Abstract
Introduction
Teledermatology has been shown to improve efficiency and reduce barriers to care for patients. However, teledermatology is limited by the inability to perform diagnostic tests. With proper planning, teletrichoscopy can be utilized with teledermatology to evaluate patients with hair loss.
Case Presentation
Diagnosis of this patient was made using images taken during the televisit, including scalp images taken by the patient using a handheld microscope and images of the hair roots taken by her referring doctor.
Conclusion
Hair tests that can be conducted during teledermatology visits include a self-performed pull test, measurement of the thickness of the ponytail, measurement of the distance from the hairline to the glabella, and evaluation of the shedding scale. These tests, in addition to mobile applications for imaging or low-cost handheld microscopes, can be utilized to virtually evaluate patients with hair loss.
Keywords: Loose anagen syndrome, Alopecia, Hair disorder, Teledermatology, Trichoscopy, Teletrichoscopy, Teledermoscopy
Established Facts
Teledermatology can be an efficient way to evaluate patients with dermatologic complaints and has been shown to decrease barriers to care.
Novel Insights
Complex hair diagnoses, including loose anagen syndrome, can be accurately made by teledermatology if utilized in combination with teletrichoscopy.
Introduction/Literature Review
Teledermatology has been shown to be a valuable approach in the diagnosis and management of dermatologic diseases, and its utility has improved healthcare accessibility prior to and during the coronavirus disease 2019 pandemic [1, 2]. Teledermatology has been reported to increase the efficiency of care for providers by reducing travel times, reducing no-show/cancellation rates, and serving as a tool for triaging patients [2]. On the receiving end, patients often face fewer barriers to receiving care, including reduced wait times and distance needed to travel, leading to increased rates of follow-up care and treatment compliance [2]. However, teledermatology has various limitations, including difficulties in performing tests that are necessary for diagnosis. We have recently shown that the most important trichology tests can be performed during teledermatology if the consultation is properly organized [3]. Here, we report an example of a complex hair diagnosis of loose anagen syndrome (LAS) made via teledermatology during the coronavirus disease 2019 pandemic and later confirmed with an in-person evaluation.
Case Report
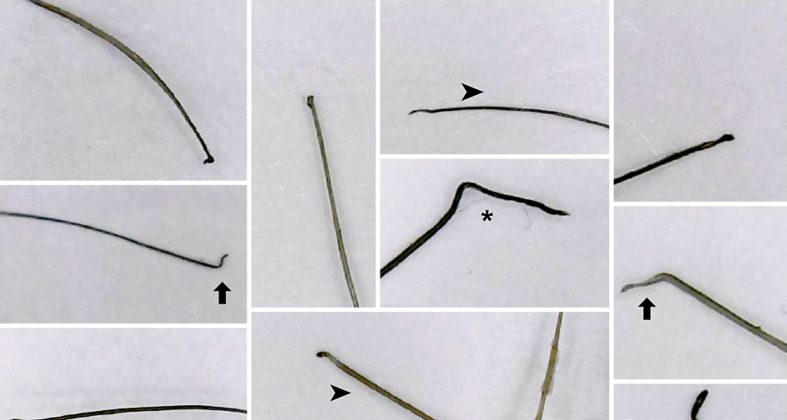
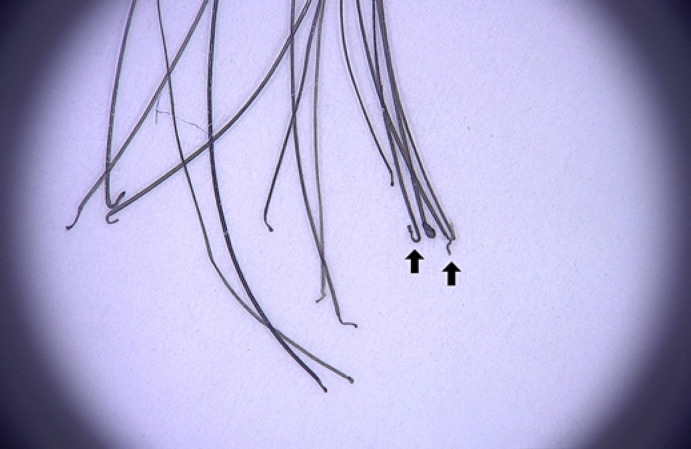
A 22-year-old woman with a past medical history of postural orthostatic tachycardia syndrome presented to a dermatologist for hair shedding that began in March 2020. She was diagnosed with telogen effluvium, and laboratory work revealed low ferritin. The patient was treated with topical minoxidil and iron supplementation. However, due to worsening hair loss, she again consulted her dermatologist, who performed a pull test that was positive. The dermatologist suggested a possible diagnosis of alopecia areata and gave the patient a copy of the records from the visit, including close-up images of the hair extracted with the pull test. She was treated with clobetasol foam three times a week with no improvement. At this time, the patient was referred to one of us (AT) by telemedicine for a third opinion. During the visit, the patient was able to show her scalp images taken with a handheld video-microscope showing few rectangular black granular structures (Fig. 1) and pull test images taken by the local dermatologist showing ruffled cuticles and anagen hairs devoid of sheaths (Fig. 2). The patient was diagnosed with loose anagen hairs and telogen effluvium and started on oral minoxidil 0.625 mg/day. At an in-person follow-up in April 2022, the hair shedding was back to normal, and the diagnosis of LAS was confirmed by a trichogram showing more than 70% anagen hair without sheaths (Fig. 3).
Fig. 1.
An image taken with a handheld video-microscope showing a rectangular black granular structure (black arrowhead).
Fig. 2.
Images from the hair pull test showing anagen hairs devoid of sheaths (black arrowhead), misshapen anagen bulbs (black arrow), and ruffled cuticles (black asterisk).
Fig. 3.
Trichogram showing misshapen anagen bulbs (black arrow) and more than 70% anagen hair without sheaths.
Discussion
This report confirms that telemedicine can provide an accurate diagnosis if utilized with teletrichoscopy exams [3]. To our knowledge, this is the first case of LAS diagnosed via telemedicine. LAS is an uncommon disorder that typically occurs in young children with light-colored hair. LAS may also be first diagnosed in adulthood, as with our patient. This occurs when a patient with subclinical LAS develops telogen effluvium or anagen effluvium that prompts evaluation by a dermatologist, who then makes the diagnosis by evaluating the hair roots and trichoscopy. Asymptomatic parents of children with LAS have also been diagnosed with subclinical LAS in instances where the family members are also evaluated. LAS has been associated with poor psychological outcomes in children, necessitating swift and accurate diagnosis and treatment [4].
In our case, the images taken by a local dermatologist and teletrichoscopy were utilized to make the correct diagnosis. A low-cost handheld microscope was effective to visualize the black granular rectangular structures of LAS. This device can also visualize broken and exclamation mark hairs in alopecia areata, hair shaft variability in androgenetic alopecia, lack of vellus hairs in frontal fibrosing alopecia, and peripilar casts in scarring alopecia [3].
Guides have been developed for dermatologists to assess alopecia using teledermatology, and these guides can be expanded to include other hair disorders [5]. As medical technologies continue to advance, we believe that teledermatology holds promise in aiding the diagnosis of complex dermatologic conditions and will enable dermatologists to triage efficiently, create a knowledge-sharing network, and improve health outcomes.
Statement of Ethics
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images. This study was deemed exempt by the University of Miami Institutional Review Board (45 CFR 46.104).
Conflict of Interest Statement
Dr. Tosti is a consultant for DS Laboratories, Monat Global, Almirall, Thirty Madison, Eli Lilly, Bristol Myers Squibb, P&G, Pfizer, and Myovant and principal investigator for Eli Lilly, Concert, and Erchonia. She is one of the editors-in-chief of Skin Appendage Disorders. The remaining authors have no conflicts of interest to declare.
Funding Sources
The authors have received no funding for this study.
Author Contributions
Erik Peterson and Antonella Tosti evaluated the patient clinically. Maria J. Lalama, Betty Nguyen, Erik L. Peterson, and Antonella Tosti were involved in the preparation of the manuscript and read and approved the final manuscript.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
Funding Statement
The authors have received no funding for this study.
References
- 1.Lee JJ, English JC., 3rd Teledermatology: a review and update. Am J Clin Dermatol. 2018 Apr;19((2)):253–260. doi: 10.1007/s40257-017-0317-6. [DOI] [PubMed] [Google Scholar]
- 2.Maddukuri S, Patel J, Lipoff JB. Teledermatology addressing disparities in health care access: a review. Curr Dermatol Rep. 2021 Mar 12;10((2)):40–47. doi: 10.1007/s13671-021-00329-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Randolph M, Al-Alola A, Tosti A. Diagnosis of hair disorders during the COVID-19 pandemic: an introduction to teletrichoscopy. J Eur Acad Dermatol Venereol. 2021 Mar;35((3)):e167–e168. doi: 10.1111/jdv.16989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Randolph MJ, Gwillim EC, Nguyen B, Tosti A. The psychologic impact of loose anagen syndrome and short anagen syndrome. Pediatr Dermatol. 2022 Apr 16;39((4)):567–569. doi: 10.1111/pde.15002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilson BN, McMichael A, Alexis A, Agbai O, Elbuluk N, Callender V. Telemedicine alopecia assessment: highlighting patients with Skin of color. Cutis. 2022 Jan;109((1)):40–42. doi: 10.12788/cutis.0419. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.