Abstract
Objective
To address the challenges of inequitable access to the COVID-19 vaccines, Kaiser Permanente Southern California developed a community-oriented and geographic vaccine strategy combining clinical data, community data, and predictive models to identify ZIP codes requiring increased resources to achieve equitable vaccine receipt.
Study Design
This is a quality-improvement implementation study.
Methods
The authors developed hot-spot maps for southern California service areas to assist clinicians in identifying specific ZIP codes to increase vaccination efforts. Data inputs for these hot spots included COVID-19 incidence, hospitalization, ecologic variables of social determinants of health, and predictive models of vaccine penetrance. Partnering with community organizations, vaccine penetrance was improved by targeting hot spots with pop-up clinics, mobile health vehicle visits, extending facility hours, and sending tailored text messages.
Results
By the end of 2021, Kaiser Permanente Southern California achieved a 70% vaccination rate in 83% of 670 ZIP codes it serves, resulting in a total vaccination rate of 81% in 2021. Further, more than 2 out of 3 individuals receiving a vaccine through the hot-spot guided mobile health vehicle were Hispanic or Black. The hot-spotting approach produced a refreshed monthly dashboard of hot spots in 7 counties covering over 670 ZIP codes to help decision makers better understand and improve vaccination in targeted communities.
Conclusion
The hot-spot methodology produced monthly lists of ZIP codes requiring additional health-care resources and vaccination strategies. This was a feasible place-based approach to mitigating disparities in vaccine uptake in historically disinvested communities that may be readily applied to other areas of care.
Keywords: COVID-19, health disparity, vaccine uptake, health equity, place-based
Introduction
As the first COVID-19 vaccines became available to the public in January 2021, the challenges of gaining adequate supply and making vaccines available were urgent priorities of health-care providers nationwide. Despite the initial logistical issues faced by providers in allocation and delivery, deep disparities in vaccine access and COVID-19 burden driven largely by socioeconomic factors proved to be the most substantial and enduring obstacle to vaccination efforts throughout 2021.
To address the challenges of inequitable access to the COVID-19 vaccine, Kaiser Permanente Southern California developed a community-oriented and geographic (ie, place-based) vaccine strategy aimed at mitigating disparities in COVID-19 vaccination by ZIP code. Kaiser Permanente Southern California is the largest vertically integrated health plan in California with over 4.7 million members, of whom 66% are people of color. The objective of this study is to describe Kaiser Permanente Southern California’s targeted efforts in 2020–2021 to ensure that its members and communities with the least vaccine access and socioeconomic resources received tailored messaging and additional health-care service accommodations to enhance vaccination opportunities.
Developing hot-spot mapping methodology to identify specific ZIP codes that require greater resources and commitment from the organization to achieve equitable vaccination receipt was critical to this vaccination strategy. Social determinants of health data and predictive statistical modeling for vaccine penetrance were creatively used to implement a place-based approach to provide more equitable delivery of COVID-19 vaccinations, with hopes to close racial and ethnic health disparities. 1,2 After identifying the geographic areas requiring more equitable allocation of resources and leveraging longstanding relationships with local community-based organizations to support vaccine delivery, Kaiser Permanente Southern California employed a range of targeted activities to improve vaccine penetrance. Activities included establishing pop-up clinics, mobile health vehicle visits, extending facility hours, sending tailored text messaging campaigns, and partnering with community-based organizations and public health agencies.
Methods
This study was conducted at Kaiser Permanente Southern California, a large managed-care system that includes 15 hospitals with nearly 4.7 million members and over 200 medical clinics. Kaiser Permanente Southern California serves over 7 counties covering over 670 ZIP codes in the region. The Kaiser Permanente Southern California member population is socioeconomically diverse and broadly representative of the racial/ethnic groups living in the southern California region. The study received a Kaiser Permanente Southern California Institutional Review Board (IRB) exemption because study activities were considered quality-improvement efforts.
Hot-spot methodology data elements
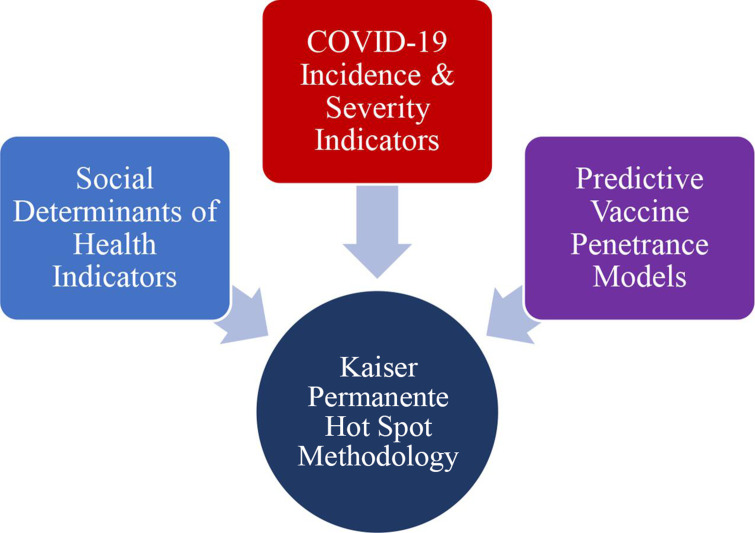
Hot-spot maps were developed in 2020–2021 to identify specific communities facing high COVID-19 incidence, severity, socioeconomic strain, and comparatively low vaccination rates. Neighborhood-level social determinants of health data, internal clinical data, and novel vaccine penetrance modeling were utilized to develop the hot-spot methodology. Key components of the hot-spot methodology are described below and in Figure 1.
Figure 1:
Conceptual framework for data used to build COVID-19 vaccine equity hot-spot methodology.
Clinical data
In developing a hot-spotting methodology for equitable COVID-19 vaccination, the authors first analyzed aggregated monthly patient data from 2020 related to COVID-19 incidence, testing positivity, and hospitalizations and found clear disproportionate clinical outcomes by patient ZIP code.
Community data
Data from the Southern California Public Health Alliance Healthy Places Index (HPI) were also used in the hot-spotting approach. The HPI combines 25 indicators of social determinants of health, including data related to economics, education, transportation, environment, housing, and health-care access for each census tract in California. 3 HPI analysts provided ZIP-code estimates based on census tract data. 4 The HPI uniquely weighs each base indicator to life expectancy at birth and provides a percentile score for each ZIP code in California. Hence, an HPI score quantifies the opportunity to live a healthy life within a given ZIP code and helps identify communities impacted by historic disinvestment, red-lining, and structural racism.
Predictive modeling
Predictive models of patient vaccination penetrance by ZIP code were employed for the hot-spotting approach. Early in 2021, Kaiser Permanente Southern California leadership set the ambitious goal to reach a 70% COVID-19 vaccination rate among its members. This rate was used as a benchmark in all modeling to predict which ZIP codes would reach 70% vaccine penetrance by the end of 2021. Model validation and optimization was approached at the ZIP-code level. For each ZIP code, the parameters of a generalized logistic function were optimized using nonlinear least squares to fit a curve approximating the cumulative vaccination rate for that area. Each month, as new data were added, these parameters were reoptimized to update year-end vaccination-rate predictions. Acceptably small root-mean-squared errors were determined for testing data across geographies and time periods.
Hot-spot methodology indicators
Indicators extracted from the electronic health records for use in the hot-spotting methodology were refreshed on the first of each month, resulting in a new list of hot spots identified approximately every 30 days.
Estimated COVID-19 incidence
Because of the rapidly shifting community spread of COVID-19 virus and the dynamics of the pandemic in southern California, quantifying the precise COVID-19 incidence among Kaiser Permanente Southern California members in each relevant ZIP code was not possible. Instead, incidence was estimated using a combination of 2 indicators: 30-day COVID-19 incidence among Kaiser Permanente Southern California members and 30-day test positivity rates at Kaiser Permanente Southern California facilities. The 30-day COVID-19 incidence was calculated by dividing the number of Kaiser Permanente Southern California members diagnosed with COVID-19 in a ZIP code during the previous 30-day period by the total number of members in the ZIP code. These data were placed on a distribution and percentile ranks were calculated for each ZIP code served by Kaiser Permanente Southern C (roughly 670 ZIP codes) to provide relative measures of COVID-19 incidence.
Test positivity
Thirty-day COVID-19 testing positivity rates were calculated at the ZIP-code level by dividing the number of Kaiser Permanente members in the ZIP code testing positive in the previous 30-day period by the total number of Kaiser P members tested during the same period. Positivity rates were placed on a distribution and percentile ranks were calculated for each ZIP code.
Once testing positivity and incidence percentile ranks were calculated, each ZIP code was assigned the higher of the 2 percentiles to represent its estimated COVID-19 incidence.
Hospitalization
Thirty-day COVID-19 severity was estimated by COVID-19 hospitalizations. Rates of COVID-19 hospitalizations (hospitalizations per 10,000 Kaiser Permanente members) were calculated for each ZIP code; the numerator was the count of patients admitted to a hospital and receiving a COVID-19 diagnosis, and denominator was the total number of Kaiser Permanente members in the ZIP code. The COVID-19 hospitalization rates per 10,000 Kaiser Permanente patients were then placed on a distribution and percentile ranks were calculated for each ZIP code.
Predicted end-of-year vaccine penetrance
Member vaccination counts were predicted programmatically using Python’s SciPy.optimize.curve_fit() function, which fits a mathematical function to member vaccination data for a given geography by ZIP code. Several basis functions were considered because of their curves’ behaviors and the interpretability of their parameters. The input of the functions was time, which was defined by the number of days since members started receiving vaccines. The output was the expected number of members to have been vaccinated at that time. Data were collected from members’ electronic medical records. A member was considered vaccinated if they received any vaccine, regardless of vaccine manufacturer or proper dosage compliance (eg, completion of a 2-dose series).
Statistical modeling
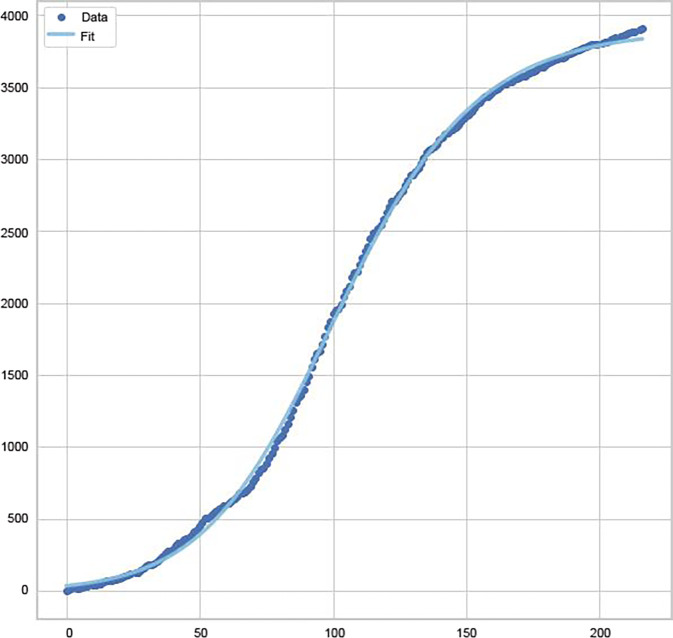
A sigmoid function, a mathematical function that produces an S-curve, was plotted (see formula in Appendix A). The function is bounded, with a slow initial growth that quickly accelerates up to an inflection point, after which growth decelerates and eventually plateaus. This mirrors the COVID-19 vaccine receipt in our membership. Few members received the vaccine when it was initially approved for Emergency Use Authorization because of age restrictions, skepticism, lack of availability, and other factors. However, over time, increasingly more members received the vaccine because of age expansion, increased confidence, and improved availability, and hence, vaccination counts quickly rose. After a certain time, fewer unvaccinated members got the vaccine. Eventually, there came a point of saturation, where most members who wanted to receive the vaccine were able to do so. The authors fit curves using the sigmoid based on Gompertz, and Richards' formulas. 5 As Richards’ curve is a generalization of the logistic (sigmoid) and Gompertz curves, this typically resulted in the best fit (ie, minimized sum of the squared residuals) which is shown in Figure 2. 5–7
Figure 2:
Example ZIP code with actual vaccine data (blue dots) fitted with Richards’ curve (blue line).
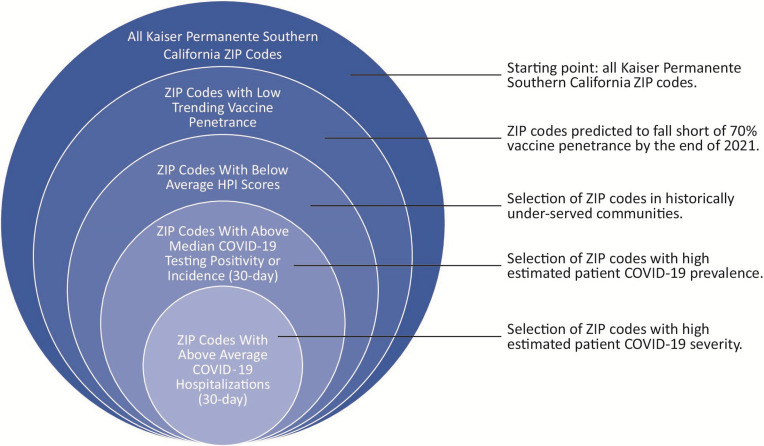
Hot-spot identification
The term COVID-19 vaccine equity hot spot in the present study refers to a ZIP code with high estimated COVID-19 incidence, high COVID-19 hospitalization rates, predicted year-end COVID-19 vaccine penetrance below 70%, and high socioeconomic strain (ie, low HPI percentile) relative to other ZIP codes in the Kaiser Permanente Southern California service areas. Standards for evaluating each of the above criteria were defined using the methodology described below. Lists of hot spots were generated using a nested analysis described in Figure 3 that incorporated data across 4 phases. Lists were updated using new data each month.
Figure 3:
Nested methodology for hot-spot identification. HPI = Healthy Places Index.
Phase I
The starting point for the list to identify hot spots was the full universe of ZIP codes in the Kaiser Permanente Southern California service areas (roughly 670 ZIP codes across 7 counties). The first selection of ZIP codes was based on vaccination penetrance predictions. All ZIP codes predicted to not reach the 70% vaccination penetrance goal were selected to move to the next phase.
Phase II
Next, the average HPI percentile was calculated for the selected ZIP codes (this average was typically around the 30th percentile). All ZIP codes below this average HPI percentile were selected to move to the next phase. Using predictive vaccine modeling and HPI in this way, the resulting list of ZIP codes indicated low predicted vaccine penetrance, severe socioeconomic strain, and comparatively sparse community resources. Because poor social determinants of health are associated with chronic diseases such as obesity and diabetes, ZIP codes selected for low HPI are also correlated with populations with comorbidities that risk severe cases of COVID-19.
Phase III
Within the list of ZIP codes with low vaccine penetrance and low HPI percentiles, a third cut of the data selected ZIP codes in the 75th percentile and above for estimated 30-day COVID-19 incidence (ie, the higher of 2 indicators: 30-day COVID-19 testing positivity or 30-day COVID-19 incidence). After this cut, the list of ZIP codes represented communities with low predicted vaccine penetrance, high socioeconomic strain, and high estimated COVID-19 incidence. This list of ZIP codes was advanced to the final phase of analysis.
Phase IV
The final cut selected ZIP codes in the 75th percentile and above for 30-day Kaiser Permanente Southern California COVID-19 hospitalization rates. In this way, the final list represented comparatively high COVID-19 hospitalization rates even among ZIP codes with high population comorbidities and low vaccine rates.
Results
The nested hot-spotting methodology was applied to the data on the first of each month in 2021. In each monthly analysis, a regional list (eg, about 20–30 ZIP codes across the universe of about 670 ZIP codes were identified) and 15 individual service area lists for each of Kaiser Permanente Southern California’s hospitals (eg, about 3–5 ZIP codes out of a universe of 30–50 ZIP codes) were produced. An example hot-spot report is displayed in Table 1.
Table 1:
Example COVID-19 equity hot spot report for a Kaiser Permanente Southern California service area.
| ZIP | Medical office building | Neighborhood | Predicted 2021 member vaccine penetrance (%) | Kaiser Permanente Southern California percentile for est. member COVID incidence | Kaiser Permanente Southern California percentile for member COVID hospitalization | Est. total members 12+ | % Non- English- Speaking members | Avg drive time to Kaiser Permanente prim care (min) | Est. vaccine hesitancy a (%) |
|---|---|---|---|---|---|---|---|---|---|
| 93505 | Lancaster MOB | California City | 56.9 | 85.1 | 90.2 | 1802 | 5.1 | 37.7 | 23.3 |
| 93544 | Palmdale MOB | Llano, Crystalaire | 68.0 | 81.5 | 95.0 | 305 | 3.0 | 27.0 | 9.7 |
| 93553 | Palmdale MOB | Pearblossom | 63.7 | 91 .4 | 92.3 | 535 | 5.3 | 32.6 | 11.5 |
Represents the percentage of the total ZIP code population (members and non-members) that is ‘somewhat’ or ‘very’ hesitant to receive a COVID-19 vaccine. Data from IMHE, University of Washington 2021.
Avg, average; IMHE, Institute for Health Metrics and Evaluation; MOB, Medical Office Building.
Community-level results
By the end of 2021, Kaiser Permanente Southern California achieved a 70% vaccination rate or higher in approximately 82.8% of its ZIP codes, representing a total vaccination rate of 80.7% in 2021. Analysis of Kaiser Permanente Southern California mobile health vehicle data deployed using the hot-spot methodology revealed that more than 2 out of 3 individuals receiving a vaccine self-identified as Hispanic or Black.
Organization-level results
In addition to the vaccination outcomes above, the hot-spotting approach resulted in key institutional shifts in data reporting and dissemination. The monthly list of hot spots in each of Kaiser Permanente Southern California’s 15 service areas was routinely provided to the respective staff in each area; this list highlighted the relevant hot spots in the service area and included additional data to help decision makers better understand the population and community barriers to vaccination (Table 1). Among these additional data were information related to the non-English-speaking population, driving time to nearest Kaiser Permanente Southern California primarycare facility, vaccine hesitancy data from the Institute for Health Metrics and Evaluation, and additional population characteristics from the Environmental Systems Research Institute. Table 1 provides 1 example of a report that became routinized and disseminated across Kaiser Permanente Southern California using the equity hot-spot list. Kaiser Permanente Southern California leaders and staff used information in the report to deploy tailored solutions to hot-spot areas, including redirecting mobile health vehicles to areas in need, extending facility hours to accommodate more vaccination appointments, and leveraging relationships with community partners in hot-spot areas to increase awareness about the vaccination programs.
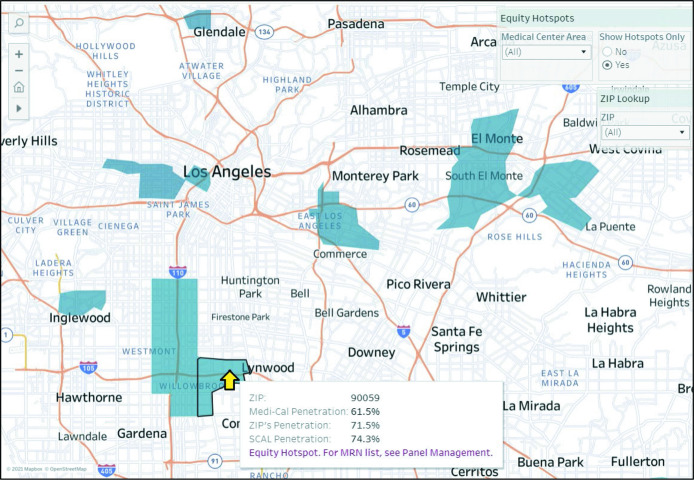
Another institutional outcome of the hot-spotting methodology was the integration of hot-spot data into organizational COVID-19 vaccine dashboards. The inclusion of COVID-19 equity hot spots through easy-to-use tools on the dashboard helped local decision makers monitor progress, compare penetrance to regional benchmarks, and visualize targeted communities. Figure 4 presents 1 example of how hot-spot ZIP codes were visualized and accompanied by relevant metrics for Kaiser Permanente Southern California staff. Data for the dashboard were pulled using Oracle SQL Version 17.3.1.279 and Build 279.0537, and visualized using Tableau version 2021.2.2. Vaccine penetrance rates were represented for all ZIP codes and were color-coded on a light-blue to dark-blue spectrum; darker colors indicated lower vaccine penetrance. Users could filter the dashboard to show only ZIP codes in certain service areas, and within those areas, only ZIP codes identified as COVID-19 vaccine equity hot spots (see upper right menus in Figure 4). By hovering the mouse over any ZIP code, the dashboard represented several data points, including the current COVID-19 vaccine penetrance, and the regional average (see yellow arrow and pop-up menu in Figure 4). Care providers could also apply the ZIP-code lists to their panel management tools to allow quick access to lists of patients residing in a hot-spot ZIP code and help drive outreach campaigns.
Figure 4:
Example of hot-spot visualization and integration into COVID-19 vaccine surveillance.MRN = Medical Record Number; SCAL = Kaiser Permanente Southern California.
For clinicians, the dashboard linked practitioners to a panel management system, which was a separate data system from the dashboard itself. Practitioners could view patient-level data and act accordingly. Practitioner actions included targeted outreach to individual patients using text messaging to encourage patients to get vaccinated, or via email sent through patients’ secure online accounts.
Discussion
This COVID-19 equity hot-spot methodology was successful in supporting the organization achieving its goal of 70% vaccine penetrance by the end of 2021 in nearly 83% of its ZIP codes despite substantial barriers and represents a major shift in approach for Kaiser Permanente Southern California in addressing disparities in health outcomes across its communities. Rather than guiding its equitable vaccination strategy with vaccine data disaggregated by race and ethnicity (ie, a race-based approach), Kaiser Permanente Southern California utilized data related to social determinants that regularly drive poor health outcomes in communities (ie., a place-based approach). This method acknowledged the historical sociopolitical factors such as structural racism, red-lining, and decades of community disinvestment at the root of the disparities in health outcomes, including vaccination status in Kaiser Permanente Southern California communities. Data from the Kaiser Permanente Southern California mobile health vehicle vaccinations guided by the hot-spotting methodology revealed that more than 2 out of 3 individuals vaccinated by the mobile health vehicle self-identified as Black or Hispanic—a disproportionally high amount as a percentage of the total Kaiser Permanente Southern California membership. This provides evidence that by leveraging data related to the root causes of health inequity, the place-based approach acknowledged important historical context and ultimately mitigated disparities in communities of color hardest hit by the COVID-19 pandemic while not framing the role of race/ethnicity as the sole contributor of poor health outcomes.
The methodology also represented an effective integration of internal clinical data with a robust index of the social determinants of health. Findings related to disparities by ZIP code in the clinical data were well aligned with research demonstrating that ZIP-code level data can capture a unique set of social and economic factors that act powerfully on residents to shape health outcomes. 8 Pairing these clinical data with contextual community data provided Kaiser Permanente Southern California clinicians a more holistic view of the pandemic burden on communities and assisted staff in targeting texting campaigns and other messaging designed to improve vaccine confidence.
Strengths
Clinical and community data in this study came from a large and diverse membership; thus, the methodology and results might be generalizable to the overall community in California. Further, as vaccinations were provided to all community members regardless of insurance status, this hot-spot methodology might have also reduced COVID-related health disparities in noninsured residents living in the southern California region. The results helped identify areas for enhanced vaccination efforts; this might have helped reduce the disparities in southern California in terms of vaccination rates and hospitalizations among the residents who acquired COVID.
Limitations
Though ZIP codes are often the default organizing geographical structure in health-care delivery, ZIP-code boundaries are intended to organize mail delivery and are not always accurate representations of coherent communities to target with health interventions. Additionally, geocoded variables based on ZIP codes may not reflect all individuals in the ZIP code. However, socioeconomic status indicators based on area-level data for has proved to be useful in monitoring health disparities in health-care systems. 8
Because of the nature of this quality-improvement project and being exempted from IRB review, there are some gaps in our analysis that warrant further study with individual-level data to assess patient-level outcomes. For example, our study could not determine percent COVID-19 positivity or percent hospitalized as the authors did not have access to raw data. Additionally, the authors could not examine sociodemographic characteristics of ZIP codes that did not reach our successful vaccination threshold of 70%. Exploring patient-level factors and barriers to vaccination in this group is a future direction that can be taken with analysis of individual-level data pending additional IRB review and approval. Further, this study most likely only examined partial vaccinations, particularly at the beginning of the pandemic before the availability of booster vaccinations. This was a quality-improvement effort that focused on effectiveness in a real-world setting; therefore, the authors are not able to assess efficacy for this project.
The authors used COVID-19 hospitalization rates as a measure of disease severity because other indicators (eg, mortality, count of patients treated in an Intensive Care Unit, etc.), did not generate an adequate sample size and distribution to apply in the hot-spot methodology meaningfully. However, the hospitalizations indicator did provide an adequate sample and was seen as capturing cases of “moderate,” “severe,” and “critical” COVID-19 disease severity criteria adopted by the Centers for Disease Control and Prevention in 2021. Finally, because data related to COVID-19 tests and diagnoses are influenced by individual willingness to access the medical system, these indicators may underestimate COVID-19 incidence.
Conclusion
In summary, the hot-spot methodology was a feasible and successful method to produce monthly lists of ZIP codes requiring additional organizational resources and enhanced vaccination strategies. It also represents a promising method for population-based care management of both infectious and chronic diseases. Months of routinized use have embedded the practice in Kaiser Permanente Southern California hospitals across our footprint, and the authors plan to use this methodology in 2022 to augment vaccination programs for COVID-19 booster doses in the fight against the COVID-19 Omicron and subsequent variants. Further, this methodology can be used to direct the health plan’s resources to close other disparities in important areas of care, such as influenza and diabetes management.
Acknowledgments
The authors thank the patients of Kaiser Permanente for helping to improve care by allowing their information to be collected through our electronic health record systems. We also acknowledge the following colleagues for their support and participation in this quality improvement project: Fatima Ajose, Kristen Andrews, Annet Arakelian, Benjamin Broder, Lisa Buffong, Nalani Coleman, Estee Copans, Mehrnaz Davoudi, Christopher De La Vega, Maria DiSalvo, Diana Halper, Patti Harvey, Timothy Ho, Tracy Imley, Donald Kaplan, Margaret Khoury, Keshia Kirtz, Yesenia Monsour, Michael Morris, MD, Michelle Pruit, Ramona Snipes, Lakiesha Tidwell, Shirley To, Giselle Willick, PharmD, and John Yamamoto.
Appendix A – Statistical Modeling Details
Sigmoid curve ("y members vaccinated on day x") formula:
where
L: curve’s maximum value (maximum possible number of vaccinated members, ie, member count
x0: x value of curve’s midpoint (days after first vaccine administered)
k: logistic growth rate (steepness of curve)
However, the asymptotic bounds of the sigmoid function are approached symmetrically. That is, the initial growth occurs at the same (but negative) rate as the final plateau. To account for a more gradual growth toward an upper bound (as observed in our data), a special case of the sigmoid function called the Gompertz function was used to improve our model.
Gompertz curve formula:
Ultimately, this function could be generalized further to a generalized logistic function called Richards’ curve. This allowed for even more flexibility with the model’s end behaviors. The generalized function can easily be expanded to combine multiple curves (eg, adding curves from different geographic or demographic populations).
Richards’ curve formula is
where if Xi equals 1, the curve becomes a sigmoid; if Xi converges to 0, the curve converges to the Gompertz function. Such a curve has been used to model cumulative COVID-19 infection cases for a given geography. 6
Footnotes
Funding: None declared
Conflicts of Interest: None declared
Author Contributions: Matthew Swope, PhD, participated in concept and design, acquisition of data, analysis and interpretation of the data, drafting and critical revision of the manuscript for important intellectual content, and supervision. Angelika C Alem, MS, MPH, participated in concept and design, drafting of the manuscript, and administrative and logistical support, including submitting the final manuscript. Steven C Russo, MS, participated in acquisition of data, drafting of the manuscript, concept and design, and analysis and critical revision of the manuscript. Nancy E Gin, MD, participated in administrative and logistical support and critical revision of the manuscript for important intellectual content. Shari G Chevez, MD, participated in drafting the manuscript, administrative and logistical support, and supervision. Reina Haque, PhD, MPH, participated in concept and design, acquisition of data, analysis and interpretation of the data, drafting and critical revision of the manuscript for important intellectual content, and supervision. All authors have given final approval to the manuscript.
References
- 1.Dankwa-Mullan I, Pérez-Stable EJ. Addressing health disparities is a place-based issue. Am J Public Health . 2016;106(4):637–639. 10.2105/AJPH.2016.303077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gayle H, Foege W, Brown L, et al. Framework for Equitable Allocation of COVID-19 Vaccine . Washington, DC: National Academies Press; 2020. 10.17226/25917 [DOI] [PubMed] [Google Scholar]
- 3.Delaney TD, Dowling H, Maizlish N. Healthy Places Index (HPI 2.0). 2018. [DOI] [PMC free article] [PubMed]
- 4.Maizlish ND, Delaney T. California Healthy Places Index for ZIP Codes. 2020. [DOI] [PMC free article] [PubMed]
- 5.Yin X, Goudriaan J, Lantinga EA, Vos J, Spiertz HJ. A flexible sigmoid function of determinate growth. Ann Bot . 2003;91(3):361–371. 10.1093/aob/mcg029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee SY, Lei B, Mallick B. Estimation of COVID-19 spread curves integrating global data and borrowing information. PLoS One . 2020;15(7). 10.1371/journal.pone.0236860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu K, Darcet D, Wang Q, Sornette D. Generalized logistic growth modeling of the COVID-19 outbreak: Comparing the dynamics in the 29 provinces in China and in the rest of the world. Nonlinear Dyn . 2020;101(3):1561–1581. 10.1007/s11071-020-05862-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berkowitz SA, Traore CY, Singer DE, Atlas SJ. Evaluating area-based socioeconomic status indicators for monitoring disparities within health care systems: Results from a primary care network. Health Serv Res . 2015;50(2):398–417. 10.1111/1475-6773.12229 [DOI] [PMC free article] [PubMed] [Google Scholar]