Abstract
Introduction:
Sequential multiple assignment randomized trials (SMART) inform the design of adaptive treatment interventions. We tested the feasibility of a SMART to deliver a stepped-care intervention among primary care patients who smoked daily.
Methods:
In a 12-week pilot SMART (NCT04020718). we tested the feasibility of recruiting and retaining (>80%) participants to an adaptive intervention starting with cessation text messages (SMS). The study randomly assigned participants (R1) to assessment of quit status, the tailoring variable, after either 4 or 8 weeks of SMS. The study offered continued SMS alone to those reporting abstinence. Those reporting smoking were randomized (R2) to SMS+mailed NRT or SMS+NRT+brief telephone coaching.
Results:
During Jan–March and July–Aug 2020, we enrolled 35 patients (>18 years) from a primary care network in Massachusetts. Two (6%) of 31 participants reported seven-day point prevalence abstinence at their tailoring variable assessment. The 29 participants who continued to smoke at 4 or 8 weeks were randomized (R2) to SMS+NRT (n=16) or SMS+NRT+coaching (n=13). Thirty of 35 participants (86%) completed 12-weeks; 13% (2/15) of those in 4-week group and 27% (4/15) of those in 8-week group had CO<6ppm at 12-weeks (p=0.65). Among 29 participants in R2, one was lost to follow-up, 19% (3/16) of the SMS+NRT group had CO<6ppm vs. 17% (2/12) of SMS+NRT+coaching (p=1.00). Treatment satisfaction was high (93%, 28 of 30 who completed 12-weeks).
Conclusions:
A SMART exploring a stepped-care adaptive intervention combining SMS, NRT, and coaching for primary care patients was feasible. Retention and satisfaction were high and quit rates were promising.
Keywords: Adaptive treatment, Smoking cessation, Mobile health, Primary care, Nicotine replacement therapy
1. Introduction
We have effective treatments to help the 37.8 million Americans who smoke cigarettes, including medications and behavioral treatment, that can double the chances of quitting (Fiore et al., 2008; Jamal et al., 2018). While most (70%) smokers visit a physician each year (Fiore et al., 2008), delivery of cessation treatment during clinic visits is sub-optimal (Babb, Malarcher, Schauer, Asman, & Jamal, 2017). We need new models to increase the reach of cessation treatment services with minimal burden to busy primary care providers (PCPs).
One promising model is an adaptive treatment model. For many chronic conditions, clinical management is sequential, adding or changing medications or behavioral treatments based on patients’ response or changing needs over time. Treatment strategies that are responsive to patients’ needs are more likely to be effective than static treatment programs (Murphy, Collins, & Rush, 2007). This approach is starting to be tested in tobacco cessation (Edelman et al., 2021; Fernandez et al., 2020; Fu et al., 2017). Few published trials have used an approach that examines an adaptive treatment model (Ebbert et al., 2017; Fu et al., 2017; Hebert et al., 2020). Text messages (SMS) are a promising option as an initial, low-cost, evidence-based cessation treatment in an adaptive treatment program (Head, Noar, Iannarino, & Harrington, 2013; Scott-Sheldon et al., 2016; Spohr et al., 2015; Substance, Mental, & General, 2020; Whittaker, McRobbie, Bullen, Rodgers, & Gu, 2016). SMS have potential as a convenient initial treatment to engage primary care patients in taking action to quit. Yet we need to understand how SMS can be effectively combined with other evidence-based treatments.
Adaptive treatment programs could conserve costlier resources, such as coaches or counselors, for only those patients who need or are ready for them. Designing these programs requires answers to questions about how and when to assess an individual’s response to tobacco cessation treatment and what to do next for those who need more help. For example, little data exist to inform whether patients should be followed-up quickly to enable rapid treatment changes for insufficient response, or if individuals are more successful if given more time to carry out a quit attempt before being offered a change.
The objective of this study is to understand the feasibility of answering these questions about adaptive treatment models for smoking cessation using a pilot sequential multiple assignment randomized trial (SMART). The SMART is a tool for testing treatment programs that adapt based on user response (Daniel Almirall, Inbal Nahum-Shani, Nancy E Sherwood, & Susan A Murphy, 2014). This article reports on the feasibility of a SMART designed to test the timing of offering nicotine replacement therapy (NRT) and/or coaching to primary care patients who agree to participate in a stepped-care intervention starting with a cessation SMS program. The SMART compared the offer of NRT or NRT + coaching after 4 versus 8 weeks of an SMS program.
2. Methods
2.1. Study design
We conducted a 12-week, open-label pilot SMART with embedded qualitative exit interviews. Feasibility of the trial methods and acceptability of treatment were measured through recruitment rates, retention (>80%), treatment engagement, and user satisfaction (>90%). The SMART was designed to test the feasibility of comparing different timings for offering NRT to patients who started an SMS program and the benefit of the additional offer of a live interaction via brief telephone coaching (Figure 1). We randomized participants to two different timings (R1) and two different NRT treatment packages (R2). We designed the treatment interventions based on the four elements of an adaptive intervention: decision stages, treatment options, tailoring variables, and a decision rule (D. Almirall, I. Nahum-Shani, N. E. Sherwood, & S. A. Murphy, 2014). We designed an intervention with one decision stage, the 4- or 8-week timepoint at which participants who continue to smoke are offered additional treatment. The treatment options are continued SMS, continued SMS + NRT, or continued SMS + NRT and telephone coaching. Almirall et al. describe baseline tailoring variables and intermediate tailoring variables (D. Almirall et al., 2014). We used an intermediate tailoring variable, measured during the study, defined as whether participants reported 7-day abstinence at their decision stage. The decision rule that links the tailoring variable to the treatment options is offering additional treatment with NRT or offering additional treatment with NRT and coaching for those who report continued smoking at their decision stage. The choice of starting with a low-intensity, evidence-based treatment is based on stepped-care models. These models have been used for treatment of alcohol use disorder, which faces similar patterns of underutilization of evidence-based treatments as tobacco (Cohen, Feinn, Arias, & Kranzler, 2007). Stepped-care models prioritize engagement first, with low-cost, highly scalable, and low burden treatments such as digital health interventions, before escalating to more intensive treatment (McKellar, Austin, & Moos, 2012).
Figure 1.
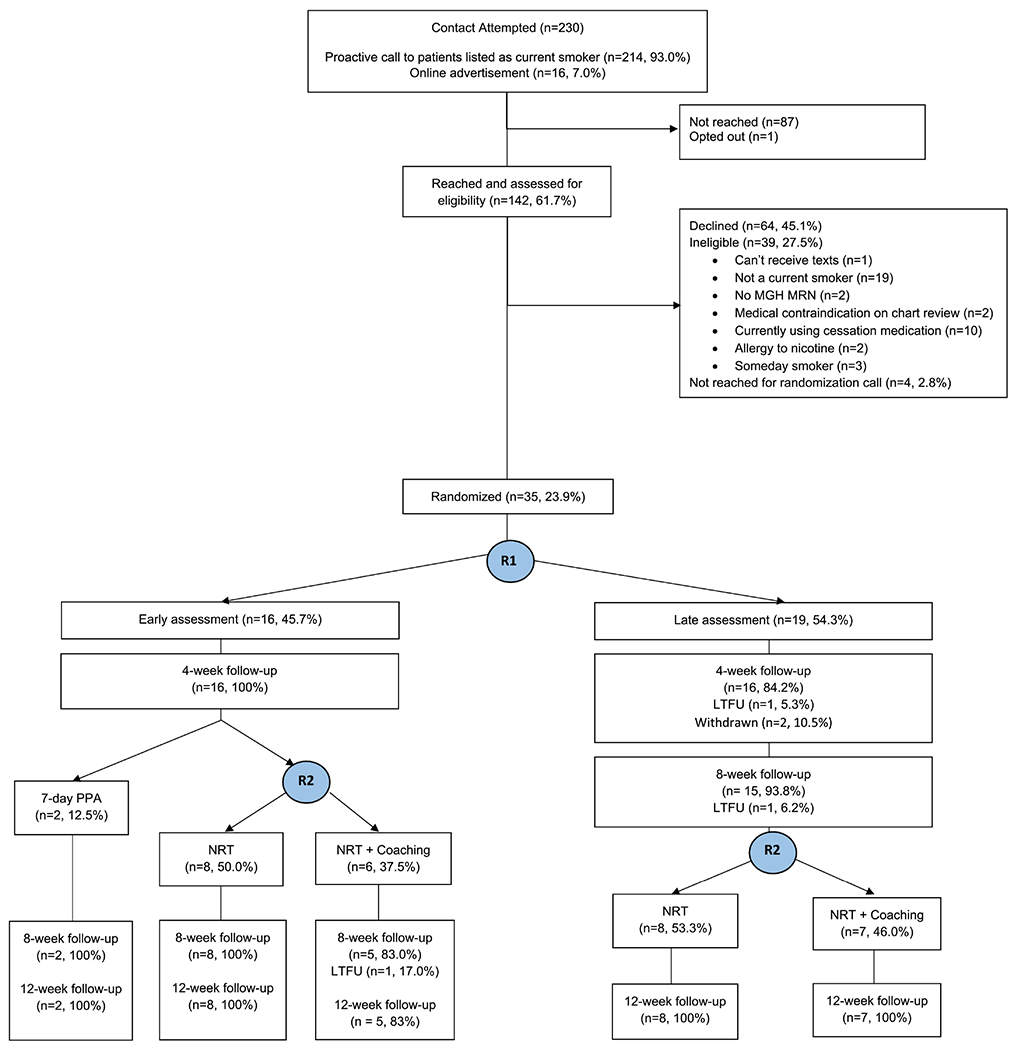
Study Flow
Figure abbreviations: MGH MRN=Massachusetts General Hospital Medical Record Number; R1=first randomization; R2=second randomization; LTFU=lost to follow-up; 7-day PPA=7-day point prevalence abstinence; NRT=nicotine replacement therapy.
Pilot trial participants had access to the SMS program throughout the 12-week study. The pilot used embedded semi-structured telephone interviews to examine participants’ experiences with study methods and treatments. The Mass General Brigham Institutional Review Board approved the study (2017P000960).
2.2. Recruitment
The study recruited participants through an institutional study recruitment website and proactive outreach to patients listed as current smokers in the Electronic Health Record (EHR) who had previously consented to be contacted directly for research studies. Our pilot study sample size was based on evaluating the feasibility and acceptability of the trial design and was not powered to measure treatment effects (Daniel Almirall, Compton, Gunlicks-Stoessel, Duan, & Murphy, 2012). Eligible participants met the following inclusion criteria: (1) ≥18 years, (2) current daily smoker in the EHR, confirmed by self-report, (3) preferred language of English in EHR, (4) primary care provider (PCP) within the primary care network, (5) visit in the last two years, (6) mobile number listed in EHR, (7) not currently pregnant, planning to become pregnant in the next three months or breastfeeding, (8) no past 30-day smoking cessation treatment use, (9) no contraindications to NRT, (10) no diagnosis of dementia, active psychosis or schizoaffective disorder based on chart review or self-report, and (11) willing to receive text messages.
2.3. Randomizations
Study staff told participants about the random assignment procedures during informed consent. Following verbal informed consent and baseline assessment, the study randomly assigned participants (R1) using a computer-generated sequence to early (4-week) assessment or late (8-week) assessment of response. At the 4- or 8-week assessment time, the study asked users about tobacco use (the tailoring variable). Those who reported abstinence from cigarettes for the past seven days were offered to continue with the SMS program. Those who were still smoking at the 4- or 8-week assessment were randomized a second time (R2). At R2, the study randomized participants to continued SMS + NRT or continued SMS + NRT + one live telephone coaching session. Participants were informed about the random assignment procedures during informed consent. The sequence was not visible to the research coordinator prior to assignment.
2.4. Interventions
2.4.1. SMS program
The initial treatment at R1 consisted of an SMS program. Study staff entered participants’ phone numbers into a messaging platform following enrolment and study consent (Mobile Commons, Upland Software). SMS content is described in prior work (G. Kruse et al., 2019). Briefly, the messages are targeted to primary care patients with information about treatment resources in their primary care network. All participants started with a welcome message that included predetermined keywords that participants could use to opt-in to one of two message campaigns the “Ready” campaign or the “Practice” campaign. Participants who opted into the “Ready” campaign were prompted to enter a quit date within the next 30 days. “Ready” messages were developed with content adapted from the National Cancer Institute’s SmokefreeTXT program (smokefree.gov). Messages also included content encouraging NRT use based on the Information-Motivation-Behavioural Skills model (IMB) of medication adherence (Fisher, Fisher, & Harman, 2003). In the IMB model, information relevant to medication adherence may facilitate or hinder adherence and may include, for example, how to take medications or adverse effects. Motivation to adhere to medications encompasses both personal and social motivations and may include beliefs about the effects of adherence and perceived social support. Behavioral skills include self-efficacy and the abilities needed to acquire and use medication, deal with adverse effects, and communicate with health care providers. Users without a quit date who opted for the “Practice” campaign were encouraged to practice quitting (Carpenter et al., 2011). Practice quitting is explained as an attempt to not smoke for hours or days without committing to permanently quit. Both campaigns sent weekly messages to assess smoking status. If smokers with a quit date had not quit, they could either transfer to the “Practice” campaign or reset their quit date. Smokers in the “Practice” campaign could either practice again or transfer to the “Ready” campaign. Participants could repeat either campaign as many times as they choose. Both campaigns included two-way interaction using keywords “CRAVE” “SLIP” and “MOOD”, a trivia game for distraction, and weekly smoking status assessments.
The study also adapted the messages for the pandemic. After implementation of a stay-at-home advisory in Massachusetts, we edited message content to remove messages that encouraged activities inconsistent with social distancing recommendations. In their place we included messages with self-care tips, messages of encouragement acknowledging the increased stress many participants could be facing, and messages to address boredom and stress during the pandemic.
Participants received between 0 and 5 SMS per day from a library of 144 total messages. The “Practice” campaign included 33 days of unique content. The “Ready” campaign had 72 days’ of unique content. Individual’s time in the program varied depending on number of times they repeated campaigns or transferred between “Ready” and “Practice”. All participants could opt-out of the SMS at any time during the 12-week study by texting the keyword “STOP”.
2.4.2. Adaptative treatment options
The study randomized all participants reporting continued smoking at the 4- or 8-week assessment a second time (R2) to an offer of SMS+NRT or SMS+NRT+coaching. NRT consisted of a 4-week supply of combination NRT. Participants could choose from patches and/or mint-flavored mini lozenges. Smokers who smoked ≥10 cigarettes per day at baseline were offered 21 mg patches and those who smoked <10 cigarettes per day were offered 14 mg patches. Participants who smoked within 30 minutes of awakening were offered the 4 mg lozenges and those who smoked >30 minutes of awakening were offered 2 mg lozenges. NRT was delivered by mail to participants’ homes. Participants randomized to NRT + coaching were also offered one telephone coaching session. The single coaching session was intended to enhance the behavioral support provided through the SMS with a live-person interaction. The scripted coaching session was provided by a research coordinator who completed Tobacco Treatment Specialist Core Certificate training (Tobacco Treatment Specialist (TTS) Core Training, University of Massachusetts Medical school). We designed the coaching sessions to last up to 15 minutes and provided information on local resources and smoking cessation medications. Both R2 groups (NRT or NRT + coaching) continued the SMS program with the addition of daily interactive SMS messages querying their NRT use.
3. Data collection/assessments
The study collected measures by telephone or email survey, depending on participant preferences, at baseline, 4-, 8- and 12-weeks post-enrollment. Surveys were conducted by the study’s research coordinator who was not blinded to treatment assignment.
The baseline survey was completed by telephone at enrollment. The study collected baseline data to understand the pilot study sample recruited for this fully remote stepped-care intervention and included predictors of cessation including sociodemographic measures, smoking characteristics, prior quit attempts, cessation treatment use, emotional symptoms, past month substance use and self-reported SMS use.
Follow-up surveys measured smoking status, treatment use, and satisfaction. Outcomes were pre-specified (NCT04020718). Participants reporting seven-day point prevalence abstinence (7-day PPA) at 12-weeks were asked to provide a carbon monoxide (CO) measurement using the iCO Smokerlyzer (Bedfont) device. They received a device in the mail, instruction to download the Smokerlyzer application, and to email their reading to the research coordinator.
All participants were invited to participate in a semi-structured telephone interview following the 12-week outcome survey. The study compensated participants for their time using gift cards as follows: $20 for completing the baseline, 4- and 8-week surveys, $40 for the 12-week outcome survey, $20 for the qualitative interview, and $80 for emailing the CO measure among those who reported 7-day PPA at 12-weeks
3.1. Feasibility outcomes
Feasibility of the SMART design was assessed by the proportion of potentially eligible patients reached, proportion enrolled and randomized, and retention in the 12-week study.
3.2. Intervention fidelity
To assess the fidelity of the SMS intervention we measured: 1) participants’ use of the HELP function as an indicator of technical challenges with the program, and 2) number of intended messages that failed to send.
3.3. Intervention engagement
Engagement with the SMS intervention was captured by the messaging platform. Measures of engagement included: number of messages sent to participant, active time defined as number of days from first incoming SMS from participant to last SMS from participant, number of incoming messages sent from the participant, number of embedded URL links clicked, and number of NRT query messages responded to. We measured engagement with NRT by any patch use or lozenge use reported in follow-up surveys and NRT use reported by SMS query. The study measured engagement with telephone coaching by participation in and duration of the coaching session per coach records.
3.4. Treatment acceptability
At 12-weeks, we measured treatment acceptability by four-point Likert scale rating satisfaction with study treatments. Participants also rated their agreement, on a five-point Likert scale ranging from “Completely agree” to “Completely disagree”, with statements that the study gave participants confidence to quit, made them feel quitting is worthwhile, made them feel as if someone cared if they quit, and that they knew the right steps to take to quit (Hoeppner, Hoeppner, & Abroms, 2017).
3.5. Tobacco cessation outcomes
Although not powered to assess differences by study arm, we defined a primary clinical outcome of self-reported 7-day PPA at 12-weeks. We defined 7-day PPA as not smoking even a puff in the past 7 days. Other clinical outcomes included 7-day PPA at 4- and 8-weeks, number of last 30 days with no smoking, use of cessation treatments and changes between baseline and 12-weeks in cigarettes per day, motivation, confidence to quit and distress. We measured biochemically verified abstinence by expired CO <6 parts per million (ppm) among participants who reported 7-day PPA at 12-weeks.(Benowitz et al., 2020; Verification, 2002)
3.6. Semi-structured interviews
The study conducted interviews after the 12-week outcome survey. The brief interviews were recorded and transcribed. The research team developed the interview guide with attention to the participants’ experience with study treatments including the SMS, NRT and coaching. During the pandemic, we revised these to explore smoking and quitting behaviors (Joyce et al., 2021).
4. Analysis
4.1. Power calculation
Our pilot sample size was based on the probability of having patients in all six treatment subgroups to assess the feasibility of a larger-scale SMART. With 30 patients randomized one-to-one in R1 (Figure 1), we expected three patients in the smallest subgroup.(G. R. Kruse et al., 2020). However, using a method by Almirall et al., the probability of reaching this minimum subgroup size by randomization was only 59%, therefore we aimed to enroll 35 patients to reach a 70% probability of having at least three patients per subgroup (D. Almirall, Compton, Gunlicks-Stoessel, Duan, & Murphy, 2012; Daniel Almirall et al., 2012).
4.2. Statistical analysis
Adherence and engagement with SMS and acceptability were calculated and reported with 95% confidence intervals. Smoking cessation outcomes were compared by early versus late assessment of response (R1) and NRT versus NRT + coaching (R2) using Fisher’s exact tests and t-tests. We tested for interaction between the two treatment factors (early/late and NRT/NRT + coaching) on categorical and continuous smoking outcomes using Cochran-Mantel-Haenszel test and ANOVA, respectively. We performed all analyses using SAS software V.9.4 (SAS Institute, Cary, North Carolina, USA).
4.3. Qualitative analysis
The study analyzed qualitative interviews using NVivo 12 software (QSR International Pty Ltd. NVivo (Version 12), 2018) (QSR Australia) using a framework approach (Ritchie J., 2013). An initial coding scheme was developed using a priori constructs from the semi-structured guide plus emergent themes from the transcribed data. Investigators applied this coding scheme to a subset of interviews in an iterative process to develop a final coding scheme. The team used the constant comparative method to promote validity (Glaser & Strauss, 2017). Coding was at the sentence level with multiple codes permitted for each sentence. All transcripts were double coded and compared, reaching a high degree of intercoder reliability (kappa ≥ 0.8). Themes were developed through analysis of codes to identify emergent patterns using matrix coding by treatment group.
5. Results
5.1. Feasibility
During two phases of recruitment (Jan-March & July-Aug 2020) we enrolled and randomized 35 participants (Supplemental Figure A). In terms of reach, 35 (34%, 95%CI [24.9, 44.0]) of 103 eligible patients agreed to participate and were randomized. This included 25 participants recruited in the first phase and 10 in the second. Recruitment was paused from March-July 2020 to modify our SMS intervention with social distancing recommendations and to update study procedures for research staff to work remotely.
Study retention at 12 weeks was 86% (30 completed, two withdrew, three lost to follow-up [LTFU]; 95%CI [69.7, 95.2]) (Figure 1). Excluding n=2 withdrew and n=2 LTFU before the R1 assessment, 6% (2/31) self-reported 7-day PPA by the time of the R1 assessment when receiving SMS alone. In R2, the 29 participants who reported continued smoking were randomized again [16 to NRT and 13 to NRT + coaching]. Table 1 shows sample characteristics for n=33 participants (excluding n=2 withdrawn).
Table 1.
Baseline characteristics by randomization, N=33*
| R1 Early 4-week assessment | R1 Late 8-week assessment | |||||
|---|---|---|---|---|---|---|
| R2 | R2 | |||||
| Quit† | NRT | NRT+ coaching | Lost to follow-up† | NRT | NRT+ coaching | |
| N (%) | N=2 | N=8 | N=6 | N=2 | N=8 | N=7 |
| Demographics | ||||||
| Gender | ||||||
| Female | 1 (50.0) | 4 (50.0) | 2 (33.3) | 1 (50.0) | 6 (75.0) | 2 (28.6) |
| Age-Mean [SD] | 56.0 [4.2] | 56.8 [14.6] | 54.5 [12.8] | 59.4 [3.5] | 43.9 [13.9] | 55.9 [15.4] |
| Race | ||||||
| Hispanic | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (12.5) | 0 (0.0) |
| African American, non-Hispan | 1 (50.0) | 2 (25.0) | 0 (0.0) | 0 (0.0) | 1 (12.5) | 0 (0.0) |
| White, non-Hispanic | 1 (50.0) | 6 (75.0) | 6 (100.0) | 2 (100.0) | 4 (50.0) | 7 (100.0) |
| Other, non-Hispanic | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (12.5) | 0 (0.0) |
| Mixed race, non-Hispanic | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (12.5) | 0 (0.0) |
| Education | ||||||
| Completed high school | 0 (0.0) | 1 (12.5) | 1 (16.7) | 0 (0.0) | 2 (25.0) | 2 (28.6) |
| Some college | 2 (100.0) | 5 (62.5() | 3 (50.0) | 0 (0.0) | 2 (25.0) | 2 (28.6) |
| 4-year degree or more | 0 (0.0) | 2 (25.0) | 2 (33.3) | 2 (100.0) | 4 (50.0) | 3 (42.9) |
| Health Insurance | ||||||
| Medicare | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 1 (14.3) |
| Medicaid | 1 (50.0) | 6 (75.0) | 3 (50.0) | 0 (0.0) | 4 (50.0) | 3 (42.9) |
| Employer | 1 (50.0) | 2 (25.0) | 2 (33.3) | 2 (100.0) | 4 (50.0) | 3 (42.9) |
| Psychological and Behavioral health | ||||||
| Unhealthy alcohol use1 | 1 (50.0) | 1 (12.5) | 1 (16.7) | 0 (0.0) | 3 (37.5) | 4 (57.1) |
| Substance use2 | 0 (0.0) | 1 (12.5) | 1 (16.7) | 0 (0.0) | 1 (12.5) | 0 (0.0) |
| PHQ-2 ≥ 3 | 0 (0.0) | 2 (25.0) | 3 (50.0) | 0 (0.0) | 1 (12.5) | 2 (28.6) |
| GAD-2 ≥ 3 | 1 (50.0) | 4 (50.0) | 3 (50.0) | 2 (100.0) | 3 (37.5) | 4 (57.1) |
| Tobacco use characteristics | ||||||
| Cigarettes per day-Mean [SD] | 13.0 [9.9] | 13.6 [6.0] | 20.0 [12.6] | 10.0 [0.0] | 15.1 [7.2] | 16.9 [6.4] |
| Ready to quit in the next 30 days | 2 (100.0) | 6 (75.0) | 5 (83.3) | 2 (100.0) | 6 (75.0) | 6 (85.7) |
| Time to first cigarette <=30 min | 2 (100.0) | 6 (75.0) | 4 (66.7) | 0 (0.0) | 5 (62.5) | 4 (57.1) |
| Confidence of quit3-Mean [SD] | 7.5 [0.7] | 3.8 [2.6] | 6.8 [1.9] | 9.5 [0.7] | 5.3 [2.1] | 4.1 [3.0] |
| Importance of quit3-Mean [SD] | 10.0 [0.0] | 8.4 [2.7] | 9.3 [1.6] | 9.5 [0.7] | 8.9 [1.5] | 8.1 [1.9] |
| Distress3-Mean [SD] | 8.5 [2.1] | 5.8 [3.2] | 8.3 [2.1] | 7.0 [1.4] | 6.0 [2.8] | 8.3 [2.0] |
| Technology use characteristics | ||||||
| Unlimited Texting plan | 2 (100.0) | 6 (75.0) | 5 (83.3) | 2 (100.0) | 7 (87.5) | 7 (100.0) |
| Text Messages/Day-Mean [SD] | 16.0 [19.8] | 11.5 [9.8] | 10.2 [10.2] | 35.0 [21.2] | 42.1 [65.6] | 12.0 [9.6] |
Abbreviations: R1-first randomization, 4- vs 8-weeks; R2-second randomization. NRT vs NRT+coaching; NRT=nicotine replacement therapy, SD=standard deviation; PHQ-2=Patient Health Questionnaire 2-item score; GAD-2=General Anxiety Disorder 2-item score.
Excluding n=2 participants who withdrew among 35 enrolled.
Subjects who were not in second randomization due to having quit with initial text message program or loss to follow-up before R2.
Single-Question Alcohol Screening Test (Smith 2009);
Single-Question Screening Test for Drug Use (Smith 2010);
11- Item Likert Scales for motivation to quit, confidence to quit, and perceived 2-week distress.
5.2. SMS fidelity
Thirteen percent (n=4) of participants used the keyword HELP. Message failures occurred with four of 33 participants (2 messages failed/127 total messages, 92/239, 71/184, 2/85). The two participants with 92 and 71 failed messages (97.6% of the total failed messages) reported their phone plans were disconnected for up to three weeks during the study.
5.3. Intervention engagement
We show measures of SMS engagement in Table 2a. Active days in the program, messages sent by the participant, and responses to NRT queries did not differ between groups. After entering an initial quit date in the program, one person in the 4-week assessment group reset their quit date and six in the 8-week assessment group reset their quite date during the study.
Table 2a.
Engagement with text message (SMS) intervention by early vs. late assessment, (N=33)
| Early 4-week assessment group (N=16) | Late 8-week assessment group (N=17) | p 2 | |
|---|---|---|---|
| Mean [SD] | |||
| Text message engagement | |||
| Active days in SMS program1 | 64.4 [21.7] | 77.5 [18.6] | 0.07 |
| No. of SMS sent from participant | 27.6 [21.4] | 38.5 [58.2] | 0.48 |
| No. of URL links clicked | 6.2 [7.9] | 4.4 [8.8] | 0.71 |
| Ratio of URL links clicked/links sent | 0.5 [0.5] | 0.2 [0.4] | 0.36 |
| NRT use SMS queries responded to | 7.3 [6.6] | 7.8 [8.6] | 0.85 |
| Ratio of NRT use queries responded to/NRT queries sent | 0.4 [0.6] | 0.5 [0.4] | 0.52 |
Days from first to last messages sent from participant
P values based on t-test
Abbreviations: SMS=text messages (short message service); SD=standard deviation; NRT=nicotine replacement therapy; URL=uniform resource locator
Engagement with NRT treatment following R2 is displayed in Table 2b. Any NRT use during the study was reported by 87.5% (n=14, 95%CI [61.7, 98.5]) of participants randomized to NRT and 84.6% (n=11, 95%CI [54.6, 98.1]) of participants randomized to NRT + coaching (p=1.00). Telephone coaching, averaging 12.8 minutes (SD 3.8) in duration, was delivered to 92.3% (n=12, 95%CI [64.0, 99.8]; n=1 declined coaching) of participants in the NRT + coaching group. On average, coaching occurred 1.2 days after R2.
Table 2b.
Engagement with NRT and telephone coaching, (N=29)
| NRT (N=16) | NRT + telephone coaching (N=13) | P | |
|---|---|---|---|
| Mean [SD]/N (%) | |||
| NRT engagement | |||
| Any past week use of NRT | 10 (62.5) | 8 (61.5) | 1.001 |
| Days of NRT use in past week among NRT users (n=18) | 5.4 [2.3] | 5.6 [2.5] | 0.892 |
| Any NRT use during study | 1.001 | ||
| Patch | 3 (18.8) | 2 (15.4) | |
| Lozenge | 6 (37.5) | 4 (30.8) | |
| Combination NRT | 5 (31.3) | 5 (38.5) | |
| None | 2 (12.5) | 2 (15.4) | |
| Coaching engagement | |||
| Completed coaching session | -- | 12 (92.3) | -- |
P value based on Fisher’s exact test
P value based on t-test
Abbreviations: NRT=nicotine replacement therapy; SD=standard deviation
5.4. Acceptability
Overall, 93.3% (n=28, 95%CI [77.9, 99.2]) of the 30 participants who completed the 12-week survey reported being somewhat or very satisfied with their treatment (Table 3). Selecting “Somewhat” or “Completely agree” with the statements that the study gave them confidence to quit, made quitting feel worthwhile, made them feel that someone cared, and that they knew the right steps to take to quit did not differ by group.
Table 3.
Tobacco use outcomes by group, (N=30)
| Early assessment-4 weeks | Late assessment-8 weeks | 4- vs. 8-weeks | NRT vs. NRT + coaching | ||||
|---|---|---|---|---|---|---|---|
| Quit before assessment | NRT | NRT + coaching | NRT | NRT + coaching | |||
| Overall | N=2 | N=8 | N=5 | N=8 | N=7 | p1 | p1 |
| N (%) / Mean [SD] | |||||||
| Smoking cessation outcomes | |||||||
| 7-day PPA, week 12 | 1 (50.0) | 0 (0.0) | 1 (20.0) | 4 (50.0) | 1 (14.3) | 0.39 | 0.67 |
| 7-day PPA, week 8 | -- | ||||||
| CO <8 ppm, week 12 | 1 (50.0) | 0 (0.0) | 1 (20.0) | 3 (37.5) | 1 (14.3) | 0.65 | 1.00 |
| Any quit attempt ≥24 hours | 2 (100) | 7 (87.5) | 4 (80.0) | 6 (75.0) | 6 (85.7) | 1.00 | 1.00 |
| No. of quit attempts | 2.0 [1.4] | 5.1 [3.9] | 3.3 [1.7] | 3.0 [1.4] | 2.7 [1.5] | 0.19 | 0.20 |
| % Past 30 days with no smoking, week 12 | 23.5 [2.1] | 4.8 [4.0] | 1.8 [1.6] | 11.8 [10.6] | 14.1 [12.3] | 0.07 | 0.85 |
| Change in cigarettes/day4 | −13.0 [9.9] | −7.0 [7.3] | −7.2 [7.7] | −12.5 [9.3] | −4.7 [7.3] | 0.74 | 0.19 |
| Cigarettes/day, week12 | 0.0 [0.0] | 6.6 [6.1] | 10.8 [16.5] | 2.6 [4.1] | 12.1 [8.6] | 0.98 | 0.079 |
| Smoking cessation treatment use | |||||||
| Any NRT during the study | 1 (50.0) | 8 (100) | 5 (100) | 7 (87.5) | 6 (85.7) | 1.00 | 1.00 |
| Psychosocial outcomes | |||||||
| Change in importance of quitting5 | 0 [0.0] | 0.5 [1.5] | −2.0 [1.9] | −1.6 [1.8] | 0.1 [0.4] | 0.54 | 0.78 |
| Change in confidence of quitting5 | −1.5 [0.0] | 0.8 [3.4] | −2.2 [1.6] | 0.4 [3.9] | 1.1 [2.9] | 0.33 | 0.51 |
| Change in distress5 | −6.5 [4.9] | −0.9 [3.9] | −0.4 [1.1] | 1.3 [2.4] | 0.1 [1.8] | 0.06 | 0.77 |
| Satisfaction/Participant experience | |||||||
| Satisfaction with treatment “Very satisfied” “Somewhat satisfied” |
2 (100) 0 (0) |
5 (62.5) 2 (25.0) |
3 (60.0) 2 (40.0) |
5 (62.5) 2 (25.0) |
4 (57.1) 3 (42.9) |
1.00 | 1.00 |
| Study gave me confidence to quit6 | 2 (100) | 7 (87.5) | 4 (80.0) | 5 (62.5) | 6 (85.7) | 0.84 | 0.74 |
| Study made quitting feel worthwhile6 | 2 (100) | 7 (87.5) | 5 (100) | 7 (87.5) | 5 (100) | 0.05 | 0.61 |
| Study made me feel someone cared6 | 2 (100) | 6 (75.0) | 3 (60.0) | 6 (75.0) | 6 (87.5) | 0.20 | 0.59 |
| Study made me feel I knew how to quit6 | 2 (100) | 7 (87.5) | 4 (80.0) | 6 (75.0) | 7 (100) | 0.65 | 0.95 |
p-value based on t-test or Fisher’s exact test
“Very satisfied” or “Somewhat satisfied”
“Completely agree” or “Somewhat agree”
Change in self-reported cigarettes per day from baseline to week 12
Change from baseline to week 12 single-item 11-point Likert scales for motivation to quit, confidence to quit, and past two-week distress,
“Completely agree” or “Somewhat agree”
Abbreviations: NRT=Nicotine replacement therapy; SD=standard deviation; 7-day PPA=self-reported 7-day point prevalence abstinence; CO=carbon monoxide
5.5. Smoking cessation outcomes
At 12-weeks, 13% (n=2) of the 4-week group and 33% (n=5) in the 8-week assessment reported 7-day PPA (p=0.39), and 13% (n=2) and 27% (n=4) had CO<6ppm, respectively (Table 3). Of those mailed NRT (R2), 19% (n=3) had CO<6ppm without coaching vs. 17% (n=2) with coaching (p=1.00). Participants with CO<6ppm were active in the SMS program for longer (87.8 vs. 71.2 days) and sent more texts back to the program (56.5 messages vs. 30.7 messages).
5.6. Treatment component interaction
ANOVA models and Cochran-Mantel-Haenszel tests of smoking cessation and treatment use outcomes did not show a significant interaction between 4- versus 8-week assessment and NRT versus NRT + coaching except for the outcome of change in importance of quitting. Importance of quitting decreased, on average in both early (mean change −0.4, 95%CI [−1.4, 0.6]) and late assessment groups (mean change −0.8, 95%CI [−1.7, 0.1]). Within assessment groups, those randomized to NRT + coaching had a decrease in importance of quitting in the early assessment participants (−2.0, 95%CI [−4.3, 0.3]) and a small increase in importance of quitting in Late assessment participants (0.1, 95%CI [−0.2, 0.5]) (p<0.001).
5.7. Qualitative treatment experience
Most participants viewed the SMS favorably. Many participants reported that the messages made them feel supported and kept them on track. In terms of the adaptive treatment program, participants described how the SMS reinforced other treatment components.
“Both the information in the texts and from the coaching session that I got where the smoking coach, you, had said to me, “People who do one or the other in addition to just willpower succeed at a higher rate.” So, both the text messages reinforced that positive benefit, and your coaching session” [Late assessment/NRT + Coaching].
Participants also noted that the SMS plus other treatments together made them feel especially supported.
“the whole program helped me to stop smoking. The text messages might have helped a little. The lozenges and the nicotine patches took the cravings away, so I don’t think it was directly the text messages. Receiving those reminded me of the program that I was in all the time and then knowing that I was going to be talking to you, so overall, the program definitely helped me” [Early assessment/NRT].
Others mentioned how live calls with study staff led them to associate the messages with a live person which made the messages more meaningful.
“Even though I know they’re not, but I always thought, in the back of my mind, it was you texting, or there was someone else texting, so. So, I thought that was important because knowing that it goes to that fact that, hey, somebody cares that you’re doing something, and you’re worthwhile” [Late assessment, NRT].
Some participants viewed the SMS less favorably and wanted more interaction, such as having someone to connect with in the moment when they were struggling.
“I didn’t have the option to—not that you have to reply, but you can only reply with certain words and get a response back. So maybe more interactive like a actual—I don’t know if it’s a computer or how it works or if it’s a actual person that you can text back at midnight like, “I’m just getting the urge.” …So if you have someone that you can be like, “Okay, I’m not thinking right,” just like AA” [Early assessment/NRT].
6. Discussion
A SMART examining adaptive cessation treatment timing and treatment components was feasible in a sample of primary care patients who smoke daily. Treatment retention and fidelity of all interventions including SMS, NRT, and coaching, were high and smoking cessation outcomes were promising. Very few studies have tested adaptive smoking cessation treatment programs. Two other published SMART trials studied systems-level or multi-level interventions, while our study examined the feasibility of an individual-level adaptive treatment design (Fernandez et al., 2020; Fu et al., 2017). Our program uptake, at 34% among those eligible, was comparable to other proactive smoking cessation treatment models. For example, a 2014 study of VA patients who smoked found 469 (30%) of 1,556 patients proactively outreached, accepted connection with treatment (Fu et al., 2014). SMS intervention fidelity was high apart from two participants who lost phone service during the study. Retention in the 12-week study, at 86%, was particularly promising considering the pandemic context where stress and inability to access social supports may have made quitting especially challenging (Joyce et al., 2021; Rosoff-Verbit et al., 2021).
Our preliminary cessation measures showed 7-day PPA was highest among individuals who were offered mailed NRT after 8 weeks of SMS. In terms of the timing of assessment, it may be that the longer period of time with the SMS program supported users to develop more skills to apply to their quit attempt by the time the NRT was offered. Although combined treatment with behavioral support and pharmacotherapy is best practice, we know little about whether individuals should be encouraged to start behavioral therapy or pharmacotherapy sequentially or concurrently. This pilot study demonstrates the feasibility and promise of a study design testing the effectiveness of offering digital behavioral therapy for a brief period prior to pharmacotherapy.
In terms of comparing NRT with NRT + coaching, it may be that more intensive telephone coaching, which was beyond the resources of this pilot study, is needed to improve cessation outcomes for those who need more help (Hejjaji et al., 2021). Although the addition of brief coaching did not yield improved cessation outcomes, it is notable that 100% of those in the NRT + coaching groups reported satisfaction with treatment, that the study made quitting feel worthwhile, and that they knew the steps to take to quit.
Most participants agreed that the study gave them confidence to quit, made quitting feel worthwhile, made them feel someone cared, and made them feel they knew the right steps to take. These responses suggest that with a program that starts with SMS may promote self-efficacy, motivation, and improve participants’ behavioral skills to quit. Our qualitative results suggest the addition of the live interaction may complement the SMS in enhancing perceptions of social support. A primary care peer navigator or case manager could serve in this role, but further research is needed to measure the added effects of a program with live interaction versus a fully automated intervention. Cost is also an important consideration in designing adaptive interventions where more expensive interventions could be reserved for only those who need them. A recent cost-effectiveness study of NRT sampling, a potential alternative initial treatment to SMS in a stepped-care intervention, measured NRT sampling costs at $75 per person (Chen, Silvestri, Dahne, Lee, & Carpenter, 2022). Costs of an SMS program vary depending on the program, but prior analyses estimate SMS cost per person between $18 and $74 per person (Guerriero et al., 2013).
6.1. Limitations
Our study had several limitations. The study relied on self-report alone to assess smoking status at baseline, 4- and 8-weeks. The study may have misclassified smoking status at R1 or R2. The research coordinator was unblinded and this could also introduce bias. The majority of participants were white and highly educated, which limits the generalizability of this single-site study. This pilot study period was insufficient to assess long-term smoking abstinence. However, 12-week cessation rates were encouraging, particularly given the low confidence in quitting in our sample and the study timeframe overlapping with the early COVID-19 pandemic. The pandemic context may also have produced different treatment experiences for some patients, particularly older patients, as we report separately (Joyce et al., 2021). With our small sample size in this proof of concept pilot we were not powered to measure differences in cessation outcomes by study arm. However, participants completed study activities in five of the six outcome groups, demonstrating the feasibility of the sequential randomization methods and excellent retention rates (>80%).
7. Conclusion
A SMART examining an adaptive treatment regimen combining SMS, NRT, and coaching for primary care patients who had high importance of quitting but only moderate confidence during the COVID-19 pandemic was feasible. The treatment program overall produced promising effects on cessation. Retention and satisfaction with the adaptive treatment model were high and quit rates were promising at 12 weeks. Our qualitative results suggested live interactions during the study may have conferred social support, but we saw no differences in the NRT + coaching arm versus NRT only. Our pilot results support the feasibility of this adaptive tobacco cessation treatment model and highlight the need to understand how to best tailor combination treatments to meet the changing needs of primary care patients, and to compare efficient, convenient automated interventions with interventions involving live interactions, in primary care settings.
Supplementary Material
Highlights.
A SMART combining SMS, NRT and coaching was feasible among primary care patients.
Satisfaction with the adaptive interventions was especially high with brief coaching.
A trial of sequential treatment including SMS and NRT shows promise.
FUNDING
This work is funded by the Massachusetts General Hospital Department of Medicine Transformative Scholars Award and the National Institute on Drug Abuse K23 DA038717.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DECLARATION OF INTERESTS
GK has a family financial interest in a mobile health company, Dimagi, Inc.
REFERENCES
- Almirall D, Compton SN, Gunlicks-Stoessel M, Duan N, & Murphy SA (2012). Designing a pilot sequential multiple assignment randomized trial for developing an adaptive treatment strategy. Stat Med, 31(17), 1887–1902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almirall D, Compton SN, Gunlicks-Stoessel M, Duan N, & Murphy SA (2012). Designing a pilot sequential multiple assignment randomized trial for developing an adaptive treatment strategy. Statistics in medicine, 31(17), 1887–1902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almirall D, Nahum-Shani I, Sherwood NE, & Murphy SA (2014). Introduction to SMART designs for the development of adaptive interventions: with application to weight loss research. Translational behavioral medicine, 4(3), 260–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almirall D, Nahum-Shani I, Sherwood NE, & Murphy SA (2014). Introduction to SMART designs for the development of adaptive interventions: with application to weight loss research. Transl Behav Med, 4(3), 260–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babb S, Malarcher A, Schauer G, Asman K, & Jamal A (2017). Quitting Smoking Among Adults - United States, 2000-2015. MMWR Morb Mortal Wkly Rep, 65(52), 1457–1464. [DOI] [PubMed] [Google Scholar]
- Bedfont. iCO™ Smokerlyzer user manual. Retrieved from: https://www.bedfont.com/documents/iCO-Smokerlyzer-manual.pdf. (Accessed March 25th 2021).
- Benowitz NL, Bernert JT, Foulds J, Hecht SS, Jacob P III, Jarvis MJ, … Piper ME (2020). Biochemical verification of tobacco use and abstinence: 2019 update. Nicotine and Tobacco Research, 22(7), 1086–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter MJ, Hughes JR, Gray KM, Wahlquist AE, Saladin ME, & Alberg AJ (2011). Nicotine therapy sampling to induce quit attempts among smokers unmotivated to quit: a randomized clinical trial. Arch Intern Med, 171(21), 1901–1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen B, Silvestri GA, Dahne J, Lee K, & Carpenter MJ (2022). The Cost-Effectiveness of Nicotine Replacement Therapy Sampling in Primary Care: a Markov Cohort Simulation Model. J Gen Intern Med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen E, Feinn R, Arias A, & Kranzler HR (2007). Alcohol treatment utilization: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend, 86(2-3), 214–221. [DOI] [PubMed] [Google Scholar]
- Ebbert JO, Little MA, Klesges RC, Bursac Z, Johnson KC, Thomas F, & Vander Weg MW (2017). Step Care treatment for smoking cessation. Health Educ Res, 32(1), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edelman EJ, Dziura J, Deng Y, Bold KW, Murphy SM, Porter E, … Bernstein SL (2021). A SMARTTT approach to Treating Tobacco use disorder in persons with HIV (SMARTTT): Rationale and design for a hybrid type 1 effectiveness-implementation study. Contemp Clin Trials, 110, 106379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez ME, Schlechter CR, Del Fiol G, Gibson B, Kawamoto K, Siaperas T, … Wetter DW (2020). QuitSMART Utah: an implementation study protocol for a cluster-randomized, multi-level Sequential Multiple Assignment Randomized Trial to increase Reach and Impact of tobacco cessation treatment in Community Health Centers. Implement Sci, 15(1), 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, … Wewers ME (2008). Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service. [Google Scholar]
- Fisher WA, Fisher JD, & Harman J (2003). The information-motivation-behavioral skills model: A general social psychological approach to understanding and promoting health behavior. Social psychological foundations of health and illness, 22, 82–106. [Google Scholar]
- Fu SS, Rothman AJ, Vock DM, Lindgren B, Almirall D, Begnaud A, … Joseph AM (2017). Program for lung cancer screening and tobacco cessation: Study protocol of a sequential, multiple assignment, randomized trial. Contemp Clin Trials, 60, 86–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu SS, van Ryn M, Sherman SE, Burgess DJ, Noorbaloochi S, Clothier B, … Joseph AM (2014). Proactive tobacco treatment and population-level cessation: a pragmatic randomized clinical trial. JAMA Intern Med, 174(5), 671–677. [DOI] [PubMed] [Google Scholar]
- Glaser BG, & Strauss AL (2017). Discovery of grounded theory: Strategies for qualitative research: Routledge. [Google Scholar]
- Guerriero C, Cairns J, Roberts I, Rodgers A, Whittaker R, & Free C (2013). The cost-effectiveness of smoking cessation support delivered by mobile phone text messaging: Txt2stop. Eur J Health Econ, 14(5), 789–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Head KJ, Noar SM, Iannarino NT, & Harrington NG (2013). Efficacy of text messaging-based interventions for health promotion: a meta-analysis. Social science & medicine, 97, 41–48. [DOI] [PubMed] [Google Scholar]
- Hebert ET, Ra CK, Alexander AC, Helt A, Moisiuc R, Kendzor DE, … Businelle MS (2020). A Mobile Just-in-Time Adaptive Intervention for Smoking Cessation: Pilot Randomized Controlled Trial. J Med Internet Res, 22(3), e16907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hejjaji V, Khetan A, Hughes JW, Gupta P, Jones PG, Ahmed A, … Josephson RA (2021). A combined community health worker and text messagingbased intervention for smoking cessation in India: Project MUKTI - A mixed methods study. Tob Prev Cessat, 7, 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoeppner BB, Hoeppner SS, & Abroms LC (2017). How do text- messaging smoking cessation interventions confer benefit? A multiple mediation analysis of Text2Quit. Addiction, 112(4), 673–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamal A, Phillips E, Gentzke AS, Homa DM, Babb SD, King BA, & Neff LJ (2018). Current cigarette smoking among adults—United States, 2016. Morbidity and Mortality Weekly Report, 67(2), 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joyce AA, Styklunas GM, Rigotti NA, Neil JM, Park ER, & Kruse GR (2021). Quit Experiences among Primary Care Patients Enrolled in a Smoking Cessation Pilot RCT Early in the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 18(3), 1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruse G, Park ER, Shahid NN, Abroms L, Haberer JE, & Rigotti NA (2019). Combining real-time ratings with qualitative interviews to develop a smoking cessation text messaging program for primary care patients. JMIR mHealth and uHealth, 7(3), e11498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruse GR, Park ER, Chang Y, Haberer JE, Abroms LC, Shahid NN, … Rigotti NA (2020). Proactively offered text messages and mailed nicotine replacement therapy for smokers in primary care practices: A pilot randomized trial. Nicotine Tob Res. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKellar J, Austin J, & Moos R (2012). Building the first step: a review of low-intensity interventions for stepped care. Addict Sci Clin Pract, 7, 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy SA, Collins LM, & Rush AJ (2007). Customizing treatment to the patient: adaptive treatment strategies. Drug Alcohol Depend, 88 Suppl 2, S1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- QSR International Pty Ltd. NVivo (Version 12). (2018). Retrieved from: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home. (Accessed.
- Ritchie J, L. J, McNaughton Nicholls C, Ormston R (2013). Qualitative research practice: a guide for social science students and researchers. (2nd ed.). London: Sage. [Google Scholar]
- Rosoff-Verbit Z, Logue-Chamberlain E, Fishman J, Audrain-McGovern J, Hawk L, Mahoney M, … Ashare R (2021). The Perceived Impact of COVID-19 among Treatment-Seeking Smokers: A Mixed Methods Approach. Int J Environ Res Public Health, 18(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott-Sheldon LA, Lantini R, Jennings EG, Thind H, Rosen RK, Salmoirago-Blotcher E, & Bock BC (2016). Text Messaging-Based Interventions for Smoking Cessation: A Systematic Review and Meta-Analysis. JMIR Mhealth Uhealth, 4(2), e49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- smokefree.gov. SmokefreeTXT. March 25th 2021).
- Spohr SA, Nandy R, Gandhiraj D, Vemulapalli A, Anne S, & Walters ST (2015). Efficacy of SMS Text Message Interventions for Smoking Cessation: A Meta-Analysis. J Subst Abuse Treat, 56, 1–10. [DOI] [PubMed] [Google Scholar]
- Substance, A., Mental, H. S. A. U., & General, O. o. t. S. (2020). Smoking Cessation: A Report of the Surgeon General. [Google Scholar]
- Tobacco Treatment Specialist (TTS) Core Training, University of Massachusetts Medical school. Retrieved from: https://www.umassmed.edu/tobacco/training/ttscore/. (Accessed February 17 2021).
- Verification, S. S. o. B. (2002). Biochemical verification of tobacco use and cessation. Nicotine Tob Res. 4, 149–159. [DOI] [PubMed] [Google Scholar]
- Whittaker R, McRobbie H, Bullen C, Rodgers A, & Gu Y (2016). Mobile phone- based interventions for smoking cessation. Cochrane database of systematic reviews(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


