (Motibot) for supporting healthy coping strategies among adults with diabetes: proof-of-concept study. JMIR Hum Factors. 2022 Jan 21;9(1):e32211. doi: 10.2196/32211. https://humanfactors.jmir.org/2022/1/e32211/ v9i1e32211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bassi G, Mancinelli E, Dell'Arciprete G, Rizzi S, Gabrielli S, Salcuni S. Efficacy of eHealth interventions for adults with diabetes: a systematic review and meta-analysis. Int J Environ Res Public Health. 2021 Aug 26;18(17):8982. doi: 10.3390/ijerph18178982. https://www.mdpi.com/resolver?pii=ijerph18178982 .ijerph18178982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mancinelli E, Bassi G, Gabrielli S, Salcuni S. The efficacy of digital cognitive-behavioral interventions in supporting the psychological adjustment and sleep quality of pregnant women with sub-clinical symptoms: a systematic review and meta-analysis. Int J Environ Res Public Health. 2022 Aug 03;19(15):9549. doi: 10.3390/ijerph19159549. https://www.mdpi.com/resolver?pii=ijerph19159549 .ijerph19159549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ergonomics of human-system interaction — Part 11: Usability: Definitions and concepts. ISO 9241-11:2018(en) International Organization for Standardization. 2018. [2022-05-19]. https://www.iso.org/obp/ui/#iso:std:iso:9241:-11:ed-2:v1:en .
- 68.Nielsen J. Usability Engineering. Burlington, MA, USA: Morgan Kaufmann; 1993. [Google Scholar]
- 69.O’Brien HL, Cairns P, Hall M. A practical approach to measuring user engagement with the refined user engagement scale (UES) and new UES short form. Int J Hum Comput Stud. 2018 Apr;112:28–39. doi: 10.1016/j.ijhcs.2018.01.004. https://www.sciencedirect.com/science/article/pii/S1071581918300041 . [DOI] [Google Scholar]
- 70.Petersen GB, Nielsen JH, Olsen JV, Kok RN. Usability guidelines for developing and evaluating web-based mental health interventions: establishing a practical framework. PsyArXiv. doi: 10.31234/osf.io/3ewz4. Preprint posted online August 21, 2019. [DOI] [Google Scholar]
- 71.Cole-Lewis H, Ezeanochie N, Turgiss J. Understanding health behavior technology engagement: pathway to measuring digital behavior change interventions. JMIR Form Res. 2019 Oct 10;3(4):e14052. doi: 10.2196/14052. https://formative.jmir.org/2019/4/e14052/ v3i4e14052 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary materials.


