Abstract
Introduction
There are increasing reports of a link between chronic constipation and allergies in children. However, similar epidemiological evidence is limited in the general adult population. Therefore, in this study, we attempted to assess the association between chronic constipation and allergy in adults aged ≥20 years in the USA.
Methods
We established a logistic regression model to test the relationship between chronic constipation and 19 specific immunoglobulin E (sIgE) types in adults aged ≥20 years using large-sample data from the National Health and Nutrition Examination Survey database (2005–2006). The weekly defecation times of the allergic and non-allergic groups were compared using the t test.
Results
We found that sIgE-sensitized participants had a 0.723 lower risk of chronic constipation than the general population (95% confidence interval (CI) = 0.566–0.923). There was a negative association between chronic constipation and sensitizations to peanut (odds ratio (OR) = 0.579, 95% CI = 0.381–0.935), egg (OR = 0.335, 95% CI = 0.134–0.838), dog (OR = 0.723, 95% CI = 0.522–0.965), and cockroach (OR = 0.540, 95% CI = 0.373–0.784). In addition, the frequency of defecation per week increased significantly in people allergic to peanuts and cockroaches (p < 0.05).
Discussion/Conclusion
The results of this study demonstrate an inverse relationship between sIgE sensitization and chronic constipation in adults. However, the specific association mechanism needs to be further studied.
Keywords: Allergens, Antigen-specific immunoglobulin E, Chronic constipation, Epidemiology, Clinical allergy
Introduction
Antigenic substances in the environment are increasing with the changes in lifestyle and living environment. Consequently, allergic disease rates are gradually rising, which pose a serious threat to human health [1]. Immunoglobulin E (IgE) is the lowest circulating antibody allotype; however, it plays an important role in mediating type I anaphylaxis [2]. Allergens, including inhaled and food allergens, are antigenic substances that cause type I allergic reactions [3]. IgE-mediated allergic diseases include eczema, food allergy, asthma, and allergic rhinitis [4]. Airway allergic diseases such as asthma and allergic rhinitis are mainly inhaled allergies. In urban centres, allergies caused by inhaled allergens are steadily increasing [5].
The prevalence of asthma in the USA was 7.8% from 2006 to 2008, which led to a huge financial burden. The cost of asthma in the USA was estimated at USD 56 billion in 2007, representing a 6% increase from USD 53 billion in 2002 [6]. In the European Union, the impact of allergic rhinitis on work efficiency is estimated at 30–50 billion Euros annually [7]. Concomitantly, food allergies exist in all age groups, and the reported prevalence of food allergies in North America is 3.9–8% in infants and children and 6.6–10% in adults [8]. Therefore, it is necessary to explore the related factors of IgE-mediated allergic diseases.
Chronic constipation is a common disease that manifests similarly in children and adults; however, differences in epidemiology, symptomatology, pathophysiology, diagnostic examination, and treatment management can be observed [9]. Approximately 15–17% adults report symptoms that meet the diagnostic criteria for chronic constipation [10]. The disease is also common in children, with an incidence rate of 3–16% in the paediatric population [11]. Although constipation is rarely associated with life-threatening complications, it can have a considerable impact on patients. Some studies have shown that allergic diseases may be associated with constipation. Moreover, food allergies may lead to gastroesophageal reflux disease and colic or constipation in infants, especially in children with milk protein allergies, causing chronic constipation, for which laxative treatments are typically ineffective [12].
An epidemiological study in Fukui Prefecture, Japan showed that constipation was related to the development of allergic rhinitis in 21,802 high school students [13]. Constipation is currently considered a pathogenic factor of intestinal ecological disorders. Intestinal microflora, such as those found in the endocrine organs, can produce bioactive metabolites, enzymes, and small molecules, which affect host physiological activity and mediate diseases [14]. Moreover, recent studies have shown that compared to the abundance of Dorea in healthy controls, that in children with asthma and allergic rhinitis is lower and is negatively associated with the total faecal IgE level. In contrast, Clostridium is abundant and positively associated with faecal IgE level in children with asthma [15].
This evidence shows the varying degrees of association between chronic constipation and allergic diseases. However, most studies on this potential association were conducted on infants or children, and only few studies explored the relationship between specific allergens and chronic constipation, especially among adult patients. Therefore, in this study, we attempted to assess the association between chronic constipation and allergy in adults aged ≥20 years in the USA by examining large-sample data from the National Health and Nutrition Examination Survey (NHANES) database.
Materials and Methods
Epidemiologic Study Population
We investigated the 2005–2006 data of participants in the NHANES, a US cross-sectional study conducted by the National Centres for Health Statistics of the Centres for Disease Control and Prevention. The database is freely available and can be accessed directly through the website (https://www.cdc.gov/nchs/nhanes/index.htm). The survey was conducted in a complex multistage design and was sampled to represent the population of the USA. The protocols and procedures adopted by NHANES protect the personal information of participants. All participants provided written informed consent. All NHANES investigations were approved by the National Center for Health Statistics Research Ethics Review Board (ERB), and the ERB protocol number of NHANES 2005–2006 is #2005-06 [16].
NHANES 2005–2006 is the only cycle of complete questionnaires including allergy-related results, wherein a total of 10,348 participants were surveyed. In this study, only 3,837 participants who had complete information on allergies, chronic constipation, and model covariates were included.
Assessment of Allergy-Related Results
We evaluated data on total IgE (tIgE) and allergen-specific IgE (sIgE) levels in the database. Blood samples were drawn at the NHANES examination site and analysed in the NHANES laboratory, and tIgE and allergen sIgE levels in serum samples were analysed using Pharmacia Diagnostics ImmunoCAP 1,000 system (Kalamazoo, MI, USA). According to the guidelines of the American Association for Clinical and Laboratory Standards, we defined sIgE sensitization as at least 1 of 19 allergens with a level of ≥0.35 kU/L [16]. A total of 19 specific allergens, including Dermatophagoides farinae, D. pteronyssinus, cat, dog, cockroach, Alternaria, peanuts, egg, milk, ragweed, rye grass, Bermuda grass, oak, birch, shrimp, aspergillus, thistle, mouse, and rat, were screened. A tIgE concentration of ≥100 kU/L indicates tIgE sensitization [17].
Assessment of Chronic Constipation
According to the responses of participants to the intestinal health questionnaire, participants were evaluated to have chronic constipation. The questionnaire was completed using the computer-assisted personal interview system in the interview room of the mobile examination centre. The intestinal health questionnaire (variable name prefix BHQ) provides personal interview data on defecation function in adults aged ≥20 years. Participants with a defecation frequency of ≤3 week were considered to have chronic constipation [18].
Covariates
We adjusted the regression model of covariates associated with allergies. In model 1, we adjusted the demographic data, including age, sex, race/ethnicity (e.g., Mexican-Americans, other Hispanics, non-Hispanic whites, and non-Hispanic blacks), and education level (e.g., above high school, high school, and below high school), obtained through the questionnaire.
In model 2, we added information on drinking and smoking habits from the relevant questionnaires. Smoking was defined as having smoked at least 100 cigarettes in a lifetime, and drinking was defined as having consumed at least 12 alcoholic beverages a year. Physical activity within a week was divided into self-reported “strenuous” and “non-strenuous” physical activity. Dietary information on total fat, protein, fibre, and total daily energy intake was collected by trained interviewers.
Statistical Analysis
Demographic and lifestyle characteristics and questionnaires data are expressed as weighted percentages of classified variables. The Rao-Scott χ2 test was used to compare the percentage of classified variables between allergic and non-allergic participants. Logistic regression analysis was performed to examine the relationship between allergy and chronic constipation [19]. In model 1, sex, age, race/ethnicity, and education level were adjusted. Meanwhile, model 2 was adjusted for model 1 covariates; smoking status; alcohol consumption; physical activity; and total fat, protein, fibre, and total daily energy intake. To further study the relationship between sIgE level and chronic constipation, restricted cubic spline analysis was performed in the fully adjusted model. A p value of <0.05 was considered statistically significant [20].
The sampling weight (WTMEC2YR) of the population sampling inspection and the research design variables (SDMVPSU and SDMVSTRA) were used for data analysis. Sampling weight is a measure of the number of people in the population represented by that sample person in the NHANES, reflecting the unequal probability of selection. It is an adjustment for sample person non-response and accounts the differences between the final sample and total population based on independent population control totals. Design variables (SDMVPSU and SDMVSTRA) are a collection of secondary sampling units aggregated into groups for variance estimation. In all analyses, the complexity of sampling design was considered using the complex sample module in SPSS (IBM Corp, New York, NY, USA) to specify the main sampling unit (SDMVPSU), stratum (SDMVSTRA), and weight.
Results
Study Population for Epidemiologic Analysis
Table 1 shows the sample size and weight characteristics of the study population. Of the 3,837 participants aged ≥20 years, 48.5% were women. The respondents were mainly non-Hispanic whites (74%), and 27.2% respondents had an education level of college graduate or above. In total, 50.5%, 25.2%, and 63.3% respondents were non-smokers, non-alcohol drinkers, and performed non-strenuous physical activity, respectively. Table 1 summarizes the other baseline characteristics of the participants stratified by sIgE sensitization. In the USA, in addition to age (p < 0.001), sex (p < 0.001), and race (p < 0.001), sIgE sensitization was related to smoking status (p < 0.001), physical activity (p < 0.047), and protein intake (p < 0.019). There was no significant relationship between sIgE sensitization and education level (p = 0.241), alcohol consumption (p = 0.233), total energy intake (p = 0.61), and total fat (p = 0.511) and fibre (p = 0.312) intake.
Table 1.
Sample size (n) and weighted characteristics of NHANES 2005–2006 participants
| Total |
Sensitized |
Non-sensitized |
p value | ||||
|---|---|---|---|---|---|---|---|
| N | Weighted | N | Weighted | N | Weighted | ||
| Characteristics | |||||||
| Sex | |||||||
| Male, % (SE) | 1,851 | 48.5 (0.7) | 923 | 23.9 (0.7) | 928 | 24.6 (0.9) | 0.000 |
| Female, % (SE) | 1,986 | 51.5 (0.7) | 804 | 19.7 (0.9) | 1,182 | 31.8 (0.8) | |
| Age | |||||||
| 18–44, % (SE) | 1,806 | 47.7 (2.3) | 937 | 24.3 (1.5) | 896 | 23.5 (1.3) | |
| 45–69, % (SE) | 1,428 | 41.3 (1.4) | 595 | 16.2 (0.6) | 833 | 25.1 (1.1) | 0.000 |
| ≥70, % (SE) | 603 | 11.0 (1.4) | 195 | 3.2 (0.4) | 408 | 7.8 (1.0) | |
| Race/ethnicity | |||||||
| Mexican American, % (SE) | 776 | 7.8 (1.0) | 349 | 3.5 (0.5) | 427 | 4.3 (0.5) | |
| Other Hispanic, % (SE) | 117 | 3.3 (0.8) | 62 | 1.8 (0.5) | 55 | 1.5 (0.4) | |
| Non-Hispanic white, % (SE) | 1,988 | 74 (2.7) | 796 | 30.2 (1.4) | 1,192 | 43.8 (2.0) | 0.000 |
| Non-Hispanic black, % (SE) | 822 | 10.4 (1.8) | 370 | 4.6 (0.8) | 452 | 5.8 (1.1) | |
| Other race, % (SE) | 134 | 4.6 (0.5) | 68 | 2.3 (0.3) | 66 | 2.2 (0.3) | |
| Education level | |||||||
| Less than 9th grade, % (SE) | 420 | 5.7 (0.8) | 166 | 2.3 (0.4) | 254 | 3.4 (0.4) | |
| 9–11th grade, % (SE) | 579 | 10.7 (1.1) | 255 | 4.1 (0.5) | 324 | 6.6 (0.7) | |
| High school grad or equivalent, % (SE) | 924 | 24.8 (0.9) | 409 | 10.4 (0.6) | 515 | 14.4 (0.8) | 0.241 |
| Some college or AA degree, % (SE) | 1,112 | 31.6 (1.2) | 514 | 14.1 (1.0) | 598 | 17.5 (0.8) | |
| College graduate or above, % (SE) | 802 | 27.2 (2.3) | 383 | 12.6 (1.5) | 419 | 14.5 (1.2) | |
| Smoking status | |||||||
| Yes, % (SE) | 1,852 | 49.5 (1.4) | 774 | 19.7 (0.6) | 1,078 | 29.8 (1.1) | 0.000 |
| No, % (SE) | 1,985 | 50.5 (1.4) | 953 | 24 (1.4) | 1,032 | 26.6 (0.7) | |
| Drinking status | |||||||
| Yes, % (SE) | 2,667 | 74.8 (1.9) | 1,228 | 33.8 (0.8) | 1,439 | 41.5 (1.6) | |
| No, % (SE) | 1,170 | 25.2 (1.9) | 499 | 10.3 (1.3) | 671 | 14.9 (1.0) | 0.233 |
| Physical activity | |||||||
| Vigorous physical activity, % (SE) | 1,198 | 36.7 (1.4) | 587 | 17.1 (1.1) | 611 | 19.6 (0.9) | |
| No vigorous activity, % (SE) | 2,639 | 63.3 (1.4) | 1,140 | 26.6 (0.8) | 1,499 | 36.7 (1.3) | 0.047 |
| Energy, kcal | |||||||
| ≤1,470, % (SE) | 959 | 23.4 (1.4) | 410 | 9.8 (1.0) | 549 | 13.6 (0.8) | |
| 1,470–2,009, % (SE) | 960 | 24.3 (0.8) | 399 | 10.0 (0.5) | 561 | 14.2 (0.7) | |
| 2,009–2,660, % (SE) | 959 | 24.8 (0.8) | 434 | 10.7 (0.5) | 525 | 14.1 (0.6) | 0.61 |
| >2,660, % (SE) | 959 | 27.5 (1.2) | 484 | 13.1 (0.8) | 475 | 14.4 (0.6) | |
| Protein, g | |||||||
| ≤53.09, % (SE) | 959 | 23.2 (1.2) | 393 | 9.2 (0.8) | 566 | 14.0 (1.0) | |
| 53.09–74.9, % (SE) | 960 | 24.0 (0.7) | 429 | 10.8 (0.6) | 531 | 13.2 (0.4) | |
| 74.9–104.16, % (SE) | 959 | 25.2 (0.9) | 415 | 10.3 (0.5) | 544 | 14.8 (0.8) | 0.019 |
| >104.16, % (SE) | 959 | 27.7 (1.0) | 490 | 13.3 (0.5) | 469 | 14.4 (0.9) | |
| Total fat, g | |||||||
| ≤49.21, % (SE) | 961 | 22.9 (1.2) | 412 | 9.7 (0.8) | 549 | 13.2 (0.7) | |
| 49.21–73.25, % (SE) | 958 | 23.9 (0.9) | 408 | 10.1 (0.7) | 550 | 13.8 (0.8) | |
| 73.25–104.22, % (SE) | 960 | 25.6 (0.7) | 439 | 11.3 (0.5) | 521 | 14.4 (0.5) | 0.511 |
| >104.22, % (SE) | 958 | 27.5 (1.3) | 468 | 12.5 (0.8) | 490 | 15.0 (0.9) | |
| Fibre, g | |||||||
| ≤9.3, % (SE) | 980 | 25.2 (1.1) | 432 | 10.5 (0.7) | 548 | 14.7 (0.9) | |
| 9.3–14.1, % (SE) | 959 | 25.3 (0.6) | 445 | 11.8 (0.7) | 514 | 13.5 (0.6) | |
| 14.1–20.4, % (SE) | 949 | 25.2 (0.7) | 436 | 11.0 (0.6) | 513 | 14.1 (0.6) | 0.312 |
| >20.4, % (SE) | 949 | 24.3 (0.8) | 414 | 10.3 (0.6) | 535 | 14.1 (0.5) | |
Sensitized = serum-specific IgE ≥0.35 kUA/L; non-sensitized = serum-specific IgE <0.35 kUA/L. Proportions were compared using the Rao-Scott χ2 test.
Associations between Chronic Constipation and Allergic Sensitization
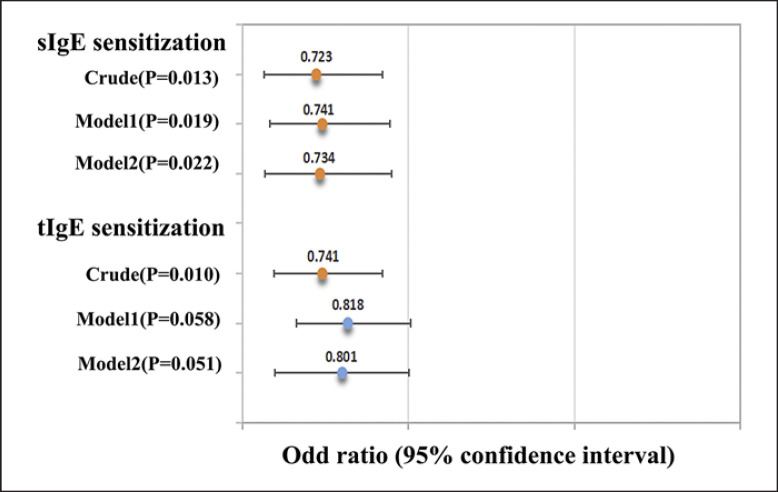
The relationship between chronic constipation and allergic sensitization was investigated using a logistic regression model (Fig. 1). The data showed that the risk of chronic constipation in patients with sIgE sensitization was 0.723 times lower than that in the general population (odds ratio [OR] = 0.723, 95% confidence interval [CI] = 0.566–0.923). In adjusted model 1, patients with sIgE sensitization were less likely to have chronic constipation than the general population (OR = 0.741, 95% CI = 0.582–0.944). In adjusted model 2, there was a negative association between sIgE sensitization and chronic constipation (OR = 0.734, 95% CI = 0.568–0.950). However, in the crude model, tIgE-sensitized participants were less likely to have chronic constipation than the general population (OR = 0.741, 95% CI = 0.596–0.922). After adjusting for confounding factors, the association between tIgE sensitization and chronic constipation disappeared.
Fig. 1.
Associations (OR [95% CI]) between chronic constipation and allergic sensitization in NHANES 2005–2006 participants. Model 1 was adjusted for gender, age, race/ethnicity, and education level. Model 2 was adjusted for Model 1, smoking status, and alcohol consumption, physical activity within a week, and total fat, protein, fibre, and total daily energy intake. Orange dots indicate statistical significance (p value < 0.05).
Association between Chronic Constipation and 19 Allergen sIgE Sensitization
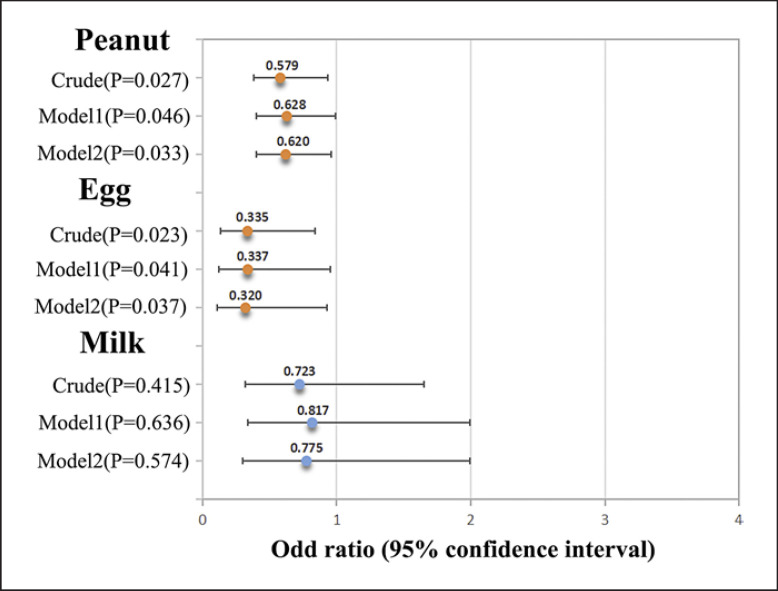
Figure 2 shows the association between chronic constipation and food allergens. The results showed that the risk of chronic constipation in patients with peanut allergy was 0.579 times lower than that in the general population (OR = 0.579, 95% CI = 0.381–0.935). Patients with egg allergy were less likely to have chronic constipation than the general population (OR = 0.335, 95% CI = 0.134–0.838). After adjusting the covariates, the direction of the association remained unchanged. However, there was no association between milk allergy and chronic constipation (OR = 0.723, 95% CI = 0.317–1.651).
Fig. 2.
Associations (OR [95% CI]) between chronic constipation and allergic sensitization of food allergen in NHANES 2005–2006 participants. Model 1 was adjusted for gender, age, race/ethnicity, and education level. Model 2 was adjusted for Model 1, smoking status, and alcohol consumption, physical activity within a week, and total fat, protein, fibre, and total daily energy intake. Orange dots indicate statistical significance (p value < 0.05).
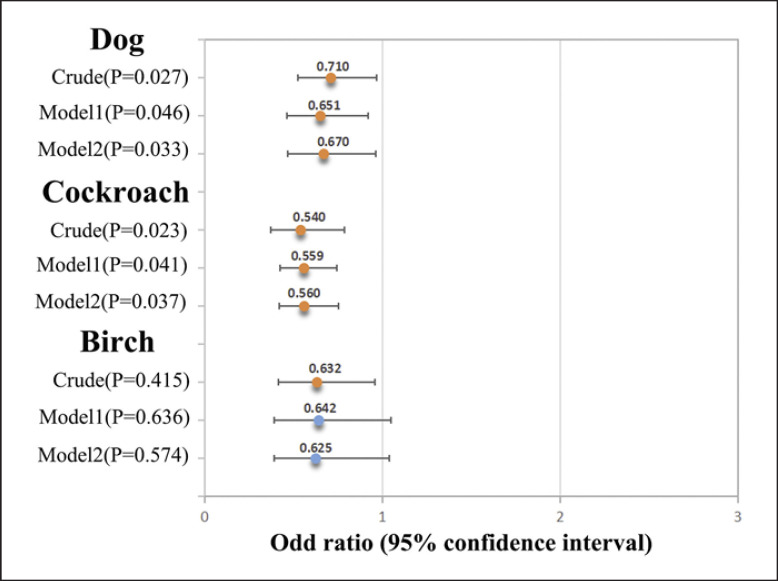
Figure 3 shows the association between chronic constipation and inhaled allergens. There was a negative association between dog allergy and chronic constipation (OR = 0.723, 95% CI = 0.522–0.965). The risk of chronic constipation in patients with cockroach allergy was 0.54 times lower than that in the general population (OR = 0.540, 95% CI, 0.373–0.784). After adjusting for covariates, the direction of the association remained unchanged. In the crude model, there was a negative association between birch allergy and chronic constipation (OR = 0.632, 95% CI = 0.416–0.959). However, after adjusting for variables, the association disappeared. No association was found between the other 13 allergens and chronic constipation (online suppl. material 1; for all online suppl. material, see www.karger.com/doi/10.1159/000527159).
Fig. 3.
Associations (OR [95% CI]) between chronic constipation and allergic sensitization of Inhaled allergen in NHANES 2005–2006 participants. Model 1 was adjusted for gender, age, race/ethnicity, and education level. Model 2 was adjusted for Model 1, smoking status, and alcohol consumption, physical activity within a week, and total fat, protein, fibre, and total daily energy intake. Orange dots indicate statistical significance (p value < 0.05).
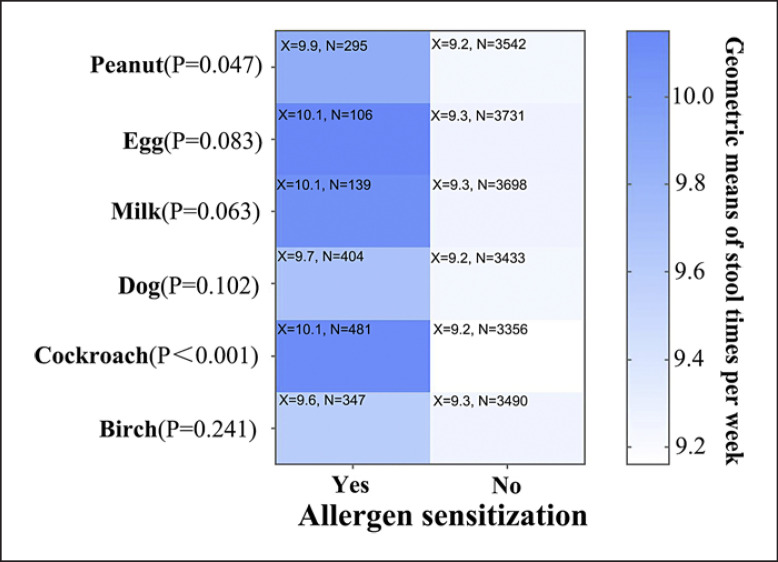
Defecation Frequency and Allergic Sensitization
Figure 4 shows the number of bowel movements in the six allergen-sensitized and non-allergen-sensitized groups. Participants sensitized to the six allergens had more bowel movements per week than those not sensitized. The number of defecations per week in participants sensitized to peanuts (9.9 ± 5.8) increased compared to that in participants not sensitized to peanuts (9.2 ± 5.2) (p = 0.047). Compared to the weekly defecation frequency in non-cockroach-sensitized participants (9.2 ± 5.1), that in cockroach-sensitized participants increased (10.1 ± 5.9) (p < 0.001).
Fig. 4.
Defecation times per week between allergen sensitized group and non-allergenic group. × geometric means of stool times per week; N: number of participants per group.
Discussion/Conclusion
This epidemiological study assessed the association between specific allergens and chronic constipation using the 2005–2006 NHANES data of participants aged ≥20 years. We found that sIgE sensitization might be negatively associated with chronic constipation. Specifically, the logistic regression model adjusted for potential confounding factors revealed that sIgE-sensitized patients had a 0.723 times lower risk of having chronic constipation than the general population; however, the association between tIgE sensitization and chronic constipation disappeared after adjusting for confounding factors.
Logistic regression was used to explore the relationship between 19 allergens and chronic constipation. Among patients with food allergies, those with peanut and egg allergies were 0.579 and 0.335 times, respectively, less likely to have chronic constipation than the general population. There was no association between milk allergy and chronic constipation. Among inhaled allergens, patients with dog and cockroach allergies were 0.723 and 0.54 times, respectively, less likely to have chronic constipation than the general population. Moreover, compared to the general population, patients allergic to peanuts and cockroaches had a significantly increased frequency of defecations per week. Thus, the findings imply that there is a negative association between adult sIgE sensitization and chronic constipation.
Few studies have shown the link between chronic constipation and allergy in adults. In a controlled trial of 60 infants with chronic functional constipation and 30 healthy infants, milk allergy was a common cause of constipation in infants and children [21]. Among the 36 children with chronic constipation, 14 were had milk intolerance and three had multiple food intolerance [22]. Rokaite et al. [23] showed that 80% children with atopic dermatitis had food allergies, and 63.4% complained of gastrointestinal diseases, most commonly constipation. Studies on the relationship between allergic diseases and constipation mostly focused on infants and young children and food allergens, especially milk. However, inhaled allergens can also pose serious health and financial burden. Therefore, studies on the impact of these allergens on adults are required.
The analysis of 19 allergens revealed that the negatively associated antigens were species aggregated. This finding could be attributed to the following. First, there is a difference between food and inhaled allergies in adults and children. Food allergies are more common among children than among adults. In the 2005 NHANES, 4.2% American children aged 1–5 years were positive for food serum sIgE; the prevalence was reduced to 3.8% in individuals aged 6–19 years and 1.3% in older adults aged ≥60 years [24]. Moreover, milk allergies account for 2.5% of all food allergies in children. However, many of these early-onset allergies are associated with the ultimate development of tolerance, which leads to a different range of allergies in adults. The most common allergens in adults are peanuts, nuts, and seafood [25]. This observation may help explain why milk allergy was not associated with constipation in adults in this study. In addition, respiratory allergic diseases, such as asthma, can be caused by various inhaled environmental allergens. Its main feature is the increased activation of smooth muscle around the airway, and the endocrine regulation of airway contraction may affect intestinal health. In particular, guanosine and uroguanosine affect airway contractility [26]; the activation of guanosine family is negatively related to constipation in irritable bowel syndrome [27]. Second, the causes of constipation in adults are different in infants and young children. The prevalence of chronic constipation increases with age. The causes of allergic exacerbation of constipation in children are mostly related to increased anal sphincter pressure and intestinal submucosal eosinophil infiltration [9]. However, in adults with slow-transit constipation, colonic motility mediated by 5-hydroxytryptamine may be impaired [28]. Moreover, inhibition of 5-hydroxytryptamine released by mast cells decreased T helper type 2 cytokines and sIgE levels in mouse models of airway inflammation [29]. Third, this study did not consider the diet of the participants; dietary avoidance may be better achieved in the adult population. Constipation caused by food allergy can be relieved after diet avoidance, and there is evidence that milk tolerance is better achieved after 12 months of strict elimination of milk [21]. Moreover, this may help explain the negative association between constipation and allergy in adults. Finally, the influence of intestinal flora on the relationship between constipation and allergy is also a factor worth considering. The association between the relatively high abundance of specific fungi (Candida albicans) and the relatively low abundance of some bacteria (such as Bifidobacterium and Lactobacillus) has been reported in human and animal models [30]. Studies in adults have consistently shown that gastrointestinal microflora, bifidobacterial, and lactobacilli abundance in constipation and irritable bowel syndrome is significantly lower than that in the control group [31]. In 1988, Koivikko et al. [32] observed that delayed allergic reaction was negatively associated with the growth of nasopharyngeal and anal C. albicans. These findings are consistent with the concept that immune impairment of C. albicans may lead to an increase in IgE response. The association between intestinal fungi and bacteria may indirectly explain the negative association between constipation and allergy in adults.
In addition, Aguilera-Lizarraga et al. [33] discovered a new mechanism of local immune response induced by food antigens. Their studies have shown that bacterial infections and toxins can trigger an immune response, causing mice to produce dietary antigen sIgE antibodies, which are limited to the gut and not the serum. IgE- and mast cell-dependent mechanisms induce increased visceral pain after intake of dietary antigens. Injection of food antigen into the intestinal mucosa of patients with irritable bowel syndrome can cause local oedema and mast cell activation. These results reveal the close relationship between allergic reactions and gastrointestinal symptoms, especially abdominal pain. However, further studies are needed to clarify the specific mechanism underlying the association between constipation and allergy.
This study has several advantages and limitations. The main strength of our study was the large sample size of adults aged ≥20 years. In addition, after fully adjusting for confounding factors, the association between chronic constipation and allergy remained unchanged; the analyses of chronic constipation and sIgE levels of 19 allergen helped elucidate this relationship. However, our study has some limitations. First, it was a cross-sectional study of 2005–2006 NHANES data. Thus, it is difficult to infer the causal relationship between chronic constipation and allergens. Second, although the assessment of constipation in NHANES is reasonable, it may be affected by subjective judgment and memory bias of participants. Third, medications, such as opioids and antipsychotics, are important factors that can cause constipation or diarrhoea [34, 35]. This study did not adjust for these factors as covariates in the model, which might have introduced bias. Finally, our results are adjusted for several major potential confounding factors; however, it is difficult to control for unknown factors.
In summary, this epidemiological study assessed the association between chronic constipation and allergy. Among the NHANES participants aged ≥20 years, representing adults in the USA, sIgE sensitization (mainly eggs, peanuts, cockroaches, and dog) was negatively associated with chronic constipation. However, the serum sIgE levels of different allergens cannot be summarized by a single positive or negative association. The specific association mechanism needs to be further studied.
Statement of Ethics
The protocols and procedures adopted by NHANES protect the personal information of participants. All participants provided written informed consent. All NHANES investigations were approved by the National Center for Health Statistics Research Ethics Review Board (ERB), and the ERB protocol number of NHANES 2005–2006 is #2005-06.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
This work was funded by the National Natural Science Foundation of China (Reference Numbers 81870705 and 81970860).
Author Contributions
Conception and design: Yang Xi, Wo-Er Jiao, and Ze-Zhang Tao. Development of methodology: Yang Xi, Wo-Er Jiao, Yu-Qin Deng, and Ze-Zhang Tao. Acquisition of data: Yang Xi, Wo-Er Jiao, and Fen Li. Analysis and interpretation of data (e.g., statistical analysis, computational analysis): Yang Xi, Wo-Er Jiao, Fen Li, and Han-Da Li. Writing, review, and/or revision of the manuscript: Yang Xi, Wo-Er Jiao, and Gan Lu. Technical or material support: Fen Li, Yu-Qin Deng, and Ze-Zhang Tao.
Data Availability Statement
All data generated or analysed during this study are included in this article and its online supplementary material files. Further enquiries can be directed to the corresponding author.
Supplementary Material
Supplementary data
Acknowledgments
We thank all colleagues who helped with this study.
Funding Statement
This work was funded by the National Natural Science Foundation of China (Reference Numbers 81870705 and 81970860).
References
- 1.Murrison LB, Brandt EB, Myers JB, Hershey GKK. Environmental exposures and mechanisms in allergy and asthma development. J Clin Invest. 2019;129((4)):1504–1515. doi: 10.1172/JCI124612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Balbino B, Conde E, Marichal T, Starkl P, Reber LL. Approaches to target IgE antibodies in allergic diseases. Pharmacol Ther. 2018;191:50, 64. doi: 10.1016/j.pharmthera.2018.05.015. [DOI] [PubMed] [Google Scholar]
- 3.Pritchard DI, Falcone FH, Mitchell PD. The evolution of IgE-mediated type I hypersensitivity and its immunological value. Allergy. 2021;76((4)):1024–1040. doi: 10.1111/all.14570. [DOI] [PubMed] [Google Scholar]
- 4.Zellweger F, Eggel A. IgE-associated allergic disorders recent advances in etiology, diagnosis, and treatment. Allergy. 2016;71((12)):1652–1661. doi: 10.1111/all.13059. [DOI] [PubMed] [Google Scholar]
- 5.Travaglini A, Masieri S, Cavaliere C, Brighetti MA. Pollens causing allergy and their monitoring by aerobiology and phenology. J Biol Regul Homeost Agents. 2018;32((1 Suppl 1)):13–18. [PubMed] [Google Scholar]
- 6.Loftus PA, Wise SK. Epidemiology and economic burden of asthma. Int Forum Allergy Rhinol. 2015;5((Suppl 1)):S7–S10. doi: 10.1002/alr.21547. [DOI] [PubMed] [Google Scholar]
- 7.Bousquet J, Anto JM, Bachert C, Baiardini I, Bosnic-Anticevich S, Walter Canonica G, et al. Allergic rhinitis. Nat Rev Dis Primers. 2020;6((1)):95. doi: 10.1038/s41572-020-00227-0. [DOI] [PubMed] [Google Scholar]
- 8.Mahdavinia M. Food allergy in adults presentations, evaluation, and treatment. Med Clin North Am. 2020;104((1)):145–155. doi: 10.1016/j.mcna.2019.08.008. [DOI] [PubMed] [Google Scholar]
- 9.Vriesman MH, Koppen IJN, Camilleri M, Di Lorenzo C, Benninga MA. Management of functional constipation in children and adults. Nat Rev Gastroenterol Hepatol. 2020;17((1)):21–39. doi: 10.1038/s41575-019-0222-y. [DOI] [PubMed] [Google Scholar]
- 10.Belsey J, Greenfield S, Candy D, Geraint M. Systematic review impact of constipation on quality of life in adults and children. Aliment Pharmacol Ther. 2010;31((9)):938–949. doi: 10.1111/j.1365-2036.2010.04273.x. [DOI] [PubMed] [Google Scholar]
- 11.Carroccio A, Iacono G. Review article chronic constipation and food hypersensitivity - an intriguing relationship. Aliment Pharmacol Ther. 2006;24((9)):1295–1304. doi: 10.1111/j.1365-2036.2006.03125.x. [DOI] [PubMed] [Google Scholar]
- 12.Heine RG. Gastroesophageal reflux disease colic and constipation in infants with food allergy. Curr Opin Allergy Clin Immunol. 2006;6((3)):220–225. doi: 10.1097/01.all.0000225164.06016.5d. [DOI] [PubMed] [Google Scholar]
- 13.Tokunaga T, Ninomiya T, Osawa Y, Imoto Y, Ito Y, Takabayashi T, et al. Factors associated with the development and remission of allergic diseases in an epidemiological survey of high school students in Japan. Am J Rhinol Allergy. 2015;29((2)):94–99. doi: 10.2500/ajra.2015.29.4135. [DOI] [PubMed] [Google Scholar]
- 14.Meng X, Zhang G, Cao H, Yu D, Fang X, de Vos WM, et al. Gut dysbacteriosis and intestinal disease mechanism and treatment. J Appl Microbiol. 2020;129((4)):787–805. doi: 10.1111/jam.14661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chiu CY, Chan YL, Tsai MH, Wang CJ, Chiang MH, Chiu CC. Gut microbial dysbiosis is associated with allergen-specific IgE responses in young children with airway allergies. World Allergy Organ J. 2019;12((3)):100021. doi: 10.1016/j.waojou.2019.100021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li S, Zhao CJ, Hua HL, Deng YQ, Tao ZZ. The association between allergy and sinusitis a cross-sectional study based on NHANES 2005-2006. Allergy Asthma Clin Immunol. 2021;17((1)):135. doi: 10.1186/s13223-021-00642-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee SE, Baek JY, Han K, Koh EH. Insulin resistance increases serum immunoglobulin E sensitization in premenopausal women. Diabetes Metab J. 2021;45((2)):175–182. doi: 10.4093/dmj.2019.0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilson PB. Associations between physical activity and constipation in adult Americans results from the National health and nutrition examination survey. Neurogastroenterol Motil. 2020;32((5)):e13789. doi: 10.1111/nmo.13789. [DOI] [PubMed] [Google Scholar]
- 19.Xi Y, Deng YQ, Chen SM, Kong YG, Xu Y, Li F, et al. Allergy-related outcomes and sleep-related disorders in adults a cross-sectional study based on NHANES 2005–2006. Allergy Asthma Clin Immunol. 2022;18((1)):27. doi: 10.1186/s13223-022-00669-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li D, Wu Q, Tong Y, Zheng H, Li Y. Dietary beta-carotene intake is inversely associated with anxiety in US midlife women. J Affect Disord. 2021;287:96, 100. doi: 10.1016/j.jad.2021.03.021. [DOI] [PubMed] [Google Scholar]
- 21.El-Hodhod MA, Younis NT, Zaitoun YA, Daoud SD. Cow's milk allergy related pediatric constipation appropriate time of milk tolerance. Pediatr Allergy Immunol. 2010;21((2 Pt 2)):e407–e412. doi: 10.1111/j.1399-3038.2009.00898.x. [DOI] [PubMed] [Google Scholar]
- 22.Iacono G, Bonventre S, Scalici C, Maresi E, Di Prima L, Soresi M, et al. Food intolerance and chronic constipation manometry and histology study. Eur J Gastroenterol Hepatol. 2006;18((2)):143–150. doi: 10.1097/00042737-200602000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Rokaite R, Labanauskas L. Gastrointestinal disorders in children with atopic dermatitis. Medicina. 2005;41((10)):837–845. [PubMed] [Google Scholar]
- 24.Liu AH, Jaramillo R, Sicherer SH, Wood RA, Bock SA, Burks AW, et al. National prevalence and risk factors for food allergy and relationship to asthma results from the National health and nutrition examination survey 2005–2006. J Allergy Clin Immunol. 2010;126((4)):798.e13–806.e13. doi: 10.1016/j.jaci.2010.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Turnbull JL, Adams HN, Gorard DA. Review article the diagnosis and management of food allergy and food intolerances. Aliment Pharmacol Ther. 2015;41((1)):3–25. doi: 10.1111/apt.12984. [DOI] [PubMed] [Google Scholar]
- 26.Bosse Y. Endocrine regulation of airway contractility is overlooked. J Endocrinol. 2014;222((2)):R61–R73. doi: 10.1530/JOE-14-0220. [DOI] [PubMed] [Google Scholar]
- 27.Forte LR., Jr Uroguanylin and guanylin peptides pharmacology and experimental therapeutics. Pharmacol Ther. 2004;104((2)):137–162. doi: 10.1016/j.pharmthera.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 28.Black CJ, Ford AC. Chronic idiopathic constipation in adults epidemiology, pathophysiology, diagnosis and clinical management. Med J Aust. 2018;209((2)):86–91. doi: 10.5694/mja18.00241. [DOI] [PubMed] [Google Scholar]
- 29.Lima C, Souza VMO, Soares AL, Macedo MS, Tavares-de-Lima W, Vargaftig BB. Interference of methysergide a specific 5-hydroxytryptamine receptor antagonist with airway chronic allergic inflammation and remodelling in a murine model of asthma. Clin Exp Allergy. 2007;37((5)):723–734. doi: 10.1111/j.1365-2222.2007.02700.x. [DOI] [PubMed] [Google Scholar]
- 30.Zeise KD, Woods RJ, Huffnagle GB. Interplay between candida albicans and lactic acid bacteria in the gastrointestinal tract impact on colonization resistance, microbial carriage, opportunistic infection, and host immunity. Clin Microbiol Rev. 2021;34((4)):e0032320. doi: 10.1128/CMR.00323-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang L, Alammar N, Singh R, Nanavati J, Song Y, Chaudhary R, et al. Gut microbial dysbiosis in the irritable bowel syndrome a systematic review and meta-analysis of case-control studies. J Acad Nutr Diet. 2020;120((4)):565–586. doi: 10.1016/j.jand.2019.05.015. [DOI] [PubMed] [Google Scholar]
- 32.Koivikko A, Kalimo K, Nieminen E, Viander M. Relationship of immediate and delayed hypersensitivity to nasopharyngeal and intestinal growth of Candida albicans in allergic subjects. Allergy. 1988;43((3)):201–205. doi: 10.1111/j.1398-9995.1988.tb00419.x. [DOI] [PubMed] [Google Scholar]
- 33.Aguilera-Lizarraga J, Florens MV, Viola MF, Jain P, Decraecker L, Appeltans I, et al. Local immune response to food antigens drives meal-induced abdominal pain. Nature. 2021;590((7844)):151–156. doi: 10.1038/s41586-020-03118-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rao SSC, Rattanakovit K, Patcharatrakul T. Diagnosis and management of chronic constipation in adults. Nat Rev Gastroenterol Hepatol. 2016;13((5)):295–305. doi: 10.1038/nrgastro.2016.53. [DOI] [PubMed] [Google Scholar]
- 35.Xu Y, Amdanee N, Zhang X. Antipsychotic-induced constipation a review of the pathogenesis, clinical diagnosis, and treatment. CNS Drugs. 2021;35((12)):1265–1274. doi: 10.1007/s40263-021-00859-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data
Data Availability Statement
All data generated or analysed during this study are included in this article and its online supplementary material files. Further enquiries can be directed to the corresponding author.