Abstract
Objective
suicide represents the second leading cause of death among adolescents (WHO, 2021). A deeper understanding of the characteristics that lead to it is crucial to increase the ability of clinicians in evaluating, treating, and preventing it. The objective of this study is to analyze the differences in impulsivity, externalizing behaviors, emotion dysregulation, and alexithymia between two groups of adolescents, the first presenting suicidal ideation (SI), the second presenting at least one suicide attempt (SA), in an ideation-to-action framework.
Method
we conducted a retrospective study with 190 adolescents (M= 14.5, SD age = 1.63; SI: n = 97, SA: n = 93). All were hospitalized in the Complex Operative Child Neuropsychiatry Hospital Unit (UOC-NPI) of the Hospital-University of Padua. Data were collected using the Youth Self-Report (YSR 11-18), Barratt’s Impulsiveness Scale (BIS-11) and the Toronto Alexithymia Scale (TAS-20) questionnaires.
Results
the SA group obtained higher clinical scores in the YSR “rule-breaking behavior” and “conduct problems” scales, and in total TAS-20.
Conclusions
the role of externalizing problems and alexithymia could open new frontiers in the understanding of suicide. These new data could be useful for the implementation of early screening protocols and for directing clinical interventions, promoting greater emotion regulation and anger management skills among patients
Keywords: adolescents, suicidality, externalizing disorders, emotion dysregulation, alexithymia, impulsivity
Introduction
As the second leading cause of death among adolescents, suicide represents a major public health concern at a global level (Ruch et al., 2019). WHO (World Health Organization) Member States have committed themselves to working towards reducing the rate of suicide by one third by 2030 in member countries, as attested in the WHO Mental Health Action Plan 2013–2030 (WHO, 2021).
Much research has been devoted to examining the risk factors, triggers, and correlates of suicidal behavior in order to facilitate prevention. Of particular relevance are those studies that have attempted to deepen the knowledge surrounding the transition from suicidal ideation to suicidal acts (ideation-to-action framework) (May & Klonsky, 2016). Specifically, Klonsky and May (2015a) have developed the “Three-Step Theory (3ST)” of suicide, which hypothesizes that 1) suicidal ideation results from the combination of pain (usually psychological) and feelings of hopelessness; 2) feelings of connectedness to significant others and/or one’s own life environment represent a key protective factor against escalating suicidal desire; 3) the progression from suicidal ideation to suicide attempts is facilitated by a range of factors (dispositional, acquired, and practical) which contribute to the individual’s capability for suicide.
In their contribution, the authors have generally focused on the common risk factors for suicidal behavior in the transition from ideation to action, and have not expanded as much on the differences that might exist between groups in this regard. Novel factors that can more effectively help in the early identification of individuals as ideators vs. attempters need to be urgently explored.
In particular, the role of impulsivity and externalizing problems in suicidal behavior is still controversial in the literature. Impulsivity has been defined as “a predisposition toward rapid, unplanned reactions to internal or external stimuli without regard to the negative consequences of these reactions to the impulsive individual or to others” (Moeller et al., 2001) and it comprises three components: cognitive impulsiveness, motor impulsiveness, and non-planning impulsiveness (Stanford et al., 2009).
According to some studies, there does not seem to be a statistically significant difference in impulsivity among individuals with suicidal ideation and individuals who have attempted suicide (Klonsky & May, 2015b; Klonsky et al., 2016; Millner et al., 2018); according to others, impulsivity seems to play a decisive role in predicting the transition from suicidal ideation to suicidal acts (Auerbach et al. 2017; Berg et al., 2015; Szanto et al., 2015). In a recent review by McHugh (2019), impulsivity emerges as a differentiating element between youth who present suicidal behavior and controls: the former group seems to be characterized by deficits in cognitive and response inhibition, and by riskier decision-making processes. The association between impulsivity and suicidal behaviors appears in line with the results from studies on adult neurocognitive functions reporting how individuals who have attempted suicide seem less inclined to calculating consequences and estimating effects than suicidal individuals who have not attempted suicide (Szanto et al., 2015), with a decline in executive functions at a 2-year follow-up (Gujral et al., 2016). The relationship between impulsivity and suicidal behavior also appears to be coherent with neurobiological aspects such as the altered development of brain areas associated with impulse inhibition and control (Casey et al., 2008).
According to Kauten and Barry (2016), the externalizing behavior encompasses a wide range of antisocial acts and it includes the aggressive behavior, ADHD and conduct disorder. The association between impulsive traits and externalizing behaviors was found (Jiménez-Barbero et al., 2016), even in longitudinal studies (Ahmad et al., 2017), highlighting that impulsivity is a risk factor for the subsequent development of externalizing problems (Beauchaine et al., 2017).Fewer studies have explored the relationship between externalizing problems and suicide attempts (Witte et al., 2018; Verona et al., 2004; Giupponi et al., 2018). ADHD seems to increase suicide risk through an increase in the severity of comorbid conditions such as mood and conduct disorders.
The relationship between antisociality and suicidality has been also investigated (Verona et al., 2001; Krysinska et al., 2006, Villabolos-Gallegos et al., 2020). Specifically, Villabolos-Gallegos and collegueas (2020) have observed the association between the lack of remorse, sexual assaults, and destruction of property during adolescence on the one hand, and suicidality in adulthood on the other. These findings were already noticed by Pompili and collegueas (2004), according to whom the antisocial personality disorder predicted suicide attempts, which were probably acted out with the purpose to manipulate others. Conversely, Brière and collegueas (2015) found that suicide attempt in adolescence predicted antisocial personality disorder in adulthood. Taking into account the specific traits of antisociality, aggression and sadism have a role in predicting suicidal behaviors (Moselli et al. 2021; Buitron et al. 2018). Moreover, Namuli and collegueas (2021), based on a sample of adolescents with HIV, reported an association between rule breaking behavior and suicidal ideation. The Hare’s theoretical model of Psychopathy (1989) describes the presence of two factors underlying psychopathy, namely, affective-interpersonal deficit and social deviance (Harpur et al., 1989). Controversial findings were observed concerning the relationship between suicidality and these two factors of Hare’s model. On one hand, Chabrol and Saint-Martin (2009) have reported that affective deficit predicted, independently from other variables, suicidal ideation. On the other hand, Verona and collegueas (2001) highlighted an association between a history of suicide attempts and the only component of social deviance. Javdani and collegueas (2011) even observed in the female sample that the callous-unemotional trait protected them from the risk of suicide attempt. On the contrary, other studies highlighted that the comorbidity between depressive symptoms and conduct disorder increased the risk of suicidal ideation, its recurrence and the risk of suicide attempt than the presence of only depressive symptoms or only conduct disorder (Vander Stoep et al., 2011). Conduct problems, which often coexisted with ADHD’s symptoms (Strandheim et al. 2014) and resulted in antisocial personality disorder afterwards (Junewicz& Billick, 2020), increased the risk of suicidal thoughts. In particular, specific traits like rule breaking behavior and impulsivity were associated with the development of suicidality (Strandheim et al., 2014). ADHD’s severe symptoms with high levels of irritability could result in externalizing problems, suicidal behaviors and delinquent traits during adolescence (Galera et al., 2021). These findings demonstrated that externalizing symptoms, in its multiple kinds of expression, are often associated with suicidality. Hence, suicide could be conceived as a self-oriented aggression (Chabrol& Saint-Martin, 2009). It is therefore plausible that the variability in the findings relative to the association between externalizing behaviors (impulsivity-antisociality) and suicidality may be correlated with the interaction between other mediating or moderating factors.
Research has predominantly focused on the connection between suicidal behaviors and internalizing problems (Evans et al., 2004; Nock et al., 2009; Nock et al., 2013; Ribeiro et al., 2018; Carballo et al., 2020). A personality trait which is often related to internalizing problems is alexithymia (Manninen et al., 2011; Coban et al., 2021), defined as the lack of words to describe one’s own feelings (Sifneos, 1973). It is a multidimensional construct, including difficulties in identifying and describing one’s feelings and in externally-oriented thinking (Bagby et al., 2020). Studies found that internalizing symptoms were mainly associated with difficulties in identifying and describing feelings (Manninen et al., 2011), whereas Coban and colleagues (2021) showed that the externally-oriented thinking was higher in a sample with externalizing disorders than a group with internalizing symptoms. Nevertheless, only a limited number of studies has investigated the interaction between alexithymic functioning and externalizing impulsivity-antisociality related elements in suicidal pediatric subjects. It was also highlighted an association with alexithymia both in individuals who present suicidal ideation (De Berardis et al., 2017) and in those who present risk and self-harming behaviors (De Berardis et al., 2017; Iskric et al., 2020; Hemming et al., 2019; Gatta et al., 2016a; Parolin et al., 2018). Especially, it was found that the alexithymic trait more associated with suicidal ideation was the difficulty in identifying feelings (De Berardis et al., 2008; Kim et al., 2016), but when comparing a sample of adolescents with suicidal ideation with a sample of adolescents with attempted suicide, no differences in alexithymic traits were detected, except when the variable of non-suicidal self-harm was considered (Raffagnato et al., 2022).
Alexithymia has an effect on the emotional processing and it is associated with difficulties in emotion regulation. In particular, this association seems to be mediated by emotional awareness and emotional differentiation both in clinical and non-clinical samples (Da Silva et al., 2017). Thompson (2019) defined emotion dysregulation as “patterns of emotional experience or expression that interfere with goal-directed activity.” The association between alexithymia and emotion dys-regulation was further revealed by Venta and colleagues (2013), who showed that this relationship was mediated by the difficulty to tolerate aversive emotional experiences. Furthermore, emotion dysregulation seemed, in turn, to mediate the relationship between alexithymia and aggression in clinical samples, differently from impulsivity which was a mediator of this relationship only in community samples (Velotti et al., 2016). Even though emotion dysregulation and impulsivity are two different constructs (Velotti et al., 2016) associated with different neural mechanisms, individuals with higher impulsivity are more vulnerable to deficits in emotion regulation, according to neurobiological findings (Beauchaine et al., 2017). Difficulty in emotion regulation was associated with both internalizing and externalizing problems (Aldao et al., 2010; Biederman et al., 2012; Thompson, 2019), such as aggressive behavior (Herts et al., 2012), and it was described as a risk factor for suicidal ideation (Joiner, 2005; Anestis et al., 2011; Hatkevich et al., 2019; De Berardis et al., 2020). In particular, Wolff and colleagues (2018) showed an association between emotion dysregulation and chronic suicidal ideation, which, in turn, was associated with a greater number of suicidal attempts. Consistent with this finding, Rajappa and colleagues (2012) also found that suicidal attempters showed higher emotion dysregulation than controls.
A study by Kämpfer and collegueas (2016) on a sample of patients with somatoform disorders further highlighted that those who had attempted suicide presented high levels of alexithymia and the frequent tendency to employ impulsive strategies of anger expression. The authors also emphasized the need for further studies aimed at identifying the mediating and moderating factors, such as personality traits, which may be associate with impulsivity.
Alexithymic characteristics, which are correlated with both somatic symptom disorders (Lanzara et al., 2020; Gatta et al., 2015) and self-harming behaviors (Shettar et al., 2018; Gatta et al., 2016b), have recently been investigated in a study by Raffagnato and collegueas (2020) relative to somatoform disorders in adolescents with non-suicidal self-injury (NSSI). The authors highlighted how the patients with NSSI who also presented both alexithymia and somatization had a more severe psychopathological picture. Over the past two decades, a large body of research has suggested that non-suicidal self-harm behavior is a risk factor for suicidal behavior (Gould & Kramer, 2001; Hamza et al., 2012). From the study by Tang and colleagues (2011) it emerges that a previous history of NSSI can be considered a strong predictor for suicidal behavior. In addition, much research has sought to shed light on the relationship between the NSSI pattern and suicidal behavior. The theories developed in this regard are first based on the diathesis-stress model (Mann, 2003), and second, on the interpersonal theory (Joiner, 2007). Finally, Hamza (2012) proposed a model that seeks to integrate the previous models by bringing them in relationship with a third variable.
Another risk factor for suicide is a psychiatric family history (Brent & Mann, 2005; Qin et al., 2002; Sørensen et al., 2009). A family member with a psychiatric disorder increases both the genetic predisposition (Brent & Mann, 2005) to the disorder, because the stressogenic/ traumatic factors at an environmental level would increase. (Pelkonen&Marttunen, 2003). According to Pelkonen and Marttunen (2003) psychiatric familiarity could contribute to the emergence of conflict situations and frequent quarrels which are considered risk factors.
Consistent with previous studies (Iskric et al., 2020; Hemming et al., 2019; De Berardis et al., 2017; Gatta et al., 2016; Kämpfer et al., 2016; Subic-Wrana et al., 2014), suicide attempts could be considered in those who are unable to express and/or communicate their emotions as the most extreme form of acting out anger and/or putting an end to intolerable emotional experiences accompanying the transition from ideation to action anti-conservative, especially in the presence of impulsive or antisocial tendencies (Hamza et al., 2012).
On the basis of this hypothesis, we propose to compare a group of adolescents with suicidal ideation with one with a suicide attempt to focus on the peculiarities of each, in view of the ideation-to-action framework.
In detail:
We expected that higher levels of impulsivity, aggression and alexithymia more frequently correspond to suicide attempts rather than suicidal ideation alone.
In particular, in the face of so much literature on the association between suicidality and internalizing disorders, we wanted to deepen the component of the externalizing dimension (impulsivity, aggression, antisociality) emotion dysregulation and alex-ithymia in relation to the suicidal phenomenon in adolescence.
The objective of our study was to explore impulsivity, antisociality, emotion dysregulation, and alexithymia in adolescent suicidality, with the aim of contributing to the understanding of suicidal acts in an ideation-to-action framework in order to promote primary and secondary prevention of self-injurious behaviors.
Materials and methods
This study is a retrospective clinical case study; data are collected from medical records, reports of clinical interviews, discharge letters, test administration.
Specifically, the clinical assessment procedure occurring during hospitalization consisted of a multidisciplinary evaluation including medical examinations, diagnostic and therapeutic neuropsychiatric interviews for the patient, and clinical interviews for his/her parents. We analyzed the scores on the psychodiagnostic tests administered to inpatients during clinical interviews for their diagnostic assessment. The anamnestic investigation and clinical interviews with the patient and his/ her parents considered all the socio-demographic, psychopathological, and clinical-symptomatological factors—also about suicidal phenomena (suicidal ideation, suicide attempts, and suicidal method) and non-suicidal self-injurious acts.
Some of the inpatients who had previous access in other mental health services or hospitalizations were involved in treatment when fill in the instruments.
Patients were selected according to the following inclusion criteria:
Inpatients admitted to the Neuropsychiatric Unit of the Padua University Hospital (Italy) between June 2015 and June 2021 with a suicidal ideation and/or attempted suicide. For all participants, it was the first admission when the history of suicidality emerged.
The exclusion criteria were:
Presence of comorbidity of intellectual disability
The adolescents selected for the study and their parents all gave their informed consent to their participation in the study (the neuropsychiatry services all adopt an approved official protocol that uses standardized forms regarding informed consent to data collection for clinical and research purposes).The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Ethics Committee of the Padua University Hospital (protocol code n. 0044914/21).
Tools
The Barratt’s Impulsiveness Scale-11 (BIS-11), measuring impulsiveness, includes 30 items that are scored to yield three factors (attentional, motor, and non-planning impulsiveness) from which combined, a total score is obtained: the higher the score, the greater the level of impulsiveness identified (Patton et al., 1995; Stanford et al., 2009; Fossati et al., 2002).
In particular, a total score greater than or equal to 72 can indicate the presence of high impulsivity, while a score between 52 and 71 is within the normal range (Stanford et al., 2009).
For each item one can select 4 options: Never/Rarely Sometimes/Often Almost always/ Always, an example is “I plan activities carefully”.
Cronbach’s alphas reported ranged from 0.69 to 0.80, which suggests that the set of items has a satisfactory homogeneous quality (Vasconcelos et al, 2012). Basically, the same degree of coefficient (0.79) was found in the Italian validation (Fossati et al., 2001)
The Toronto Alexithymia Scale (TAS 20) is a self-report questionnaire that measures the three factors defining alexithymia: “difficulty in identifying feelings”, “difficulty in communicating feelings to others”, and “externally oriented thinking” (Rieffe et al., 2006; Bressi et al., 1996) For each item, subjects have to express the degree of agreement with the statement, resulting in a score between 20 and 100. Scores below 51 assume that the person does not have alexithymic functioning, a score between 51 and 60 is considered borderline, and a score greater than or equal to 61 indicates the presence of clinically relevant traits of alexithymia. For each item, the subject has to express the degree of agreement with the statement on a 5-point Likert scale. An example of an item is “I am often confused about the emotions I feel,” resulting in a score between 20 and 100. Scores below 51 assume that the person does not have alexithymic functioning, a score between 51 and 60 is considered borderline, and a score greater than or equal to 61 indicates the presence of clinically relevant traits of alexithymia.
Regarding the psychometric properties, coefficient alphas for the full TAS-20 (Toronto Alexithymia Scale) indicate adeguate internal consistency (alpha 0.52-0.77, F1=0.77, F2=0.67, F3=0.52) (Bressi et al., 1996) (for further Italian validation, see Craparo et al., 2015).
The Youth Self Report (YSR) (Achenbach & Rescorla, 2001) is a self-report instrument completed by young people aged 11 years and older, and consists of 112 items on problem behavior and 20 items on patient competence. The items are grouped into scales: those that investigate Problems or Disorders, both in general (Total, Internalizing and Externalizing Problems) and specifically, by means of symptom groupings and attribution of DSM-IV diagnostic classifications. With regard to symptoms, eight Syndrome Scales are provided: withdrawal, somatic complaints, anxiety-depression, social problems, thinking problems, attention problems, destructive behaviour, aggressive behaviour. There are also six DSM-IV diagnostic codings: somatization, anxiety disorders, affective disorders, ADHD, oppositional defiant disorder, conduct disorder. Skills scales, on the other hand, investigate areas of the child's global functioning, including school and extra-school activities, interests and socialization. The answers of each item are divided into: 0 not true (as far as you know), 1 sometimes or somewhat true, and 2 very true or often true, an item example is “Can’t concentrate, can’t pay attention for long.”
The raw scores obtained in the test can be converted into T-scores and behaviors or competences can be assessed as “normal”, “borderline” or “clinical”.
YSR 11–18 (Youth Self-Report), shows good internal validity (Cronbach α=.71-.95) (Pace &Muzi, 2019; Cena et al., 2022; Ebesutani et al., 2011). It is widely used in clinical setting and research to rate juvenile behavior. YSR has been validated in samples of young Italian patients and their parents, showing a good validity and reliability (Frigerio et al., 2004)
Deficient Emotional Self-Regulation (DESR) Profile, which is an index of behavioral and emotional dys-regulation, was calculated by summing the scores of attention problems, anxious/depressed and aggressive problems’ scales. Moderate level of dysregulation is indicated by a score between 180 and 210; a severe level of dysregulation is indicated by a score equal or higher than 210 (Achenbach et al., 2001; Ivanova et al., 2007; Frigerio et al., 2006; Biederman et al., 2012).
Specifically, the cut-offs are as follows: regarding the “syndromic” scales and for the “DSM-oriented” scales a score >69 is considered “clinical”, a score between 65 and 69 “borderline,” and a score <65 “normal”.
Statistics
Data analyses were analyzed using the statistical software Jamovi (2019, https://www.jamovi.org). Clinical data from the test administration were processed using descriptive and inferential statistics. The Chi-square was conducted to analyze possible associations between categorical and ordinal variables (psychiatric familiarity, range of normal, borderline, clinical scores of self-report questionnaire). The threshold for statistical significance was set at p < 0.05.
Participants
Participants were 190 adolescents aged between 10 and 18 years who were followed for suicidal ideation and/or suicide attempt between June 2015 and June 2021. Within the sample, 97 adolescents with suicidal ideation and 93 with a history of suicide attempt were considered. The average age of the sample was 14.5 years.
Results
There aren’t significant differences between age of the group with suicide attempt (mean = 14.5; SD = 1.57) and suicidal ideation (mean = 14.5; SD = 1.69). As regards gender, there is a statistically significant difference in the distribution within the groups (χ2 = 6.79; p = .009): girls represented 80.5% (n = 153) of the sample and 46.4% of them (n = 71) presented suicidal ideation while 53.6% (n = 82) suicide attempt. Males, instead, were 19.5% (n = 37) of the total sample and, among these, 70.3% (n = 26) had suicidal ideation and 29.7% (n = 11) presented a history of suicide attempt.
As regards the presence of non-suicidal self-harm, it was observed in 70.8% of subjects with suicidal ideation (n = 63) and 71.4% of subjects with suicide attempt (n = 60), with no statistically significant difference between the groups (χ2 = 1.40; p = .497). Specifically, in subjects with ideation NSSI was occasional (< 5 acts/ year) in 38.2% (n = 34) and habitual (> or = 5 acts/ year) in 32.6% (n = 29) of subjects. 31.0% of patients with suicide attempt (n = 26) presented occasional non-suicidal self-harm, and 40.5% of the subjects (n = 34) habitual self-harm. 58.1% (n = 32) of patients with suicidal ideation and 51.9% (n = 27) of patients with attempted suicide reported finding emotion relief from mental suffering as the main motivation for NSSI. As to psychiatric familiarity, this was present in 75% (n = 67) of patients with suicide attempt and in 55% (n = 51) of subjects with suicidal ideation alone, with a statistically significant difference between the two groups (χ2 = 8.34; p = .004).
Results concerning the psychopathological profile of the sample examined are presented below. The externalizing behaviors detected with YSR 11-18 are reported first (YSR 11-18 “rule-breaking behavior”, “aggressive behavior” syndromic scale, “conduct disorders” and “ADHD” DSM-Oriented scales), followed by data on impulsivity detected with BIS-11, emotional regulation, with regard to emotional dysregulation profile of the YSR 11-18 (YSR DESR) and the alexithymic characteristics (TAS-20). Comparison data between suicidal ideation group and the suicide attempt group are specified.
Impulsivity (BIS 11)
A Chi-square test was conducted to investigate the distribution of total impulsivity scores (BIS 11) in the normal, borderline and clinical range. The analysis showed no statistically significant differences between the two groups (χ2 = 3.72; p = .156); specifically, scores exceeded the clinical cut-off in 21.9% (n = 7) of the subjects with ideation and in 28.6% (n = 14) of the subjects with suicide attempt (see table 1).
Table 1.
Distribution of total impulsivity scores BIS-11 in borderline and clinical range
| GROUPS | Mean (SD) | %Borderline | %Clinical | Chi-square (χ2;p) | |
|---|---|---|---|---|---|
| BIS 11 TOT | Ideation | 67.22(8.79) | 12.5% | 21.9% | χ2= 3.72 |
| Attempt | 70.04(13.52) | 26.5% | 28.6% | p= .156 |
Note. SD= standard deviation; Effect size of δ≥0.746
Externalising behaviors (YSR 11-18)
The distribution of score range (clinical, borderline, non-clinical) in the two groups was studied by Chi-square test. As regards the variable ‘Rule-breaking behavior,’ emerged a statistically significant difference between the suicidal ideation and suicide attempt groups on the distribution of the score levels (χ2 = 9.04; p = .011): the group of adolescents with attempted suicide revealed clinical level scores compared to the subjects with suicidal ideation who presented scores mostly distributed in the borderline range.
Also, with regard to the DSM-oriented scale of conduct disorder showed statistically significant differences between the two groups (χ2 = 7.72; p = .021), with more frequent borderline and clinical levels in the group with attempted suicide than in the subjects with suicidal ideation, who more often presented scores in the normal range (See table 2).
Table 2.
Esternalising behaviours YSR 11-18
| YSR 11-18 | GROUPS | Mean (SD) | %Borderline | %Clinical | Chi-square (χ2;p) |
|---|---|---|---|---|---|
| Rule-breaking behavior | Ideation | 56.7 (6.72) | 19.2 % | 1.4 % | χ2= 9.04 |
| Attempt | 59.2 (9.29) | 13.2 % | 14.7 % | p=. 011 | |
| Aggressive behavior | Ideation | 59.5 (8.25) | 19.2 % | 9.6 % | χ2= .830 |
| Attempt | 59.9 (9.26) | 14.7 % | 13.2 % | p= .661 | |
| Attention deficit/hyperactivity | Ideation | 57.8 (6.75) | 12.3% | 4.1% | χ2= 4.21 |
| Attempt | 59.3 (8.31) | 13.6% | 13.6% | p=.122 | |
| Conduct problems | Ideation | 56.9 (7.80) | 8.2 % | 6.8 % | χ2= 7.72 |
| Attempt | 59.6 (9.42) | 19.1 % | 16.2 % | p= .021 | |
| Oppositional defiant problems | Ideation | 59.4 (7.80) | 19.2 % | 15.1 % | χ2= .524 |
| Attempt | 59.8 (9.16) | 16.2 % | 19.1 % | p=. 770 |
Note. SD= standard deviation; Effect sizes of δ≥0.55
Emotional Dysregulation
As to the study of emotional regulation, the DESR profile calculated from the subscales Anxiety-Depressive (AD), Aggressive Behaviour (AGG), and Attention Problems (AP) of the YSR 11-18 was examined.
With regard to the DERS profile, in the group with suicidal ideation this is shown at a moderate level in 49.3% of the subjects (n = 36) and severe in 23.3% (n = 17). In the group with suicide attempt the DESR profile was moderate in 38.2% (n = 26) and severe in 29.4% (n = 20) of the cases. No statistically significant differences emerged in the Chi-square test (χ2= 1.78; p= .411) (see table 3).
Table 3.
DESR profile
| GROUPS | Mean (SD) | %Borderline | %Clinical | Chi-square (χ2;p) | |
|---|---|---|---|---|---|
| DESR | Ideation | 193 (25.4) | 49.3% | 23.3% | χ2=1.78; |
| Profile | Attempt | 197 (30.1) | 38.2% | 29.4% | p=.410 |
Note. SD= standard deviation
Alexithymia
With regard to alexithymic characteristics, significant difficulties in managing feelings emerged in the attempted suicide group than in the group with only suicidal ideation. The distribution analysis of the range of the alexithymia total scores (normal, borderline, and clinical) performed by Chi square, shows statistically significant differences between the two groups (χ2 = 8.16; p = .017). In subjects with suicidal ideation the score is clinical in 63.4% (n = 26) and borderline in 19.5% (n = 8) of cases, while in subjects with suicide attempt it was found in 86.0% (n = 43) of cases a clinical score and in 12.0% (n = 6) a score in the borderline range (see table 4).
Table 4.
The distribution of the range of the alexithymia (TAS-20) total scores
| GROUPS | Mean (SD) | %Borderline | %Clinical | χ2;p | |
|---|---|---|---|---|---|
| TAS-20 | Ideation | 65.9 (12.60) | 19.5% | 64.4% | 8.16; |
| TOT | Attempt | 69.7 (9.21) | 12.0% | 86.0% | p=0.017 |
Note. SD= standard deviation; Effect size of δ≥0.686; χ2= Chi-square
Mediation role of externalizing behaviours
We computed the GLM Mediation Analysis to investigate the mediation role of conduct problems and rule-breaking behavior in the relationship between groups (ideation and attempt) and the presence of affective problems that in the t-test differ statistically between the two groups (ideation mean=72.9, SD=11.9; attempt mean=78.1, SD=14.1, F=-2.36, p=.020). The results of GLM (figure 1 and table 5) showed that conduct problems and rule-breaking behavior play a role in mediating the relationship between groups and affective problems.
Figure 1.
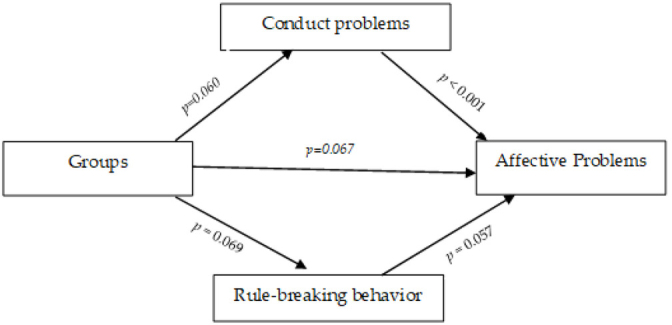
Mediation role of conduct problems and rule breaking behavior
Table 5.
Mediation role of conduct problems and rule breaking behavior
| Effect | Estimate | SE | 95% C.I. | β | z | p | ||
|---|---|---|---|---|---|---|---|---|
| Type | Lower | Upper | ||||||
| Indirect | Groups1 - Conduct problems Affective Problems | 1.924 | 1.073 | -0.179 | 4.027 | 0.069 | 1.79 | 0.073 |
| Groups1 - Rule-breaking behavior - Affective Problems | -0.595 | 0.453 | -1.483 | 0.293 | -0.021 | -1.31 | 0.189 | |
| Groups 1 - Conduct problems | 2.714 | 1.442 | -0.114 | 5.541 | 0.156 | 1.88 | 0.060 | |
| Component | ||||||||
| Conduct problems - Affective Problems | 0.709 | 0.120 | 0.475 | 0.943 | 0.440 | 5.93 | <.001 | |
| Groups 1 - Rule-breaking behavior | 2.449 | 1.349 | -0.194 | 5.093 | 0.151 | 1.82 | 0.069 | |
| Rule-breaking behavior Affective Problems | -0.243 | 0.128 | -0.493 | 0.007 | -0.141 | -1.90 | 0.057 | |
| Direct | Groups 1 - Affective Problems | 3.840 | 2.096 | -0.268 | 7.948 | 0.137 | 1.83 | 0.067 |
| Total | Groups1 - Affective Problems | 5.169 | 2.187 | 0.883 | 9.456 | 0.196 | 2.36 | 0.018 |
Note. Confidence intervals computed with method: Standard (Delta method)
Note. Betas are completely standardized effect sizes
Discussion
The present study aimed at investigating the relationship between impulsivity, externalizing behavior, alexithymia, and emotional dysregulation in adolescent patients with suicidal ideation and suicide attempt, comparing the two subgroups in the perspective of the ideation-to-action framework (May & Klonsky, 2016). The innovative aspect of this study concerns the focus on the externalizing behavior related to the suicidal phenomenon in adolescence, deepening this aspect in view of conspicuous existing literature on the association between suicidality and internalizing disorders (Evans et al., 2004; Nock et al., 2009; Nock et al., 2013, Ribeiro et al., 2018, Carballo et al., 2020). Regarding the characteristics of our sample, an initial finding that differentiated the two subgroups and corroborated the existing literature on risk factors for suicidality (Langhinrichsen-Rohling et al., 2009; May & Klonsky, 2013) was the more significant presence of psychiatric familiarity in the group of adolescents with a suicide attempt, detected to a lesser extent in the group with only suicidal ideation. A family member with a psychiatric disorder deposes both a genetic predisposition to the mental disorder and stressogenic/traumatic factors at the environmental level. A family member with psychiatric pathology could contribute to the emergence of conflictual relational situations and environmental stress that are considered risk factors for children’s development and well-being (Pelkonen & Marttunen, 2003; Zanato et al., 2021). Instead, a family that is able to contain and affectively validate the child could be a resource and a protective factor, creating better conditions to developing emotional self-regulation (Gatta et al., 2016c). In addition, the experiences of stigmatization and exclusion often experienced by the families of those with a psychiatric syndrome could also compromise the sense of belonging to a social network and reduce the protective role of social support (Nock et al., 2008; Pompili et al., 2013).
Focusing on the externalizing behaviors, the considered syndromic and DSM-oriented scales related to these (disrespect for rules, aggressive behavior, conduct disorder, ADHD) we found in those who have attempted suicide significantly higher clinical levels of disregard of rules and conduct disorder than in those who present only anti-conservative ideation.
Among the few studies about the relationship between self-injury and externalizing behaviors, we found McCloskey and Ammerman’s one, highlighting that the presence of an aggressive disorder generally increased the risk of suicide attempts and mortality. Furthermore, it is suggested that the severity of aggression is associated with suicide attempt risk in aggression-related disorders (McCloskey &Ammerman, 2018)
Our data support the hypothesis that a higher level of behavioral problems was expected in the suicide attempt group. Regarding impulsivity, in agreement with other previous studies (Klonsky & May 2015b; Klonsky & May, 2016; Millner et al., 2018), no significant evidence emerged, which might suggest a crucial role of the inability to manage emotions and regulate them rather than impulsivity. In this sense, the data about the level of alexithymia recalls a deficit of emotional regulation, prevalent in our sample, with slightly higher frequency in the subgroup attempted suicide.
Anestis and colleagues' (2011) findings highlight that high levels of emotional dysregulation associated with higher rates of suicidal ideation may act as a protective factor against suicidal acting out. However, the study by Anestis and colleagues (2011) considered a nonclinical sample aged 18-39 years, which may explain the non-overlapping results. A further study, recalling Joiner’s (2005) Interpersonal Theory of Suicide, reported a positive association between the level of emotional dysregulation and the desire to die and a negative association between emotional dysregulation and the acquisition of suicidal capacity, except when non-suicidal self-injury is present, which makes the latter association positive (Heffer & Willoughby, 2018). Moreover, our finding related to the absence of any differences in emotion dysregulation between two groups can be read in light of the fact that literature has found deficits in emotion dysregulation both in samples of suicidal attempters (Rajappa et al., 2012) and in samples with only suicidal ideation (Hatkevich et al., 2019; De Berardis et al., 2020).
About not significant group differences in non-suicidal self-harm we reflect on the role of the NSSI in suicidality. NSSI appears to increase the suicidal risk (Tang et al., 2011; Gould & Kramer, 2001) but it is predictive not only of the suicide attempt but also of suicidal ideation alone (Burke et al., 2016; Guan et al., 2012; Chu et al., 2018). Furthermore, it is possible that suicidal ideation might evolve into attempted suicide.
Regarding alexithymic functioning, the present study goes toward those that speak of an association between alexithymia and suicidal phenomenon (Iskric et al., 2020; Hemming et al., 2019; De Berardis et al., 2017). In particular, in contrast to the study by Hemming and colleagues (2019), where alexithymia was found to be more associated with suicidal ideation than with suicide attempts, in our study, data showed that the group with suicide attempts obtain higher scores in the TAS-20.
In general, the results of the present study can also be conceptualized in the light of Hare's (1989) model. This model proposes a distinction between aspects of social deviance and emotional-interpersonal deficits (Harpur et al., 1989).
As previously underlined by other studies (Verona et al., 2001; Krysinska et al., 2006; Villalobos-Gallegos et al., 2020), the significantly greater presence of clinically relevant antisocial behaviors in the relationship with others and with the environment (e.g., disrespect for the rules and presence of behavioral problems that are expressed in the damage other’s things, lies, acts of cruelty) in the group with attempted suicide rather than in the group with only suicidal ideation suggests how the aspects of social deviance specifically characterize the subjects who carry out a suicidal behavior.
Compared to the deficits in the emotional-interpersonal area, we note on the one hand the absence of differences in emotional dysregulation and aggression, which also represents an index of emotional dysregulation (Achenbach &Rescorla, 2001; Ivanova et al., 2007; Frigerio et al., 2006; Biederman et al., 2012), on the other hand the presence of major traits clinically level alexithymics in the suicide attempted sample. The sample with attempted suicide, therefore, presents more relevant clinically levels in the emotions’ processing (e.g. identification, differentiation and communication of emotions) than those with only suicidal ideation, without this translating into a clinically relevant difference in emotional dysregulation between the two groups.
Moreover, studies highlighted that the comorbidity between depressive symptoms and conduct disorder increased the risk of suicidal ideation, its recurrence and the risk of suicide attempt than the presence of depressive symptoms or conduct disorder only (Vander Stoep et al., 2011); in our research the results of GLM show that conduct problems and rule-breaking behavior play a role in mediating the relationship between suicidality and affective problems.
In light of research, which has shown an association between alexithymia and empathy deficits (Grynberg et al., 2010; Speyer et al., 2022), and between this latter variable and antisocial traits (Burghart et al. 2022; Trivedi-Bateman & Crook, 2022), future studies are needed to better investigate the relationship between alexithymia, empathic abilities, and antisocial behaviors in the samples with suicidality, in order to understand what factors come into play in the relationship between suicidal behavior and antisocial aspects.
The main limitations of this study are the small sample size, the use of self-report instruments, the retrospective design of the study, and the incompleteness of some data related to texting. Data are not available for all subjects included in the study for reasons related to the course of hospitalization, the questionnaires chosen in the clinical evaluation, and the age of the patient.
Therefore, further longitudinal studies and follow-ups at a time distance use multi-method modalities to assess the variables under investigation.
Conclusions
This study outlines some differences between suicidal ideation and suicide attempt in adolescents, specifically regarding the sphere of antisociality and alexithymia.
In agreement with the initial hypotheses and previous studies (Iskric et al., 2020; Hemming et al., 2019; De Berardis et al., 2017; Gatta et al., 2016; Kämpfer et al., 2016; Subic-Wrana et al., 2014), the data collected propose more severe externalizing behaviors and alexithymia in the group with suicide attempts, suggesting that they could play a significant role in implementing suicidal ideation in adolescents with psychological distress, consistently with Hare’s (1989) model (Harpur et al., 1989). According to Subic-Wrana and collegueas (2014) and Kämpfer and collegueas (2016), the suicide attempt could therefore be considered, in those who are unable to express and/ or communicate their emotions, as the most extreme form of acting out anger and/or put an end to intolerable emotional experiences (because poorly adjustable, lack of emotional regulation) accompanying the transition from ideation to anti-conservative act.
In this perspective, the ability of identifying and communicating one's emotions could be a protective factor in the context of suicidality, to be considered therefore in the planning of preventive actions in the self-injurious context. Given the finding of externalizing behaviors as peculiar to those who attempt suicide compared to those who have only suicidal ideation, further prospective studies should investigate the issue, with particular reference to the role of behavioral problems (aggression-antisociality) in the transition from ideation to attempted suicide.
References
- Achenbach, T. M., & Rescorla, L. (2001). Manual for the ASEBA school-age forms and profiles: An integrated system of multi-informant assessment. University of Vermont, Research Center for Children, Youth, & Families: Burlington, VT, USA. [Google Scholar]
- Ahmad, S. I., & Hinshaw, S. P. (2017). Attention-Deficit/ Hyperactivity Disorder, Trait Impulsivity, and Externalizing Behavior in a Longitudinal Sample. Journal of Abnormal Child Psychology, 45(6), 1077-1089. 10.1007/s10802-016-0226-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldao, A., Nolen-Hoeksema, S., & Schweizer, S. (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30(2), 217-37. 10.1016/j.cpr.2009.11.004 [DOI] [PubMed] [Google Scholar]
- Anestis, M. D., Bagge, C. L., Tull, M. T., & Joiner, T. E. (2011). Clarifying the role of emotion dysregulation in the interpersonal-psychological theory of suicidal behavior in an undergraduate sample. Journal of Psychiatric Research, 45(5), 603–611. 10.1016/j.jpsychires.2010.10.013 [DOI] [PubMed] [Google Scholar]
- Auerbach, R. P., Stewart, J. G., & Johnson, S. L. (2017). Impulsivity and suicidality in adolescent inpatients. Journal of Abnormal Child Psychology, 45(1), 91–103. 10.1007/s10802-016-0146-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagby, R. M., Parker, J. D. A., & Taylor, G. J. (2020). Twenty-five years with the 20-item Toronto Alexithymia Scale. Journal of Psychosomatic Research, 131, 109940. 10.1016/j.jpsychores.2020.109940 [DOI] [PubMed] [Google Scholar]
- Berg, J. M., Latzman, R. D., Bliwise, N. G., & Lilienfeld, S. O. (2015). Parsing the heterogeneity of impulsivity: A meta-analytic review of the behavioral implications of the UPPS for psychopathology. Psychological Assessment, 27(4), 1129–1146. 10.1037/pas0000111 [DOI] [PubMed] [Google Scholar]
- Beauchaine, T. P., Zisner, A. R., & Sauder, C. L. (2017). Trait impulsivity and the externalizing spectrum. Annual Re- view of Clinical Psychology, 13, 343-368. 10.1146/annurev-clinpsy-021815-093253 [DOI] [PubMed] [Google Scholar]
- Biederman, J., Perry, C. R., Day, H., Goldin, R. L., Spencer, T., Faraone, S. V., Surman, C. B., & Wozniak, J. (2012). Severity of the aggression/anxiety-depression/ attention (A-A-A) CBCL profile discriminates between different levels of deficits in emotional regulation in youth with ADHD. Journal of Developmental and Behavioral Pediatrics, 33(3), 236-243. 10.1097/dbp.0b013e3182475267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent, D. A., & Mann, J. J. (2005). Family genetic studies, suicide, and suicidal behavior. American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 133(1), 13-24. 10.1002/ajmg.c.30042 [DOI] [PubMed] [Google Scholar]
- Bressi, C., Taylor, G., Parker, J., Bressi, S., Brambilla, V., Aguglia, E., Allegranti, I., Bongiorno, A., Giberti, F., Bucca, M., Todarello, O., Callegari, C., Vender, S., Gala, C., & Invernizzi, G. (1996). Cross validation of the factor structure of the 20-item Toronto Alexithymia Scale: an Italian multicenter study. Journal of Psychosomatic Research, 41(6), 551–559. 10.1016/s0022-3999(96)00228-0 [DOI] [PubMed] [Google Scholar]
- Brière, F. N., Rohde, P., Seeley, J. R., Klein, D., & Lewinsohn, P.M. (2015). Adolescent suicide attempts and adult adjustment. Depression and Anxiety, 32(4), 270-276. https://doi.org/10.1002/da.22296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buitron, V., Hartley, C. M., Pettit, J. W., Hatkevich, C., & Sharp, C. (2018). Aggressive Behaviors and Suicide Ideation in Inpatient Adolescents: The Moderating Roles of Internalizing Symptoms and Stress. Suicide and Life-Threatening Behavior, 48(5), 580-588. 10.1111/sltb.12375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burghart, M., & Mier, D. (2022). No feelings for me, no feelings for you: A meta-analysis on alexithymia and empathy in psychopathy. Personality and Individual Diferences, 194, 111658. 10.1016/j.paid.2022.111658 [DOI] [Google Scholar]
- Burke, T. A., Hamilton, J. L., Cohen, J. N., Stange, J. P., & Alloy, L. B. (2016). Identifying a physical indicator of suicide risk: Non-suicidal self-injury scars predict suicidal ideation and suicide attempts. Comprehensive psychiatry, 65, 7987. 10.1016/j.comppsych.2015.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carballo, J. J., Llorente, C., Kehrmann, L., Flamarique, I., Zuddas, A., Purper-Ouakil, D., Hoekstra, P. J., Coghill, D., Schulze, U., Dittmann, R. W., Buitelaar, J. K., Castro-Fornieles, J., Lievesley, K., Santosh, P., & Arango, C. (2020). Psychosocial risk factors for suicidality in children and adolescents. European Child & Adolescent Psychiatry, 29(6), 759–776. 10.1007/s00787-018-01270-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey, B. J., Jones, R. M., & Hare, T. A. (2008). The Adolescent Brain. Annals of the New York Academy of Sciences, 1124, 111–126. 10.1196/annals.1440.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cena, L., Rota, M., Trainini, A., Zecca, S., Zappa, S. B., Tralli, N., & Stefana, A. (2022). Investigating Adolescents’ Video Gaming and Gambling Activities, and Their Relationship With Behavioral, Emotional, and Social Dificulties: Protocol for a Multi-Informant Study. JMIR Research Proto cols, 11(2), e33376. 10.2196/33376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chabrol, H., & Saint-Martin, C. (2009). Psychopathic traits and suicidal ideation in high-school students. Archives of Suicide Research, 13(1),64-73. 10.1080/13811110802572155 [DOI] [PubMed] [Google Scholar]
- Chu, C., Hom, M. A., Stanley, I. H., Gai, A. R., Nock, M. K., Gutierrez, P. M., & Joiner, T. E. (2018). Non-suicidal self-injury and suicidal thoughts and behaviors: A study of the explanatory roles of the interpersonal theory variables among military service members and veterans. Journal of consulting and clinical psychology, 86(1), 56. 10.1037/ccp0000262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Çoban, Ö. G., & Önder, A. (2021). Alexithymia Is Associated With Internalizing Disorders in a Clinical Adolescent Outpatient Sample. Journal of Nervous and Mental Disease, 209(9), 636-639. 10.1097/nmd.0000000000001390 [DOI] [PubMed] [Google Scholar]
- Craparo, G., Faraci, P., & Gori, A. (2015). Psychometric Properties of the 20-Item Toronto Alexithymia Scale in a Group of Italian Younger Adolescents. Psychiatry investigation, 12(4), 500–507. 10.4306/pi.2015.12.4.500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Da Silva, N. A., Vasco, A. B., & Watson, J. C. (2017). Alexithymia and Emotional Processing: A Mediation Model. Journal of Clinical Psychology, 73(9), 1196-1205. 10.1002/jclp.22422 [DOI] [PubMed] [Google Scholar]
- De Berardis, D., Fornaro, M., Orsolini, L., Valchera, A., Carano, A., Vellante, F., Perna, G., Serafini, G., Gonda, X., Pompili, M., Martinotti, G., & Di Giannantonio, M. (2017). Alexithymia and suicide risk in psychiatric disorders: a mini-review. Frontiers in Psychology, 8, 148. 10.3389/fpsyt.2017.00148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Berardis, D., Fornaro, M., Orsolini, L., Ventriglio, A., Vellante, F., & Di Giannantonio, M. (2020). Emotional Dysregulation in Adolescents: Implications for the Development of Severe Psychiatric Disorders, Substance Abuse, and Suicidal Ideation and Behaviors. Brain Sciences, 10(9), 591. 10.3390/brainsci1009059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Berardis, D., Serroni, N., Campanella, D., Carano, A., Caltabiano, M., Pizzorno, A. M., Valchera, A., Tancredi, L., Sepede, G., Moschetta, F. S., & Ferro, F. M. (2008). Suicide risk among patients with obsessive-compulsive disorder: the role of alexithymia and insight. Giornale Italiano di Psicopatologia, 14, 185-196. [Google Scholar]
- Ebesutani, C., Bernstein, A., Martinez, J. I., Chorpita, B. F., & Weisz, J. R. (2011). The youth self report: Applicability and validity across younger and older youths. Journal of Clinical Child & Adolescent Psychology, 40(2), 338-346. 10.1080/15374416.2011.546041 [DOI] [PubMed] [Google Scholar]
- Evans, E., Hawton, K., & Rodham, K. (2004). Factors associated with suicidal phenomena in adolescents: a systematic review of population-based studies. Clinical Psychology Review, 24(8), 957–979. 10.1016/j.cpr.2004.04.005 [DOI] [PubMed] [Google Scholar]
- Fossati, A., Barratt, E. S., Acquarini, E., & Di Ceglie, A. (2002). Psychometric properties of an adolescent version of the Barratt Impulsiveness Scale-11 for a sample of Italian high school students. Perceptual and Motor Skills, 95(2), 621–635. 10.2466/pms.2002.95.2.621 [DOI] [PubMed] [Google Scholar]
- Fossati, A., Di Ceglie, A., Acquarini, E., & Barratt, E. S. (2001). Psychometric properties of an Italian version of the Barratt Impulsiveness Scale-11 (BIS-11) in nonclinical subjects. Journal of Clinical Psychology, 57, 815-828. 10.1002/jclp.1051 [DOI] [PubMed] [Google Scholar]
- Frigerio, A., Cattaneo, C., Cataldo, M., Schiatti, A., Molteni, M., & Battaglia, M. (2004). Behavioral and emotional problems among Italian children and adolescents aged 4 to 18 years as reported by parents and teachers. European Journal of Psychological Assessment, 20(2), 124-133. 10.1027/1015-5759.20.2.124 [DOI] [Google Scholar]
- Frigerio, A., Vanzin, L., Pastore, V., Nobile, M., Giorda, R., Marino, C., Molteni, M., Rucci, P., Ammaniti, M., Lucarelli, L., Lenti, C., Walder, M., Martinuzzi, A., Carlet, O., Muratori, F., Milone, A., Zuddas, A., Cavolina, P., Nardocci, F., Tullini, A., Morosini, P., Polidori, G., & De Girolamo, G. (2006). The Italian preadolescent mental health project (PrISMA): rationale and methods. International Journal of Methods in Psychiatric Research, 15(1), 22–35. 10.1002/mpr.25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galera, C., Orri, M., Vergunst, F., Melchior, M., Van der Waerden, J., Bouvard, M. P., Collet, O., Boivin, M., Tremblay, R. E., & Côté, S. M. (2021). Developmental profiles of childhood attention-deficit/hyperactivity disorder and irritability: association with adolescent mental health, functional impairment, and suicidal outcomes. Journal of Child Psychology and Psychiatry, 62(2), 232-243. 10.1111/jcpp.13270 [DOI] [PubMed] [Google Scholar]
- Gatta, M., Dal Santo, F., Rago, A., Spoto, A., & Battistella, P. A. (2016a). Alexithymia, impulsiveness, and psychopathology in nonsuicidal self-injured adolescents. Neuropsychiatric Disease and Treatment, 12, 2307–2317. 10.2147/ndt.s106433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatta, M., Rago, A., Dal Santo, F., Spoto, A., & Battistella, P. A. (2016b). Non-suicidal self-injury among Northern Italian High School students: emotional, interpersonal and psychopathological correlates. Journal of Psychopathology, 22(3), 185–190. [Google Scholar]
- Gatta, M., Sisti, M., Sudati, L., Miscioscia, M., & Simonelli, A. (2016c). The Lausanne Trilogue Play within the outcome evaluation in infant mental health: a preliminary report. Research in Psychotherapy: Psychopathology, Process and Outcome, 19(1), 19-30. 10.4081/ripppo.2016.198 [DOI] [Google Scholar]
- Gatta, M., Spitaleri, C., Balottin, U., Spoto, A., Balottin, L., Mangano, S., & Battistella, P. A. (2015). Alexithymic characteristics in pediatric patients with primary headache: a comparison between migraine and tension-type headache. The Journal of Headache and Pain, 16, 98. 10.1186/s10194-015-0572-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giupponi, G., Giordano, G., Maniscalco, I., Erbuto, D.,Berardelli, I., Conca, A., Lester, D., Girardi, P., & Pompili, M. (2018). Suicide risk in attention-deficit/ hyperactivity disorder. Psychiatria Danubina, 30(1), 2–10. 10.24869/psyd.2018.2 [DOI] [PubMed] [Google Scholar]
- Gould, M. S., & Kramer, R. A. (2001). Youth suicide prevention. Suicide & Life-Threatening Behavior, 3, 6–31. 10.1521/suli.31.1.5.6.24219 [DOI] [PubMed] [Google Scholar]
- Grynberg, D., Luminet, O., Corneille, O., Grèzes, J., & Berthoz, S. (2010). Alexithymia in the interpersonal domain: A general deficit of empathy? Personality and individual diferences, 49(8),845-850. https://psycnet.apa.org/doi/10.1016/j.paid.2010.07.013 [Google Scholar]
- Guan, K., Fox, K. R., & Prinstein, M. J. (2012). Nonsuicidal self-injury as a time-invariant predictor of adolescent suicide ideation and attempts in a diverse community sample. Journal of consulting and clinical psychology, 80(5), 842. 10.1037/a0029429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gujral, S., Ogbagaber, S., Dombrovski, A. Y., Butters, M. A., Karp, J. F., & Szanto, K. (2016). Course of cognitive impairment following attempted suicide in older adults. International Journal of Geriatric Psychiatry, 31(6), 592–600. 10.1002/gps.4365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamza, C. A., Stewart, S. L., & Willoughby, T. (2012). Examining the link between nonsuicidal self-injury and suicidal behavior: A review of the literature and an integrated model. Clinical Psychology Review, 32(6), 482–495. 10.1016/j.cpr.2012.05.003 [DOI] [PubMed] [Google Scholar]
- Harpur, T. J., Hare, R. D., & Hakstian, A. R. (1989). Two-factor conceptualization of psychopathy: Construct validity and assessment implications. Psychological Assessment: A Journal of Consulting and Clinical Psychology, 1(1), 6–17. 10.1037/1040-3590.1.1.6 [DOI] [Google Scholar]
- Hatkevich, C., Penner, F., & Sharp, C. (2019). Dificulties in emotion regulation and suicide ideation and attempt in adolescent inpatients. Psychiatry Research, 271, 230-238. 10.1016/j.psychres.2018.11.038 [DOI] [PubMed] [Google Scholar]
- Hefer, T., & Willoughby, T. (2018). The role of emotion dysregulation: a longitudinal investigation of the interpersonal theory of suicide. Psychiatry Research, 260, 379–383. htt 10.1016/j.psychres.2017.11.075 [DOI] [PubMed] [Google Scholar]
- Hemming, L., Taylor, P., Haddock, G., Shaw, J., & Pratt, D. (2019). A systematic review and meta-analysis of the association between alexithymia and suicide ideation and behaviour. Journal of Afective Disorders, 254, 34–48. 10.1016/j.jad.2019.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herts, K. L., McLaughlin, K. A. & Hatzenbuehler, M. L. (2012). Emotion Dysregulation as a Mechanism Linking Stress Exposure to Adolescent Aggressive Behavior. Journal of Abnormal Child Psychology, 40, 1111–1122. 10.1007/s10802-012-9629-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iskric, A., Ceniti, A. K., Bergmans, Y., McInerney, S., & Rizvi, S. J. (2020). Alexithymia and self-harm: a review of nonsuicidal self-injury, suicidal ideation, and suicide attempts. Psychiatry Research, 288, 112920. 10.1016/j.psychres.2020.112920 [DOI] [PubMed] [Google Scholar]
- Ivanova, M. Y., Achenbach, T. M., Rescorla, L. A., Dumenci, L., Almqvist, F., Bilenberg, N., Bird, H., Broberg, A. G.,Dobrean, A., Döpfner, M., Erol, N., Forns, M., Hannesdottir, H., Kanbayashi, Y., Lambert, M. C., Leung, P., Minaei, A., Mulatu, M. S., Novik, T., Oh, K. J., Roussos, A., Sawyer, M., Simsek, Z., Steinhausen, H. C., Weintraub, S., Metzke, C. W., Wolanczyk, T., Zilber, N., Zukauskiene, R., & Verhulst, F. C. (2007). The generalizability of the Youth Self-Report syndrome structure in 23 societies. Journal of Consulting and Clinical Psychology, 75(5), 729–738. 10.1037/0022-006x.75.5.729 [DOI] [PubMed] [Google Scholar]
- The jamovi project. (2022). jamovi (Version 2.3) [Computer Software]. Retrieved from https://www.jamovi.orgJavdani,S., Sadeh, N., & Verona, E. (2011). Suicidality as a function of impulsivity, callous–unemotional traits, and depressive symptoms in youth. Journal of Abnormal Psychology, 120(2), 400–413. 10.1037/a0021805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiménez-Barbero, J. A., Ruiz-Hernández, J. A., Llor-Esteban, B., & Waschgler, K. (2016). Influence of attitudes, impulsivity, and parental styles in adolescents' externalizing behavior. Journal of Health Psychology, 21(1), 10.1177/1359105314523303 [DOI] [PubMed] [Google Scholar]
- Joiner, T.E. (2005). Why people die by suicide. Cambridge: Harvard University press. [Google Scholar]
- Joiner, T.E. (2007). Why people die by suicide. Cambridge: Harvard University press. [Google Scholar]
- Junewicz, A., & Billick, S. B. (2020). Conduct Disorder: Biology and Developmental Trajectories. Psychiatric Quarterly, 91(1), 77-90. 10.1007/s11126-019-09678-5 [DOI] [PubMed] [Google Scholar]
- Kämpfer, N., Staufenbiel, S., Wegener, I., Rambau, S., Urbach, A. S., Mücke, M., Geiser, F., & Conrad, R. (2016). Suicidality in patients with somatoform disorder – the speechless expression of anger? Psychiatry Research, 246, 485–491. 10.1016/j.psychres.2016.10.022 [DOI] [PubMed] [Google Scholar]
- Kauten, R., & Barry, C. T. (2016). Externalizing Behavior. In Zeigler-Hill V. & Shackelford T. K. (Eds.), Encyclopedia of Personality and Individual Diferences (pp. 1-4). Berlin:Springer. [Google Scholar]
- Kim, H., Seo, J., Namkoong, K., Hwang, E. H., Sohn, S. Y.,Kim, S. J., & Kang, J. I. (2016). Alexithymia and perfectionism traits are associated with suicidal risk in patients with obsessive-compulsive disorder. Journal of Afective Disorders, 192, 50-55. 10.1016/j.jad.2015.12.018 [DOI] [PubMed] [Google Scholar]
- Klonsky, E. D., & May, A. M. (2015a). The Three-Step Theory (3ST): A new theory of suicide rooted in the “Ideation-to-Action” framework. International Journal of Cognitive Therapy, 8(2), 114–129. 10.1521/ijct.2015.8.2.114 [DOI] [Google Scholar]
- Klonsky, E. D., & May, A. M. (2015b). Impulsivity and suicide risk: review and clinical implications. Psychiatric Times, 32(8), 13-13. [Google Scholar]
- Klonsky, E. D., May, A. M., & Safer, B. Y. (2016). Suicide, suicide attempts, and suicidal ideation. Annual Review of Clinical Psychology, 12, 307–330. 10.1146/annurev-clinpsy-021815-093204 [DOI] [PubMed] [Google Scholar]
- Krysinska, K., Heller, T. S., & De Leo, D. (2006). Suicide and deliberate self-harm in personality disorders. Current Opinion in Psychiatry, 19(1), 95-101. 10.1097/01yco.0000191498.69281.5e [DOI] [PubMed] [Google Scholar]
- Langhinrichsen-Rohling, J., Friend, J., & Powell, A. (2009). Adolescent suicide, gender, and culture: a rate and risk factor analysis. Aggression and Violent Behavior, 14(5), 402–414. 10.1016/j.avb.2009.06.010 [DOI] [Google Scholar]
- Lanzara, R., Conti, C., Camelio, M., Cannizzaro, P., Lalli, V., Bellomo, R. G., Saggini, R., & Porcelli, P. (2020). Alexithymia and somatization in chronic pain patients: a sequential mediation model. Frontiers in Psychology, 11, 545881. 10.3389/fpsyg.2020.545881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann, J. J. (2003). Neurobiology of suicidal behaviour. Nature Reviews Neuroscience, 4(10), 819–828. 10.1038/nrn1220 [DOI] [PubMed] [Google Scholar]
- Manninen, M., Therman, S., Suvisaari, J., Ebeling, H., Moilanen, I., Huttunen, M., & Joukamaa, M. (2011). Alexithy mia is common among adolescents with severe disruptive behavior. Journal of Nervous and Mental Disease, 199(7), 506-509. 10.1097/nmd.0b 013e3182214281 [DOI] [PubMed] [Google Scholar]
- May, A. M., & Klonsky, E. D. (2013). Assessing motivations for suicide attempts: development and psychometric properties of the inventory of motivations for suicide attempts. Suicide and Life-Threatening Behavior, 43(5), 532-546. 10.1111/sltb.12037 [DOI] [PubMed] [Google Scholar]
- May, A. M., & Klonsky, E. D. (2016). What distinguishes suicide attempters from suicide ideators? A meta‐ analysis of potential factors. Clinical Psychology: Science and Practice, 23(1), 5-20. 10.1111/cpsp.12136 [DOI] [Google Scholar]
- McCloskey, M. S., & Ammerman, B. A. (2018). Suicidal behavior and aggression-related disorders. Current Opinion in Psychology, 22, 54–58. 10.1016/j.copsyc.2017.08.010 [DOI] [PubMed] [Google Scholar]
- McHugh, C. M., Chun Lee, R. S., Hermens, D. F., Corderoy, A., Large, M., & Hickie, I. B. (2019). Impulsivity in the self-harm and suicidal behavior of young people: a systematic review and meta-analysis. Journal of Psychiatric Research, 116, 51–60. 10.1016/j.jpsychires.2019.05.012 [DOI] [PubMed] [Google Scholar]
- Millner, A. J., Lee, M. D., Hoyt, K., Buckholtz, J. W., Auerbach, R. P., & Nock, M. K. (2018). Are suicide attempters more impulsive than suicide ideators? General Hospital Psychiatry, 63, 103–110. 10.1016/j.genhosppsych.2018.08.002 [DOI] [PubMed] [Google Scholar]
- Moeller, F. G., Barratt, E. S., Dougherty, D. M., Schmitz, J. M., & Swann, A. C. (2001). Psychiatric aspects of impulsivity. The American Journal of Psychiatry, 58(11), 1783-1793. 10.1176/appi.ajp.158.11.1783 [DOI] [PubMed] [Google Scholar]
- Moselli, M., Casini, M. P., Frattini, C., & Williams, R. (2021). Suicidality and Personality Pathology in Adolescence: A Systematic Review. Child Psychiatry & Human Development. 10.1007/s10578-021-01239-x [DOI] [PMC free article] [PubMed]
- Namuli, J. D., Nalugya, J. S., Bangirana, P., & Nakimuli-Mpungu, E. (2021). Prevalence and Factors Associated With Suicidal Ideation Among Children and Adolescents Attending a Pediatric HIV Clinic in Uganda. Frontiers in Sociology, 6, 656739. 10.3389/fsoc.2021.656739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock, M. K., Borges, G., Bromet, E. J., Cha, C. B., Kessler, R. C., & Lee, S. (2008). Suicide and suicidal behavior. Epidemiologic Reviews, 30(1), 133–154. 10.1093/epirev/mxn002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock, M. K., Green, J. G., Hwang, I., McLaughlin, K. A., Sampson, N. A., Zaslavsky, A. M., & Kessler, R. C. (2013). Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the national comorbidity survey replication adolescent supplement. JAMA Psychiatry, 70(3), 300-310. 10.1001/2013.jamapsychiatry.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock, M. K., Hwang, I., Sampson, N., Kessler, R. C., Angermeyer, M., Beautrais, A., Borges, G., Bromet, E., Brufaerts, R., De Girolamo, G., De Graaf, R., Florescu, S., Gureje, O., Haro, J. M., Hu, C., Huang, Y., Karam, E. G., Kawakami, N., Kovess, V., Levinson, D., Posada-Villa, J., Sagar, R., Tomov, T., Viana, M. C., & Williams, D. R. (2009). Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO world mental health surveys. PLOS Medicine, 6(8), e1000123. 10.1371/journal.pmed.1000123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace, C. S., & Muzi, S. (2019). Binge-eating symptoms, emotional-behavioral problems and gender diferences among adolescents: a brief report. Mediterranean Journal of Clinical Psychology, 7(2), 1-9. 10.6092/2282-1619/2019.7.2161 [DOI] [Google Scholar]
- Parolin, M., Miscioscia, M., De Carli, P., Cristofalo, P., Gatta, M., & Simonelli, A. (2018). Alexithymia in young adults with substance use disorders: critical issues about specificity and treatment predictivity. Frontiers in Psychology, 9, 645. 10.3389/fpsyg.2018.00645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton, J. H., Stanford, M. S., & Barratt, E. S. (1995). Factor structure of the Barratt impulsiveness scale. Journal of Clinical Psychology, 51(6), 768–774. [DOI] [PubMed] [Google Scholar]
- Pelkonen, M., & Marttunen, M. (2003). Child and adolescent suicide: epidemiology, risk factors, and approaches to prevention. Pediatric Drugs, 5(4), 243–265. 10.2165/00128072-200305040-00004 [DOI] [PubMed] [Google Scholar]
- Pompili, M., Ruberto, A., Girardi, P., & Tatarelli, R. (2004). Suicidality in DSM IV cluster B personality disorders. An overview. Annali dell'Istituto Superiore di Sanità, 40(4), 475-483. [PubMed] [Google Scholar]
- Pompili, M., Sher, L., Serafini, G., Forte, A., Innamorati, M., Dominici, G., Lester, D., Amore, M., & Girardi, P. (2013). Posttraumatic stress disorder and suicide risk among veterans: a literature review. Journal of Nervous and Mental Disease, 201(9), 802–812. 10.1097/nmd.0b013e3182a21458 [DOI] [PubMed] [Google Scholar]
- Qin, P., Agerbo, E., & Mortensen, P. B. (2002). Suicide risk in relation to family history of completed suicide and psychiatric disorders: a nested case-control study based on longitudinal registers. The Lancet, 360(9340), 1126-1130. 10.1016/s0140-6736(02)11197-4 [DOI] [PubMed] [Google Scholar]
- Rafagnato, A., Angelico, C., Valentini, P., Miscioscia, M., & Gatta, M. (2020). Using the body when there are no words for feelings: alexithymia and somatization in self-harming adolescents. Frontiers in Psychology, 11, 262. 10.3389/fpsyt.2020.00262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rafagnato, A., Iannattone, S., Fasolato, R., Parolin, E., Ravaglia, B., Biscalchin, G., Traverso, A., Zanato, S., Miscioscia, M., & Gatta, M. (2022). A Pre-Adolescent and Adolescent Clinical Sample Study about Suicidal Ideation, Suicide Attempt, and Self-Harming. European Journal of Investigation in Health, Psychology and Education, 12(10), 1441-1462. 10.3390/ejihpe12100100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajappa, K., Gallagher, M., & Miranda, R. (2012). Emotion Dysregulation and Vulnerability to Suicidal Ideation and Attempts. Cognitive Therapy and Research, 36, 833–839. 10.1007/s10608-011-9419-2 [DOI] [Google Scholar]
- Ribeiro, J. D., Huang, X., Fox, K. R., & Franklin, J. C. (2018). Depression and hopelessness as risk factors for suicide ideation, attempts and death: meta-analysis of longitudinal studies. British Journal of Psychiatry, 212, (5), 279-286. 10.1192/bjp.2018.27 [DOI] [PubMed] [Google Scholar]
- Riefe, C., Oosterveld, P., & Terwogt, M. M. (2006). An alexithymia questionnaire for children: factorial and concurrent validation results. Personality and Individual Diferences, 40(1), 123–133. 10.1016/j.paid.2005.05.013 [DOI] [Google Scholar]
- Ruch, D. A., Sheftall, A. H., Schlagbaum, P., Rausch, J., Campo, J. V., & Bridge, J. A. (2019). Trends in suicide among youth aged 10 to 19 years in the United States, 1975 to 2016. JAMA Network Open, 2(5), e193886. https://doi.org/10.1001%2Fjamanetworkopen.2019.3886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sifneos, P. E. (1973). The Prevalence of ‘Alexithymic’ Characteristics in Psychosomatic Patients. Psychotherapy and Psychosomatics, 22(2), 255-262. 10.1159/000286529 [DOI] [PubMed] [Google Scholar]
- Shettar, M., Kakunje, A., Karkal, R., Mendonsa, R. D., Kini, G., & Mohan Chandran, V. V. (2018). Suicidality in somatization and undiferentiated somatoform disorders: a hospital-based study. Archives of Medicine and Health Sciences, 6, 36-39. [Google Scholar]
- Sørensen, H. J., Mortensen, E. L., Wang, A. G., Juel, K., Silverton, L., & Mednick, S. A. (2009). Suicide and mental illness in parents and risk of suicide in ofspring. Social psychiatry and psychiatric epidemiology, 44(9), 748-751. 10.1007/s00127-009-0495-5 [DOI] [PubMed] [Google Scholar]
- Speyer, L. G., Brown, R. H., Camus, L., Murray, A. L., & Auyeung, B. (2022). Alexithymia and Autistic Traits as Contributing Factors to Empathy Dificulties in Preadolescent Children. Journal of Autism and Developmental Disorders, 52, 823–834. 10.1007/s10803-021-04986-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanford, M. S., Mathias, C. W., Dougherty, D. M., Lake, S. L., Anderson, N. E., & Patton, J. H. (2009). Fifty years of the Barratt Impulsiveness Scale: an update and review. Personality and Individual Diferences, 47(5), 385–395. 10.1016/j.paid.2009.04.008 [DOI] [Google Scholar]
- Strandheim, A., Bjerkeset, O., Gunnell, D., Sigrid Bjørnelv, S., Holmen, T. L., & Bentzen, N. (2014). Risk factors for suicidal thoughts in adolescence-a prospective cohort study: the Young-HUNT study. BMJ Open, 4, e005867. 10.1136/bmjopen-2014-005867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subic-Wrana, C., Beutel, M. E., Brähler, E., Stöbel-Richter, Y., Knebel, A., Lane, R. D., Wiltink, J. (2014). How is emotional awareness related to emotion regulation strategies and self- reported negative afect in the general population? PloS one, 9, e91846. 10.1371/journal.pone.0091846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szanto, K., De Bruin, W. B., Parker, A. M., Hallquist, M. N., Vanyukov, P. M., & Dombrovski, A. Y. (2015). Decision-making competence and attempted suicide. The Journal of Clinical Psychiatry, 76(12), e1590-e1597. 10.4088/jcp.15M09778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang, J., Yu, Y., Wu, Y., Du, Y., Ma, Y., Zhu, H., Zhang, P.,& Liu, Z. (2011). Association between Non-Suicidal Self-Injuries and Suicide Attempts in Chinese Adolescents and College Students: A Cross-Section Study. PLoS ONE, 6(4), e17977. 10.1371/journal.pone.0017977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson, R. (2019). Emotion dysregulation: A theme in search of definition. Development and Psychopathology, 31(3), 805-815. 10.1017/s0954579419000282 [DOI] [PubMed] [Google Scholar]
- Trivedi-Bateman, N., & Crook, E. L. (2022). The optimal application of empathy interventions to reduce antisocial behaviour and crime: a review of the literature. Psychology, Crime & Law, 28(8), 796-819. 10.1080/1068316X.2021.1962870 [DOI] [Google Scholar]
- Vander Stoep, A., Adrian, M., McCauley, E., Crowell, S. E., Stone, A., & Flynn, C. (2011). Risk for suicidal ideation and suicide attempts associated with co‐occurring depression and conduct problems in early adolescence. Suicide and Life‐Threatening Behavior, 41(3), 316-329. 10.1111/j.1943-278X.2011.00031.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasconcelos, A. G., Malloy-Diniz, L., & Correa, H. (2012). Systematic review of psychometric proprieties of Barratt Impulsiveness Scale Version 11 (BIS-11). Clinical neuropsychiatry: Journal of Treatment Evaluation, 9(2), 61–74. [Google Scholar]
- Velotti, P., Garofalo, C., Petrocchi, C., Cavallo, F., Popolo, R., & Dimaggio, G. (2016). Alexithymia, emotion dysregulation, impulsivity and aggression: A multiple mediation model. Psychiatry Research, 237, 296-303. 10.1016/j.psychres.2016.01.025 [DOI] [PubMed] [Google Scholar]
- Venta, A., Hart, J., & Sharp, C. (2013). The relation between experiential avoidance, alexithymia and emotion regulation in inpatient adolescents. Clinical Child Psychology and Psychiatry, 18(3), 398-410. 10.1177/1359104512455815 [DOI] [PubMed] [Google Scholar]
- Verona, E., Patrick, C. J., & Joiner, T. E. (2001). Psychopathy, antisocial personality, and suicide risk. Journal of Abnormal Psychology, 110(3), 462–470. 10.1037/0021-843X.110.3.462 [DOI] [PubMed] [Google Scholar]
- Verona, E., Sachs-Ericsson, N., & Joiner, T. E. (2004). Suicide attempts associated with externalizing psychopathology in an epidemiological sample. The American Journal of Psychiatry, 161(3), 444–451. 10.1176/appi.ajp.161.3.444 [DOI] [PubMed] [Google Scholar]
- Villalobos-Gallegos, L., Pérez-Matus, S., Valdez-Santiago, R., & Marín-Navarrete, R. (2020). Individual Contribution of Youth Antisocial Symptoms to Suicide Behavior in Adults with Substance Use Disorders. Archives of Suicide Research, 24, 126-135. 10.1080/13811118.2019.1577193 [DOI] [PubMed] [Google Scholar]
- Witte, T. K., Gauthier, J. M., Huang, X., Ribeiro, J. D., & Franklin, J. C. (2018). Is externalizing psychopathology a robust risk factor for suicidal thoughts and behaviors? A meta-analysis of longitudinal studies. Journal of Clinical Psychology, 74(9), 1607–1625. 10.1002/jclp.22625 [DOI] [PubMed] [Google Scholar]
- Wolf, J. C., Davis, S., Liu, R. T., Cha, C. B., Cheek, S. M., Nestor, B. A., Frazier, E. A., Schafer, M. M., & Spirito, A. (2018). Trajectories of Suicidal Ideation among Adolescents Following Psychiatric Hospitalization. Journal of Abnormal Child Psychology, 46(2), 355-363. 10.1007/s10802-017-0293-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO). (2021). Comprehensive Mental Health Action Plan 2013-2030. WHO, Geneva, Switzerland. https://www.who.int/publications/i/item/9789240031029 [Google Scholar]
- Zanato, S., Miscioscia, M., Traverso, A., Gatto, M., Poli, M., Rafagnato, A., & Gatta, M. (2021). A Retrospective study on the factors associated with long-stay hospitalization in a Child Neuropsychiatry Unit. Healthcare, 9(9), 1241. 10.3390/healthcare9091241 [DOI] [PMC free article] [PubMed] [Google Scholar]


